Estimating Airway Resistance from Forced Expiration in Spirometry
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Pulmonary Function Tests
2.2.1. Spirometry
2.2.2. Whole-body Plethysmography
2.2.3. Diffusion Capacity
2.3. Computed Tomography Densiometry
2.4. Airway Resistance from Spirometry
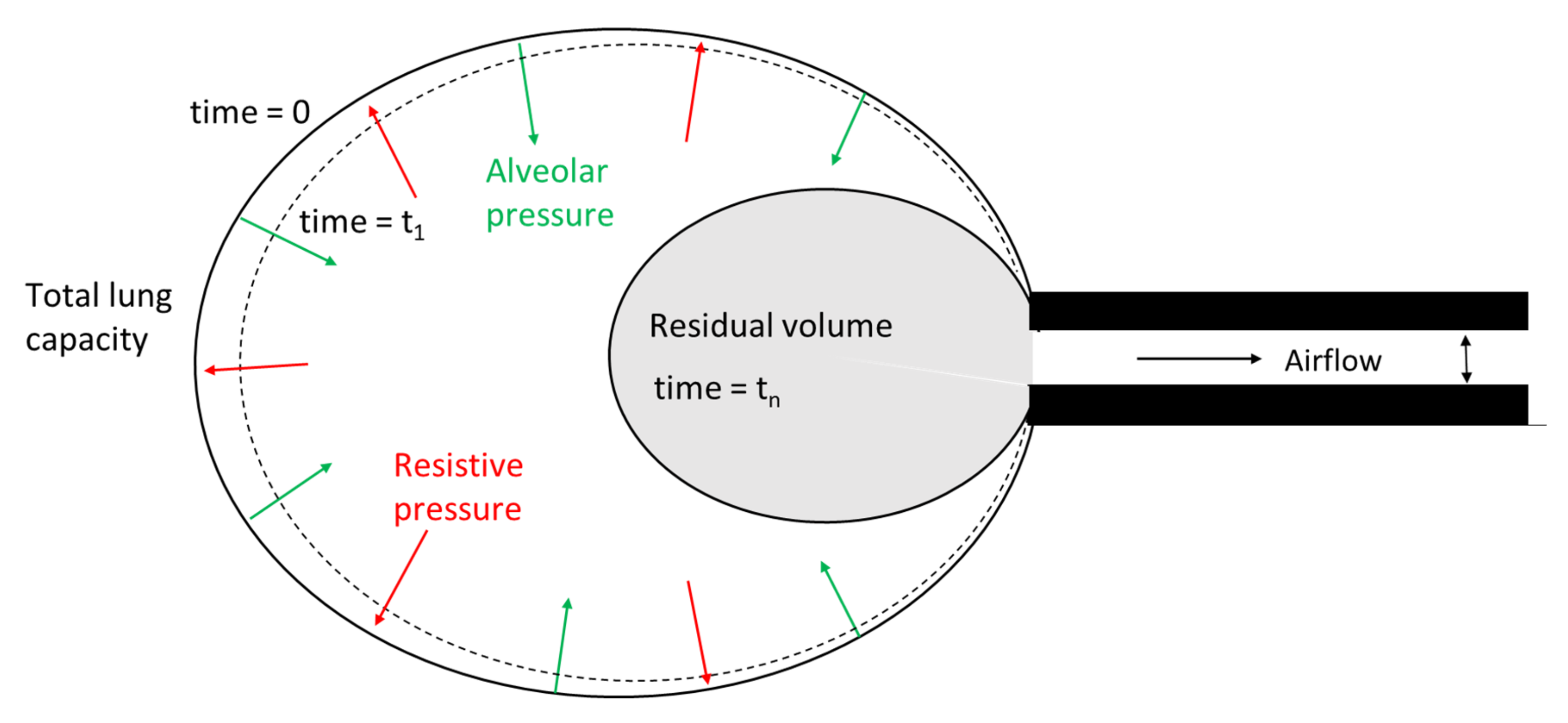
2.4.1. Deflating Balloon Model of Forced Expiration
2.4.2. Estimation of ζ
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.1.1. Study Population
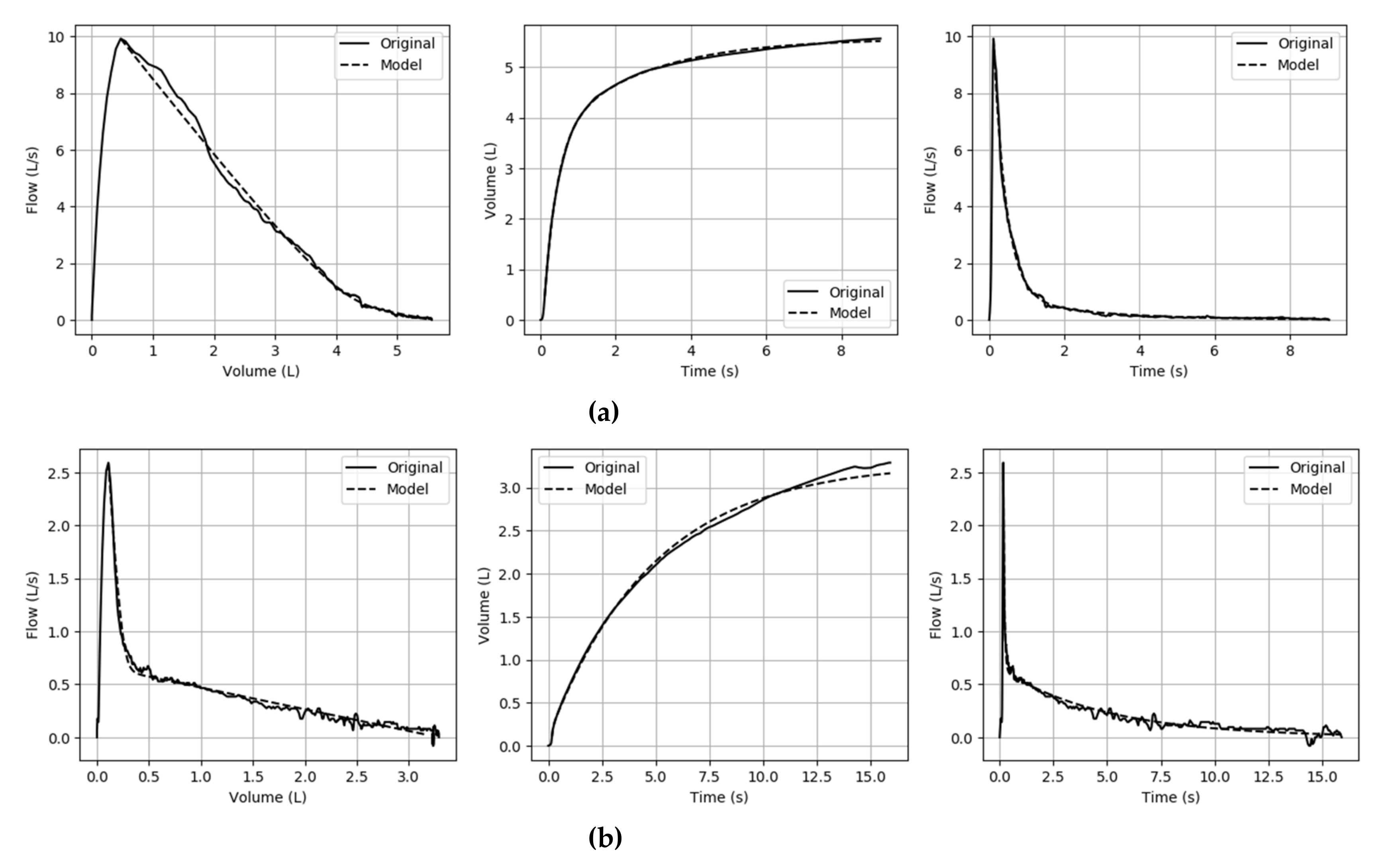
3.1.2. Model Fit
3.1.3. Model Parameters
3.2. Association Studies of ζ
3.2.1. Spirometry
3.2.2. Raw and sGaw
3.2.3. DLCO and RV/TLC
3.2.4. CT Densitometry
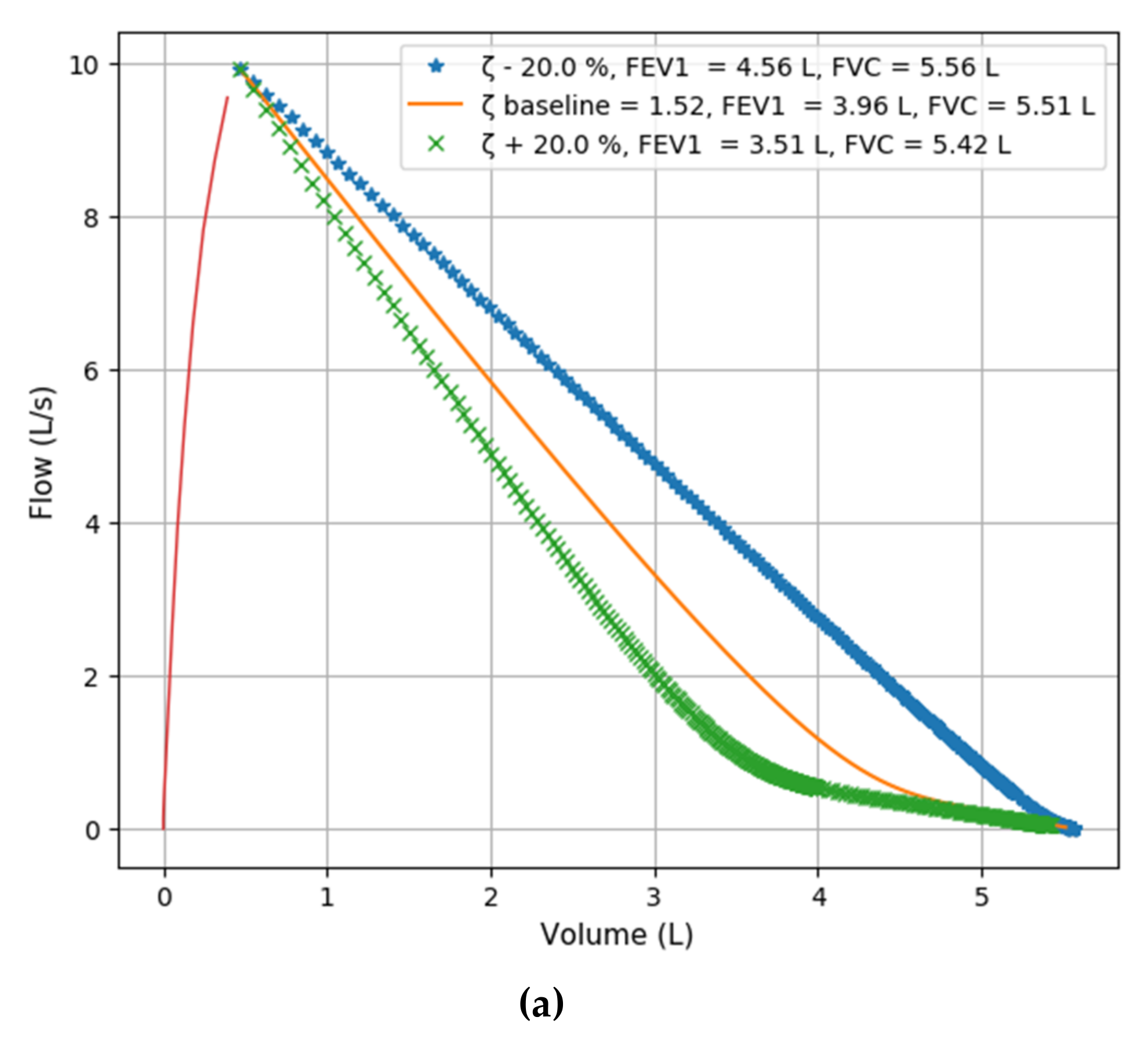
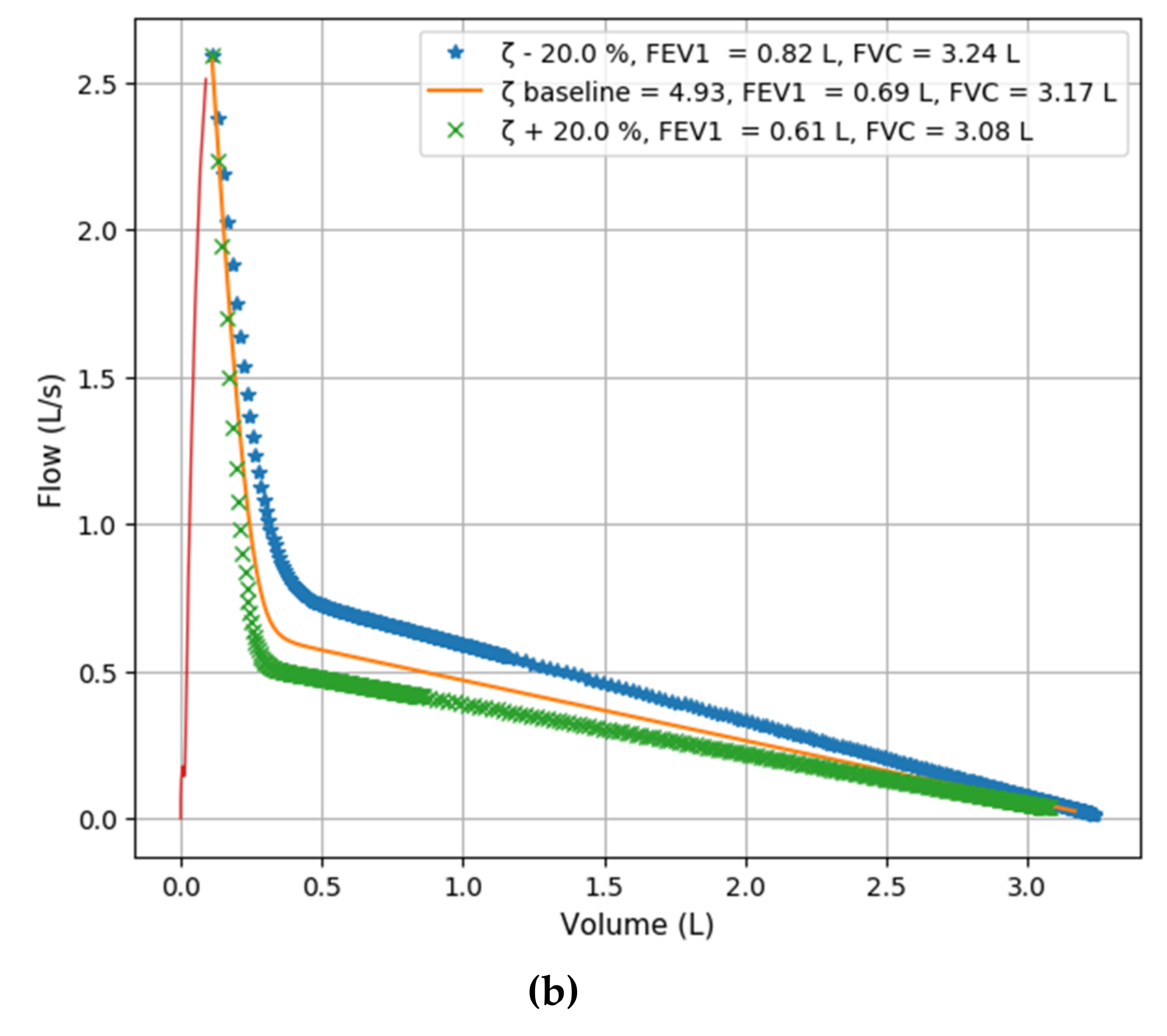
3.3. ζ simulation Studies
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
References
- O’Donnell, D.E.; Laveneziana, P. Physiology and consequences of lung hyperinflation in COPD. Eur. Respir. Rev. 2006, 15, 61–67. [Google Scholar] [CrossRef]
- Bousquet, J.; Jeffery, P.K.; Busse, W.W.; Johnson, M.; Vignola, A.M. Asthma: From bronchoconstriction to airways inflammation and remodeling. Am. J. Respir. Crit. Care Med. 2000, 161, 1720–1745. [Google Scholar] [CrossRef]
- Vestbo, J.; Hurd, S.S.; Agustí, A.G.; Jones, P.W.; Vogelmeier, C.; Anzueto, A.; Barnes, P.J.; Fabbri, L.M.; Martinez, F.J.; Nishimura, M.; et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary (updated 2014). Glob. Initiat. Chronic Obstr. Lung Dis. 2014, 21–26. [Google Scholar] [CrossRef]
