Effects of Psychoactive Massage in Outpatients with Depressive Disorders: A Randomized Controlled Mixed-Methods Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Instruments for Assessing Mental and Somatic Symptoms
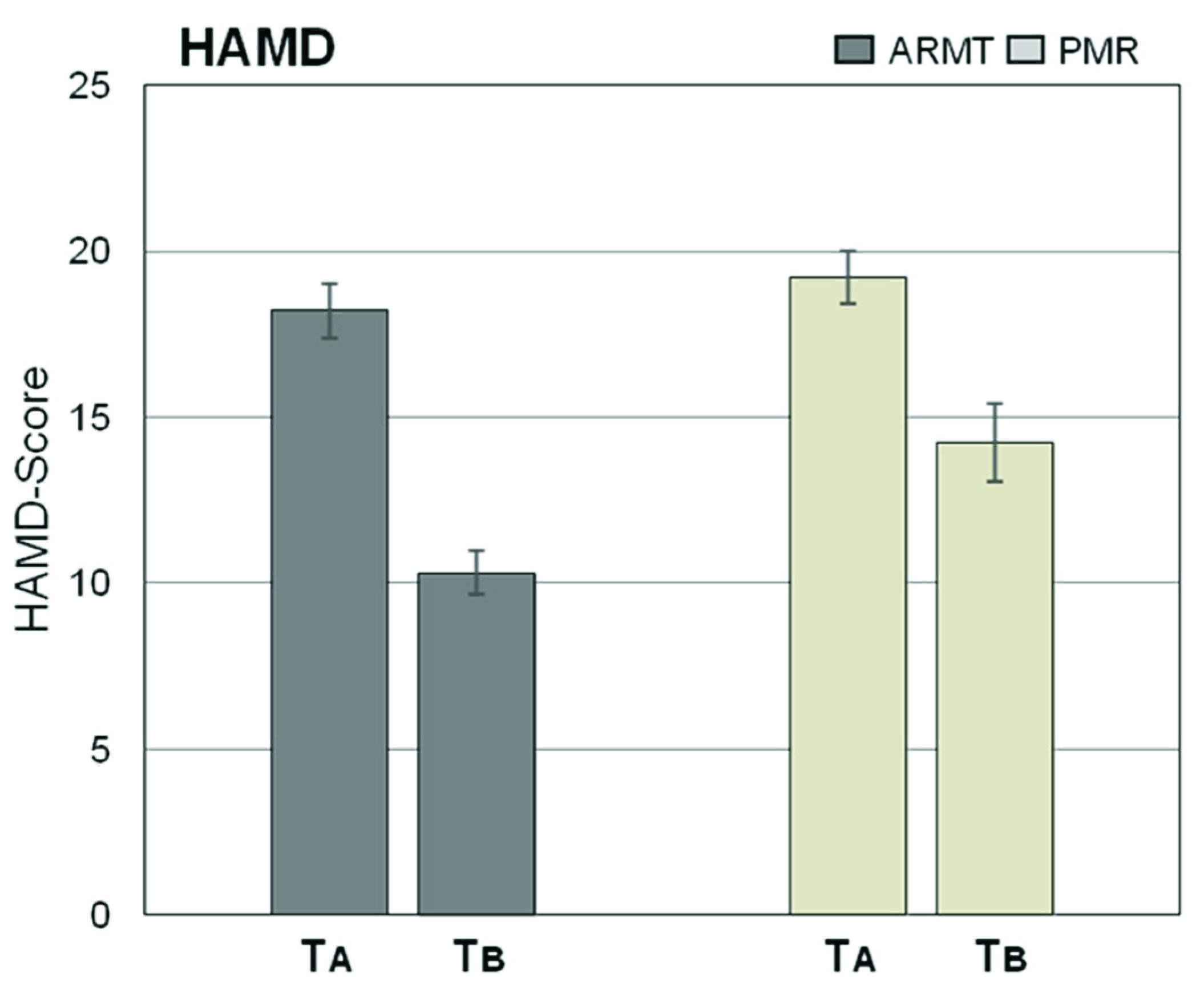
2.2.1. HAMD
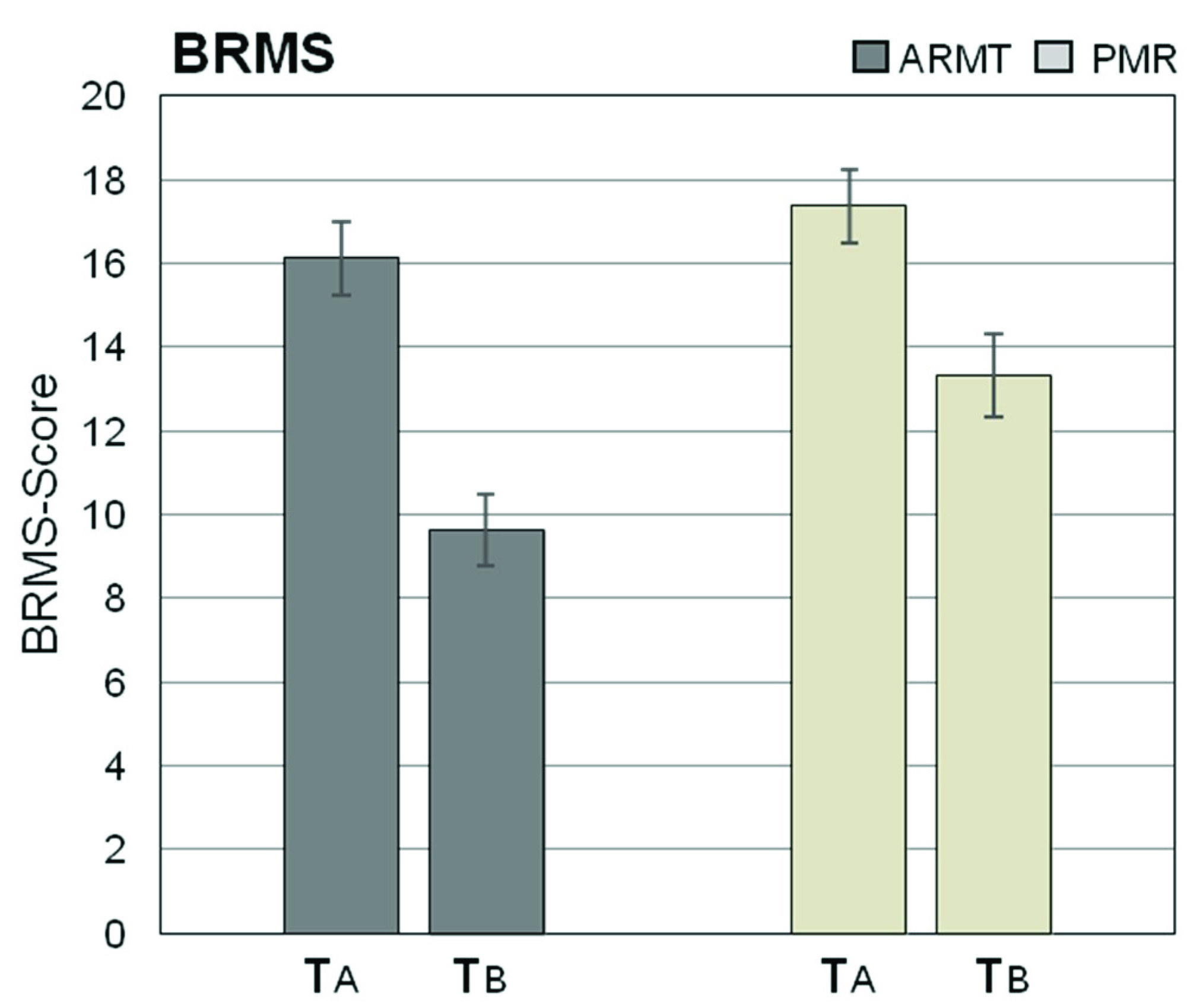
2.2.2. BRMS
2.2.3. VAS
- VAS 1:
- Stress/tension“I’m very tense”/“I’m completely relaxed”
- VAS 2:
- Hopelessness“I feel hopeless”/“I’m full of hope”
- VAS 3:
- Internal unrest“I am very restless”/“I am full of inner peace”
- VAS 4:
- Pain sensations“I’m feeling pain”/“I’m not feeling any pain”
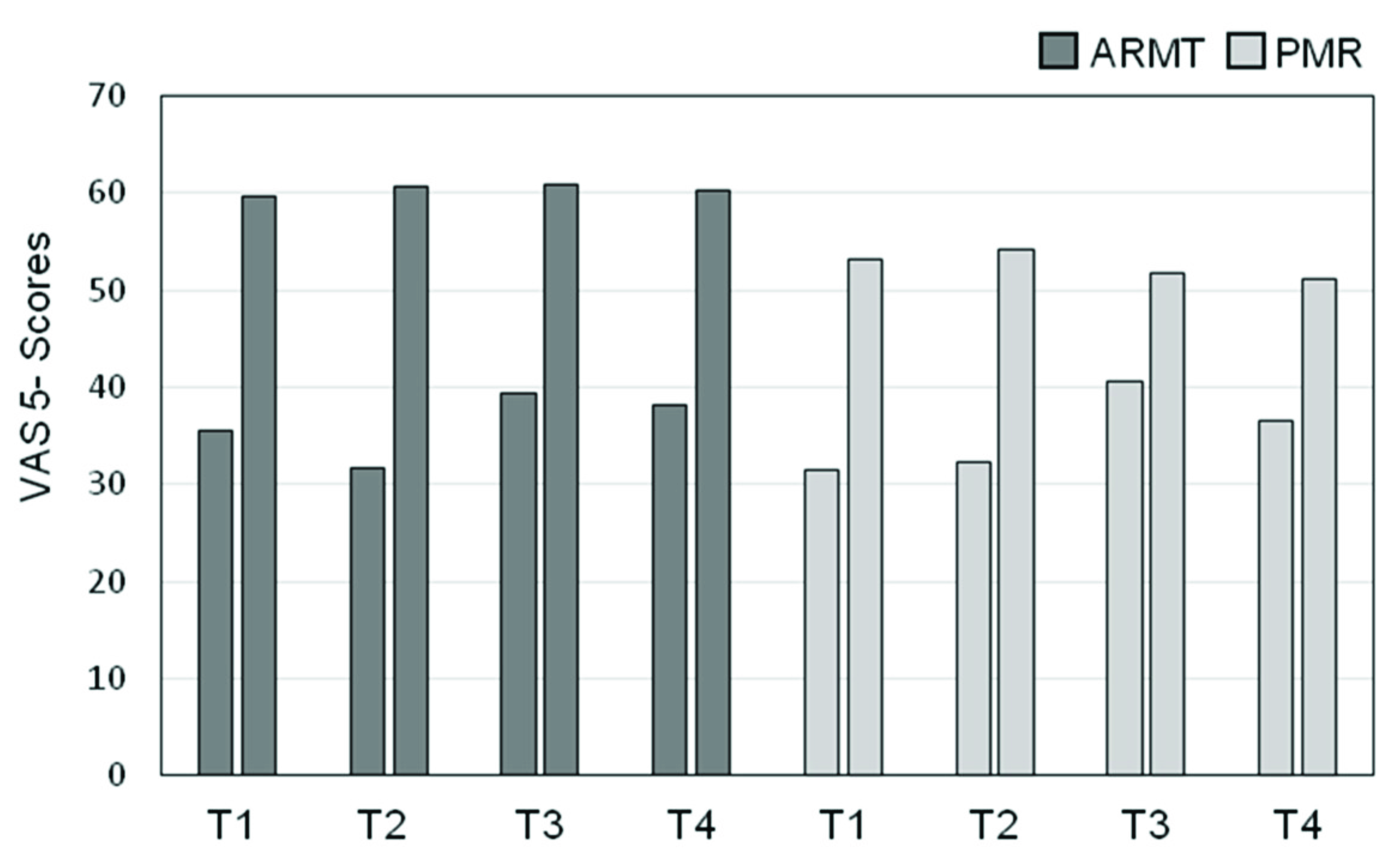
- VAS 5:
