Comparative Survival of Restorations in MIH-Affected Pediatric Teeth Using Total-Etch Versus Self-Etch Adhesive Systems: A Systematic Review and Meta-Analysis
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Registration and Protocol
2.2. Eligibility Criteria
2.3. Information Sources and Search Strategy
2.4. Selection Process
2.5. Data Collection Process
2.6. Quality Assessment
2.7. Data Analysis and Synthesis
3. Results
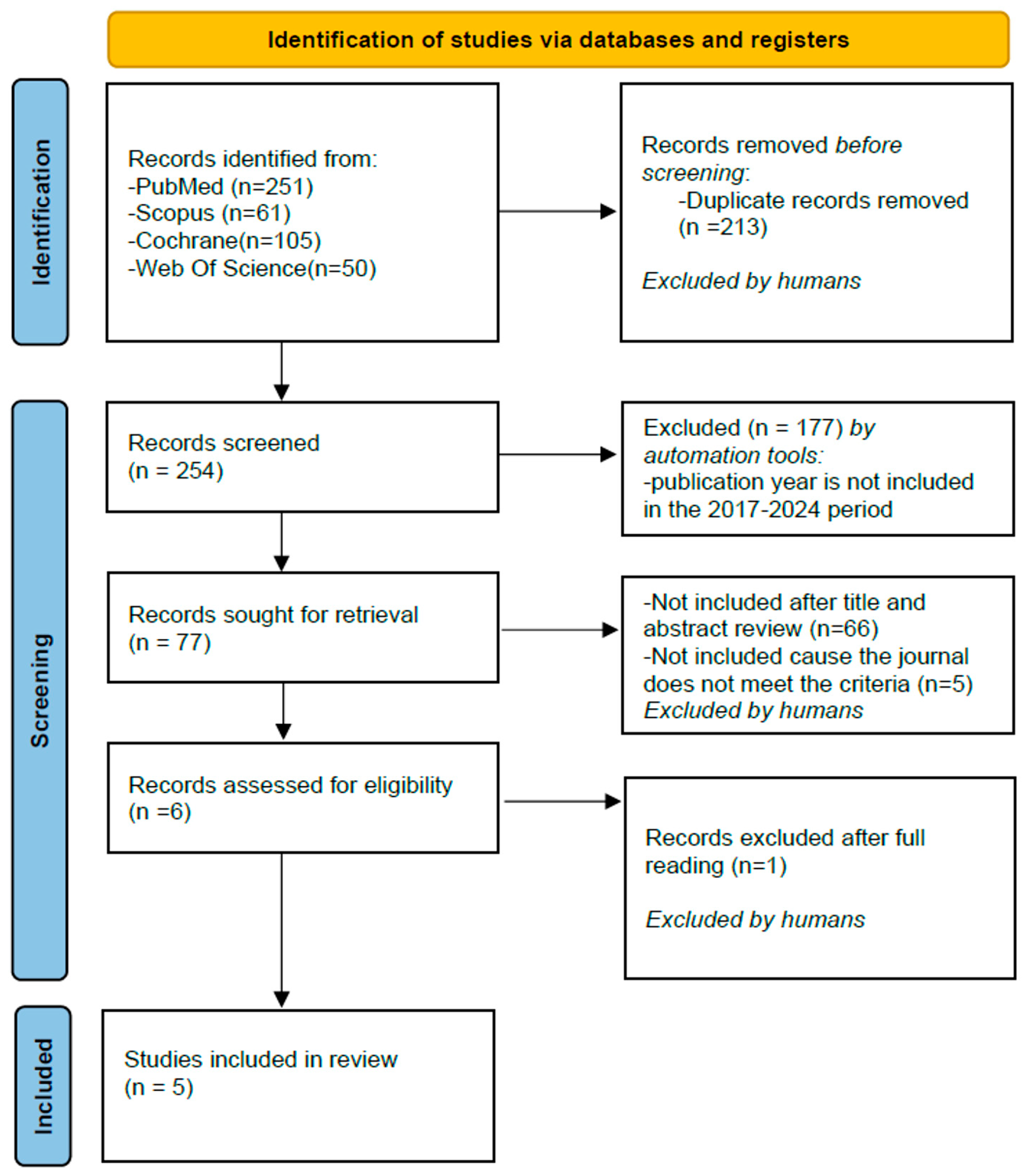
3.1. Study Selection
3.2. Study Characteristics
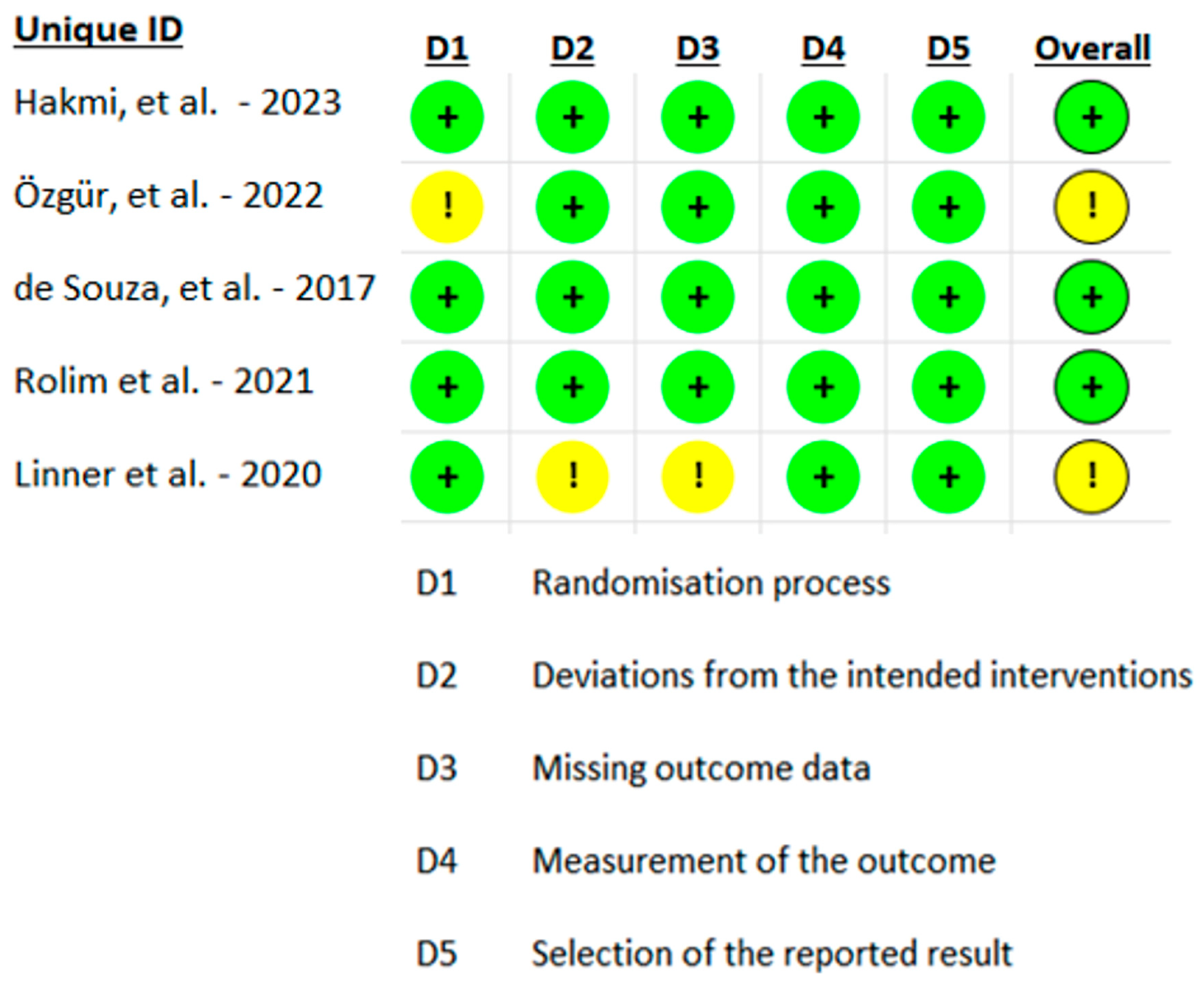
3.3. Study Risk of Bias Assessment
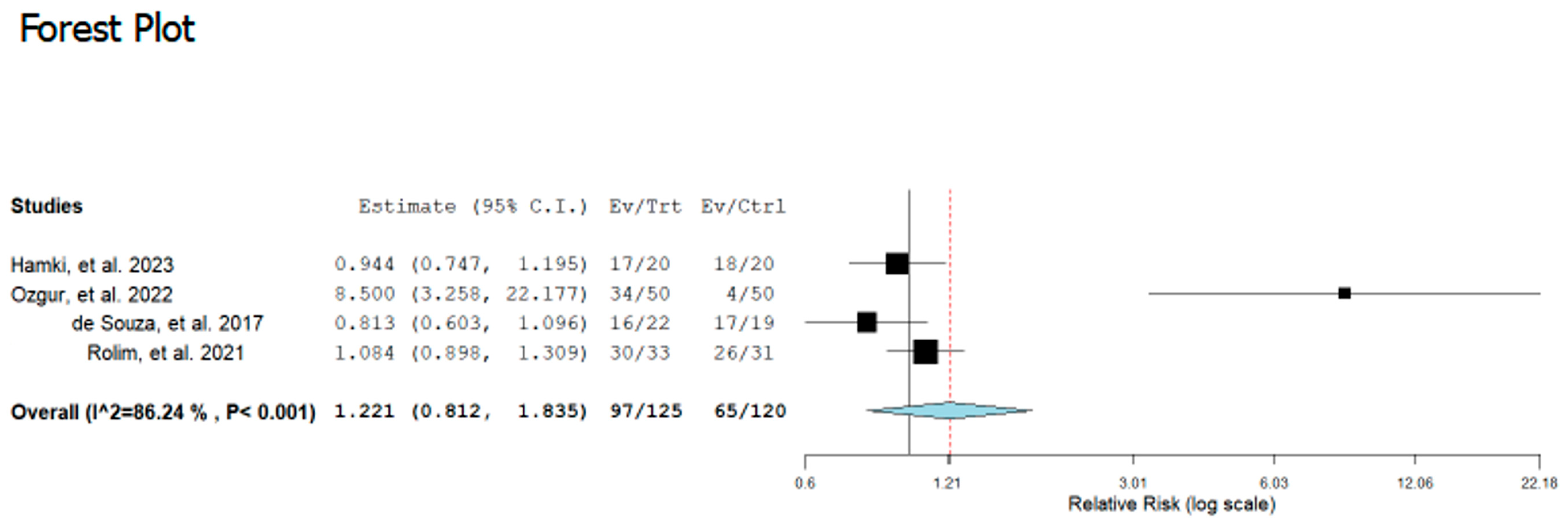
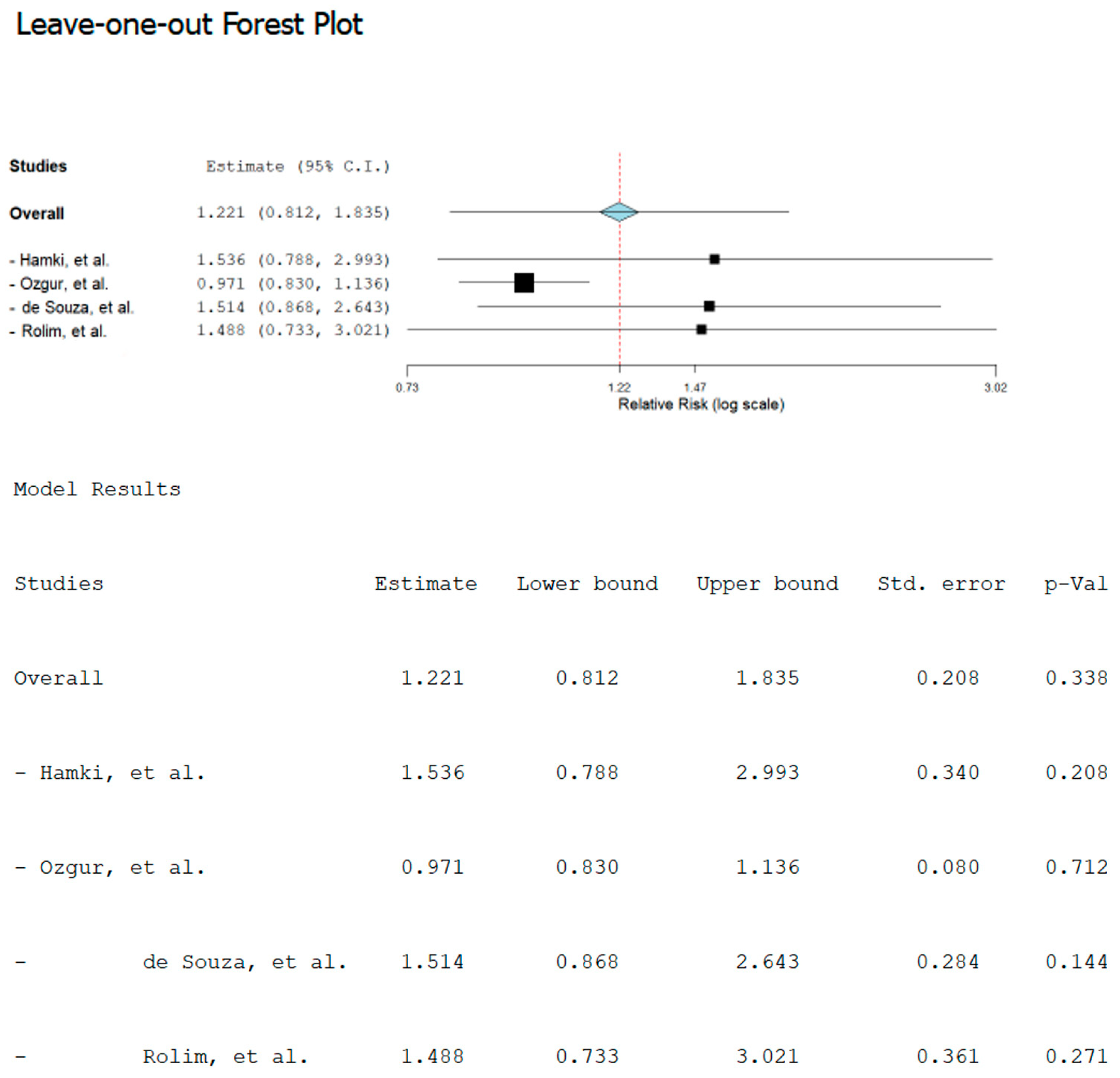
3.4. Synthesis Methods
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Juárez-López, M.L.A.; Salazar-Treto, L.V.; Hernández-Monjaraz, B.; Molina-Frechero, N. Etiological Factors of Molar Incisor Hypomineralization: A Systematic Review and Meta-Analysis. Dent. J. 2023, 11, 111. [Google Scholar] [CrossRef]
- Lygidakis, N.A.; Garot, E.; Somani, C.; Taylor, G.D.; Rouas, P.; Wong, F.S.L. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): An updated European Academy of Paediatric Dentistry policy document. Eur. Arch. Paediatr. Dent. 2022, 23, 3–21. [Google Scholar] [CrossRef]
- Lopes, L.B.; Machado, V.; Mascarenhas, P.; Mendes, J.J.; Botelho, J. The prevalence of molar-incisor hypomineralization: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 22405. [Google Scholar] [CrossRef]
- Elfrink, M.E.C.; ten Cate, J.M.; Jaddoe, V.W.V.; Hofman, A.; Moll, H.A.; Veerkamp, J.S.J. Deciduous Molar Hypomineralization and Molar Incisor Hypomineralization. J. Dent. Res. 2012, 91, 551–555. [Google Scholar] [CrossRef]
- Jorge, R.C.; Dos Papoula GorniReis, P.; Marañón-Vásquez, G.A.; Masterson, D.; Cople Maia, L.; Mendes Soviero, V. Are yellow-brownish opacities in hypomineralized teeth more prone to breakage than white-creamy ones? A systematic review. Clin. Oral Investig. 2022, 26, 5795–5808. [Google Scholar] [CrossRef]
- Elhennawy, K.; Manton, D.J.; Crombie, F.; Zaslansky, P.; Radlanski, R.J.; Jost-Brinkmann, P.-G.; Schwendicke, F. Structural, mechanical and chemical evaluation of molar-incisor hypomineralization- affected enamel: A systematic review. Arch. Oral Biol. 2017, 83, 272–281. [Google Scholar] [CrossRef]
- Jalevik, B.; Klingberg, G.A. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. Int. J. Paediatr. Dent. 2022, 12, 24–32. [Google Scholar] [CrossRef]
- Americano, G.C.A.; Jacobsen, P.E.; Soviero, V.M.; Haubek, D. A systematic review on the association between molar incisor hypomineralization and dental caries. Int. J. Pediatr. Dent. 2017, 27, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Fagrell, T.G.; Dietz, W.; Jalevik, B.; Noren, J.G. Chemical, mechanical and morphological properties of hypomineralized enamel of permanent first molars. Acta Odontol. Scand. 2010, 68, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, E.K.; Rohanizadeh, R.; Ismail, F.S.M.; Kilpatrick, N.; Swain, M. Mechanical properties and microstructure of hypomineralised enamel of permanent teeth. Biomaterial 2004, 25, 5091–5100. [Google Scholar] [CrossRef]
- Gevert, M.V.; Wambier, L.M.; Ito, L.Y.; Feltrin de Souza, J.; Chibinski, A.C.R. Which are the clinical consequences of Molar Incisor hypomineralization (MIH) in children and adolescents? Systematic review and meta-analysis. Clin. Oral Investig. 2024, 28, 415. [Google Scholar] [CrossRef]
