Radiological Healing Patterns and Functional Outcomes After Conservative Treatment of Unilateral Condylar Fractures: A Report of Two Cases
Abstract
1. Introduction
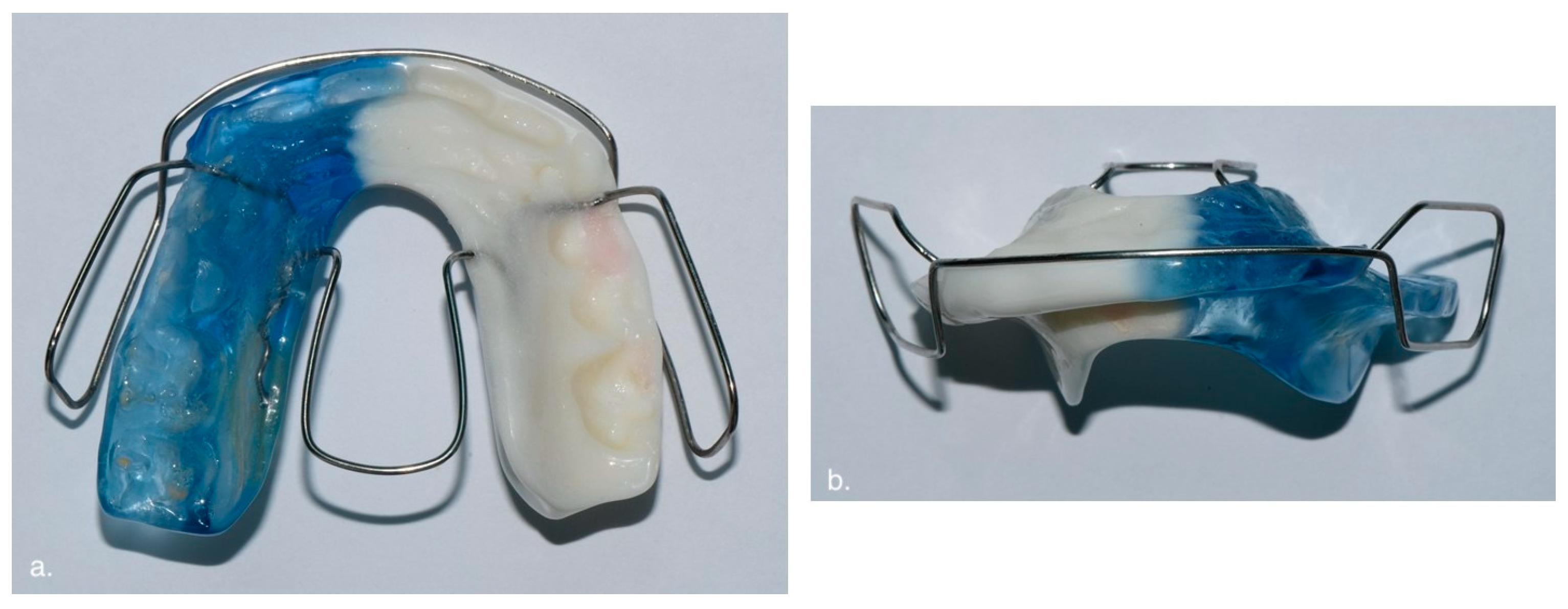
2. Materials and Methods
2.1. Participants
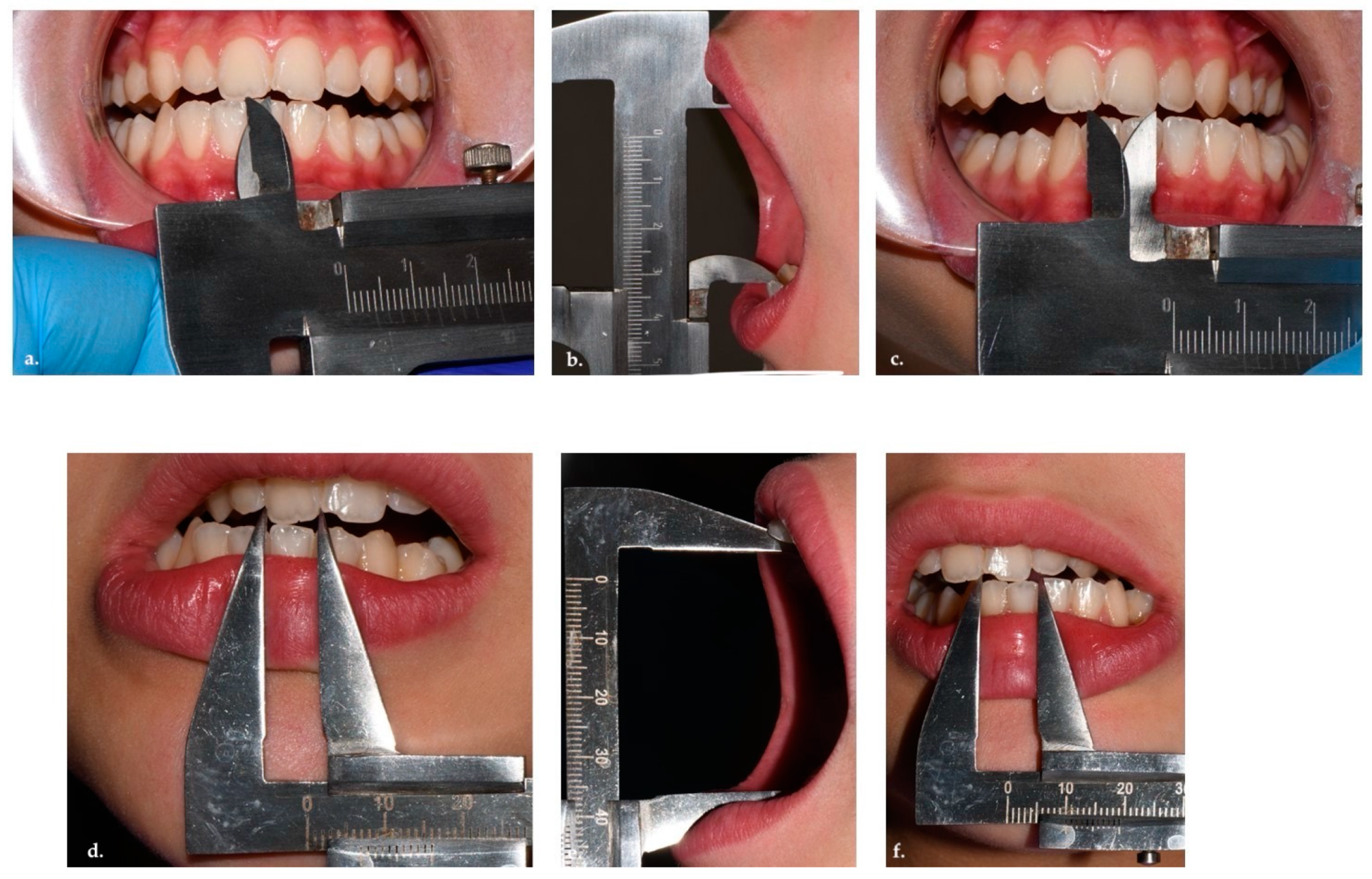
2.2. Clinical Evaluation
2.3. Functional Evaluation
- Maximum mouth opening (MMO);
- Temporomandibular joint (TMJ) functional activity (lateral excursion movements);
- Midline deviation (MD);
- Presence/absence of articular noise (clicking, popping, crepitus);
- Presence/absence of algic symptoms.