- Psychomotor retardation“I feel rigid and immobile”/“I feel light and lively”
- VAS 6:
- Tendency to brood“Negative thoughts are circulating in my head”/“I’m thinking positive and optimistic”
- VAS 7:
- Loss of drive“I feel limp and listless”/“I feel full of energy and drive”
- VAS 8:
- Unpleasant physical sensations“I’m not comfortable in my body”/“I’m comfortable in my body”
2.2.4. Assessment on Clinical Interview
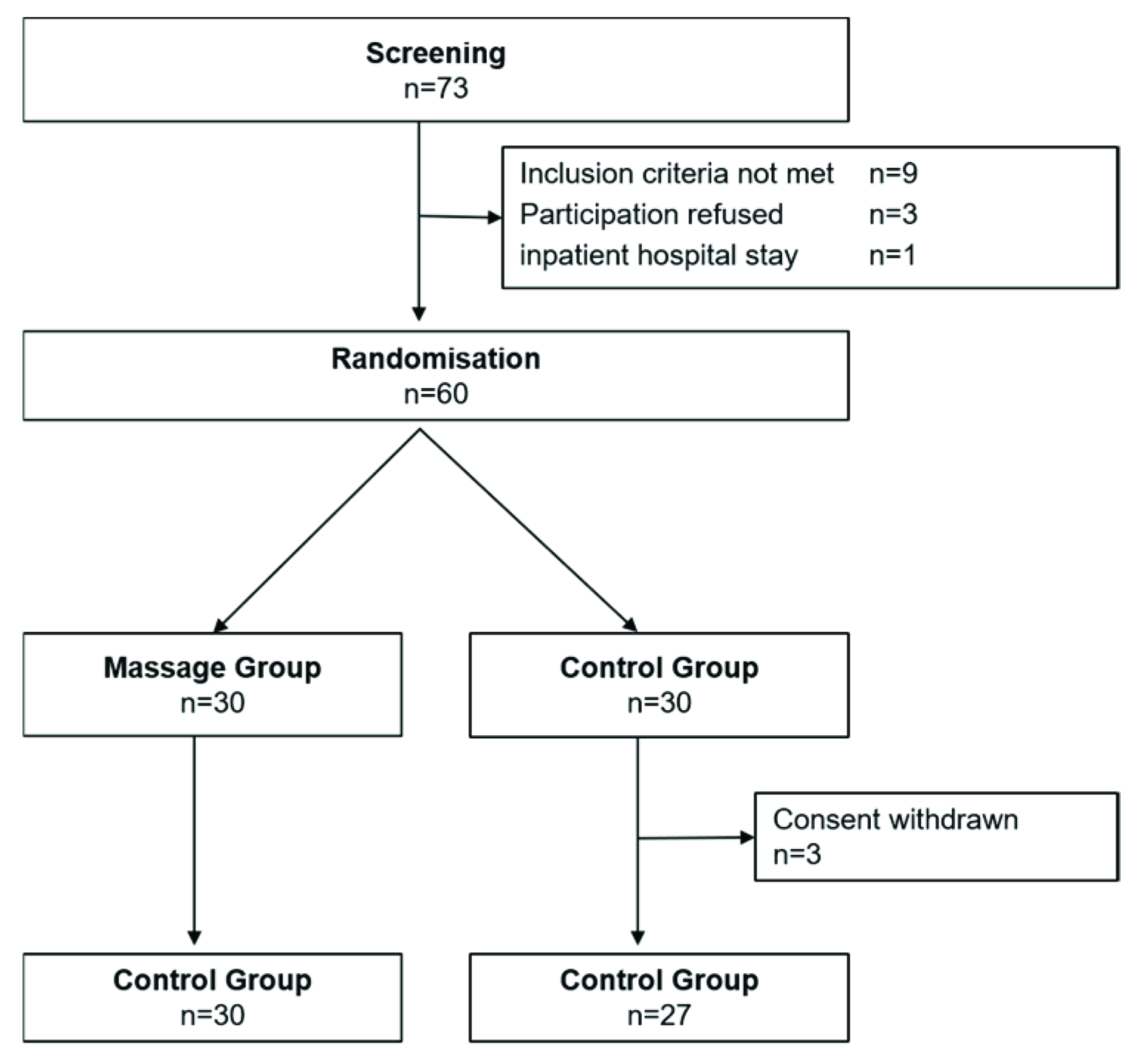
2.3. Conducting the Study
2.3.1. Sample Size Calculation
2.3.2. Ethical Approval
2.3.3. Recruitment and Randomization
- Patients of both sexes between the ages of 18 and 65;
