Abstract
The aim of this study was to assess the mechanical properties of experimental flow composites incorporating remineralizing and bactericidal fillers (hydroxyapatite (HAp), calcium fluoride, and nanosilver). The evaluated properties included wear resistance, dynamic properties (impact strength), hardness, and static strength (compressive and bending strength). This work includes SEM analysis. The specimens were prepared using a commercial light-cured composite material based on bisphenol A-glycidyl dimethacrylate (Bis-GMA) (Arkona Flow Art, Niemce, Poland) and composite material modified by adding 2 wt%, 5 wt% of hydroxyapatite powder containing fluoride (calcium fluoride), and nanosilver. For this purpose, hydroxyapatite (HAp) with a grain size of 30 μm, which was previously synthesized using the wet method, was used. The results were evaluated against the ISO 4049 standard. The results were subjected to statistical analysis using IBM SPSS Statistics, version 29 (IBM Corp., Armonk, NY, USA). A significance level of 5% (α = 0.05) was established. Based on the hardness measurements obtained in this study, it can be concluded that the incorporation of hydroxyapatite, calcium fluoride, and nanosilver fillers increased the hardness of the flowable composites (89 ShD). The results revealed that incorporating fillers such as hydroxyapatite, nanosilver, and calcium fluoride led to a decrease in the impact strength of the material (0.095 J/cm2). The results of the compressive strength tests revealed that the flowable composite containing 2 wt% of HAp, F, and Ag exhibited the highest compressive strength (190 MPa) among all of the tested materials. Among the experimental composites, the highest bending strength was observed in the variant containing 2 wt% of HAp, F, and Ag, with a value of 76.48 MPa. Significantly higher wear was observed for the composite containing nanosilver filler (4.02 × 10−4 Mm3/Nm) compared to the other composites. However, the inclusion of nanosilver as a filler in the composite matrix was found to significantly deteriorate the mechanical properties of the material.
1. Introduction
Dental caries is classified as a bacterial disease affecting the hard tissues of the tooth. Its primary etiology lies in the presence of specific bacteria within the oral cavity. Among these, the most pronounced is anaerobic, Gram-positive Streptococcus mutans (S. mutans) [1,2,3]. These microorganisms, present within dental plaque, metabolize dietary sugars, leading to the production of acids that demineralize and degrade tooth structures [1,2,3,4,5].
Modern dentistry provides various solutions for reconstructing lost tooth tissues, depending on the size and location of the defect. Among the most frequently employed materials are ceramics and composites. Ceramic materials are typically utilized for extensive defects requiring prosthetic treatment, while chemically cured and light-cured composites are preferred for direct restorations [6]. Dental composites consist of the following three primary components: a resin matrix (bisphenol A, urethane dimethacrylate), fillers (silicon oxide, quartz), and a coupling agent (vinyl silane) [7,8,9,10]. Light-cured composites contain camphorquinone, a photoinitiator responsible for initiating the polymerization process under visible light. The free radical polymerization reaction is triggered upon exposure to light at a wavelength of 470 nm [11,12,13]. For chemically cured composites, the polymerization process is initiated by mixing two components: an organic amine and an organic peroxide [14]. The composition of the organic matrix significantly influences the resulting composite’s properties, including its mechanical strength, sorption, solubility, polymerization shrinkage, abrasion resistance, color stability, and biocompatibility [15,16,17,18]. Dental composites have become widely popular due to their aesthetics and favorable mechanical and functional properties, as well as their cost effectiveness. Despite these advantages, further advancements are needed, particularly in improving aesthetics and enhancing mechanical strength. Recent research efforts have concentrated on enhancing the properties of composites by either modifying the binder or developing novel fillers. For instance, Chistyakov et al. [19] explored the use of a mixture of cyclotriphosphazenes containing 4-allyl-2-methoxyphenoxy and βcarboxyethylphenoxy groups as a binder modifier. This approach has the potential to improve the adhesion of composite materials to dental tissues. Additionally, binder modification with aliphatic acid chlorides has been demonstrated to reduce both the viscosity and polymerization shrinkage of composite materials.
Over the past decade, nanotechnology has significantly advanced the development of dental materials for reconstructing lost tooth tissues. Nanoparticles have been incorporated into polymer matrices to enhance material properties. These particles, characterized by small size (from 0.1 to 100 nm) and a high specific surface area, allow us to obtain superior mechanical, chemical, optical, and magnetic properties compared to the particles in macroscale [20,21,22]. Mechanical properties can be enhanced by improving the bending strength, hardness, and resistance to tribological wear. Certain nanoparticles also exhibit good electrical insulation, thermal stability, and corrosion resistance. Furthermore, particles like zirconium oxide, which possesses a high refractive index and a low absorption coefficient, can significantly enhance the optical properties of the materials. Beyond classifications based on size and shape, functional fillers also represent a distinct category, as illustrated in Figure 1.
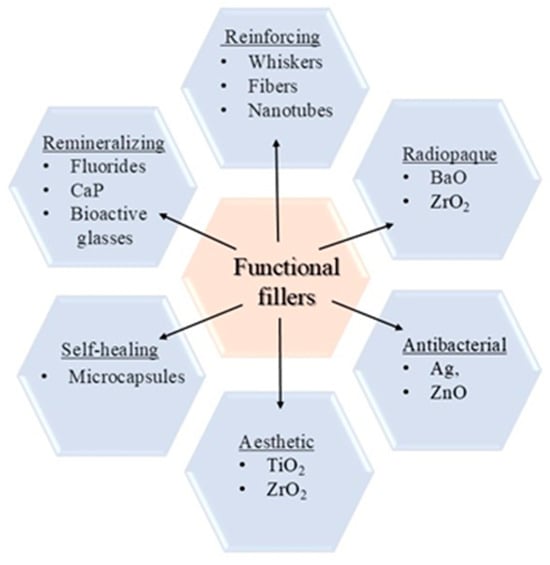
Figure 1.
Types of functional fillers.
