In Vitro Wear Properties of a New CAD/CAM Dental Resin Composite in a Chewing Simulation Test Opposing Itself
Abstract
:1. Introduction
2. Materials and Methods
2.1. Samples Fabrication
2.2. Antagonist Abraders Fabrication
2.3. Polishing Procedures
2.4. Wear Testing
2.5. Data Analysis
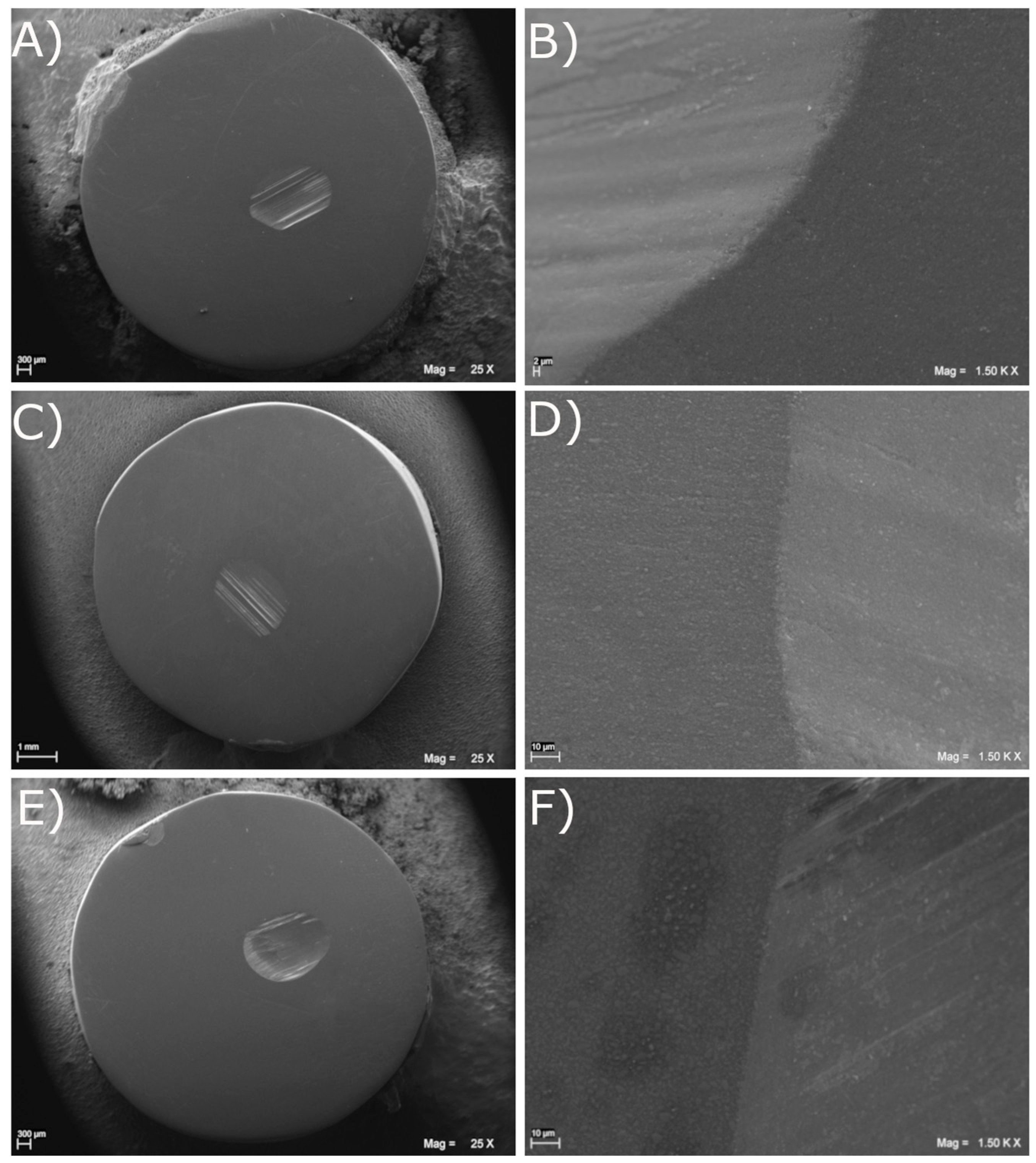
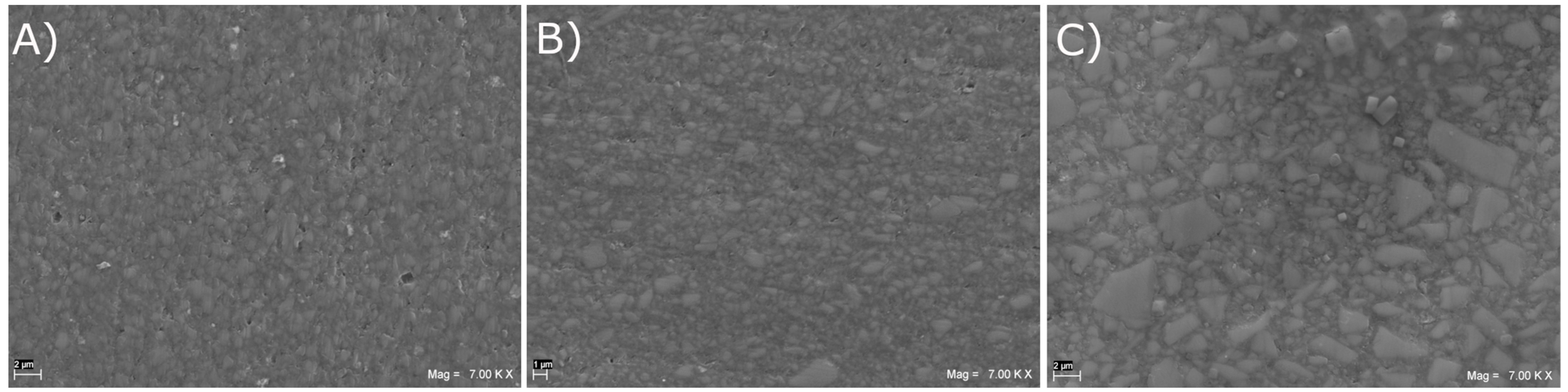
2.6. Scanning Electron Microscopy Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lambrechts, P.; Braem, M.; Vuylsteke-Wauters, M.; Vanherle, G. Quantitative in vivo wear of human enamel. J. Dent. Res. 1989, 68, 1752–1754. [Google Scholar] [CrossRef]
- Seghi, R.R.; Rosenstiel, S.F.; Bauer, P. Abrasion of human enamel by different dental ceramics in vitro. J. Dent. Res. 1991, 70, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Yip, K.H.; Smales, R.J.; Kaidonis, J.A. Differential wear of teeth and restorative materials: Clinical implications. Int. J. Prosthodont. 2004, 17, 350–356. [Google Scholar]
- Dahl, B.L.; Oilo, G. In vivo wear ranking of some restorative materials. Quintessence Int. 1994, 25, 561–565. [Google Scholar] [PubMed]
- Ramp, M.H.; Suzuki, S.; Cox, C.F.; Lacefield, W.R.; Koth, D.L. Evaluation of wear: Enamel opposing three ceramic materials and a gold alloy. J. Prosthet. Dent. 1997, 77, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Sato, Y.; Ohkubo, C.; Hosoi, T. In vitro wear resistance of three types of composite resin denture teeth. J. Prosthet. Dent. 2005, 94, 453–457. [Google Scholar] [CrossRef]
- Ogle, R.E.; Davis, E.L. Clinical wear study of three commercially available artificial tooth materials: Thirty-six month results. J. Prosthet. Dent. 1998, 79, 145–151. [Google Scholar] [CrossRef]
- De Angelis, F.; Buonvivere, M.; Sorrentino, E.; Rondoni, G.D.; D’Arcangelo, C. Wear Properties of Conventional and High-Translucent Zirconia-Based Materials. Materials 2022, 15, 7324. [Google Scholar] [CrossRef]
- Johnson, R.; Verrett, R.; Haney, S.; Mansueto, M.; Challa, S. Marginal Gap of Milled versus Cast Gold Restorations. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2017, 26, 56–63. [Google Scholar] [CrossRef]
- Christensen, G.J. The most conservative and longest lasting restorative service. Dent. Clin. N. Am. 1976, 20, 351–364. [Google Scholar] [CrossRef]
- Park, J.M.; Hong, Y.S.; Park, E.J.; Heo, S.J.; Oh, N. Clinical evaluations of cast gold alloy, machinable zirconia, and semiprecious alloy crowns: A multicenter study. J. Prosthet. Dent. 2016, 115, 684–691. [Google Scholar] [CrossRef]
- Barco, M.T., Jr.; Synnott, S.A. Precision metal occlusal surfaces for removable partial dentures. Int. J. Prosthodont. 1989, 2, 365–367. [Google Scholar] [PubMed]