- The presence of a mild to moderate depressive episode diagnosed by a general practitioner or specialist, including the following ICD-10 diagnoses: F32.0, F32.1, F32.2, F32.8, F32.9, F33.0, F33.1, F33.2, F33.8, F33.9.
- Acute comorbid medical condition.
- Eczematous skin disease;
- Marked varicose veins or venous thrombosis;
- Pregnancy;
- Simultaneous participation in another clinical trial.
2.4. Description of Interventions (ARMT and PMR)
2.4.1. Massage Group (ARMT)
2.4.2. Control Group (PMR)
2.5. Accompanying Therapy
2.6. Statistical Evaluation
3. Results
3.1. Description of Sample
3.1.1. Sociodemographic Data
3.1.2. Depression-Related Data
3.2. Effects of ARMT and PMR Assessed by HAMD and BRMS
- HAMD 1: Depressive mood (p = 0.004, r = 0.39)
- HAMD 13: Somatic symptoms (p = 0.021, r = 0.30)
- BRMS 8: Emotional retardation (p = 0.037, r = 0.28)
- BRMS 9: Sleep disorders (p = 0.038, r = 0.28)
3.3. Results of Participant’s Self-Assessment (VAS)
- VAS 1: Stress/tension (p = 0.035, r = 0.28)
- VAS 2: Hopelessness (p = 0.032, r = 0.28)
- VAS 3: Internal unrest (p = 0.009, r = 0.35)
- VAS 4: Pain sensations (p = 0.003, r = 0.39)
- VAS 5: Psychomotor retardation (p = 0.012, r = 0.33)
- VAS 8: Unpleasant physical sensations (p = 0.011, r = 0.34)
3.4. Statements of Study Participants in Clinical Interviews
- Better body awareness and deep relaxation;
- Interruption of brooding and negative thoughts;
- Increased motivation for everyday life activities.