- Bozal, C.B.; Kaplan, A.; Ortolani, A.; Cortese, S.G.; Biondi, A.M. Ultrastructure of the surface of dental enamel with molar incisor hypomineralization (MIH) with and without acid etching. Acta Odontol. Latinoam. 2015, 28, 192–198. [Google Scholar]
- Somani, C.; Taylor, G.D.; Garot, E.; Rouas, P.; Lygidakis, N.A.; Wong, F.S.L. An update of treatment modalities in children and adolescents with teeth affected by molar incisor hypomineralisation (MIH): A systematic review. Eur. Arch. Paediatr. Dent. 2021, 23, 39–64. [Google Scholar] [CrossRef] [PubMed]
- Farah, R.A.; Monk, B.C.; Swain, M.V.; Drummond, B.K. Protein content of molar-incisor hypomineralisation enamel. J. Dent. 2010, 38, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Saikaew, P.; Sattabanasuk, V.; Harnirattisai, C.; Chowdhury, A.F.M.A.; Carvalho, R.; Sano, H. Role of the smear layer in adhesive dentistry and the clinical applications to improve bonding performance. Jpn. Dent. Sci. Rev. 2022, 58, 59–66. [Google Scholar] [CrossRef]
- Perdigão, J.; Geraldeli, S.; Hodges, J.S. Total-etch versus self-etch adhesive: Effect on postoperative sensitivity. J. Am. Dent. Assoc. 2003, 134, 1621–1629. [Google Scholar] [CrossRef] [PubMed]
- Krämer, N.; Bui Khac, N.N.; Lücker, S.; Stachniss, V.; Frankenberger, R. Bonding strategies for MIH-affected enamel and dentin. Dent. Mater. 2018, 34, 331–340. [Google Scholar] [CrossRef]
- Lygidakis, N.; Dimou, G.; Stamataki, E. Retention of fissure sealants using two different methods of application in teeth with hypomineral ised molars (MIH): A 4-year clinical study. Eur. Arch. Paediatr. Dent. 2009, 10, 223–226. [Google Scholar] [CrossRef]
- Fragelli, C.M.; Souza, J.F.; Jeremias, F.; Cordeiro Rde, C.; Santos-Pinto, L. Molar incisor hypomineralization (MIH): Conservative treat ment management to restore affected teeth. Braz. Oral Res. 2015, 29, S1806-83242015000100271. [Google Scholar] [CrossRef]
- D’Amario, M.; Piccioni, C.; Di Carlo, S.; De Angelis, F.; Caruso, S.; Capogreco, M. Effect of Airborne Particle Abrasion on Microtensile Bond Strength of Total-Etch Adhesives to Human Dentin. BioMed Res. Int. 2017, 2017, 2432536. [Google Scholar] [CrossRef]
- Inchingolo, A.M.; Inchingolo, A.D.; Viapiano, F.; Ciocia, A.M.; Ferrara, I.; Netti, A.; Dipalma, G.; Palermo, A.; Inchingolo, F. Treatment Approaches to Molar Incisor Hypomineralization: A Systematic Review. J. Clin. Med. 2023, 12, 7194. [Google Scholar] [CrossRef]
- Dhareula, A.; Goyal, A.; Gauba, K.; Bhatia, S.K. Esthetic rehabilitation of first permanent molars affected with severe form of molar incisor hypomineralization using indirect composite onlays—A case series. Pediatr. Dent. J. 2018, 28, 62–67. [Google Scholar] [CrossRef]
- Dhareula, A.; Goyal, A.; Gauba, K.; Bhatia, S.; Kapur, A.; Bhandari, S. A clinical and radiographic investigation comparing the efficacy of cast metal and indirect resin onlays in rehabilitation of permanent first molars affected with severe molar incisor hypomineralisation (MIH): A 36-month randomised controlled clinical trial. Eur. Arch. Paediatr. Dent. 2019, 20, 489–500. [Google Scholar] [CrossRef] [PubMed]
- Durmus, B.; Sezer, B.; Tugcu, N.; Caliskan, C.; Bekiroglu, N.; Kargul, B. Two-year survival of high-viscosity glass ionomer in children with molar incisor hypomineralization. Med. Princ. Pract. 2021, 30, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Villani, F.A.; Aiuto, R.; Dioguardi, M.; Paglia, L.; Caruso, S.; Gatto, R.; Re, D.; Garcovich, D. Caries prevalence and molar incisor hypomineralisation (MIH) in children. Is there an association? A systematic review. Eur. J. Paediatr. Dent. 2023, 24, 312–320. [Google Scholar]