- Miller, M.R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Crapo, R.; Enright, P.V.; Van Der Grinten, C.P.M.; Gustafsson, P.; et al. Standardisation of spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef]
- Pellegrino, R.; Viegi, G.; Brusasco, V.; Crapo, R.O.; Burgos, F.; Casaburi, R.; Coates, A.; Van Der Grinten, C.P.M.; Gustafsson, P.; Hankinson, J.; et al. Interpretative strategies for lung function tests. Eur. Respir. J. 2005, 26, 948–968. [Google Scholar] [CrossRef]
- Mead, J. Analysis of the configuration of maximum expiratory flow-volume curves. J. Appl. Physiol. 1978, 44, 156–165. [Google Scholar] [CrossRef]
- Kaminsky, D.A. What Does Airway Resistance Tell Us about Lung Function? Respir. Care 2012, 57, 85–99. [Google Scholar] [CrossRef]
- Petty, T.L.; Silvers, G.W.; Stanford, R.E. Radial Traction and Small Airways Disease in Excised Human Lungs. Am. Rev. Respir. Dis. 2015, 133, 132–135. [Google Scholar]
- Zach, M.S. The physiology of forced expiration. Paediatr. Respir. Rev. 2000, 1, 36–39. [Google Scholar] [CrossRef]
- Larsson, K. Aspects on pathophysiological mechanisms in COPD. J. Intern. Med. 2007, 262, 311–340. [Google Scholar] [CrossRef]
- Criée, C.P.; Sorichter, S.; Smith, H.J.; Kardos, P.; Merget, R.; Heise, D.; Berdel, D.; Köhler, D.; Magnussen, H.; Marek, W.; et al. Body plethysmography—Its principles and clinical use. Respir. Med. 2011, 105, 959–971. [Google Scholar]
- Stocks, J.; Godfrey, S.; Beardsmore, C.; Bar-Yishay, E.; Castile, R. Plethysmographic measurements of lung volume and airway resistance. Eur. Respir. J. 2001, 17, 302–312. [Google Scholar] [CrossRef]