- Fong, H.; Dickens, S.H.; Flaim, G.M. Evaluation of dental restorative composites containing polyhedral oligomeric silsesquioxane methacrylate. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2005, 21, 520–529. [Google Scholar] [CrossRef] [PubMed]
- Mokhtar, M.M.; Farahat, D.S.; Eldars, W.; Osman, M.F. Physico-mechanical properties and bacterial adhesion of resin composite CAD/CAM blocks: An in-vitro study. J. Clin. Exp. Dent. 2022, 14, e413–e419. [Google Scholar] [CrossRef] [PubMed]
- D’Arcangelo, C.; Vadini, M.; Buonvivere, M.; De Angelis, F. Safe clinical technique for increasing the occlusal vertical dimension in case of erosive wear and missing teeth. Clin. Case Rep. 2021, 9, e04747. [Google Scholar] [CrossRef]
- Daronch, M.; Rueggeberg, F.A.; De Goes, M.F. Monomer conversion of pre-heated composite. J. Dent. Res. 2005, 84, 663–667. [Google Scholar] [CrossRef]
- Peutzfeldt, A. Resin composites in dentistry: The monomer systems. Eur. J. Oral Sci. 1997, 105, 97–116. [Google Scholar] [CrossRef]
- Amirouche-Korichi, A.; Mouzali, M.; Watts, D.C. Effects of monomer ratios and highly radiopaque fillers on degree of conversion and shrinkage-strain of dental resin composites. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2009, 25, 1411–1418. [Google Scholar] [CrossRef]
- Vadini, M.; D’Amario, M.; De Angelis, F.; Falco, A.; D’Arcangelo, C. No-Prep Rehabilitation of Fractured Maxillary Incisors with Partial Veneers. J. Esthet. Restor. Dent. Off. Publ. Am. Acad. Esthet. Dent. 2016, 28, 351–358. [Google Scholar] [CrossRef]
- Grazioli, G.; Francia, A.; Cuevas-Suárez, C.E.; Zanchi, C.H.; Moraes, R.R. Simple and Low-Cost Thermal Treatments on Direct Resin Composites for Indirect Use. Braz. Dent. J. 2019, 30, 279–284. [Google Scholar] [CrossRef]
- Lepesqueur, M.; Surriaga, P.; Masache, M.E.; Vasquez, B.; Pena, M.; Gomes, O.M.M.; Dominguez, J.A. Effects on Micro-Hardness and Conversion Level of Two Types of Resins Undergoing Post-Polymerization Treatments/Efectos sobre microdureza y grado de conversion de dos tipos de resinas sometidas a tratamientos de pospolimerizacion/Efeitos sobre microdureza e grau de conversao de dois tipos de resinas submetidas a tratamentos de pos-polimerizacao. Rev. Nac. De. Odontol. 2015, 11, 49–57. [Google Scholar]
- Cruz, F.L.G.; Carvalho, R.F.; Batista, C.H.T.; Siqueira-Júnior, H.M.; Queiroz, J.R.C.; Leite, F.P.P. Efecto del tratamiento térmico y de fibras de polietileno en la resistencia a la flexión de resinas compuestas. Acta Odontol. Venez. 2014, 52, 3–4. [Google Scholar]
- Zamalloa-Quintana, M.; López-Gurreonero, C.; Santander-Rengifo, F.M.; Ladera-Castañeda, M.; Castro-Pérez Vargas, A.; Cornejo-Pinto, A.; Cervantes-Ganoza, L.; Cayo-Rojas, C. Effect of additional dry heat curing on microflexural strength in three types of resin composite: An in vitro study. Crystals 2022, 12, 1045. [Google Scholar] [CrossRef]
