Fracture Toughness of CAD/CAM Resin-Based Materials vs. Direct Composite Resins: A Scoping Review
Featured Application
Abstract
1. Introduction
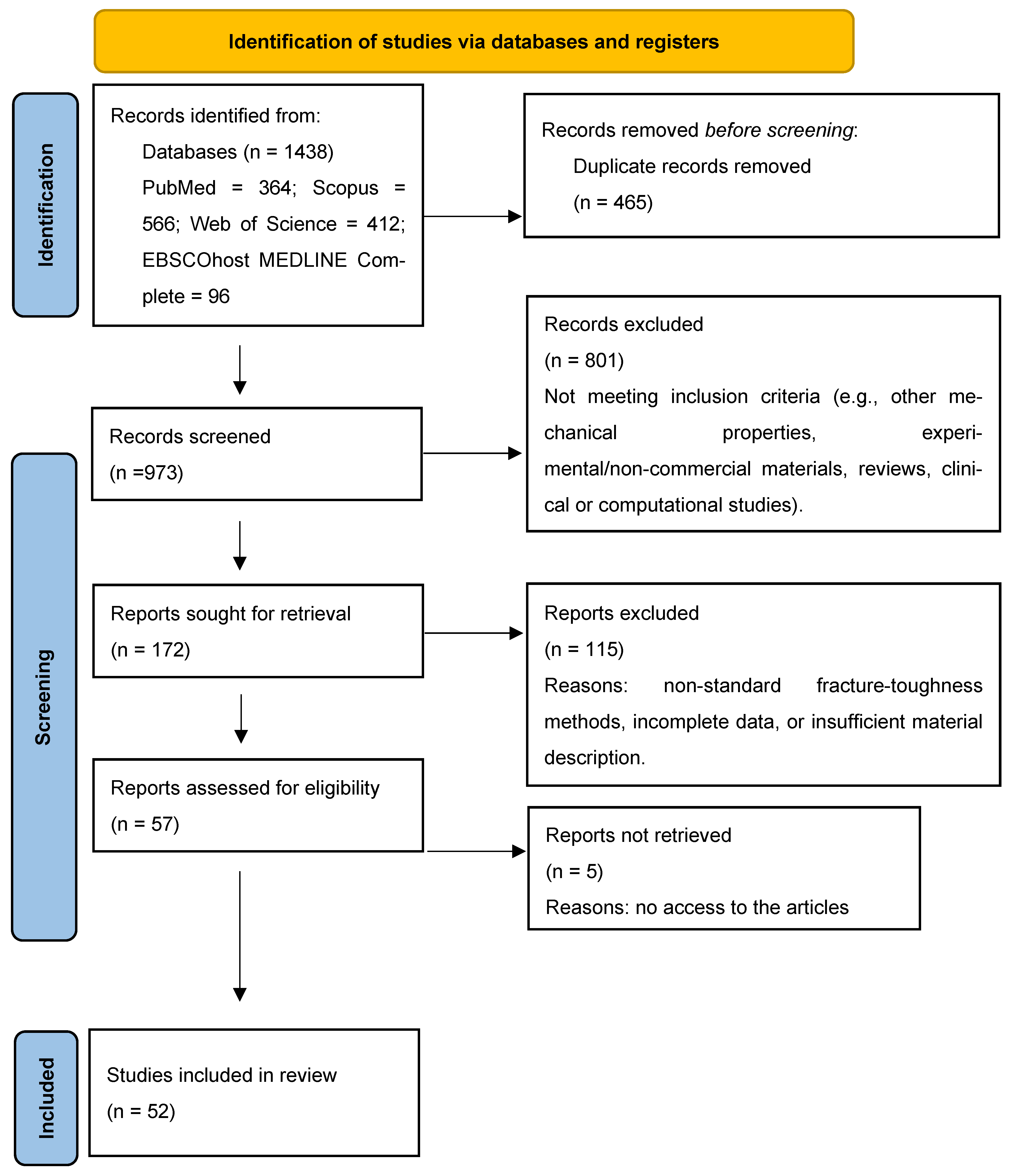
2. Materials and Methods
2.1. Sources and Search Strategy
2.2. Selection, Inclusion, and Exclusion Criteria
2.3. Data Extraction
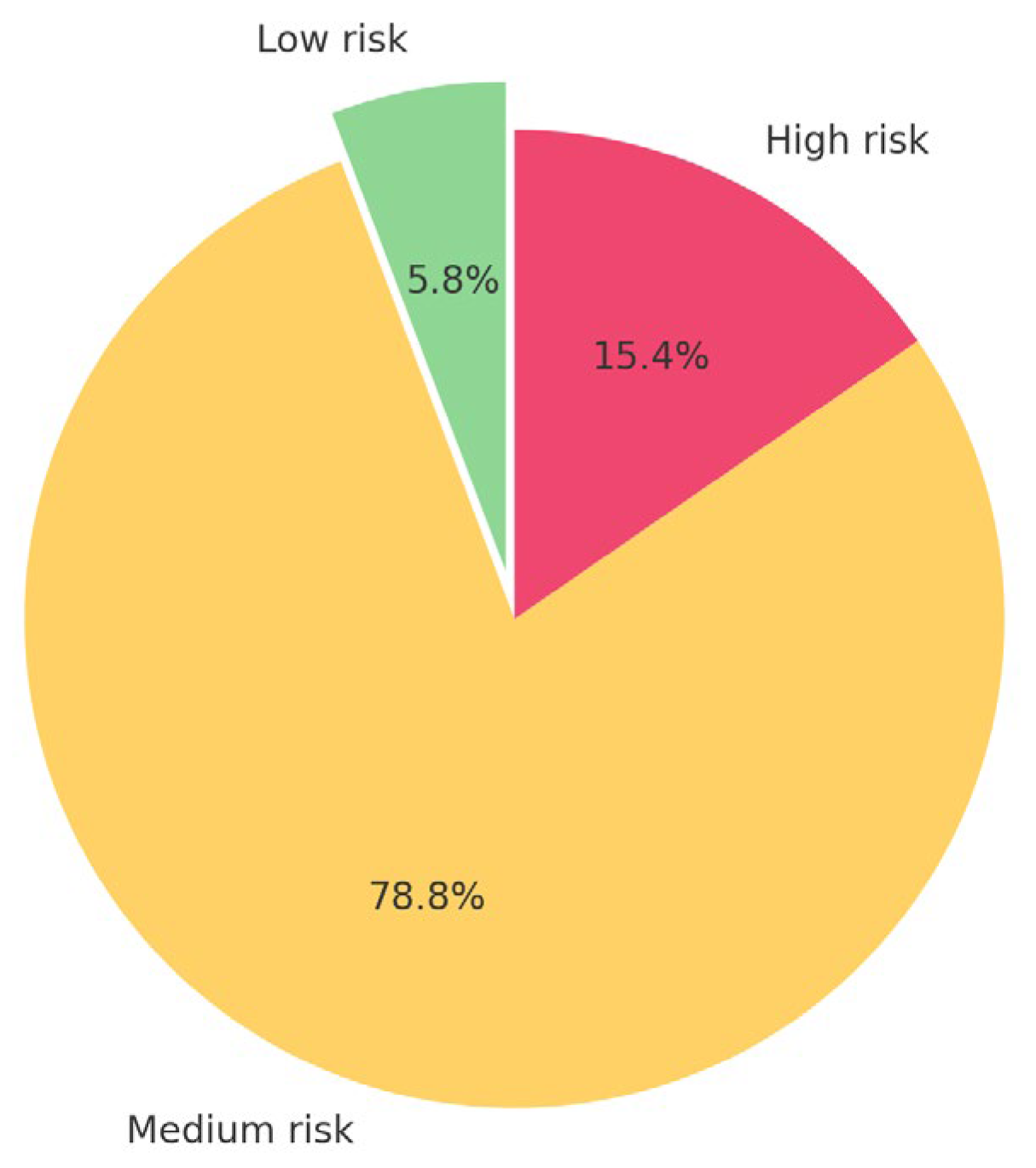
2.4. Risk of Bias Assessment
2.5. Studies Included in the Study
3. Results
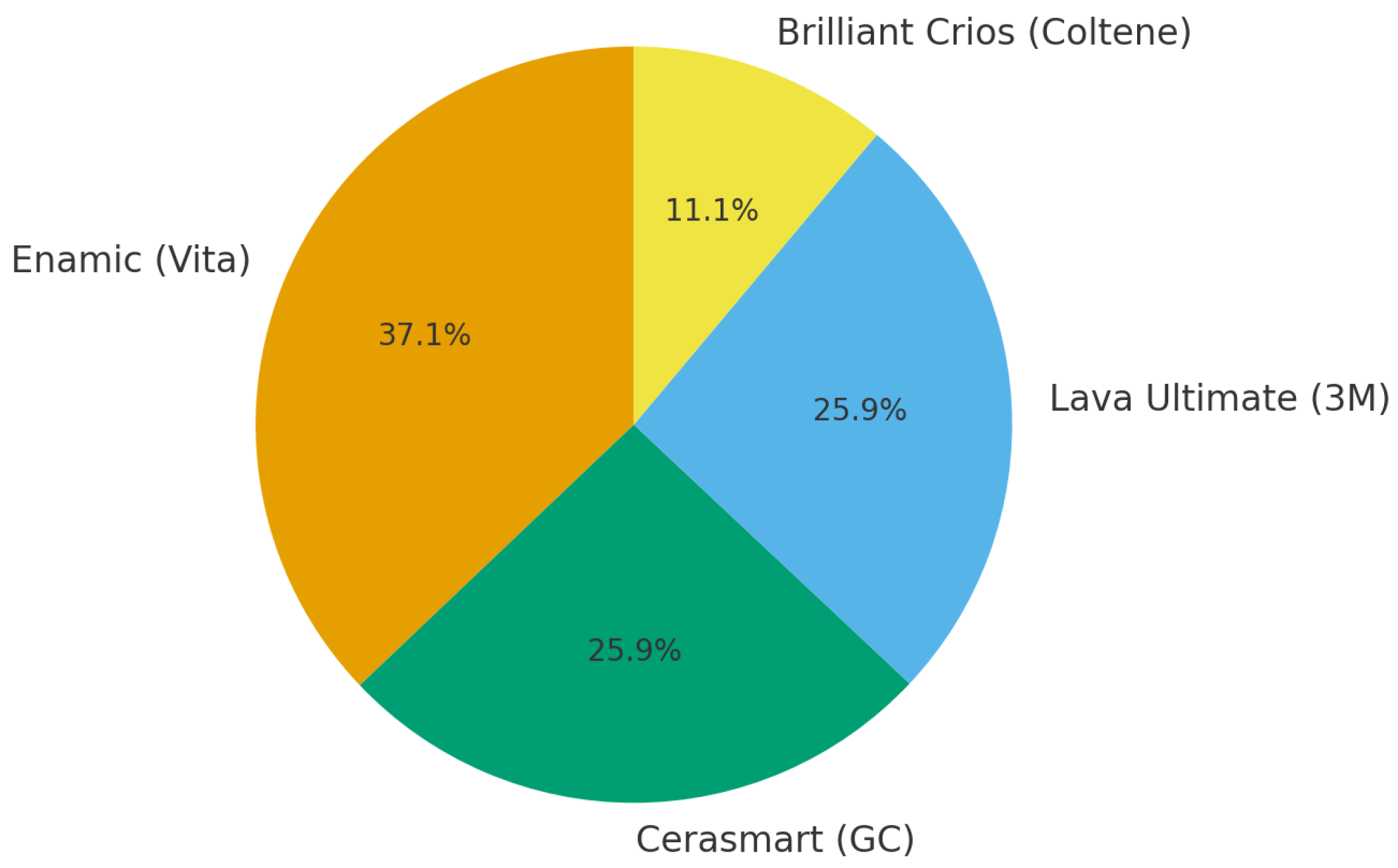
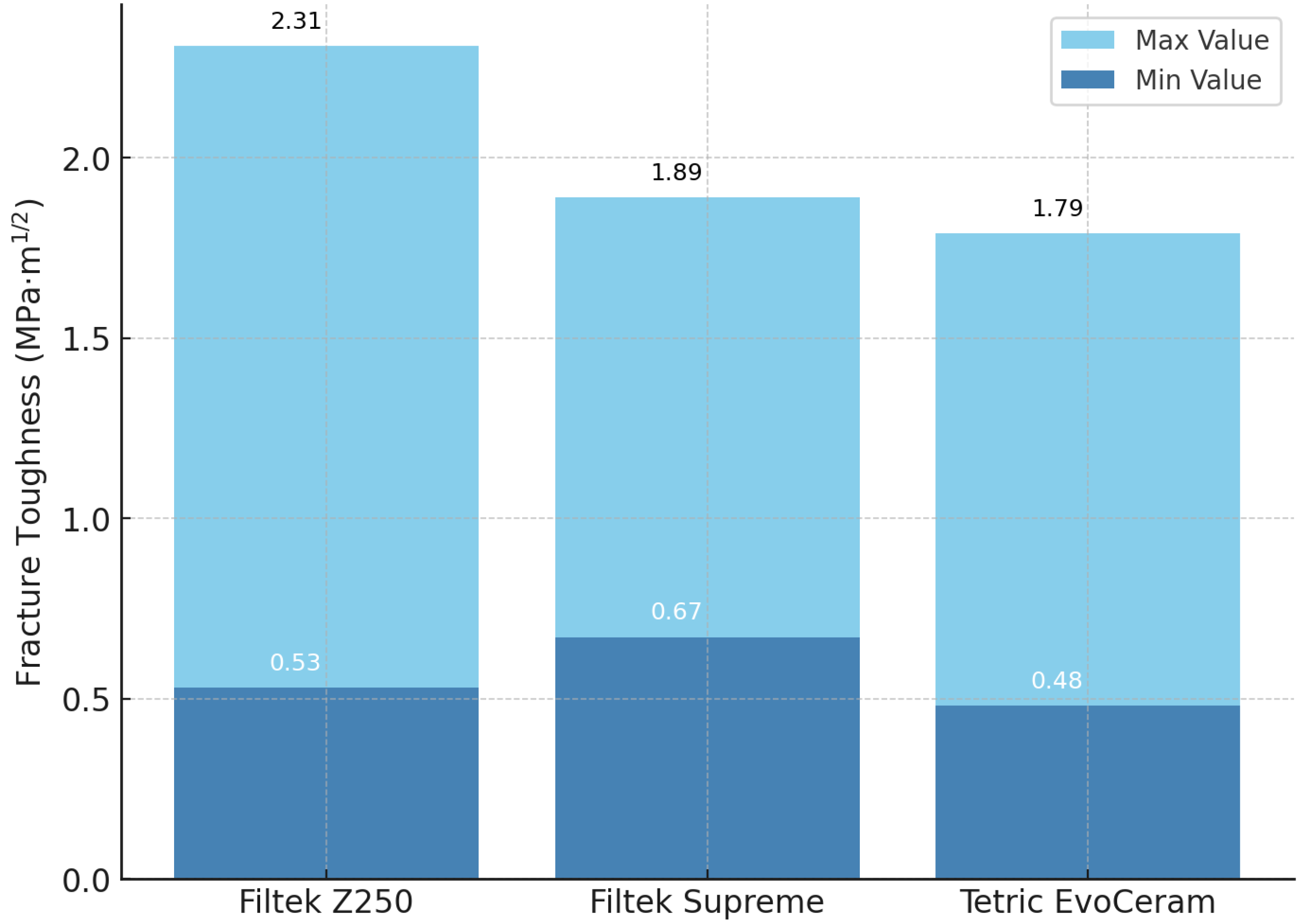
3.1. Descriptive Statistics
3.2. Subgroup Analysis by Material Type
3.3. Effect of Testing Method and Environment
3.4. Risk of Bias Summary
3.5. Summary of Results
4. Discussion
4.1. Fracture Toughness Tests
4.2. Materials for CAD/CAM Restorations
4.3. Crack Propagation and Inorganic Fillers
4.4. Crack Propagation in PICN
4.5. Influence of Resin Matrix and Composite Formulation
4.6. Fracture Toughness and Clinical Performance of CAD/CAM Materials
4.7. Limitations of the Review
4.8. Clinical Implications and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CAD CAM | Computer-assisted design computer-assisted manufacture |
| SENB | Single-edge notched specimen |
| CT | Compact tension specimen |
| NP | Notchless triangular prism |
| K_IC | Fracture Toughness |
| BisGMA | bisphenol A-glycidyl methacrylate |
| TEGDMDA | Triethylene glycol dimethacrylate |
| UDMA | Urethane dimethacrylate |
| SENB | Single-edge notched bending |
| SENVB | Single-edge notched bending with a V-shaped notch |
| ASTM | American Society for Testing and Materials |
Appendix A. Abbreviated Form for Risk of Bias According to QUIN Tool
| Author Year | Risk of Bias |
|---|---|
| 1. Abdulhameed 2020 [40]. | medium |
| 2. Alshabib 2019 [42]. | medium |
| 3. Attik 2022 [44]. | medium |
| 4. Bijelic-Donova 2016a [46]. | medium |
| 5. Bijelic-Donova 2016b [47]. | medium |
| 6. Bonilla 2000 [48]. | medium |
| 7. Bonilla 2003 [50]. | medium |
| 8. Cho 2009 [51]. | medium |
| 9. Choi 2000 [52]. | medium |
| 10. Engelhardt 2016 [53]. | medium |
| 11. Garoushi 2013 [54]. | high |
| 12. Garoushi 2024 [55]. | medium |
| 13. Jun 2013 [56]. | medium |
| 14. Ilie 2012 [57]. | medium |
| 15. Ilie 2021 [58]. | medium |
| 16. Kamourieh 2024 [19]. | low |
| 17. Kim 2002b [60]. | medium |
| 18. Kim 2002b [61]. | high |
| 19. Knobloch 2002 [59]. | high |
| 20. Lassila 2019 [62]. | medium |
| 21. Lassila 2020 [63]. | medium |
| 22. Lien 2010 [64]. | medium |
| 23. Lin 2009 [65]. | medium |
| 24. Lohbauer 2020 [67]. | medium |
| 25. Manhart 2000 [68]. | medium |
| 26. Mese 2016 [69]. | medium |
| 27. Nakade 2024 [71]. | medium |
| 28. Ribeiro 2025 [72]. | low |
| 29. Scherrer 2000 [74]. | high |
| 30. Sochacki 2022 [75]. | medium |
| 31. St-Georges 2003 [76]. | high |
| 32. Thadathil Varghese 2024 [77]. | medium |
| 33. Thomaidis 2013 [78]. | medium |
| 34. Yang 2022 [79]. | medium |
| 35. Yap 2004 [80]. | medium |
| 36. Watanabe 2008 [81]. | medium |
| CAD CAM | |
| 37. Alsarani 2024 [82]. | low |
| 38. Della Bona 2014 [83]. | high |
| 39. Elraggal 2022 [85]. | medium |
| 40. Goujat 2018 [52]. | medium |
| 41. Hampe 2019 [15]. | medium |
| 42. Harada 2015 [16]. | medium |
| 43. Karaer 2020 [88]. | medium |
| 44. Ling 2022 [89]. | medium |
| 45. Lucsanszky 2020 [90]. | medium |
| 46. Moradi 2020 [91]. | medium |
| 47. Nguyen 2012 [92]. | medium |
| 48. Sonmez 2018 [93]. | medium |
| 49. Sulaiman 2022 [94]. | medium |
| 50. Suzaki 2020 [95]. | high |
| 51. Swain 2016 [96]. | high |
| 52. Wendler 2021 [97]. | medium |
References
- Incekara, M.S.; Karadas, M. Clinical comparison of direct and indirect class II composite restorations: A prospective 12-month follow-up study. BMC Oral Health 2025, 25, 1217. [Google Scholar] [CrossRef]
