2.1. Sample Preparation
The materials and tools used in this study are summarized in
Table 1.
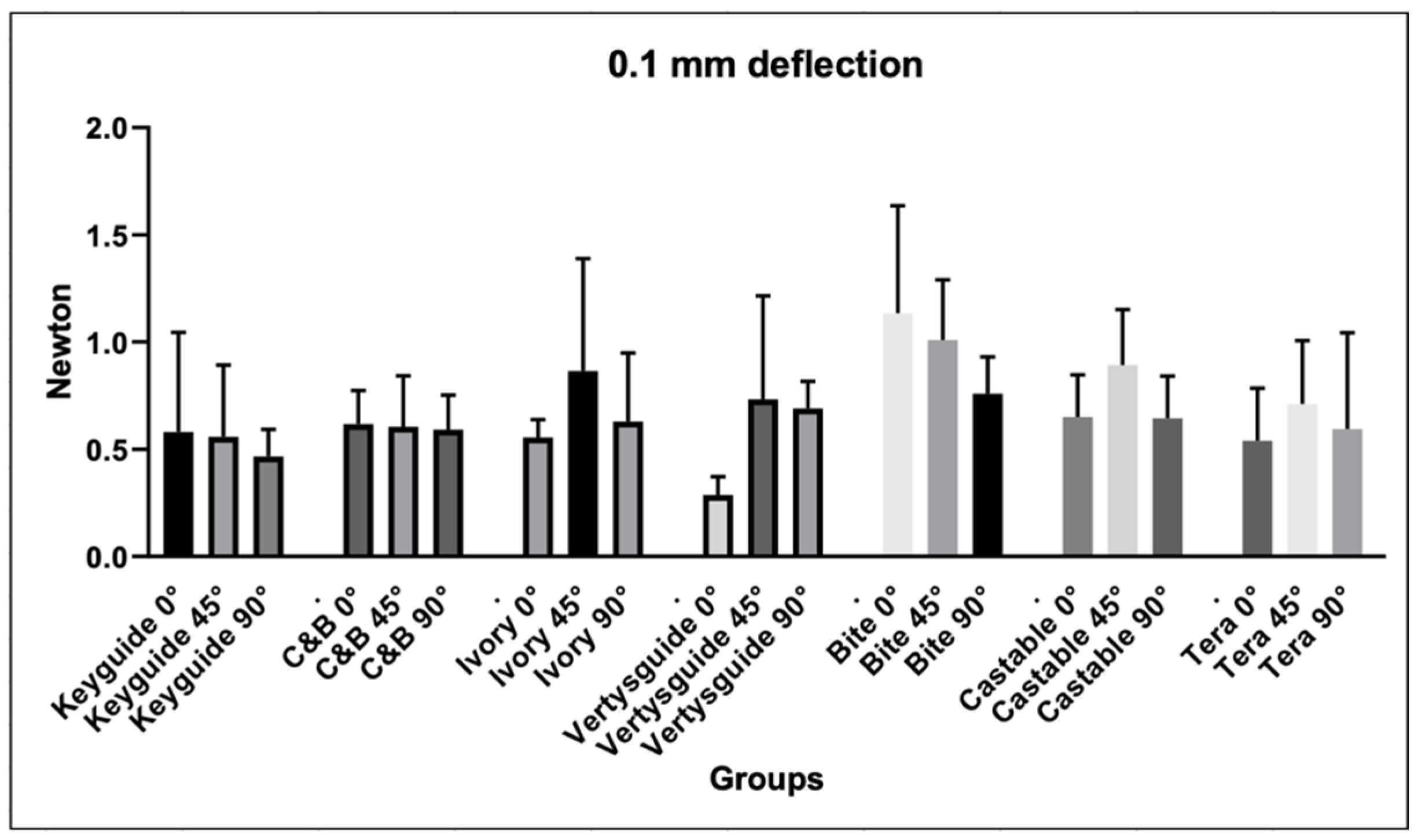
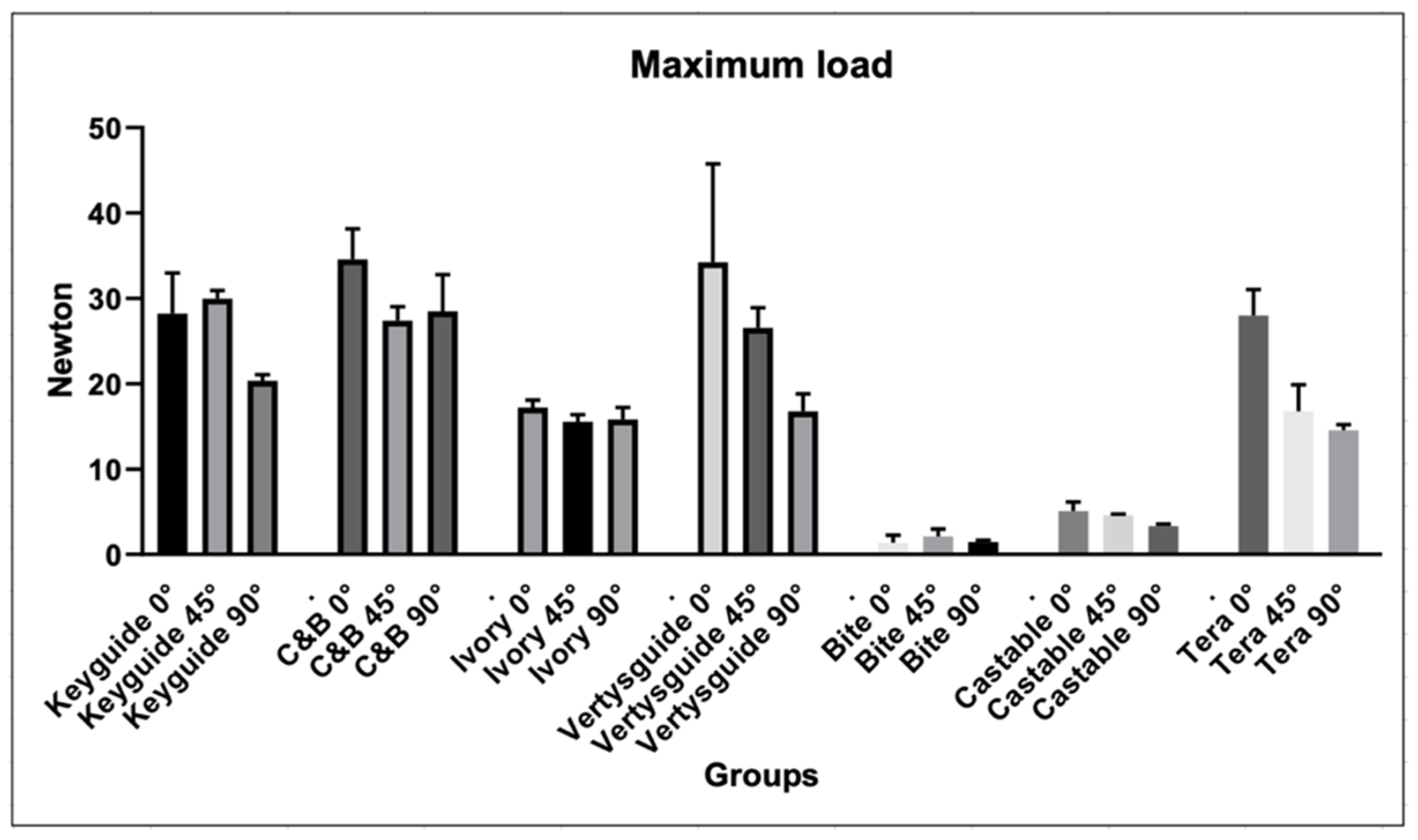
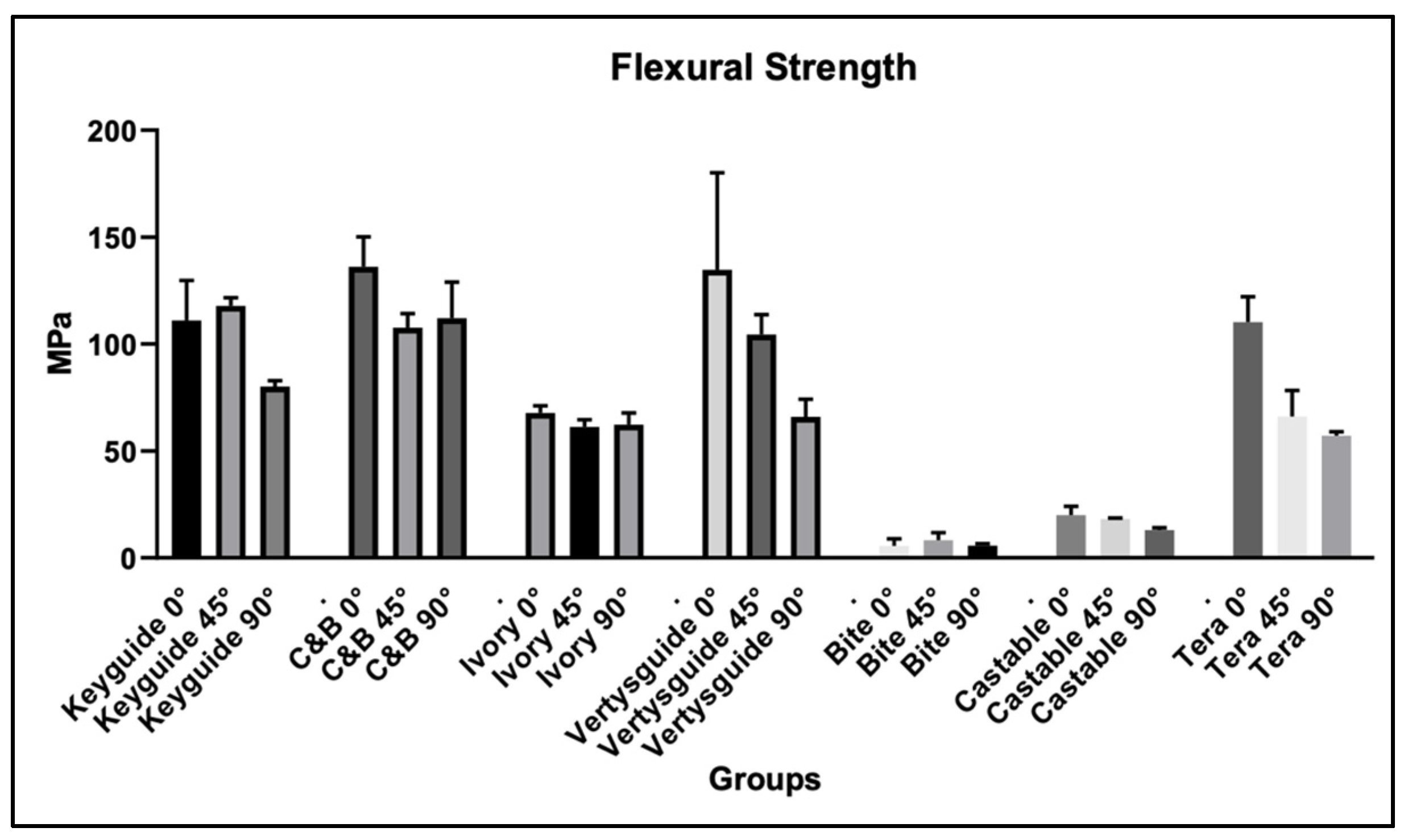
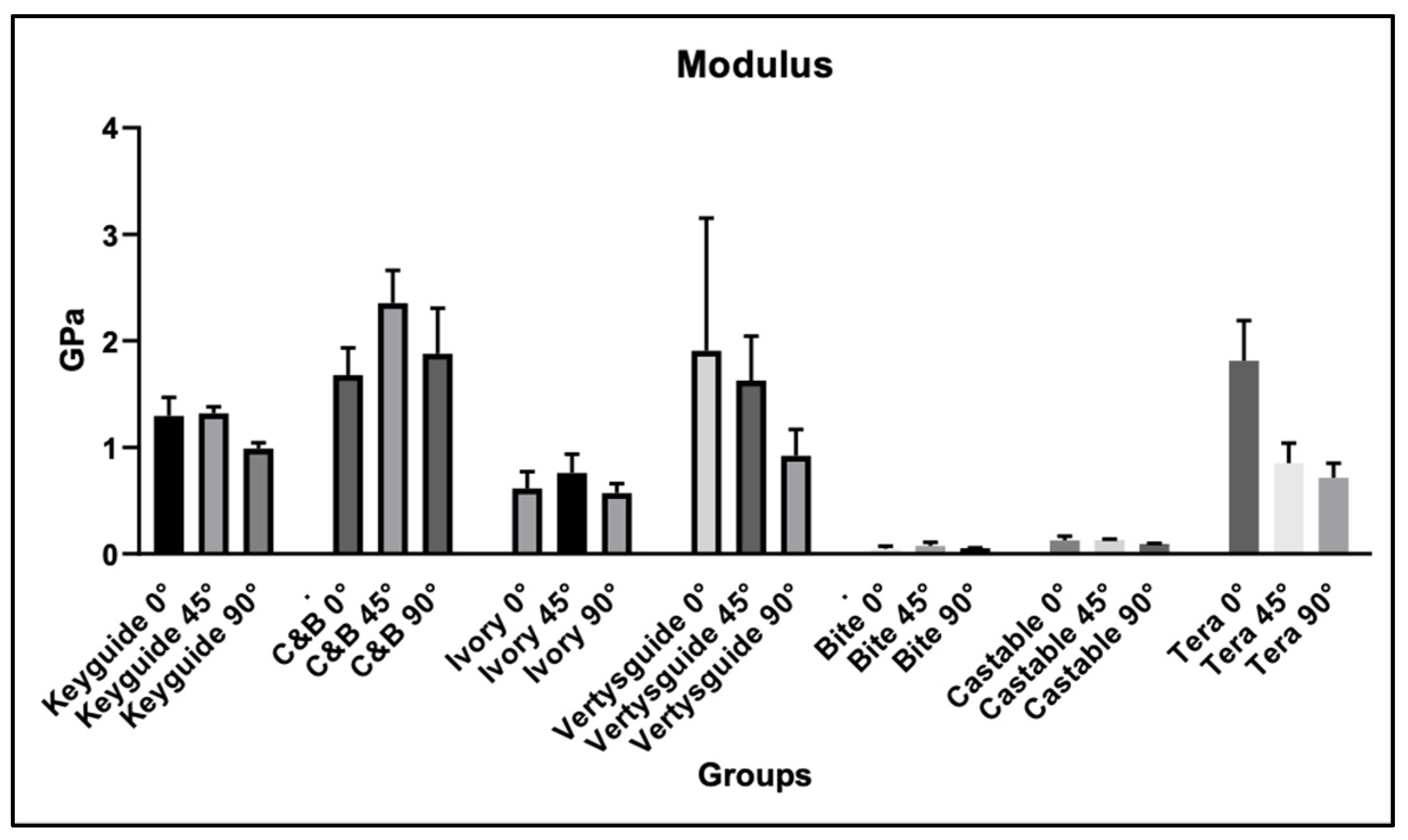
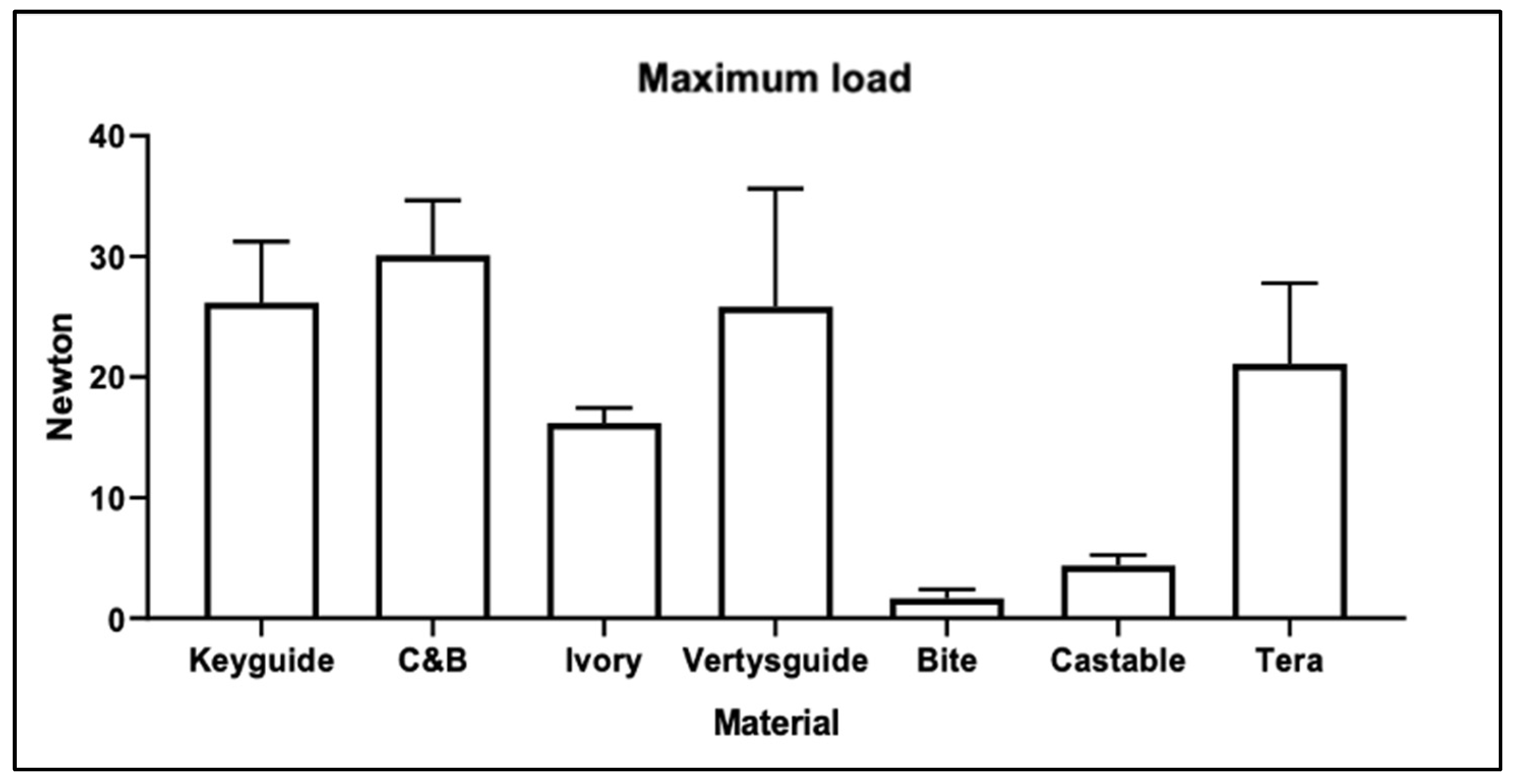
The seven resin materials chosen and used for printing the specimens in this phase of the experiment were Keyguide (Keystone Industries GmbH Stockholzstr., Singen, Germany), C&B (NextDent, Centurionbaan 190, Soesterberg, The Netherlands), Ivory (Keystone Industries GmbH Stockholzstr., Singen, Germany), Vertysguide (Keystone Industries GmbH Stockholzstr, Singen, Germany), Bite (Keystone Industries GmbH Stockholzstr., Singen, Germany), Tera (Graphy Inc., Geumcheon-gu, Seoul, Republic of Korea), Nextdent Cast (NextDent, Centurionbaan 190, Soesterberg, The Netherlands).
Keyguide is a Class I, rigid, and biocompatible photopolymer resin specifically engineered for Digital Light Processing (DLP) 3D printers operating within the 385–405 nm wavelength range. Its chemical formulation primarily consists of urethane acrylate oligomers combined with dimethacrylate monomers, including 2-hydroxyethyl methacrylate (HEMA) and hexanediol diacrylate. In addition, the resin contains phosphine oxide-based photoinitiators (TPOs) and stabilizing agents such as 4-methoxyphenol (MEHQ) to ensure efficient polymerization and long-term storage stability.
