1. Introduction
Healthcare accessibility is a pervasive issue, particularly in medically underserved regions often categorized as healthcare deserts [
1]. These areas are characterized by a deficiency in healthcare professionals, substandard medical infrastructure, and logistical challenges that inhibit timely access to essential medical services [
2]. The World Health Organization (WHO) articulates that medically underserved areas have a lesser density of healthcare providers than necessary to meet community medical needs, resulting in elevated morbidity and mortality rates [
3]. Similarly, the Healthcare Accessibility Index (HAI) is often used to quantify disparities by evaluating factors such as travel time to healthcare facilities, the number of available specialists per capita, and healthcare affordability [
4]. In South Korea, regional disparities in healthcare access remain a pressing concern. A previous study applied the geospatial platform (ArcGIS Pro Ver.3.0.2., ESRI Inc., Redlands, CA, USA) and the Two-Step Floating Catchment Area (2SFCA) method to evaluate spatial accessibility to diabetes care, calculating an Accessibility Index to reveal significant regional inequalities—particularly in underserved areas like Hoengseong County in Gangwon Province [
5]. These findings, along with the limited availability of specialized services such as trauma care and hyperbaric oxygen therapy in low-HAI regions, underscore the urgent need for digital collaborative platforms like Dr. LINK, which aim to enhance care accessibility in medically marginalized communities. In South Korea, healthcare disparities are particularly evident in rural and remote regions. A national study on medical service accessibility found that over 60% of residents in non-metropolitan areas face difficulties in accessing specialized medical care, often traveling more than an hour to reach a tertiary hospital [
6]. Additionally, emergency medical response times in these regions are significantly longer, leading to higher rates of preventable deaths from acute conditions such as stroke and myocardial infarction [
7]. These challenges highlight the urgent need for innovative healthcare delivery models that can overcome geographical and infrastructural limitations.
One of the most promising solutions to mitigate healthcare accessibility gaps is telemedicine, which leverages digital communication technologies to provide remote medical consultations, diagnosis, and treatment [
8]. Telemedicine has been widely recognized for its potential to enhance healthcare equity by offering real-time consultations and remote patient monitoring, particularly in regions with limited medical personnel [
9]. Recent advancements in digital technologies, including artificial intelligence (AI), the Internet of Medical Things (IoMT), and cloud-based healthcare systems, have collectively enhanced telemedicine by enabling more efficient, data-driven, and coordinated healthcare delivery [
10]. Among various telemedicine models, remote collaborative care platforms have emerged as an essential approach to improving medical service delivery. These platforms integrate telecommunication tools with electronic health records (EHRs), AI-driven clinical decision support systems, and real-time patient monitoring to facilitate seamless cooperation among healthcare providers. By enabling multidisciplinary collaboration between primary care physicians and specialists, these platforms improve the accuracy of diagnoses, enhance treatment efficiency, and reduce the need for unnecessary hospital visits [
11].
Despite the growing adoption of telemedicine, existing solutions often focus on individual remote consultations rather than integrated, interdisciplinary collaboration. This limitation underscores the need for remote collaborative care platforms that facilitate continuous patient management through a team-based approach. By bridging the gap between local primary care providers and urban specialists, these platforms can ensure that patients in medically underserved regions receive high-quality medical care without requiring long-distance travel [
12].
Furthermore, real-world applications of telemedicine have demonstrated significant improvements in healthcare outcomes. A recent national study in South Korea reported that a web- and mobile-based tele-emergency system significantly reduced unnecessary patient transfers from rural areas, particularly in non-severe trauma cases. The expansion of telemedicine during the COVID-19 pandemic provided practical evidence of its potential, demonstrating improved medication adherence and care continuity for chronic disease patients [
13], thereby reinforcing the relevance of remote healthcare models such as Dr. LINK. Similar trends have been observed globally, with countries implementing AI-assisted telehealth platforms to optimize remote diagnostics and treatment plans [
14].
This study aims to develop a remote collaborative care platform tailored to the needs of medically underserved regions and to empirically evaluate its impact through real-world clinical application. Specifically, the platform will be deployed to support the treatment of patients requiring trauma care and hyperbaric oxygen therapy in geographically isolated or resource-limited areas. Through this empirical investigation, the study seeks to provide evidence for the clinical utility and scalability of remote collaborative care platforms as a sustainable solution to address healthcare disparities in underserved populations. The platform has undergone continuous refinement through pilot clinical applications at affiliated institutions. It remains a non-commercial research system without financial or proprietary conflicts of interest.
2. Platform Development and Empirical Study Design
2.1. Needs Assessment and Conceptualization of Dr. LINK Platform
Prior to the development of the remote collaborative care platform for trauma and hyperbaric oxygen therapy in underserved areas (Dr. LINK Platform®, HESEL Incorp., Seoul, Republic of Korea), a comprehensive needs assessment was conducted to identify the functional and service requirements for a remote collaborative care system. The development process involved several key steps: (1) environmental analysis, including examination of teleconsultation workflows and existing hospital information systems in regional hospitals to identify opportunities for process improvement and strategies for wider implementation; (2) information environment analysis and user requirements analysis, which synthesized insights and derived improvement directions; and (3) interviews and surveys with medical doctors to identify critical issues, workflow challenges, and user requirements.
A structured questionnaire comprising 11 categories was developed to collect user needs and expectations: (1) demographic characteristics, (2) awareness of non-face-to-face collaborative care, (3) experience with non-face-to-face collaboration care, (4) requirements for hospitals in vulnerable areas, (5) required patient information input for collaborative cases (tertiary hospitals), (6) importance of post-collaboration data entry for emergency teleconsultations (vulnerable-areas), (7) required information input for hyperbaric oxygen therapy (HBOT) cases (tertiary hospitals), (8) importance of post-collaboration data entry for HBOT cases (vulnerable-areas), (9) interface composition requirements for “collaboration acceptance” screens (vulnerable-areas), (10) interface requirements for teleconsultation video screens, and (11) expected effects of operating the remote collaborative care system.