- Aguirre, B.C.; Chen, J.H.; Kontogiorgos, E.D.; Murchison, D.F.; Nagy, W.W. Flexural strength of denture base acrylic resins processed by conventional and CAD-CAM methods. J. Prosthet. Dent. 2020, 123, 641–646. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J. A Comparison of the Flexural and Impact Strengths and Flexural Modulus of CAD/CAM and Conventional Heat-Cured Polymethyl Methacrylate (PMMA). J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2020, 29, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J.; Özcan, M. A Comparison of the Surface Properties of CAD/CAM and Conventional Polymethylmethacrylate (PMMA). J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2019, 28, 452–457. [Google Scholar] [CrossRef]
- Al-Qarni, F.D.; Goodacre, C.J.; Kattadiyil, M.T.; Baba, N.Z.; Paravina, R.D. Stainability of acrylic resin materials used in CAD-CAM and conventional complete dentures. J. Prosthet. Dent. 2020, 123, 880–887. [Google Scholar] [CrossRef]
- Gruber, S.; Kamnoedboon, P.; Özcan, M.; Srinivasan, M. CAD/CAM Complete Denture Resins: An In Vitro Evaluation of Color Stability. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2021, 30, 430–439. [Google Scholar] [CrossRef]
- Alp, G.; Johnston, W.M.; Yilmaz, B. Optical properties and surface roughness of prepolymerized poly(methyl methacrylate) denture base materials. J. Prosthet. Dent. 2019, 121, 347–352. [Google Scholar] [CrossRef]
- Murat, S.; Alp, G.; Alatalı, C.; Uzun, M. In Vitro Evaluation of Adhesion of Candida albicans on CAD/CAM PMMA-Based Polymers. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2019, 28, e873–e879. [Google Scholar] [CrossRef]
- Al-Fouzan, A.F.; Al-Mejrad, L.A.; Albarrag, A.M. Adherence of Candida to complete denture surfaces in vitro: A comparison of conventional and CAD/CAM complete dentures. J. Adv. Prosthodont. 2017, 9, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Ayman, A.D. The residual monomer content and mechanical properties of CAD\CAM resins used in the fabrication of complete dentures as compared to heat cured resins. Electron. Physician 2017, 9, 4766–4772. [Google Scholar] [CrossRef]
- Kattadiyil, M.T.; Jekki, R.; Goodacre, C.J.; Baba, N.Z. Comparison of treatment outcomes in digital and conventional complete removable dental prosthesis fabrications in a predoctoral setting. J. Prosthet. Dent. 2015, 114, 818–825. [Google Scholar] [CrossRef]
- Srinivasan, M.; Schimmel, M.; Naharro, M.; Neill, C.O.; McKenna, G.; Müller, F. CAD/CAM milled removable complete dentures: Time and cost estimation study. J. Dent. 2019, 80, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.Y.; Yang, T.C.; Wang, T.M.; Lin, L.D. Effects of fabrication techniques on denture base adaptation: An in vitro study. J. Prosthet. Dent. 2020, 124, 740–747. [Google Scholar] [CrossRef]