- Oh, A.; Morris, T.A.; Yoshii, I.T.; Morris, T.A. Flow Decay: A Novel Spirometric Index to Quantify Dynamic Airway Resistance. Respir. Care 2017, 62, 928–935. [Google Scholar] [CrossRef]
- Vogelmeier, C.F.; Criner, G.J.; Martinez, F.J.; Anzueto, A.; Barnes, P.J.; Bourbeau, J.; Celli, B.R.; Chen, R.; Decramer, M.; Fabbri, L.M.; et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am. J. Respir. Crit. Care Med. 2017, 195, 557–582. [Google Scholar] [CrossRef]
- Jensen, R.L.; Crapo, R.O. Diffusing capacity: How to get it right. Respir. Care 2003, 48, 777–782. [Google Scholar]
- O’Donnell, D.E.; Webb, K.A.; Neder, J.A. Lung hyperinflation in COPD: Applying physiology to clinical practice. COPD Res. Pract. 2015, 1, 4. [Google Scholar] [CrossRef]
- Lynch, D.A.; Al-Qaisi, M.A. Quantitative computed tomography in chronic obstructive pulmonary disease. J. Thorac. Imaging 2013, 28, 284–290. [Google Scholar] [CrossRef]
- Bencowitz, H.Z. Single breath diffusing capacity in a representative sample of the population of Michigan, a large industrial state. Am. Rev. Respir. Dis. 1983, 127, 270–277. [Google Scholar]
- Krowka, M.J.; Enright, P.L.; Rodarte, J.R.; Hyatt, R.E. Effect of Effort on Measurement of Forced Expiratory Volume in One Second. Am. Rev. Respir. Dis. 1987, 136, 829–833. [Google Scholar] [CrossRef]
- Hayes, D.; Kraman, S.S. The Physiologic Basis of Spirometry. Respir. Care 2009, 54, 1717–1726. [Google Scholar]
