PISIoT: A Machine Learning and IoT-Based Smart Health Platform for Overweight and Obesity Control
Abstract
1. Introduction
2. Related Work
3. Materials and Methods
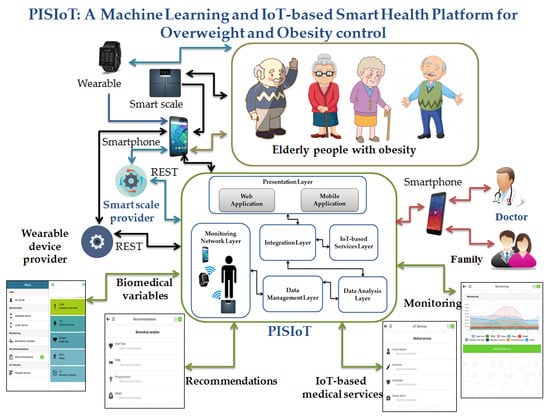
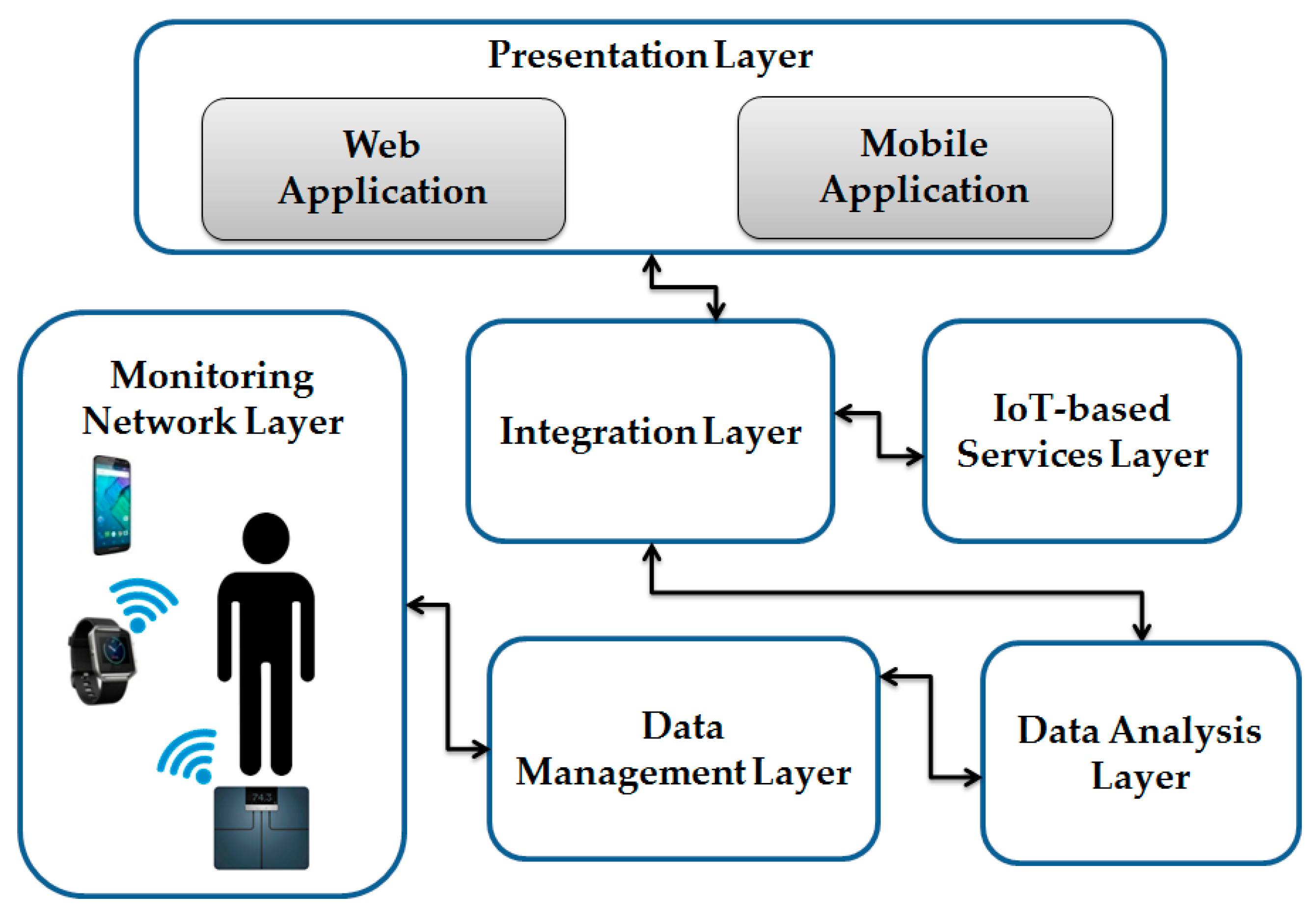
3.1. Architecture Description
3.2. PISIoT: Architecture and Functionality
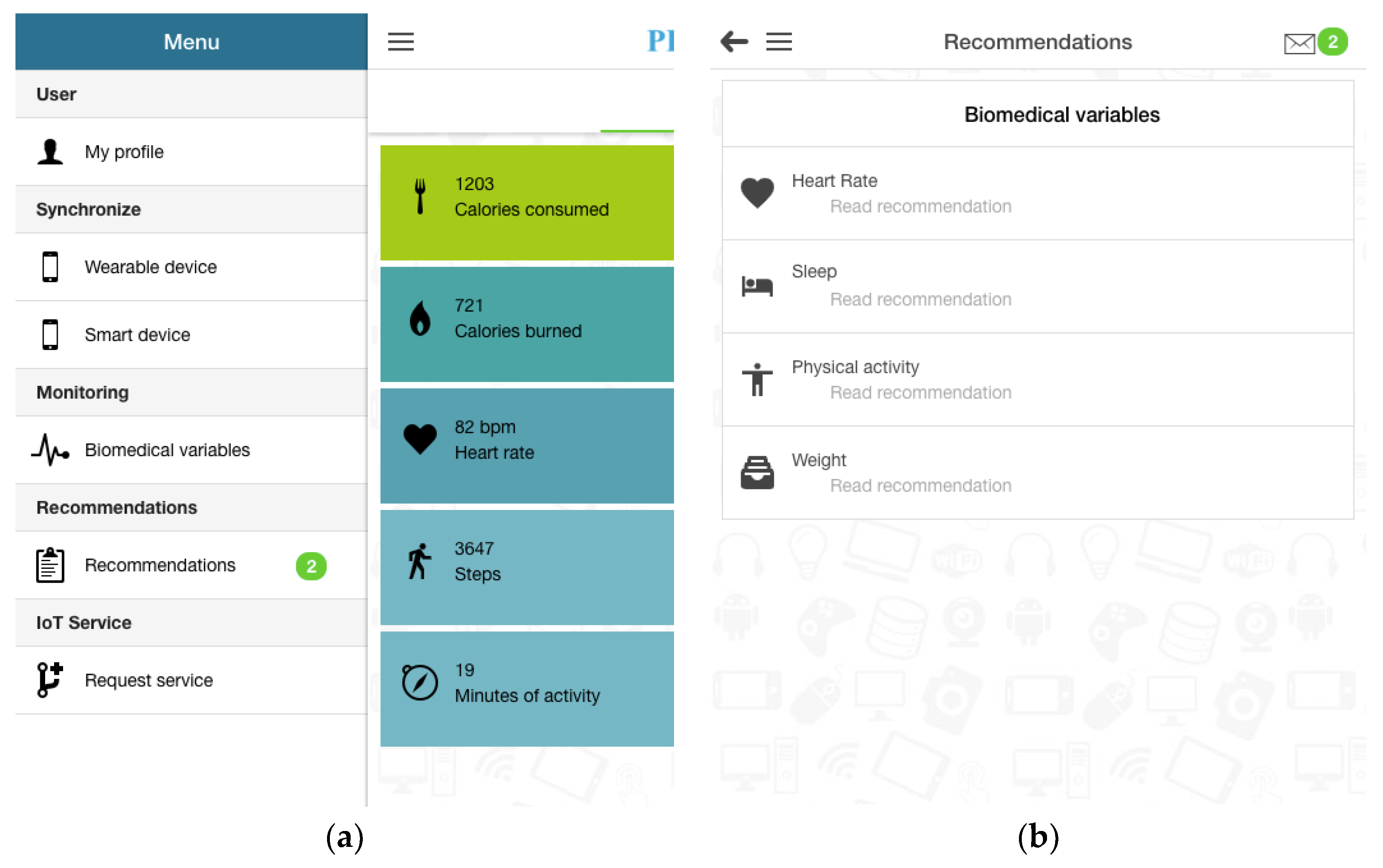
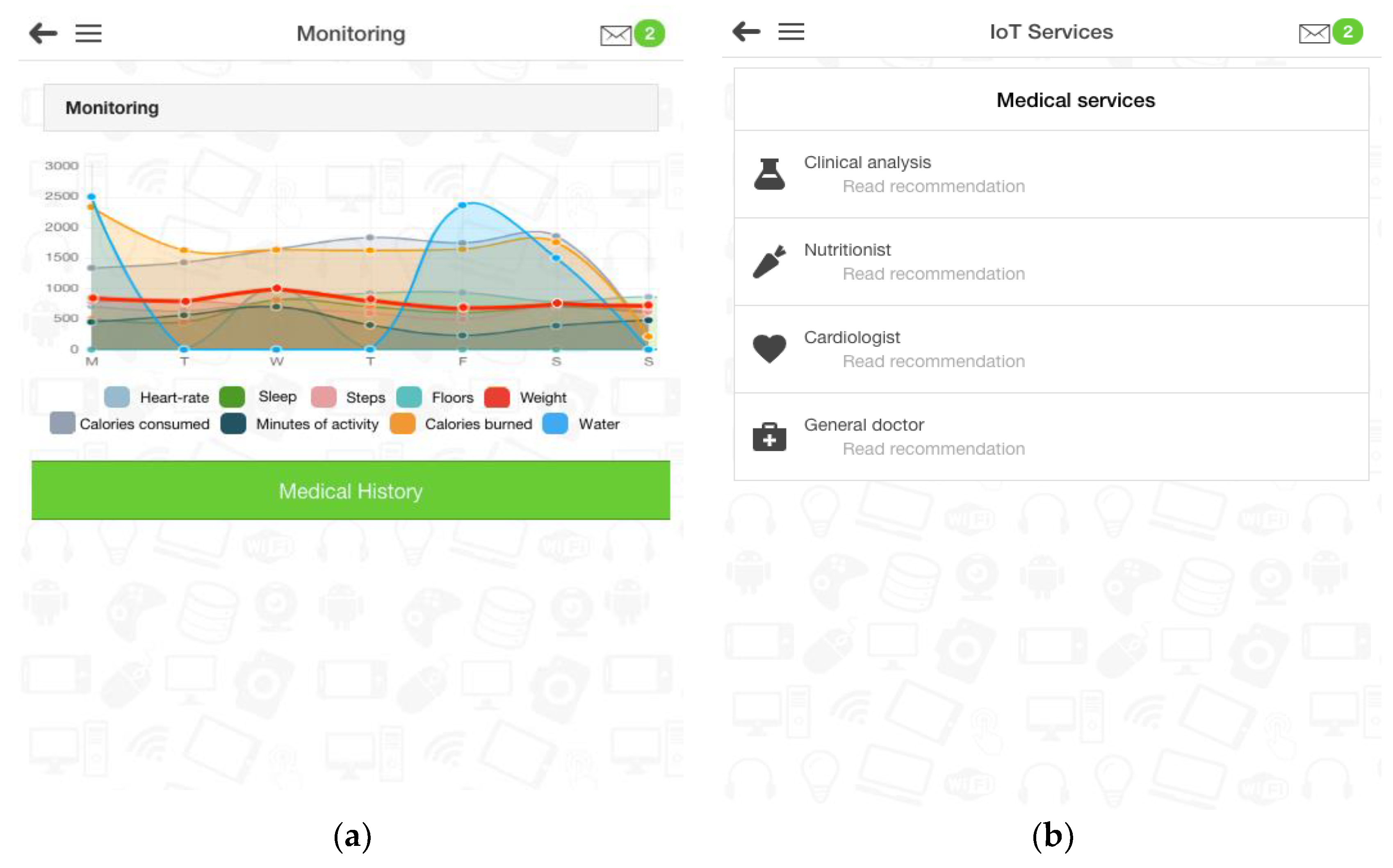
- Presentation layer. Through this layer, communication is made between the patient and the platform, thus facilitating a web application and a mobile application through which patients are able to view and track their biomedical variables, available IoT-based services, medical history, and recommendations. In addition, the platform allows manual input of water and food consumed during the day. When patients enter food or drinks consumed using a smartphone or computer with Internet access linked to the wearable device, calories, carbohydrates, fat, and proteins are automatically obtained from the database of the device provider. Nevertheless, in PISIoT, it is possible to enter food or a beverage not included in the provider’s database, in addition to any physical activity performed by the patient.
- Monitoring network layer. This layer is made up of different IoT-based devices such as wearable and smart devices linked to telecommunication equipment, which have communication interfaces that facilitate the exchange of information. These devices make it possible to collect information on the patient’s biomedical variables (heart rate, calories burned, sleep, minutes of physical activity and weight), based on the activities performed during a day. All the information collected is sent to the data management layer for further processing and analysis.
- Integration layer. This layer is made up of the wearable and smart device providers and receives the patient’s data and consultations to generate the requested answers. In addition, this layer is responsible for requesting services from the IoT-based services layer based on the PISIoT recommendations.
- Data analysis layer. This layer is responsible for identifying critical variables and generates medical recommendations. In addition, this layer protects useful information for the PISIoT and patients’ medical history.
- IoT-based services layer. This layer is responsible for linking, invoking, selecting and confirming the availability of IoT-based services.
- Data management layer. This layer is responsible for the storage and backup of the patient’s medical history and the data collected by the devices used.