- McLaughlin, J.B.; Ramos, V., Jr.; Dickinson, D.P. Comparison of Fit of Dentures Fabricated by Traditional Techniques Versus CAD/CAM Technology. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2019, 28, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Cantin, Y.; Mehl, A.; Gjengedal, H.; Müller, F.; Schimmel, M. CAD/CAM milled removable complete dentures: An in vitro evaluation of trueness. Clin. Oral. Investig. 2017, 21, 2007–2019. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, B.J.; Goodacre, C.J.; Baba, N.Z.; Kattadiyil, M.T. Comparison of denture base adaptation between CAD-CAM and conventional fabrication techniques. J. Prosthet. Dent. 2016, 116, 249–256. [Google Scholar] [CrossRef]
- da Costa, L.P.G.; Zamalloa, S.I.D.; Alves, F.A.M.; Spigolon, R.; Mano, L.Y.; Costa, C.; Mazzo, A. 3D printers in dentistry: A review of additive manufacturing techniques and materials. Clin. Lab. Res. Dent. 2021, 1–10. [Google Scholar] [CrossRef]
- Abualsaud, R.; Gad, M.M. Flexural Strength of CAD/CAM Denture Base Materials: Systematic Review and Meta-analysis of In-vitro Studies. J. Int. Soc. Prev. Community Dent. 2022, 12, 160–170. [Google Scholar] [CrossRef]
- Nguyen, J.F.; Migonney, V.; Ruse, N.D.; Sadoun, M. Resin composite blocks via high-pressure high-temperature polymerization. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2012, 28, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Lambert, H.; Durand, J.C.; Jacquot, B.; Fages, M. Dental biomaterials for chairside CAD/CAM: State of the art. J. Adv. Prosthodont. 2017, 9, 486–495. [Google Scholar] [CrossRef]
- McCabe, J.F.; Ogden, A.R. The relationship between porosity, compressive fatigue limit and wear in composite resin restorative materials. Dent. Mater. Off. Publ. Acad. Dent. Mater. 1987, 3, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Brosh, T.; Ferstand, N.; Cardash, H.; Baharav, H. Effect of polymerization under pressure on indirect tensile mechanical properties of light-polymerized composites. J. Prosthet. Dent. 2002, 88, 381–387. [Google Scholar] [CrossRef]
- De Angelis, F.; D’Arcangelo, C.; Malíšková, N.; Vanini, L.; Vadini, M. Wear Properties of Different Additive Restorative Materials Used for Onlay/Overlay Posterior Restorations. Oper. Dent. 2020, 45, E156–E166. [Google Scholar] [CrossRef] [PubMed]
- D’Arcangelo, C.; Vanini, L.; Rondoni, G.D.; Vadini, M.; De Angelis, F. Wear Evaluation of Prosthetic Materials Opposing Themselves. Oper. Dent. 2018, 43, 38–50. [Google Scholar] [CrossRef]
