Early Onset Epilepsy Caused by Low-Grade Epilepsy-Associated Tumors and Focal Meningeal Involvement
Abstract
:1. Introduction
2. Materials and Methods
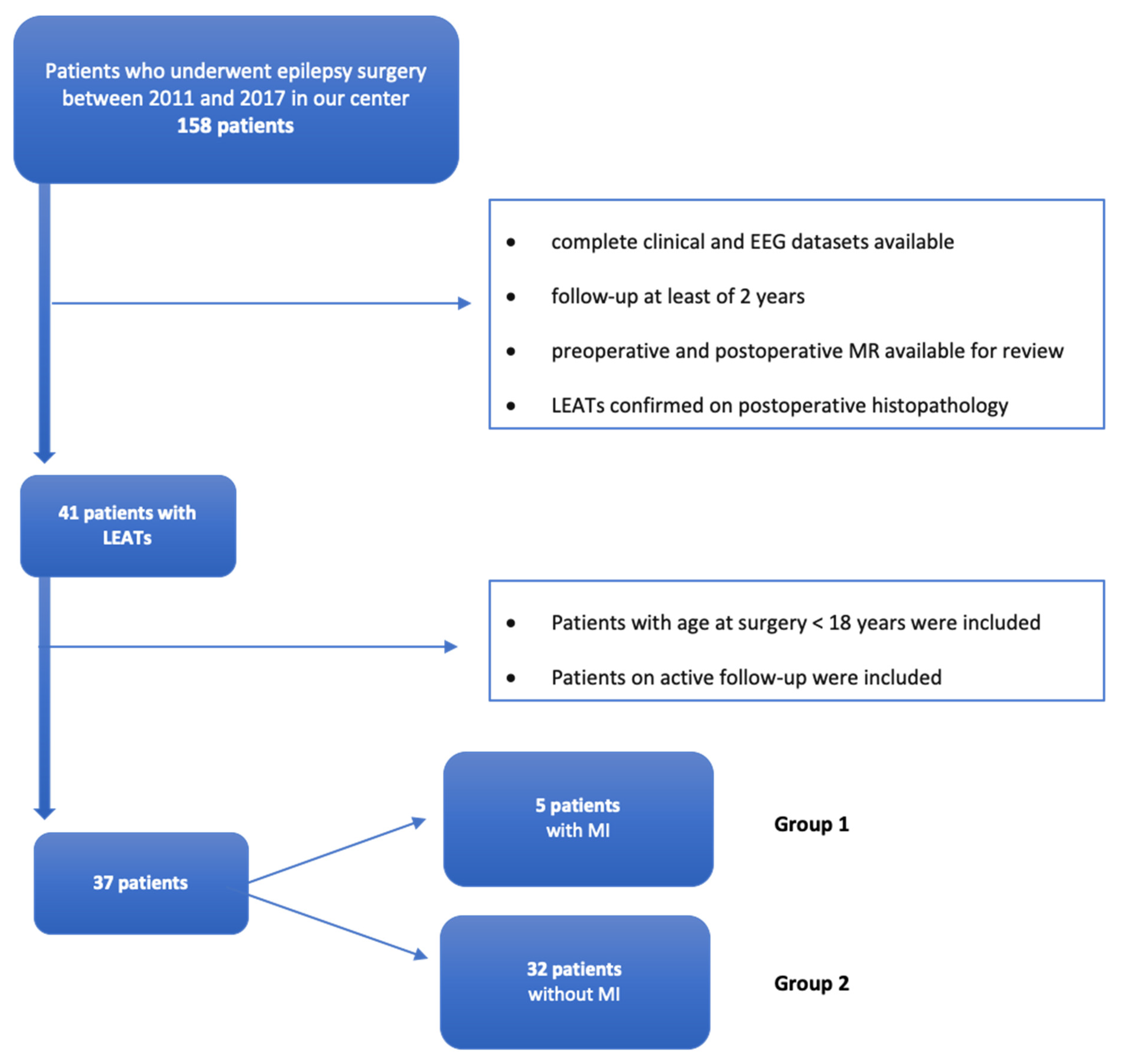
2.1. Patients Selection
2.2. Presurgical Evaluations
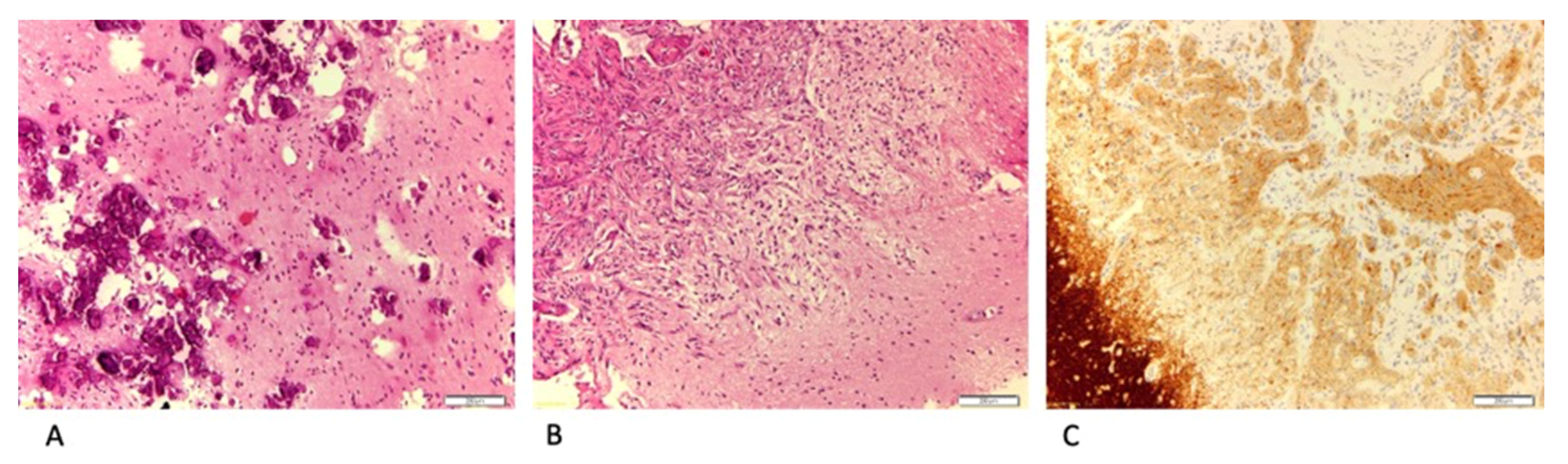
2.3. Surgical Procedures and Histopathological Diagnosis
2.4. Follow-Up and Surgical Outcomes
3. Results
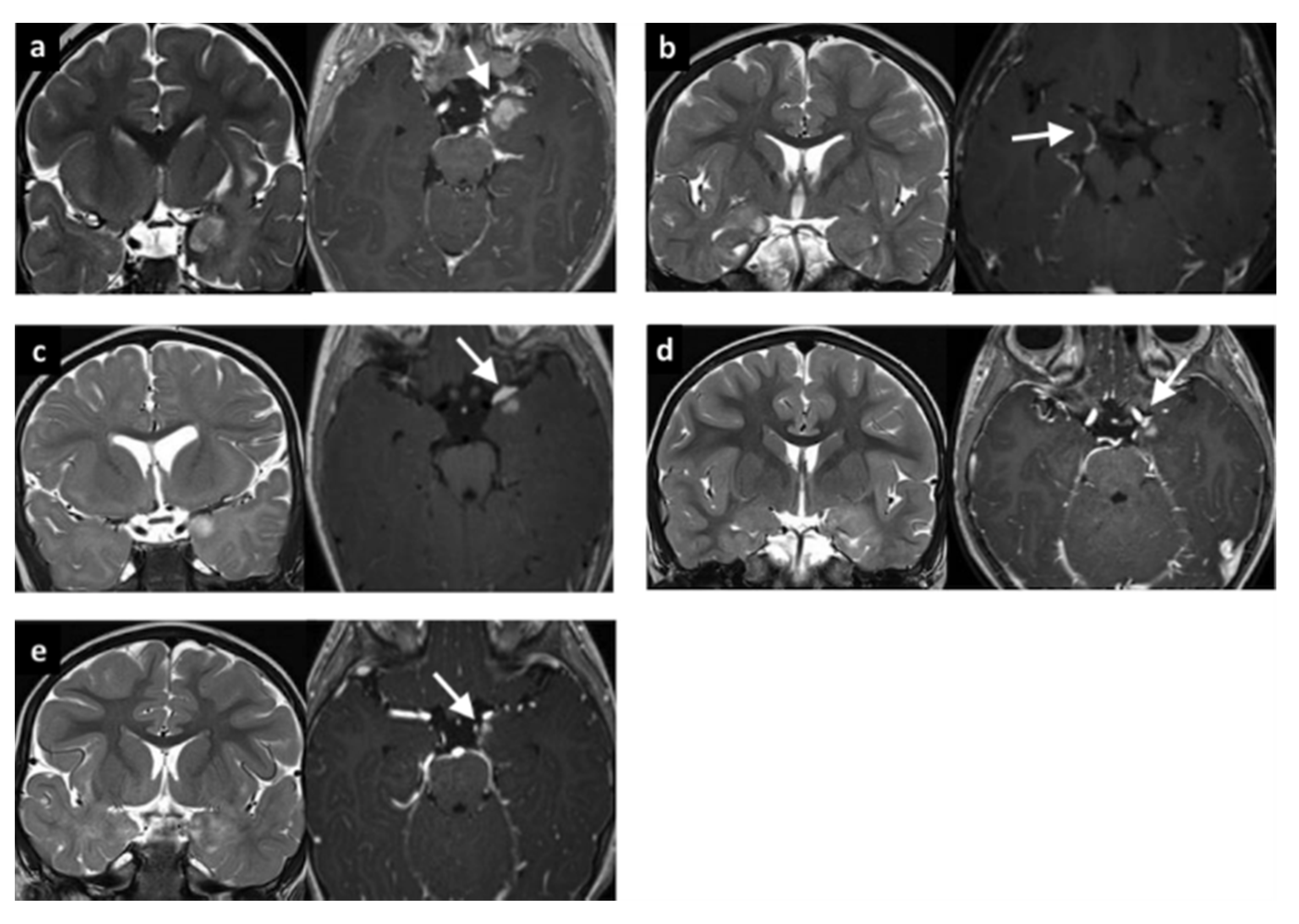
3.1. LEATs with MI (Group 1)
3.2. LEATs without MI (Group 2)
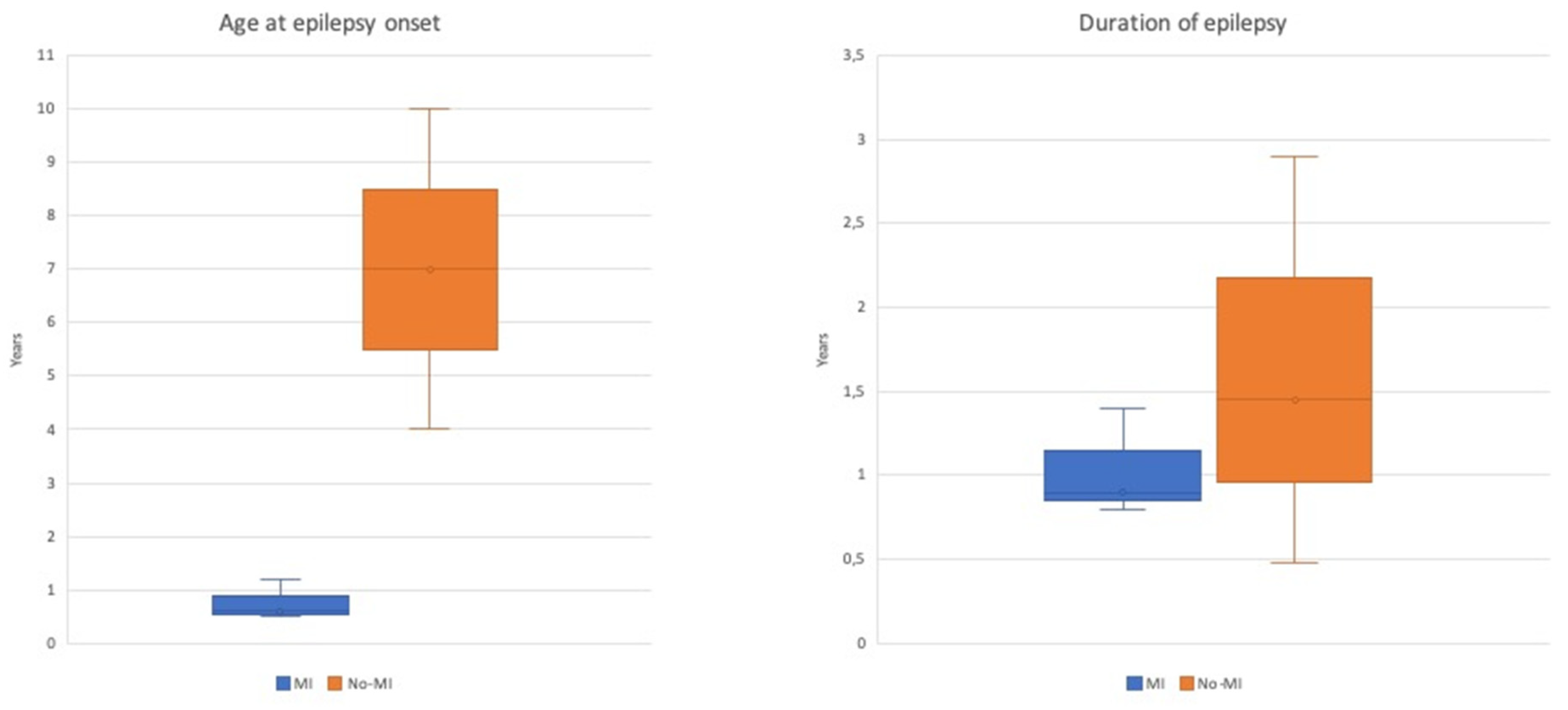
3.3. Comparison between Group 1 and Group 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Babini, M.; Giulioni, M.; Galassi, E.; Marucci, G.; Martinoni, M.; Rubboli, G.; Volpi, L.; Zucchelli, M.; Nicolini, F.; Marliani, A.F.; et al. Seizure outcome of surgical treatment of focal epilepsy associated with low-grade tumors in children. J. Neurosurg. Pediatr. 2013, 11, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Aronica, E.; Leenstra, S.; Van Veelen, C.W.; Van Rijen, P.C.; Hulsebos, T.J.; Tersmette, A.C.; Yankaya, B.; Troost, D. Glioneuronal tumors and medically intractable epilepsy: A clinical study with long-term follow-up of seizure outcome after surgery. Epilepsy Res. 2001, 43, 179–191. [Google Scholar] [CrossRef]
- Minkin, K.; Klein, O.; Mancini, J.; Lena, G. Surgical strategies and seizure control in pediatric patients with dysembryoplastic neuroepithelial tumors: A single-institution experience. J. Neurosurg. Pediatr. 2008, 1, 206–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takahashi, A.; Hong, S.-C.; Seo, D.W.; Lee, M.; Suh, Y.-L.; Hong, S.B. Frequent association of cortical dysplasia in dysembryoplastic neuroepithelial tumor treated by epilepsy surgery. Surg. Neurol. 2005, 64, 419–427. [Google Scholar] [CrossRef]
- Englot, D.J.; Chang, E.F.; Vecht, C.J. Epilepsy and brain tumors. Handb. Clin. Neurol. 2016, 134, 267–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thom, M.; Blümcke, I.; Aronica, E. Long-Term Epilepsy-Associated Tumors. Brain Pathol. 2012, 22, 350–379. [Google Scholar] [CrossRef] [PubMed]
- Blumcke, I.; Aronica, E.; Urbach, H.; Alexopoulos, A.; Gonzalez-Martinez, J.A. A neuropathology-based approach to epilepsy surgery in brain tumors and proposal for a new terminology use for long-term epilepsy-associated brain tumors. Acta Neuropathol. 2014, 128, 39–54. [Google Scholar] [CrossRef] [Green Version]
