Abstract
Background: Post-operative rehabilitation after total hip arthroplasty (THA) and total knee arthroplasty (TKA) is a crucial phase in the recovery process. The choice between clinic-based rehabilitation (CBR) and home-based rehabilitation (HBR) depends on the patient’s specific needs, available resources, and individual preferences. This study aimed to compare CBR and HBR in terms of short-term post-operative functionality in patients who underwent THA and TKA. Methods: A prospective matched cohort study was performed on 120 patients who underwent primary THA and TKA; 60 patients underwent HBR, and 60 underwent CBR. Data gathered included instrumental activities of daily living (IADLs), as well as visual analogue scale (VAS), Vail Hip Score (VHS), and Western Ontario and McMaster Universities (WOMAC) questionnaire results. Results: Statistically significant recovery was found in terms of VAS, VHS, and WOMAC in the HBR and CBR groups (all p < 0.001) after THA and TKA. Multivariate regression analysis demonstrated that higher values of VHS and WOMAC at 1 month were associated with better values of VAS, VHS, and WOMAC preoperatively (r = 0.095, p = 0.021). Conclusion: HBR showed similar short-term postoperative outcomes when compared with CBR for patients who underwent total joint arthroplasty. Greater preoperative joint functionality, a lower level of pain, and a female gender predicted better functional outcomes at 1 month after surgery in both groups.
1. Introduction
Total hip arthroplasty (THA) and total knee arthroplasty (TKA) are successful and safe surgical procedures for patients with end-stage hip and knee osteoarthritis to reduce pain, restore joint functionality, and improve quality of life [1,2]. In recent years, with the continuous advancement of surgical techniques and the shortening of hospitalization and rehabilitation times, the costs incurred after joint replacement surgery have decreased significantly [3]. Post-operative rehabilitation is a crucial phase in the recovery process [4], and is traditionally conducted in clinical settings, under the direct supervision of qualified healthcare professionals. However, alternatives are emerging, such as home-based rehabilitation (HBR) [5,6,7].
In the event of epidemic outbreaks, such as COVID-19, it may be difficult to seek clinic-based rehabilitation (CBR). During the pandemic period, the number of hip and knee replacement surgeries decreased by 76.5%, compared with the same period in 2019 (from 706 surgeries in 2019 to 166 in 2020) [8,9]; additionally, the challenge of identifying rehabilitation facilities capable of managing postoperative rehabilitation while ensuring patient safety led to the exploration of alternative solutions. Consequently, HBR has become a viable alternative. This method offers patients flexible rehabilitation options, eliminating the need for travel and personalized care. Furthermore, there has been remarkable progress in recent years in integrating digital smart devices with HBR [10]. Previous studies have confirmed the effectiveness and safety of HBR, demonstrating comparable improvements in pain, functional outcomes, activities of daily living, patient satisfaction, and cost-effectiveness [10,11]. Moreover, when considering the activities of daily living (ADLs), the home environment is deemed to be more meaningful to patients than an external clinical setting [12]. This could also enhance the feasibility of rehabilitation and significantly reduce costs for patients. It has also been suggested that this trend provides new opportunities and greater convenience in the field of rehabilitation, offering a more accessible range of rehabilitation options. However, it should be noted that HBR is not without challenges. The success of this type of treatment depends on the adherence of the patients to the prescribed physiotherapy program. In the case of older patients, a technological barrier often exists, necessitating supervision and assistance from the family network. No less important is variability in the quality of rehabilitation, attributable to the availability of resources and physiotherapists [10,13,14].
The choice between CBR and HBR depends on various factors, including the patient’s specific needs, the complexity of the surgical intervention, available resources, and individual preferences [5,7]. However, there are limited data concerning comparisons of these rehabilitation approaches when both are viable. The surgeon’s ability to correctly indicate the best post-operative rehabilitation path is therefore limited.
The aim of this study was to compare CBR and HBR in terms of short-term postoperative functionality in patients who underwent THA and TKA.
2. Materials and Methods
A prospective matched cohort study was performed involving collection of data on 130 consecutive patients who underwent primary THA and TKA for osteoarthritis (OA) between May 2023 and November 2023. The study protocol was approved by the local ethics committee, and the research was conducted in compliance with the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study. The inclusion criteria were (1) primary and elective THA and TKA for OA, (2) age older than 18 years at the time of surgery, (3) postoperative rehabilitation in CBR or HBR, and (4) participation in a minimum 1-month follow-up. The exclusion criteria were (1) revision THA and TKA, (2) THA and TKA performed for any diagnosis other than primary OA, (3) concomitant neurological and orthopedic diseases of the lower limbs, and (4) failure to understand or complete the questionnaires. Ten patients were excluded for different reasons; therefore, 120 of 130 patients, or 92.3%, were enrolled and evaluated (60 THA and 60 TKA) (Figure 1). Data gathered included the age and sex of the patients, as well as their side and body mass index (BMI).
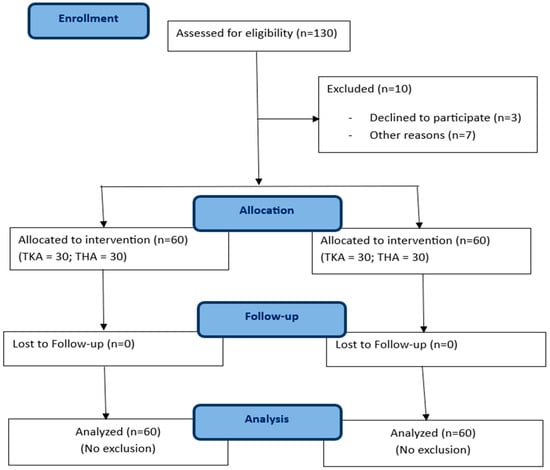
Figure 1.