- Fang, K.; Chen, K.; Shi, M.; Wang, L. Effect of different adhesive systems on dental defects and sensitivity to teeth in composite resin restoration: A systematic review and meta-analysis. Clin. Oral Investig. 2023, 27, 2495–2511. [Google Scholar] [CrossRef]
- Prud’homme, T.; Hyon, I.; Dajean Trutaud, S.; Lopez Cazaux, S. Different applicabilities of the etch-bleach-seal technique for treating opacities on permanent incisor damage by molar incisor hypomineralisation in three young patients. BMJ Case Rep. 2017, 2017, bcr2017221442. [Google Scholar] [CrossRef]
- Hickel, R.; Peschke, A.; Tyas, M.; Mjör, I.; Bayne, S.; Peters, M.; Hiller, K.-A.; Randall, R.; Vanherle, G.; Heintze, S.D. FDI World Dental Federation—Clinical criteria for the evaluation of direct and indirect restorations. Update and clinical exam ples. Clin. Oral Investig. 2010, 14, 349–366. [Google Scholar] [CrossRef]
- Bekes, K.; Boeckler, L.; Gernhardt, C.R.; Schaller, H.G. Clinical performance of a self-etching and a total-etch adhesive system—2-year results. J. Oral Rehabil. 2007, 34, 855–861. [Google Scholar] [CrossRef] [PubMed]
- Chermont, A.B.; Carneiro, K.K.; Lobato, M.F.; Machado, S.M.M. Clinical evaluation of postoperative sensitivity using self-etching adhesives containing glutaraldehyde. Braz. Oral Res. 2010, 24, 349–354. [Google Scholar] [CrossRef]
- Cruz, J.; Silva, A.L.; Eira, R.; Coito, C.; Lopes, M.; Cavalheiro, A. 24-Month clinical performance of a universal adhesive on non-carious cervical lesions: Self-etch and etch-and-rinse techniques. J. Adhes. Dent. 2021, 23, 379–387. [Google Scholar] [PubMed]
- Kasahara, Y.; Takamizawa, T.; Hirokane, E.; Tsujimoto, A.; Ishii, R.; Barkmeier, W.W.; Latta, M.A.; Miyazaki, M. Comparison of different etch-and-rinse adhesive systems based on shear fatigue dentin bond strength and morphological features the interface. Dent. Mater. 2021, 37, e109–e117. [Google Scholar] [CrossRef]
- Taylor, G.D.; Pearce, K.F.; Vernazza, C.R. Management of compromised first permanent molars in children: Cross-Sectional analysis of attitudes of UK general dental practitioners and specialists in paediatric dentistry. Int. J. Paediatr. Dent. 2019, 29, 267–280. [Google Scholar] [CrossRef]
- Kotsanos, N.; Kaklamanos, E.G.; Arapostathis, K. Treatment manage ment of first permanent molars in children with molar-incisor hypomineralisation. Eur. J. Paediatr. Dent. 2005, 6, 179–184. [Google Scholar]
- Chan, Y.L.; Ngan, A.H.; King, N.M. Degraded prism sheaths in the transition region of hypomineralized teeth. J. Dent. 2010, 38, 237–244. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Lagarde, M.; Vennat, E.; Attal, J.P.; Dursun, E. Strategies to optimize bonding of adhesive materials to molar-incisor hypomineralization-affected enamel: A systematic review. Int. J. Paediatr. Dent. 2020, 30, 405–420. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Zhang, Y.; Huang, L.; Wang, D.; Ren, P.; Hong, Q.; Kang, D. The ROBINS-I and the NOS had similar reliability but differed in applicability: A random sampling observational studies of systematic reviews/meta-analysis. J. Evid. Based Med. 2021, 14, 112–122. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [PubMed]