- Racz, A.; Müller, A.-M.; Schwerdt, J.; Becker, A.; Vatter, H.; Elger, C.E. Age at epilepsy onset in patients with focal cortical dysplasias, gangliogliomas and dysembryoplastic neuroepithelial tumours. Seizure 2018, 58, 82–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faramand, A.M.; Barnes, N.; Harrison, S.; Gunny, R.; Jacques, T.; Tahir, Z.M.; Varadkar, S.; Cross, H.J.; Harkness, W.; Tisdall, M. Seizure and cognitive outcomes after resection of glioneuronal tumors in children. Epilepsia 2017, 59, 170–178. [Google Scholar] [CrossRef] [Green Version]
- Pelliccia, V.; DeLeo, F.; Gozzo, F.; Sartori, I.; Mai, R.; Cossu, M.; Tassi, L. Early and late epilepsy surgery in focal epilepsies associated with long-term epilepsy-associated tumors. J. Neurosurg. 2017, 127, 1147–1152. [Google Scholar] [CrossRef] [Green Version]
- Englot, D.J.; Berger, M.S.; Barbaro, N.M.; Chang, E.F. Factors associated with seizure freedom in the surgical resection of glioneuronal tumors. Epilepsia 2011, 53, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Tomita, T.; Volk, J.M.; Shen, W.; Pundy, T. Glioneuronal tumors of cerebral hemisphere in children: Correlation of surgical resection with seizure outcomes and tumor recurrences. Child’s Nerv. Syst. 2016, 32, 1839–1848. [Google Scholar] [CrossRef] [PubMed]
- Taillibert, S.; Chamberlain, M. Leptomeningeal metastasis. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2018; pp. 169–204. [Google Scholar] [CrossRef]
- Dapaah, A.; Biswas, S.; Srikandarajah, N.; Crooks, D.; Das, K.; Farah, J.O. Serial imaging and management of ganglioglioma with unusual presentation and meningeal spread. Acta Neurochir. 2016, 159, 481–483. [Google Scholar] [CrossRef] [PubMed]
- Perilongo, G.; Garrè, M.L.; Giangaspero, F. Low-grade gliomas and leptomeningeal dissemination: A poorly understood phenomenon. Child’s Nerv. Syst. 2003, 19, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Riesberg, G.; Bathla, G.; Gupta, S.; Watal, P.; Moritani, T. Malignant transformation and leptomeningeal spread of recurrent ganglioglioma: Case report and review of literature. Clin. Imaging 2018, 48, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Scheffer, I.E.; Berkovic, S.; Meletti, S.; Connolly, M.B.; French, J.; Guilhoto, L.; Hirsch, E.; Jain, S.; Mathern, G.W.; Moshé, S.L.; et al. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia 2017, 58, 512–521. [Google Scholar] [CrossRef] [Green Version]