The current literature indicates a significant interest among researchers in the use of functional fillers in dentistry, primarily due to their applicability across various dental specialties. Commonly used fillers for modifying polymer matrices include silicon dioxide (SiO2), titanium dioxide (TiO2), and zirconium dioxide (ZrO2) [21]. A study by Tian et al. demonstrated that incorporating SiO2 particles into composite resin led to a substantial enhancement in flexural strength [10]. Similar findings were reported by Hameed and Abdul Rahman, who researched the incorporation of ZrO2 particles [23]. Recently, there has also been a growing use of antibacterial fillers [24,25,26,27,28], which play a crucial role in addressing the issue of secondary caries [24,29,30]. Additionally, calcium phosphate fillers (i.e., hydroxyapatite (HAp)) are gaining attention due to their excellent biocompatibility and bioactivity [31,32]. Worryingly, some studies report unsatisfactory mechanical properties when these materials are used as fillers in dental composites [11,33]. This highlights the need for further research to enhance their performance. An effort to address this issue was made by Mohammad Mahdi Taheri et al. [34], who utilized fluorohydroxyapatite (FHA) nanotubes in their experiments. Their findings demonstrated improved mechanical properties in composites based on Bis-GMA resin [34]. Additionally, our findings suggest that the incorporation of various fillers, including remineralizing and antibacterial agents, holds significant potential for enhancing composite properties. A synergistic effect can often be achieved by combining different fillers. For instance, the addition of nanosilver enhances the antibacterial properties of the composite, potentially addressing the issue of secondary caries formation. Without any doubt, achieving strong adhesion between the composite and tooth tissues remains a critical aspect of development. While studies such as those by Mohammad Mahdi Taheri [34] have explored the use of nanotubes, our research focused on the use of nanoparticles as fillers. Notably, no prior research has simultaneously employed three distinct filler particles hydroxyapatite, calcium fluoride, and nanosilver to modify the same composite.
In recent years, most researchers have focused on the modification of composite materials using hydroxyapatite (HAp) fillers. The introduction of this type of filler is intended to achieve much better aesthetic results. Commercial dental composites discolor after some time. This is caused by aggressive conditions in the oral cavity and the intake of coloring liquids such as coffee, tea, and red wine. However, achieving better aesthetic results may involve the deterioration of mechanical properties. Therefore, attempts have been made to improve mechanical properties while maintaining aesthetics. For this purpose, additional fillers, such as fluoride and nanosilver, have been introduced. Additionally, the introduction of nanosilver was intended to reduce bacterial adhesion. So far, scientists have not introduced the three different functional fillers hydroxyapatite, fluorine, and nanosilver into the flow composite based on bisphenol A-glycidyl dimethacrylate (Bis-GMA). Our work is the only one that focuses on the introduction of different fillers such as hydroxyapatite (HAp), fluoride, and nanosilver. Most of the current research work has been conducted on other types of composites, such as (UDMA), TEGDMA, and glass ionomers, and using only one or two functional fillers. Previous research work has focused on the use of nano-sized hydroxyapatite. In our work, hydroxyapatite was used in the macroscale. We are the only ones who have performed impact strength tests for dental composites.
The aim of this study was to assess the mechanical properties of experimental flow composites incorporating remineralizing and bactericidal fillers (hydroxyapatite, calcium fluoride, and nanosilver). The evaluated properties included wear resistance, dynamic properties (impact strength), hardness, and static strength (compressive and bending strength). The null hypothesis posited that the incorporation of hydroxyapatite, calcium fluoride, and nanosilver as fillers in dental composites does not affect their mechanical properties.
2. Materials and Methods
To carry out the research experiment, 25 specimens were prepared using a commercial flowable light-cured composite material based on bisphenol A-glycidyl dimethacrylate (Bis-GMA) (Arkona Flow Art, Niemce, Poland) and composite material modified by adding 2 wt% and 5 wt% of hydroxyapatite powder containing fluoride (calcium fluoride) and nanosilver. Hydroxyapatite (HAp) with a grain size of 30 μm was used for this purpose. Anhydrous calcium fluoride (Sigma-Aldrich, Saint Louis, MO, USA) with a purity of 99.99% was incorporated at a concentration of 0.2 wt%. Nanosilver (Sigma-Aldrich, Saint Louis, MO, USA) was added in nanopowder form at a concentration of 1 wt% with a particle size of less than 100 nm. Table 1 contains the designations of the individual specimens.

Table 1.
Designations of individual groups of specimens.
Table 2 provides a detailed description of each group of specimens (n = 5).

Table 2.
Characteristics of the researched specimens.
All of the experimental specimens were prepared in accordance with ISO standards and norms [35,36,37,38,39,40]. Firstly, the hydroxyapatite filler was synthesized using the so-called wet method. Calcium hydroxide (Ca(OH)2) (Sigma-Aldrich, Saint Louis, MO, USA) and orthophosphoric acid (H3PO4) (Sigma-Aldrich, Saint Louis, MO, USA) were utilized as starting materials for the synthesis of hydroxyapatite. Hydroxyapatite crystals were formed through a precipitation reaction, followed by washing through decantation using distilled water. The resulting hydroxyapatite was then fractionated with the aid of a LPzE-3e laboratory shaker (MULTISERW-Morek, Brzeźnica, Poland). The grinding and fractionation process was carried out to produce hydroxyapatite grains with a maximum particle size of 30 µm. The following set of sieves with different-sized openings were used: 0.035 mm, 0.05 mm, and 0.1 mm. The obtained hydroxyapatite was subjected to grinding using a planetary ball mill (Retsch PM 100, Retsh GmbH, Haan, Germany). The hydroxyapatite powder was subsequently enriched with additives calcium fluoride and nanosilver. It was integrated into the composite material in a microvial using a Roti-Speed agitator (Carl Roth GmbH + Co., KG, Karlsruhe, Germany) at a speed of 5000 rpm for approx. 5 min. The mixing was performed under standardized conditions of temperature and humidity in a darkened room. The obtained composite was stored in polypropylene syringes with a plunger in order to protect the material surface from oxygen inhibition. The specimens were subsequently subjected to polymerization for 20 s using a diode light-curing lamp (Elipar S10, 3M ESPE, St. Paul, MS, USA). This polymerization lamp delivers a light intensity of 1400 mW/cm2 within the wavelength range of 450–490 nm. Each polymerized material layer was 1 mm thick. To fabricate the specimens, a celluloid strip was positioned on a glass slide, over which a silicone mold designed with dimensions specific to the intended test was placed. The portions of the composite material were introduced into the silicone mold using an inserter. Subsequently, the celluloid strip and glass slide were repositioned on the leveled surface of the material to shield it from the inhibitory effects of oxygen exposure. Finally, the specimens were artificially aged by incubation at 37 °C in distilled water for 24 h. These prepared specimens were then subjected to mechanical testing.