According to the manufacturer’s technical specifications, Keyguide exhibits a flexural strength ranging from approximately 106 to 140 MPa, a flexural modulus between 2400 and 2500 MPa, and a Shore D hardness value of 95. These properties confirm its mechanical rigidity and clinical suitability, particularly for the fabrication of intraoral surgical guides. For safe handling and manipulation, the use of protective nitrile or latex gloves is recommended [
39].
The C&B resin used in this study is a light-curable photopolymer specifically designed for the additive manufacturing of temporary crowns and bridges. Its chemical formulation comprises a methacrylic oligomer, glycol methacrylate, and phosphine oxide as the primary photoinitiator. Classified as a high-molecular-weight acrylic resin, C&B combines ease of handling with excellent esthetic and mechanical performance.
It offers notable advantages such as enhanced resistance to abrasion and fracture, low bacterial plaque accumulation, and high biocompatibility, even when fabricated at reduced thicknesses. Due to its superior mechanical stability, this resin exhibits minimal polymerization shrinkage and deformation during the printing process, ensuring consistent dimensional accuracy compared to similar materials.
According to the manufacturer’s technical documentation, C&B resin demonstrates a flexural strength of approximately 107 MPa, low water sorption (54 µg/mm
3), and minimal solubility (5.9 µg/mm
3) [
40].
Ivory (KeyModel Ultra™) is a photopolymer resin specifically developed for the high-resolution 3D printing of dental models, optimized for use with 4K DLP printers. Its low-shrinkage formulation makes it suitable for the fabrication of highly accurate bridge and crown models, implant models, aligner models, and diagnostic casts.
It can be employed for rapid prototyping, enabling the production of physical prototypes directly from CAD data with minimal dimensional deviation and reduced resin odor. This resin is composed of urethane oligomers, acrylate monomers, photoinitiators, and titanium dioxide. Ivory exhibits a maximum tensile strength greater than 50 MPa and a tensile modulus above 1700 MPa.
It shows an elongation at break of 5%, while the maximum flexural strength exceeds 70 MPa, with a flexural modulus above 1940 MPa. Its viscosity at 25 °C ranges between 500 and 600 cP. These characteristics make Ivory a rigid, dimensionally stable resin with sufficient resistance for dental model applications. The material provides ultra-fast printing, detail reproduction, availability in multiple colors, and the presence of a thermoforming quick-release agent, which facilitates the fabrication of orthodontic aligner models; printed parts can be trimmed without chipping.
Although not indicated for intraoral use, Ivory is suitable for the production of accurate, durable, and reliable dental models and prototypes [
41].
Vertysguide is a transparent, pressure-thermopolymerizable resin designed for low-temperature processing, primarily used in implantology and orthodontics. It is a Class I biocompatible material developed for the 3D printing of surgical guides for implant placement and occlusal splints. The resin provides dimensional stability, compactness, mechanical resistance, and high polishability, making it suitable for clinical use.
Vertysguide is composed of acetone, toluene, 2-hydroxy-2-methylpropiophenone, diphenylphosphine oxide, isobutanol, isobutyl acetate, acrylate oligomers, diacrylates, trimethylolpropane and additional photoinitiators. Vertysguide exhibits an ultimate flexural strength of 85 MPa (ISO 20795-1) and a flexural modulus of approximately 2118 MPa [
42]. The residual monomer content is <0.1%, well below the limit of 2.2% required by ISO standards, ensuring safety and material stability.
Furthermore, Vertysguide complies with ISO 10993-1 biocompatibility standards, being classified as non-cytotoxic, non-mutagenic, and non-sensitizing [
43]. These properties highlight Vertysguide as a stable and reliable resin for the fabrication of precise surgical guides and orthodontic devices, ensuring both mechanical strength and high clinical safety [
44].
The Bite resin is a transparent, pressure-thermopolymerizable, low-temperature 3D printing material designed for implantology and orthodontics, ideal for the fabrication of bite splints, flexible dental splints, and night guards. It is composed of methacrylate monomers and a photoinitiator. This resin is characterized by dimensional stability, compactness, high resistance, and excellent polishability.
Optimized for DLP technology, it combines the mechanical strength required to protect teeth from disorders such as bruxism with enhanced flexibility, ensuring greater patient comfort. Among its main advantages are biocompatibility (ISO 10993-1; USP Class VI compliance), easy cleaning and polishing, resistance, and flexibility.
The resin demonstrates a flexural strength of 2.6–4.4 MPa (ISO 20795-2) [
45], a flexural modulus of 1356 MPa (ASTM D790) [
46], a tensile strength of 52 MPa (ASTM D638), and a tensile Young’s modulus of 1790 MPa (ASTM D638) [
47].
It exhibits elongation at break of 110% (ASTM D638), which highlights its flexibility, and water sorption below 18 µg/mm
3 (ISO 20795-2), ensuring durability and dimensional stability in the oral environment [
48].
Tera Harz TC-80DP is a Class IIa photopolymer resin designed for 3D printing with DLP/LCD 405 nm UV technology, certified for the additive manufacturing of long-term dental restorations. With a flexural strength of ≥220 MPa and a flexural modulus ≥ 4500 MPa, this material is suited for the fabrication of permanent and provisional restorations on natural teeth and implants, including bridges, crowns, implant-supported superstructures, long-term substructures, inlays, onlays, and overlays.
It represents the first 3D printing resin worldwide approved for the production of long-term bridges, crowns, Toronto prostheses, and substructures, overcoming the limitations of conventional resins typically restricted to temporary applications. Its mechanical properties, such as a Shore D hardness ≥ 90 and a biaxial flexural strength ≥ 350 MPa, are comparable to zirconia, allowing the creation of highly durable and functional restorations with an additive process that maximizes efficiency while minimizing waste.
Tera Harz TC-80DP ensures high aesthetics along with excellent dimensional stability, durability, and precision. This combination of strength, hardness, and rigidity makes it a groundbreaking material for permanent 3D-printed dental restorations [
49].
NextDent Cast is a castable, violet-colored resin specifically developed for 3D printing with DLP/LCD 405 nm UV technology. It is optimized to ensure complete and residue-free burnout, making it suitable for the lost-wax casting process.
This material can be employed for the fabrication of supporting structures, removable partial denture frameworks, orthodontic appliances, and study models, including both full arches and removable dies. Its ease of use and predictable burnout behavior allow for the production of high-definition objects that can be subsequently cast in the desired metal alloy.
NextDent Cast exhibits a flexural strength of 85 MPa, a flexural modulus of 2193 MPa, and a Shore D hardness of 83, all in compliance with ISO 178 standards [
50]. These properties provide dimensional stability and adequate handling performance during the design and processing phases, without compromising its complete combustibility [
51].