- Hakmi, A.; Dashash, M. Direct or indirect composite for restoring permanent first molars affected by Molar Incisor Hypomineralisation (MIH): A randomized clinical controlled trial. BDJ Open 2023, 9, 37. [Google Scholar] [CrossRef] [PubMed]
- Özgür, B.; Kargın, S.T.; Ölmez, M.S. Clinical evaluation of giomer- and resin-based fissure sealants on permanent molars affected by molar-incisor hypomineralization: A randomized clinical trial. BMC Oral Health 2022, 22, 275. [Google Scholar] [CrossRef]
- de Souza, J.F.; Fragelli, C.B.; Jeremias, F.; Paschoal, M.A.B.; Santos-Pinto, L.; de Cássia Loiola Cordeiro, R. Eighteen-month clinical performance of composite resin restorations with two different adhesive systems for molars affected by molar incisor hypomineralization. Clin. Oral Investig. 2017, 21, 1725–1733. [Google Scholar] [CrossRef] [PubMed]
- Rolim, T.Z.C.; da Costa, T.R.F.; Wambier, L.M.; Chibinski, A.C.; Wambier, D.S.; da Silva Assunção, L.R.; de Menezes, J.V.B.N.; Feltrin-Souza, J. Adhesive restoration of molars affected by molar incisor hypomineralization: A randomized clinical trial. Clin. Oral Investig. 2021, 25, 1513–1524. [Google Scholar] [CrossRef]
- Linner, T.; Khazaei, Y.; Bücher, K.; Pfisterer, J.; Hickel, R.; Kühnisch, J. Comparison of four different treatment strategies in teeth with molar-incisor hypomineralization-related enamel breakdown-A retrospective cohort study. Int. J. Paediatr. Dent 2020, 30, 597–606. [Google Scholar] [CrossRef]
- Weber, K.R.; Wierichs, R.J.; Meyer-Lueckel, H.; Flury, S. Restoration of teeth affected by molar-incisor hypomineralisation: A systematic review. Swiss Dent. J. 2021, 131, 988–997. [Google Scholar] [CrossRef] [PubMed]

| PubMed | Scopus | Cochrane | Web of Science |
|---|---|---|---|
| (mottled enamel OR nonendemic mottling of enamel OR internal enamel hypoplasia OR cheese molars OR non-fluoride enamel opacities OR idiopathic enamel opacities OR enamel hypomineralization OR enamel hypomineralisation OR hypomineralized molars OR hypomineralised molars OR molar incisor hypomineralization OR molar incisor hypomineralisation OR MIH [MeSH Terms]) AND (bond strength OR bonding OR retention OR survival OR longevity OR infiltration [MeSH Terms]) | molar AND incisor AND hypomineralization AND therapy [title abstract keyword] | molar incisor hypomineralization [title abstract keyword] | molar incisor hypomineralization (All Fields) AND therapy (All Fields) |
| Authors, Year | Journal | Study Design | Number of Patients (Age Range) | Number of Teeth | Severity of Hypomineralization | Group 1 | Group 2 | Pretratment | Final Margins | Protocol G1 | Protocol G2 | Materials Used | Follow Up Period | Survival Rate | Results | Authors’ Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hakmi, A. & Dashash, M.—2023 [41]. | BDJ Open | Randomized clinical controlled trial | 20 children, aged 7–11 years | 40 (20 G1 and 20 G2) | SEVERE MIH according to EAPD classification (demarcated enamel opacities with breakdown and caries, spontaneous and persistent hypersensitivity affecting function e.g., brushing, mastication) that could be restored. | Self-Etch | Total-Etch | All prepared walls were wiped with cotton moistened in sodium hypochlorite 5.25% before applying the acid etch and bond [41]. | The final margins of the preparation were placed on a sound enamel. | Teeth were cleaned after completing the preparation, and then the impressions were taken for both jaws using an additional silicone rubber impression material. The impression was