2.1. SEM Analysis
SEM images were taken using a JEOL JSM-6610LV (Tokyo, Japan) scanning electron microscope. The analysis of fracture surfaces was performed in high-vacuum mode, the accelerating voltage was 20 kV, and the beam current was 60 mA. Due to the fact that the composite and HAp powder samples are not good conductors, they were coated with a layer of silver. A device for sputtering layers was used (ora POWER SYSTEMS, Wrocław, Poland). The fractures were obtained using liquid nitrogen. The specimens were placed in liquid nitrogen for about 1 min and were then broken using special pincers.
2.2. Hardness Measurements
Hardness measurements were conducted on specimens shaped like cuboid beams with dimensions of 5 mm × 10 mm × 20 mm using a Shore D-type indenter (Elcometer Inc., Warren, MI, USA). A load of 4 kg was applied for 15 s. Measurements were taken from five randomly selected areas on the surfaces of 10 specimens from each group.
2.3. Impact Strength Test
The impact strength was evaluated using rectangular specimens measuring 5 mm × 10 mm × 20 mm. A HIT 5.5p hammer drill (Zwick/Roell, Ulm, Germany) with an energy of 5.5 J was used for the test. The test was carried out on 10 specimens from each group.
2.4. Compressive Strength Test
The compressive strength test was conducted on cylindrical specimens with a diameter of 4 mm and a height of 6 mm using a Walter + Bai testing machine (Walter + Bai AG, Lohningen, Switzerland). The test was carried out on 10 specimens from each group.
2.5. Bending Strength Test
The bending strength test was performed on cuboid beam specimens with dimensions of 2 mm × 2 mm × 25 mm using a multifunctional UMT TriboLab device (Bruker, Karlsruhe, Germany). The traverse speed was set to 0.5 mm/min, with a constant support span of 20 mm. The radii of the supports and the mandrel used as the input were both 1 mm. A total of 10 specimens from each group were tested.
2.6. Tribological Wear Resistance Test
The wear resistance test was conducted on cylindrical specimens, each 2 mm in height and 21 mm in diameter, using a Tribometer device (CSM Instruments, Freiburg, Germany) with Tribox 2.5 software. The test parameters included a speed of 0.05 m/s, a friction radius of 6.75 mm, a load of 1 N, and a friction distance of 100 m. The test was carried out on 10 samples from each group at a temperature of 25 °C in an artificial saliva environment, prepared according to the Fusayama/Meyer formula, as follows: 2 dm3 distilled water, 0.8 g NaCl, 0.8 g KCl, 1.59 g CaCl2·2H2O, 1.56 g NaH2PO4·2H2O, 0.01 g Na2S·9H2O, and 2 g of urea [41]. The specimens were placed in a designated Teflon holder, which was filled with artificial saliva. The friction counter sample used was a zirconium oxide ball with a diameter of 1/8 inch. Wear was assessed by measuring the linear wear traces in the friction area based on surface roughness analysis performed using a Hommel Wave-line 200 profilometer (ITA, Skórzewo, Poland).
The tribological wear was calculated as the volumetric loss of material relative to the friction area [42]. The wear of the composites was assessed by measuring the linear wear along the friction trace, utilizing surface roughness measurements obtained with a profilometer. The wear factor of the dental composites was subsequently calculated using the roughness profile and the following formulas:
Wd—wear factor
Vf—volume war
Fn—load force
L—distance
Vf—volume wear
A—average track cross section
L—distance
The results were subjected to statistical analysis using IBM SPSS Statistics, version 29 (IBM Corp., Armonk, NY, USA). The normality of all variables was not verified by the Shapiro–Wilk test of normality (p < 0.05). Consequently, non-parametric Kruskall–Wallis tests, followed by multiple comparisons with Bonferroni correction, were employed to compare the types of specimens within the variables. A significance level of 5% (α = 0.05) was established.
2.7. Statistical Analysis of Measured Data
Data analysis of the results was carried out using the software IBM SPSS Statistics, version 29 (IBM Corp., Armonk, NY, USA). Since data of all variables did not show a normal distribution, checked by a Shapiro–Wilk normality test (p < 0.05) and Levene homogeneity of variance test (p < 0.05), non-parametric Kruskall–Wallis tests, followed by multiple comparisons (with Bonferroni correction), were used to compare the experimental groups within the variables. All tests were based on a significance level of 5% (α = 0.05)
3. Results
Scanning electron microscopy (SEM) was used to analyze the fracture surfaces of dental composites. To assess the degree of homogeneity of the material, fractures of the prepared composite samples were performed. The fractures of composites containing hydroxyapatite with silver and fluorine are shown in Figure 2.
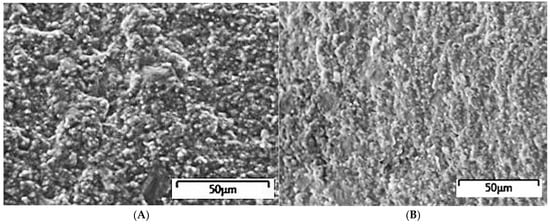
Figure 2.
Surface morphology of fracture composites with HAp, F, and Ag. (A) Fracture of the composite with 2% HAp, F, and Ag. (B) Fracture of the composite with 5% HAp, F, and Ag.
Based on the analysis of the presented SEM images, it can be stated that the flow composite has a homogeneous surface. HAp fillings have particles with significant irregular shapes. The surface of these materials is characterized by irregularity and roughness, which is characteristic of composites with filler particle sizes of the order of several μm. Homogeneity (uniformity) is important because it affects the properties of the obtained materials. The surface morphology may be affected to some extent by changing the proportions of additives.