A 2D square was selected with 3D Builder software version 20.0.4.0. (Microsoft, Redmond, WA, USA) and transformed into a 3D cube, which, in turn, was modified with MeshMixer 3.5.0 (Autodesk, Inc., San Rafael, CA, USA) software to make it a rectangular parallelepiped with the dimensions of 2 mm × 2 mm × 25 mm. The software was used to create .stl files of 15 Keyguide material samples, 15 C&B material samples, 15 Ivory material samples, 15 Vertysguide material samples, 15 Bite material samples, 15 Tera material samples, and 15 Nextdent Cast material samples.
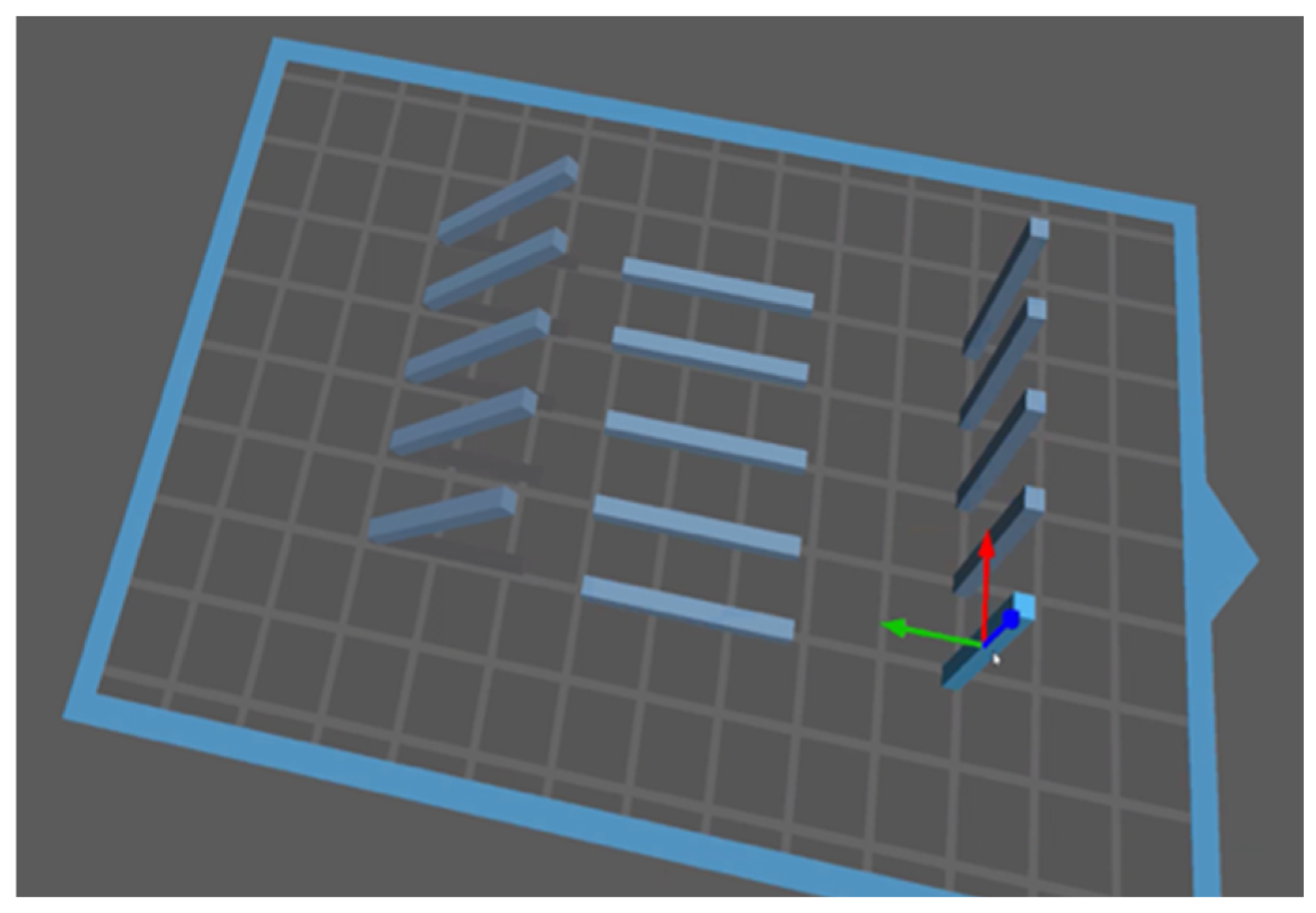
Finally, Chitubox 2.0.8 (CTB Systems, Shenzhen, China) (
Figure 1) is the software that was used to finalize and add printing supports to the Keyguide, C&B, Bite, Vertysguide, Tera, Ivory, and Nextdent Cast samples before sending them to print with the Moon Night 3D printer by Vertysystem (Vertysystem, Altavilla Vicentina (VI)-Italy).
The sample size was calculated using the following equation:
where Z
α/2 = 1.96 for a confidence interval of 5% (α = 0.05), Z
β = 0.84 for a power of 80% (1 − β = 0.80), σ = 14.1 MPa (standard deviation), and ∆ = 25 MPa (expected difference), considering the results from previous studies [
26].
