Impact of Core Exercise Training on Gait and Exercise Capacity in People with Multiple Sclerosis: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction
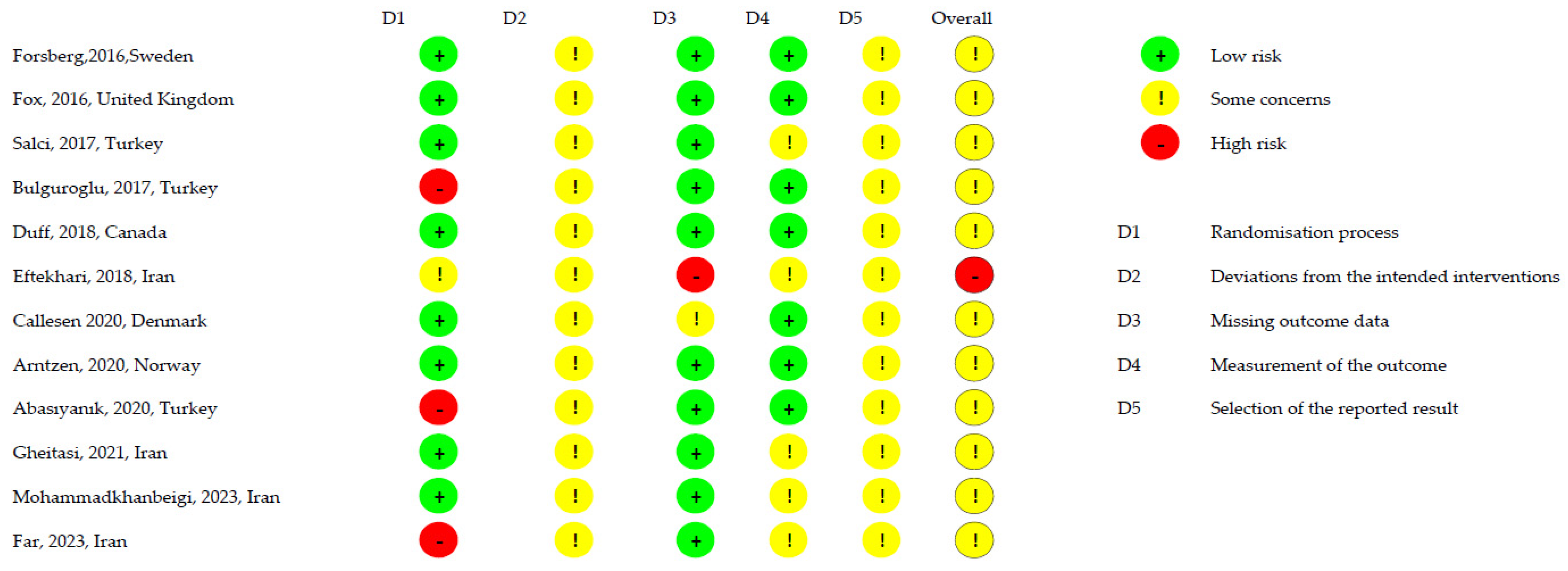
2.5. Methodological Quality of Included Studies
2.6. Risk of Bias of Included Studies
3. Results
3.1. Search Selection
3.2. Characteristics of the Included Studies and Participants
3.3. Characteristics of Interventions
3.4. Methodological Quality and Risk of Bias
4. Discussion
4.1. Multiple Sclerosis and Gait
4.2. Core-Focused Training
4.3. Core Training for Gait and Exercise Capacity
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MS | Multiple Sclerosis |
| TUG | Timed Up and Go |
| MSWS | Multiple Sclerosis Walking Scale |
| 6MWT | 6-Minute Walking Test |
| 10MWT | 10-Meter Walk Test |
| 2MWT | 2-Minute Walk Test |
| T25FWT | Timed 25-Foot Walk Test |
| SSST | Six-Spot Step Test |
| QoL | Quality of Life |
Appendix A
| Database | Cinahl |
|---|---|
| Date | 3 September 2024 |
| Strategy | #1 AND #2 AND #3 AND #4 |
| #1 | AB (“Multiple Sclerosis” [MeSH] OR “multiple sclerosis” OR “disseminated sclerosis”) |
| #2 | AB (“Core Stability” [MeSH] OR “core” OR “trunk” OR “lumbopelvic hip complex” OR “Pelvic Floor” [MeSH] OR “pelvic floor” OR “diaphragm” OR “Abdominal Muscles” [MeSH] OR “abdomin*” OR “low back” OR “multifid*” OR “lumbar” OR “quadratus lumborum” OR “erector spinae” OR “external oblique” OR “internal oblique”) |
| #3 | AB (“Resistance Training” [MeSH] OR “Endurance Training” [MeSH] OR “train*” OR “Exercise” [MeSH] OR “Exercise Therapy” [Mesh] OR “Exercise Movement Techniques” [MeSH] OR “exercis*” OR “Pilates” OR “strength*” OR “stabili*” OR “intervention” OR “Rehabilitation” [MeSH] OR “rehabilitation”) |
| #4 | AB (“gait” OR “exercise capacity” OR “walking” OR “cardiorespiratory outcome” OR “locomotion”) |
| Database | Medline (via Pubmed) |
| Date | 3 September 2024 |
| Strategy | #1 AND #2 AND #3 AND #4 |
| #1 | AB (“Multiple Sclerosis” [MeSH] OR “multiple sclerosis” OR “disseminated sclerosis”) |
| #2 | AB (“Core Stability” [MeSH] OR “core” OR “trunk” OR “lumbopelvic hip complex” OR “Pelvic Floor” [MeSH] OR “pelvic floor” OR “diaphragm” OR “Abdominal Muscles” [MeSH] OR “abdomin*” OR “low back” OR “multifid*” OR “lumbar” OR “quadratus lumborum” OR “erector spinae” OR “external oblique” OR “internal oblique”) |
| #3 | AB (“Resistance Training” [MeSH] OR “Endurance Training” [MeSH] OR “train*” OR “Exercise” [MeSH] OR “Exercise Therapy” [Mesh] OR “Exercise Movement Techniques” [MeSH] OR “exercis*” OR “Pilates” OR “strength*” OR “stabili*” OR “intervention” OR “Rehabilitation” [MeSH] OR “rehabilitation”) |
| #4 | AB (“gait” OR “exercise capacity” OR “walking” OR “cardiorespiratory outcome” OR “locomotion”) |
| Database | Scopus |
| Date | 3 September 2024 |
| Strategy | #1 AND #2 AND #3 AND #4 |
| #1 | AB (“Multiple Sclerosis” [MeSH] OR “multiple sclerosis” OR “disseminated sclerosis”) |
| #2 | AB (“Core Stability” OR “core” OR “trunk” OR “lumbopelvic hip complex” OR “Pelvic Floor” OR “pelvic floor” OR “diaphragm” OR “Abdominal Muscles” OR “abdominal” OR “low back” OR “multifidos” OR “lumbar” OR “quadratus lumborum” OR “erector spinae” OR “external oblique” OR “internal oblique”) |
| #3 | AB “Resistance Training” OR “Endurance Training” OR “training” OR “Exercise” OR “Exercise Therapy” OR “Exercise Movement Techniques” OR “exercise” OR “Pilates” OR “strength” OR “stability” OR “intervention” OR “Rehabilitation” OR “rehabilitation”) |
| #4 | AB (“gait” OR “exercise capacity” OR “walking” OR “cardiorespiratory outcome” OR “locomotion”) |
| Database | Web of Science |
| Date | 3 September 2024 |
| Strategy | #1 AND #2 AND #3 AND #4 |
| #1 | AB (“Multiple Sclerosis” [MeSH] OR “multiple sclerosis” OR “disseminated sclerosis”) |
| #2 | AB (“Core Stability” [MeSH] OR “core” OR “trunk” OR “lumbopelvic hip complex” OR “Pelvic Floor” [MeSH] OR “pelvic floor” OR “diaphragm” OR “Abdominal Muscles” [MeSH] OR “abdomin*” OR “low back” OR “multifid*” OR “lumbar” OR “quadratus lumborum” OR “erector spinae” OR “external oblique” OR “internal oblique”) |