- Useful in everyday life and as a sleeping aid;
- Easy relaxation and better body awareness.
4. Discussion
4.1. Strengths of the Study
4.1.1. Control Group
4.1.2. Study Participants
4.1.3. Assessments
4.1.4. Conducting the Study
4.2. Limitation
4.3. Outlook
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jacobi, F.; Höfler, M.; Strehle, J.; Mack, S.; Gerschler, A.; Scholl, L.; Busch, M.A.; Maske, U.; Hapke, U.; Gaebel, W.; et al. Psychische Störungen in der Allgemeinbevölkerung: Studie zur Gesundheit Erwachsener in Deutschland und ihr Zusatzmodul Psychische Gesundheit (DEGS1-MH). Nervenarzt 2014, 85, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017.
- Kapfhammer, H.P. Somatic symptoms in depression. Dial. Clin. Neurosci. 2006, 8, 227–239. [Google Scholar]
- Fuchs, T.; Schlimme, J.E. Embodiment and psychopathology: A phenomenological perspective. Curr. Opin. Psychiatry 2009, 22, 570–575. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, T. Melancholia as a desynchronization. Towards a psychopathology of interpersonal time. Psychopathology 2001, 34, 179–186. [Google Scholar] [CrossRef]
- Danielsson, L.; Rosberg, S. Depression embodied: An ambigous striving against fading. Nord. Coll. Caring Sci. 2014, 29, 501–509. [Google Scholar] [CrossRef]
- Paykel, E.S.; Ramana, R.; Cooper, Z.; Hayhurst, H.; Kerr, J.; Barocka, A. Residual symptoms after partial remission: An important outcome in depression. Psychol. Med. 1995, 25, 1171–1180. [Google Scholar] [CrossRef]
- Nierenberg, A.A. Residual symptoms in depression: Prevalence and impact. J. Clin. Psychiatry 2015, 76, e1480. [Google Scholar] [CrossRef]
- Lohse, M.; Müller-Oerlinghausen, B. Psychopharmaka. In Arzneiverodnungsreport 2019; Schwabe, U., Paffrath, D., Ludwig, W.-D., Klauber, J., Eds.; Springer: Berlin, Germany, 2019; pp. 927–959. [Google Scholar]
- Cuiipers, P.; Cristea, A. What if a placebo effect explained all the activity of depression treatments? World Psychiatry 2015, 14, 310–311. [Google Scholar] [CrossRef]
- Munkholm, K.; Paludan-Müller, A.S.; Boesen, K. Considering the methodological limitations in the evidence base of antidepressants for depression: A reanalysis of a network meta-analysis. BMJ Open 2019, 9, e024886. [Google Scholar] [CrossRef]
- Pigott, H.E.; Leventhal, A.M.; Alter, G.S.; Boven, J.J. Efficacy and effectiveness of antidepressants: Current status of research. Psychother. Psychosom. 2010, 79, 267–279. [Google Scholar] [CrossRef]
- Fava, G.A.; Tomba, E.; Grandi, S. The road to recovery from depression. Don’t drive today with yesterday’s map. Psychother. Psychosom. 2007, 6, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Andrews, P.W.; Thomson, J.A.; Amstadter, A.; Neale, M.C. Primum nil nocere: An evolutionary analysis of whether antidepressants do more harm than good. Front. Psychol. 2012, 3, 117. [Google Scholar] [CrossRef] [PubMed]
- Cuiipers, P.; van Straten, A.; Bohlmeijer, E. The effects of psychotherapy for adult depression are overestimated: A meta-analysis of study quality and effect size. Psychol. Med. 2010, 40, 211–223. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Fuller, C.; Liu, X.; Lee, H.; Fan, B.; Hoven, C.W.; Mandell, D.; Wade, C.; Kronenberg, F. Use of complementary and alternative medicine among women with depression: Results of a national survey. Psychiatr. Serv. 2007, 58, 349–356. [Google Scholar] [CrossRef]
- Röhricht, F.; Papadopoulos, N.; Priebe, S. An exploratory randomized controlled trial of body psychotherapy for patients with chronic depression. J. Affect. Dis. 2013, 151, 85–91. [Google Scholar] [CrossRef]
- Cooney, G.M.; Dwan, K.; Greig, C.A.; Lawlor, D.A.; Rimer, J.; Waugh, F.R.; McMurdo, M.; Mead, G.E. Exercise for depression. Cochrane Database Syst. Rev. 2013, CD004366. [Google Scholar] [CrossRef]