- D’Arcangelo, C.; Vanini, L.; Rondoni, G.D.; De Angelis, F. Wear properties of dental ceramics and porcelains compared with human enamel. J. Prosthet. Dent. 2016, 115, 350–355. [Google Scholar] [CrossRef]
- D’Arcangelo, C.; Vanini, L.; Rondoni, G.D.; Pirani, M.; Vadini, M.; Gattone, M.; De Angelis, F. Wear properties of a novel resin composite compared to human enamel and other restorative materials. Oper. Dent. 2014, 39, 612–618. [Google Scholar] [CrossRef]
- Heintze, S.D. How to qualify and validate wear simulation devices and methods. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2006, 22, 712–734. [Google Scholar] [CrossRef]
- Heintze, S.D.; Faouzi, M.; Rousson, V.; Ozcan, M. Correlation of wear in vivo and six laboratory wear methods. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2012, 28, 961–973. [Google Scholar] [CrossRef]
- Heintze, S.D.; Reichl, F.X.; Hickel, R. Wear of dental materials: Clinical significance and laboratory wear simulation methods -A review. Dent. Mater. J. 2019, 38, 343–353. [Google Scholar] [CrossRef]
- Grütter, L.; Vailati, F. Full-mouth adhesive rehabilitation in case of severe dental erosion, a minimally invasive approach following the 3-step technique. Eur. J. Esthet. Dent. Off. J. Eur. Acad. Esthet. Dent. 2013, 8, 358–375. [Google Scholar]
- Bencharit, S.; Schardt-Sacco, D.; Border, M.B.; Barbaro, C.P. Full mouth rehabilitation with implant-supported prostheses for severe periodontitis: A case report. Open Dent. J. 2010, 4, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, K.E.; Whitters, J.; Ju, X.; Pierce, S.G.; MacLeod, C.N.; Murray, C.A. Clinical Monitoring of Tooth Wear Progression in Patients over a Period of One Year Using CAD/CAM. Int. J. Prosthodont. 2017, 30, 153–155. [Google Scholar] [CrossRef] [PubMed]
- Anusavice, K.J.; Shen, C.; Rawls, H.R. Phillips’ Science of Dental Materials; Elsevier Health Sciences: Philadelphia, PA, USA, 2012. [Google Scholar]
- Suzuki, S.; Leinfelder, K.F. Wear of enamel cusps opposed by posterior composite resin. Quintessence Int. 1993, 24, 885–890. [Google Scholar]
- Shimane, T.; Endo, K.; Zheng, J.H.; Yanagi, T.; Ohno, H. Wear of opposing teeth by posterior composite resins--evaluation of newly developed wear test methods. Dent. Mater. J. 2010, 29, 713–720. [Google Scholar] [CrossRef]
- Fischer, T.E.; Anderson, M.P.; Jahanmir, S. Influence of fracture toughness on the wear resistance of yttria-doped zirconium oxide. J. Am. Ceram. Soc. 1989, 72, 252–257. [Google Scholar] [CrossRef]
- Garoushi, S.; Lassila, L.; Vallittu, P.K. Impact of Fast High-Intensity versus Conventional Light-Curing Protocol on Selected Properties of Dental Composites. Materials 2021, 14, 1381. [Google Scholar] [CrossRef]