cast using yellow gypsum to obtain gypsum samples. Resin composite resin was applied to the gypsum samples in layering technique after they were isolated using silica, as the thickness of one layer does not exceed 2 mm, then each layer was light cured separately for 20 s. The finishing and polishing process was performed. using Fine and extra fine diamond burs, and then rubber points were applied until a smooth and polished surface was obtained. The inner surfaces of the restoration were sandblasted using air abrasion with 50 μm aluminum oxide, then silane was applied to the inner surface of the restoration with gentle air. A self-adhesive dual-cure resin cement was applied using light-cured for 40 s from all sides to ensure that the light reached the full thickness of the resin cement [41]. | The phosphoric acid 37% was applied to the enamel for 15 s, then to the enamel and dentin for 15 s, followed by thoroughly rinsing under running water for 10 s and dried with a gentle air. The single bond was placed on the enamel and was light cured for 20 s with a diode light. The resin composite was applied in a layering technique, as the thickness of one layer does not exceed 2 mm, then each layer was light cured separately for 20 s. The finishing and polishing process was done using Fine and extra fine diamond burs, and then rubber points were applied until a smooth and polished surface was obtained [41]. | Light-emitting diode lightcuring unit (Elipar Freelight II, 3M ESPE) G1: additional silicone rubber impression material (Neosilk, Calmed Invest Kft, Busan, Korea), silane (Ceramic Bond Silane, Voco), selfadhesive dual-cure resin cement (Breeze-Pentron Clinical). G2: phosphoric acid 37% (3 M Universal Etchant, 3 M/Oral Care, USA), single bond (3 M/ESPE), resin composite (Filtek 350, 3M ESPE, St Paul, MN, USA) [41]. | 3, 6, and 12 months | Kaplan–Meier survival analysis; Modified USHPH criteria. | The clinical success rate was 90% in the group 1 versus 85% in the group 2 after 12 months of follow-up without statistically significant differences (p = 0.218). | Both groups can be considered effective restorations with acceptable clinical performance in the restoration of hypomineralised first permanent molars [41]. |
| Özgür, B.; et al.—2022 [42]. | BMC Oral Health | Randomized clinical trial | 39 children, aged 6–12 years | 100 (50 G1 and 50 G2) | MILD MIH with occlusal defects (demarcated white, yellow or brown lesions), sound surfaces and no incipient enamel caries. | Total-etch | Self-etch | Non-fuoridated paste [42]. | Enamel affected by MIH was not removed. | A dental isolation device was used throughout the procedures. the occlusal surfaces were etched with 37% phosphoric acid for 30 s, rinsed with air–water spray for 30 s and dried with oil-free air for 15 s. Proper etching was confirmed by a dull frosty-white appearance of the enamel. The resin sealant applied into the occlusal fissures was light-cured with 460–500 nm wavelength halogen light unit for 20 s. The surfaces were checked with an explorer to ensure that no voids were present. The occlusion was checked and, if necessary, adjusted [42]. | A dental isolation device was used throughout the procedures. The self-etch primer was applied to the occlusal fissures with a fine microbrush. After waiting for 5 s, and homogenizing the bond layer with gentle air stream for 5 s, the giomer sealant was placed and light-cured for 20 s. The surfaces were checked