2.4. Radiological Evaluation and Measurements
2.4.1. CBCT Segmentation
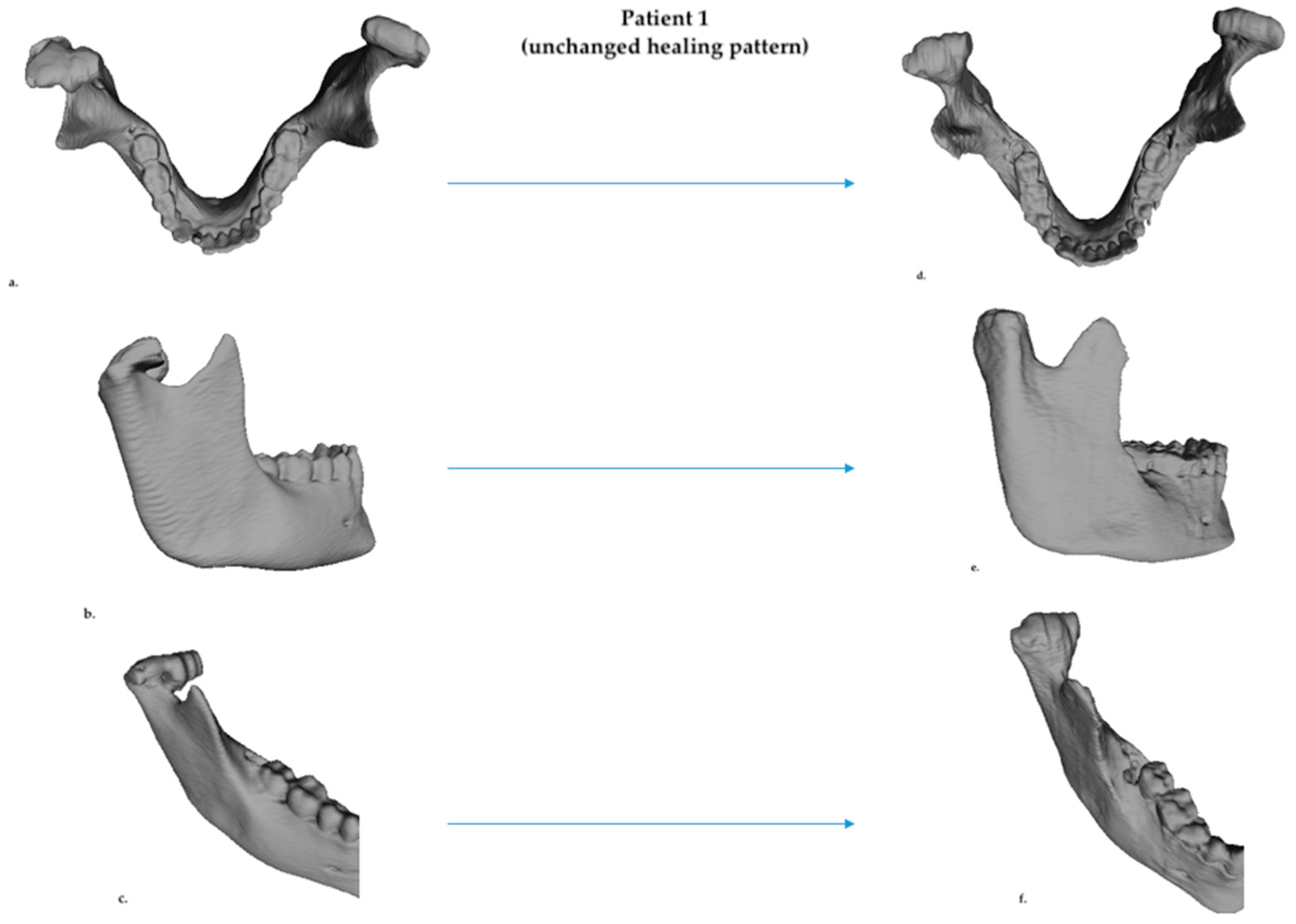
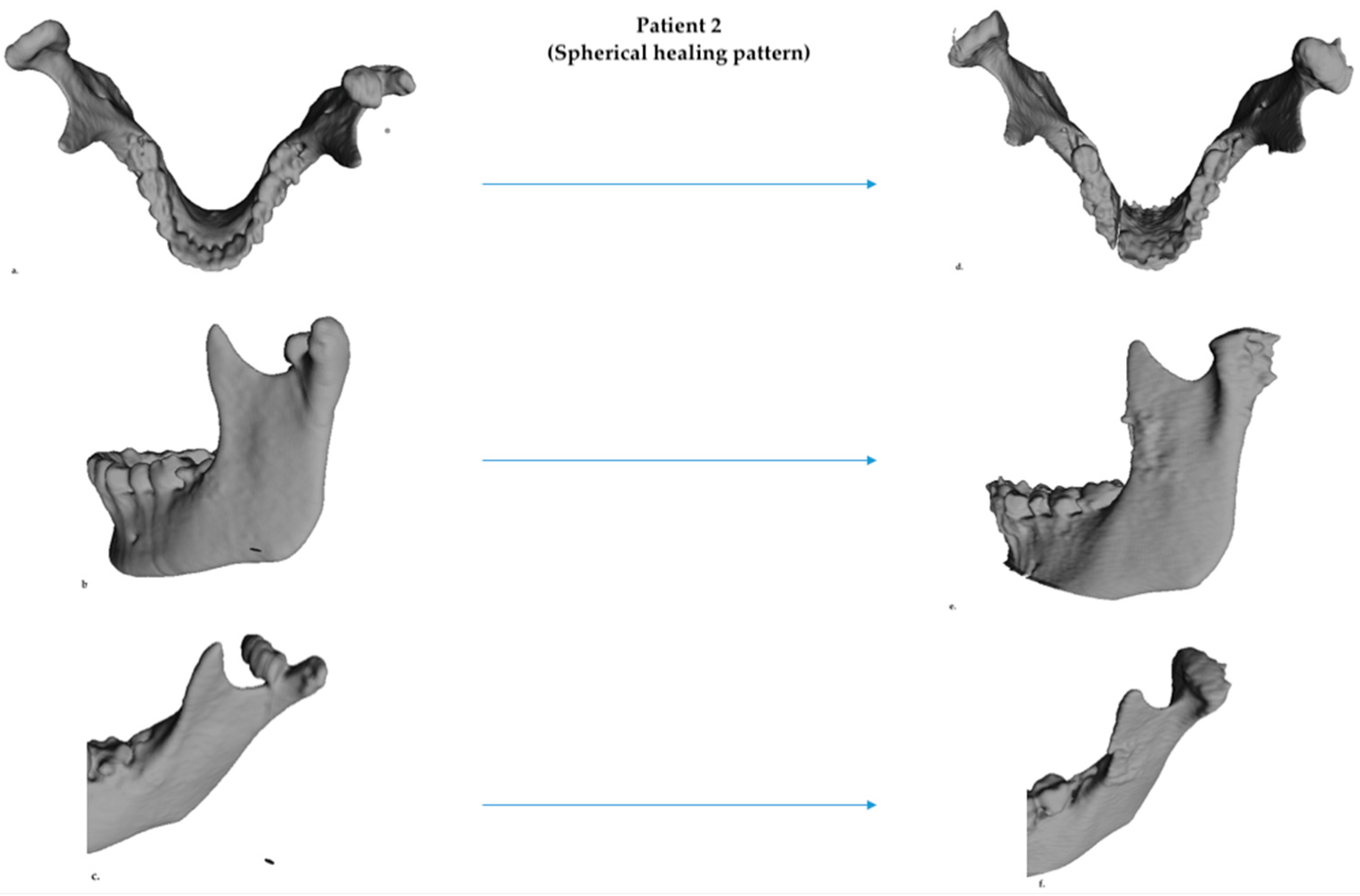
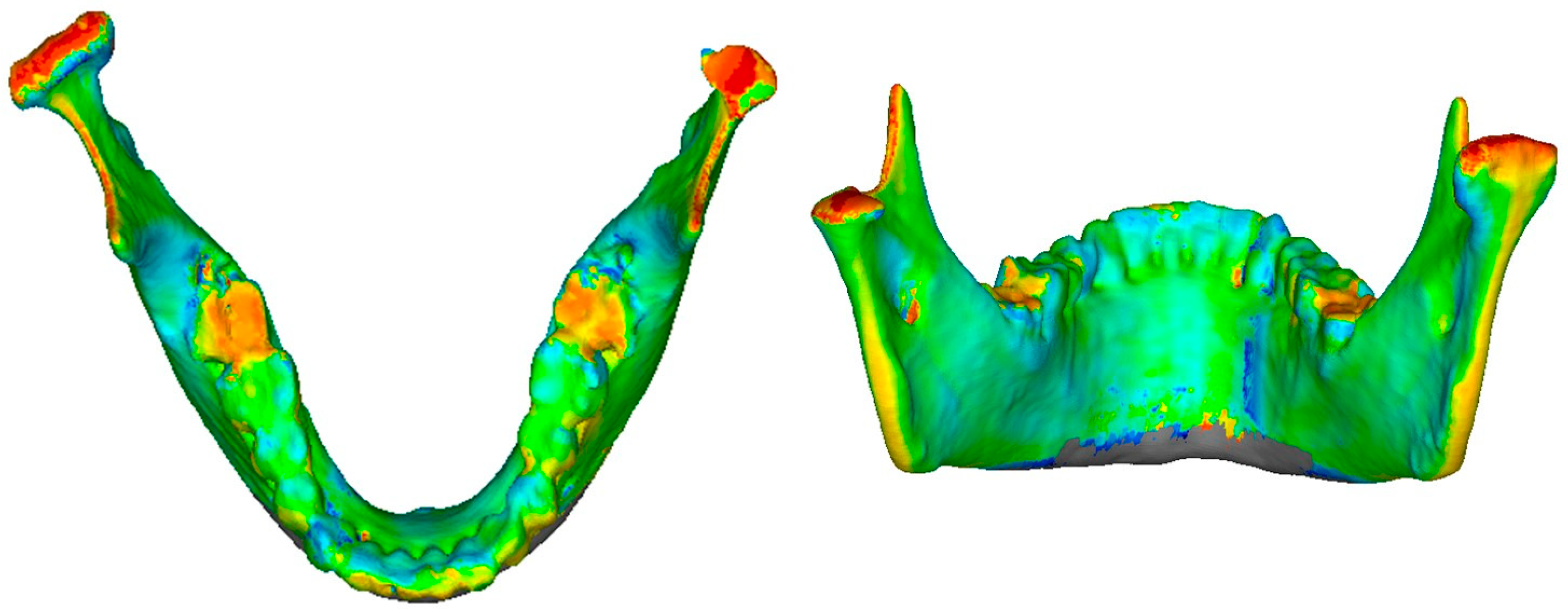
2.4.2. D Qualitative Assessment
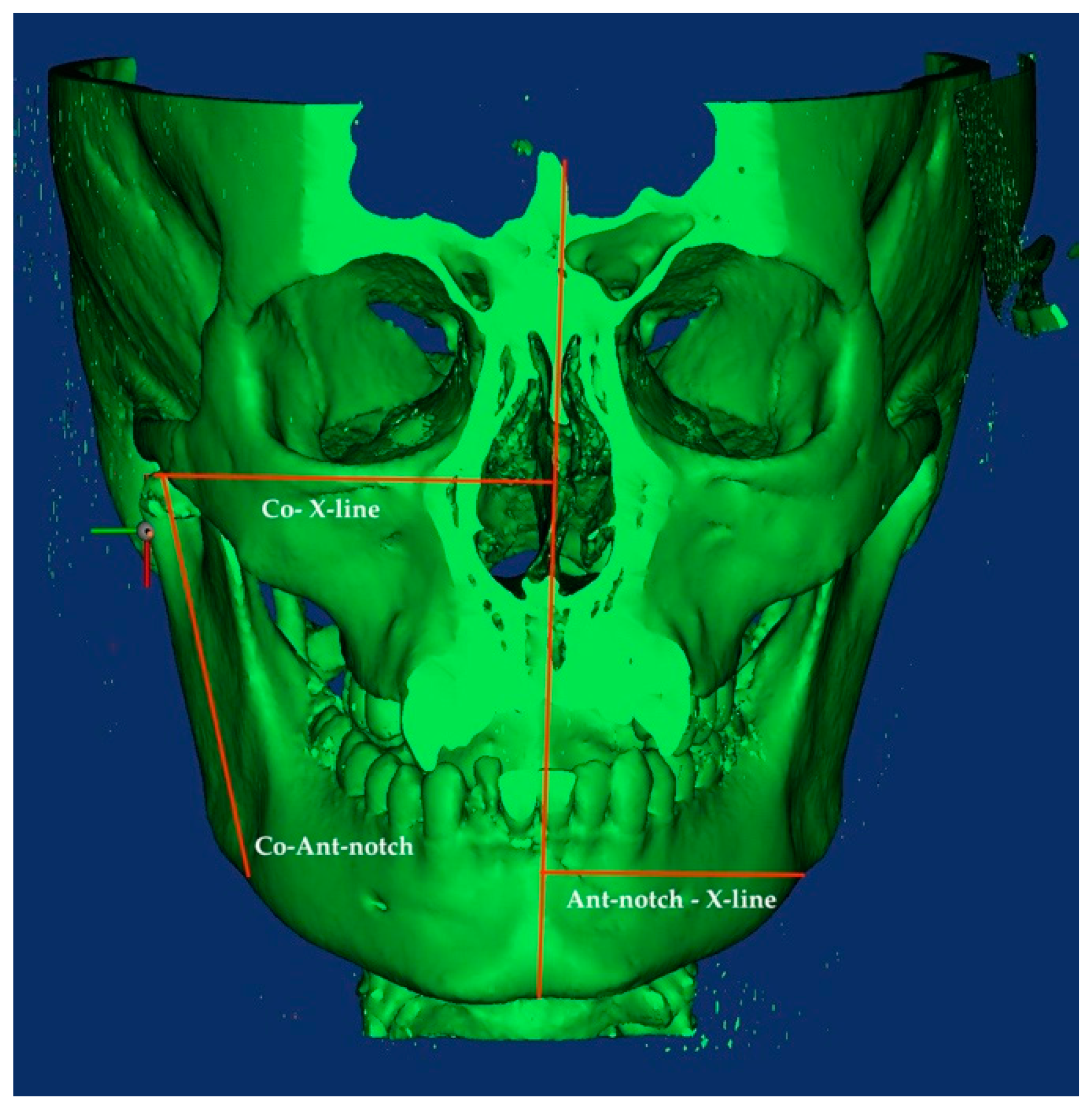
2.4.3. D Skeletal Asymmetry Assessment
- Condylion—X-Line distance: horizontal distance between the X-Line and the upper point of the condylar head;