- Cha, H.S.; Lee, Y.K.; Lim, B.S.; Rhee, S.H.; Yang, H.C. Evaluation of wear resistance of dental resin composites with a 3D profilometer. J. Biomed. Mater. Res. Part. B Appl. Biomater. 2004, 71, 414–420. [Google Scholar] [CrossRef]
- Lim, B.S.; Ferracane, J.L.; Condon, J.R.; Adey, J.D. Effect of filler fraction and filler surface treatment on wear of microfilled composites. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2002, 18, 1–11. [Google Scholar] [CrossRef]
- Bayne, S.C.; Taylor, D.F.; Heymann, H.O. Protection hypothesis for composite wear. Dent. Mater. Off. Publ. Acad. Dent. Mater. 1992, 8, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Sumino, N.; Tsubota, K.; Takamizawa, T.; Shiratsuchi, K.; Miyazaki, M.; Latta, M.A. Comparison of the wear and flexural characteristics of flowable resin composites for posterior lesions. Acta Odontol. Scand. 2013, 71, 820–827. [Google Scholar] [CrossRef]
- Zaim, B.; Serin Kalay, T.; Purcek, G. Friction and wear behavior of chairside CAD-CAM materials against different types of antagonists: An in vitro study. J. Prosthet. Dent. 2022, 128, 803–813. [Google Scholar] [CrossRef] [PubMed]
- Lukomska-Szymanska, M.; Radwanski, M.; Kharouf, N.; Mancino, D.; Tassery, H.; Caporossi, C.; Inchingolo, F.; de Almeida Neves, A.; Chou, Y.F.; Sauro, S. Evaluation of Physical-Chemical Properties of Contemporary CAD/CAM Materials with Chromatic Transition “Multicolor”. Materials 2023, 16, 4189. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Someya, T.; Kawada, E.; Ohyama, T.; Yoshinari, M.; Takemoto, S.; Hattori, M. In vitro wear behavior of restorative resin composites against bovine enamel. Dent. Mater. J. 2020, 39, 915–923. [Google Scholar] [CrossRef]
- Elfakhri, F.; Alkahtani, R.; Li, C.; Khaliq, J. Influence of filler characteristics on the performance of dental composites: A comprehensive review. Ceram. Int. 2022, 48, 27280–27294. [Google Scholar] [CrossRef]
- Blackham, J.T.; Vandewalle, K.S.; Lien, W. Properties of hybrid resin composite systems containing prepolymerized filler particles. Oper. Dent. 2009, 34, 697–702. [Google Scholar] [CrossRef]
- Koottathape, N.; Takahashi, H.; Iwasaki, N.; Kanehira, M.; Finger, W.J. Two- and three-body wear of composite resins. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2012, 28, 1261–1270. [Google Scholar] [CrossRef]
- Turssi, C.P.; De Moraes Purquerio, B.; Serra, M.C. Wear of dental resin composites: Insights into underlying processes and assessment methods--a review. J. Biomed. Mater. Res. Part. B Appl. Biomater. 2003, 65, 280–285. [Google Scholar] [CrossRef]
- Preis, V.; Behr, M.; Handel, G.; Schneider-Feyrer, S.; Hahnel, S.; Rosentritt, M. Wear performance of dental ceramics after grinding and polishing treatments. J. Mech. Behav. Biomed. Mater. 2012, 10, 13–22. [Google Scholar] [CrossRef]