The Shore hardness values varied between 53 Shore D in a HAp0%, Ag specimen, and 93 Shore D in a HAp2%, F, Ag specimen (Figure 3). There were statistically significant differences in the Shore D hardness of the tested composite specimens (p < 0.001). HAp0%, Ag specimens obtained lower hardness than HAp2%, F, Ag specimens (p < 0.001) and HAp5%, F, Ag specimens (p = 0.006). Also, the differences were statistically significant between HAp0%, F, and HAp2%, F, Ag (p = 0.026). All of the other comparisons were not statistically significant (p > 0.05).
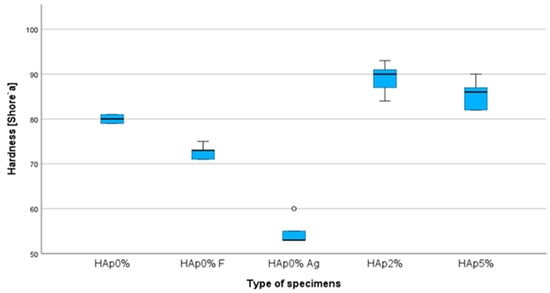
Figure 3.
Box plots of hardness (Shore D) for modified flowable composite resins (n = 5) (◦ symbol represents an outlier).
The impact strength values varied between 0.049 J/cm2, found in a HAp0%, Ag specimen, and 0.138 J/cm2, found in the HAp0% specimen (Figure 4). There were statistically significant differences in the strength of the specimens (p = 0.001). The specimens of HAp0%, F and HAp0%, Ag groups presented statically significant lower strength values than HAp0% (p = 0.024 and p < 0.001, respectively). The differences were also statistically significant between HAp0%, Ag and HAp2%, F, Ag (p = 0.012). Nevertheless, differences between the combined fillers (HAp2%, F, Ag, and HAp5%, F, Ag) and the HAp0% were not statistically significant (p > 0.05).
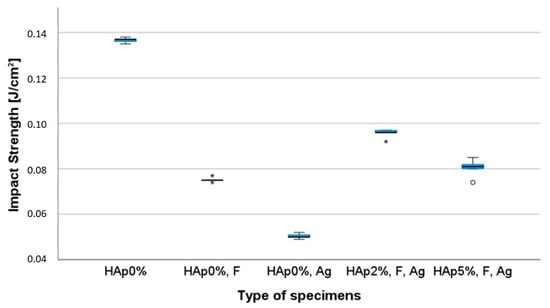
Figure 4.
Box plots of impact strength (J/cm2) for modified flowable composite resins (n = 5) (◦, * symbols represent outliers).
The compressive strength values varied between 100 MPa, found in a HAp0%, Ag specimen, and 195 MPa, found in the HAp2%, F, Ag specimen (Figure 5). There were statistically significant differences in the compressive strength of the specimens (p = 0.003). The differences were statistically significant between HAp0%, Ag compared to HAp2%, F, Ag (p = 0.005) and HAp0% (p = 0.044), with HAp0%, Ag showing lower strength. All of the other comparisons were not found to be statistically significant, showing that combined fillers HAp2%, F, Ag and HAp5%, F, Ag had similar results to the HAp0% specimens (p > 0.05).
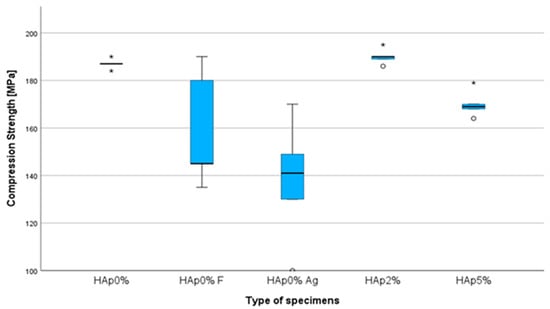
Figure 5.
Box plots of compressive strength (MPa) for modified flowable composite resins (n = 5) (◦, * symbols represent outliers).
The bending strength values varied between 46 MPa, found in a HAp0%, Ag specimen, and 128 MPa, found in a HAp0% specimen (Figure 6). Although statistically significant differences in the bending strength were found (p < 0.001), multiple comparisons showed lower values of HAp0%, Ag specimens when compared to HAp0% (p < 0.001) and HAp2%, F, Ag (p = 0.013) specimens. Also, HAp 0%, F specimens revealed lower bending strength than the HAp0% specimens (p = 0.013). All of the other comparisons were not statistically significant, showing that combined fillers HAp2%, F, Ag and HAp5%, F, Ag had similar results to the HAp0% specimens (p = 0.502 and p = 0.190, respectively).
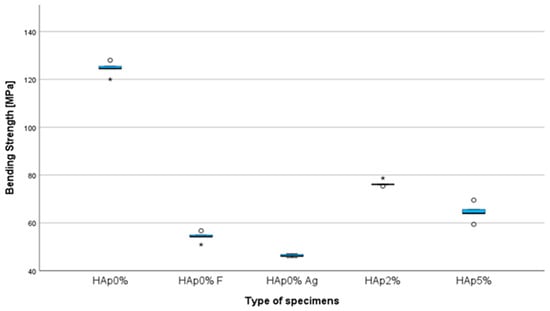
Figure 6.
Box plots of bending strength (MPa) for modified flowable composite resins (n = 5) (◦, * symbols represent outliers).
When tribological wear was tested, the values varied between 1.22 × 10−4 mm3/Nm, obtained by a HAp2%, F, Ag specimen and 5 × 10−4 mm3/Nm, obtained by a HAp0% specimen (Figure 7). Statistically significant differences in the tribological wear were found between the groups (p < 0.001). The differences were statistically significant between HAp0%, Ag and HAp2%, F, Ag (p < 0.001); HAp0% and HAp2%, F, Ag (p = 0.01); and HAp0%, Ag and HAp0%, F (p = 0.026). All of the other comparisons were not statistically significant, including differences between the HAp5%, F, Ag specimens and the HAp0% specimens (p > 0.05).
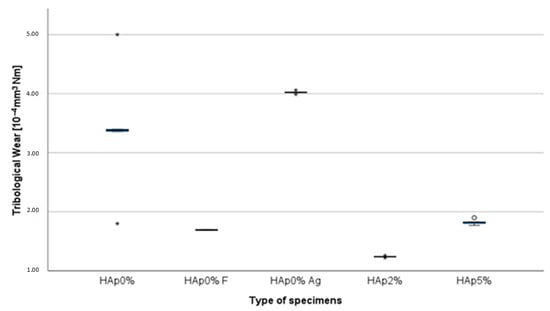
Figure 7.