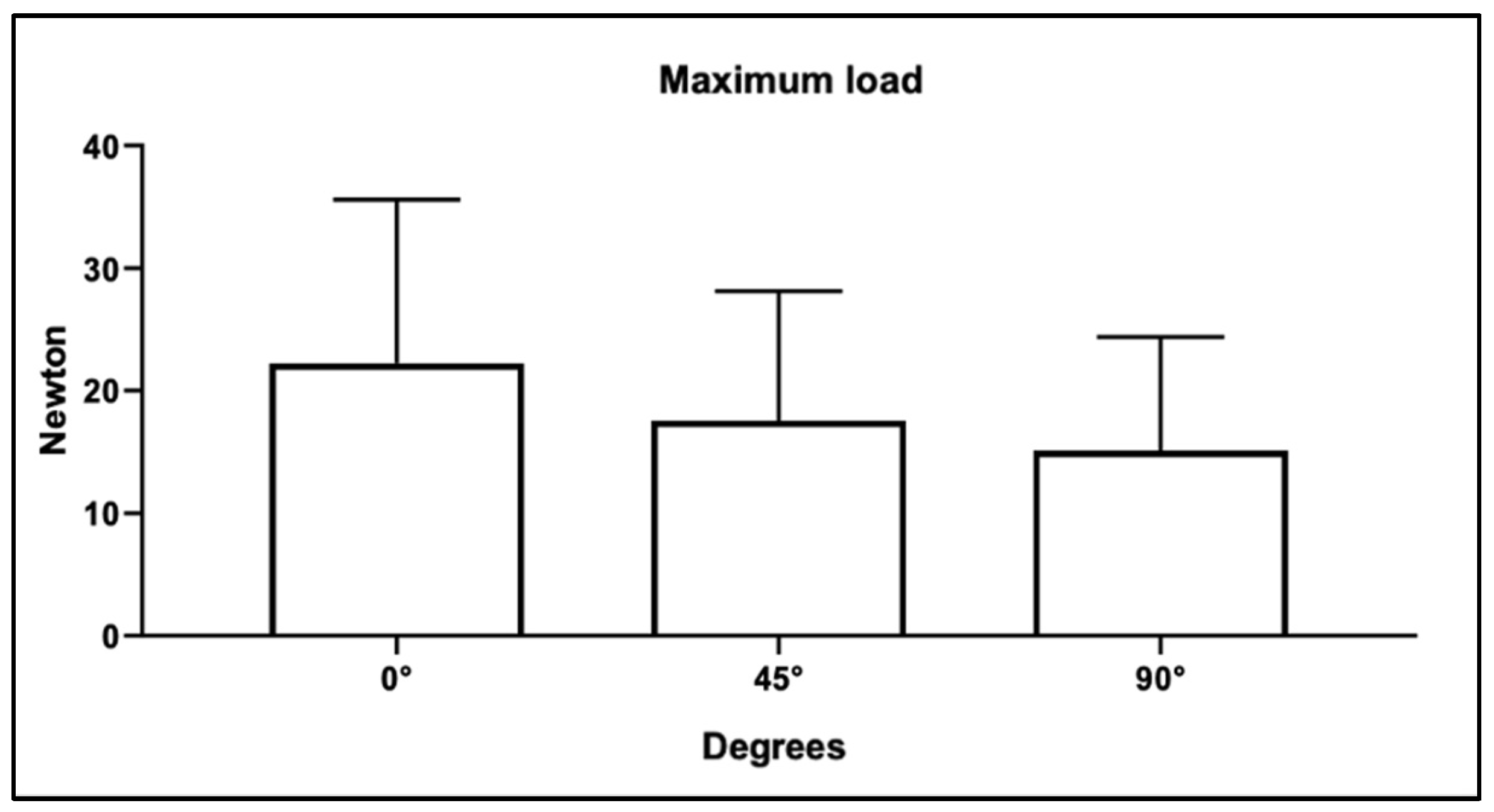
Based on preliminary data and expected effect sizes, an a priori power analysis determined that five specimens per group were sufficient to detect significant differences in flexural strength with appropriate statistical power. Specimen geometries were designed in MeshMixer and subsequently imported into Chitubox 2.0.8 (CTB Systems, Zhongcheng Future Industrial Park, Shenzhen, China) for print preparation. Within the software, groups of five specimens at 0°, 45°, and 90° orientations were positioned on the reference build plane [
38,
52,
53,
54].
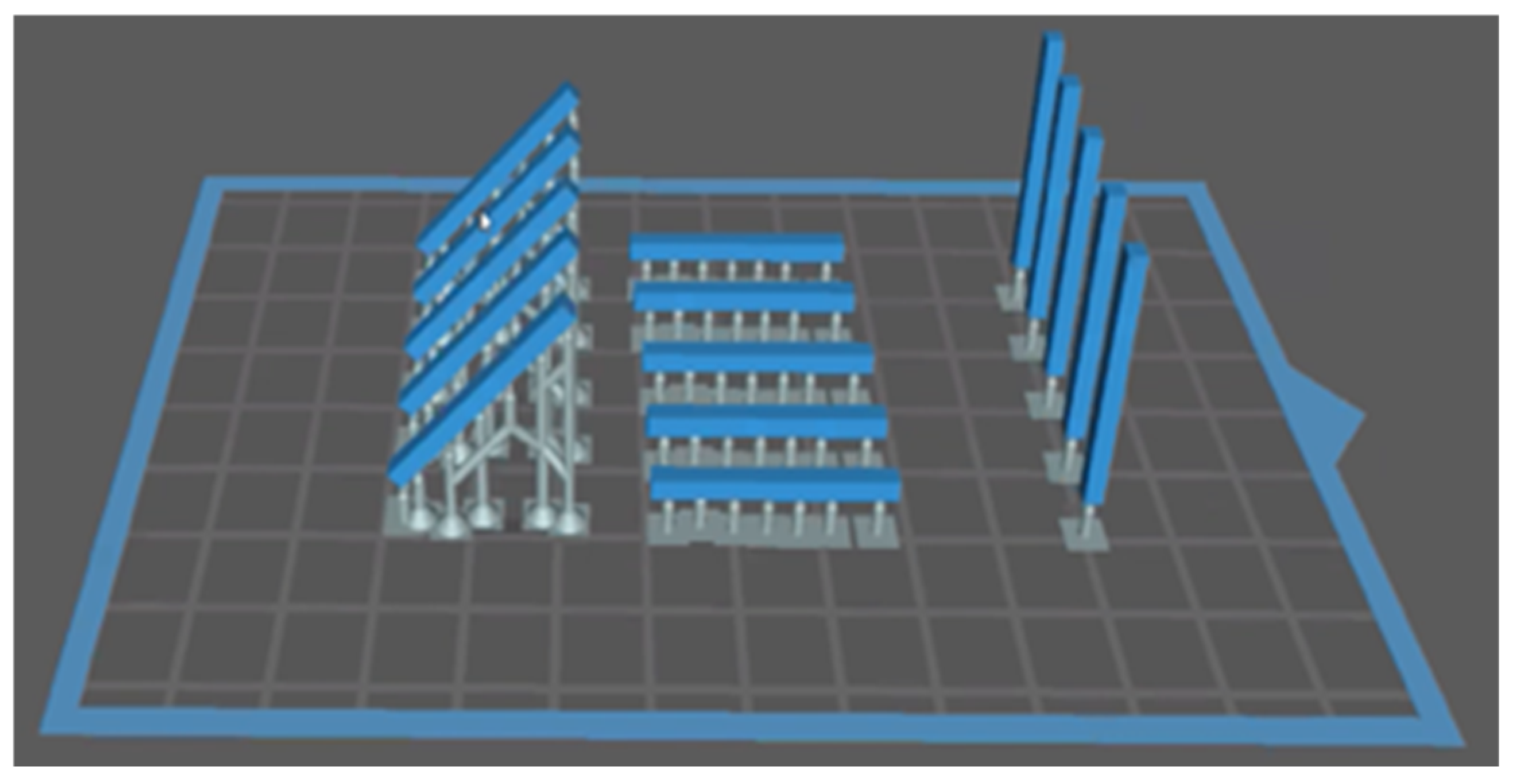
Automatic support generation was employed using the software’s intelligent algorithm to ensure specimen stability while minimizing the number of supports. Additional manual supports were added as needed to optimize printing accuracy and prevent potential distortions: four supports for the 45° specimens, one for the 90° specimens, and four for the 0° specimens. Although flat models typically do not require supports, they were deliberately included to standardize experimental conditions across all groups.