- Quanjer, P.H.; Lebowitz, M.D.; Gregg, I.; Miller, M.R.; Pedersen, O.F. Peak expiratory flow: Conclusions and recommendations of a Working Party of the European Respiratory Society. Eur. Respir. J. Suppl. 1997, 10, 2s. [Google Scholar]
- Fry, D.L.; Hyatt, R.E. Pulmonary mechanics. A unified analysis of the relationship between pressure, volume and gasflow in the lungs of normal and diseased human subjects. Am. J. Med. 1960, 29, 672–689. [Google Scholar] [CrossRef]
- Agostoni, E.; Fenn, W.O. Velocity of Muscle Shortening As a Limiting Factor in Respiratory Air Flow. J. Appl. Physiol. 1960, 15, 349–353. [Google Scholar] [CrossRef]
- Rao, S.S. Mechanical Vibrations; Addison-Wesley Longman: University of Michigan, MI, USA, 1990. [Google Scholar]
- Storn, R.; Price, K. Differential Evolution—A Simple and Efficient Heuristic for Global Optimization over Continuous Spaces. J. Glob. Optim. 1997, 11, 341–359. [Google Scholar] [CrossRef]
- Millman, K.J.; Aivazis, M. Python for scientists and engineers. Comput. Sci. Eng. 2011, 13, 9–12. [Google Scholar] [CrossRef]
- RStudio Team. RStudio: Integrated Development for R; RStudio, Inc.: Boston, MA, USA, 2016; Available online: http//www.rstudio.com (accessed on 15 June 2019).
- O’Donnell, R.; Breen, D.; Wilson, S.; Djukanovic, R. Inflammatory cells in the airways in COPD. Thorax 2006, 61, 448–454. [Google Scholar] [CrossRef]
- Yan, F.; Gao, H.; Zhao, H.; Bhatia, M.; Zeng, Y. Roles of airway smooth muscle dysfunction in chronic obstructive pulmonary disease. J. Transl. Med. 2018, 16, 262. [Google Scholar] [CrossRef]