- Da Rosa Rodolpho, P.A.; Donassollo, T.A.; Cenci, M.S.; Loguércio, A.D.; Moraes, R.R.; Bronkhorst, E.M.; Opdam, N.J.; Demarco, F.F. 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent. Mater. 2011, 27, 955–963. [Google Scholar] [CrossRef]
- Ferracane, J.L. Resin-based composite performance: Are there some things we can’t predict? Dent. Mater. 2013, 29, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Spyropoulou, N.; Diamantopoulou, S.; Patrinos, S.; Papazoglou, E. Retrospective Clinical Study of Resin Composite and Ceramic Indirect Posterior Restorations up to 11 Years. Prosthesis 2025, 7, 108. [Google Scholar] [CrossRef]
- François, D.; Pineau, A.; Zaoui, A. Brittle fracture. In Mechanical Behaviour of Materials. Solid Mechanics and Its Applications, Vol. 191; Springer: Dordrecht, The Netherlands, 2013; pp. 103–191. [Google Scholar] [CrossRef]
- Al-Ibrahim, I.; Shono, N.; Al-Saud, L.; Al-Nahedh, H. Five years of restorative resin-based composite advancements: A narrative review. BMC Oral Health 2025, 25, 1061. [Google Scholar] [CrossRef]
- Ilie, N.; Hilton, T.J.; Heintze, S.D.; Hickel, R.; Watts, D.C.; Silikas, N.; Stansbury, J.W.; Cadenaro, M.; Ferracane, J.L. Academy of dental materials guidance-resin composites: Part I-mechanical properties. Dent. Mater. 2017, 33, 880–894. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Ilie, N.; Hickel, R.; Reis, A.; Loguercio, A.; Rousson, V. Laboratory mechanical parameters of composite resins and their relation to fractures and wear in clinical trials—A systematic review. Dent. Mater. 2017, 33, e101–e114. [Google Scholar] [CrossRef]
- Hançer Sarıca, S.; Arslan, S.; Balkaya, H. Comparison of the 2-year clinical performances of class II restorations using different restorative materials. Clin. Oral Investig. 2025, 29, 128. [Google Scholar] [CrossRef] [PubMed]
- Tyas, M.J. Correlation between fracture properties and clinical performance of composite resins in class IV cavities. AustDent J. 1990, 35, 46–49. [Google Scholar] [CrossRef]
- Lehmann, A.; Nijakowski, K.; Jankowski, J.; Donnermeyer, D.; Ramos, J.C.; Drobac, M.; Martins, J.F.B.; Hatipoğlu, Ö.; Omarova, B.; Javed, M.Q.; et al. Clinical difficulties related to direct composite restorations: A multinational survey. Int. Dent. J. 2025, 75, 797–806. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Veerman, A.; Pereira, G.K.R.; Kleverlaan, C.J.; Dal Piva, A.M.d.O. Comparative strength study of indirect permanent restorations: 3D-printed, milled, and conventional dental composites. Clin. Pract. 2024, 14, 1940–1952. [Google Scholar] [CrossRef]
- Ozakar-Ilday, N.; Zorba, Y.O.; Yildiz, M.; Erdem, V.; Seven, N.; Demirbuga, S. Three-year clinical performance of two indirect composite inlays compared to direct composite restorations. Med. Oral Patol. Oral Cir. Bucal 2013, 18, e521–e528. [Google Scholar] [CrossRef] [PubMed]
- Morel, C.; Baranger, E.; Lamon, J.; Braun, J.; Lorrette, C. The influence of internal defects on the mechanical behavior of filament wound SiC/SiC composite tubes under uniaxial tension. J. Eur. Ceram. Soc. 2022, 43, 1797–1807. [Google Scholar] [CrossRef]
- Hampe, R.; Theelke, B.; Lümkemann, N.; Eichberger, M.; Stawarczyk, B. Fracture toughness analysis of ceramic and resin composite CAD/CAM material. Oper. Dent. 2019, 44, E190–E201. [Google Scholar] [CrossRef] [PubMed]
- Harada, A.; Nakamura, K.; Kanno, T.; Inagaki, R.; Örtengren, U.; Niwano, Y.; Sasaki, K.; Egusa, H. Fracture resistance of computer-aided design/computer-aided manufacturing-generated composite resin-based molar crowns. Eur. J. Oral Sci. 2015, 123, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Duarte, S., Jr.; Phark, J.H. Advances in dental restorations: A comprehensive review of machinable and 3D-printed ceramic-reinforced composites. J. Esthet. Restor. Dent. 2025, 37, 257–276. [Google Scholar] [CrossRef]