| #3 | AB (“Resistance Training” [MeSH] OR “Endurance Training” [MeSH] OR “train*” OR “Exercise” [MeSH] OR “Exercise Therapy” [Mesh] OR “Exercise Movement Techniques” [MeSH] OR “exercis*” OR “Pilates” OR “strength*” OR “stabili*” OR “intervention” OR “Rehabilitation” [MeSH] OR “rehabilitation”) |
| #4 | AB (“gait” OR “exercise capacity” OR “walking” OR “cardiorespiratory outcome” OR “locomotion”) |
| Database | ScienceDirect |
| Date | 3 September 2024 |
| Strategy | #1 AND #2 AND #3 AND #4 |
| #1 | AB (“Multiple Sclerosis” [mesh]) |
| #2 | AB (“core” OR “trunk”) |
| #3 | AB (“Resistance Training” [mesh] OR “Endurance Training” [mesh] “Exercise” [mesh]) |
| #4 | AB (“gait” OR “exercise capacity” OR “walking) |
| Database | PEDro |
| Date | 3 September 2024 |
| Strategy | #1 AND #2 + #3 AND #4 |
| #1 | (“Multiple Sclerosis”) |
| #2 | (“core”) |
| #3 | (“Multiple Sclerosis”) |
| #4 | (“trunk”) |
References
- Geurts, J.J.; Barkhof, F. Grey matter pathology in multiple sclerosis. Lancet Neurol. 2008, 7, 841–851. [Google Scholar] [CrossRef]
- Cameron, M.H.; Wagner, J.M. Gait abnormalities in multiple sclerosis: Pathogenesis, evaluation, and advances in treatment. Curr. Neurol. Neurosci. Rep. 2011, 11, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Oliva Ramirez, A.; Keenan, A.; Kalau, O.; Worthington, E.; Cohen, L.; Singh, S. Prevalence and burden of multiple sclerosis-related fatigue: A systematic literature review. BMC Neurol. 2021, 21, 468. [Google Scholar] [CrossRef]
- Torres-Costoso, A.; Martínez-Vizcaíno, V.; Reina-Gutiérrez, S.; Álvarez-Bueno, C.; Guzmán-Pavón, M.J.; Pozuelo-Carrascosa, D.P.; Fernández-Rodríguez, R.; Sanchez-López, M.; Cavero-Redondo, I. Effect of Exercise on Fatigue in Multiple Sclerosis: A Network Meta-Analysis Comparing Different Types of Exercise. Arch. Phys. Med. Rehabil. 2022, 103, 970–987. [Google Scholar] [CrossRef] [PubMed]
- Hao, Z.; Zhang, X.; Chen, P. Effects of Different Exercise Therapies on Balance Function and Functional Walking Ability in Multiple Sclerosis Disease Patients-A Network Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2022, 19, 7175. [Google Scholar] [CrossRef]
- Manocchio, N.; Argento, O.; Bossa, M.; Spanò, B.; Pellicciari, L.; Foti, C.; Nocentini, U. The Role of the Cerebellum in Multiple Sclerosis-Related Fatigue and Disability. J. Clin. Med. 2025, 14, 2840. [Google Scholar] [CrossRef]
- Wingerchuk, D.M.; Lucchinetti, C.F.; Noseworthy, J.H. Multiple sclerosis: Current pathophysiological concepts. Lab. Investig. 2001, 81, 263–281. [Google Scholar] [CrossRef] [PubMed]
- Comber, L.; Galvin, R.; Coote, S. Gait deficits in people with multiple sclerosis: A systematic review and meta-analysis. Gait Posture 2017, 51, 25–35. [Google Scholar] [CrossRef]
- Menascu, S.; Vinogradsky, A.; Baransi, H.; Kalron, A. Range of motion abnormalities in the lower limb joints during gait in youth with multiple sclerosis. Mult. Scler. Relat. Disord. 2024, 82, 105417. [Google Scholar] [CrossRef]
- Goldstein, R.E. Chapter 8. Exercise capacity. In Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed.; Walker, H.K., Hall, W.D., Hurst, J.W., Eds.; Butterworths: Boston, MA, USA, 1990. [Google Scholar]
- Savci, S.; Inal-Ince, D.; Arikan, H.; Guclu-Gunduz, A.; Cetisli-Korkmaz, N.; Armutlu, K.; Karabudak, R. Six-minute walk distance as a measure of functional exercise capacity in multiple sclerosis. Disabil. Rehabil. 2005, 27, 1365–1371. [Google Scholar] [CrossRef]
- Romberg, A.; Virtanen, A.; Aunola, S.; Karppi, S.L.; Karanko, H.; Ruutiainen, J. Exercise capacity, disability and leisure physical activity of subjects with multiple sclerosis. Mult. Scler. 2004, 10, 212–218. [Google Scholar] [CrossRef]
- Cameron, M.H.; Nilsagard, Y. Balance, gait, and falls in multiple sclerosis. Handb. Clin. Neurol. 2018, 159, 237–250. [Google Scholar] [PubMed]
- Yoosefinejad, A.K.; Motealleh, A.; Khademi, S.; Hosseini, S.F. Lower Endurance and Strength of Core Muscles in Patients with Multiple Sclerosis. Int. J. MS Care 2017, 19, 100–104. [Google Scholar] [CrossRef]