- Kvam, S.; Kleppe, C.L.; Nordhus, I.H.; Hovland, A. Exercise as a treatment for depression: A meta-analysis. J. Affect. Disord. 2016, 202, 67–86. [Google Scholar] [CrossRef]
- Cramer, H.; Lauche, R.; Langhorst, J.; Dobos, G. Yoga for depression: A systematic review and meta-analysis. Depress Anxiety 2013, 30, 1068–1083. [Google Scholar] [CrossRef]
- Oh, B.; Choi, S.M.; Inamori, A.; Rosenthal, D.; Yeung, A. Effects of qigong on depression: A systemic review. Evid. Based Complement. Alternat. Med. 2013, 2013, 134737. [Google Scholar] [CrossRef]
- Jaffe, D.H.; Rive, B.; Denee, T.R. The humanistic and economic burden of treatment-resistant depression in Europe: A cross-sectional study. BMC Psychiatry 2019, 19, 247. [Google Scholar] [CrossRef]
- Ernst, E. The safety of massage therapy. Rheumatology 2003, 42, 1101–1106. Available online: https://academic.oup.com/rheumatology/article/42/9/1101/1772218 (accessed on 2 May 2020). [CrossRef] [PubMed]
- Moyer, C.A.; Rounds, J.; Hannum, J.W. A meta-analysis of massage therapy research. Psychol. Bull. 2004, 130, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Peters, R.H. The effectiveness of therapeutic touch: A meta-analytic view. Nurs. Sci. Q. 1999, 12, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Hou, W.H.; Chiang, P.T.; Hsu, Y.T.; Chiu, S.; Yen, Y.C. Treatment effects of massage therapy in depressed p 2eople: A meta-analysis. J. Clin. Psychiatry 2010, 71, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Baumgart, S.; Müller-Oerlinghausen, B.; Schendera, C.F.G. Efficacy of massage therapy on depression and anxious disorders as well as on depressiveness and anxiety as comorbidity. A systematic overview of controlled studies. (Article in German with English abstract). Phys. Rehab. Kur. Med. 2011, 21, 167–182. [Google Scholar] [CrossRef]
- Reichert, B. (Ed.) Massage-Therapie; Georg Thieme: Stuttgart, Germany, 2015. [Google Scholar]
- Hoyme, R.J. The Complete Guide to Modern Massage: Step-by-Step Massage Basis and Techniques from Around the World; Althea Press: New York, NY, USA, 2018. [Google Scholar]
- Müller-Oerlinghausen, B.; Kiebgis, G.M. Berührung- Warum Wir Sie Brauchen und Wie Sie Uns Heilt, 2nd ed.; Ullstein: München, Germany, 2018. [Google Scholar]
- Müller-Oerlinghausen, B.; Berg, C.; Scherer, P.; Mackert, A.; Moestl, H.P.; Wolf, J. Effects of slow-stroke massage as complimentary treatment of depressed hospitalized patients: Results of a controlled study (SeSeTra). (Article in German with English abstract). Dtsch. Med. Wochenschr. 2004, 129, 1363–1368. [Google Scholar]
- Jacobson, E. Entspannung als Therapie: Progressive Relaxation in Theorie und Praxis, 7th ed.; Klett-Cotta: Stuttgart, Germany, 2011. [Google Scholar]
- Petermann, F. Entspannungsverfahren: Das Praxishandbuch. Mit E-Book Inside; Neuausgabe, 6., überarbeitete Auflage; Julius Beltz GmbH & Co: Weinheim, Germany, 2020. [Google Scholar]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef]
- Weyer, G.; Koeppen, D. Internationale Skalen für Psychiatrie 6; überarb. und erw. Aufl; Beltz-Test: Göttingen, Germany, 2015. [Google Scholar]
- Zimmerman, M.; Martinez, J.H.; Young, D.; Chelminski, I.; Dalrymple, K. Severity classification on the Hamilton Depression Rating Scale. J. Affect. Disord. 2013, 150, 384–388. [Google Scholar] [CrossRef]
- Stieglitz, R.D. Bech-Rafaelsen-Melancholie-Skala; Hogrefe: Göttingen, Germany, 1998. [Google Scholar]
- Maier, W.; Philipp, W. Comparative analysis of observer rating scales. Acta Psychiatr. Scand. 1985, 72, 239–245. [Google Scholar] [CrossRef]
- Schomacher, J. Gütekriterien der visuellen Analogskala zur Schmerzbewertung. Physioscience 2008, 4, 125–133. [Google Scholar] [CrossRef]
