Effect of Psycho-Regulatory Massage Therapy on Pain and Depression in Women with Chronic and/or Somatoform Back Pain: A Randomized Controlled Trial
Abstract
1. Introduction
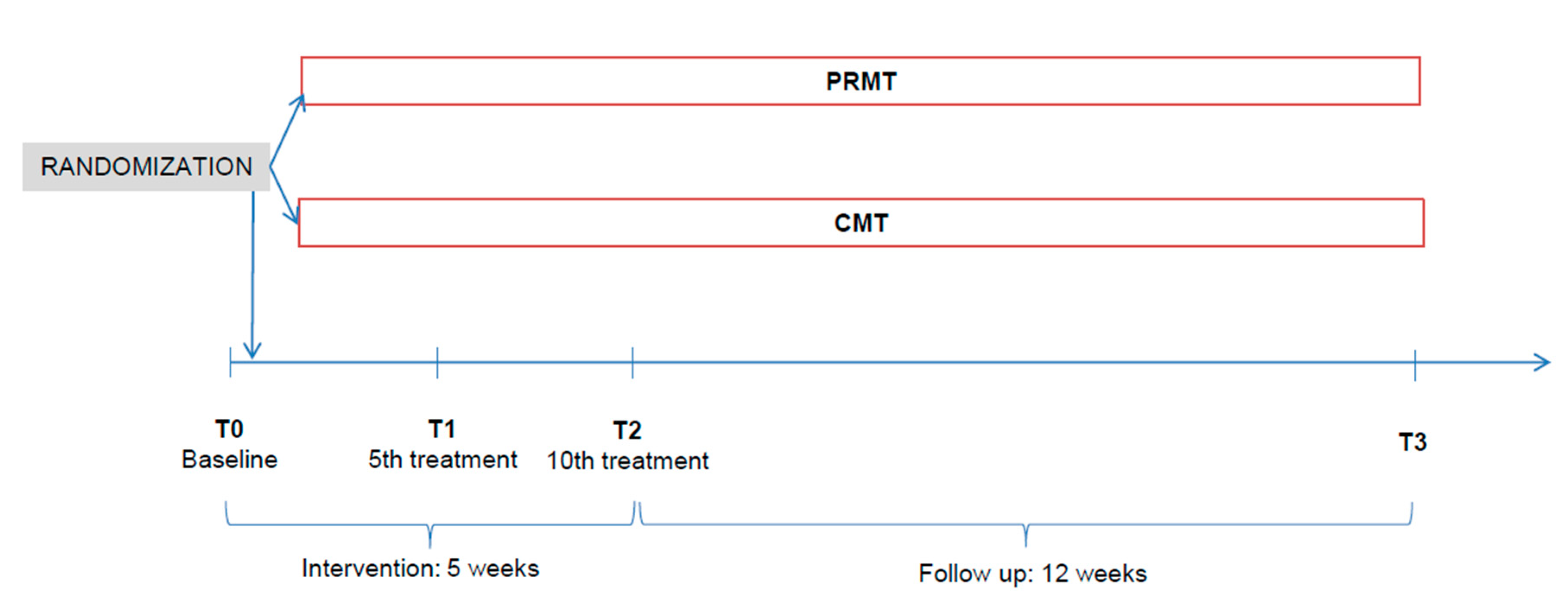
2. Materials and Methods
2.1. Eligibility Criteria