- Choobsaz, H.; Sangtarash, F.; Javaherian, M.; Hadizadeh, M. Investigating the effects of core stability training on balance and gait in people with multiple sclerosis: A systematic review and meta-analysis. Mult. Scler. Relat. Disord. 2024, 87, 105686. [Google Scholar] [CrossRef]
- Ketelhut, N.B.; Kindred, J.H.; Manago, M.M.; Hebert, J.R.; Rudroff, T. Core muscle characteristics during walking of patients with multiple sclerosis. J. Rehabil. Res. Dev. 2015, 52, 713–724. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Salcı, Y.; Fil, A.; Armutlu, K.; Yildiz, F.G.; Kurne, A.; Aksoy, S.; Nurlu, G.; Karabudak, R. Effects of different exercise modalities on ataxia in multiple sclerosis patients: A randomized controlled study. Disabil. Rehabil. 2017, 39, 2626–2632. [Google Scholar] [CrossRef]
- Bulguroglu, I.; Guclu-Gunduz, A.; Yazici, G.; Ozkul, C.; Irkec, C.; Nazliel, B.; Batur-Caglayan, H.Z. The effects of Mat Pilates and Reformer Pilates in patients with Multiple Sclerosis: A randomized controlled study. NeuroRehabilitation 2017, 41, 413–422. [Google Scholar] [CrossRef]
- Abasıyanık, Z.; Ertekin, Ö.; Kahraman, T.; Yigit, P.; Özakbaş, S. The effects of Clinical Pilates training on walking, balance, fall risk, respiratory, and cognitive functions in persons with multiple sclerosis: A randomized controlled trial. Explore 2020, 16, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Eftekhari, E.; Etemadifar, M. Impact of Clinical Mat Pilates on Body Composition and Functional Indices in Female Patients With Multiple Sclerosis. Crescent J. Med. Biol. Sci. 2018, 5, 297–305. [Google Scholar]
- Gheitasi, M.; Bayattork, M.; Andersen, L.L.; Imani, S.; Daneshfar, A. Effect of twelve weeks pilates training on functional balance of male patients with multiple sclerosis: Randomized controlled trial. J. Bodyw. Mov. Ther. 2021, 25, 41–45. [Google Scholar] [CrossRef]
- Mohammadkhanbeigi, S.; Tabrizi, Y.; Nabavi, S.; Minoonejad, H. The Comparable Effect of tDCS and Core Exercises on Balance and Mobility in Patients With Multiple Sclerosis. Iran. Rehabil. J. 2023, 20, 569–578. [Google Scholar] [CrossRef]
- Far, S.S.; Amiri, B.; Sahebozamani, M.; Ebrahimi, H.A.; Zemková, E. The effect of multi-function swing suspension training on upper and lower extremities function and quality of life in multiple sclerosis women with different disability status. Mult. Scler. Relat. Disord. 2023, 80, 105113. [Google Scholar] [CrossRef]
- Forsberg, A.; von Koch, L.; Nilsagård, Y. Effects on Balance and Walking with the CoDuSe Balance Exercise Program in People with Multiple Sclerosis: A Multicenter Randomized Controlled Trial. Mult. Scler. Int. 2016, 2016, 7076265. [Google Scholar] [CrossRef]
- Callesen, J.; Cattaneo, D.; Brincks, J.; Kjeldgaard Jørgensen, M.L.; Dalgas, U. How do resistance training and balance and motor control training affect gait performance and fatigue impact in people with multiple sclerosis? A randomized controlled multi-center study. Mult. Scler. 2020, 26, 1420–1432. [Google Scholar] [CrossRef] [PubMed]
- Arntzen, E.C.; Straume, B.; Odeh, F.; Feys, P.; Normann, B. Group-based, individualized, comprehensive core stability and balance intervention provides immediate and long-term improvements in walking in individuals with multiple sclerosis: A randomized controlled trial. Physiother. Res. Int. 2020, 25, e1798. [Google Scholar] [CrossRef]
- Duff, W.R.D.; Andrushko, J.W.; Renshaw, D.W.; Chilibeck, P.D.; Farthing, J.P.; Danielson, J.; Evans, C.D. Impact of Pilates Exercise in Multiple Sclerosis: A Randomized Controlled Trial. Int. J. MS Care 2018, 20, 92–100. [Google Scholar] [CrossRef]
- Fox, E.E.; Hough, A.D.; Creanor, S.; Gear, M.; Freeman, J.A. Effects of Pilates-Based Core Stability Training in Ambulant People With Multiple Sclerosis: Multicenter, Assessor-Blinded, Randomized Controlled Trial. Phys. Ther. 2016, 96, 1170–1178. [Google Scholar] [CrossRef]
- Abasıyanık, Z.; Kahraman, T.; Veldkamp, R.; Ertekin, Ö.; Kalron, A.; Feys, P. Changes in Gait Characteristics During and Immediately After the 6-Minute Walk Test in Persons With Multiple Sclerosis: A Systematic Review. Phys. Ther. 2022, 102, pzac036. [Google Scholar] [CrossRef] [PubMed]