- Müller-Oerlinghausen, B.; Berg, C.; Droll, W. Die Slow Stroke Massage als ein körpertherapeutischer Ansatz bei Depression. Psychiatr. Prax. 2007, 34, S305–S308. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, T. Corporealized and disembodied minds. A phenomenological view of the body in melancholia and schizophrenia. Psychiatry Psychol. 2005, 12, 95–107. [Google Scholar]
- Rosa, H. Resonanz: Eine Soziologie der Weltbeziehung, 1st ed.; Suhrkamp: Berlin, Germany, 2016. [Google Scholar]
- Faller, H. Depression: Klinik, Ursachen, Therapie; Königshausen & Neumann: Würzburg, Germany, 2011. [Google Scholar]
- Röhricht, F. Leibgedächtnis und Körper-Ich: Zwei zentrale Bezugspunkte in der störungsspezifischen körperorientierten Psychotherapie. Psychol. Österreich. 2011, 4, 239–248. [Google Scholar]
- Gallagher, S. How the Body Shapes the Mind; Oxford University Press: New York, NY, USA, 2005. [Google Scholar]
- Seligman, M.E.P. Learned helpnessless. Ann. Rev. Med. 1972, 23, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Eggart, M.; Lange, A.; Binser, M.J.; Queri, S.; Müller-Oerlinghausen, B. Major Depressive disorder is associated with Impaired interoceptive accuracy: A systematic review. Brain Sci. 2019, 9, 131. [Google Scholar] [CrossRef] [PubMed]
- Arikha, N. The Interoceptive Turn. The Science of How We Sense Ourselves from within, Including Our Bodily States, is Creating a Radical Picture of Selfhood. 2019. Available online: https://aeon.co/essays/the-interoceptive-turn-is-maturing-as-a-rich-science-of-selfhood (accessed on 9 June 2020).
- Eggart, M.; Queri, S.; Müller-Oerlinghausen, B. Are the antidepressive effects of massage therapy mediated by restoration of impaired interoceptive functioning? A novel hypothetical mechanism. Med. Hypotheses 2019, 128, 28–32. [Google Scholar] [CrossRef]
- Von Mohr, M.; Kirsch, L.P.; Fotopoulou, A. The soothing function of touch: Affective touch reduces feelings of social exclusion. NeuroImage 2018, 169, 162–171. [Google Scholar] [CrossRef]
- Takeuchi, M.S.; Miyaoka, H.; Tomoda, A.; Suzuki, M.; Liu, Q.; Kitamura, T. The effect of interpersonal touch during childhood on adult attachment and depression: A neglected area of family and developmental psychology? J. Child Fam. Stud. 2010, 19, 109–117. [Google Scholar] [CrossRef]
- Olausson, H.; Wessberg, J.; Morrison, I.; McGlone, F. Affective Touch and the Neurophysiology of CT Afferents; Springer: New York, NY, USA, 2016. [Google Scholar]
- Montagu, A. Touching: The Human Significance of the Skin; Columbia University Press: New York, NY, USA; London, UK, 1971. [Google Scholar]
- Field, T. Massage therapy research review. Complement. Ther. Clin. Pract. 2016, 24, 19–31. [Google Scholar] [CrossRef]
- Reich, W. Character Analysis, 3rd ed.; Farrar, Straus, Giroux: New York, NY, USA, 1972. [Google Scholar]
- Röhricht, F. Body oriented psychotherapy—The state of the art in empirical research and evidence based practice: A clinical perspective. Body Mov. Dance 2009, 4, 135–156. [Google Scholar] [CrossRef]
- Changaris, M. Touch: The Neurobiology of Health, Healing, and Human Connection; LifeRhythm: Mendocino, CA, USA, 2015. [Google Scholar]
- Field, T.; Hernandez-Reif, M.; Diego, M.; Schanberg, S.; Kuhn, C. Cortisol decreases and serotonin and dopamine increase following massage therapy. Int. J. Neurosci. 2005, 115, 1397–1413. Available online: https://www.tandfonline.com/doi/pdf/10.1080/00207450590956459?needAccess=true (accessed on 2 May 2020). [CrossRef] [PubMed]
- Kosfeld, M.; Heinrichs, M.; Zak, P.J.; Fischbacher, U.; Fehr, E. Oxytocin increases trust in humans. Nature 2005, 435, 673–676. [Google Scholar] [CrossRef] [PubMed]