Flow chart of patient selection.
2.1. Surgical Technique and Early Rehabilitation
All surgical procedures were performed by one surgeon (GC) with high levels of experience in hip and knee arthroplasty. For both THA and TKA, deep vein thrombosis (DVT) prophylaxis was carried out by the administration of low-molecular-weight heparin [15]. Antibiotic prophylaxis was administered intravenously as recommended [16]. In the absence of contraindications, either spinal or epidural anesthesia was performed for all procedures.
THA was performed using a modified Hardinge approach in the lateral decubitus position with a cementless, proximally coated, tapered stem with cementless, hemispherical acetabular fixation, a ceramic femoral head, and a polyethylene acetabular liner (Exacta® femoral stems and BIOLOX® delta acetabular component; Permedica S.p.A., Merata (LC), Italy; H-MAX S® femoral stems and Delta TT® acetabular component; Lima Corporate S.p.A., Udine (UD), Italy).
TKA was performed using a medial parapatellar approach [17] while the patient was in the supine position with a cemented implant (SymphoKnee® knee implant system; Waldemar Link GmbH Co., Hamburg, Germany).
An injectable nonsteroidal anti-inflammatory drug (diclofenac 75 mg every 12 h for 4 days), an oral opioid (Tapentadol 50 mg every 12 h for 3 days), and cryotherapy (Game Ready® system, 1 h twice a day for the first 5 days) were used in the absence of specific contraindications to improve post-operative pain and reduce the consumption of each agent [18]. In the first five days after surgery, during the hospitalization period, physiotherapy was started which included the following: exercises of dorsiflexion and plantarflexion of the ankle; passive extension of the knee using a rise under the calcaneus; isometric contractions of quadriceps, gluteus, and flexors of the ankle; abduction with a straight leg; flexion and extension of the knee, with or without the aid of a machine (Kinetec medical products Aldershot, UK); lifts with a straight leg; assisted active knee flexion while sitting on a bed; and thrice-daily cryotherapy. From the second day after surgery, the patient was also allowed to get out of bed with assistance and sit on a highchair. If there were no contraindications following the operation, the patient could start walking with an axillary walker and then with two crutches to tackle longer paths and climb stairs. Discharge from the hospital occurred five days post-surgery. The patients were informed of the two possible settings, i.e., CBR or HBR. They then decided independently where to continue the rehabilitation program. All patients in the two different groups performed the same types of exercises to avoid further bias.
2.2. Clinic-Based Rehabilitation
Following hospital discharge, a new admission to a rehabilitation clinic was arranged. All patients continued to perform the exercises that had been administered during the first five days post-surgery. As their condition improved, they continued with exercises as follows: flexion and extension of knee and hip; transfer of weight from one foot to another; balance exercises on the operated leg; elevation of the leg with a stretch strap; high squats; step on the step; muscle reinforcement and isometry with the fit ball of quadriceps, femoral biceps, adductors and abductors with elastics; training of the step; and stretching (quadriceps, hamstring, and calf stretch; heel slide stretch; glute bridge and seated hamstring stretch). All patients performed the same types of exercises without any type of contraindication, no other types of additional physical and instrumental treatment were performed. The patients practiced 1 h of physiotherapy a day for 20 days.
2.3. Home-Based Rehabilitation
Following discharge from the hospital, each patient returned to their home with a rehabilitation kit. This kit contained a USB stick with all exercises to perform, a fit ball, a high sliding top, a stretch strap, 2 kg gym weights, medical elastic bands, and an ice knee brace. The patient was also given self-assessment tests to be completed and sent to the physiotherapist daily. These included questions about the pain level according to the VAS scale, the presence of wound secretions, the presence of fever, general clinical conditions, and whether the patient had performed the scheduled physiotherapy program. The physiotherapist conducted an initial home visit to assess the setting, explain the exercises and check that they were executed correctly, and advise on how to send the daily report. The physiotherapist also assessed the patients’ execution of the exercises during home visits at 15 days and one month after surgery. The patients practiced exercises as follows: flexing and extension of knee and hip; transfer of weight from one foot to another; balance exercises on the operated leg; elevation of the leg with the stretch strap; high squats; step on the step; muscle reinforcement and isometry with the fit ball of quadriceps, femoral biceps, adductors and abductors with elastics; training of the step and stretching (quadriceps, hamstring, and calf stretch; heel slide stretch; glute bridge and seated hamstring stretch). The patients practiced 1 h of physiotherapy a day for 20 days.
2.4. Functional Assessment
Preoperatively (t0) each patient was evaluated with instrumental activities of daily living (IADLs) scales [19]. IADLs are used to measure the activities that allow an individual to live independently in a community, thereby improving quality of life. Lawton’s IADL Scale [19] is composed of 8 items, and assesses a person’s ability to perform tasks such as using a telephone or handling finances. Responses to each of the eight items in the scale are coded as 0 (unable or partially able) or 1 (able), and the responses are summed. The summary score ranges from 0 (low functioning, dependent) to 8 (high functioning, independent).