- González del Rio, M.; Merchan Ruiz, M. Escala de Movilidad de 12 ítems para esclerosis múltiple: Análisis Mediante Diagnósticos de Enfermería. Rev. Científica Soc. Española Enfermería Neurológica 2020, 51, 23–26. [Google Scholar] [CrossRef]
- Hoffman, J.; Gabel, P. Expanding Panjabi’s stability model to express movement: A theoretical model. Med. Hypotheses 2013, 80, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Farid, R.; Norasteh, A.A.; Hatamian, H. The Effect of Core Stability Exercise Program on the Balance of Patients with Multiple Sclerosis. Casp. J. Neurol. Sci. 2016, 2, 9–17. [Google Scholar] [CrossRef]
- Van Criekinge, T.; Truijen, S.; Schröder, J.; Maebe, Z.; Blanckaert, K.; van der Waal, C.; Vink, M.; Saeys, W. The effectiveness of trunk training on trunk control, sitting and standing balance and mobility post-stroke: A systematic review and meta-analysis. Clin. Rehabil. 2019, 33, 992–1002. [Google Scholar] [CrossRef] [PubMed]
- Haruyama, K.; Kawakami, M.; Otsuka, T. Effect of Core Stability Training on Trunk Function, Standing Balance, and Mobility in Stroke Patients. Neurorehabilit. Neural Repair 2017, 31, 240–249. [Google Scholar] [CrossRef]
- Al-Nemr, A.; Kora, A.N. Effect of core stabilization versus rebound therapy on balance in children with cerebral palsy. Acta Neurol. Belg. 2024, 124, 843–851. [Google Scholar] [CrossRef]
- Akuthota, V.; Ferreiro, A.; Moore, T.; Fredericson, M. Core stability exercise principles. Curr. Sports Med. Rep. 2008, 7, 39–44. [Google Scholar] [CrossRef]
- Tramontano, M.; Argento, O.; Manocchio, N.; Piacentini, C.; Orejel Bustos, A.S.; De Angelis, S.; Bossa, M.; Nocentini, U. Dynamic Cognitive-Motor Training versus Cognitive Computer-Based Training in People with Multiple Sclerosis: A Preliminary Randomized Controlled Trial with 2-Month Follow-Up. J. Clin. Med. 2024, 13, 2664. [Google Scholar] [CrossRef]
- Bennett, S.E.; Bromley, L.E.; Fisher, N.M.; Tomita, M.R.; Niewczyk, P. Validity and Reliability of Four Clinical Gait Measures in Patients with Multiple Sclerosis. Int. J. MS Care 2017, 19, 247–252. [Google Scholar] [CrossRef]
- Valet, M.; Lejeune, T.; Devis, M.; van Pesch, V.; El Sankari, S.; Stoquart, G. Timed Up-and-Go and 2-Minute Walk Test in patients with multiple sclerosis with mild disability: Reliability, responsiveness and link with perceived fatigue. Eur. J. Phys. Rehabil. Med. 2019, 55, 450–455. [Google Scholar] [CrossRef]
- Chorschew, A.; Kesgin, F.; Bellmann-Strobl, J.; Flachenecker, P.; Schiffmann, I.; Rosenthal, F.; Althoff, P.; Drebinger, D.; Arsenova, R.; Rasche, L.; et al. Translation and validation of the multiple sclerosis walking scale 12 for the German population—The MSWS-12/D. Health Qual. Life Outcomes 2023, 21, 110. [Google Scholar] [CrossRef]
- Feys, P.; Bibby, B.; Romberg, A.; Santoyo, C.; Gebara, B.; de Noordhout, B.M.; Knuts, K.; Bethoux, F.; Skjerbæk, A.; Jensen, E.; et al. Within-day variability on short and long walking tests in persons with multiple sclerosis. J. Neurol. Sci. 2014, 338, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Lam, H.S.P.; Lau, F.W.K.; Chan, G.K.L.; Sykes, K. The validity and reliability of a 6-Metre Timed Walk for the functional assessment of patients with stroke. Physiother. Theory Pract. 2010, 26, 251–255. [Google Scholar] [CrossRef]
- Arvidsson Lindvall, M.; Anderzén-Carlsson, A.; Appelros, P.; Forsberg, A. Validity and test-retest reliability of the six-spot step test in persons after stroke. Physiother. Theory Pract. 2020, 36, 211–218. [Google Scholar] [CrossRef]
- Liu, T.W.; Ng, S.S.; Cheung, K.Y.; Cheung, M.Y.; Hung, R.N.; Lam, M.F.; Wong, A.T.; Lai, C.Y.; Tse, M.M. Reliability and validity of Six-Spot Step Test (SSST) in stroke survivors. Eur. J. Phys. Rehabil. Med. 2021, 57, 879–888. [Google Scholar] [CrossRef] [PubMed]