- Louis, D.N.; Perry, A.; Reifenberger, G.; Von Deimling, A.; Figarella-Branger, D.; Cavenee, W.K.; Ohgaki, H.; Wiestler, O.D.; Kleihues, P.; Ellison, D.W. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: A summary. Acta Neuropathol. 2016, 131, 803–820. [Google Scholar] [CrossRef] [Green Version]
- Blümcke, I.; Thomas, J.; Aronica, E.; Armstrong, D.D.; Vinters, H.V.; Palmini, A.; Jacques, T.S.; Avanzini, G.; Barkovich, A.J.; Battaglia, G.; et al. The clinicopathologic spectrum of focal cortical dysplasias: A consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission 1. Epilepsia 2010, 52, 158–174. [Google Scholar] [CrossRef] [Green Version]
- Blumcke, I.; Thom, M.; Aronica, E.; Armstrong, D.D.; Bartolomei, F.; Bernasconi, A.; Bernasconi, N.; Bien, C.G.; Cendes, F.; Coras, R.; et al. International consensus classification of hippocampal sclerosis in temporal lobe epilepsy: A Task Force report from the ILAE Commission on Diagnostic Methods. Epilepsia 2013, 54, 1315–1329. [Google Scholar] [CrossRef]
- Engel, J.J.; Van Ness, P.C.; Rasmussen, T.B.; Ojemann, L.M. Outcome with respect to epileptic seizures. In Surgical Treatment of the Epilepsies; 1993. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3854719/ (accessed on 15 September 2013).
- Giulioni, M.; Marucci, G.; Cossu, M.; Tassi, L.; Bramerio, M.; Barba, C.; Buccoliero, A.M.; Vornetti, G.; Zenesini, C.; Consales, A.; et al. CD34 Expression in Low-Grade Epilepsy-Associated Tumors: Relationships with Clinicopathologic Features. World Neurosurg. 2019, 121, e761–e768. [Google Scholar] [CrossRef] [PubMed]
- Giulioni, M.; Marucci, G.; Pelliccia, V.; Gozzo, F.; Barba, C.; Didato, G.; Villani, F.; Di Gennaro, G.; Quarato, P.P.; Esposito, V.; et al. Epilepsy surgery of “low grade epilepsy associated neuroepithelial tumors”: A retrospective nationwide Italian study. Epilepsia 2017, 58, 1832–1841. [Google Scholar] [CrossRef] [PubMed]