Box plots of tribological wear (10−4 mm3/Nm) for modified flowable composite resins (n = 5) (◦, * symbols represent outliers).
4. Discussion
The null hypothesis of this study was rejected, as the inclusion of hydroxyapatite, calcium fluoride, and nanosilver as fillers in dental composites was found to have a significant impact on their mechanical properties across all evaluated cases. The differences observed were statistically significant.
Hardness is a crucial property for composite materials, as it reflects the material’s resistance to deformation. It is frequently used as an auxiliary parameter to assess mechanical performance. Based on the hardness measurements obtained in this study, it can be concluded that the incorporation of hydroxyapatite, calcium fluoride, and nanosilver fillers increased the hardness of the flowable composites (89 ShD). This increase in hardness is consistent with findings from another study [43], which examined a composite based on urethane dimethacrylate (UDMA), achieving a hardness value of 85 ShD. Other studies by Taheri, M.M. [34] and Kutbay, I. [44] also confirm the enhancement of mechanical properties, likely due to the strengthening effect of fluoride ions on hydroxyapatite. A key characteristic of hydroxyapatite is its ability to exchange ions, including its interaction with fluoride [44,45]. When hydroxide ions are replaced by fluoride, fluorapatite is formed. According to Tredwin, C.H.J. et al. [46], fluorapatites exhibit superior crystallinity, hardness, and resistance to chemical and physical damage, and are less soluble. As confirmation of this statement, it was observed that composite materials containing fluoride fillers exhibited lower hardness values compared to composites that also included hydroxyapatite. Furthermore, composite samples containing nanosilver without hydroxyapatite or fluoride showed a significant decrease in hardness (54.8 ShD). This reduction in hardness may be attributed to the polymerization process. Jürgen Durner and colleagues [47] suggest that silver nanoparticles may influence the polymerization process in dental materials, leading to an increase in the amount of elutable substances. This process can be attributed to the interaction between silver nanoparticles and various physical and chemical mechanisms. One possible explanation is the reflection and scattering of light from the curing lamp on the surface of the nanoparticles. Chemically, electrons from the metallic silver nanoparticles may react with unpaired electrons in the photoinitiator system. Silver nanoparticles can transfer an electron to the photoinitiator system, accept it, and then store the electrons [47,48]. This effect may hinder the penetration of light into the deeper layers of the composite material. To further investigate this and gain a deeper understanding, future studies should focus on examining the impact of individual fillers on the polymerization process.
In order to assess the materials’ resistance to cracking under dynamic loading, an impact test was performed. The results revealed that incorporating fillers such as hydroxyapatite, nanosilver, and calcium fluoride led to a decrease in the impact strength of the material (0.095 J/cm2), which was proportional to the increasing hydroxyapatite content. A similar reduction in impact strength relative to HAp content was observed in previous research [47], where a different composite based on urethane dimethacrylate resin was used. However, when a hybrid composite containing 2% hydroxyapatite with fluoride and nanosilver was tested (0.128 J/cm2), a higher impact strength was recorded compared to the control sample (0.072 J/cm2).
Given that specific occlusal forces are present within the oral cavity, amounting to approximately 100–150 N in the incisor region [16,49], it is crucial to analyze the forces acting on teeth and dental fillings. The results of the compressive strength tests revealed that the flowable composite containing 2 wt% of HAp, F, and Ag exhibited the highest compressive strength (190 MPa) among all of the tested materials. In comparison, hybrid composites with the same fillers (2 wt% of HAp, F, and Ag) tested in another study achieved an even higher compressive strength (264 MPa) [43]. Other research [50], which tested a flowable composite modified with hydroxyapatite alone, showed a compressive strength of 100 MPa. These findings suggest that the modification of hydroxyapatite with fluoride and nanosilver significantly enhanced the compressive strength of the flowable composites.
The conducted bending tests revealed a decrease in the bending strength of all flowable composites. To assess the applicability of the experimental composites, the ISO 4049 Dentistry Polymer-based restorative materials 2009 standard [35] was applied, which specifies a required bending strength of at least 50 MPa. Therefore, all of the tested flowable composites met this requirement, except for the composite containing nanosilver (46.3 MPa). This difference is minimal. Among the experimental composites, the highest bending strength was observed in the variant containing 2 wt% of HAp, F, and Ag, with a value of 76.48 MPa. In terms of flexural strength, a decline in performance is observed with the inclusion of HAp compared to HAp0%, similar to the trend seen in the wear properties. Additionally, there was a noticeable trend of strength deterioration as the HAp content increased, a finding that aligns with the work of Sirait, M. [51]. They suggest that the strength of composites is influenced by factors such as the type, quantity, and particle size of the material used [52,53,54].
To assess the durability of the material, a tribological wear test was conducted on the experimental composites. The results indicate that the type of filler used significantly influences the abrasive wear of dental composites. The lowest wear values were observed in the experimental composites containing 2 wt% hydroxyapatite, calcium fluoride, and nanosilver (1.24 × 10−4 Mm3/Nm and 5 wt% hydroxyapatite, calcium fluoride, and nanosilver (1.82 × 10−4 Mm3/Nm), compared to the control composite (3.38 × 10−4 Mm3/Nm). Similar studies on hybrid composites containing hydroxyapatite, calcium fluoride, and nanosilver also showed an improvement in tribological properties [50]. The hybrid composite with 1 wt% hydroxyapatite, calcium fluoride, and nanosilver exhibited a wear factor of 1.29 × 10−4 Mm3/Nm, which was very similar to the results observed in this study [50]. The current literature supports the idea that the morphology and particle size of the added filler can influence the tribological and mechanical properties of dental composites [8,9,50,55]. Significantly higher wear was observed for the composite containing nanosilver filler (4.02 × 10−4 Mm3/Nm) compared to the other composites. This effect may be attributed to an improper polymerization process resulting from the addition of nanosilver particles as a filler. Therefore, further investigation into the interaction between nanosilver and other fillers is recommended for future studies.