- Sandroff, B.M.; Motl, R.W.; Sosnoff, J.J.; Pula, J.H. Further validation of the Six-Spot Step Test as a measure of ambulation in multiple sclerosis. Gait Posture 2015, 41, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Pommerich, U.M.; Brincks, J.; Skjerbæk, A.G.; Dalgas, U. The subjective minimal important change for the Six Spot Step Test in people with multiple sclerosis—The Danish MS Hospitals Rehabilitation study. Acta Neurol. Belg. 2022, 122, 893–901. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Crouch, R. Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: A systematic review. J. Eval. Clin. Pract. 2017, 23, 377–381. [Google Scholar] [CrossRef]
- Bowman, T.; Mestanza Mattos, F.G.; Allera Longo, C.; Bocini, S.; Gennuso, M.; Marazzini, F.; Giuseppe Materazzi, F.; Pelosin, E.; Putzolu, M.; Salvalaggio, S.; et al. The minimally clinically important difference in the 2-minute walk test for people in the subacute phase after a stroke. Top. Stroke Rehabil. 2024, 11, 1–9. [Google Scholar] [CrossRef]
- Coleman, C.I.; Sobieraj, D.M.; Marinucci, L.N. Minimally important clinical difference of the Timed 25-Foot Walk Test: Results from a randomized controlled trial in patients with multiple sclerosis. Curr. Med. Res. Opin. 2012, 28, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Hosoi, Y.; Kamimoto, T.; Sakai, K.; Yamada, M.; Kawakami, M. Estimation of minimal detectable change in the 10-meter walking test for patients with stroke: A study stratified by gait speed. Front. Neurol. 2023, 14, 1219505. [Google Scholar] [CrossRef] [PubMed]
- Gautschi, O.P.; Stienen, M.N.; Corniola, M.V.; Joswig, H.; Schaller, K.; Hildebrandt, G.; Smoll, N.R. Assessment of the Minimum Clinically Important Difference in the Timed Up and Go Test After Surgery for Lumbar Degenerative Disc Disease. Neurosurgery 2017, 80, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Mehta, L.; McNeill, M.; Hobart, J.; Wyrwich, K.W.; Poon, J.L.; Auguste, P.; Zhong, J.; Elkins, J. Identifying an important change estimate for the Multiple Sclerosis Walking Scale-12 (MSWS-12v1) for interpreting clinical trial results. Mult. Scler. J. Exp. Transl. Clin. 2015, 1, 2055217315596993. [Google Scholar] [CrossRef]
- Du, L.; Xi, H.; Zhang, S.; Zhou, Y.; Tao, X.; Lv, Y.; Hou, X.; Yu, L. Effects of exercise in people with multiple sclerosis: A systematic review and meta-analysis. Front. Public Health 2024, 12, 1387658. [Google Scholar] [CrossRef]
- Reynolds, E.R.; Ashbaugh, A.D.; Hockenberry, B.J.; McGrew, C.A. Multiple Sclerosis and Exercise: A Literature Review. Curr. Sports Med. Rep. 2018, 17, 31–35. [Google Scholar] [CrossRef]
- Heine, M.; van de Port, I.; Rietberg, M.B.; van Wegen, E.E.; Kwakkel, G. Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst. Rev. 2015, 11, CD009956. [Google Scholar] [CrossRef]
- Paltamaa, J.; Sjögren, T.; Peurala, S.H.; Heinonen, A. Effects of physiotherapy interventions on balance in multiple sclerosis: A systematic review and meta-analysis of randomized controlled trials. J. Rehabil. Med. 2012, 44, 811–823. [Google Scholar] [CrossRef]
- Kjølhede, T.; Vissing, K.; Dalgas, U. Multiple sclerosis and progressive resistance training: A systematic review. Mult. Scler. 2012, 18, 1215–1228. [Google Scholar] [CrossRef]
- Halabchi, F.; Alizadeh, Z.; Sahraian, M.A.; Abolhasani, M. Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC Neurol. 2017, 17, 185. [Google Scholar] [CrossRef]
- Kerling, A.; Keweloh, K.; Tegtbur, U.; Kück, M.; Grams, L.; Horstmann, H.; Windhagen, A. Effects of a Short Physical Exercise Intervention on Patients with Multiple Sclerosis (MS). Int. J. Mol. Sci. 2015, 16, 15761–15775. [Google Scholar] [CrossRef] [PubMed]

| First Author, Year, Country | Number of Groups | Number of Participants Total (EG/CG) | Number of Participants Analyzed Total (Post-Intervention) (EG/CG) | Mean Age (SD) (Years) Total (EG/CG) | Sex (% Female) Total (EG/CG) | Inclusion Criteria | Exclusion Criteria | Type of Multiple Sclerosis n (%) | Mean Time (SD) Since Onset (Years) of Multiple Sclerosis (EG/CG) |
|---|---|---|---|---|---|---|---|---|---|