- Kwan, P.; Arzimanoglou, A.; Berg, A.T.; Brodie, M.J.; Hauser, W.A.; Mathern, G.; Moshé, S.L.; Perucca, E.; Wiebe, S.; French, J. Definition of drug resistant epilepsy: Consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2009, 51, 1069–1077. [Google Scholar] [CrossRef] [PubMed]
- Wacker, M.R.; Cogen, P.H.; Etzell, J.E.; Daneshvar, L.; Davis, R.L.; Prados, M.D. Diffuse leptomeningeal involvement by a ganglioglioma in a child. J. Neurosurg. 1992, 77, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Hukin, J.; Siffert, J.; Velasquez, L.; Zagzag, D.; Allen, J. Leptomeningeal dissemination in children with progressive low-grade neuroepithelial tumors. Neuro-Oncology 2002, 4, 253–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giulioni, M.; Marucci, G.; Martinoni, M.; Marliani, A.F.; Toni, F.; Bartiromo, F.; Volpi, L.; Riguzzi, P.; Bisulli, F.; Naldi, I.; et al. Epilepsy associated tumors: Review article. World. J. Clin. Cases 2014, 2, 623–641. [Google Scholar] [CrossRef]
- Boshuisen, K.; Arzimanoglou, A.; Cross, J.H.; Uiterwaal, C.; Polster, T.; Van Nieuwenhuizen, O.; Braun, K.P.J. Timing of Antiepileptic Drug Withdrawal and Long-Term Seizure Outcome after Paediatric Epilepsy Surgery (TimeToStop): A retrospective observational study. Lancet Neurol. 2012, 11, 784–791. [Google Scholar] [CrossRef]
- Huse, J.T.; Snuderl, M.; Jones, D.T.W.; Brathwaite, C.D.; Altman, N.; Lavi, E.; Saffery, R.; Sexton-Oates, A.; Blumcke, I.; Capper, D.; et al. Polymorphous low-grade neuroepithelial tumor of the young (PLNTY): An epileptogenic neoplasm with oligodendroglioma-like components, aberrant CD34 expression, and genetic alterations involving the MAP kinase pathway. Acta Neuropathol. 2016, 133, 417–429. [Google Scholar] [CrossRef] [Green Version]
- Nunes, R.H.; Hsu, C.C.-T.; Da Rocha, A.; Amaral, L.D.; Godoy, L.; Watkins, T.; Marussi, V.; Warmuth-Metz, M.; Alves, H.; Gonçalves, F.G.; et al. Multinodular and Vacuolating Neuronal Tumor of the Cerebrum: A New “Leave Me Alone” Lesion with a Characteristic Imaging Pattern. Am. J. Neuroradiol. 2017, 38, 1899–1904. [Google Scholar] [CrossRef] [Green Version]