- Ling, L.; Ma, Y.; Malyala, R. A novel CAD/CAM resin composite block with high mechanical properties. Dent. Mater. 2021, 37, 1150–1155. [Google Scholar] [CrossRef] [PubMed]
- Kamourieh, N.; Faigenblum, M.; Blizard, R.; Leung, A.; Fine, P. Fracture toughness of short fibre-reinforced composites—In vitro study. Materials 2024, 17, 5368. [Google Scholar] [CrossRef]
- Borgia, E.; Baron, R.; Borgia, J.L. Quality and survival of direct light-activated composite resin restorations in posterior teeth: A 5- to 20-year retrospective longitudinal study. J. Prosthodont. 2019, 28, e195–e203. [Google Scholar] [CrossRef]
- Angeletaki, F.; Gkogkos, A.; Papazoglou, E.; Kloukos, D. Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis. J. Dent. 2016, 53, 12–21. [Google Scholar] [CrossRef]
- Azeem, R.A.; Sureshbabu, N.M. Clinical performance of direct versus indirect composite restorations in posterior teeth: A systematic review. J. Conserv. Dent. 2018, 21, 2–9. [Google Scholar]
- McGrath, C.E.; Bonsor, S.J. Survival of direct resin composite onlays and indirect tooth-coloured adhesive onlays in posterior teeth: A systematic review. Br. Dent. J. 2022, 233, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Moussa, C.; Savard, G.; Rochefort, G.; Renaud, M.; Denis, F.; Daou, M.H. Fracture resistance of direct versus indirect restorations on posterior teeth: A systematic review and meta-analysis. Bioengineering 2024, 11, 536. [Google Scholar] [CrossRef]
- Tennert, C.; Maliakal, C.; Suarèz, M.L.; Jaeggi, T.; Meyer-Lueckel, H.; Wierichs, R.J. Longevity of posterior direct versus indirect composite restorations: A systematic review and meta-analysis. Dent. Mater. 2024, 40, e95–e101. [Google Scholar] [CrossRef] [PubMed]
- de Kuijper, M.C.F.M.; Cune, M.S.; Özcan, M.; Gresnigt, M.M.M. Clinical performance of direct composite resin versus indirect restorations on endodontically treated posterior teeth: A systematic review and meta-analysis. J. Prosthet. Dent. 2023, 130, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Elmoselhy, H.A.S.; Hassanien, O.E.S.; Haridy, M.F.; Salam El Baz, M.A.E.; Saber, S. Two-year clinical performance of indirect restorations fabricated from CAD/CAM nano hybrid composite versus lithium disilicate in mutilated vital teeth. A randomized controlled trial. BMC Oral Health 2024, 24, 101. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hassan, A.; Hamdi, K.; Ali, A.I.; Al-Zordk, W.; Mahmoud, S.H. Clinical performance comparison between lithium disilicate and hybrid resin nano-ceramic CAD/CAM onlay restorations: A two-year randomized clinical split-mouth study. Odontology 2024, 112, 601–615. [Google Scholar] [CrossRef]
- El-Din, M.S.; Adel, S.; Naguib, A.; Nabil, O. Evaluation of marginal and internal adaptation of endocrowns fabricated from nano-ceramic hybrid and lithium disilicate ceramic materials: A randomized controlled clinical trial. J. Contemp. Dent. Pract. 2025, 26, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Hofsteenge, J.W.; Fennis, W.M.M.; Kuijs, R.H.; Özcan, M.; Cune, M.S.; Gresnigt, M.M.M.; Kreulen, C.M. Clinical survival and performance of premolars restored with direct or indirect cusp-replacing resin composite restorations with a mean follow-up of 14 years. Dent. Mater. 2023, 39, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Mourouzis, P. Critical methodological factors influencing the accuracy of intraoral scanners in digital dentistry research. Comput. Biol. Med. 2025, 187, 109780. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.5 (Updated August 2024); Cochrane: Houston, TX, USA, 2024; Available online: www.cochrane.org/handbook (accessed on 10 November 2025).