| Forsberg, 2016, Sweden [27] | 2: EG, CG | 73 EG = 35 CG = 38 | 73 EG = 35 CG = 38 | Total = NS EG = 52(10) CG = 56.6(11) | Total = NS EG = 80 CG = 82 | MS diagnosis, ability to walk 100 m independently, ability to rise from the ground with minimal assistance, balance impairment (inability to perform heel-to-toe walking for 30 s) | No MS, or cognitive difficulties that prevented taking the tests | RR = 33 (45) SP = 31 (43) PP = 9 (12) | Total = NS EG = 15 (9) CG = 16 (11) |
| Fox, 2016, United Kingdom [31] | 3: G1, G2, CG | 100 G1 = 33 G2 = 35 CG = 32 | 84 G1 = 29 G2 = 30 CG = 25 | Total = 54.13(10,14) G1 = 53.97 (9.19) G2 = 54.60 (11.54) CG = 53.78 (9.72) | Total = 74 G1 = 84.9 G2 = 71.4 CG = 65.6 | MS diagnosis, >18 years old, 4–6.5 EDSS | Contraindications for Pilates, relapse in the last 3 months | RR = 38 (38) SP = 30 (30) PP = 31 (31) Benign = 1 (1) | Total = 13.11(10.50) G1 = 13.18 (10.06) G2 = 13.91(10.97) CG = 12.14(10.68) |
| Salci, 2017, Turkey [20] | 3: G1, G2, G3 | 48 G1 = 16 G2 = 16 G3 = 16 | 42 G1 = 14 G2 = 14 G3 = 14 | Total = NS G1 = 37.29(9.75) G2 = 35.36(8.14) G3 = 34.36(7.90) | Total: NS G1 = 43 G2 = 64 G3 = 71 | >18 years old, 3–5 EDSS, no relapses in the last 3 months, no corticosteroids in the last 3 months | Participation in a physiotherapy program within 6 months, existence of orthopedic and systemic problems, using walking aids and orthoses | RR = 34 (81) PP = 2 (5) SP= 6 (14) | Total = NS G1 = 8.54 (8.44) G2 = 6.18 (4.08) G3 = 5.82 (4.5) |
| Bulguroglu, 2017, Turkey [21] | 3: G1, G2, CG | 59 G1: NS G2: NS CG: NS | 38 G1: 12 G2: 13 CG: 13 | NS G1: 45 (39.3, 49.5) G2: 37 (29.5, 40) CG: 40 (26, 43) | NS | >18 years old, no relapses or surgery in 6 months, less than 4.5 EDSS | BMI of 30 or higher; no perceptual issues that may affect the results | NS | Total: NS G1: NS G2: NS CG: NS |
| Duff, 2018, Canada [30] | 2: EG, CG | 30 GE = 15 CG = 15 | 30 GE = 15 CG = 15 | Total = NE GE = 45.7 (9.4) CG = 45.1 (7.4) | Total = NE GE = 80 CG = 73 | MS diagnosis, being able to move to the evaluation site, and not being in a wheelchair | Exercise contraindications, no MS | RR = 25 (83) SP = 2 (7) PP = 3 (10) | NS |
| Eftekhari, 2018, Iran [23] | 2: EG, CG | 30 EG: NS CG: NS | EG: 13 CG: 12 | 33 (8.08) EG: 34.46 (7.29) CG: 31.41 (8.89) | 100% | Women, EDDS 2–6 | Performed exercises in the last 3 months, back problems, pregnancy, epilepsy, or cancer | RR = 25 | NS |
| Callesen 2020, Denmark [28] | 3: G1, G2, CG | 71 G1: 23 G2: 28 CG: 20 | 53 G1: 17 G2: 24 CG: 12 | 52 (30.75) G1: 52 (38.64) G2: 51 (31.75) CG: 56 (30.73) | 77 G1: 70 G2: 82 CG: 80 | >18 years old, EDSS 2–6.5, SSST >8s or T25FW >5s, no crisis in the last 8 weeks | Unable to undergo the treatment | RR: 70 SP: 17 PP: 13 | Total = 12 (1.40) G1: 15 (2.40) G2: 10 (2.33) CG: 11(1.32) |
| Arntzen, 2020, Norway [29] | 2: EG, CG | 80 EG: 40 CG: 40 | 79 EG: 39 CG: 40 | 34.09(10.52) EG: 36.36(12.13) CG: 31.81(8.61) | GE: 69.29 CG: 72.5 | Diagnosis of MS, residing in the selected municipalities, >18 years old, able to provide written consent, EDSS 1–6.5 | Pregnancy, exacerbation 2 weeks prior to recruitment, other acute issues affecting balance | RR: 68 PP: 7 SP: 4 | EG: 10.04 (7.85) CG: 10.68 (7.27) |
| Abasıyanık, 2020, Turkey [22] | 2: EG, CG | 42 EG = 21 CG = 21 | 33 EG = 16 CG = 17 | Total: 45.45 (9.98) EG = 42.50 (6.76) CG = 48.24 (11.79) | Total: 69.7 EG = 75 CG = 65.7 | Diagnosis of MS, >18 years old, able to walk 100 m independently, desire to participate | No MS diagnosis, under 18 years old, cardiac or orthopedic conditions that interfere with the results | RR: 28 (84.8) SP = 5 (15) | Total = 11.84 (6.88) EG = 12.59 (6.23) CG = 9.83 (8.7) |
| Gheitasi, 2021, Iran [24] | 2: EG, CG | 30 EG: 15 CG: 15 | 30 EG: 15 CG: 15 | 31.35 (5.7) EG: 30.6 (5.27) CG: 32.10 (6.3) | 0% | 25–40 years old, no history of heart disease, epilepsy, metabolic or orthopedic problems; no crisis in the past 2 months | Unable to undergo the intervention, no neurological symptoms in the previous 3 weeks | NS | EG: 5.5 (1.5) CG: 4 (1) |