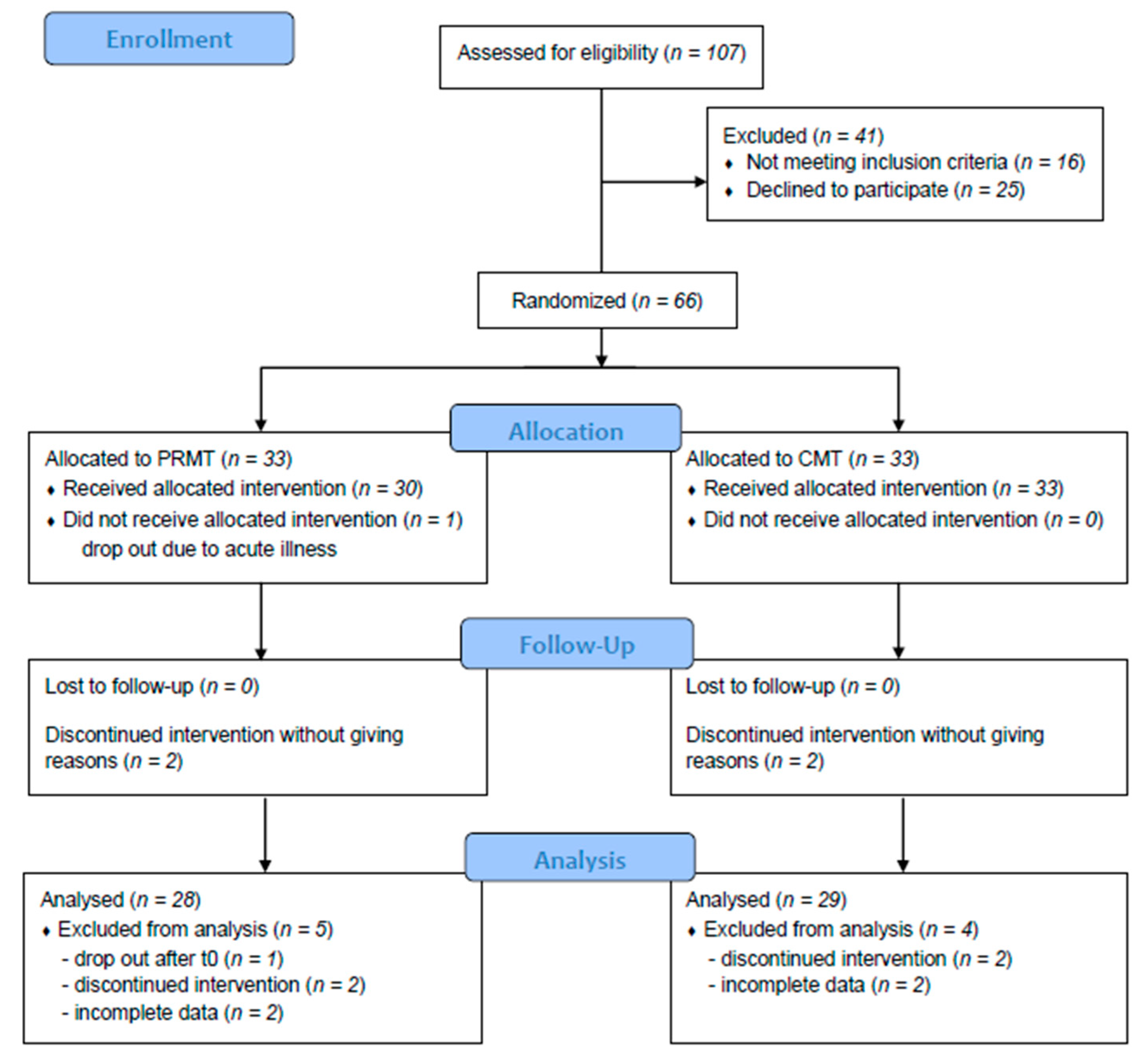
2.2. Participants
2.3. Interventions
2.4. Data collection
- 0–8
- no depression;
- 9–13
- minimal depression;
- 14–19
- mild depression;
- 20–28
- moderate depression;
- 29–63
- severe depression [41].