- Antegonial notch—X-Line distance: horizontal distance between the Antegonial notch and the X-Line;
- Antegonial-notch—Condylion distance: vertical distance between the upper point of the condylar head and the antegonial notch.
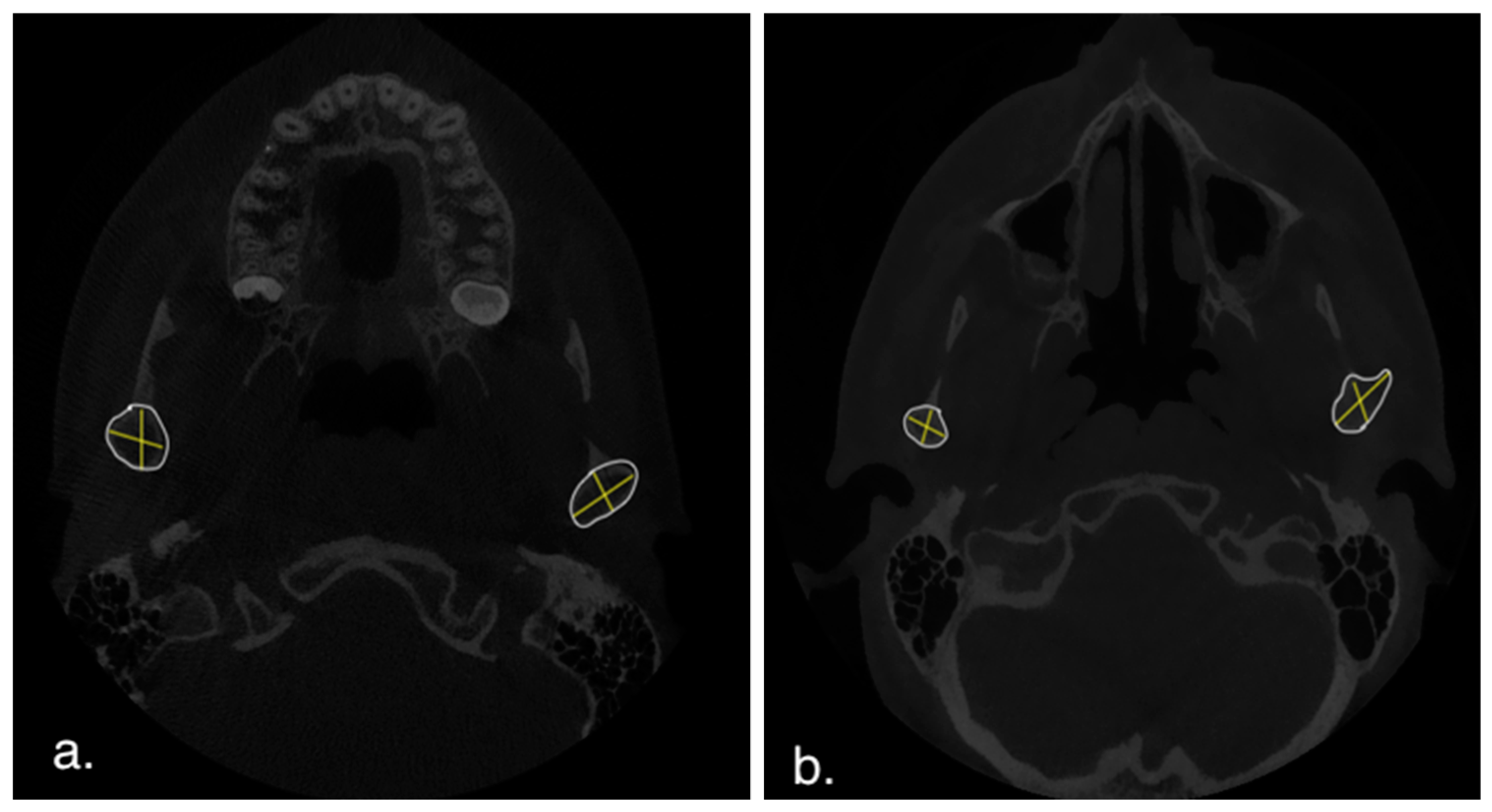
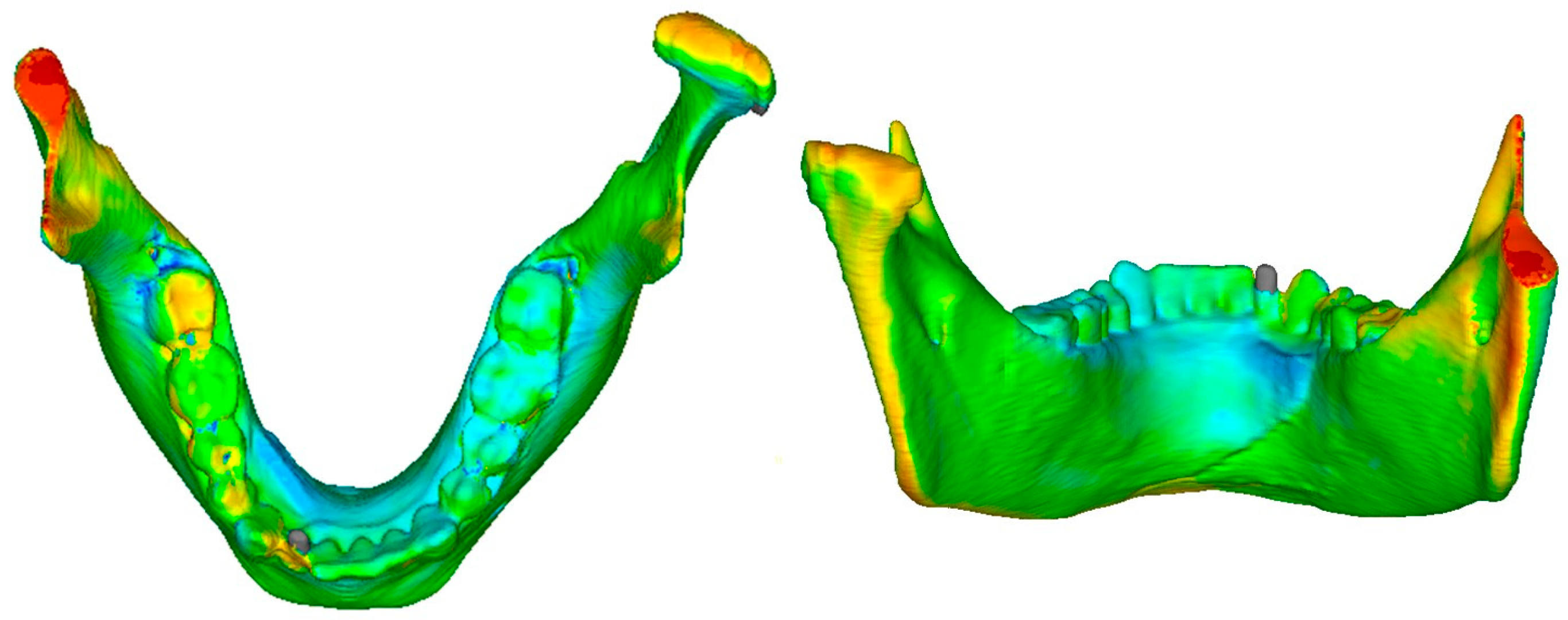
2.4.4. D Quantitative Assessment
2.4.5. Fractal Analysis
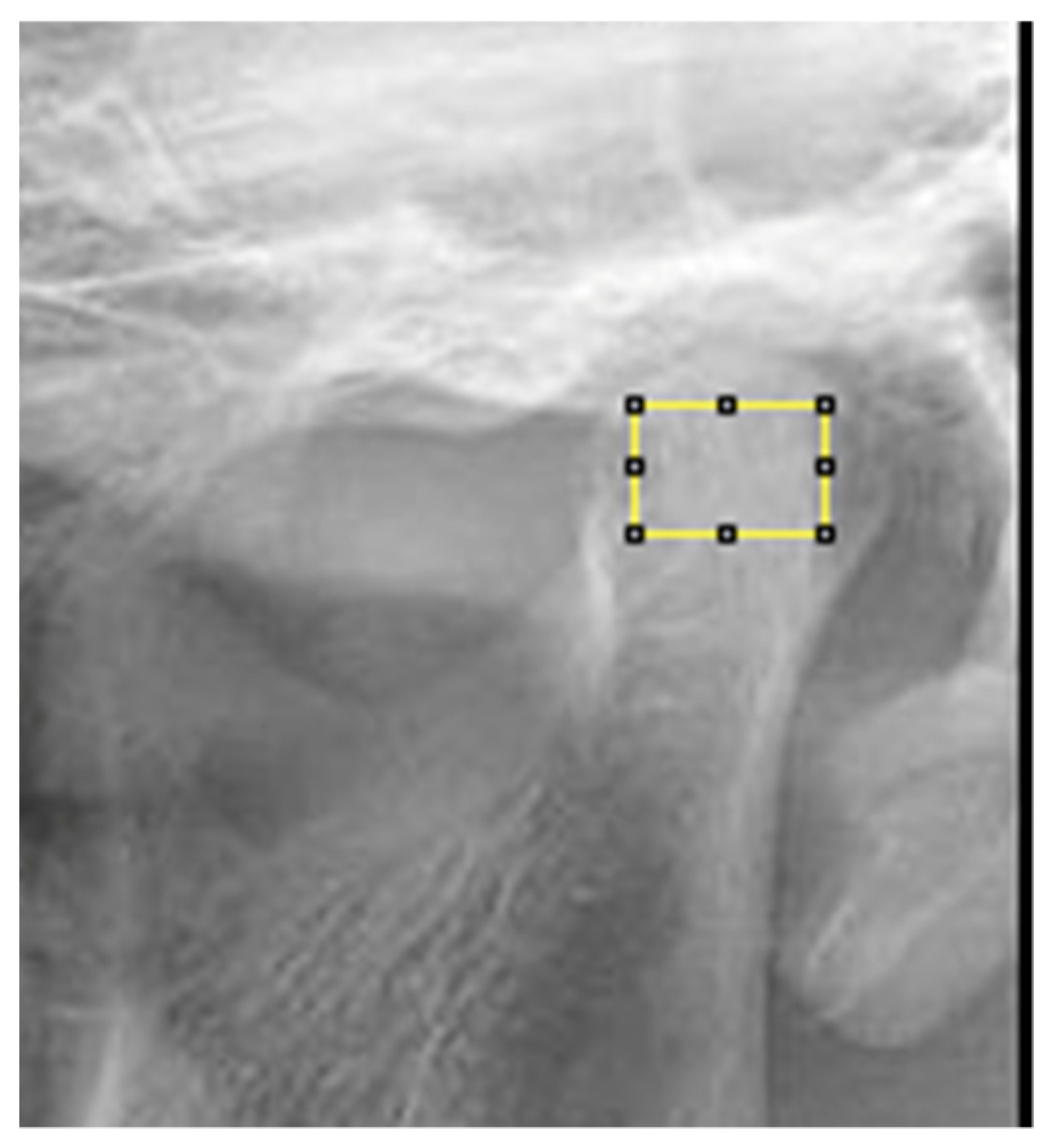
- Defining the region of interest (ROI: region of interest): condylar process, subcortical area of the condyle for OPTs (Figure 6);
- Application of Gaussian blurring, an image processing aimed at removing the “background noise” in the grayscale present in the radiograph, related to overlapping soft tissue or different thicknesses of bone tissue (Figure 7);
- Application of the binary filter to separate an object from the background (Figure 7);
- Erosion and dilation, two morphological operations that remove/add pixels to the contours of an object;
- Invert, a tool that inverts the tones (black and white) of an image, thus obtaining its negative, in photographic terms;
- Skeletonization, a tool that converts objects in the foreground of a binary image into a skeleton that preserves the original extent and interconnections;
- Finally, the fractal dimension (FD) was calculated.