with an explorer to ensure that no voids were present. The occlusion was checked and, if necessary, adjusted [42]. | Dental isolation device (Mr. Tisty One Step, Zirc Dental, Bufalo, MN, USA), light-cured with 460–500 nm wavelength halogen light unit (Hilux Dental Curing Light Unit 250, Benlioğlu Dental Inc, Turkey). G1: 37% phosphoric acid for 30 s (i-GEL N, i-dental, Lithuania), resin sealant (Conceal F, SDI, Australia). G2: self-etch primer (BeautiSealant Primer, Shofu, Japan), giomer sealant (BeautiSealant Paste, Shofu, Japan) [42]. | 1, 3, 6 and 12 months | Long-rank test and Kaplan–Meier survival analysis; Modified USHPH criteria. | At 12 months, the retention rates in Group 1 and Group 2 were 68% and 8%, respectively (p = 0.000). The cumulative survival rates of G1 were significantly higher than G2 for all follow-up visits (p < 0.05). The average survival time was found as 10.46 ± 3.21 months in Group 1 and 4.02 ± 4.43 months in Group 2. | The conventional resin-based sealants yielded a better clinical performance over the 12-month evaluation period than the giomer sealants which were applied with self-etch primer. The high failure rate observed in giomer sealants could be explained by the possible deficiency in the etching capacity of self-etch primer on MIH affected teeth [42]. |
| de Souza, J.F.; et al.—2017 [43]. | Clin Oral Investig | Randomized clinical trial | 18 children, aged 6–8 years | 41 (19 G1 and 22 G2) | SEVERE MIH classified as enamel posteruptive breakdown (PEB) or unsatisfactory atypical restoration (UATR), with or without carious lesions. | Self-etch | Total-etch | 1 month of fluoride varnish application with cotton roll isolation. After it, infiltrative anaesthesia, rubber dam, caries removal with low speed, 1% chlorhexidine application, protection of the dentin-pulp complex with calcium hydroxide if necessary, temporary restoration with Ketac. After 2 months, the teeth were randomly divided into two groups that received the definitive restoration [43]. | Not specificated. | The SEA teeth were restored according to the following operative sequence: prophylaxis, infiltrative anesthesia, rubber dam, partial removal of GIC, primer application using an applicator (20 s), air jet (5 s) from 10-cm distance with 45° angle of the tip, adhesive application (5 s) using an applicator. After application of the dentin adhesive using an applicator, Filtek Z350 XT was inserted in increments of 1.0–1.5 mm, and each increment was polymerized for 40 s, followed by removal of rubber dam, examination of occlusal contact, and final polishing [43]. | The TEA teeth underwent the following clinical steps: prophylaxis, infiltrative anesthesia, rubber dam, partial removal of GIC, application of 37.5% phosphoric acid to enamel (30 s) and dentine (15 s), extensive washing, drying with cotton and air jet (5 s) from 10-cm distance with 45° angle of the tip, priming (5 s) using a applicator, air jet (5 s) from 10-cm distance with 45° angle of the tip, adhesive application (5 s) using an applicator, light curing (20 s), restoration with Filtek Z350 XT inserted in increments of 1.0–1.5 mm, where each increment was polymerized for 40 s, removal of rubber dam, examination of occlusal contact, and final polishing [43]. | Filtek XT350 restoration (3M ESPE, St. Paul, MN, USA), SEA (Clearfil SE Bond, Kuraray Medical, Tokyo, Japan), TEA (Adper Scotchbond Multi-Purpose, 3M ESPE, St. Paul, MN, USA), a light-curing