- Ramos, F.L.; Krahnke, J.S.; Kim, V. Clinical issues of mucus accumulation in COPD. Int. J. COPD 2014, 9, 139. [Google Scholar]
- Cottin, V.; Nunes, H.; Brillet, P.Y.; Delaval, P.; Devouassaoux, G.; Tillie-Leblond, I.; Israel-Biet, D.; Valeyre, D.; Cordier, J.F. Combined pulmonary fibrosis and emphysema: A distinct underrecognised entity. Eur. Respir. J. 2005, 26, 586–593. [Google Scholar] [CrossRef]
- Topalovic, M.; Exadaktylos, V.; Decramer, M.; Troosters, T.; Berckmans, D.; Janssens, W. Modelling the dynamics of expiratory airflow to describe chronic obstructive pulmonary disease. Med. Biol. Eng. Comput. 2014, 52, 997–1006. [Google Scholar] [CrossRef]
- Mead, J. Mechanical properties of the lungs. Acta Physiol. Pol. 1961, 41, 281–330. [Google Scholar] [CrossRef]
- Hess, D.R. Respiratory Mechanics in Mechanically Ventilated Patients. Respir. Care 2014, 59, 1773–1794. [Google Scholar] [CrossRef]
- Grinnan, D.C.; Truwit, J.D. Clinical review: Respiratory mechanics in spontaneous and assisted ventilation. Crit. Care 2005, 9, 472. [Google Scholar] [CrossRef]
- Dubois, A.B. Airway Resistance. Am. J. Respir. Crit. Care Med. 2000, 162, 345–346. [Google Scholar] [CrossRef]
- Crossley, D.; Renton, M.; Khan, M.; Low, E.V.; Turner, A.M. CT densitometry in emphysema: A systematic review of its clinical utility. Int. J. COPD 2018, 13, 547. [Google Scholar] [CrossRef]
- Bailey, K.L. The importance of the assessment of pulmonary function in COPD. Med. Clin. N. Am. 2012, 96, 745–752. [Google Scholar] [CrossRef]