Preoperatively (t0), at hospital discharge (t1), at 15 days after surgery (t2), and at one month (t3) after surgery, each patient was evaluated with the visual analogue scale (VAS), while the Vail Hip Score (VHS) was used for patients who underwent THA, and the Western Ontario and McMaster Universities (WOMAC) questionnaire was used for patients who underwent TKA.
The VAS was used as a subjective measure of pain perception. A VAS score > 3 at the last follow-up indicated residual pain [20].
The VHS is a self-administrated sensitive scale. It includes 10 questions focused on pain, stiffness, gait, and function. The scale has a maximum of 100 points divided on the basis on the assessed items. Pain includes three questions with a total of 50 points; stiffness includes two questions with a total of 20 points; gait includes one question with a total of 5 points; and function includes four questions with a total of 25 points [21]
The WOMAC questionnaire is a self-administered disease-specific validated outcome measure; this was used to assess pain (5 items), stiffness (2 items), and physical function disability (17 items) in patients suffering from knee osteoarthritis [22]. The WOMAC questionnaire provides either single domain scores or a total score (0–100); lower scores are associated with lower levels of pain and stiffness and better function.
Patient satisfaction was assessed, and patients were asked if they would undergo the same type of surgery again.
2.5. Statistical Analysis
All data were measured, collected, and reported to an accuracy of one decimal place. Values for mean, standard deviation, and range were noted for the continuous variables; for the categorical variables, counts were recorded. The distribution of the numeric samples was assessed by the Kolmogorov–Smirnov normality test. Based on this preliminary analysis, parametric tests were adopted. To evaluate the significance of differences between preoperative and postoperative values and between the groups, two-tailed paired- and unpaired-sample Student’s t-tests were performed. Univariate and multivariate linear regression was performed on the whole population to test possible outcome predictors. The explanatory and confounding preoperative and postoperative variables included in the analysis were sex (categorical), age (continuous), VAS (continuous), IADLs (continuous), VHS (continuous), and WOMAC (continuous). The postoperative functional score (a continuous variable) was treated as an outcome of the variables. Only explanatory and confounding variables that showed a trend toward an association (e.g., p < 0.10) with the outcome of interest in the univariate analysis were included in the multiple regression analysis. Post hoc power was calculated by considering the sample size, the observed effect size, and an α-value of 0.05; a post hoc power greater than 80% was considered appropriate.
IBM SPSS Statistics software (version 26, IBM Corp., Armonk, NY, USA) and G*Power (version 3.1.9.2, Institut für Experimentelle Psychologie, Heinrich Heine Universität, Düsseldorf, Germany) were used for database construction and statistical analysis. A p-value of less than 0.05 was considered significant.
3. Results
Sixty (50%) patients underwent THA, of whom 30 (50%) and 30 (50%) underwent CBR and HBR, respectively. Adherence to, and compliance with HBR and CBR was checked with the physiotherapist during the study, and found to be 100%. The characteristics of the study population are summarized in Table 1.

Table 1.
Characteristics of the patients.
Overall, numbers of female patients were 38 (63.3%) and 41 (68.3%) in the THA and TKA groups, respectively, and overall mean age was 70.7 ± 8.8 and 68.9 ± 8.7 years in the TKA and THA groups, respectively.
Table 2 presents functional outcomes at t3, as well as complications and minimum clinically important differences (MCIDs). The significance of differences between preoperative and postoperative values and between the groups, was assessed using two-tailed paired- and unpaired-sample Student’s t-tests.

Table 2.
Outcomes of HBR and CBR groups.
Table 3 shows the differences among IADL, VAS, and VHS scores at t0, t1, t2, and t3 in the HBR and CBR groups for patients who underwent THA. The comparisons between the scores were performed using paired t-tests, with a p-value less than 0.05 being considered significant. A statistically significant recovery was found in terms of VAS and VHS in the HBR and CBR groups (all p < 0.001). No differences were found at t0 and t3 between the HBR and CBR groups in terms of IADLs, VAS, and VHS.

Table 3.
Functional scores of patients who underwent total hip arthroplasty.
Table 4 shows the differences among IADL, VAS, and WOMAC scores at t0, t1, t2, and t3 in the HBR and CBR groups for patients who underwent TKA. Comparisons between scores were obtained using paired t-tests, with p-values lower than 0.05 being considered significant. A statistically significant recovery was found in terms of VAS and WOMAC in the HBR and CBR groups (all p < 0.001). No differences were found at t0 and t3 between HBR and CBR groups in terms of IADLs, VAS, and WOMAC.

Table 4.
Functional scores of patients who underwent total knee arthroplasty.
Changes with surgery were compared with MCIDs. For reference values of MCID, previously published data for each outcome were used: VAS MCID = 2.9 [23]; WOMAC MCID = 10 [24]; and VHS = 10 [25]. All patients were beyond the MCID in all cases. Patient satisfaction was assessed, with 100% of the patients declaring that they were satisfied and would undergo the same operation again. The univariate regression analysis for the patients who underwent THA demonstrated that VAS and VHS at t0 was associated with better functional outcomes at 1 month after surgery.
Table 5 shows these results.

Table 5.
Univariate Regression analysis: factors affecting postoperative Vail Hip Score.
The multivariate regression analysis demonstrated that higher values of VHS at t3 were associated with better values of VAS and VHS at t0 (r = 0.095, p = 0.021).
The univariate regression analysis for patients who underwent TKA shows that female gender and WOMAC at t0 were associated with better functional outcomes at t3. Table 6 shows the results.

Table 6.
Univariate Regression analysis: Factors Affecting Postoperative WOMAC Score.