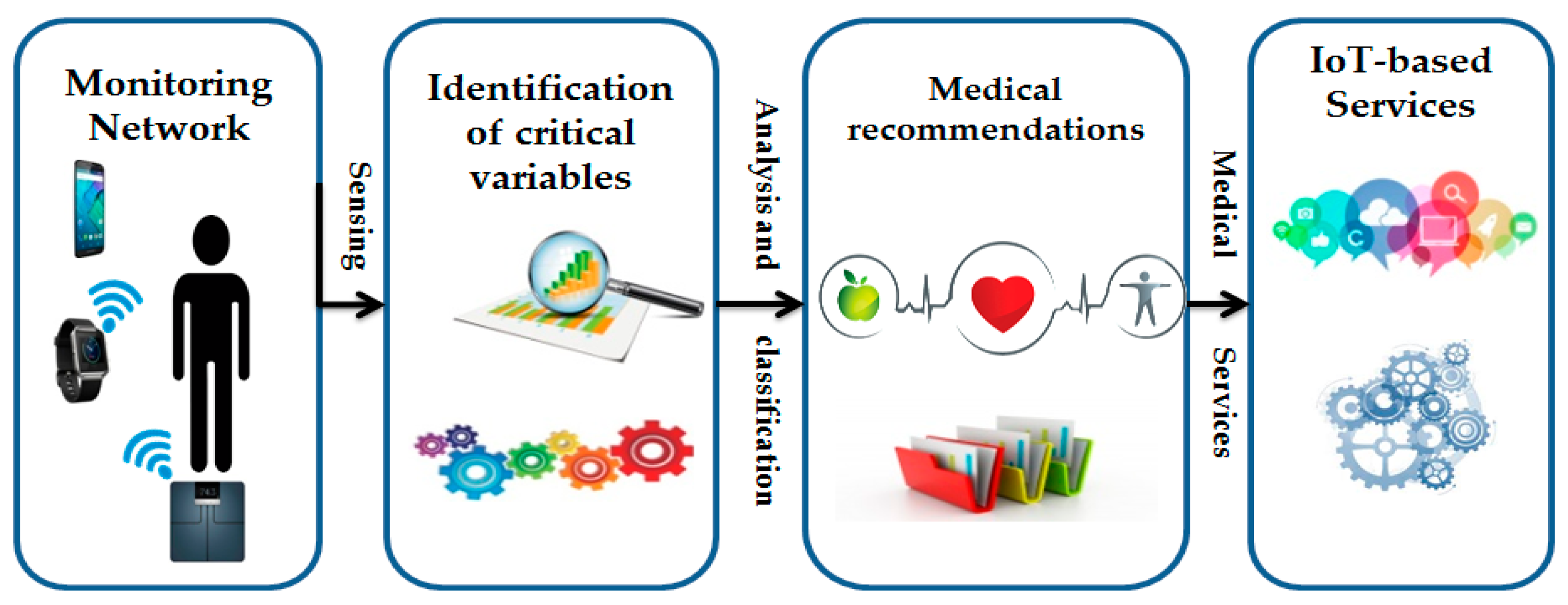
3.2.1. Monitoring Network Layer
- Wearable devices. Wearable devices are responsible for monitoring and collecting most of the biomedical variables, as well as other variables generated from the patient’s actions. The wearable devices in the IoT provide a high-tech infrastructure that enables communication and links between portable sensors to monitor a person’s activities, including but not limited to the person’s biomedical variables, behavior, and welfare, with the purpose of improving quality of life [15]. Wearable devices are classified according to their appearance, functionality, portability on the body, characteristics, and functional capacity in order to provide a better description of different sectors. For this reason, the authors of [47] classified wearable devices into smartwatch, smart eyewear, fitness tracker, smart clothing, wearable camera, and wearable biomedical device. PISIoT works with devices from some suppliers, but its scalability makes it possible to consider wearable devices from other suppliers.
- Smart devices. These devices are responsible for the smart collection of weight or other variables not identified by wearable devices (e.g., smart scale, temperature sensor, motion sensor). Smart devices are the driving force of the IoT because they provide fast and accurate information in real time and identify various patterns. In this sense, PISIoT includes some smart device suppliers but ensures that other smart device providers can be incorporated.
- Smartphones. Smartphones are in charge of maintaining communication between the devices, the providers, and PISIoT. The wearable devices used in the IoT lack an operating system as such; therefore, they must be linked to a smartphone or a computer with Internet access because the information collected by the devices must be safeguarded by the storage and support scheme of PISIoT and of its suppliers. PISIoT is multiplatform; however, depending on the model and provider of the wearable device that you wish to use, there are specific compatible smartphone models.
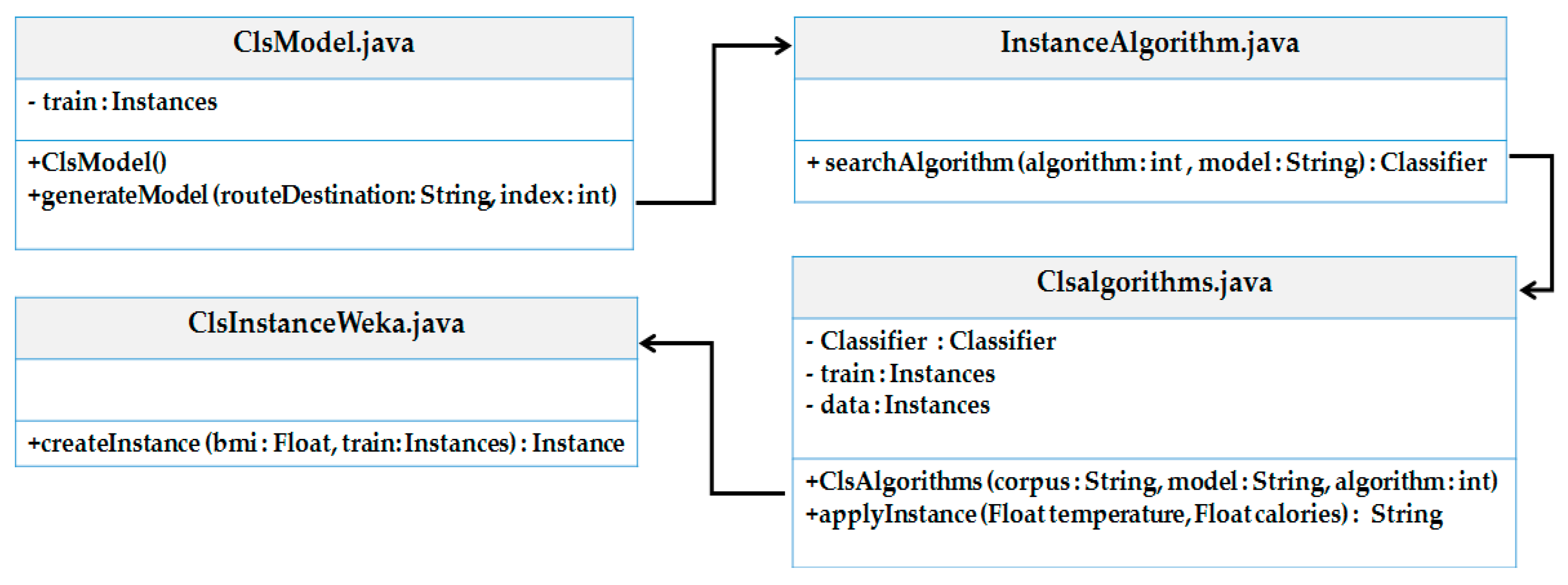
3.2.2. Data Analysis Layer
- ClsModel.java serves primarily to generate the model from the training set. In addition, it contains two methods, one to receive the data set and another to generate the model based on the data set received. The class starts with an instance of the “Instances” type called “train”. Likewise, the ClsModel constructor is sent, which, through the generateModel method, indicates the destination and the algorithm used. In addition, the searchAlgorithm method is invoked.
- InstanceAlgorithm.java contains the selection of the algorithm to be used. The method search Algorithm receives the algorithm selection and the model path.
- Clsalgorithms.java processes the data set, the model, and the incoming information to apply the corresponding algorithm, in addition to providing a timely response to the request. This class starts with a classifier of the “Classifier” type, train of the “Instances” type, and data object of the “Instances” type. In addition, it uses the applyInstance method to apply the changes made and designate the information to be analyzed. The ClsAlgorithms method also receives the model, the data set, and the algorithm to process the information and generate a response.
- ClsInstanceWeka.java generates an instance based on incoming information; this class is responsible for selecting the set of parameters to be processed. The CreateInstance method uses the Instances object and the number of elements contained in the data set, ignoring the class label.
3.2.3. IoT-Based Services Layer
3.2.4. Integration Layer
3.2.5. Presentation Layer
3.3. Case Study: Prevention of Myocardial Infarction in Elderly Patients with Obesity by Monitoring Biomedical Variables
- Elderly people with obesity need to know the number of calories ingested, calories burned, sleep, heart rate, the amount of water consumed, daily steps, and necessary physical activity to achieve gradual weight loss without health complications, helping to avoid myocardial infarction.