| Case No. | Gender | Age at Onset (y) | Seizure Type | Seizure Frequency | DR | Age at Surgery (y) | Epilepsy Duration (y) | Location | Surgery | Complete Resection | Pathology | Oncological Outcome | F-U (y) | Engel Class | Medication Free | MI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| #1 | M | 0.6 | Focal aware, non-motor (behavior arrest) | weekly | yes | 2 | 1.4 | R mesial temporal | ATL | Yes | LGG +FCD I | No progression | 6.1 | II | no | yes |
| #2 | M | 1.2 | Focal, impaired awareness, tonic | weekly | no | 2 | 0.8 | L mesial temporal | ATL | No | LGG | No progression | 4.1 | Ia | yes | yes |
| #3 | M | 0.5 | Focal aware, non-motor (behavior arrest) | daily | yes | 1.4 | 0.9 | L mesial temporal | ATL | Yes | LGG | No progression | 4.2 | Ia | yes | yes |
| #4 | F | 1.2 | Focal aware, non-motor (behavior arrest) | weekly | yes | 1.7 | 0.5 | L mesial temporal | ATL | Yes | GG | No progression | 3 | Ia | yes | yes |
| #5 | F | 0.2 | Focal aware, motor with automatisms | monthly | no | 4 | 3.8 | L mesial temporal | ATL | No | GG | No progression | 2.8 | Ia | yes | yes |
| Case No. | Gender | Age at Onset (y) | Seizure Type | Seizure Frequency | DR | Age at Surgery (y) | Epilepsy Duration (y) | Location | Surgery | Complete Resection | Pathology | Oncological Outcome | F-U (y) | Engel Class | Medication Free | MI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| #1 | F | 13 | Focal to bilateral | monthly | no | 13.9 | 0.9 | L mesial temporal | ATL | Yes | LGG+FCD I | No progression | 5 | Ia | yes | no |
| #2 | F | 9.30 | Focal, impaired awareness, non-motor (behavior arrest) | sporadic | no | 10.2 | 0.9 | R lateral temporal | Lesionect. | Yes | DNT | No progression | 7 | Ia | yes | no |
| #3 | M | 9.00 | Focal aware, non-motor with automatisms | daily | no | 9.4 | 0.4 | R mesial temporal | ATL | Yes | GG+FCD I | No progression | 6 | Ia | yes | no |
| #4 | F | 14.0 | Focal to bilateral | sporadic | no | 14.7 | 0 | L lateral temporal | Lesionect. | Yes | LGG | No progression | 5 | Ia | yes | no |
| #5 | F | 12 | Focal to bilateral | daily | yes | 13 | 1 | R mesial temporal | ATL | Yes | GG+FCD I | No progression | 5 | Ia | yes | no |
| #6 | M | 6 | Focal aware, motor with automatisms | monthly | no | 8.9 | 2.9 | R lateral temporal | Lesionect. | Yes | GG+FCD I | No progression | 5 | Ia | yes | no |
| #7 | F | 11 | Focal, impaired awareness, non-motor (autonomic) | weekly | no | 13 | 1.9 | L mesial temporal | Lesionect. | No | DNT | No progression | 4 | Ia | yes | no |