| Mohammadkhanbeigi, 2023, Iran [25] | 3: G1, G2, CG | 29 G1: 10 G2: 9 CG: 10 | 29 G1: 10 G2: 9 CG: 10 | NS G1: 40.2 (2.43) G2: 37.44 (7.89) CG: 37.70 (7.78) | NS | MS diagnosis according to McDonald criterio; stable symptoms in the last month | Head trauma, new neurological episode in the last month, drug or alcohol use | NS | NS G1: 4.35 (1.12) G2: 3.33 (1.75) CG: 3.85 (1.08) |
| Far, 2023, Iran [26] | 3: G1, G2, CG | 47 G1: 16 G2: 18 CG: 13 | 47 G1: 16 G2: 18 CG: 13 | NS G1: 36.87(6.31) G2: 35.55 (3.74) CG: 37.34 (4.82) | NS | Diagnosis of relapsing-remitting MS, EDDS score of 2–6.5, able to walk | Relapse 2 months before or during study, orthopedic or rheumatic disorders in the last 6 months, musculoskeletal injury within + weeks, pregnancy or changes to medication | RR: 100 | NS |
| First Author, Year, Country | EG Intervention | Other Interventions/CG | Session Duration/Frequency (Times Per Week) | Intervention Duration | Outcomes | Time Point of Assessment | Main Results |
|---|---|---|---|---|---|---|---|
| Forsberg, 2016, Sweden [27] | Core stability exercises | Recommended to maintain usual physical activity level | 60 min/2 sessions per week | 7 weeks | TUG, MSWS | Baseline, post-intervention | EG: significant decrease (p = 0.0026) in MSWS (−3.4 ± 5) compared to CG (0.1 ± 5.2); no significant differences for TUG test |
| Fox, 2016, United Kingdom [31] | Pilates sessions maintaining transverse activation | G2 = standard exercise: mobility and strength exercises in supine, standing, quadruped, and prone positions CG = relaxation | 1 session per week + 15 min of daily home exercises | 12 weeks | MSWS, 10MWT | Baseline, post-intervention, 16 weeks after the start | No significant differences |
| Salci, 2017, Tur-key [20] | Balance exercises maintaining transverse activation. Lumbar stabilization exercises with transverse activation. | G2: balance exercises. Sensory and motor facilitation strategies. G3: transfers and tasks (sit-to-stand from different chair heights, reaching objects from the maximum possible range, walking around obstacles) | 45 min balance + 45 min lumbar stabilization/3 sessions | 6 weeks | 2MWT | Baseline, post-intervention | EG: significant increase (p < 0.02) in 2MWT (25.55 ± 16.90 m) compared to CG (10.75 ± 9.97 m); no significant differences for other outcomes |
| Bulguroglu, 2017, Turkey [21] | Pilates sessions maintaining transverse muscle activation | G1: mat Pilates G2: reformer Pilates CG: relaxation and breathing exercises. | 60–90 min/2 sessions | 8 weeks | TUG | Baseline, post-intervention | EG: significant within-group decrease in G1 (p = 0.06) and G2 (p = 0.011) in TUG (−0.8 s G1 and −1s G2) compared to CG (−0.3 s) |
| Duff, 2018, Canada [30] | Pilates sessions maintaining transverse muscle activation | Manual therapy (massage) | 50 min/2 sessions | 12 weeks | 6MWT, TUG | Baseline, post-intervention | EG: significant increase (p = 0.03) in TUG (−1.5 ± 1.1 s) compared to CG (+0.3 ± 1.1 s). EG: significant increase (p = 0.01) in 6MWT (52.4 ± 19.7 m) compared to CG (15 ± 19.7 m) |
| Eftekhari, 2018, Iran [23] | Pilates sessions based on core stability | CG: normal activity | 60 min/3 sessions | 8 weeks | 10MWT, 6MWT | Baseline, post-intervention | EG: significant increase (p = 0.00) in 10MWT (+0.38 m/s) compared to CG (−0.18 m/s); EG: significant increase (p = 0.004) in 6MWT (+3.5 m) compared to CG (−1.21 m) |
| Callesen 2020, Denmark [28] | Motor control and proprioception exercises | G2: progressive resistance exercises; CG: usual care | 1 h/2 sessions | 10 weeks | T25FW, SSST, MSWS, 6MWT | Baseline, post-intervention | EG: significant increase (p = 0.04) in T25FW (0.14 m/s) compared to CG (0.04 m/s); significant decrease (p < 0.01) in SSST (−2.6 s) compared to CG (−0.4 s); significant decrease (p = 0.01) in MSWS (−9.3) compared to CG (−1.3) |
| Arntzen, 2020, Norway [29] | Exercise protocol, all based on core activation; progressive difficulty | CG: usual care | 60 min/3 sessions | 6 weeks | 2MWT, 10MWT MSWS | Baseline, 7 weeks, 18 weeks, 30 weeks | EG: significant increase (p < 0.001) in 2MWT (186 m) compared to CG (169 m); significant decrease (p = 0.01) in 10MWT-fast speed (−0.83 s) compared to CG (+0.09 s); significant decrease (p = 0.04) in MSWS (−5.5) compared to CG (+1.1) |