- Heintze, S.D.; Cavalleri, A.; Forjanic, M.; Zellweger, G.; Rousson, V. Wear of ceramic and antagonist--a systematic evaluation of influencing factors in vitro. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2008, 24, 433–449. [Google Scholar] [CrossRef] [PubMed]
- Matzinger, M.; Hahnel, S.; Preis, V.; Rosentritt, M. Polishing effects and wear performance of chairside CAD/CAM materials. Clin. Oral Investig. 2019, 23, 725–737. [Google Scholar] [CrossRef] [PubMed]
- Bollen, C.M.; Lambrechts, P.; Quirynen, M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dent. Mater. Off. Publ. Acad. Dent. Mater. 1997, 13, 258–269. [Google Scholar]
- Aydın, N.; Topçu, F.T.; Karaoğlanoğlu, S.; Oktay, E.A.; Erdemir, U. Effect of finishing and polishing systems on the surface roughness and color change of composite resins. J. Clin. Exp. Dent. 2021, 13, e446–e454. [Google Scholar] [CrossRef]
- Soriano-Valero, S.; Román-Rodriguez, J.L.; Agustín-Panadero, R.; Bellot-Arcís, C.; Fons-Font, A.; Fernández-Estevan, L. Systematic review of chewing simulators: Reality and reproducibility of in vitro studies. J. Clin. Exp. Dent. 2020, 12, e1189–e1195. [Google Scholar] [CrossRef]
- Condon, J.R.; Ferracane, J.L. Evaluation of composite wear with a new multi-mode oral wear simulator. Dent. Mater. Off. Publ. Acad. Dent. Mater. 1996, 12, 218–226. [Google Scholar] [CrossRef]
- Heintze, S.D.; Barkmeier, W.W.; Latta, M.A.; Rousson, V. Round robin test: Wear of nine dental restorative materials in six different wear simulators—Supplement to the round robin test of 2005. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2011, 27, e1–e9. [Google Scholar] [CrossRef]
- Heintze, S.D.; Zellweger, G.; Cavalleri, A.; Ferracane, J. Influence of the antagonist material on the wear of different composites using two different wear simulation methods. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2006, 22, 166–175. [Google Scholar] [CrossRef]
- Hu, X.; Zhang, Q.; Ning, J.; Wu, W.; Li, C. Study of Two-Body Wear Performance of Dental Materials. J. Natl. Med. Assoc. 2018, 110, 250–255. [Google Scholar] [CrossRef]
- Yılmaz, E.C.; Sadeler, R. Investigation of three-body wear of dental materials under different chewing cycles. Sci. Eng. Compos. Mater. 2018, 25, 781–787. [Google Scholar] [CrossRef]
- Aksel, H.; Askerbeyli-Örs, S.; Deniz-Sungur, D. Vertical root fracture resistance of simulated immature permanent teeth filled with MTA using different vehicles. J. Clin. Exp. Dent. 2017, 9, e178–e181. [Google Scholar] [CrossRef] [PubMed]

| Material | Lot Number | Shade | Manufacturer | Technical Data |
|---|---|---|---|---|