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pineda-Vélez, E.; Yadalam, P.K.; Ardila, C.M. Efficacy of the finite element analysis in assessing the effects of light curing on the mechanical properties of direct restorative composites: A systematic review. J. Clin. Exp. Dent. 2024, 16, e1411–e1421. [Google Scholar] [CrossRef]
- Waffenschmidt, S.; Knelangen, M.; Sieben, W.; Bühn, S.; Pieper, D. Single screening versus conventional double screening for study selection in systematic reviews: A methodological systematic review. BMC Med. Res. Methodol. 2019, 19, 132. [Google Scholar] [CrossRef]
- Furlan, J.C.; Singh, J.; Hsieh, J.; Fehlings, M.G. Methodology of systematic reviews and recommendations. J. Neurotrauma 2011, 28, 1335–1339. [Google Scholar] [CrossRef] [PubMed]
- Tractenberg, R.E.; Yumoto, F.; Jin, S.; Morris, J.C. Sample size requirements for training to a kappa agreement criterion on clinical dementia ratings. Alzheimer Dis. Assoc. Disord. 2010, 24, 264–268. [Google Scholar] [CrossRef]
- Sheth, V.H.; Shah, N.P.; Jain, R.; Bhanushali, N.; Bhatnagar, V. Development and validation of a risk-of-bias tool for assessing in vitro studies conducted in dentistry: The QUIN. J. Prosthet. Dent. 2024, 131, 1038–1042. [Google Scholar] [CrossRef]
- Abdulhameed, N.; Angus, B.; Wanamaker, J.; Mecholsky, J.J., Jr. Quantitative fractography as a novel approach to measure fracture toughness of direct resin composites. J. Mech. Behav. Biomed. Mater. 2020, 109, 103857. [Google Scholar] [CrossRef] [PubMed]
- ISO 13586:2018; Plastics—Determination of Fracture Toughness (GIC and KIC)—Linear Elastic Fracture Mechanics (LEFM) Approach. International Organization for Standardization: Geneva, Switzerland, 2018.
- Alshabib, A.; Silikas, N.; Watts, D.C. Hardness and fracture toughness of resin-composite materials with and without fibers. Dent. Mater. 2019, 35, 1194–1203. [Google Scholar] [CrossRef]
- BS ISO 12135:2021; Metallic Materials—Unified Method of Test for the Determination of Quasistatic Fracture Toughness. British Standards Institution: Milton Keynes, UK, 2021.
- Attik, N.; Colon, P.; Gauthier, R.; Chevalier, C.; Grosgogeat, B.; Abouelleil, H. Comparison of physical and biological properties of a flowable fiber reinforced and bulk filling composites. Dent. Mater. 2022, 38, e19–e30. [Google Scholar] [CrossRef]
- ISO 20795–1:2013; Dentistry—Base Polymers—Part 1: Denture Base Polymers. International Organization for Standardization: Geneva, Switzerland, 2013.
- Bijelic-Donova, J.; Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Mechanical properties, fracture resistance, and fatigue limits of short fiber reinforced dental composite resin. J. Prosthet. Dent. 2016, 115, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Bijelic-Donova, J.; Garoushi, S.; Lassila, L.V.; Keulemans, F.; Vallittu, P.K. Mechanical and structural characterization of discontinuous fiber-reinforced dental resin composite. J. Dent. 2016, 52, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, E.D.; Mardirossian, G.; Caputo, A.A. Fracture toughness of various core build-up materials. J. Prosthodont. 2000, 9, 14–18. [Google Scholar] [CrossRef] [PubMed]
- ASTM-Standard-E399-24; Standard Test Method for Plane Strain Fracture Toughness of Metallic Materials. American Society for Testing and Materials. Annual Book of ASTM Standards: Philadelphia, PA, USA, 2024.
- Bonilla, E.D.; Yashar, M.; Caputo, A.A. Fracture toughness of nine flowable resin composites. J. Prosthet. Dent. 2003, 89, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.D.; Bulpakdi, P.; Matis, B.A.; Platt, J.A. Effect of bleaching on fracture toughness of resin composites. Oper. Dent. 2009, 34, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.K.; Ferracane, J.L.; Hilton, T.J.; Charlton, D. Properties of packable dental composites. J. Esthet. Dent. 2000, 12, 216–226. [Google Scholar] [CrossRef] [PubMed]
- Engelhardt, F.; Hahnel, S.; Preis, V.; Rosentritt, M. Comparison of flowable bulk-fill and flowable resin-based composites: An in vitro analysis. Clin. Oral Investig. 2016, 20, 2123–2130. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Säilynoja, E.; Vallittu, P.K.; Lassila, L. Physical properties and depth of cure of a new short fiber reinforced composite. Dent. Mater. 2013, 29, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Garoushi, S.; Säilynoja, E.; Frater, M.; Keulemans, F.; Vallittu, P.K.; Lassila, L. A comparative evaluation of commercially available short fiber-reinforced composites. BMC Oral Health 2024, 24, 1573. [Google Scholar] [CrossRef]
- Jun, S.K.; Kim, D.A.; Goo, H.J.; Lee, H.H. Investigation of the correlation between the different mechanical properties of resin composites. Dent. Mater. J. 2013, 32, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Hickel, R.; Valceanu, A.S.; Huth, K.C. Fracture toughness of dental restorative materials. Clin. Oral Investig. 2012, 16, 489–498. [Google Scholar] [CrossRef]
- Ilie, N. Microstructural dependence of mechanical properties and their relationship in modern resin-based composite materials. J. Dent. 2021, 114, 103829. [Google Scholar] [CrossRef]
- Knobloch, L.A.; Kerby, R.E.; Seghi, R.; Berlin, J.S.; Clelland, N. Fracture toughness of packable and conventional composite materials. J. Prosthet. Dent. 2002, 88, 307–313. [Google Scholar] [CrossRef]
- Kim, K.H.; Ong, J.L.; Okuno, O. The effect of filler loading and morphology on the mechanical properties of contemporary composites. J. Prosthet. Dent. 2002, 87, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Okuno, O. Microfracture behaviour of composite resins containing irregular-shaped fillers. J. Oral Rehabil. 2002, 29, 1153–1159. [Google Scholar] [CrossRef]
- Lassila, L.; Säilynoja, E.; Prinssi, R.; Vallittu, P.; Garoushi, S. Characterization of a new fiber-reinforced flowable composite. Odontology 2019, 107, 342–352. [Google Scholar] [CrossRef]
- Lassila, L.; Keulemans, F.; Vallittu, P.K.; Garoushi, S. Characterization of restorative short-fiber reinforced dental composites. Dent. Mater. J. 2020, 39, 992–999. [Google Scholar] [CrossRef] [PubMed]
- Lien, W.; Vandewalle, K.S. Physical properties of a new silorane-based restorative system. Dent. Mater. 2010, 26, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Drummond, J.L. Cyclic loading of notched dental composite specimens. Dent. Mater. 2010, 26, 207–214. [Google Scholar] [CrossRef][Green Version]
- ASTM PS070-97; Standard Test Methods for the Determination of Fracture Toughness of Advanced Ceramics at Ambient Temperature. ASTM Standards: Philadelphia, PA, USA, 1997.
- Lohbauer, U.; Belli, R. The Mechanical Performance of a Novel Self-Adhesive Restorative Material. J. Adhes. Dent. 2020, 22, 47–58. [Google Scholar] [CrossRef]
- Manhart, J.; Kunzelmann, K.H.; Chen, H.Y.; Hickel, R. Mechanical properties and wear behavior of light-cured packable composite resins. Dent. Mater. 2000, 16, 33–40. [Google Scholar] [CrossRef]
- Mese, A.; Palamara, J.; Bagheri, R.; Fani, M.; Burrow, M.F. Fracture toughness of seven resin composites evaluated by three methods of mode I fracture toughness (KIC). Dent. Mater. J. 2016, 35, 893–899. [Google Scholar] [CrossRef] [PubMed]
- ASTM D 5045-14 A; Standard Test Methods for Plane-Strain Fracture Toughness and Strain Energy Release Rate of Plastic Materials. ASTM Standards: Philadelphia, PA, USA, 2014.