- 0–2
- minimal disability (all activities of daily living (ADL) are mostly possible, often no therapy necessary, activation of life is enough);
- 21–40
- moderate disability (participation is already limited and incapacity to work often occurs, conservative treatment);
- 41–60
- severe disability (pain is the main problem and ADL are affected, intensive diagnostics are necessary);
- 61–80
- crippled (all areas of life are affected);
- 81–100
2.5. Sample Size and Randomization
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Vos, T.; Barber, R.M.; Bell, B.; Bertozzi-Villa, A.; Biryukov, S.; Bolliger, I.; Charlson, F.; Davis, A.; Degenhardt, L.; Dicker, D.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [Google Scholar] [CrossRef]
- Schneider, S.; Randoll, D.; Buchner, M. Why do women have back pain more than men? Clin. J. Pain 2006, 22, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Van Middelkoop, M.; Rubinstein, S.M.; Kuijpers, T.; Verhagen, A.P.; Ostelo, R.W.; Koes, B.W.; van Tulder, M. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur. Spine J. 2010, 20, 19–39. [Google Scholar] [CrossRef] [PubMed]
- Khadilkar, A.; Milne, S.; Brosseau, L.; Wells, G.; Tugwell, P.; Robinson, V.; Shea, B.; Saginur, M. Transcutaneous electrical nerve stimulation for the treatment of chronic low back pain: A systematic review. Spine 2005, 30, 2657–2666. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Yan, S.; Yin, X.; Li, X.; Gao, S.; Han, R.; Wei, L.; Luo, W.; Lei, G. Acupuncture for chronic low back pain in long-term follow-up: A meta-analysis of 13 randomized controlled trials. Am. J. Chin. Med. 2013, 41, 1–19. [Google Scholar] [CrossRef]
- Glazov, G.; Yelland, M.; Emery, J. Low-level laser therapy for chronic non-specific low back pain: A meta-analysis of randomised controlled trials. Acupunct. Med. 2016, 34, 328–341. [Google Scholar] [CrossRef] [PubMed]
- Seco-Calvo, J.; Kovacs, F.M.; Urrútia, G. The efficacy, safety, effectiveness, and cost-effectiveness of ultrasound and shock wave therapies for low back pain: A systematic review. Spine J. 2011, 11, 966–977. [Google Scholar] [CrossRef]
- Oliveira, C.B.; Maher, C.G.; Pinto, R.Z.; Traeger, A.C.; Lin, C.-W.C.; Chenot, J.-F.; van Tulder, M.; Koes, B.W. Clinical practice guidelines for the management of non-specific low back pain in primary care: An updated overview. Eur. Spine J. 2018, 27, 2791–2803. [Google Scholar] [CrossRef]
- Airaksinen, O.; Brox, J.I.; Cedraschi, C.; Hildebrandt, J.; Klaber-Moffett, J.; Kovacs, F.; Mannion, A.F.; Reis, S.; Staal, J.B.; Ursin, H.; et al. Chapter 4 European guidelines for the management of chronic nonspecific low back pain. Eur. Spine J. 2006, 15, 192–300. [Google Scholar] [CrossRef]
- Chou, R. Nonpharmacologic therapies for low back pain. Ann. Intern. Med. 2017, 167, 606–607. [Google Scholar] [CrossRef]