The multivariate regression analysis demonstrated that a better value of the WOMAC score at t3 was associated with the female gender and a better value of the WOMAC score at t0 (r = 0.319, p < 0.001).
Complications
A total of three patients reported complications. Two patients in the TKA group had surgical wound dehiscence; one of these was in the HBR group and the other in the CBR group. One patient in the TKA-CBR group had a capsule rupture.
4. Discussion
The aim of this study was to compare CBR and HBR in terms of short-term postoperative functionality in patients who underwent THA and TKA. The most important finding of the present study was that no differences were found between HBR and CBR for patients who underwent TKA and THA in terms of functional outcomes and pain. A greater preoperative joint functionality, a lower level of pain, and a female gender predicted higher functional outcomes at 1 month after surgery in both groups.
TKA and THA are the most common procedures for knee and hip osteoarthritis, but few studies have compared outcomes based on the type of post-operative rehabilitation (i.e., HBR or CBR). In detail, HBR and CBR differ in methodology, treatment adherence, and economic aspects (REFs). Our study suggests that both HBR and CBR achieve comparable functional outcomes and pain control. This result is similar to that of a meta-analysis by Zhang et al. [10], who reported that long-term pain and functional outcomes were comparable in patients who underwent TKA, but found that ROM was superior in the HBR group at 14 weeks. Similarly, a study by Lopez-Liria et al. [26], who analyzed patients who underwent TKA, demonstrated that results were comparable between the HBR and CBR groups. Osterloh et al. [27] analyzed 26 patients who underwent TKA and THA, and found that WOMAC and VAS were comparable for digital-assisted rehabilitation, compared with the control group; they also found positive effects on quality of life, stiffness, and physical function in the digital-assisted group. A study by Eichler et al. [28] reported results similar to ours, with a follow-up of 3 months. Several studies [29,30,31,32,33] have found comparable results for HBR and CBR using validated outcome scores at short- and long-term follow-up. In general, HBR is an adequate solution for autonomous patients; using this approach, it is possible to gain more control over pain and functionality, as well as the timing and duration of therapy [26]. Other authors [34] have analyzed pain using data extracted from WOMAC and VAS scores, suggesting that HBR can be as effective as CBR in terms of pain control in the short term. A study by Wang et al. concurred with our results, finding that at 6 and 10 weeks postoperatively patients who performed HBR reported positive effects on pain and functional outcomes [35].
In our multivariate regression analysis, we found that better WOMAC scores at t3 were associated with female gender and better values of WOMAC at t0. Significant differences between women and men with regard to postoperative outcomes have been reported in the literature; generally, women report worse scores on pain and functional outcomes, and they also show lower quadriceps muscle strength before surgery in comparison with men. Postoperatively, women tend to recover better and faster than men. These results are probably due to increased motivation as well as differences in pain perception and preoperative expectations [36,37,38]. Regarding THA, the multivariate regression indicated that patients with better values of VAS and VHS preoperatively had better VHS at t3. These results, as indicated by the literature, suggest that patients with greater preoperative pain experience an improvement in pain after surgery but functional status may not improve the quality of patients with lower preoperative pain [39]. Considering HBR, there is greater concern regarding adherence to exercise prescription, compared with CBR. In this regard, Ettinger et al. [40] found a strong association between adherence and exercise and functional outcomes. HBR requires specific assessment, and it is also important to have a network of primary-care and home-care programs that can establish the entire program; there may be some initial difficulties, but HBR patients have reported higher levels of satisfaction [30]. Moreover, Mithcell et al. [33] reported that HBR patients would prefer any future therapy to be home-based because they had a positive experience with this type of therapy program. In our study, patients reported 100% adherence to the rehabilitation protocol carried out at home. The daily report was effective in providing feedback on the patient; this included both the general conditions and the execution of the scheduled program. The report was enabled patients to understand if they were improving, and the visits of the physiotherapist, at 15 days and a month after surgery, allowed any improvement to be evaluated. The telephone report was effective in monitoring the patient, both in requesting protocol explanations and in clinical monitoring. In this context, a study by Szöts et al. [41] reported that telephone follow-up increased short-term self-efficacy and also required fewer follow-up visits.
We also reported the complications that occurred in the short-term follow-up. A surgical wound problem was reported by single patients in both the HBR and CBR groups. The patient who underwent HBR was referred to the surgeon who performed TKA; this surgeon then performed an ultrasound aspiration of the joint fluid which was analyzed for a microbiological assessment. Following the negativity of the analysis, the patient carried out medical therapy and used taping. Differently, in the case of the patient in the CBR group with a similar wound complication, the ultrasound was performed without the removal of liquid, and empirical, broad-spectrum antibiotic therapy was administered according to the physician of the clinic. After one month, the patient was referred to the surgeon who suspended the antibiotic therapy. After one week this surgeon performed a collection of joint fluid that proved negative for bacterial growth. Some authors advocate that CBR can lead to an earlier detection of adverse events in the early postoperative period, while others suggest that patients who are referred to the surgeon should better follow the guidelines than those referred to general doctor without experience in the field.