- Nakade, P.; Thaore, S.; Bangar, B.; Grover, I.; Alharethi, N.; Adsure, G.; Kulkarni, D. Comparative evaluation of fracture toughness and flexural strength of four different core build-up materials: An in vitro study. J. Contemp. Dent. Pract. 2024, 25, 191–195. [Google Scholar] [CrossRef]
- Ribeiro, M.T.H.; Price, R.B.; Michaud, P.L.; Soares, C.J. Physicomechanical properties of resin-based composites photo-polymerized using laser, polywave and quadwave curing lights. Dent. Mater. 2025, 41, 699–707. [Google Scholar] [CrossRef] [PubMed]
- ASTM-E1820-13; Standard Test Method for Measurement of Fracture Toughness. ASTM International: Philadelphia, PA, USA, 2013.
- Scherrer, S.S.; Botsis, J.; Studer, M.; Pini, M.; Wiskott, H.W.; Belser, U.C. Fracture toughness of aged dental composites in combined mode I and mode II loading. J. Biomed. Mater. Res. 2000, 53, 362–370. [Google Scholar] [CrossRef]
- Sochacki, S.; Karczewski, A.; Platt, J.; Roberts, H.W. Effect of post-irradiation polymerization on selected mechanical properties of six direct resins. Dent. Mater. J. 2022, 41, 230–240. [Google Scholar] [CrossRef]
- St-Georges, A.J.; Swift, E.J.; Thompson, J.Y.; Heymann, H.O. Irradiance effects on the mechanical properties of universal hybrid and flowable hybrid resin composites. Dent. Mater. 2003, 19, 406–413. [Google Scholar] [CrossRef]
- Thadathil Varghese, J.; Raju, R.; Farrar, P.; Prentice, L.; Prusty, B.G. Comparative analysis of self-cure and dual cure-dental composites on their physico-mechanical behaviour. Aust. Dent. J. 2024, 69, 124–138. [Google Scholar] [CrossRef] [PubMed]
- Thomaidis, S.; Kakaboura, A.; Mueller, W.D.; Zinelis, S. Mechanical properties of contemporary composite resins and their interrelations. Dent. Mater. 2013, 29, e132–e141. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Silikas, N.; Watts, D.C. Polymerization and shrinkage kinetics and fracture toughness of bulk-fill resin-composites. Dent. Mater. 2022, 38, 1934–1941. [Google Scholar] [CrossRef] [PubMed]
- Yap, A.U.; Chung, S.M.; Chow, W.S.; Tsai, K.T.; Lim, C.T. Fracture resistance of compomer and composite restoratives. Oper. Dent. 2004, 29, 29–34. [Google Scholar]
- Watanabe, H.; Khera, S.C.; Vargas, M.A.; Qian, F. Fracture toughness comparison of six resin composites. Dent. Mater. 2008, 24, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Alsarani, M.M.; Khan, A.A.; Bautista, L.S.J.; Alsunbul, H.; Matinlinna, J.P. Effect of peroxide-free and peroxide-based in-office bleaching on the surface and mechanical properties of CAD/CAM esthetic restorative materials. Eur. J. Oral Sci. 2024, 132, e13016. [Google Scholar] [CrossRef]
- Della Bona, A.; Corazza, P.H.; Zhang, Y. Characterization of a polymer-infiltrated ceramic-network material. Dent. Mater. 2014, 30, 564–569. [Google Scholar] [CrossRef]
- ASTM C 1421-10; Standard Test Methods for Determination of Fracture Toughness of Advanced Ceramics at Ambient Temperature. Annual Book of ASTM Standards: Houston, Texas, USA, 2010.
- Elraggal, A.; Afifi, R.; Abdelraheem, I. Effect of erosive media on microhardness and fracture toughness of CAD-CAM dental materials. BMC Oral Health. 2022, 22, 191. [Google Scholar] [CrossRef]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Mechanical properties and internal fit of 4 CAD-CAM block materials. J. Prosthet. Dent. 2018, 119, 384–389. [Google Scholar] [CrossRef] [PubMed]
- ISO-6872:2008; International Organization for Standardization. Dentistry Ceramic Materials. International Organization for Standardization: Geneva, Switzerland, 2008.
- Karaer, O.; Yamaguchi, S.; Nakase, Y.; Lee, C.; Imazato, S. In silico non-linear dynamic analysis reflecting in vitro physical properties of CAD/CAM resin composite blocks. J. Mech. Behav. Biomed. Mater. 2020, 104, 103697. [Google Scholar] [CrossRef] [PubMed]
- Ling, L.; Lai, T.; Malyala, R. Fracture toughness and brittleness of novel CAD/CAM resin composite block. Dent. Mater. 2022, 38, e308–e317. [Google Scholar] [CrossRef]
- Lucsanszky, I.J.R.; Ruse, N.D. Fracture toughness, flexural strength, and flexural modulus of new CAD/CAM resin composite blocks. J. Prosthodont. 2020, 29, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Moradi, Z.; Abbasi, M.; Khalesi, R.; Tabatabaei, M.H.; Shahidi, Z. Fracture toughness comparison of three indirect composite resins using 4-point flexural strength method. Eur. J. Dent. 2020, 14, 212–216. [Google Scholar] [CrossRef][Green Version]
- Nguyen, J.F.; Migonney, V.; Ruse, N.D.; Sadoun, M. Resin composite blocks via high-pressure high-temperature polymerization. Dent. Mater. 2012, 28, 529–534. [Google Scholar] [CrossRef]
- Sonmez, N.; Gultekin, P.; Turp, V.; Akgungor, G.; Sen, D.; Mijiritsky, E. Evaluation of five CAD/CAM materials by microstructural characterization and mechanical tests: A comparative in vitro study. BMC Oral Health 2018, 18, 5. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Suliman, A.A.; Mohamed, E.A.; Rodgers, B.; Altak, A.; Johnston, W.M. Mechanical properties of bisacryl-, composite-, and ceramic-resin restorative materials. Oper. Dent. 2022, 47, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Suzaki, N.; Yamaguchi, S.; Hirose, N.; Tanaka, R.; Takahashi, Y.; Imazato, S.; Hayashi, M. Evaluation of physical properties of fiber-reinforced composite resin. Dent. Mater. 2020, 36, 987–996. [Google Scholar] [CrossRef]
- Swain, M.V.; Coldea, A.; Bilkhair, A.; Guess, P.C. Interpenetrating network ceramic-resin composite dental restorative materials. Dent. Mater. 2016, 32, 34–42. [Google Scholar] [CrossRef]
- Wendler, M.; Stenger, A.; Ripper, J.; Priewich, E.; Belli, R.; Lohbauer, U. Mechanical degradation of contemporary CAD/CAM resin composite materials after water ageing. Dent. Mater. 2021, 37, 1156–1167. [Google Scholar] [CrossRef]
- ISO-10477:1992; International Organization for Standardization. Dentistry Polymer-Based Crown and Bridge Materials. International Organization for Standardization: Geneva, Switzerland, 1992.