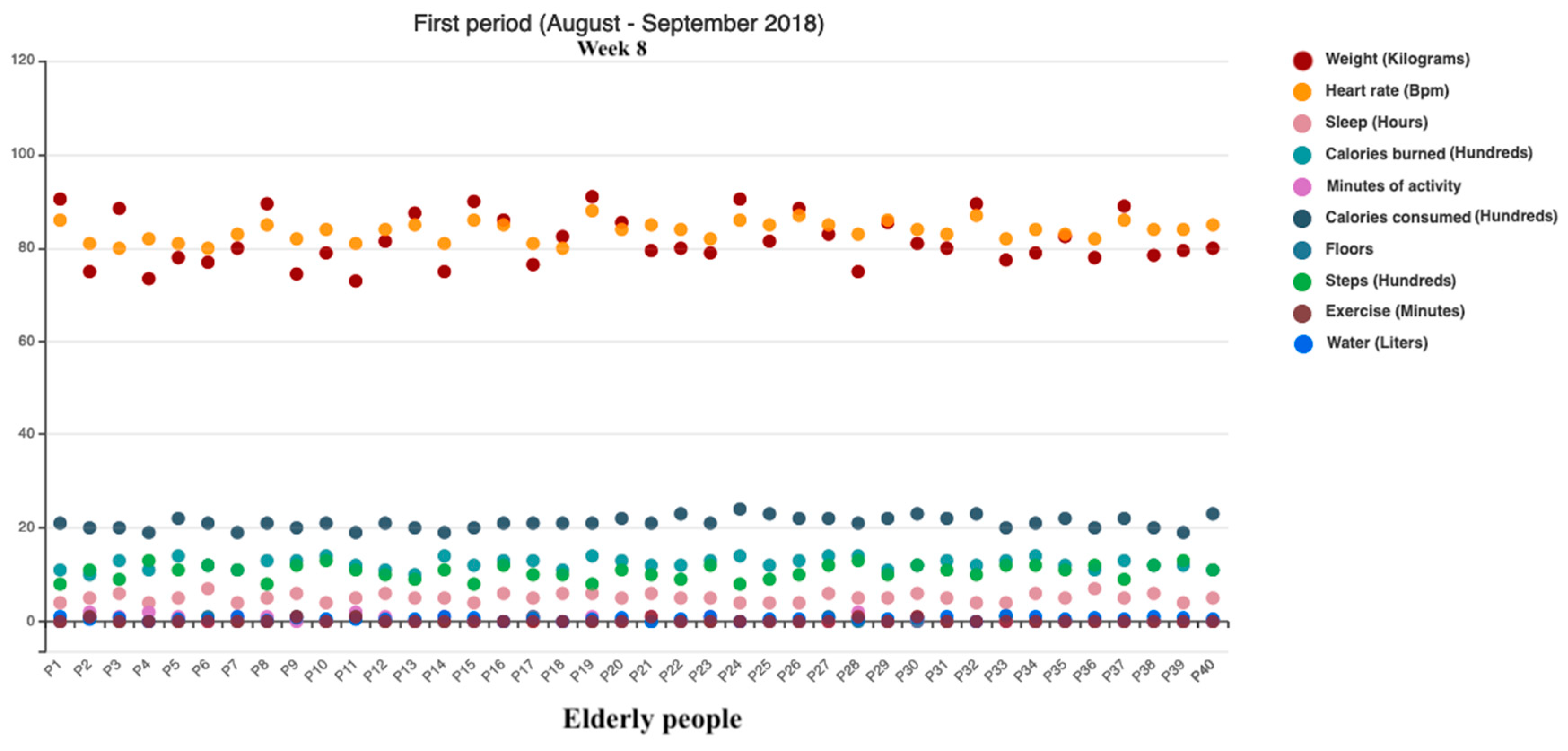
Methodology
- Initial monitoring was performed over a period of two months (August—September 2018) using the wearable device; at the end of that period, weight was obtained with the smart scale. Both devices were linked to a smartphone to send the data to the device provider. A relative of the patient recorded food and water consumption using the platform for the wearable device. During this period, only the mobile application for the wearable device and smart scale were used. These focused only on monitoring the patient’s biomedical variables and did not provide any type of alert or medical recommendation to lose weight.
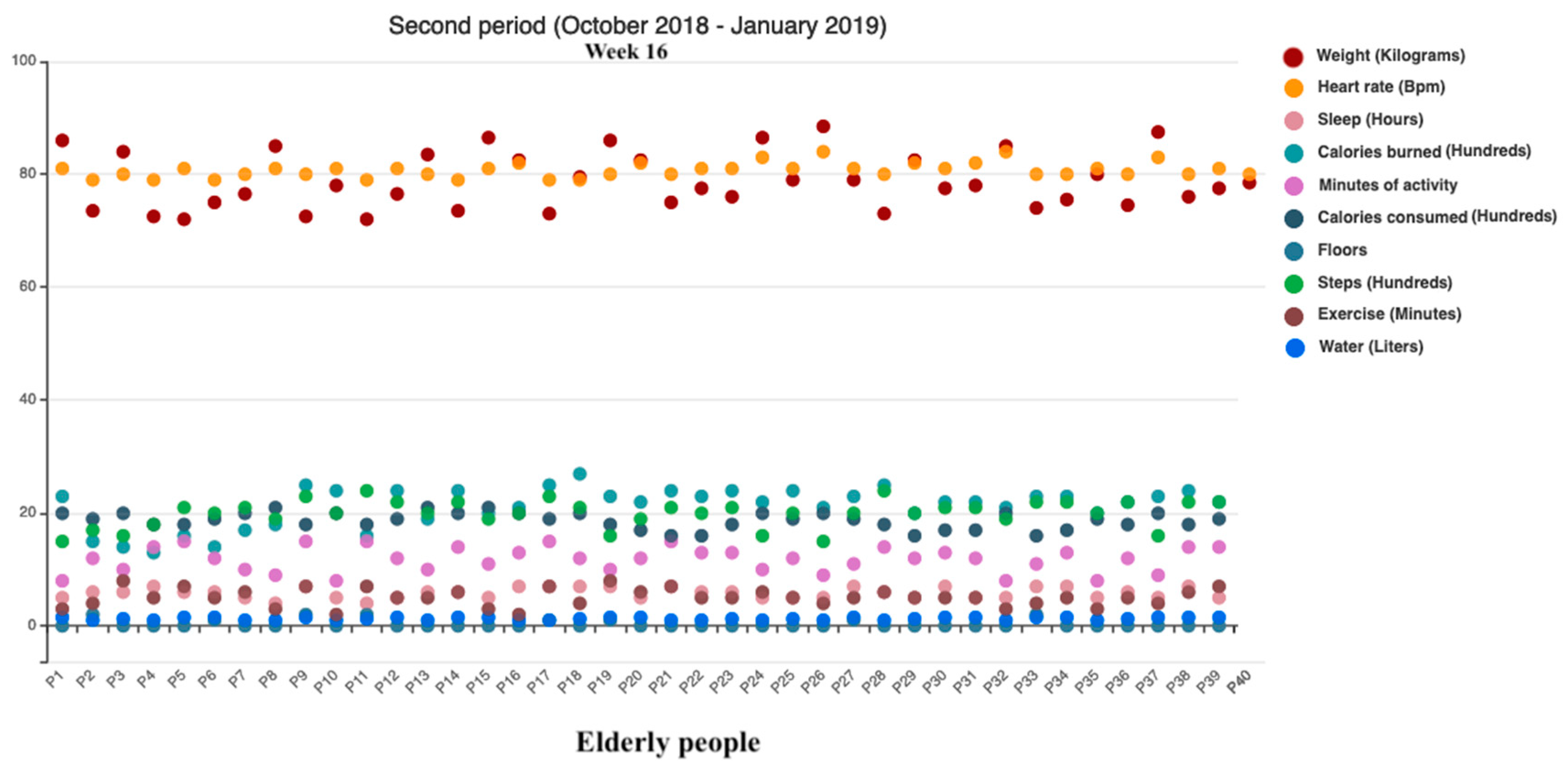
- Implementation of PISIoT. Afterwards, a second monitoring period ran for four months (October 2018—January 2019); the biomedical variables of the elderly people were requested from the device providers. Subsequently, the elderly patients’ BMI was calculated using the formula BMI = weight (kg) ÷ height2 (m) [1,61]. Then, the patients were classified to predict obesity with the classes ClsModel.java, Clsalgorithms.java, ClsInstanceWeka.java, and InstanceAlgorithm.java using the machine learning algorithm J48. Table 1 shows the classification used to determine the type of obesity according to the World Health Organization (WHO) [61]. In addition, the patient’s biomedical variables (heart rate, calories burned, sleep, minutes of physical activity, and weight) and other variables (steps, floors, calories consumed, distance traveled, water consumed, and exercise) were considered in the classification to describe the behavior of elderly patients with obesity. With the data obtained by the wearable device and smart scale, a dataset was created with 17 predictor attributes (calories consumed, calories burned, carbohydrates, fat, proteins, water consumed, exercise duration, heart rate during exercise, resting heart rate, minutes of physical activity at peak level, minutes at cardio level, minutes at fat burning level, steps, floors, distance traveled, sleep duration, and weight), one class label attribute (obesity), and 7200 instances; daily data were registered for each patient and classified as the type of obesity that patients will exhibit, according to the values of the predictor attributes, if they maintain this behavior.