| Abasıyanık, 2020, Turkey [22] | Pilates sessions with transverse contraction; resistance exercises: squats, sit-to-stand, bridge, curl-up; balance exercises: tiptoeing, heel-to-toe, single-leg balance, feet together | CG: home exercises not focused on core contraction | 55–60 min/3 sessions | 8 weeks | 6MWT, T25FW, MSWS | Baseline, post-intervention | EG: significant increase (p = 0.001) in 6MWT (75.06 ± 46.17 m) compared to CG (26.35 ± 28.17 m); no significant differences for other outcomes |
| Gheitasi, 2021, Iran [24] | Pilates sessions with core stability exercises | CG: usual care | 60 min/3 sessions | 12 weeks | TUG | Baseline, post-intervention | EG: significant decrease (p = 0.003) in TUG (−1.9 s) compared to CG (+0.3 s) |
| Mohammad-khanbeigi, 2023, Iran [25] | Exercise protocol with 2–3 difficulty levels | G2: transcranial direct current stimulation PG: placebo | 30 min/3 sessions + 15 min daily at home | 6 weeks | TUG, 6MWT | Baseline, post-intervention | EG: within-group significant improvement in TUG (0.04) and 6MWT (p < 0.001); significant differences (p = 0.01) in 6MWT in comparison to PG |
| Far, 2023, Iran [26] | Swing suspension exercise protocol with core stabilization exercises with 4 levels of difficulty for every exercise | CG: relaxation exercises G2: same protocol as G1 | 55–60 min/3 sessions | 8 weeks | T25FW | Baseline, 4 weeks, 6 weeks, 8 weeks | G1 and G2: significant within-group differences (p < 0.001) in T25FW between baseline and post-intervention; significant change between the time and groups, (p = 0.001, F = 13.81) |
| First Author, Year, Country | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Final Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Forsberg, 2016, Sweden [27] | ✓ | ✓ | ✓ | ✓ | ✓ | X | X | ✓ | ✓ | ✓ | ✓ | 9/11 |
| Fox, 2016, United Kingdom [31] | ✓ | ✓ | ✓ | ✓ | X | X | ✓ | ✓ | ✓ | ✓ | ✓ | 9/11 |
| Salci, 2017, Turkey [20] | ✓ | ✓ | ✓ | ✓ | X | X | X | ✓ | ✓ | ✓ | ✓ | 8/11 |
| Bulguroglu, 2017, Turkey [21] | ✓ | ✓ | X | X | X | X | ✓ | ✓ | ✓ | ✓ | ✓ | 7/11 |
| Duff, 2018, Canada [30] | ✓ | ✓ | ✓ | ✓ | X | X | ✓ | ✓ | ✓ | ✓ | ✓ | 9/11 |
| Eftekhari, 2018, Iran [23] | ✓ | ✓ | ✓ | ✓ | X | X | X | X | ✓ | ✓ | ✓ | 7/11 |
| Callesen 2020, Denmark [28] | ✓ | ✓ | ✓ | ✓ | ✓ | X | X | X | ✓ | ✓ | ✓ | 8/11 |
| Arntzen, 2020, Norway [29] | ✓ | ✓ | ✓ | ✓ | X | X | ✓ | ✓ | ✓ | ✓ | ✓ | 9/11 |
| Abasıyanık, 2020, Turkey [22] | ✓ | ✓ | X | ✓ | X | X | ✓ | ✓ | ✓ | ✓ | ✓ | 8/11 |
| Gheitasi, 2021, Iran [24] | ✓ | ✓ | ✓ | ✓ | X | X | X | ✓ | ✓ | ✓ | ✓ | 8/11 |
| Mohammad-khanbeigi, 2023, Iran [25] | ✓ | ✓ | ✓ | ✓ | X | X | X | ✓ | ✓ | ✓ | ✓ | 8/11 |
| Far, 2023, Iran [26] | ✓ | ✓ | X | ✓ | X | X | ✓ | ✓ | ✓ | ✓ | ✓ | 8/11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Martínez, J.D.; Regalado-Cabello, P.; Rodríguez-Montes, M.; Cabrera-Martos, I.; Martín-Nuñez, J.; Valenza, M.C. Impact of Core Exercise Training on Gait and Exercise Capacity in People with Multiple Sclerosis: A Systematic Review. Appl. Sci. 2025, 15, 5054. https://doi.org/10.3390/app15095054
Rodríguez-Martínez JD, Regalado-Cabello P, Rodríguez-Montes M, Cabrera-Martos I, Martín-Nuñez J, Valenza MC. Impact of Core Exercise Training on Gait and Exercise Capacity in People with Multiple Sclerosis: A Systematic Review. Applied Sciences. 2025; 15(9):5054. https://doi.org/10.3390/app15095054
Chicago/Turabian StyleRodríguez-Martínez, Juan Domingo, Paula Regalado-Cabello, María Rodríguez-Montes, Irene Cabrera-Martos, Javier Martín-Nuñez, and Marie Carmen Valenza. 2025. "Impact of Core Exercise Training on Gait and Exercise Capacity in People with Multiple Sclerosis: A Systematic Review" Applied Sciences 15, no. 9: 5054. https://doi.org/10.3390/app15095054
APA StyleRodríguez-Martínez, J. D., Regalado-Cabello, P., Rodríguez-Montes, M., Cabrera-Martos, I., Martín-Nuñez, J., & Valenza, M. C. (2025). Impact of Core Exercise Training on Gait and Exercise Capacity in People with Multiple Sclerosis: A Systematic Review. Applied Sciences, 15(9), 5054. https://doi.org/10.3390/app15095054