- Fujishima, A.; Ferracane, J.L. Comparison of four modes of fracture toughness testing for dental composites. Dent. Mater. 1996, 12, 38–43. [Google Scholar] [CrossRef]
- Lange, F.F.; Radford, K.C. Fracture energy of an epoxy composite system. J. Mater. Scie 1971, 10, 1197. [Google Scholar] [CrossRef]
- Kim, K.H.; Park, J.H.; Imai, Y.; Kishi, T. Microfracture mechanisms of dental resin composites containing spherically shaped filler particles. J. Dent. Res. 1994, 73, 499. [Google Scholar] [CrossRef] [PubMed]
- Ikejima, I.; Nomoto, R.; McCabe, J.F. Shear punch strength and flexural strength of model composites with varying filler volume fraction, particle size and silanation. Dent. Mater. 2003, 19, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef]
- Lloyd, C.H.; Mitchell, L. The fracture toughness of tooth coloured restorative materials. J. Oral Rehabil. 1984, 11, 257–272. [Google Scholar] [CrossRef] [PubMed]
- Asmussen, E.; Peutzfeldt, A. Influence of UEDMA BisGMA and TEGDMA on selected mechanical properties of experimental resin composites. Dent. Mater. 1998, 14, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, N.A.; Wakasa, K.; Priyawan, R.; Yamaki, M. Dental application of binary urethane monomer mixtures:strengthened resin matrix. J. Mater. Sci. Mater. Med. 1997, 8, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Yuen, J.J.X.; Saw, Z.K.; Chua, H.S.; Beh, Y.H. Clinical behavior and survival of CAD-CAM resin nanoceramic and polymer interpenetrating ceramic network material restorations on endodontically treated teeth: A systematic review and meta-analysis. J. Prosthet. Dent. 2025, 133, e1–e1437. [Google Scholar] [CrossRef]
- Fasbinder, D.J.; Neiva, G.F.; Heys, D.; Heys, R. Clinical evaluation of chairside Computer Assisted Design/Computer Assisted Machining nano-ceramic restorations: Five-year status. J. Esthet. Restor. Dent. 2020, 32, 193–203. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Scholz, K.J.; Strub, J.R.; Vach, K.; Gierthmuehlen, P.C. Polymer-infiltrated ceramic CAD/CAM inlays and partial coverage restorations: 3-year results of a prospective clinical study over 5 years. Clin. Oral Investig. 2018, 22, 1973–1983. [Google Scholar] [CrossRef]
- Bustamante-Hernández, N.; Montiel-Company, J.M.; Bellot-Arcís, C.; Mañes-Ferrer, J.F.; Solá-Ruíz, M.; Agustín-Panadero, R.; Fernández-Estevan, L. Clinical behavior of ceramic, hybrid and composite onlays. A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 7582. [Google Scholar] [CrossRef] [PubMed]
- Rocha Gomes Torres, C.; Caroline Moreira Andrade, A.; Valente Pinho Mafetano, A.P.; Stabile de Abreu, F.; de Souza Andrade, D.; Cintra Mailart, M.; Aun de Barros Lima Rocha Campello de Souza, M.L.; Guimarães Alarça Nunes, L.; Ariel Rodrigues de Araújo, C.; Di Nicoló, R.; et al. Computer-aided design and computer-aided manufacturer indirect versus direct composite restorations: A randomized clinical trial. J. Esthet. Restor. Dent. 2022, 34, 776–788. [Google Scholar] [CrossRef] [PubMed]
| Author Year of Publication | Composite Resin | Light Curing Unit | Curing Mode | Irradiance (mW/cm2) | Exposure Time (s) | Number of Specimens | Methodology | Fracture Toughness |
|---|---|---|---|---|---|---|---|---|
| 1. Abdulhameed, 2020 [40] | Tetric EvoCeram Tetric EvoCeram Bulk Fill Tetric EvoFlow Tetric EvoFlow Bulk Fill (IVOCLAR/VIVADENT) | IVOCLAR/VIVADENT Bluephase Style | Polywave | 1000 | 10 | 8 | SENB ASTM D 5045-14 [41] | 0.48 (0.15) 0.53 (0.13) 0.68 (0.7) 0.80 (0.15) |
| 2. Alshabib, 2019 [42] | NovaPro Universal, (NANOVA INC.) NovaPro Flow, (NANOVA INC.), ever X Posterior, (GC) Filtek Supreme XTE (3M/ESPE) Filtek Supreme XTE Flowable (3M/ESPE) Filtek Bulk fill (3M/ESPE) | Elipar S10 | NR | 1200 | 6 × 20 overlapping | 12 | SENB British Standard 12135:2021 [43] | 1.23 (0.14) 0.96 (0.09) 2.14 (0.16) 1.37 (0.23) 0.97 (0.08) 1.46 (0.17) 1.45 (0.09) |
| 3. Attik, 2022 [44] | everX Flow, (GC) Filtek Bulk Fill Posterior Restorative SDR Flow+ | Elipar DeepCure S | NR | No data available | No data available | 8 | ISO 20795-1 [45] | 2.55 1.87 1.92 |
| 4. Bijelic-Donova, 2016a [46] | everX Posterior (GC) G-ænial anterior (GC) | Elipar S10 | Monowave | 1600 | 5 × 20 overlapping | 10 | SENB ISO 20795-1 [45] | 2.6 1.03 |
| 5. Bijelic-Donora, 2016b [47] | everX Posterior (GC) G-ænial Anterior (GC) Filtek Supreme XTE (3M/ESPE) Filtek Bulk Fill (3M/ESPE) | Elipar S10 | Monowave | 1600 | 5 × 20 overlapping | 8 | SENB ISO 20795-1 [45] | 2.4 (0.5) 0.9 (0.1) 1.1 (0.1) 1.1 (0.1) |
| 6. Bonilla, 2000 [48] | Ti-Core (ESSENTIAL DENTAL SYSTEMS) Fluorocore (CAULK) | Astralis5 (IVOCLAR/VIVADENT) | NR | NR | 120 | NR | SENB ASTM E399 [49] | 1.41 (0.05) 1.66 (0.09) |
| 7. Bonilla, 2003 [50] | Aeliteflo (BISCO) Crystal Essence (CONFI-DENTAL) Flow-It (JENERIC/PENTRON) Permaflo (ULTRADENT) Revolution (KERR) Tetric Flow (IVOCLAR) VersaFlo (CENTRIX) Wave (SDI) FloRestore (DEN-MAT) | Coltolux 4 (COLTENE) | NR | 650 | 45 incrementally | 10 | SENB ASTM E399-90 [49] | 1.39 (0.17) 1.31 (0.19) 1.38 (0.2) 1.65 (0.13) 1.32 (0.18) 1.43 (0.09) 1.26 (0.13) 1.15 (0.1) 1.35 (0.14) |
| 8. Cho, 2009 [51] | Filtek Supreme Plus (3M/ESPE) Tetric EvoCeram (IVOCLAR) Premise (KERR) Esthet-X (DENTSPLY) | Demetron Model VCL 401 (KERR) | NR | 588 | No data available | 10 | SENB ASTM E399 [49] | 1.08 (0.17) 1.16 (0.11) 1.25 (0.06) 1.47 (0.08) |
| 9. Choi, 2000 [52] | ALERT (JENERIC/PENTRON) Pyramid-Enamel (BISCO) Pyrarnid-Dentin (BISCO) Solitaire (KULZER) SureFil (CAULK) Heliomolar (VIVADENT) ZlOO (3M/ESPE) | Curing unit Triad 11 (DENTSPLY) | NR | NR | 40 | 6 | SENB ASTM E399 [49] | 1.8 1.2 1.6 0.9 1.4 1.2 1.6 |
| 10. Engelhardt, 2016 [53] | ENAMEL plus HFO Flow ENAMEL plus Hri Flow G-aenial Flo(GC) G-aenial Universal Flo (GC) Tetric Evo Flow x-tra base SDR Venus Bulk Fill Sinfony Enamel (GC) | Elipar S 10 | NR | 1200 | 40 s in 2 mm layers | 10 | SENB | 0.76 (0.05) 1.33 (0.19) 0.64 (0.60) 1.26 (0.18) 0.76 (0.05) 1.34 (0.13) 1.33 (0.28) 1.22 (0.14) 1.00 |
| 11. Garoushi, 2013 [54] | X-tra base (VOCO) Venus bulk fill (KULZER) TetricEvoCeram (3M/ESPE) SDR (DENTSPLY) Filtek Bulk Fill (3M/ESPE) Alert (JENERIC/PENTRON) SonicFill (KERR) | TC-01 (SPRING HEALTH PRODUCTS) | Polywave | 1100 | manufacturer recommendations | 6 | SENB | 2.0 2.2 2.2 2.6 1.7 2.9 3.0 |
| 12. Garoushi, 2024 [55] | Essentia Universal (GC) Alert (GENERIC PENTRON) Fibrafill Flow (ADM) Fibrafill Dentin (ADM) everX flow (GC) everX Posterior (GC) | Elipar S10 | Monowave | 1600 | 20 s in five different parts | 8 | SENB ISO 20795-13 [45] | 1.1 (0.1) 1.7 (0.4) 1.1 (0.07) 1.2 (0.1) 2.8 (0.4) 2.6 (0.4) |