2.5. Clinical-Functional Analysis
2.6. Statistical Analysis
3. Results
3.1. D Qualitative Assessment
3.2. D Skeletal Asymmetry Assessment
3.3. D Quantitative Assessment
3.4. Fractal Analysis
3.5. Clinical-Functional Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kozakiewicz, M.; Walczyk, A. Current Frequency of Mandibular Condylar Process Fractures. J. Clin. Med. 2023, 12, 1394. [Google Scholar] [CrossRef] [PubMed]
- Sahm, G.; Witt, E. Long-term results after childhood condylar fractures. A computer-tomographic study. Eur. J. Orthod. 1989, 11, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Montazem, A.H.; Anastassov, G. Management of condylar fractures. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2009, 17, 55–69. [Google Scholar] [CrossRef] [PubMed]
- Brandt, M.T.; Haug, R.H. Open versus closed reduction of adult mandibular condyle fractures: A review of the literature regarding the evolution of current thoughts on management. J. Oral Maxillofac. Surg. 2003, 61, 1324–1332. [Google Scholar] [CrossRef]
- Choi, K.Y.; Yang, J.-D.; Chung, H.-Y.; Cho, B.-C. Current Concepts in the Mandibular Condyle Fracture Management Part II: Open Reduction Versus Closed Reduction. Arch. Plast. Surg. 2012, 39, 301–308. [Google Scholar] [CrossRef]
- Wheeler, J.; Phillips, J. Pediatric facial fractures and potential long-term growth disturbances. Craniomaxillofac. Trauma Reconstr. 2011, 4, 43–52. [Google Scholar] [CrossRef]
- Medina, A.C. Functional appliance treatment for bilateral condylar fracture in a pediatric patient. Pediatr. Dent. 2009, 31, 432–437. [Google Scholar]
- Melsen, B.; Bjerregaard, J.; Bundgaard, M. The effect of treatment with functional appliance on a pathologic growth pattern of the condyle. Am. J. Orthod. Dentofac. Orthop. 1986, 90, 503–512. [Google Scholar] [CrossRef]
- Du, C.; Xu, B.; Zhu, Y.; Zhu, M. Radiographic evaluation in three dimensions of condylar fractures with closed treatment in children and adolescents. J. Craniomaxillofac. Surg. 2021, 49, 830–836. [Google Scholar] [CrossRef]
- Rutges, J.; Kruizinga, E.; Rosenberg, A.; Koole, R. Functional results after conservative treatment of fractures of the mandibular condyle. Br. J. Oral Maxillofac. Surg. 2007, 45, 30–34. [Google Scholar] [CrossRef]
- Reichenbach, E. Zur Diskusluxation und deren funktionskieferorthopädischer Behandlung. J. Orofac. Orthop./Fortschritte Kieferorthopädie 1958, 19, 44–48. [Google Scholar] [CrossRef]
- Assael, L.A. Open versus closed reduction of adult mandibular condyle fractures: An alternative interpretation of the evidence. J. Oral Maxillofac. Surg. 2003, 61, 1333–1339. [Google Scholar] [CrossRef] [PubMed]
- Tavares, C.A.; Allgayer, S. Conservative orthodontic treatment for a patient with a unilateral condylar fracture. Am. J. Orthod. Dentofac. Orthop. 2012, 141, e75–e84. [Google Scholar] [CrossRef] [PubMed]
- Hennig, C.L.; Krause, F.; Nitzsche, A.; Tolksdorf, K.; Reise, M.; Kranz, S.; Dederichs, M.; Schultze-Mosgau, S.; Jacobs, C. Functional Orthodontic Therapy for Mandibular Condyle Fracture: A Systematic Review. Medicina 2024, 60, 1336. [Google Scholar] [CrossRef]
- Azzi, L.; Moretto, P.; Vinci, R.; Croveri, F.; Boggio, A.; Silvestre-Rangil, J.; Tettamanti, L.; Tagliabue, A.; Passi, A. Human beta2-defensin in oral lichen planus expresses the degree of inflammation. J. Biol. Regul. Homeost. Agents 2017, 31 (Suppl. S1), 77–87. [Google Scholar]
- Schienbein, H. Treatment of temporomandibular fractures with an activator (II). Quintessence Int. Dent. Dig. 1977, 8, 9–18. [Google Scholar]
- Kirchner, L. Die funktionskieferorthopädische Behandlung der Kiefergelenkfrakturen. J. Orofac. Orthop. 1958, 19, 60–68. [Google Scholar] [CrossRef]
- Steinhardt, G. Behandlung der Frakturen des Kieferbereiches im Kindesalter. Zahnarztl Mitt. 1979, 69, 34–40. [Google Scholar]
- Hirschfelder, U. Eine klinische und computertomographische Untersuchung. Fortschritte Der Kieferorthopädie 1987, 48, 504–515. [Google Scholar] [CrossRef]
- Lajolo, C.; Tranfa, M.; Patini, R.; Fiorino, A.; Musarra, T.; Boniello, R.; Moro, A. Clinical Evaluation of the Optical Filter for Autofluorescence Glasses for Oral Cancer Curing Light Exposed (GOCCLES((R))) in the Management of Potentially Premalignant Disorders: A Retrospective Study. Int. J. Environ. Res. Public Health 2022, 19, 5579. [Google Scholar]
- Sabbagh, H.; Nikolova, T.; Kakoschke, S.C.; Wichelhaus, A.; Kakoschke, T.K. Functional Orthodontic Treatment of Mandibular Condyle Fractures in Children and Adolescent Patients: An MRI Follow-Up. Life 2022, 12, 1596. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.H.; Lv, K.; Yang, R.-T.; Li, Z.; Li, Z.-B. Extracapsular Condylar Fractures Treated Conservatively in Children: Mechanism of Bone Remodelling. J. Craniofac. Surg. 2021, 32, 1440–1444. [Google Scholar] [CrossRef] [PubMed]