- Levenig, C.G.; Kellmann, M.; Kleinert, J.; Belz, J.; Hesselmann, T.; Hasenbring, M.I. Body image is more negative in patients with chronic low back pain than in patients with subacute low back pain and healthy controls. Scand. J. Pain 2019, 19, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Rohricht, F.; Beyer, W.; Priebe, S. Disturbances of body-experience in acute anxiety and depressive disorders neuroticism or somatization? Psychother. Psych. Med. 2002, 52, 205–213. [Google Scholar]
- Field, T. Massage therapy. Med. Clin. North Am. 2002, 86, 163–171. [Google Scholar] [CrossRef]
- Baumgart, S. Psychoaktive massage und atemtherapie-konzept und fallbericht. Phys. Ther. Theor. Prax. 2008, 6, 277–281. [Google Scholar]
- Dogs, W. Psychomotorik der massage. Phys. Ther. 1988, 1, 12–14. [Google Scholar]
- Baumgart, S.; Müller-Oerlinghausen, B.; Schendera, C.F.G. Wirksamkeit der massagetherapie bei depression und angsterkrankungen sowie bei depressivität und angst als komorbidität—eine systematische übersicht kontrollierter studien. Phys. Med. Rehabil. Kurortmed. 2011, 21, 167–182. [Google Scholar] [CrossRef]
- Müller-Oerlinghausen, B.; Berg, C.; Droll, W. Die Slow Stroke® massage als ein körpertherapeutischer ansatz bei depression. Psychiatr. Prax. 2007, 34, 305–308. [Google Scholar] [CrossRef]
- Listing, M.; Reißhauer, A.; Krohn, M.; Voigt, B.; Tjahono, G.; Becker, J.; Klapp, B.F.; Rauchfuß, M. Massage therapy reduces physical discomfort and improves mood disturbances in women with breast cancer. Psychol. Oncol. 2009, 18, 1290–1299. [Google Scholar] [CrossRef]
- Diego, M.A.; Field, T.; Sanders, C.; Hernandez-Reif, M. Massage therapy of moderate and light pressure and vibration effects on EEG and heart rate. Int. J. Neurosci. 2004, 114, 31–44. [Google Scholar] [CrossRef]
- Olausson, H.W.; Wessberg, J.; Morrison, I.; McGlone, F.; Vallbo, Å. The neurophysiology of unmyelinated tactile afferents. Neurosci. Biobehav. Rev. 2010, 34, 185–191. [Google Scholar] [CrossRef]
- Moyer, C.A. Massage therapy: An examination of the contextual model. Diss. Abstr. Int. Sect. B Sci. Eng. 2008, 69, 1337. [Google Scholar]
- Kolster, B.C. Wirkprinzipien der massage. In Massage; Springer: Berlin/Heidelberg, Germany, 2003; pp. 22–34. [Google Scholar]
- Uvnas-Moberg, K.; Petersson, M. Oxytocin, a mediator of anti-stress, well-being, social interaction, growth and healing. Z Psychosom. Med. Psychother. 2005, 51, 57–80. [Google Scholar] [PubMed]
- Walker, S.C.; McGlone, F.P. The social brain: Neurobiological basis of affiliative behaviours and psychological well-being. Neuropeptides 2013, 47, 379–393. [Google Scholar] [CrossRef] [PubMed]
- McGlone, F.; Wessberg, J.; Olausson, H. Discriminative and affective touch: Sensing and feeling. Neuron 2014, 82, 737–755. [Google Scholar] [CrossRef] [PubMed]
- Kain, K.L.; Levine, P.A.; Terrell, S.J. Nurturing Resilience: Helping Clients Move Forward from Developmental Trauma; North Atlantic Books: Berkeley, CA, USA, 2018. [Google Scholar]
- Shaikh, S.; Nagi, S.S.; McGlone, F.; Mahns, D.A. Psychophysical Investigations into the role of low-threshold C fibres in non-painful affective processing and pain modulation. PLoS ONE 2015, 10, e0138299. [Google Scholar] [CrossRef] [PubMed]