| 13. Jun, 2013 [56] | Spectrum TPH (DENTPLY) Arabesk Top (VOCO) Charisma (KULZER) Revolution2 (KERR) Dyract flow (DENTSPLY) Filtek supreme (3M/ESPE) Grandio (VOCO) | L.E.Demetron I (KERR) | NR | 700 | 40 | 3 | SENB | 2.42 (0.48) 2.57 (1.08) 1.30 (0.32) 2.32 (0.07) 1.58 (0.05) 2.33 (0.18) 1.97 (0.34) |
| 14. Ilie, 2012 [57] | Venus (KULZER) Tetric Ceram (IVOCLAR) Z100 (3M/ESPE) Clearfil ST (KURARAY) Charisma (KULZER) Point 4 (KERR) Herculite XRV (KERR) TPH Spectrum (DENTSPLY) Synergy Duo Shade (COLTENE) Esthet X (DENTSPLY) Z250 (3M/ESPE) Enamel plus (GDF) Miris (COLTENE) Filtek Supreme (3M/ESPE) | oven Dentacolor XS (KULZER) | Polywave | NR | 40 | 8 | SENB ASTM E399 [49] | 1.18 (0.21) 1.70 (0.18) 1.81 (0.22) 1.81 (0.44) 1.87 (0.20) 1.89 (0.40) 1.96 (0.25) 2.09 (0.22) 2.12 (0.21) 2.15 (0.25) 2.31 (0.16) 2.40 (0.56) 2.17 (0.33) 1.46 (0.28) |
| 15. Ilie, 2021 [58] | Venus Venus Diamond Charisma Classic Charisma Topaz | BluePhase Style (IVOCLAR/VIVADENT) | Polywave | NR | 20 | 15 | Notchless triangular prism (NTP) | 1.54 2.01 1.04 0.96 |
| 16. Kamourieh, 2024 [19] | ever X Posterior ever X Flow | Demi Plus (KERR) | Monowave | 700 | 9 overlapping Window technique | 10 | SENB ISO 20795 [45] | 1.90 (0.19) 2.72 (0.37) |
| 17. Knobloch, 2002 [59] | Alert (JENERIC/PENTRON) SureFil (DENTSPLY) Solitaire (HERAEUS KULZER) Heliomolar (IVOCLAR/VIVADENT) Belleglass (BELLE DE ST.CLAIRE) | NR | NR | NR | Manufacturer’s specifications | Compact tension specimen ASTM E399 [49] | 1.57 1.25 0.67 0.80 1.27 | |
| 18. Kim, 2002 [60] | Silux Plus (3M/ESPE) Heliomolar (IVOCLAR/VIVADENT) Aelitefil (BISCO) Charisma (KULZER) Herculite XR (KERR) TPH (DENTSPLY) Z-100 (3M/ESPE) | Powerlite 100 (LONE STAR DENTAL CORP) | NR | NR | 30 | 5 | SENB ASTM E399 [49] | 0.81 (0.07) 0.84 (0.02) 0.98 (0.03) 0.75 (0.02) 0.85 (0.01) 1.04 (0.04) 0.97 (0.04) |
| 19. Kim, 2002 [61] | AElitefil (BISCO) Charisma (KULZER) Herculite XR (KERR) Hipolite (B&P, INCHEON) TPH (DENTSPLY) Veridonfil (HYOSUNG) | NR | NR | NR | Five 30 s steps | 5 | SENB ASTM E399 [49] | 0,98 (0,03) 0.75 (0.02) 1.02 (0.01) 1.14 (0.07) 1.04 (0.04) 1.08 (0.03) |
| 20. Lassila, 2019 [62] | SDR (DENTSPLY) Filtek Bulk Fill Flowable (3M/ESPE) Tetric EvoFlow Bulk Fill (IVOCLAR/VIVADENT) Estelite Bulk Fill Flow (TOKUYAMA) Short fiber flowable (GC) | Elipar S10 (3M/ESPE) | Monowave | 1600 | 20 in five separate overlapping portions | 6 | SENB ISO 20795 [45] | 1.6 (0.1) 1.2 (0.1) 1.4 (0.2) 1.3 (0.1) 2.8 (0.4) |
| 21. Lassila, 2020 [63] | Alert (JENERIC/PENTRON) NovaPro Flow (NANOVA) NovaPro Fill (NANOVA) everX Flow (GC) everX Posterior (GC) | Elipar TM S10 (3M/ESPE) | Monowave | 1600 | 20 | 8 | SENB ISO 20795 [45] | 1.7 (0.4) 1.6 (0.3) 1.3 (0.2) 2.8 (0.4) 2.6 (0.4) |
| 22. Lien, 2010 [64] | Beautifil-II (SHOFU) Esthet-X (DENTSPLY) Filtek LS (3M/ESPE) Filtek Supreme (3M/ESPE) Filtek Z250 (3M/ESPE) | (Bluephase 16i, IVOCLAR) | Polywave | 1600 | 20 | 10 | SENB | 0.59 0.58 0.68 0.59 0.67 |
| 23. Lin, 2009 [65] | Micronew (BISCO) Renew (BISCO) Filtek Supreme Plus (3M/ESPE) BelleGlass HP (SDS-KERR) | Oven Triad (DENTSPLY) | NR | NR | 120 each side | N/A | SENB ASTM Standard PS070-097 [66] | 0.82 (0.35) 1.41 (0.11) 1.40 (0.05) 2.06 (0.08) |
| 24. Lohbauer, 2020 [67] | Ceram X mono (DENTSPLY) Filtek Supreme XTE (3M/ESPE) Heliomolar (IVOCLAR) | Elipar Trilight | NR | 750 | 20 | 15 | SENB ISO 13586 [41] (ASTM E399) [49] | 0.83 (0.03) 1.03 (0.08) 0.74 (0.04) |
| 25. Manhart, 2000 [68] | Alert (JENERIC PENTRON) Surefil (DENTSPLY) Solitaire (KULZER) Definite (DEGUSA) Tetric Ceram (VIVADENT) | Elipar Highlight (ESPE) | NR | 700 | 40 | 10 | SENB ASTM E399 [49] | 2.3 (0.2) 2.0 (0.2) 1.4 (0.2) 1.6 (0.3) 2.0 (0.1) |
| 26. Mese, 2016 [69] | Estelite Sigma Quick (TOKUYAMA) Esthet X HD (DENTPLY) Filtek Supreme XT (3M/ESPE) Heliomolar (IVOCLAR/VIVADENT) RoK (SDI) Vit-l-escence (ULTRADENT) | Raddi Plus (SDI) | Monowave | 1500 | 40 × 3 incrementally | 6 | SENB ASTM D5045 [70] | 0.51 (0.15) 0.90 (0.17) 0.91 (0.17) 0.56 (0.07) 1.45 (0.24) 1.34 (0.20) 0.58 (0.05) 1.48 (0.20) 1.45 (0.13) 0.49 (0.06) 1.05 (0.19) 1.13 (0.08) 0.56 (0.06) 1.28 (0.24) 1.16 (0.17) 0.75 (0.08) 1.75 (0.09) 1.48 (0.07) 0.53 (0.10) 1.17 (0.07) 1.08 (0.15) |
| 27. Nakade, 2024 [71] | Luxacore Z Lumiglass DeepCure SelfComp | NR | NR | NR | NR | 15 | SENB ASTM E399 [49] | 0.99 0.82 0.36 |
| 28. Ribeiro, 2025 [72] | Tetric PowerFill (IVOCLAR) Tetric EvoCeram (IVOCLAR) Filtek Supreme (3M/ESPE) Admira Fusion X-tra (VOCO) | Monet Laser (AMD Lasers) PowerCure (IVOCLAR) PinkWave (APEX VISTA) | Laser Dual-wave Quad-wave | 1 10/3 3 | 2000–2400 1200/3000 >1515 | 10 | ASTM E1820 [73] | 0.5 (0.06) 0.6 (0.07) 0.6 (0.06) 0.5 (0.08) 0.4 (0.07) 0.6 (0.06) 0.6 (0.05) 0.5 (0.09) 0.4 (0.09) 0.5 (0.05) 0.6 (0.08) 0.6 (0.09) 0.4 (0.04) 0.4 (0.04) 0.5 (0.05) 0.4 (0.04) |
| 29. Scherrer, 2000 [74] | Columbus (CENDRES ET METAUX S.A) Artglass (KULZER) Targis (IVOCLAR) | UniXst oven, (KULZER) | NR | NR | 180 | 6 | chevron-notched precracked Brazilian disk test | 0.60 (0.09) 0.63 (0.04) 0.48 (0.03) |
| 30. Sochacki, 2022 [75] | ceramX Universal (3M/ESPE) Esthet X HD (3M/ESPE) TPH Spectra HT HV (3M/ESPE)) TPH Spectra HT LV (3M/ESPE) | Bluephase G2 (IVOCLAR) | Polywave | 1000 | manufacturer recommended time | 12 | SENB ASTM D5045 [70] | 0.491 (0.04) 0.655 (0.05) 0.721 (0.03) 0.610 (0.06) 0.620 (0.04) |
| 31. St-Georges, 2003 [76] | Herculite XRV (KERR) Revolution formula 2 (KERR) Spectrum 800 (DENTSPLY) Elipar Trilight soft start mode (ESPE) Elipar Trilight regular mode (3M/ESPE) Virtuosoc (DEN-MAT) | Accucure 3000 (LASERMED) | QTH QTH QTH PAC Argon-ion laser | 40 40 40 3/5 15 | 550 100–850 860 1980 725 | NR | non-standard, excluded from pooled interpretation | 1.40 (0.11) 1.43 (0.11) 1.35 (0.09) 1.44 (0.07) |
| 32. Thadathil Varghese, 2024 [77] | ACTIVA Bioactive (PULPDENT) Fill Up! (COLTENE) Surefil One (DENTSPLY) Cention N (IVOCLAR) Stela Automix (SDI) Stela Capsule (SDI) | Radii plus | NR | 1500 | NR | 5 | SENB ISO 20795 [45] | 1.2 0.8 0.43 1.4 1.0 1.41 |
| 33. Thomaidis, 2013 [78] | Filtek Z-250 (3M/ESPE) Filtek Ultimate (3M/ESPE) Admira (VOCO) Majesty Posterior (KURARAY) | Radii plus (SDI) | Monowave | 950 | five slightly overlapping irradiations (40 s each) | 10 | SENB ASTM E399 [49] Brazilian test | 1.52 (0.16)/0.63 (0.09) 1.43 (0.11)/0.52 (0.04) 1.15 (0.20)/0.45 (0.10) 1.20 (0.20)/0.58 (0.08) |
| 34. Yang, 2022 [79] | Beautifil-Bulk Restorative (SHOFU) Filtek One Bulk fill (3M/ESPE) SonicFill 3 (KERR) Viscalor (VOCO) | Elipar S10 | NR | 1200 | 280 seven center-overlapping areas | 6 | SENB British Standard 54749:1978 E399 [49] | 1.13 (0.04) 1.58 0.20) 1.44 (0.04) 1.38 (0.10) |