- Neff, A.; Kolk, A.; Deppe, H.; Horch, H.H. New aspects for indications of surgical management of intra-articular and high temporomandibular dislocation fractures. Mund-Kiefer-Und Gesichtschirurgie MKG 1999, 3, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Hlawitschka, M.; Eckelt, U. Assessment of patients treated for intracapsular fractures of the mandibular condyle by closed techniques. J. Oral Maxillofac. Surg. 2002, 60, 784–791; discussion 792. [Google Scholar] [CrossRef]
- Riley, D.S.; Barber, M.S.; Kienle, G.S.; Aronson, J.K.; von Schoen-Angerer, T.; Tugwell, P.; Kiene, H.; Helfand, M.; Altman, D.G.; Sox, H.; et al. CARE guidelines for case reports: Explanation and elaboration document. J. Clin. Epidemiol. 2017, 89, 218–235. [Google Scholar] [CrossRef]
- World Medical, A. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Loukota, R.A.; Neff, A.; Rasse, M. Nomenclature/classification of fractures of the mandibular condylar head. Br. J. Oral Maxillofac. Surg. 2010, 48, 477–478. [Google Scholar] [CrossRef]
- Powers, D.B. Classification of Mandibular Condylar Fractures. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2017, 25, 1–10. [Google Scholar] [CrossRef]
- Long, X. The relationship between temporomandibular joint ankylosis and condylar fractures. Chin. J. Dent. Res. 2012, 15, 17–20. [Google Scholar]
- Hirjak, D.; Machon, V.; Beno, M.; Galis, B.; Kupcova, I. Surgical treatment of condylar head fractures, the way to minimize the postraumatic TMJ ankylosis. Bratisl. Lek. Listy 2017, 118, 17–22. [Google Scholar] [CrossRef]
- Ma, X.; Zhang, X.; Liu, X.; Hou, C.; Hou, W. A case report of conservative treatment of sagittal condylar fracture in a child: 13 years of follow up. Chin. J. Stomatol. 2015, 50, 217–219. [Google Scholar]
- Naeije, M.; Hansson, T.L. Short-term effect of the stabilization appliance on masticatory muscle activity in myogenous craniomandibular disorder patients. J. Craniomandib. Disord. 1991, 5, 245–250. [Google Scholar] [PubMed]
- Fatima, J.; Kaul, R.; Jain, P.; Saha, S.; Halder, S.; Sarkar, S. Clinical Measurement of Maximum Mouth Opening in Children of Kolkata and Its Relation with Different Facial Types. J. Clin. Diagn. Res. 2016, 10, ZC01. [Google Scholar] [CrossRef] [PubMed]
- Gomes, C.A.F.d.P.; Dibai-Filho, A.V.; da Silva, J.R.; de Oliveira, P.M.; Politti, F.; Biasotto-Gonzalez, D.A. Correlation between severity of temporomandibular disorder and mandibular range of motion. J. Bodyw. Mov. Ther. 2014, 18, 306–310. [Google Scholar]
- Staderini, E.; Guglielmi, F.; Cornelis, M.A.; Cattaneo, P.M. Three-dimensional prediction of roots position through cone-beam computed tomography scans-digital model superimposition: A novel method. Orthod. Craniofac. Res. 2019, 22, 16–23. [Google Scholar] [CrossRef]
- Li, J.; Zhang, H.; Yin, P.; Su, X.; Zhao, Z.; Zhou, J.; Li, C.; Li, Z.; Zhang, L.; Tang, P. A New Measurement Technique of the Characteristics of Nutrient Artery Canals in Tibias Using Materialise’s Interactive Medical Image Control System Software. BioMed Res. Int. 2015, 2015, 171672. [Google Scholar] [CrossRef]
- Grummons, D.C.; van de Coppello, M.A.K. A frontal asymmetry analysis. J. Clin. Orthod. 1987, 21, 448–465. [Google Scholar]
- Janson, G.R.; Metaxas, A.; Woodside, D.G.; de Freitas, M.R.; Pinzan, A. Three-dimensional evaluation of skeletal and dental asymmetries in Class II subdivision malocclusions. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 406–418. [Google Scholar] [CrossRef]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An open-source platform for biological-image analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef]
- Kahl-Nieke, B.; Fischbach, R.; Gerlach, K.L. CT analysis of temporomandibular joint state in children 5 years after functional treatment of condylar fractures. Int. J. Oral Maxillofac. Surg. 1994, 23 Pt 1, 332–337. [Google Scholar] [CrossRef]
- Demiralp, K.O.; Kurşun-Çakmak, E.Ş.; Bayrak, S.; Akbulut, N.; Atakan, C.; Orhan, K. Trabecular structure designation using fractal analysis technique on panoramic radiographs of patients with bisphosphonate intake: A preliminary study. Oral Radiol. 2019, 35, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Kursun-Cakmak, E.S.; Bayrak, S. Comparison of fractal dimension analysis and panoramic-based radiomorphometric indices in the assessment of mandibular bone changes in patients with type 1 and type 2 diabetes mellitus. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 126, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Cesur, E.; Bayrak, S.; Kursun-Çakmak, E.Ş.; Arslan, C.; Köklü, A.; Orhan, K. Evaluating the effects of functional orthodontic treatment on mandibular osseous structure using fractal dimension analysis of dental panoramic radiographs. Angle Orthod. 2020, 90, 783–793. [Google Scholar] [CrossRef]
- Turker, G.; Yasar, M.O. Evaluation of associations between condylar morphology, ramus height, and mandibular plane angle in various vertical skeletal patterns: A digital radiographic study. BMC Oral Health 2022, 22, 330. [Google Scholar]