- This made it possible to perform an analysis to identify possible critical variables that influence the emergence of obesity in elderly people, generate recommendations, and propose the IoT-based medical services that patients require to lose weight. The J48 algorithm has been adopted in PISIoT using the data set to obtain the predictive model with the 10-fold cross-validation technique. This kind of validation was used because, in general, it is recommended for estimation accuracy (even if computational power enables the use of more folds) due to its relatively low bias and variance [62]. Moreover, the J48 algorithm was selected since it was proven in previous studies to have performed better than other algorithms [63,64,65,66].
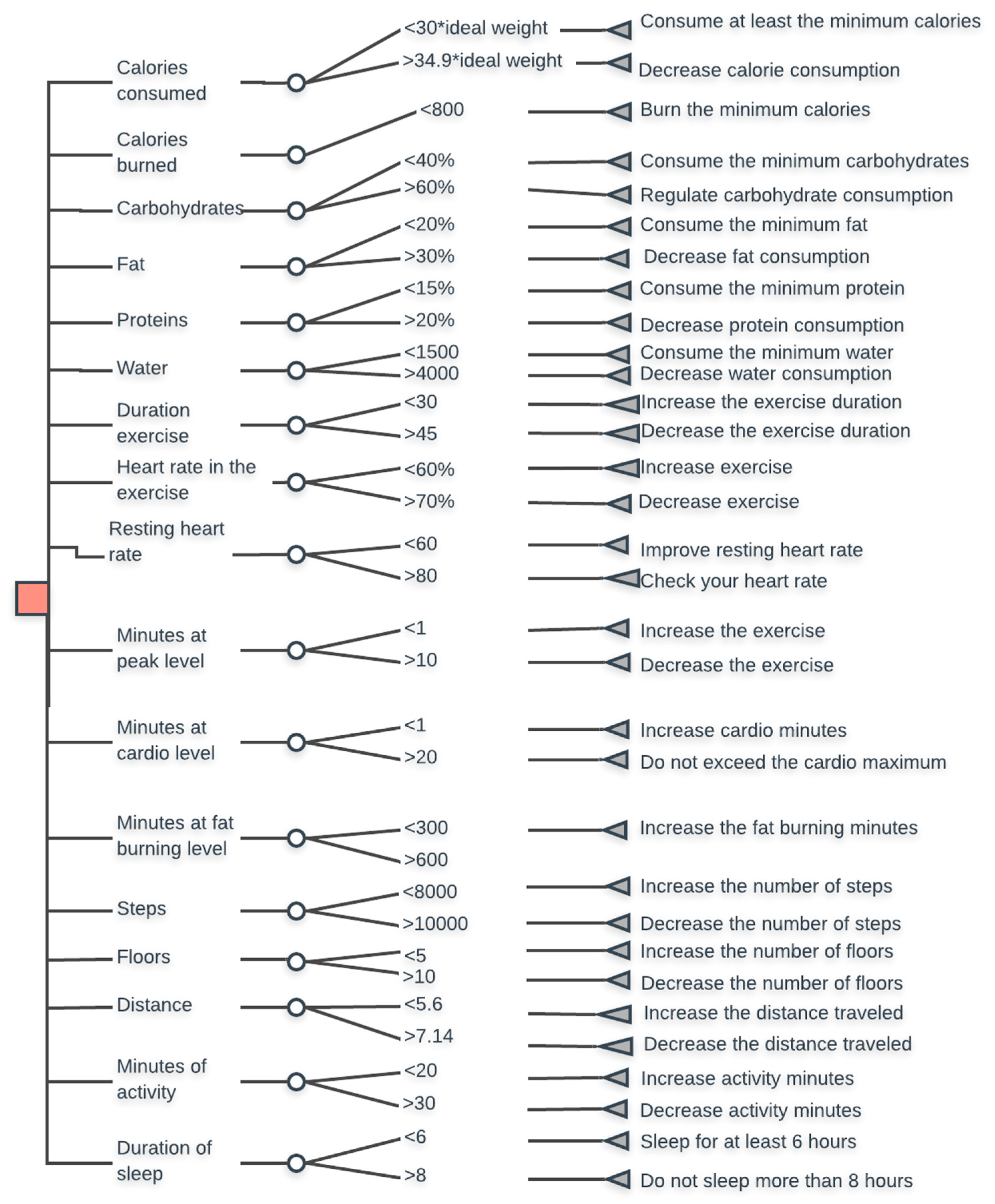
- Once the type of classification has been identified, the established rules are selected depending on the type of obesity. Likewise, with the formula weight = (height − 40)/2 [2], the patient’s ideal weight is identified, which serves as a basis to identify critical variables that are greater or smaller than the values permitted in each classification. Figure 7 shows the classification rules for obesity 1 and also includes recommendations based on the critical variables detected on a daily basis.
- The medical recommendations section is complex, as they influence different factors. For this reason, the decrease in calories should be gradual, that is, portions of 500 kcal every 2 weeks to avoid any decompensation. Patients should not attempt to accelerate the process or exceed the limits established by the PISIoT.
- If the patient does not follow the daily recommendations issued by the PISIoT, after a period of time, a greater medical recommendation is generated. Table 2 presents the rules for recommendations for patients with any type of obesity, which were made by specialized healthcare personnel (two doctors, a nutritionist with a master’s degree in food and nutritional health, and a nurse with a master’s degree in public health). The table includes the column “Variable”, which gives the variable used; “Rule”, which specifies the rule for the recommendation; “Frequency”, which is how often the analysis is made; and “Recommendation”, which contains the recommendation to be given if the rule is not met. The rules described above identify and describe the operation of the medical recommendation process, which aims to improve quality of life in a manner that is simple, gradual and non-invasive, and the use of the values obtained by the smart devices and those entered by the patient or the patient’s family member.
- These recommendations also include the medical services that patients require to achieve their goal of weight control or loss (clinical analysis, nutritionist or cardiologist). The medical recommendations and suggested medical services were validated by specialized healthcare personnel. The elderly patients monitored in this second period showed progress in weight loss from using PISIoT, which performs real-time monitoring, identifies critical variables that lead to weight gain, analyzes biomedical variables through machine learning techniques, provides recommendations for weight loss, and is monitored and supported by experts in healthcare.
- Finally, the elderly people were monitored again for four more months (February–May 2019) to evaluate PISIoT’s contribution and impact on the elderly patients’ weight loss and health. This third period was proposed to verify PISIoT’s contribution to weight loss and/or an improvement to elderly people’s health, reducing the risk of a myocardial infarction or obesity-related diseases. In addition, in this period, the increase in elderly people’s outlook and quality of life was evaluated following the recommendations provided by PISIoT.
4. Results and Discussion
4.1. Monitoring Analysis
4.2. Findings
- Weight gain in patients is due to an increase in calorie consumption, few or no minutes of physical activity, a reduction in the number of steps and floors, little exercise, little or no water consumption, and a decrease in calories burned, and this is likely to produce an increase in heart rate.
- High cardiac frequency in patients correlates with other variables such as an increase in sleep and, hence, in weight due to a decrease in minutes of physical activity, exercise, steps, floors, and calories burned.