- Okabe, S.; Yoshida, M.; Takayanagi, Y.; Onaka, T. Activation of hypothalamic oxytocin neurons following tactile stimuli in rats. Neurosci. Lett. 2015, 600, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Richard, P.; Moos, F.; Freund-Mercier, M.J. Central effects of oxytocin. Physiol. Rev. 1991, 71, 331–370. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Peirce-Sandner, S.; Baron, R.; Bellamy, N.; Burke, L.B.; Chappell, A.; Chartier, K.; Cleeland, C.S.; Costello, A.; et al. Research design considerations for confirmatory chronic pain clinical trials: IMMPACT recommendations. Pain 2010, 149, 177–193. [Google Scholar] [CrossRef]
- Henningsen, P. The psychosomatics of chronic back pain. Classification, aetiology and therapy. Orthopäde 2004, 33, 558–567. [Google Scholar] [CrossRef]
- Abraham, I.; Killackey-Jones, B. Lack of evidence-based research for idiopathic low back pain. Arch. Intern. Med. 2002, 162, 1442–1444. [Google Scholar] [CrossRef]
- Deyo, R.A. Diagnostic Evaluation of LBP. Arch. Intern. Med. 2002, 162, 1444–1447. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, R.H.; Turk, D.C.; Wyrwich, K.W.; Beaton, D.; Cleeland, C.S.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Kerns, R.D.; Ader, D.N.; et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: Immpact recommendations. J. Pain 2008, 9, 105–121. [Google Scholar] [CrossRef] [PubMed]
- Moyer, C.A.; Rounds, J.; Hannum, J.W. A meta-analysis of massage therapy research. Psychol. Bull. 2004, 130, 3–18. [Google Scholar] [CrossRef]
- Sherman, K.J.; Cook, A.J.; Wellman, R.D.; Hawkes, R.J.; Kahn, J.R.; Deyo, R.A.; Cherkin, D.C. Five-week outcomes from a dosing trial of therapeutic massage for chronic neck pain. Ann. Fam. Med. 2014, 12, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, F. Hamburger Schmerz-Adjektiv-Liste (HSAL); Beltz: Weinheim, Germany, 1991. [Google Scholar]
- Lehrl, S.; Cziske, R.; Blaha, L. Schmerzmessung Durch die Mehr Dimensionale Schmerzskala—MSS; Vless GmbH: Munich, Germany, 1980. [Google Scholar]
- Laux, L.; Glanzmann, P.; Schaffner, P.; Spielberger, C.D. Das State-Trait-Angstinventar. Theoretische Grundlagen und Handanweisung; State Trait Anxiety Inventory. Theoretical Foundations and Manual; Beltz: Weinheim, Germany, 1981. [Google Scholar]
- Hautzinger, M.; Keller, F.; Kühner, C. BDI-II Beck-Depressions-Inventar Revision, 2nd ed.; Pearson Assessment: Frankfurt, Germany, 2009. [Google Scholar]
- Beck, A.T.; Steer, R.A.; Brown, G.K. Manual for the beck depression inventory-II. San Antonio. TX Psychol. Corp. 1996, 1, 82. [Google Scholar]
- Hiroe, T.; Kojima, M.; Yamamoto, I.; Nojima, S.; Kinoshita, Y.; Hashimoto, N.; Watanabe, N.; Maeda, T.; Furukawa, T.A. Gradations of clinical severity and sensitivity to change assessed with the Beck Depression Inventory-II in Japanese patients with depression. Psychiatry Res. 2005, 135, 229–235. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Couper, J.; Davies, J.B.; O’Brien, J.P. The Oswestry low back pain disability questionnaire. Physiotherapy 1980, 66, 271–273. [Google Scholar]