unit (Elipar FreeLight 2, 3M ESPE) with 500 mW/cm2 intensisty. Fluoride varnish application (Duraphat, Colgate, New York, NY, USA). Ketac Molar Easymix (3M ESPE, St. Paul, MN, USA) [43]. | 1, 6, 12, and 18 months | Long-rank MantelCox test; Modified USHPH criteria. | The cumulative survival rates were 100% at 1 month, 89% at 6 months, 73% at 12 months, and 68% at 18 months in SEA, and 95% at 1 month, 72% at 6 months, 59% at 12 months, and 54% at 18 months in TEA. | There was no difference in clinical survival of restorations in FPMs affected by MIH using TEA or SEA adhesives [43]. |
| Rolim, T.Z.C.; et al.—2021 [44]. | Clin Oral Investig | Randomized clinical trial | 35 children, aged 7–16 years | 64 (37 G1 and 37 G2) | Different manifestations of MIH. | Total-etch | Self-etch | Prophylaxis was performed using pumice stone and water prior to the restorative treatment [44]. | Hypomineralized enamel removal was selective—removal of the hypomineralized enamel with an opaque appearance, which crumbles on contact with the instruments until more resistant enamel is obtained. | Local anesthesia with 5% Emla topical cream and then local infiltration anesthesia with 2% mepivacaine. Absolute isolation was performed using clamps and rubber dam. The carious tissue was removed with a dental excavator. Thus, the soft decayed dentin was completely removed using a sharp excavator following the principles of minimum intervention dentistry. In the TE group, ultra-etch 35% phosphoric acid was used for etching the enamel (30 s) and dentin (15 s) and the cavity was washed thoroughly with water and dried with a sterile cotton ball. The adhesive was actively applied with a microbrush for 10 s and air blasting was used for 10 s at a distance of 15 cm from the cavity. The same steps were repeated, adding curing light for 20 s with low power. Restorations in both groups were made with Tetric N-Ceram bulk-fill composite resin in a single increment (up to 5 mm) with light curing for 20 s at a high power at a distance of 9 mm from the material. Occlusal adjustments, finishing, and polishing of the restorations were performed after removing the absolute insulation [44]. | Local anesthesia with 5% Emla topical cream and then local infiltration anesthesia with 2% mepivacaine. Absolute isolation was performed using clamps and rubber dam. The carious tissue was removed with a dental excavator. Thus, the soft decayed dentin was completely removed using a sharp excavator following the principles of minimum intervention dentistry. The adhesive was actively applied with a microbrush for 10 s and air blasting was used for 10 s at a distance of 15 cm from the cavity. The same steps were repeated, adding curing light for 20 s with low power. Restorations in both groups were made with Tetric N-Ceram bulk-fill composite resin in a single increment (up to 5 mm) with light curing for 20 s at a high power at a distance of 9 mm from the material. Occlusal adjustments, finishing, and polishing of the restorations were performed after removing the absolute insulation [44]. | Ultra-etch 35% phosphoric acid (Ultradent, USA), Universal Ambar adhesive (FGM Brazil), Tetric N-Ceram Bulk Fill composite resin (Ivoclar Vivadent, Liechtenstein). Light Bluephase N (Bluephase N, IvoclarVivadent, Austria) [44]. | 1, 6, and 12 months | Long-rank test and Kaplan–Meier survival analysis; Modified USHPH criteria. | A total of 64 FPMs were restored (TE = 33; SE = 31). Survival rates were 96.9% (TE) and 96.7% (SE) after 1 month, 90.5% (TE) and 80.6% (SE) after 6 months, and 80.8% (TE) and 62.3% (SE) after 12 months (p > 0.05). | Both restorative protocols presented similar longevity [44]. |