- Uvnäs-Moberg, K. The Hormone of Closeness: The Role of Oxytocin in Relationships1. Aufl; Springer Spektrum: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Wang, J.; Lloyd-Evans, B.; Giacco, D.; Forsyth, R.; Nebo, C.; Mann, F.; Johnson, S. Social isolation in mental health: A conceptual and methodological review. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 1451–1461. [Google Scholar] [CrossRef] [PubMed]
- Paloyelis, Y.; Krahé, C.; Maltezos, S.; Williams, S.C.; Howard, M.A.; Fotopoulou, A. The Analgesic Effect of Oxytocin in Humans: A Double-Blind, Placebo-Controlled Cross-Over Study Using Laser-Evoked Potentials. J. Neuroendocrinol. 2016, 28. [Google Scholar] [CrossRef] [PubMed]
- Diego, M.A.; Field, T.; Hernandez-Reif, M. Vagal Activity, Gastric Motility, and Weight Gain in Massaged Preterm Neonates. J. Pediatrics 2005, 147, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Listing, M.; Reißhauer, A.; Krohn, M.; Voigt, B.; Tjahono, G.; Becker, J.; Klapp, B.F.; Rauchfuß, M. Massage therapy reduces physical discomfort and improves mood disturbances in women with breast cancer. Psycho-Oncology 2009, 18, 1290–1299. [Google Scholar] [CrossRef]
- Moustgard, H.; Clayton, G.L.; Jones, H.E.; Boutron, I. Impact of blinding on estimated treatment effects in randomized clinical trials: Meta-epidemiological study. BMJ 2020, 368, 6802. [Google Scholar] [CrossRef]
- Dorsett, M.D.; Friccione, G.L.; Benson, H. A new era for mind-body medicine. N. Engl. J. Med. 2020, 382, 1390–1391. [Google Scholar] [CrossRef]
- Michalak, J.; Burg, J.; Heidenreich, T. Don’t forget your body: Mindfulness embodiment and the treatment of depression. Mindfulness 2012, 3, 190–199. [Google Scholar] [CrossRef]

| ARMT | n = 30 | PMR | n = 27 | |
|---|---|---|---|---|
| M | SD | M | SD | |
| Age (years) | 45.2 | 9.43 | 44.9 | 12.29 |
| Sex | n | % | n | % |
| female (n) | 22 | 73.33 | 22 | 81.48 |
| male (n) | 8 | 26.67 | 5 | 18.52 |
| Civil status | ||||
| single | 9 | 30.00 | 9 | 33.33 |
| married/partnership | 16 | 53.33 | 15 | 55.55 |
| divorced/widowed | 5 | 16.67 | 3 | 11.11 |
| Children | ||||
| childless | 11 | 36.67 | 15 | 55.55 |
| one or two children | 13 | 43.33 | 6 | 22.22 |
| three or more children | 6 | 20.00 | 6 | 22.22 |
| Education | ||||
| primary school | 7 | 23.33 | 1 | 3.7 |
| secondary school | 13 | 43.33 | 25 | 92.6 |
| high school | 10 | 33.33 | 1 | 3.7 |
| Employment | ||||
| vocational training | 23 | 76.67 | 22 | 81.48 |
| academic career | 7 | 23.33 | 5 | 18.52 |
| unemployed | 6 | 20.00 | 7 | 25.92 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arnold, M.M.; Müller-Oerlinghausen, B.; Hemrich, N.; Bönsch, D. Effects of Psychoactive Massage in Outpatients with Depressive Disorders: A Randomized Controlled Mixed-Methods Study. Brain Sci. 2020, 10, 676. https://doi.org/10.3390/brainsci10100676
Arnold MM, Müller-Oerlinghausen B, Hemrich N, Bönsch D. Effects of Psychoactive Massage in Outpatients with Depressive Disorders: A Randomized Controlled Mixed-Methods Study. Brain Sciences. 2020; 10(10):676. https://doi.org/10.3390/brainsci10100676
Chicago/Turabian StyleArnold, Michaela Maria, Bruno Müller-Oerlinghausen, Norbert Hemrich, and Dominikus Bönsch. 2020. "Effects of Psychoactive Massage in Outpatients with Depressive Disorders: A Randomized Controlled Mixed-Methods Study" Brain Sciences 10, no. 10: 676. https://doi.org/10.3390/brainsci10100676
APA StyleArnold, M. M., Müller-Oerlinghausen, B., Hemrich, N., & Bönsch, D. (2020). Effects of Psychoactive Massage in Outpatients with Depressive Disorders: A Randomized Controlled Mixed-Methods Study. Brain Sciences, 10(10), 676. https://doi.org/10.3390/brainsci10100676