The conducted studies highlight the significant impact of fillers on dental compo-sites. Despite the deterioration of some mechanical properties, the obtained results are within the standards used for dental composites. The obtained results could have been influenced by the size of the filler particles and their surface properties, which allow for better bonding with the matrix. Filler crystals of different sizes can mutually fill empty spaces, which can result in the strengthening of the material. Materials containing macrofillers show low resistance to abrasion due to the phenomenon of abrasion of the resin surrounding large filler particles and loss of polymer blocks and cohesive fractures of filler particles with the matrix. Composite materials with microfillers have greater resistance to wear due to their more homogeneous structure and high surface smoothness. In these composites, other factors also have an influence on abrasive wear, as follows: the strength of the particle–matrix connection, resistance to brittle fracture of particles, progressive strengthening of the metal matrix caused by strain, and the loss of matrix plasticity. The condition for increasing resistance to abrasive wear is that the load is absorbed by the ceramic particles. However, when particles crack under high loads, subsurface voids accumulate, causing cracking of the subsurface layer and increased abrasive wear of the composite. In turn, nanoscale materials show significant agglomeration of grains. This phenomenon is characteristic of nanoscale materials and can negatively affect the homogeneity of the material.
The studies that were conducted highlight the impact of fillers on flowable composites. Nevertheless, further research is essential to look for their mechanical and functional impact after using a bigger sample size that can allow a regular distribution of the sample without strong deviations of the results. Future studies should focus on determining the influence of fillers (hydroxyapatite, calcium fluoride, and nanosilver) on the polymerization process through the degree of cure evaluations through FTIR or Raman spectroscopy. Additionally, it would be valuable to investigate the effects of aging on the mechanical properties and color stability of the experimental composites, especially in materials incorporating silver that can bring an aesthetic deviation to the composite performance. In this future research, it is also very important to add liberation profile studies of all of the fillers and biocompatibility studies to check if nano-toxicity can be an issue for these combined resins, especially because of silver fillers.
5. Conclusions
The studies that were conducted demonstrate the impact of fillers (hydroxyapatite, calcium fluoride, and nanosilver) on the mechanical properties of flowable dental composites. The best properties were exhibited by the composite containing 2 wt% of hydroxyapatite, calcium fluoride, and nanosilver, as follows: hardness at the level of 89 (Shore D), compressive strength of 264 (MPa), impact strength of 0.128 (J/cm2), bending strength of 76.48 (MPa), and tribological wear of 1.24 (×10−4 Mm3/Nm). The findings suggest that the combination of fillers promoted higher hardness (p < 0.001) and lower tribological wear (p = 0.01) than the non-filler specimens, showing similar results on the other properties. However, the individual inclusion of nanosilver as a filler in the composite matrix was found to significantly deteriorate the impact, compressive, and bending properties of the material. Overall, the modified resins met the adequate mechanical requirements for flowable composites, except for the composite containing only nanosilver. Further experiments should be conducted in the future to improve these materials’ performance.
6. Patents
Modified light-cured composite for dental fillings and its application, Pat.243701.
Author Contributions
Conceptualization, Z.K. and L.K.; methodology, Z.K.; software, C.B.N. and J.C.R.; validation, C.B.N. and J.C.R.; formal analysis, K.D.; investigation, K.D.; resources, Z.K.; data curation, Z.K.; writing—original draft preparation, Z.K.; writing—review and editing, Z.K., L.K., C.B.N. and K.D.; visualization, Z.K. and K.D.; supervision, Z.K.; project administration, Z.K. and L.K.; funding acquisition, Z.K. and L.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
No applicable.
Informed Consent Statement
No applicable.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- Kreth, J.; Merritt, J.; Qi, F. Bacterial and host interactions of oral streptococci. DNA Cell Biol. 2009, 28, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.S.; Chu, C.-H.; Yu, O.Y. Oral Microbiome and Dental Caries Development. Dent. J. 2022, 10, 184. [Google Scholar] [CrossRef] [PubMed]
- De Soet, J.J.; Van Gemert-Schriks, M.C. Host and microbiological factors related to dental caries development. Caries Res. 2008, 42, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Daliri, E.B.-M.; Kim, N.; Kim, J.-R.; Yoo, D.; Oh, D.-H. Microbial Etiology and Prevention of Dental Caries: Exploiting Natural Products to Inhibit Cariogenic Biofilms. Pathogens 2020, 9, 569. [Google Scholar] [CrossRef]
- Do Nascimento, C.; Pita, M.S.; de Souza Santos, E.; Monesi, N.; Pedrazzi, V.; de Albuquerque Junior, R.F.; Ribeiro, R.F. Microbiome of titanium and zirconia dental implants abutments. Dent. Mater. 2016, 32, 93–101. [Google Scholar] [CrossRef]
- Paolone, G.; Scolavino, S.; Gherlone, E.; Spagnuolo, G. Direct Esthetic Composite Restorations in Anterior Teeth: Managing Symmetry Strategies. Symmetry 2021, 13, 797. [Google Scholar] [CrossRef]
- Aminoroaya, A.; Esmaeely, N.R.; Nouri, K.S.; Panahi, P.; Das, O.; Ramakrishna, S. A Review of Dental Composites: Methods of Characterizations. ACS Biomater. Sci. Eng. 2020, 13, 3713–3744. [Google Scholar] [CrossRef]
- Yadav, R.; Lee, H.; Lee, J.H.; Singh, J.K.; Lee, H.H. A comprehensive review: Physical, mechanical, and tribological characterization of dental resin composite materials. Tribol. Int. 2023, 179, 108102. [Google Scholar] [CrossRef]