| Linner, T.; et al.—2020 [45]. | Int J Paediatr Dent | A retrospective cohort study | 52 children, mean age 11.2 years | 153 (126 G1 and 27 G2) | MILD and SEVERE MIH: Disintegration of hard tissue with small- to mediumsized defect (G1) and disintegration of hard tissue with small- to large-sized defects (G2). | Self-etch | Total-etch | Not indicated [45]. | Removal of MIH tissue for G2 and no-removal of MIH tissue for G1. | No local or general anaesthesia; Tooth cleaning, no cavity preparation, cotton roll isolation, self-etching adhesive, application and light polymerization of flowable composite and occlusion control [45]. | No, local or general anaesthesia in relation to patients’ cooperation and treatment needs; Tooth cleaning, removal of MIH tissue, preparation of cavity margins, cotton roll isolation, total etch and total bond, composite application, light polymerization, and occlusion control [45]. | G1: adhesive bonding agent (Adper Prompt L-Pop or Scotchbond Universal L-Pop, 3M Deutschland GmbH) and composite material (Tetric EvoFlow, Ivoclar Vivadent AG, Schaan, Liechtenstein). G2: adhesive bonding agent (Syntac Classic, Ivoclar Vivadent AG, Schaan, Liechtenstein) and composite restorations (Tetric EvoCeram, Ivoclar Vivadent AG, Schaan, Liechtenstein) [45]. | For a mean of 42.9 month | Kaplan-Meier estimators and the Cox regression model. | The cumulative survival probabilities after 12 months were 68% in G1 and 95% in G2 in Kaplan-Meier survival curves. They differed significantly in the regression analysis. | Conventional restorations (G2) were associated with moderate-to-high survival rates in MIH teeth. In contrast, non-invasive composite restorations (G1), which were predominately used in younger or less cooperative children, were linked to lower survival rates [45]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Amario, M.; Vitocco, E.; Jahjah, A.; Capogreco, A.; Mauro, S.; D’Arcangelo, C.; De Angelis, F. Comparative Survival of Restorations in MIH-Affected Pediatric Teeth Using Total-Etch Versus Self-Etch Adhesive Systems: A Systematic Review and Meta-Analysis. Appl. Sci. 2025, 15, 12445. https://doi.org/10.3390/app152312445
D’Amario M, Vitocco E, Jahjah A, Capogreco A, Mauro S, D’Arcangelo C, De Angelis F. Comparative Survival of Restorations in MIH-Affected Pediatric Teeth Using Total-Etch Versus Self-Etch Adhesive Systems: A Systematic Review and Meta-Analysis. Applied Sciences. 2025; 15(23):12445. https://doi.org/10.3390/app152312445
Chicago/Turabian StyleD’Amario, Maurizio, Elena Vitocco, Ali Jahjah, Antonio Capogreco, Stefania Mauro, Camillo D’Arcangelo, and Francesco De Angelis. 2025. "Comparative Survival of Restorations in MIH-Affected Pediatric Teeth Using Total-Etch Versus Self-Etch Adhesive Systems: A Systematic Review and Meta-Analysis" Applied Sciences 15, no. 23: 12445. https://doi.org/10.3390/app152312445
APA StyleD’Amario, M., Vitocco, E., Jahjah, A., Capogreco, A., Mauro, S., D’Arcangelo, C., & De Angelis, F. (2025). Comparative Survival of Restorations in MIH-Affected Pediatric Teeth Using Total-Etch Versus Self-Etch Adhesive Systems: A Systematic Review and Meta-Analysis. Applied Sciences, 15(23), 12445. https://doi.org/10.3390/app152312445