- Wieckowska, B.; Kubiak, K.B.; Jóźwiak, P.; Moryson, W.; Stawińska-Witoszyńska, B. Cohen’s Kappa Coefficient as a Measure to Assess Classification Improvement following the Addition of a New Marker to a Regression Model. Int. J. Environ. Res. Public Health 2022, 19, 10213. [Google Scholar] [CrossRef]
- Arslan, S.; Korkmaz, Y.N.; Buyuk, S.K.; Tekin, B. Effects of reverse headgear therapy on mandibular trabecular structure: A fractal analysis study. Orthod. Craniofac. Res. 2022, 25, 562–568. [Google Scholar] [CrossRef]
- Moss, M.L. The functional matrix hypothesis revisited. 1. The role of mechanotransduction. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 8–11. [Google Scholar] [CrossRef]
- Zhao, Y.M.; Yang, J.; Bai, R.-C.; Ge, L.-H.; Zhang, Y. A retrospective study of using removable occlusal splint in the treatment of condylar fracture in children. J. Craniomaxillofac. Surg. 2014, 42, 1078–1082. [Google Scholar] [CrossRef]
- Zheng, J.; Zhang, S.; Yang, C.; Abdelrehem, A.; He, D.; Chiu, H. Assessment of magnetic resonance images of displacement of the disc of the temporomandibular joint in different types of condylar fracture. Br. J. Oral Maxillofac. Surg. 2016, 54, 74–79. [Google Scholar] [CrossRef]
- Yu, Y.H.; Wang, M.H.; Zhang, S.Y.; Fang, Y.M.; Zhu, X.H.; Pan, L.L.; Yang, C. Magnetic resonance imaging assessment of temporomandibular joint soft tissue injuries of intracapsular condylar fracture. Br. J. Oral Maxillofac. Surg. 2013, 51, 133–137. [Google Scholar] [CrossRef]
- Choi, J.; Oh, N.; Kim, I.K. A follow-up study of condyle fracture in children. Int. J. Oral Maxillofac. Surg. 2005, 34, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Neff, A.; Cornelius, C.-P.; Rasse, M.; Torre, D.; Audigé, L. The Comprehensive AOCMF Classification System: Condylar Process Fractures-Level 3 Tutorial. Craniomaxillofac Trauma Reconstr. 2014, 7 (Suppl. S1), S044–S058. [Google Scholar] [CrossRef]


| Patient 1 (Right Condylar Fracture) | Patient 2 (Left Condylar Fracture) | |||||
|---|---|---|---|---|---|---|
| Cond-X Line | ||||||
| Healthy | Injured | AI | Healthy | Injured | AI | |
| Before | 75 mm | 70 mm | 3.44% | 68.46 mm | 65.33 mm | 2.33% |
| After | 75.1 mm | 74.2 mm | 0.66% | 68.64 mm | 67.1 mm | 1.11% |
| Ant-notch-X Line | ||||||
| Healthy | Injured | AI | Healthy | Injured | AI | |
| Before | 72.16 mm | 68.5 mm | 2.60% | 60.1 mm | 57.4 mm | 2.56% |
| After | 72.2 mm | 71.6 mm | 0.4% | 60.7 mm | 59.04 mm | 0.84% |
| Ant-notch-Cond | ||||||
| Healthy | Injured | AI | Healthy | Injured | AI | |
| Before | 65.9 mm | 61.8 mm | 3.20% | 60.5 mm | 56.9 mm | 2.40% |
| After | 65.89 mm | 64.3 mm | 1.38% | 60.25 mm | 60.9 mm | 0.75% |
| Patient 1 (Right Condylar Fracture) | Patient 2 (Left Condylar Fracture) | |||||
|---|---|---|---|---|---|---|
| TC measurements | ||||||
| Healthy | Injured | AI | Healthy | Injured | AI | |
| Antero-posterior width | 11.5 mm | 11.8 mm | 1.28% | 5.9 mm | 9.22 mm | 21.1% |
| Medio-lateral width | ||||||
| 20.17 mm | 19.4 mm | 1.2% | 14.84 mm | 17.9 mm | 9.6% | |
| Patient 1 (Right Condylar Fracture) | Patient 2 (Left Condylar Fracture) | |||
|---|---|---|---|---|
| FD Values | Healthy | Injured | Healthy | Injured |
| Before | 2.249 | 2.016 | 2.211 | 1.986 |
| After | ||||
| 2.248 | 2.182 | 2.218 | 2.063 | |
| Patient 1 (Right Condylar Fracture) | Patient 2 (Left Condylar Fracture) | |||
|---|---|---|---|---|
| Functional measurements | ||||
| Before | After | Before | After | |
| MMO * | 29 mm | 44 mm | 40 mm | 42 mm |
| Lateral Excursion (towards right) | ||||
| 11 mm | 10 mm | 6 mm | 8 mm | |
| Lateral Excursion (towards left) | 5 mm | 11 mm | 10 mm | 10 mm |
| MD ** | 2 mm | 0.2 mm | 1 mm | 0 mm |
| Articular noise (yes/no) | No | No | No | No |
| Algic symptoms (yes/no) | Yes | No | Yes | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Staderini, E.; Cavalcanti, I.; Schiavelli, A.; Gallenzi, P.; Di Carlo, G.; Cordaro, M. Radiological Healing Patterns and Functional Outcomes After Conservative Treatment of Unilateral Condylar Fractures: A Report of Two Cases. Appl. Sci. 2025, 15, 4261. https://doi.org/10.3390/app15084261
Staderini E, Cavalcanti I, Schiavelli A, Gallenzi P, Di Carlo G, Cordaro M. Radiological Healing Patterns and Functional Outcomes After Conservative Treatment of Unilateral Condylar Fractures: A Report of Two Cases. Applied Sciences. 2025; 15(8):4261. https://doi.org/10.3390/app15084261
Chicago/Turabian StyleStaderini, Edoardo, Irene Cavalcanti, Anna Schiavelli, Patrizia Gallenzi, Gabriele Di Carlo, and Massimo Cordaro. 2025. "Radiological Healing Patterns and Functional Outcomes After Conservative Treatment of Unilateral Condylar Fractures: A Report of Two Cases" Applied Sciences 15, no. 8: 4261. https://doi.org/10.3390/app15084261
APA StyleStaderini, E., Cavalcanti, I., Schiavelli, A., Gallenzi, P., Di Carlo, G., & Cordaro, M. (2025). Radiological Healing Patterns and Functional Outcomes After Conservative Treatment of Unilateral Condylar Fractures: A Report of Two Cases. Applied Sciences, 15(8), 4261. https://doi.org/10.3390/app15084261