Studies in the literature [11,42] involving comparisons in terms of adverse reactions have reported no statistically significant differences between the two groups. Lebleu et al. [43] conducted a study on 87 patients who were monitored telematically via an app during rehabilitation after TKA. This app sends an alert to a clinician when the patients answer the daily questions. Interestingly, 85% of the alerts sent by the patient were managed in telemedicine, avoiding consultations; the authors suggested that the overall low complication rate was due to the rapid dispatch of the alert. Moreover, immediate medical responses through the app may have been a factor in preventing more serious complications. In our study, the patients sent a daily report on their physical condition to the physiotherapist; if the answers in the report showed alerts or a worsening of clinical condition, the patient was recalled for a check and referred to the orthopedic surgeon if necessary. In our study, these adverse events were not related to the type of physiotherapy program performed but they did allow us to assess the benefit of daily monitoring, enabling an immediate response and intervention. These results highlighted the potential benefits of implementing direct contact to simplify communication between patients and surgeons, especially in the HBR context. In the future, the increased use of mobile devices and AI in daily life may help to improve adherence to HBR after surgery. Physicians can leverage these devices to supervise patients’ exercise effectively, while patients can provide timely feedback to their physicians on the effectiveness of their treatment when they are far away or find it inconvenient to come to the hospital [10]. Moreover, AI tools can also be used to detect surgical wound problems through telemedicine [44]. Indeed, a review [45] demonstrated that telemedicine is an alternative for post-operative follow-up care that can identify surgical site infections with an accuracy of 70–100%.
The socio-economic burden aspect of rehabilitation is no less important. In current study, the average cost of HBR was EUR 800, compared with the approximately EUR 250 daily average of the CBR. A meta-analysis by Zhao et al. [11] reported that the social cost of HBR was lower than that of CBR, with a cost-effectiveness advantage of about 43%. These data can also be reported in different health systems, suggesting a cost saving when using HBR rather than CBR. In our study, a comparison between HBR and CBR in terms of direct costs was not possible. It should also be considered that the costs associated with the health care provided by the physiotherapist and surgeon, the technology used, and daily living were not the aim of the study and were not investigated in depth; however, it would be useful to evaluate such costs in future studies, as this would further support the greater effectiveness of HBR over CBR.
Our study allowed us to evaluate functional outcomes and pain in the short term, and thus enabled an immediate response on the effectiveness of the therapy by the patient. Our study also allowed assessment of the effectiveness of a timely response in case of complications. However, this study has several limitations. First, the sample size was limited, and the results reported were obtained at a short-term follow-up (1 month). Second, the patient allocation was decided by the patient himself, based on economic possibilities and the possibility of the presence of a caregiver. Third, any statistical differences relating to times of execution or exercise sessions between the two groups were not assessed. Fourth, we excluded cases with neurological disorders and orthopedic diseases of the lower limbs, and clinical scores were not considered to evaluate bone quality or mental status [46,47]. These conditions may be present in other patients and may affect their postoperative outcomes; moreover, these factors could influence the decision for treatment and rehabilitation in addition to having already been associated with impaired functional recovery after various orthopedic procedures [48,49]. Fifth, we did not analyze any functional assessment or range of motion that could be more useful in a long-term study.
In conclusion, we found that there were no differences between HBR and CBR for patients who underwent TKA and THA in terms of functional outcomes and pain at 1 month after surgery. Greater preoperative joint functionality, a lower level of pain, and a female gender all predicted greater functional outcomes at 1 month after surgery in both groups. HBR is therefore confirmed as a valid option. In addition, it also seems more affordable than traditional CBR. Further studies with larger numbers of patients, longer follow-up times, and direct cost evaluations are required to confirm these findings and help to confirm the validity of HBR as a replacement of CBR in terms of compliance, functional outcomes, complications, and economic burden.
5. Conclusions
Home-based rehabilitation showed similar short-term postoperative outcomes when compared with traditional clinic-based rehabilitation for patients who underwent total joint arthroplasty. Greater preoperative joint functionality, a lower level of pain, and a female gender predicted better functional outcomes in both groups. In the future, a rehabilitation protocol in a comfort contest would be recommended for patients who do not need hospital care, satisfying individual needs and ensuring savings in economic and social terms.
Author Contributions
Conceptualization: F.F. and G.C.; methodology: G.C., T.M. and E.C.; software, M.M., A.G. and E.C.; validation, M.M. and F.F.; formal analysis, E.C.; investigation, E.C., G.C. and A.V.; data curation, E.C.; writing—original draft preparation, E.C.; writing—review and editing, M.M. and E.C.; visualization, F.F.; supervision, G.G. and F.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Mater Domini Ethics Committee No. 14/2015.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study, and written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Mercurio, M.; Gasparini, G.; Sanzo, V.; Familiari, F.; Castioni, D.; Galasso, O. Cemented Total Knee Arthroplasty Shows Less Blood Loss but a Higher Rate of Aseptic Loosening Compared with Cementless Fixation: An Updated Meta-Analysis of Comparative Studies. J. Arthroplast. 2022, 37, 1879–1887.e4. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.W.P.; Ng, S.W.L.; Chen, J.Y.; Liow, M.H.L.; Lo, N.N.; Yeo, S.J. Long-Term Functional Outcomes and Quality of Life at Minimum 10-Year Follow-Up After Fixed-Bearing Unicompartmental Knee Arthroplasty and Total Knee Arthroplasty for Isolated Medial Compartment Osteoarthritis. J. Arthroplast. 2021, 36, 1269–1276. [Google Scholar] [CrossRef]
- Pamilo, K.J.; Torkki, P.; Peltola, M.; Pesola, M.; Remes, V.; Paloneva, J. Fast-Tracking for Total Knee Replacement Reduces Use of Institutional Care without Compromising Quality. Acta Orthop. 2018, 89, 184–189. [Google Scholar] [CrossRef]
- Jones, C.A.; Beaupre, L.A.; Johnston, D.W.C.; Suarez-Almazor, M.E. Total Joint Arthroplasties: Current Concepts of Patient Outcomes after Surgery. Rheum. Dis. Clin. N. Am. 2007, 33, 71–86. [Google Scholar] [CrossRef]
- Familiari, F.; Mercurio, M.; Napoleone, F.; Galasso, O.; Giuzio, E.; Simonetta, R.; Palco, M.; DePhillipo, N.N.; Gasparini, G. Anterior Referencing versus Posterior Referencing in Primary Total Knee Arthroplasty: A Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2023, 12, 7453. [Google Scholar] [CrossRef] [PubMed]
- López-Liria, R.; Padilla-Góngora, D.; Catalan-Matamoros, D.; Rocamora-Pérez, P.; Pérez-de La Cruz, S.; Fernández-Sánchez, M. Home-Based versus Hospital-Based Rehabilitation Program after Total Knee Replacement. BioMed Res. Int. 2015, 2015, 450421. [Google Scholar] [CrossRef] [PubMed]
- Mercurio, M.; Gasparini, G.; Carbone, E.A.; Galasso, O.; Segura-Garcia, C. Personality Traits Predict Residual Pain after Total Hip and Knee Arthroplasty. Int. Orthop. 2020, 44, 1263–1270. [Google Scholar] [CrossRef]
- Benedetta Report Annuale Riap 2019 e Compendio. Available online: https://riap.iss.it/riap/it/attivita/report/2020/10/19/report-riap-2019/ (accessed on 3 April 2025).