| #8 | M | 10 | Focal, impaired awareness, non-motor (behavior arrest) | daily | no | 10 | 0 | L lateral temporal | Lesionect. | Yes | GG+FCD I | No progression | 4 | Ia | yes | no |
| #9 | F | 8 | Focal, impaired awareness, non-motor (autonomic) | weekly | yes | 11 | 3 | L lateral temporal | Lesionect. | Yes | DNT | No progression | 4 | Ia | yes | no |
| #10 | F | 8 | Focal aware, non-motor (autonomic) | daily | yes | 9 | 1 | R lateral temporal and thalamic | Lesionect. | No | DNT | No progression | 4 | Ia | yes | no |
| #11 | F | 5.5 | Focal impaired awareness, motor with automatisms | weekly | yes | 8 | 2.5 | R mesial temporal | ATL | No | GNT | No progression | 4 | Ia | yes | no |
| #12 | M | 5 | Focal, impaired awareness, non-motor (behavior arrest) | daily | yes | 7, 8 | 2 | L lateral and mesial temporal | ATL | Yes | LGG | No progression | 4 | Ia | yes | no |
| #13 | F | 11.6 | Focal aware, non-motor (sensory) | monthly | no | 12 | 0.4 | L mesial temporal | Lesionect. | Yes | DNT | No progression | 3 | Ia | yes | no |
| #14 | M | 7 | Focal impaired awareness, motor (clonic) | sporadic | no | 7 | 0 | L mesial temporal | ATL | Yes | PXA | No progression | 5 | Ia | yes | no |
| #15 | F | 6 | Focal aware, non-motor (behavior arrest) | daily | no | 9 | 3 | R mesial temporal | ATL | No | DNT+FCD I | No progression | 4 | Ia | yes | no |
| #16 | M | 5.8 | Focal impaired awareness, motor (clonic) | daily | yes | 5.9 | 0.1 | R parietal | Lesionect. | Yes | GG | No progression | 7 | Ia | yes | no |
| #17 | M | 7 | Focal aware, non-motor (behavior arrest) | daily | yes | 9 | 2.0 | R parietal | Lesionect. | Yes | PXA | No progression | 3 | Ia | yes | no |
| #18 | M | 8 | Focal, impaired awareness, non-motor (behavior arrest) | daily | no | 9 | 1 | R parietal | Lesionect. | No | GG | No progression | 2 | Ia | yes | no |
| #19 | M | 9 | Focal, impaired awareness, non-motor (behavior arrest) | sporadic | no | 9 | 1 | L parietal | Lesionect. | Yes | GG | No progression | 2 | Ia | yes | no |
| #20 | M | 5.1 | Focal aware, motor (clonic) | sporadic | yes | 8 | 2.9 | R parietal | Lesionect. | Yes | DNT+FCD I | No progression | 3 | Ia | yes | no |