- Mannion, A.F.; Junge, A.; Fairbank, J.C.T.; Dvořák, J.; Grob, D. Development of a German version of the Oswestry Disability Index. Part 1: Cross-cultural adaptation, reliability, and validity. Eur. Spine J. 2005, 15, 55–65. [Google Scholar] [CrossRef]
- Mannion, A.F.; Junge, A.; Grob, D.; Dvořák, J.; Fairbank, J.C.T. Development of a German version of the Oswestry Disability Index. Part 2: Sensitivity to change after spinal surgery. Eur. Spine J. 2005, 15, 66–73. [Google Scholar] [CrossRef]
- Van Hooff, M.L.; Spruit, M.; Fairbank, J.C.T.; van Limbeek, J.; Wilco, J.C.H. The Oswestry Disability Index (version 2.1 a): Validation of a Dutch language version. Spine 2015, 40, 83–90. [Google Scholar] [CrossRef]
- Fairbank, J.C.T.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2953. [Google Scholar] [CrossRef] [PubMed]
- Tal-Akabi, A.; Oesch, P. Behinderung bei rückenbeschwerden: Oswestry Disability questionnaire—Deutsche version (ODI-D.). In Assessments in der Rehabilitation, 2nd ed.; Oesch, P., Hilfiker, R., Keller, S., Kool, J., Luomajoki, H., Schädler, S., Tal-Akabi, A., Verra, M., Leu, C.W., Eds.; Verlag Hans Huber: Bern, Switzerland, 2011; Volume 2, pp. 296–300. [Google Scholar]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N.; et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.M.; Preuper, H.R.S.; Reneman, M.F.; Posthumus, J.B.; Stewart, R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 2008, 31, 165–169. [Google Scholar] [CrossRef]
- Cherkin, D.C.; Sherman, K.J.; Kahn, J.; Wellman, M.R.; Cook, A.J.; Johnson, M.E.; Erro, R.J.; Delaney, M.K.; Deyo, R.A. A comparison of the effects of 2 types of massage and usual care on chronic low back pain. Ann. Intern. Med. 2011, 155. [Google Scholar] [CrossRef]
- Walach, H.; Güthlin, C.; König, M. Efficacy of massage therapy in chronic pain: A pragmatic randomized trial. J. Altern. Complement. Med. 2003, 9, 837–846. [Google Scholar] [CrossRef]
- Hamre, H.J.; Witt, C.M.; Glockmann, A.; Ziegler, R.; Willich, S.N.; Kiene, H. Rhythmical massage therapy in chronic disease: A 4-year prospective cohort study. J. Altern. Complement. Med. 2007, 13, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, D.M.; McGlone, F.P.; Yosipovitch, G. Somatosensory pleasure circuit: From skin to brain and back. Exp. Dermatol. 2015, 24, 321–324. [Google Scholar] [CrossRef] [PubMed]
- Krahé, C.; Drabek, M.M.; Paloyelis, Y.; Fotopoulou, A. Affective touch and attachment style modulate pain: A laser-evoked potentials study. Philos. Trans. R. Soc. B Biol. Sci. 2016, 371, 20160009. [Google Scholar] [CrossRef]
- Liljencrantz, J.; Olausson, H. Tactile C fibers and their contributions to pleasant sensations and to tactile allodynia. Front. Behav. Neurosci. 2014, 8, 37. [Google Scholar] [CrossRef]
- Kaplan, C. An Examination of Brain Network Organization and the Analgesic Mechanisms of a Non-Pharmacological Treatment in Chronic Centralized Pain. Ph.D. Thesis, University of Michigan, Ann Arbor, MI, USA, 2018. [Google Scholar]