- D’Apolito, R.; Faraldi, M.; Ottaiano, I.; Zagra, L. Disruption of Arthroplasty Practice in an Orthopedic Center in Northern Italy During the Coronavirus Disease 2019 Pandemic. J. Arthroplast. 2020, 35, S6–S9. [Google Scholar] [CrossRef]
- Zhang, H.; Wang, J.; Jiang, Z.; Deng, T.; Li, K.; Nie, Y. Home-Based Tele-Rehabilitation versus Hospital-Based Outpatient Rehabilitation for Pain and Function after Initial Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. Medicine 2023, 102, e36764. [Google Scholar] [CrossRef]
- Zhao, B.; Liu, H.; Du, K.; Zhou, W.; Li, Y. Effectiveness and Safety of Outpatient Rehabilitation versus Home-Based Rehabilitation after Knee Arthroplasty: A Systematic Review and Meta-Analysis. J. Orthop. Surg. 2023, 18, 704. [Google Scholar] [CrossRef]
- Doig, E.; Fleming, J.; Cornwell, P.L.; Kuipers, P. Qualitative Exploration of a Client-Centered, Goal-Directed Approach to Community-Based Occupational Therapy for Adults with Traumatic Brain Injury. Am. J. Occup. Ther. 2009, 63, 559–568. [Google Scholar] [CrossRef]
- Windsor, E.N.; Sharma, A.K.; Gkiatas, I.; Elbuluk, A.M.; Sculco, P.K.; Vigdorchik, J.M. An Overview of Telehealth in Total Joint Arthroplasty. HSS J. 2021, 17, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Leemrijse, C.J.; de Boer, M.E.; van den Ende, C.H.M.; Ribbe, M.W.; Dekker, J. Factors Associated with Physiotherapy Provision in a Population of Elderly Nursing Home Residents; a Cross Sectional Study. BMC Geriatr. 2007, 7, 7. [Google Scholar] [CrossRef] [PubMed]
- Falck-Ytter, Y.; Francis, C.W.; Johanson, N.A.; Curley, C.; Dahl, O.E.; Schulman, S.; Ortel, T.L.; Pauker, S.G.; Colwell, C.W. Prevention of VTE in Orthopedic Surgery Patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th Ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012, 141, e278S–e325S. [Google Scholar] [CrossRef] [PubMed]
- Fillingham, Y.A.; Della Valle, C.J.; Suleiman, L.I.; Springer, B.D.; Gehrke, T.; Bini, S.A.; Segreti, J.; Chen, A.F.; Goswami, K.; Tan, T.L.; et al. Definition of Successful Infection Management and Guidelines for Reporting of Outcomes After Surgical Treatment of Periprosthetic Joint Infection: From the Workgroup of the Musculoskeletal Infection Society (MSIS). J. Bone Jt. Surg. Am. 2019, 101, e69. [Google Scholar] [CrossRef]
- Mercurio, M.; Gasparini, G.; Galasso, O.; Familiari, F.; Cofano, E.; Sanzo, V.; Ciolli, G.; Corona, K.; Cerciello, S. Lateral versus Medial Approach for Total Knee Arthroplasty for Valgus Knee Deformity Shows Comparable Functional Outcomes, Hip–Knee–Ankle Angle Values, and Complication Rates: A Meta-Analysis of Comparative Studies. Arch. Orthop. Trauma Surg. 2023, 144, 869–878. [Google Scholar] [CrossRef]
- Castioni, D.; Galasso, O.; Iannò, B.; Mercurio, M.; Gasparini, G. Posterior versus Lateral Surgical Approach: Functionality and Quality of Life after Total Hip Arthroplasty in a Matched Cohort Study. BMC Musculoskelet. Disord. 2021, 22, 932. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontol. 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Erlenwein, J.; Müller, M.; Falla, D.; Przemeck, M.; Pfingsten, M.; Budde, S.; Quintel, M.; Petzke, F. Clinical Relevance of Persistent Postoperative Pain after Total Hip Replacement—A Prospective Observational Cohort Study. J. Pain Res. 2017, 10, 2183–2193. [Google Scholar] [CrossRef]
- Wahoff, M.; Dischiavi, S.; Hodge, J.; Pharez, J.D. Rehabilitation after Labral Repair and Femoroacetabular Decompression: Criteria-Based Progression through the Return to Sport Phase. Int. J. Sports Phys. Ther. 2014, 9, 813–826. [Google Scholar]
- Salaffi, F.; Leardini, G.; Canesi, B.; Mannoni, A.; Fioravanti, A.; Caporali, R.; Lapadula, G.; Punzi, L.; GOnorthrosis and Quality Of Life Assessment (GOQOLA). Reliability and Validity of the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index in Italian Patients with Osteoarthritis of the Knee. Osteoarthr. Cartil. 2003, 11, 551–560. [Google Scholar] [CrossRef] [PubMed]