| #21 | F | 4 | Focal impaired awareness, motor (clonic) | daily | yes | 10 | 6 | R parietal | Lesionect. | Yes | GG | No progression | 2 | Ia | yes | no |
| #22 | M | 14.5 | Focal to bilateral | sporadic | yes | 15 | 0.5 | L occipital | Lesionect. | Yes | DNT | No progression | 3 | Ia | yes | no |
| #23 | F | 4 | Focal impaired awareness, motor with automatisms | weekly | no | 4, 10 | 0 | L frontal | Lesionect. | Yes | DNT | No progression | 2 | Ia | yes | no |
| #24 | M | 11 | Focal impaired awareness, hypermotor | monthly | no | 13.9 | 2.9 | R frontal | Lesionect. | No | Pilocytic astrocytoma | No progression | 4 | Ia | yes | no |
| #25 | M | 10 | Focal impaired awareness, hypermotor | monthly | no | 10, 16 | 16 | R frontal | Lesionect. | Yes | Extraventricular neurocytoma | No progression | 2 | Ia | yes | no |
| #26 | F | 0.8 | Focal impaired awareness, non-motor (behavior arrest) | weekly | no | 1 | 0.4 | L mesial temporal | ATL | No | LG Astroc. +FCD I | No progression | 8.8 | Ia | yes | no |
| #27 | F | 1 | Focal, impaired awareness, motor with automatisms | daily | yes | 3 | 2 | R frontal | Lesionect. | Yes | GG | No progression | 5 | Ia | yes | no |
| #28 | M | 2 | Focal impaired awareness, epileptic spasms | monthly | yes | 15 | 13 | R frontal | Lesionect. | Yes | GNT | No progression | 2 | Ia | yes | no |
| #29 | M | 3 | Focal, impaired awareness, motor with automatisms | weekly | yes | 4 | 8 | L mesial temporal | Lesionect. | No | GG | No progression | 3 | Ia | yes | no |
| #30 | M | 3 | Focal, aware, non-motor (behavior arrest) | daily | no | 15 | 12 | L mesial temporal | ATL | Yes | DNT | No progression | 2 | Id | no | no |
| #31 | F | 2.90 | Focal, impaired awareness, clonic | weekly | yes | 5 | 2.1 | L frontal | Lesionect. | No | DNT | No progression | 2.5 | III | no | no |
| #32 | M | 3 | Focal, impaired awareness, tonic | daily | yes | 8 | 5 | L frontal | Lesionect. | Yes | GNT | No progression | 3 | Ia | yes | no |
| Variable | Group 1 | Group 2 | Total |
|---|---|---|---|
| Number (% of total) | 5 (13.6%) | 32 (86.4%) | 37 (100.0%) |
| Median age at seizure onset (IQR), y | 0.6 (0.5–1.2) | 7.0 (4.0–10.0) | 6.00 (3.0–9.3) |
| Median age at surgery (IQR), y | 2.0 (1.7–2.0) | 9.0 (7.7–12.3) | 9.0 (5.0–11.0) |
| Median duration of epilepsy (IQR), y | 0.9 (0.8–1.4) | 1.5 (0.4–2.9) | 1.0 (0.5–2.9) |