- Boehme, R.; van Ettinger-Veenstra, H.; Olausson, H.; Gerdle, B.; Nagi, S.S. Anhedonia to gentle touch in fibromyalgia: Normal sensory processing but abnormal evaluation. Brain Sci. 2020, 10, 306. [Google Scholar] [CrossRef] [PubMed]
- Weiss, T. Fibromyalgie-ein chronisch-generalisierendes Sensitivierungssyndrom? PiD Psychother. im Dialog 2005, 6, 59–65. [Google Scholar] [CrossRef]
- Craig, A.D. How do you feel--now? The anterior insula and human awareness. Nat. Rev. Neurosci. 2009, 10, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Devue, C.; Collette, F.; Balteau, E.; Degueldre, C.; Luxen, A.; Maquet, P.; Brédart, S. Here I am: The cortical correlates of visual self-recognition. Brain Res. 2007, 1143, 169–182. [Google Scholar] [CrossRef]
- Damasio, A.R. Descartes' Error: Emotion, Reason and the Human Brain; Putnam: New York, NY, USA, 1994. [Google Scholar]
- Paulus, M.P.; Stein, M.B. Interoception in anxiety and depression. Brain Struct. Funct. 2010, 214, 451–463. [Google Scholar] [CrossRef]
- Pfeifer, A.-C.; Ditzen, B.; Neubauer, E.; Schiltenwolf, M. Wirkung von Oxytocin auf das menschliche Schmerzerleben Effect of oxytocin on human pain perception. Schmerz 2016, 30, 457–469. [Google Scholar] [CrossRef]
- Lund, I.; Yu, L.C.; Uvnäs-Moberg, K.; Wang, J.; Yu, C.; Kurosawa, M.; Agren, G.; Rosen, A.; Lekman, M.; Lundeberg, T. Repeated massage-like stimulation induces long term effects on nociception: Contribution of oxytonergic mechanisms. Eur. J. Neurosci. 2005, 22, 1553–1554. [Google Scholar] [CrossRef]
- Miranda-Cardenas, Y.; Rojas-Piloni, G.; Martínez-Lorenzana, G.; Rodríguez-Jiménez, J.; López-Hidalgo, M.; Freund-Mercier, M.J.; Condés-Lara, M. Oxytocin and electrical stimulation of the paraventricular hypothalamic nucleus produce antinociceptive effects that are reversed by an oxytocin antagonist. Pain 2006, 122, 182–189. [Google Scholar] [CrossRef]
- DeLaTorre, S.; Rojas-Piloni, G.; Martinez-Lorenzana, G.J.; Villanueva, L.; Rodrigues-Jimenez, J.; Villanueva, L.; Condes-Lara, M. Paraventricular oxitocinergic hypothalamic prevention or interruption of long-term potentiation in dorsal horn nociceptive neurons: Electrophysiological and behavioral evidence. Pain 2009, 144, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.H.; Stoeckel, M.E.; Freund-Mercier, M.J.; Schlichter, R. Oxytocin modulates glutamatergic synaptic transmission between cultured neonatal spinal cord dorsal horn neurons. J. Neurosci. 1998, 18, 2377–2386. [Google Scholar] [CrossRef]
- Sprott, H. Pathophysiologie der peripheren Schmerzentstehung–therapeutische Angriffspunkte. Praxis 2016, 105, 1267–1271. [Google Scholar] [CrossRef]
- Schleip, R.; Jäger, H. Lehrbuch Faszien: Grundlagen, Forschung, Behandlung; Urban & Fischer: Munich, Germany, 2014; pp. 65–68. [Google Scholar]
- Chiesa, A.; Serretti, A.; Jakobsen, J.C. Mindfulness: Top–down or bottom–up emotion regulation strategy? Clin. Psychol. Rev. 2013, 33, 82–96. [Google Scholar] [CrossRef] [PubMed]
- Triscoli, C.; Croy, I.; Steudte-Schmiedgen, S.; Olausson, H.; Sailer, U. Heart rate variability is enhanced by long-lasting pleasant touch at CT-optimized velocity. Biol. Psychol. 2017, 128, 71–81. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Parameters | PRMT | CMT |