- Akoumianaki, E.; Maggiore, S.M.; Valenza, F.; Bellani, G.; Jubran, A.; Loring, S.H.; Pelosi, P.; Talmor, D.; Grasso, S.; Chiumello, D.; et al. The application of esophageal pressure measurement in patients with respiratory failure. Am. J. Respir. Crit. Care Med. 2014, 189, 520–531. [Google Scholar] [CrossRef]
- Macklem, P.T.; Mead, J. Resistance of central and peripheral airways measured by a retrograde catheter. J. Appl. Physiol. 1967, 22, 395–401. [Google Scholar] [CrossRef]
- Kaczka, D.W.; Ingenito, E.P.; Suki, B.; Lutchen, K.R. Partitioning airway and lung tissue resistances in humans: Effects of bronchoconstriction. J. Appl. Physiol. 1997, 82, 1531–1541. [Google Scholar] [CrossRef]
- Brashier, B.; Salvi, S. Measuring lung function using sound waves: Role of the forced oscillation technique and impulse oscillometry system. Breathe 2015, 11, 57–65. [Google Scholar] [CrossRef]

| Healthy | GOLD I | GOLD II | GOLD III | GOLD IV | p | |
|---|---|---|---|---|---|---|
| N | 135 | 63 | 111 | 92 | 61 | |
| Age (years) | 62 (6) | 63 (6) | 68 (8) | 69 (9) | 63 (7) | <0.001 |
| Sex (female %) | 21 | 24 | 23 | 20 | 26 | 0.9 |
| Smoking (pack-years) | 42 (21) | 50 (28) | 49 (23) | 49 (24) | 52 (25) | 0.06 |
| FEV1 (%pred) | 97 (13) | 93 (10) | 65 (9) | 40 (5) | 23 (5) | <0.001 |
| FVC (%pred) | 103 (14) | 115 (15) | 95 (16) | 82 (15) | 62 (14) | <0.001 |
| FEV1/FVC (%) | 74 (4) | 64 (4) | 55 (9) | 39 (8) | 30 (6) | <0.001 |
| Raw (kPa/L/s) | 0.32 (0.10) | 0.35 (0.12) | 0.44 (0.12) | 0.60 (0.16) | 0.82 (0.29) | <0.001 |
| sGaw (1/(kPa s)) | 0.9 (0.2) | 0.75 (0.21) | 0.55 (0.18) | 0.34 (0.11) | 0.22 (0.07) | 0.01 |