- Little sleep correlates with an increase in heart rate and, consequently, increased calorie consumption. Likewise, there is a decrease in calories burned and, consequently, a possible increase in weight.
- A lack of calories burned correlates with low physical activity, steps, and exercise, and there is an increase in heart rate, sleep, and possibly weight.
- Increased physical activity contributes to an increase in the number of steps, floors, and exercise, and an improvement in heart rate is possible. In addition, there is an increase in calories burned, and if the same calorie intake is maintained, weight decreases.
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 10 May 2019).
- D’Hyver, C.; Gutiérrez Robledo, L.M. Geriatrics, 3rd ed.; Modern Manual: Mexico City, Mexico, 2014; pp. 2–13. [Google Scholar]
- Health Secretary. Technical Guide for the National Health Book—Adults over 60 Years of Age or Older, 1st ed.; Health Secretary: Mexico City, Mexico, 2008; pp. 13–20. [Google Scholar]
- Lin, Q.; Zhang, D.; Connelly, K.; Ni, H.; Yu, Z.; Zhou, X. Disorientation detection by mining GPS trajectories for cognitively-impaired elders. Pervasive Mob. Comput. 2015, 19, 71–85. [Google Scholar] [CrossRef]
- Mexican Social Security Institute. Evaluation and Nutritional Monitoring Elderly in the Care First Level; Quick Reference Guide, IMSS-095-08; CENETEC: Mexico City, Mexico, 2014; pp. 2–13. [Google Scholar]
- Li, L.; Li, S.; Zhao, S. QoS-Aware Scheduling of Services-Oriented Internet of Things. IEEE Trans. Ind. Inform. 2014, 10, 1497–1505. [Google Scholar]
- Xu, L.D.; He, W.; Li, S. Internet of Things in Industries: A Survey. IEEE Trans. Ind. Inform. 2014, 10, 2233–2243. [Google Scholar] [CrossRef]
- Hantao, H.; Hao, Y. Compact and Fast Machine Learning Accelerator for IoT Devices; Computer Architecture and Design Methodologies; Springer: Singapore, 2019; pp. 9–11. [Google Scholar] [CrossRef]
- Bhatt, Y.; Bhatt, C. Internet of Things in HealthCare. In Internet of Things and Big Data Technologies for Next Generation Healthcare; Bhatt, C., Dey, N., Ashour, A.S., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; Volume 23, pp. 13–33. [Google Scholar] [CrossRef]
- Vazquez-Briseno, M.; Navarro-Cota, C.; Nieto-Hipólito, J.; Jiménez-García, E.; Sanchez-Lopez, J. A proposal for using the internet of things concept to increase children’s health awareness. In Proceedings of the CONIELECOMP 2012, 22nd International Conference on Electrical Communications and Computers, Puebla, Mexico, 27–29 February 2012; pp. 168–172. [Google Scholar]
- Vilallonga, R.; Lecube, A.; Fort, J.M.; Boleko, M.A.; Hidalgo, M.; Armengol, M. Internet of Things and bariatric surgery follow-up: Comparative study of standard and IoT follow-up. Minim. Invasive Ther. Allied Technol. 2013, 22, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.M.; Ouyang, J. Application Protocol adapted to Health Awareness for Smart Healthcare Service. Adv. Sci. Technol. Lett. 2013, 43, 101–104. [Google Scholar]
- Zaragozá, I.; Guixeres, J.; Alcañiz, M.; Cebolla, A.; Saiz, J.; Álvarez, J. Ubiquitous monitoring and assessment of childhood obesity. Pers. Ubiquit. Comput. 2013, 17, 1147–1157. [Google Scholar] [CrossRef]
- Lee, B.M.; Ouyang, J. Intelligent Healthcare Service by using Collaborations between IoT Personal Health Devices. Int. J. Bio-Sci. Bio-Technol. 2014, 6, 155–164. [Google Scholar] [CrossRef]
- Hiremath, S.; Yang, G.; Mankodiya, K. Wearable Internet of Things: Concept, Architectural Components and Promises for Person-Centered Healthcare. In Proceedings of the 4th International Conference on Wireless Mobile Communication and Healthcare—Transforming Healthcare Through Innovations in Mobile and Wireless Technologies (MOBIHEALTH), Athens, Greece, 3–5 November 2014; pp. 304–307. [Google Scholar]
- Vázquez, M.; Jimenez, E.; Nieto, J.I.; Sánchez, J.D.D.; Garcia, A.; Torres, J.P. Development of a Mobile Health Architecture to Prevent Childhood Obesity. IEEE Lat. Am. Trans. 2015, 13, 1520–1527. [Google Scholar] [CrossRef]
- Kim, K.K.; Logan, H.C.; Young, E.; Sabee, C.M. Youth-centered design and usage results of the iN Touch mobile self-management program for overweight/obesity. Pers. Ubiquit. Comput. 2015, 9, 59–68. [Google Scholar] [CrossRef]
- Alloghani, M.; Hussain, A.; AI-Jumeily, D.; Fergus, P.; Abuelma’atti, O.; Hamden, H. A Mobile Health Monitoring Application for Obesity Management and Control Using the Intemet-of-Things. In Proceedings of the 2016 Sixth International Conference on Digital Information Processing and Communications (ICDIPC), Beirut, Lebanon, 21–23 April 2016; pp. 19–24. [Google Scholar] [CrossRef]
- Wibisono, G.; Astawa, I.G.B. Designing Machine-to-Machine (M2M) Prototype System for Weight Loss Program for Obesity and Overweight Patients. In Proceedings of the 2016 7th International Conference on Intelligent Systems, Modelling and Simulation (ISMS), Bangkok, Thailand, 25–27 January 2016; pp. 138–143. [Google Scholar]
- Dobbins, C.; Rawassizadeh, R.; Momeni, E. Detecting physical activity within lifelogs towards preventing obesity and aiding ambient assisted living. Neurocomputing 2016, 230, 1–23. [Google Scholar] [CrossRef]
- Shin, S.-A.; Lee, N.-Y.; Park, J.-H. Empirical study of the IoT-learning for obese patients that require personal training. In Advances in Computer Science and Ubiquitous Computing; Park, J.J., Pan, Y., Yi, G., Loia, V., Eds.; Springer: Singapore, 2017; Volume 421, pp. 1005–1012. [Google Scholar] [CrossRef]
- Aupetit, M.; Fernandez-Luque, L.; Singh, M.; Srivastava, J. Visualization of Wearable Data and Biometrics for Analysis and Recommendations in Childhood Obesity. In Proceedings of the 2017 IEEE 30th International Symposium on Computer-Based Medical Systems (CBMS), Thessaloniki, Greece, 22–24 June 2017; pp. 678–679. [Google Scholar]
- Yang, H.J.; Kang, J.-H.; Kim, O.H.; Choi, M.; Oh, M.; Nam, J.; Sung, E. Interventions for Preventing Childhood Obesity with Smartphones and Wearable Device: A Protocol for a Non-Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2017, 14, 184. [Google Scholar] [CrossRef] [PubMed]
- Laing, B.; Mangione, C.; Tseng, C.; Leng, M.; Vaisberg, E.; Mahida, M.; Bholat, M.; Glazier, E.; Morisky, D.; Bell, D. Effectiveness of a Smartphone Application for Weight Loss Compared with Usual Care in Overweight Primary Care Patients. Ann. Intern. Med. 2014, 161, S5–S12. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.U.; Bjorkman, M.; Causevic, A.; Fotouhi, H.; Lindén, M. An Overview on the Internet of Things for Health Monitoring Systems. Internet Things IoT Infrastruct. 2016, 429–436. [Google Scholar] [CrossRef]