Supports played a critical role in maintaining print success, particularly for specimens oriented at positive or negative angles up to 45°, and facilitated detachment from the aluminum build plate.
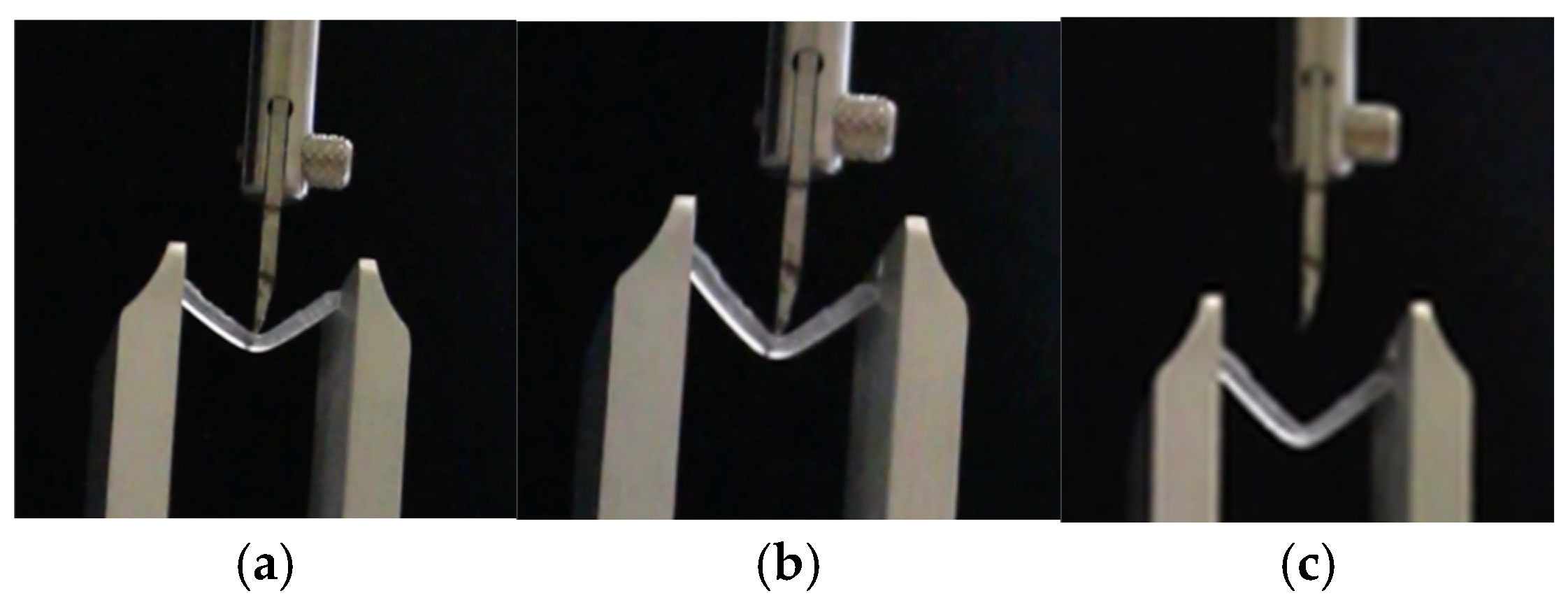
At a layer resolution of 20 µm, supports preserved surface integrity and minimized the risk of collapse in unsupported resin layers. In some cases, intermediate supports were added between existing structures to further enhance stability and maintain dimensional accuracy of the printed specimens (
Figure 2).
This procedure was repeated for the 5 samples with a print orientation of 0° and then replicated for the other 5 with orientations of 45° and 90°, respectively, for all resin materials used in this study: Keyguide, C&B, Ivory, Bite, Tera, Vertysguide, and NextDent Cast.
2.3. Post-Processing
Post-processing represents a fundamental phase in the additive manufacturing workflow, as it determines the final precision, mechanical reliability, and long-term stability of printed parts. Immediately after fabrication, each specimen was subjected to a cleaning step to eliminate residual, non-polymerized resin from the surface. In this study, cleaning was carried out with the MoonWash 2 device (Vertysystem, Altavilla Vicentina, Italy), a unit specifically developed for the treatment of 3D-printed dental resins. The process involved the use of isopropyl alcohol (IPA) as the primary solvent, which efficiently dissolves remaining resin residues.
To enhance the removal of uncured components, auxiliary cleaning products, Vertys Splash, Vertys Spray Dry, and Vertys Flusher (Vertysystem, Altavilla Vicentina, Italy), were applied in sequence as part of a multi-stage washing protocol. This approach ensured the complete elimination of superficial contaminants, thereby improving the consistency of subsequent polymerization and reducing potential cytotoxic effects associated with unreacted monomers.
After cleaning, specimens underwent a secondary curing process to achieve full polymer cross-linking and optimal material performance. The MoonLight 2 polymerization chamber (Vertysystem, Altavilla Vicentina, Italy) was used for this purpose. Controlled UV exposure promoted completion of the curing reaction, enhancing the flexural strength, dimensional accuracy, and wear resistance of the printed resins. Insufficient or irregular post-curing, conversely, could negatively affect both the mechanical integrity and the biological safety of the material.