| Ena Cad | 030724 | UD 3.5 | Micerium S.p.A (Genova, Italy) | Highly cross-linked polymer blends (UDMA, BDDMA), in which inorganic silicate glass filling material are embedded to 71.56% by weight. Average particle size: 0.80 µm and a variation range of 0.20 µm to 3.0 µm. Stabilizers, light stabilizers and pigments are included |
| Brilliant Crios | M85399 | A2 | Coltene/Whaledent AG (Altstätten, Switzerland) | Resin matrix: Cross-linked methacrylates; Filler: SiO2 (size < 20 nm), Barium glass (size < 1.0 µm); Inorganic pigments |
| Grandio disc | 2336410 | A2 | VOCO GmbH (Cuxhaven, Germany) | Nano-hybrid composite. Grandio disc contains 86% w/w inorganic fillers embedded within a polymer matrix |
| Aurocast 8 | 15L 02 55 | - | Nobil-Metal S.p.A. (Villafranca d’Asti, Italy) | Type 3 high-gold dental alloy. Composition (w/w): Au = 85.4%, Ag = 9.0%, Cu = 5.0%, Pd = 1.0%, Ir = 1.0% |
| Material | Sample Vertical Wear (SD) A | Antagonist Vertical Wear (SD) B | Total Vertical Wear (SD) A + B |
|---|---|---|---|
| Ena Cad | 0.061 (0.044) a | 0.140 (0.037) a | 0.202 (0.045) a |
| Brilliant Crios | 0.067 (0.036) a | 0.212 (0.107) a | 0.279 (0.093) a |
| Grandio disc | 0.086 (0.050) a | 0.179 (0.079) a | 0.265 (0.097) a |
| Aurocast 8 | 0.076 (0.017) a | 0.141 (0.050) a | 0.217 (0.045) a |
| Material | Sample Volumetric Loss (SD) C | Antagonist Volumetric Loss (SD) D | Total Volumetric Loss (SD) C + D |
|---|---|---|---|
| Ena Cad | 0.055 (0.042) b | 0.062 (0.029) a | 0.117 (0.043) a |
| Brilliant Crios | 0.049 (0.030) b | 0.156 (0.128) a | 0.206 (0.118) a |
| Grandio disc | 0.078 (0.066) b | 0.109 (0.092) a | 0.186 (0.125) a |
| Aurocast 8 | 0.148 (0.065) a | 0.066 (0.036) a | 0.213 (0.069) a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Arcangelo, C.; Vadini, M.; Vanini, L.; Rondoni, G.D.; Sorrentino, E.; De Angelis, F. In Vitro Wear Properties of a New CAD/CAM Dental Resin Composite in a Chewing Simulation Test Opposing Itself. Appl. Sci. 2025, 15, 5023. https://doi.org/10.3390/app15095023
D’Arcangelo C, Vadini M, Vanini L, Rondoni GD, Sorrentino E, De Angelis F. In Vitro Wear Properties of a New CAD/CAM Dental Resin Composite in a Chewing Simulation Test Opposing Itself. Applied Sciences. 2025; 15(9):5023. https://doi.org/10.3390/app15095023
Chicago/Turabian StyleD’Arcangelo, Camillo, Mirco Vadini, Lorenzo Vanini, Giuseppe Daniele Rondoni, Edoardo Sorrentino, and Francesco De Angelis. 2025. "In Vitro Wear Properties of a New CAD/CAM Dental Resin Composite in a Chewing Simulation Test Opposing Itself" Applied Sciences 15, no. 9: 5023. https://doi.org/10.3390/app15095023
APA StyleD’Arcangelo, C., Vadini, M., Vanini, L., Rondoni, G. D., Sorrentino, E., & De Angelis, F. (2025). In Vitro Wear Properties of a New CAD/CAM Dental Resin Composite in a Chewing Simulation Test Opposing Itself. Applied Sciences, 15(9), 5023. https://doi.org/10.3390/app15095023