- Fernández-Caballero, A.; Fern, A. Improvement of the Elderly Quality of Life and Care through Smart Emotion Regulation Improvement of the Elderly Quality of Life and Care through Smart Emotion Regulation. In Proceedings of the 6th International Work-Conference, IWAAL 2014, Belfast, UK, 2–5 December 2014; pp. 348–355. [Google Scholar] [CrossRef]
- Chetty, G.; White, M.; Akther, F. Smart Phone Based Data Mining for Human Activity Recognition. Procedia Comput. Sci. 2015, 46, 1181–1187. [Google Scholar] [CrossRef]
- Hussain, A.; Wenbi, R.; Da Silva, A.L.; Nadher, M.; Mudhish, M. Health and emergency-care platform for the elderly and disabled people in the Smart City. J. Syst. Softw. 2015, 110, 253–263. [Google Scholar] [CrossRef]
- Muralidharan, S.; Ranjani, H.; Anjana, R.M.; Allender, S.; Mohan, V. Mobile Health Technology in the Prevention and Management of Type 2 Diabetes. Indian J. Endocrinol. Metab. 2017, 21, 334–340. [Google Scholar] [PubMed]
- Mathai, M.; Ginige, A.; Srinivasan, U.; Girosi, F.; Au, M.H.A.; Castiglione, A.; Choo, K.-K.R.; Palmieri, F.; Li, K.-C. Digital Knowledge Ecosystem for Empowering Users to Self-manage Diabetes through Context Specific Actionable Information. In Green, Pervasive, and Cloud Computing: 12th International Conference, GPC 2017, Cetara, Italy; Au, A., Castiglione, A., Choo, K.-K.R., Palmieri, F., Li, K.-C., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 672–684. [Google Scholar] [CrossRef]
- Miah, S.J.; Hasan, N.; Hasan, R.; Gammack, J. Healthcare support for underserved communities using a mobile social media platform. Inf. Syst. 2017, 66, 1–12. [Google Scholar] [CrossRef]
- Lim, S.; Tucker, C.S.; Kumara, S. An unsupervised machine learning model for discovering latent infectious diseases using social media data. J. Biomed. Inform. 2017, 66, 82–94. [Google Scholar] [CrossRef]
- De Ramón-Fernández, A.; Ruiz-Fernández, D.; Ramírez-Navarro, J.; Marcos-Jorquera, D.; Gilart-Iglesias, V.; Soriano-Payá, A. Architecture of a Monitoring System for Hipertensive Patients. In Biomedical Applications Based on Natural and Artificial Computing: International Work-Conference on the Interplay between Natural and Artificial Computation, IWINAC 2017, Corunna, Spain, 19–23 June 2017, Proceedings, Part II; Vicente, J.M.F., Álvarez-Sánchez, J.R., López, F.D., Moreo, J.T., Adeli, H., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 473–480. [Google Scholar] [CrossRef]
- Jeong, J.-S.; Han, O.; You, Y.-Y. A Design Characteristics of Smart Healthcare System as the IoT Application. Indian J. Sci. Technol. 2016, 9, 1–8. [Google Scholar] [CrossRef]
- Maharaj, B.T.; Gupta, P.K.; Malekian, R. A novel and secure IoT based cloud centric architecture to perform predictive analysis of users activities in sustainable health centres. Multimed. Tools Appl. 2016, 76, 18489–18512. [Google Scholar]
- Chen, M.; Ma, Y.; Song, J.; Lai, C.-F.; Hu, B. Smart Clothing: Connecting Human with Clouds and Big Data for Sustainable Health Monitoring. Mob. Netw. Appl. 2016, 21, 825–845. [Google Scholar] [CrossRef]
- Jung, H. A conceptual framework for trajectory-based medical analytics with IoT contexts. J. Comput. Syst. Sci. 2016, 82, 610–626. [Google Scholar] [CrossRef]
- Santos, J.; Rodrigues, J.P.C.; Silva, B.; Casal, J.; Saleem, K.; Denisov, V. An IoT-based mobile gateway for intelligent personal assistants on mobile health environments. J. Netw. Comput. Appl. 2016, 71, 194–204. [Google Scholar] [CrossRef]
- Hossain, M.S.; Muhammad, G. Cloud-assisted Industrial Internet of Things (IIoT)—Enabled framework for health monitoring. Comput. Netw. 2016, 101, 192–202. [Google Scholar] [CrossRef]
- Ganzha, M.; Paprzycki, M.; Pawłowski, W.; Szmeja, P.; Wasielewska, K. Semantic interoperability in the Internet of Things: An overview from the INTER-IoT perspective. J. Netw. Comput. Appl. 2016, 81, 1–23. [Google Scholar] [CrossRef]
- Raza, M.; Hoa Le, M.; Aslam, N.; Hieu Le, C.; Tam Le, N.; Ly Le, T. Telehealth Technology: Potentials, Challenges and Research Directions for Developing Countries. IFMBE Proc. 2017, 63, 523–528. [Google Scholar]
- Camara-Brito, J.M. Trends in wireless communications towards 5G networks—The influence of e-health and IoT applications. In Proceedings of the International Multidisciplinary Conference on Computer and Energy Science (SpliTech), Split, Croatia, 13–15 July 2016; pp. 1–7. [Google Scholar] [CrossRef]
- Ifrim, C.; Pintilie, A.-M.; Apostol, E.; Dobre, C.; Pop, F. The art of advanced healthcare applications in big data and IoT systems. In Advances in Mobile Cloud Computing and Big Data in the 5G Era; Mavromoustakis, C.X., Mastorakis, G., Dobre, C., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; Volume 22, pp. 133–149. [Google Scholar] [CrossRef]
- Ouaddah, A.; Mousannif, H.; Elkalam, A.A.; Ouahman, A.A. Access control in the Internet of Things: Big challenges and new opportunities. Comput. Netw. 2017, 112, 237–262. [Google Scholar] [CrossRef]
- Goudos, S.K.; Dallas, P.I.; Chatziefthymiou, S.; Kyriazakos, S. A Survey of IoT Key Enabling and Future Technologies: 5G, Mobile IoT, Sematic Web and Applications. Wirel. Pers. Commun. 2017, 97, 1645–1675. [Google Scholar] [CrossRef]
- Trappey, A.J.; Trappey, C.V.; Govindarajan, U.H.; Chuang, A.C.; Sun, J.J. A review of essential standards and patent landscapes for the Internet of Things: A key enabler for Industry 4.0. Adv. Eng. Inform. 2017, 33, 208–229. [Google Scholar] [CrossRef]
- Mardonova, M.; Choi, Y. Review of Wearable Device Technology and Its Applications to the Mining Industry. Energies 2018, 11, 547. [Google Scholar] [CrossRef]
- Sathyadevi, G. Application of CART algorithm in hepatitis disease diagnosis. In Proceedings of the 2011 International Conference on Recent Trends in Information Technology (ICRTIT), Tamil Nadu, India, 3–5 June 2011; pp. 1283–1287. [Google Scholar]
- Pattanapairoj, S.; Silsirivanit, A.; Muisuk, K.; Seubwai, W.; Cha’On, U.; Vaeteewoottacharn, K.; Sawanyawisuth, K.; Chetchotsak, D.; Wongkham, S. Improve discrimination power of serum markers for diagnosis of cholangiocarcinoma using data mining-based approach. Clin. Biochem. 2015, 48, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Tartar, A.; Kilic, N.; Akan, A. A new method for pulmonary nodule detection using decision trees. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July 2013; pp. 7355–7359. [Google Scholar] [CrossRef]
- Chen, X.; Ching, W.-K.; Aoki-Kinoshita, K.F.; Furuta, K. Support Vector Machine Methods for the Prediction of Cancer Growth. In Proceedings of the 2010 Third International Joint Conference on Computational Science and Optimization, Huangshan, China, 28–31 May 2010; pp. 229–232. [Google Scholar] [CrossRef]