- Wang, X.; Cai, Q.; Zhang, X.; Wei, Y.; Xu, M.; Yang, X.; Ma, Q.; Cheng, Y.; Deng, X. Improved performance of Bis-GMA/TEGDMA dental composites by net-like structures formed from SiO2 nanofiber fillers. Mater. Sci. Eng. 2016, 59, 464–470. [Google Scholar] [CrossRef]
- Tian, M.; Gao, Y.; Liu, Y.; Liao, Y.; Hedin, N.E.; Fong, H. Fabrication and evaluation of Bis-GMA/TEGDMA dental resins/composites containing nano fibrillar silicate. Dent. Mater. 2008, 24, 235–243. [Google Scholar] [CrossRef]
- De Santis, R.; Gloria, A.; Maietta, S.; Martorelli, M.; De Luca, A.; Spagnuolo, G.; Riccitiello, F.; Rengo, S. Mechanical and Thermal Properties of Dental Composites Cured with CAD/CAM Assisted Solid-State Laser. Materials 2018, 11, 504. [Google Scholar] [CrossRef] [PubMed]
- Sila, P.C.; Porto-Neto, S.; Lizarelli, R.F.; Bagnato, V.S. Orthodontic brackets removal under shear and tensile bond strength resistance tests—A comparative test between light sources. Laser Phys Lett. 2007, 3, 220–226. [Google Scholar]
- Silva, E.H.; Albuquerque, R.C.; Lanza, L.D.; Vieira, G.C.; Peixoto, R.; Alvim, H.; Yoshida, M. Influence of different light sources on the conversion of composite resins. Indian J. Dent. Res. 2011, 22, 790–794. [Google Scholar] [CrossRef] [PubMed]
- García, A.H.; Lozano, M.A.M.; Vila, J.C.; Escribano, A.B.; Galve, P.F. Composite resins. A review of the materials and clinical indications. Med. Oral Patol. Oral Cir. Bucal. 2006, 11, 215–220. [Google Scholar]
- Van Landuyt, K.L.; Snauwaert, J.; De Muncka, J.; Peumansa, M.; Yoshidac, Y.; Poitevin, A.; Coutinho, E.; Suzuki, K.; Lambrechts, P.; Van Meerbeeka, B. Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials 2007, 28, 3757–3785. [Google Scholar] [CrossRef] [PubMed]
- Rüttermann, S.; Dluzhevskaya, I.; Großsteinbeck, C.; Raab, W.H.M.; Janda, R. Impact of replacing Bis-GMA and TEGDMA by other commercially available monomers on the properties of resin-based composites. Dent. Mater. 2010, 26, 353–359. [Google Scholar] [CrossRef]
- Domingo, C.; Arcís, R.W.; Osorio, E.; Osorio, R.; Fanovich, M.A.; Rodríguez-Clemente, R.; Toledano, M. Hydrolytic stability of experimental hydroxyapatite-filled dental composite materials. Dent. Mater. 2003, 19, 478–486. [Google Scholar] [CrossRef]
- Mirică, I.-C.; Furtos, G.; Bâldea, B.; Lucaciu, O.; Ilea, A.; Moldovan, M.; Câmpian, R.-S. Influence of Filler Loading on the Mechanical Properties of Flowable Resin Composites. Materials 2020, 13, 1477. [Google Scholar] [CrossRef]
- Chistyakov, E.M.; Kolpinskaya, N.; Posokhova, V.; Chuev, V. Dental Composition Modified with Aryloxyphosphazene Containing Carboxyl Groups. Polymers 2020, 12, 1176. [Google Scholar] [CrossRef]
- Karabela, M.M.; Sideridou, I.D. Synthesis and study of properties of dental resin composites with different nanosilica particles size. Dent. Mater. 2011, 27, 825–835. [Google Scholar] [CrossRef]
- Azmy, E.; Al-Kholy, M.R.Z.; Fattouh, M.; Kenawi, L.M.M.; Helal, M.A. Impact of nanoparticles additions on the strength of dental composite resin. Int. J. Biomater. 2022, 2022, 1165431. [Google Scholar] [CrossRef]
- Ghada, H.; Naguib, T.B.; Jumana, M.; Alaa, T.; Abdulghani, M.; Rabab, A.; Hamed, M. Noninvasive assessment of novel nanohybrid resin cement adaptation using cross-polarization optical coherence tomography. Dent. Mater. 2024, 40, 643–652. [Google Scholar]
- Hameed, H.K.; Abdul Rahman, H. The effect of addition nano particle ZrO2 on some properties of Autoclave Processed Heat cure acrylic denture base material. J. Baghdad Coll. Dent. 2015, 27, 32–39. [Google Scholar] [CrossRef]
- Yazi, W.; Meifang, Z. Functional fillers for dental resin composites. Acta Biomater. 2022, 122, 50–65. [Google Scholar] [CrossRef]
- Mirhashemi, A.; Bahador, A.; Sodagar, A.; Pourhajibagher, M.; Amiri, A.; Gholamrezayi, E. Evaluation of antimicrobial properties of nano-silver particles used in orthodontics fixed retainer composites: An experimental in-vitro study. J. Dent. Res. Dent. Clin. Dent. Prospect. 2021, 15, 87–93. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hanif, A.; Ghani, F. Mechanical properties of an experimental resin based composite containing silver nanoparticles and bioactive glass. Pak. J. Med. Sci. 2020, 36, 776–781. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dan-Lei, Y.; Ya-Nan, C.; Qian, S.; Mei, L.; Hao, N.; Jie-Xin, W. Antibacterial activity and reinforcing effect of SiO2–ZnO complex cluster fillers for dental resin composites. Biomater. Sci. 2021, 9, 1795–1804. [Google Scholar] [CrossRef]
- Şomoghi, R.; Semenescu, A.; Pasăre, V.; Chivu, O.R.; Nițoi, D.F.; Marcu, D.F.; Florea, B. The Impact of ZnO Nanofillers on the Mechanical and Anti-Corrosion Performances of Epoxy Composites. Polymers 2024, 16, 2054. [Google Scholar] [CrossRef]
- Demarco, F.F.; Correa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Longevity of posterior composite restorations: Not only a matter of materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef]
- Astvaldsdottir, A.; Dagerhamn, J.; van Dijken, J.W.; Naimi-Akbar, A.; Sandborgh-Englund, G.; Tranaeus, S.; Nilsson, M. Longevity of posterior resin composite restorations in adults—A systematic review. J. Dent. 2015, 43, 934–954. [Google Scholar] [CrossRef]
- Liu, Z.; Liang, H.; Shi, T.; Xie, D.; Chen, R.; Han, X.; Shen, L.; Wang, C.; Tian, Z. Additive manufacturing of hydroxyapatite bone scaffolds via digital light processing and in vitro compatibility. Ceram. Int. 2019, 45, 11079–11086. [Google Scholar] [CrossRef]
- Sousa, A.C.; Biscaia, S.; Alvites, R.; Branquinho, M.; Lopes, B.; Sousa, P.; Valente, J.; Franco, M.; Santos, J.D.; Mendonça, C.; et al. Assessment of 3D-Printed Polycaprolactone, Hydroxyapatite Nanoparticles and Diacrylate Poly(ethylene glycol) Scaffolds for Bone Regeneration. Pharmaceutics 2022, 14, 2643. [Google Scholar] [CrossRef] [PubMed]
- Klimek, L.; Kopacz, K.; Śmielak, B.; Kula, Z. An Evaluation of the Mechanical Properties of a Hybrid Composite Containing Hydroxyapatite. Materials 2023, 16, 4548. [Google Scholar] [CrossRef] [PubMed]
- Taheri, M.M. Fluoridated hydroxyapatite nanorods as novel fillers for improving mechanical properties of dental composite: Synthesis and application. Mater. Desing 2015, 82, 119–125. [Google Scholar] [CrossRef]
- EN ISO 4049; Dentistry–Polymer-Based Restorative Materials. ISO: Geneva, Switzerland, 2009.