- Danoff, J.R.; Goel, R.; Sutton, R.; Maltenfort, M.G.; Austin, M.S. How Much Pain Is Significant? Defining the Minimal Clinically Important Difference for the Visual Analog Scale for Pain After Total Joint Arthroplasty. J. Arthroplast. 2018, 33, S71–S75.e2. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Maffulli, N.; Schäfer, L.; Simeone, F.; Bell, A.; Hofmann, U.K. Minimal Clinically Important Difference (MCID), Substantial Clinical Benefit (SCB), and Patient-Acceptable Symptom State (PASS) in Patients Who Have Undergone Total Knee Arthroplasty: A Systematic Review. Knee Surg. Relat. Res. 2024, 36, 3. [Google Scholar] [CrossRef]
- Achten, J.; Parsons, N.R.; Edlin, R.P.; Griffin, D.R.; Costa, M.L. A Randomised Controlled Trial of Total Hip Arthroplasty versus Resurfacing Arthroplasty in the Treatment of Young Patients with Arthritis of the Hip Joint. BMC Musculoskelet. Disord. 2010, 11, 8. [Google Scholar] [CrossRef] [PubMed]
- Lopez, H.L. Nutritional Interventions to Prevent and Treat Osteoarthritis. Part II: Focus on Micronutrients and Supportive Nutraceuticals. PM R 2012, 4, S155–S168. [Google Scholar] [CrossRef]
- Osterloh, J.; Knaack, F.; Bader, R.; Behrens, M.; Peschers, J.; Nawrath, L.; Bergschmidt, P.; Darowski, M. The Effect of a Digital-Assisted Group Rehabilitation on Clinical and Functional Outcomes after Total Hip and Knee Arthroplasty—A Prospective Randomized Controlled Pilot Study. BMC Musculoskelet. Disord. 2023, 24, 190. [Google Scholar] [CrossRef]
- Eichler, S.; Salzwedel, A.; Rabe, S.; Mueller, S.; Mayer, F.; Wochatz, M.; Hadzic, M.; John, M.; Wegscheider, K.; Völler, H. The Effectiveness of Telerehabilitation as a Supplement to Rehabilitation in Patients after Total Knee or Hip Replacement: Randomized Controlled Trial. JMIR Rehabil. Assist. Technol. 2019, 6, e14236. [Google Scholar] [CrossRef]
- Barker, K.L.; Room, J.; Knight, R.; Dutton, S.; Toye, F.; Leal, J.; Kenealy, N.; Maia Schlüssel, M.; Collins, G.; Beard, D.; et al. Home-Based Rehabilitation Programme Compared with Traditional Physiotherapy for Patients at Risk of Poor Outcome after Knee Arthroplasty: The CORKA Randomised Controlled Trial. BMJ Open 2021, 11, e052598. [Google Scholar] [CrossRef]
- Buhagiar, M.A.; Naylor, J.M.; Harris, I.A.; Xuan, W.; Kohler, F.; Wright, R.; Fortunato, R. Effect of Inpatient Rehabilitation vs a Monitored Home-Based Program on Mobility in Patients with Total Knee Arthroplasty: The HIHO Randomized Clinical Trial. JAMA 2017, 317, 1037–1046. [Google Scholar] [CrossRef]
- Kauppila, A.-M.; Kyllönen, E.; Ohtonen, P.; Hämäläinen, M.; Mikkonen, P.; Laine, V.; Siira, P.; Mäki-Heikkilä, P.; Sintonen, H.; Leppilahti, J.; et al. Multidisciplinary Rehabilitation after Primary Total Knee Arthroplasty: A Randomized Controlled Study of Its Effects on Functional Capacity and Quality of Life. Clin. Rehabil. 2010, 24, 398–411. [Google Scholar] [CrossRef]
- Mahomed, N.N.; Davis, A.M.; Hawker, G.; Badley, E.; Davey, J.R.; Syed, K.A.; Coyte, P.C.; Gandhi, R.; Wright, J.G. Inpatient Compared with Home-Based Rehabilitation Following Primary Unilateral Total Hip or Knee Replacement: A Randomized Controlled Trial. J. Bone Jt. Surg. Am. 2008, 90, 1673–1680. [Google Scholar] [CrossRef]
- Mitchell, C.; Walker, J.; Walters, S.; Morgan, A.B.; Binns, T.; Mathers, N. Costs and Effectiveness of Pre- and Post-Operative Home Physiotherapy for Total Knee Replacement: Randomized Controlled Trial. J. Eval. Clin. Pract. 2005, 11, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Yang, Z.; Kang, P.; Xie, X. Home-Based Compared with Hospital-Based Rehabilitation Program for Patients Undergoing Total Knee Arthroplasty for Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Am. J. Phys. Med. Rehabil. 2017, 96, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Hunter, S.; Lee, R.L.-T.; Chan, S.W.-C. The Effectiveness of a Mobile Application-Based Programme for Rehabilitation after Total Hip or Knee Arthroplasty: A Randomised Controlled Trial. Int. J. Nurs. Stud. 2023, 140, 104455. [Google Scholar] [CrossRef]