- Shoaip, N.; Elmogy, M.M.; Riad, A.M.; Zaghloul, H.; Badria, F.A.; Giannoccaro, I.; Hassanien, A.E.; Gaber, T. Early-Stage Ovarian Cancer Diagnosis Using Fuzzy Rough Sets with SVM Classification. In Handbook of Research on Machine Learning Innovation and Trends; IGI Global: Hershey, PA, USA, 2017; pp. 43–60. [Google Scholar]
- Subbalakshmi, G.; Ramesh, K.; Rao, C. Decision Support in Hearth Disease Prediction System using Naive Bayes. Indian J. Comput. Sci. Eng. 2011, 2, 170–176. [Google Scholar]
- Fageeri, S.O.; Ahmed, S.M.M.; Almubarak, S.A.; Mu’Azu, A.A. Eye refractive error classification using machine learning techniques. In Proceedings of the 2017 International Conference on Communication, Control, Computing and Electronics Engineering (ICCCCEE), Khartoum, Sudan, 16–18 January 2017; pp. 1–6. [Google Scholar] [CrossRef]
- Hashemi, A.; Pilevar, A.H.; Rafeh, R.; Moallem, P.; Karimizadeh, A.; Yazdchi, M. Mass Detection in Lung CT Images Using Region Growing Segmentation and Decision Making Based on Fuzzy Inference System and Artificial Neural Network. Int. J. Image Graph. Signal Process. 2013, 5, 16–24. [Google Scholar] [CrossRef]
- Abdalla, A.M.M.; Dress, S.; Zaki, N. Detection of Masses in Digital Mammogram Using Second Order Statistics and Artificial Neural Network. Int. J. Comput. Sci. Inf. Technol. 2011, 3, 176–186. [Google Scholar] [CrossRef]
- Yang, Y.; Chen, H.; Wang, D.; Luo, W.; Zhu, B.; Zhang, Z. Diagnosis of pancreatic carcinoma based on combined measurement of multiple serum tumor markers using artificial neural network analysis. Chin. Med. J. 2014, 127, 1891–1896. [Google Scholar] [PubMed]
- Kureshi, N.; Abidi, S.S.R.; Blouin, C. A Predictive Model for Personalized Therapeutic Interventions in Non-small Cell Lung Cancer. IEEE J. Biomed. Health Inform. 2016, 20, 424–431. [Google Scholar] [CrossRef] [PubMed]
- Sood, S.K.; Mahajan, I. A Fog-Based Healthcare Framework for Chikungunya. IEEE Internet Things J. 2018, 5, 794–801. [Google Scholar] [CrossRef]
- World Health Organization. Cardiovascular Disease. Available online: https://www.who.int/cardiovascular_diseases/en/ (accessed on 17 May 2019).
- World Health Organization. Global Strategy on Diet, Physical Activity and Health. Available online: https://www.who.int/dietphysicalactivity/childhood/en/ (accessed on 19 May 2019).
- Han, J.; Kamber, M.; Pei, J. Classification: Basic Concepts, Chapter 8, Data Mining: Concepts and Techniques, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2012; pp. 327–391. ISBN 978-0-12-381479-1. [Google Scholar]
- Dugan, T.M.; Mukhopadhyay, S.; Carroll, A.; Downs, S. Machine Learning Techniques for Prediction of Early Childhood Obesity. Appl. Clin. Inform. 2015, 6, 506–520. [Google Scholar]
- Abdullah, F.S.; Nor Manan, S.A.; Ahmad, A.; Wafa, S.W.; Shahril, M.R.; Zulaily, N.; Amin, R.M.; Ahmed, A. Data Mining Techniques for Classification of Childhood Obesity Among Year 6 School Children. In Proceedings of the Recent Advances on Soft Computing and Data Mining: The Second International Conference on Soft Computing and Data Mining (SCDM-2016), Bandung, Indonesia, 18–20 August 2016; pp. 465–474. [Google Scholar] [CrossRef]
- Daud, N.; Noor, N.L.M.; Aljunid, S.A.; Noordin, N.; Teng, N.I.M.F. Predictive Analytics: The Application of J48 Algorithm on Grocery Data to Predict Obesity. In Proceedings of the 2018 IEEE Conference on Big Data and Analytics (ICBDA), Langkawi Island, Malaysia, 21–22 November 2018; pp. 1–6. [Google Scholar] [CrossRef]
- De-La-Hoz-Correa, E.; Mendoza Palechor, F.; De-La-Hoz-Manotas, A.; Morales Ortega, R.; Sánchez Hernández, A.B. Obesity Level Estimation Software based on Decision Trees. J. Comput. Sci. 2019, 15, 1–11. [Google Scholar] [CrossRef]



| Classification | Minimum Value | Maximum Value |
|---|---|---|
| Normal | 18.50 | 24.99 |
| Overweight | 25.00 | 29.99 |
| Obesity 1 | 30.00 | 34.99 |
| Obesity 2 | 35.00 | 39.99 |
| Obesity 3 | 40.00 | + |
| Variable | Rule | Frequency | Recommendation |
|---|---|---|---|
| Calories consumed | >(20 * ideal weight) | 3 times per week | Watch food intake due to possible increase in BMI |
| Calories consumed | <1500 | 3 times per week | Request clinical analysis service and seek medical evaluation |
| Exercise | <75 | Per week | Perform exercise |
| Heart rate | >100 or <60 | 3 times per week | Go to medical assessment |
| Minutes at peak level | >10 | 3 times per week | Go to medical assessment |
| Resting heart rate | >120 or < 40 | At all times | Request ambulance; possible tachycardia or infarction. Request cardiologist service |
| Weight | (Weight)2 * 34.9 | Per month | Request a nutritionist service for a new nutritional plan |
| Weight | (Weight)2 * 30 | Per month | Request a nutritionist service for a new nutritional plan |
| Sleep | <6 | Every 3 days | You should sleep at least 8 h a day |
| Sleep | >8 | Every 3 days | Stay active |
| Biomedical Variables | Weight | Heart Rate | Sleep | Calories Burned | Minutes of Physical Activity |
|---|---|---|---|---|---|
| Variables correlation | Calories consumed | Sleep | Heart rate | Minutes of physical activity | Steps |
| Minutes of physical activity | Minutes of physical activity | Calories burned | Steps | Floors | |
| Steps | Exercise | Calories consumed | Floors | Exercise | |
| Floors | Steps | Weight | Exercise | Heart rate | |
| Exercise | Floors | Heart rate | Calories burned | ||
| Water | Calories consumed | Weight | Calories consumed | ||
| Heart rate | Weight | Sleep | Weight | ||
| Calories burned |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Machorro-Cano, I.; Alor-Hernández, G.; Paredes-Valverde, M.A.; Ramos-Deonati, U.; Sánchez-Cervantes, J.L.; Rodríguez-Mazahua, L. PISIoT: A Machine Learning and IoT-Based Smart Health Platform for Overweight and Obesity Control. Appl. Sci. 2019, 9, 3037. https://doi.org/10.3390/app9153037
Machorro-Cano I, Alor-Hernández G, Paredes-Valverde MA, Ramos-Deonati U, Sánchez-Cervantes JL, Rodríguez-Mazahua L. PISIoT: A Machine Learning and IoT-Based Smart Health Platform for Overweight and Obesity Control. Applied Sciences. 2019; 9(15):3037. https://doi.org/10.3390/app9153037
Chicago/Turabian StyleMachorro-Cano, Isaac, Giner Alor-Hernández, Mario Andrés Paredes-Valverde, Uriel Ramos-Deonati, José Luis Sánchez-Cervantes, and Lisbeth Rodríguez-Mazahua. 2019. "PISIoT: A Machine Learning and IoT-Based Smart Health Platform for Overweight and Obesity Control" Applied Sciences 9, no. 15: 3037. https://doi.org/10.3390/app9153037
APA StyleMachorro-Cano, I., Alor-Hernández, G., Paredes-Valverde, M. A., Ramos-Deonati, U., Sánchez-Cervantes, J. L., & Rodríguez-Mazahua, L. (2019). PISIoT: A Machine Learning and IoT-Based Smart Health Platform for Overweight and Obesity Control. Applied Sciences, 9(15), 3037. https://doi.org/10.3390/app9153037