| Tumor location, temporal/extratemporal | 5/0 | 18/14 | 23/14 |
| Degree of tumor resection, total/partial | 3/2 | 25/7 | 28/9 |
| Seizure outcome, Class Ia/All other | 4/1 | 30/2 | 34/3 |
| Drug resistant/responsive | 3/2 | 15/17 | 18/19 |
| Case No. | Age at Onset | Location | Pathology | MI | Complete Resection | Outcome |
|---|---|---|---|---|---|---|
| #1 | 5 y | L lateral and mesial temporal | LGG | no | yes | Ia |
| #2 | 3 y | L mesial temporal | GG | no | yes | Ia |
| #3 | 0.5 y | L mesial temporal | LGG | yes | yes | Ia |
| #4 | 11 | R frontal | Pilocytic astrocytoma | no | yes | Ia |
| #5 | 4 | L frontal | DNT | no | yes | Ia |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Palma, L.; Pepi, C.; De Benedictis, A.; Pietrafusa, N.; Mastronuzzi, A.; Cacchione, A.; Carfì-Pavia, G.; Rossi-Espagnet, C.; Diomedi-Camassei, F.; Rossi, S.; et al. Early Onset Epilepsy Caused by Low-Grade Epilepsy-Associated Tumors and Focal Meningeal Involvement. Brain Sci. 2020, 10, 752. https://doi.org/10.3390/brainsci10100752
De Palma L, Pepi C, De Benedictis A, Pietrafusa N, Mastronuzzi A, Cacchione A, Carfì-Pavia G, Rossi-Espagnet C, Diomedi-Camassei F, Rossi S, et al. Early Onset Epilepsy Caused by Low-Grade Epilepsy-Associated Tumors and Focal Meningeal Involvement. Brain Sciences. 2020; 10(10):752. https://doi.org/10.3390/brainsci10100752
Chicago/Turabian StyleDe Palma, Luca, Chiara Pepi, Alessandro De Benedictis, Nicola Pietrafusa, Angela Mastronuzzi, Antonella Cacchione, Giusy Carfì-Pavia, Camilla Rossi-Espagnet, Francesca Diomedi-Camassei, Sabrina Rossi, and et al. 2020. "Early Onset Epilepsy Caused by Low-Grade Epilepsy-Associated Tumors and Focal Meningeal Involvement" Brain Sciences 10, no. 10: 752. https://doi.org/10.3390/brainsci10100752
APA StyleDe Palma, L., Pepi, C., De Benedictis, A., Pietrafusa, N., Mastronuzzi, A., Cacchione, A., Carfì-Pavia, G., Rossi-Espagnet, C., Diomedi-Camassei, F., Rossi, S., Napolitano, A., Carai, A., Colafati, G. S., Longo, D., Curatolo, P., Vigevano, F., Marras, C. E., & Specchio, N. (2020). Early Onset Epilepsy Caused by Low-Grade Epilepsy-Associated Tumors and Focal Meningeal Involvement. Brain Sciences, 10(10), 752. https://doi.org/10.3390/brainsci10100752