- Koenen, P.; Bäthis, H.; Schneider, M.M.; Fröhlich, M.; Bouillon, B.; Shafizadeh, S. How Do We Face Patients’ Expectations in Joint Arthroplasty? Arch. Orthop. Trauma Surg. 2014, 134, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Moretti, B.; Spinarelli, A.; Varrassi, G.; Massari, L.; Gigante, A.; Iolascon, G.; Benedetti, M.G.; Moretti, A.M. Influence of Sex and Gender on the Management of Late-Stage Knee Osteoarthritis. Musculoskelet. Surg. 2022, 106, 457–467. [Google Scholar] [CrossRef]
- Volkmann, E.R.; FitzGerald, J.D. Reducing Gender Disparities in Post-Total Knee Arthroplasty Expectations through a Decision Aid. BMC Musculoskelet. Disord. 2015, 16, 16. [Google Scholar] [CrossRef]
- Fortin, P.R.; Clarke, A.E.; Joseph, L.; Liang, M.H.; Tanzer, M.; Ferland, D.; Phillips, C.; Partridge, A.J.; Bélisle, P.; Fossel, A.H.; et al. Outcomes of Total Hip and Knee Replacement: Preoperative Functional Status Predicts Outcomes at Six Months after Surgery. Arthritis Rheum. 1999, 42, 1722–1728. [Google Scholar] [CrossRef]
- Ettinger, W.H.; Burns, R.; Messier, S.P.; Applegate, W.; Rejeski, W.J.; Morgan, T.; Shumaker, S.; Berry, M.J.; O’Toole, M.; Monu, J.; et al. A Randomized Trial Comparing Aerobic Exercise and Resistance Exercise with a Health Education Program in Older Adults with Knee Osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). JAMA 1997, 277, 25–31. [Google Scholar] [CrossRef]
- Szöts, K.; Konradsen, H.; Solgaard, S.; Østergaard, B. Telephone Follow-Up by Nurse After Total Knee Arthroplasty: Results of a Randomized Clinical Trial. Orthop. Nurs. 2016, 35, 411–420. [Google Scholar] [CrossRef]
- Issa, K.; Kurowicki, J.; Novack, T.A.; Pierce, T.P.; Festa, A.; Scillia, A.J.; McInerney, V.K. Factors Complicating Discharge to Home Following Total Knee Arthroplasty—A Single Institution Initiative. J. Knee Surg. 2021, 34, 644–647. [Google Scholar] [CrossRef] [PubMed]
- Lebleu, J.; Pauwels, A.; Anract, P.; Parratte, S.; Van Overschelde, P.; Van Onsem, S. Digital Rehabilitation after Knee Arthroplasty: A Multi-Center Prospective Longitudinal Cohort Study. J. Pers. Med. 2023, 13, 824. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-Y.; Cao, M.-Q.; Xu, T.-Y. Progress in the Application of Artificial Intelligence in Skin Wound Assessment and Prediction of Healing Time. Am. J. Transl. Res. 2024, 16, 2765. [Google Scholar] [CrossRef] [PubMed]
- Ng, H.J.H.; Huang, D.; Rajaratnam, V. Diagnosing Surgical Site Infections Using Telemedicine: A Systematic Review. Surgeon 2022, 20, e78–e85. [Google Scholar] [CrossRef] [PubMed]
- Mercurio, M.; Familiari, F.; de Filippis, R.; Varano, C.; Napoleone, F.; Galasso, O.; Gasparini, G. Improvement in Health Status and Quality of Life in Patients with Osteoporosis Treated with Denosumab: Results at a Mean Follow-up of Six Years. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 16–23. [Google Scholar] [CrossRef]
- Mercurio, M.; de Filippis, R.; Spina, G.; De Fazio, P.; Segura-Garcia, C.; Galasso, O.; Gasparini, G. The Use of Antidepressants Is Linked to Bone Loss: A Systematic Review and Metanalysis. Orthop. Rev. 2022, 14, 38564. [Google Scholar] [CrossRef]
- de Filippis, R.; Mercurio, M.; Segura-Garcia, C.; De Fazio, P.; Gasparini, G.; Galasso, O. Defining the Minimum Clinically Important Difference (MCID) in the Hospital Anxiety and Depression Scale (HADS) in Patients Undergoing Total Hip and Knee Arthroplasty. Orthop. Traumatol. Surg. Res. OTSR 2024, 110, 103689. [Google Scholar] [CrossRef]
- Mercurio, M.; Castioni, D.; De Filippis, R.; De Fazio, P.; Familiari, F.; Gasparini, G.; Galasso, O. Postoperative Psychological Factors and Quality of Life but Not Shoulder Brace Adherence Affect Clinical Outcomes after Arthroscopic Rotator Cuff Repair. J. Shoulder Elb. Surg. 2023, 32, 1953–1959. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).