| RV/TLC (%) | 37 (6) | 38 (6) | 47 (7) | 57 (8) | 68 (8) | <0.001 |
| DLCO (mmol/min/kPa) | 7.7 (1.8) | 7.1 (2.2) | 5.5 (2.0) | 4.2 (1.4) | 2.9 (1) | <0.001 |
| 15th percentile (HU) | −935 (41) | −938 (34) | −943 (49) | −953 (39) | −968 (44) | <0.001 |
| % below -950 HU | 10 (12) | 11 (11) | 15 (16) | 19 (16) | 26 (17) | <0.001 |
| Healthy | GOLD I | GOLD II | GOLD III | GOLD IV | p | |
|---|---|---|---|---|---|---|
| ζ | 1.64 (0.18) | 1.78 (0.23) | 2.10 (0.36) | 2.83 (0.77) | 3.96 (0.99) | <0.0001 |
| ω (rad/s)0.5 | 1.58 (0.53) | 1.42 (0.61) | 1.43 (0.53) | 1.46 (0.49) | 1.75 (0.53) | <0.01 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Das, N.; Verstraete, K.; Topalovic, M.; Aerts, J.-M.; Janssens, W. Estimating Airway Resistance from Forced Expiration in Spirometry. Appl. Sci. 2019, 9, 2842. https://doi.org/10.3390/app9142842
Das N, Verstraete K, Topalovic M, Aerts J-M, Janssens W. Estimating Airway Resistance from Forced Expiration in Spirometry. Applied Sciences. 2019; 9(14):2842. https://doi.org/10.3390/app9142842
Chicago/Turabian StyleDas, Nilakash, Kenneth Verstraete, Marko Topalovic, Jean-Marie Aerts, and Wim Janssens. 2019. "Estimating Airway Resistance from Forced Expiration in Spirometry" Applied Sciences 9, no. 14: 2842. https://doi.org/10.3390/app9142842
APA StyleDas, N., Verstraete, K., Topalovic, M., Aerts, J.-M., & Janssens, W. (2019). Estimating Airway Resistance from Forced Expiration in Spirometry. Applied Sciences, 9(14), 2842. https://doi.org/10.3390/app9142842