| 35. Yap, 2004 [80] | Tetric Ceram (VIVADENT) Z250 (3M/ESPE) Esthet X (DENTSPLY) | Max (DENTSPLY) | NR | 402 | top and bottom surfaces of the specimens were then light polymerized in three overlapping manufacturer’s curing time | 7 | SENB | 1.75 (0.23) 1.79 (0.37) 1.92 (0.38) |
| 36. Watanabe 2008 [81] | Venus (KULZER) Filtek z250 (3M/ESPE) Filtek Supreme (3M/ESPE) Gradia Direct Anterior (GC) Durafil (KUZLER) Point 4 (KERR) | Optilux 501 (KERR) | NR | 500 | 200 | 5 | Brazilian Test | 0.53 (0.03) 0.48 (0.04) 0.42 (0.01) 0.38 (0.01) 0.37 (0.00) 0.26 (0.02) |
| CAD CAM | ||||||||
| 37. Alsarani, 2024 [82] | Cerasmart (GC) Lava Ultimate (3M/ESPE) Shofu Block HC (SHOFU) Enamic (VITA) IPS Emax CAD (IVOCLAR) | NR | NR | NR | NR | 8 | SENB | 1.17 (0.15) 1.24 (0.23 1.20 (0.24) 1.39 (0.29) 1,78 (0,21) |
| 38. Della Bona, 2014 [83] | Enamic (VITA) | NR | NR | NR | NR | 7 | SENB ASTM C1421-10 [84] | 1.09 (0.05) |
| 39. Elraggal, 2022 [85] | Enamic; VITA Grandio blocks; VOCO IPS Emax CAD (IVOCLAR) | NR | NR | NR | NR | 10 | Quantitative fractographic analysis | 0.76 (0.17) 1.21 (0.09) 1.89 (0.23) |
| 40. Goujat, 2018 [86] | Cerasmart (GC) Lava Ultimate (3M/ESPE) Enamic (VITA) IPS EmaxCAD (IVOCLAR) | NR | NR | NR | NR | 10 | SEVNB ISO 6872 [87] | 1.2 1.4 1.6 1.8 |
| 41. Hampe, 2019 [15] | Ambarino High-Class (CREAMED) Brilliant Crios (COLTENE) Cerasmart (GC) Katana Avencia (KURARAY) Lava Ultimate (3M/ESPE) Enamic (VITA) IPS Emax CAD (IVOCLAR IPS Empress CAD (IVOCLAR) | NR | NR | NR | NR | 10 | SENB ISO 6872 [87] | 1.43 (0.27) 1.41 (0.14) 1.22 (0.20) 1.47 (0.28) 1.29 (0.15) 1.24 (0.18) 2.15 (0.24) 0.84 (0.48) |
| 42. Harada, 2015 [16] | Lava Ultimate Estenia C&B IPS Emax Press | NR | NR | NR | NR | 5 | SENB ISO 6872 [87] | 1.4 1.3 2.3 |
| 43. Karaer, 2020 [88] | Cerasmart 300 (GC) Katana Avencia P (KURARAY) KZR-CAD HR3 Gamma Theta (YAMAKIN) | NR | NR | NR | NR | 10 | notchless triangular prism (NTP) | 5.057 4.193 4.880 |
| 44. Ling, 2022 [89] | Paradigm MZ100 (3M ESPE), Lava Ultimate (3M ESPE), Grandio blocs (VOCO, Germany), Cerasmart (GC, Japan), Shofu Block HC (SHOFU) | NR | NR | NR | NR | 10 | SENB ASTM D5045-14 [70] | 1.74 (0.15) 1.15 (0.09) 1.73 (0.17) 1.71 (0.21) 1.06 (0.09) 1.38 (0.16) |
| 45. Lucsanszky, 2020 [90] | Enamic Universal HT (VITA) RCB; KZR-CAD HR2 (YAMAKIN) CERASMART (GC) CAMouflageNOW (GLIDEWELL DENTAL LABORATORIES, USA) | NR | NR | NR | NR | 25 | notchless triangular prism (NTP) | 0.83 (0.16) 0.64 (0.11) 1.37 (0.33) 0.68 (0.11) 1.47 (0.19) |
| 46. Moradi, 2020 [91] | HIPC (BREDENT) Crios (COLTENE) Gradia (GC) | Woodpecker | NR | 800 | 40 | 10 | SENB ASTM E399 [49] | (the values here represent flexular strength) 16.27 22.44 16.42 |
| 47. Nguyen, 2012 [92] | Gradia (GC) Grandio (VOCO) EsthetX (DENTSPLY) VitaVM LC (VITA) Paradigm (3M/ESPE) | Radii, (SDI) 30 min post cure in curing chamber | NR | 897 | 40 | 8 | notchless triangular prism (NTP) | 1.58 (0.18) 1.17 (0.21) 1.52 (0.10) 0.99 (0.17) 0.78 (0.21) |
| 48. Sonmez, 2018 [93] | Lava Ultimate (3M/ESPE) Enamic (VITA) Vita Mark II (VITA) IPS Empress CAD (IVOCLAR) IPS Emax CAD (IVOCLAR) | NR | NR | NR | NR | 10 | non-standard (excluded) | 1.29 (0.03) 1.23 (0.02) 2.34(0.04) 1.9 (0.03) 1.67 (0.03) |
| 49. Sulaiman, 2022 [94] | Luxacrown ( DMG) Filtek Supreme Ultra (3M/ESPE) Enamic, (VITA) | (Elipar DeepCure-S, 3M | NR | 1200 | NR | N/A | SENB ASTM D5045-14 [70] | 1.28(0.5) 1.48 (1.0) 1.45 (0.7) |
| 50. Suzaki, 2020 [95] | Trinia (SHOFU) everX Posterior (GC) Beauti core flow paste (SHOFU) | PenCure 2000, Kyoto, Japan (MORITA) | 2000 | 30 both upper and side surfaces | NR | Notchless triangular prism | 9 2 3.5 2.5 | |
| 51. Swain, 2016 [96] | Enamic (72%) Enamic (64%) Emax CAD (IVOCLAR) | NR | NR | NR | NR | No data available | SENB | 1 (00.4) 1.51 (0.11) 2.37 (0.28) |
| 52. Wendler, 2021 [97] | Gradio blocks (VOCO) Lava Ultimate (3M/ESPE) CeraSmart (GC) Brilaint Crios (COLTENE) Gradio SO (VOCO) | Elipar TriLight 3M | Halogen | 700–800 | NR | 10 | compact tension C(T) ASTM E1820-13 [73] | 1.42 (0.07) 1.14 (0.05) 0.99 (0.15) 0.97 (0.12) |
| Testing Method | Strengths | Weaknesses | Typical Outcomes |
|---|---|---|---|
| SENB (single-edge notched beam) | Most widely used; standardized; reliable K_IC values; allows cross-study comparison [54,57] | Specimen prep demanding; requires precise notch; time-consuming [5] | Moderate-to-high K_IC, reproducible values [15,16] |
| NTP (Notchless Triangular Prism) | Simple specimen preparation; less machining required [58] | Sensitive to notch geometry; often underestimates K_IC; less standardized [94] | Lower K_IC values, more variable [92] |
| C(T) (Compact Tension) | Well-established in fracture mechanics; accurate K_IC for large specimens [72] | Requires large specimens; difficult in dental context [97] | Values comparable to SENB but fewer studies [69] |
| Brazilian Disk Test | Easy setup; widely known in ceramics testing [81] | Low reproducibility; high variability; questionable validity for composites [78] | Lower, inconsistent K_IC [78] |
| Indentation (Vickers Crack Length) | Quick, requires minimal equipment; small specimens possible [76] | Not standardized; often underestimates toughness; indirect method [93] | Lowest reported values, often underestimated [93] |
| Fractography | Direct examination of fracture surfaces; identifies true crack origins [4] | Qualitative; not suitable for quantitative comparison across materials [4] | Confirmed fracture origins, qualitative insights [4] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thomaidis, S.; Pappa, E.; Antoniadou, M. Fracture Toughness of CAD/CAM Resin-Based Materials vs. Direct Composite Resins: A Scoping Review. Appl. Sci. 2025, 15, 12308. https://doi.org/10.3390/app152212308
Thomaidis S, Pappa E, Antoniadou M. Fracture Toughness of CAD/CAM Resin-Based Materials vs. Direct Composite Resins: A Scoping Review. Applied Sciences. 2025; 15(22):12308. https://doi.org/10.3390/app152212308
Chicago/Turabian StyleThomaidis, Socratis, Eftychia Pappa, and Maria Antoniadou. 2025. "Fracture Toughness of CAD/CAM Resin-Based Materials vs. Direct Composite Resins: A Scoping Review" Applied Sciences 15, no. 22: 12308. https://doi.org/10.3390/app152212308
APA StyleThomaidis, S., Pappa, E., & Antoniadou, M. (2025). Fracture Toughness of CAD/CAM Resin-Based Materials vs. Direct Composite Resins: A Scoping Review. Applied Sciences, 15(22), 12308. https://doi.org/10.3390/app152212308