- ASTM G133-05; Standard Test Method for Linearly Reciprocating Ball-on-Flat Sliding Wear. ISO: Geneva, Switzerland, 2010.
- PN-EN ISO 868; Plastics and Ebonite—Determination of Indentation Hardness by Means of a Durometer (Shore Hardness). ISO: Geneva, Switzerland, 2003.
- PN-EN ISO 604; Plastics—Determination of Compressive Properties 2002. ISO: Geneva, Switzerland, 2002.
- PN-EN ISO 179-2:2020-12; Plastics—Determination of Charpy Impact Properties. ISO: Geneva, Switzerland, 2020.
- ASTM D2240; Standard Test Method for Rubber Property—Durometer Hardness. ISO: Geneva, Switzerland, 2017.
- Banaszek, K.; Klimek, L. Ti(C, N) as Barrier. Coatings 2019, 9, 432. [Google Scholar] [CrossRef]
- Dziedzic, K.; Zubrzycka-Wróbel, J. Research on tribological properties of dental composite materials. Adv. Sci. Technol. Res. J. 2016, 10, 144–149. [Google Scholar] [CrossRef]
- Kula, Z.; Klimek, L.; Dąbrowska, K.; Neves, C.B.; Roque, J.C. Selected Mechanical Properties of Dental Hybrid Composite with Fluorine, Hydroxyapatite and Silver Fillers. J. Compos. Sci. 2024, 8, 232. [Google Scholar] [CrossRef]
- Kutbay, I.; Yilmaz, B.; Evis, Z.; Usta, M. Effect of calcium fluoride on mechanical behavior and sinterability of nano-hydroxyapatite and titania composites. Ceram. Int. 2014, 40, 14817–14826. [Google Scholar] [CrossRef]
- Seyedmajidi, S.; Seyedmajidi, M. Fluorapatite: A Review of Synthesis, Properties and Medical Applications vs. Hydroxyapatite. Iran. J. Mater. Sci. Eng. 2022, 19, 1–8. [Google Scholar]
- Tredwin, C.H.J.; Young, A.M.; Neel, E.A.A. Hydroxyapatite, fluor-hydroxyapatite and fluorapatite produced via the sol–gel method: Dissolution behaviour and biological properties after crystallization. J. Mater. Sci. Mater. Med. 2014, 25, 47–53. [Google Scholar] [CrossRef]
- Durner, J.; Stojanovic, M.; Urcan, E.; Hickel, R.; Reichl, F.X. Influence of silver nano-particles on monomer elution from light-cured composites. Dent. Mater. 2011, 27, 631–636. [Google Scholar] [CrossRef]
- Gryczynski, Z.; Lukomska, J.; Lakowicz, J.R.; Matveeva, E.G.; Gryczynski, I. Depolarized light scattering from silver nanoparticles. Chem. Phys. Lett. 2006, 421, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Chadda, H.; Satapathy, B.K.; Patnaik, A.; Ray, A.R. Mechanistic interpretations of fracture toughness and correlations to wear behavior of hydroxyapatite and silica/hydroxyapatite filled bis-GMA/TEGDMA micro/hybrid dental restorative composites. Compos. Part B Eng. 2017, 130, 132–146. [Google Scholar] [CrossRef]
- Kula, Z.; Klimek, L.; Kopacz, K.; Śmielak, B. Evaluation of the Effect of the Addition of Hydroxyapatite on Selected Mechanical and Tribological Properties of a Flow-Type Composite. Materials 2022, 15, 9016. [Google Scholar] [CrossRef] [PubMed]
- Sirait, M.; Sinulingga, K.; Siregar, N.; Doloksaribu, M.E. Characterization of hydroxyapatite by cytotoxicity test and bending test. J. Phys. Conf. Ser. 2022, 2193, 012039. [Google Scholar] [CrossRef]
- Annur, H.; Kaelani, Y. Pengujian Bending Biomaterial Hidroksiapatit dari Tulang Sapi sebagai Prosthesis Sendi Rahang (TMJ) pada Manusia. J. Tek. ITS 2015, 4, 37–40. [Google Scholar]
- Neves, C.B.; Costa, J.; Nepomuceno, L.; Madeira, A.; Portugal, J.; Bettencourt, A. Microhardness and Flexural Strength after Chemical Aging of chlorhexidine delivery systems based on acrylic resin. Rev. Port. Estomatol. Med. Dentária Cir. Maxilofac. 2019, 60, 104–110. [Google Scholar] [CrossRef]
- Costa, J.; Bettencourt, A.; Madeira, A.; Nepomuceno, L.; Portugal, J.; Neves, C.B. Surface Properties after Chemical Aging of chlorhexidine delivery systems based on acrylic resin. Rev. Port. Estomatologi. Med. Dentária Cir. Maxilofac. 2019, 60, 155–162. [Google Scholar] [CrossRef]
- Sajewicz, E. On evaluation of wear resistance of tooth enamel and dental materials. Wear 2006, 260, 1256. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).