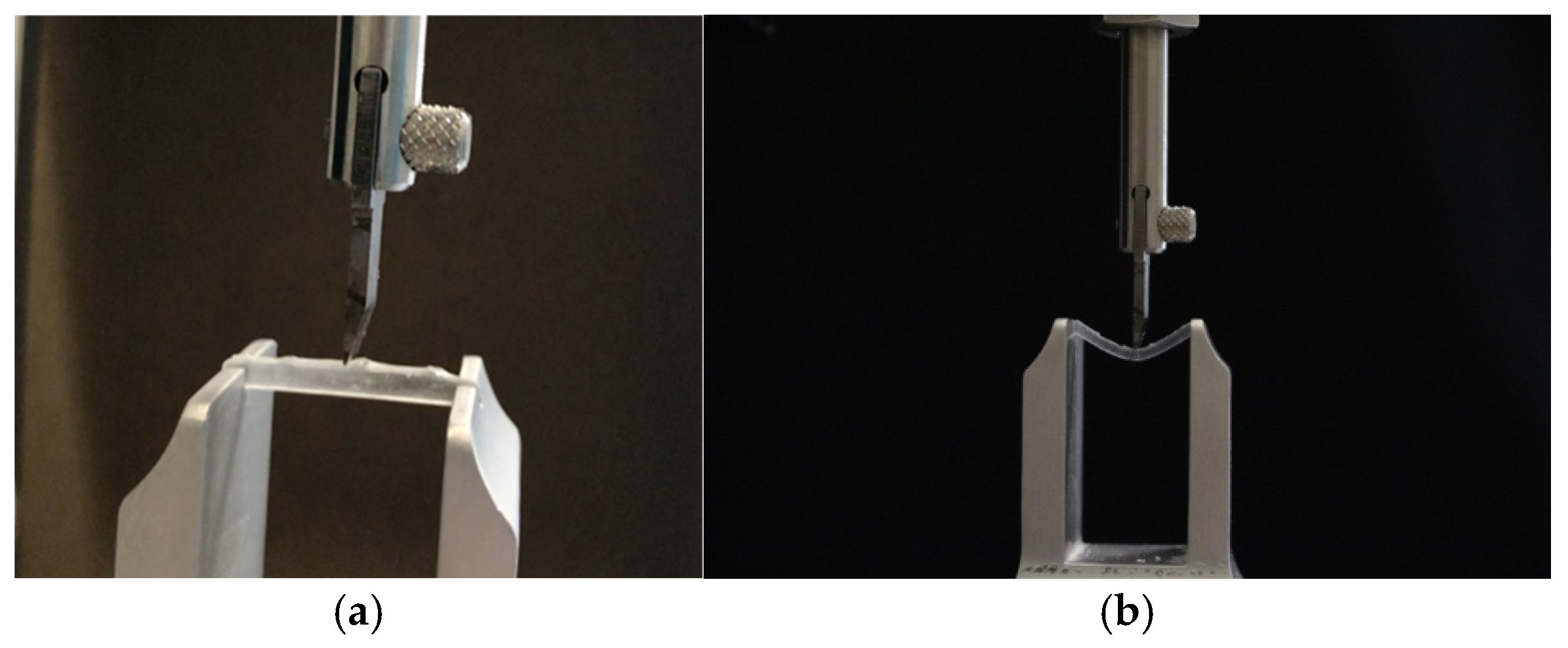
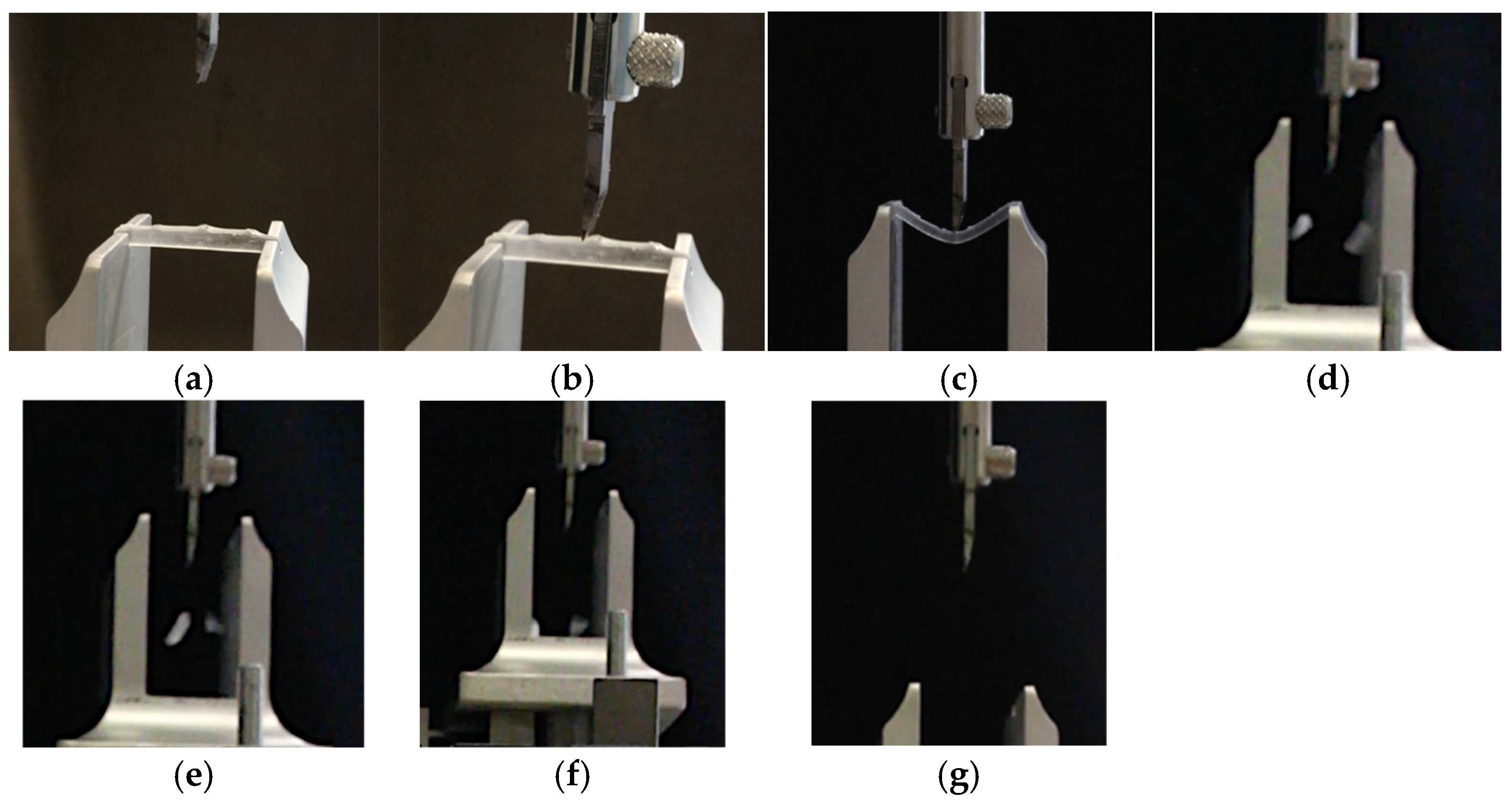
After post-processing, the temporary support structures generated during printing were carefully detached using precision cutters. This operation required particular attention to avoid deformation or surface defects that could compromise the dimensional accuracy of the specimens. The fabrication protocol was reproduced for each selected build orientation, 0° (horizontal), 45° (oblique), and 90° (vertical), which were chosen following the reference framework proposed by Unkovskiy et al. [
34].
These orientations represent typical manufacturing configurations, allowing evaluation of how the printing angle influences the mechanical response of photopolymer resins. Specifically, the 0° configuration corresponds to layers stacked parallel to the build platform, the 45° orientation represents an intermediate inclination, and the 90° setup involves layers deposited perpendicular to the platform.
Together, these positions provide a comprehensive overview of the role of layer orientation on structural performance. At the completion of all fabrication and curing steps, fifteen specimens were produced for each of the seven resin types investigated (Keyguide, Crown & Bridge, Bite, Vertysguide, Tera Harz TC-80DP, Ivory, and NextDent Cast). All samples exhibited standardized rectangular bar dimensions of 2 mm × 2 mm × 25 mm (height × width × length). Printing was performed with the Moon Night DLP system (Vertysystem, Altavilla Vicentina, Italy), ensuring consistent manufacturing parameters and reproducibility across all experimental groups.