|---|---|---|
| Pressure |
|
|
| Speed |
|
|
| Direction |
|
|
| Rhythm |
|
|
| T0 | T1 | T2 | T3 | ||
|---|---|---|---|---|---|
| CMT | 108.72 | 113.34 | 104.76 | 102.62 | |
| SD | 51.86 | 61.75 | 62 | 61.92 | |
| HSAL-Total | PRMT | 124.82 | 115.04 | 72.14 | 67.32 |
| SD | 57.81 | 51.38 | 36.16 | 32.86 | |
| Wilcoxon_Z | −1.76 | −1.04 | −4.47 | −3.65 | |
| p | n.s. | n.s. | <0.001 | <0.001 | |
| CMT | 66.38 | 67.03 | 61.79 | 60.86 | |
| SD | 34.79 | 38.7 | 38.28 | 38.49 | |
| HSAL-Affective | PRMT | 75.86 | 70.39 | 44.75 | 43.93 |
| SD | 33.13 | 30.68 | 23.3 | 21.83 | |
| Wilcoxon Z | −0.84 | −1.763 | −3.54 | −3.38 | |
| p | n.s. | n.s. | <0.001 | <0.001 | |
| CMT | 44.66 | 46.31 | 42.97 | 41.69 | |
| HSAL-Sensory | SD | 23.73 | 26.34 | 26.41 | 26.45 |
| PRMT | 48.93 | 44.29 | 27.39 | 23.75 | |
| SD | 26.91 | 23.72 | 16.17 | 15.8 | |
| Wilcoxon Z | −0.61 | −1.91 | −3.86 | −3.94 | |
| p | n.s. | n.s. | <0.001 | <0.001 | |
| BDI-II score | CMT | 19.3 | 20.52 | 19.59 | 18.69 |
| SD | 9.64 | 10.61 | 11.4 | 10.36 | |
| PRMT | 23.29 | 20.46 | 12.25 | 10.32 | |
| SD | 11.58 | 10.7 | 7.62 | 5.9 | |
| Wilcoxon Z | −0.6 | −2.35 | −4.21 | −4.41 | |
| p | n.s. | <0.05 | <0.001 | 0.001 | |
| ODI (%) | CMT | 39.9 | 39.73 | 39.09 | 38.52 |
| SD | 14.1 | 16.23 | 16.86 | 16.42 | |
| PRMT | 38.26 | 36.12 | 25.95 | 23.82 | |
| SD | 12.5 | 14.06 | 10.49 | 11.6 | |
| Wilcoxon Z | −0.09 | −2.09 | −4.19 | −4.2 | |
| p | n.s. | <0.05 | <0.001 | <0.001 |
| Level of Disability | PRMT n = 28 | CMT n = 29 | ||
|---|---|---|---|---|
| T0 | T3 | T0 | T3 | |
| Minimal | 6.25% | 43.33% | 9.09% | 10.34% |
| Moderate | 46.87% | 43.33% | 45.45% | 51.73% |
| Severe | 43.75% | 13.34% | 33.34% | 20.69% |
| Crippled | 3.12% | 0% | 12.12% | 17.24% |
| Bedridden | 0% | 0% | 0% | 0% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baumgart, S.B.-E.; Baumbach-Kraft, A.; Lorenz, J. Effect of Psycho-Regulatory Massage Therapy on Pain and Depression in Women with Chronic and/or Somatoform Back Pain: A Randomized Controlled Trial. Brain Sci. 2020, 10, 721. https://doi.org/10.3390/brainsci10100721
Baumgart SB-E, Baumbach-Kraft A, Lorenz J. Effect of Psycho-Regulatory Massage Therapy on Pain and Depression in Women with Chronic and/or Somatoform Back Pain: A Randomized Controlled Trial. Brain Sciences. 2020; 10(10):721. https://doi.org/10.3390/brainsci10100721
Chicago/Turabian StyleBaumgart, Sabine B.-E., Anja Baumbach-Kraft, and Juergen Lorenz. 2020. "Effect of Psycho-Regulatory Massage Therapy on Pain and Depression in Women with Chronic and/or Somatoform Back Pain: A Randomized Controlled Trial" Brain Sciences 10, no. 10: 721. https://doi.org/10.3390/brainsci10100721
APA StyleBaumgart, S. B.-E., Baumbach-Kraft, A., & Lorenz, J. (2020). Effect of Psycho-Regulatory Massage Therapy on Pain and Depression in Women with Chronic and/or Somatoform Back Pain: A Randomized Controlled Trial. Brain Sciences, 10(10), 721. https://doi.org/10.3390/brainsci10100721