Findings from this needs assessment directly informed the technical design and clinical validation framework of the Dr. LINK platform, ensuring that it could support efficient, accurate, and scalable remote collaborative care services tailored to the needs of healthcare providers in medically underserved regions.
2.2. Architecture of Dr. LINK Platform
Dr. LINK is a cloud-native teleconsultation platform developed to facilitate real-time collaborative care for emergency, trauma, and hyperbaric oxygen therapy (HBOT). It is provided in a Software-as-a-Service (SaaS) model, thereby minimizing the IT adoption risk on institutions and stakeholders (e.g., patch management, update deployment) by offering a fully managed service. Internally, the system is operated in a Platform-as-a-Service (PaaS) environment, enabling application development and operations on cloud infrastructure without dedicated physical servers. Unlike on-premises approaches that require hospitals to install physical servers and manage the entire lifecycle from infrastructure to applications, Dr. LINK is built and operated on cloud platforms that support application development, testing, and deployment. This architecture allows seamless data exchange between local and remote hospitals, enabling real-time data storage, processing, and visualization throughout the consultation workflow.
The platform is designed with a multi-layered system architecture that integrates both the deployment-level cloud infrastructure and modularized software components into a unified framework. This architecture ensures operational scalability, maintainability, and security across all platform functionalities. A Zero Trust security model is applied throughout all layers to safeguard data integrity and prevent unauthorized access. The overall system architecture is presented through the following two views: the Physical Infrastructure View and the Logical & Component View.
2.3. Physical Infrastructure View
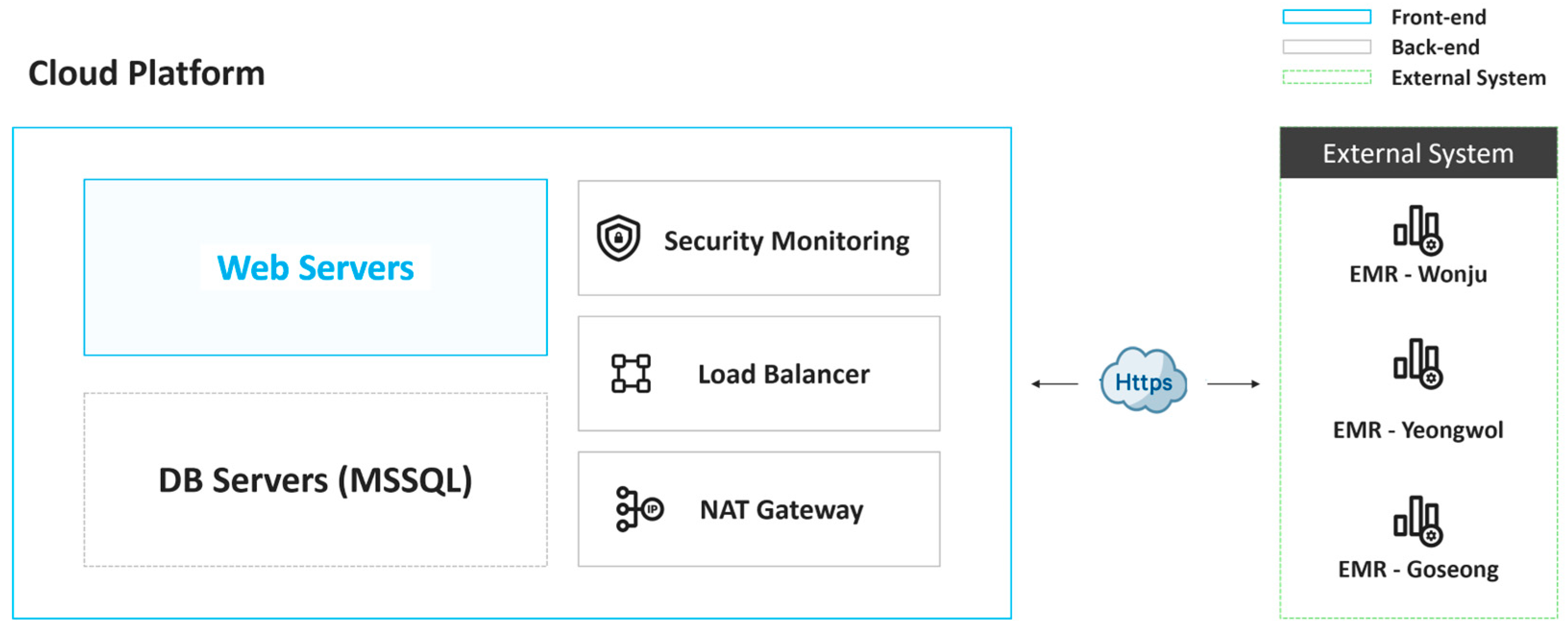
Dr. LINK operates within a cloud environment to optimize system scalability, resilience, and security (
Figure 1). The platform utilizes a load balancer to distribute incoming requests across auto-scaling web servers, ensuring consistent service availability and performance under varying loads. Clinical and consultation data are stored securely in a managed MSSQL database instance. To ensure secure communication and protect data in transit, all transmissions are encrypted using Secure Sockets Layer (SSL) protocols and routed through Network Address Translation (NAT) gateways. Furthermore, 24/7 security monitoring systems are implemented to detect and respond to potential threats in real time, thus maintaining the platform’s operational integrity and data protection standards.
2.4. Software Architecture as Logical & Component View
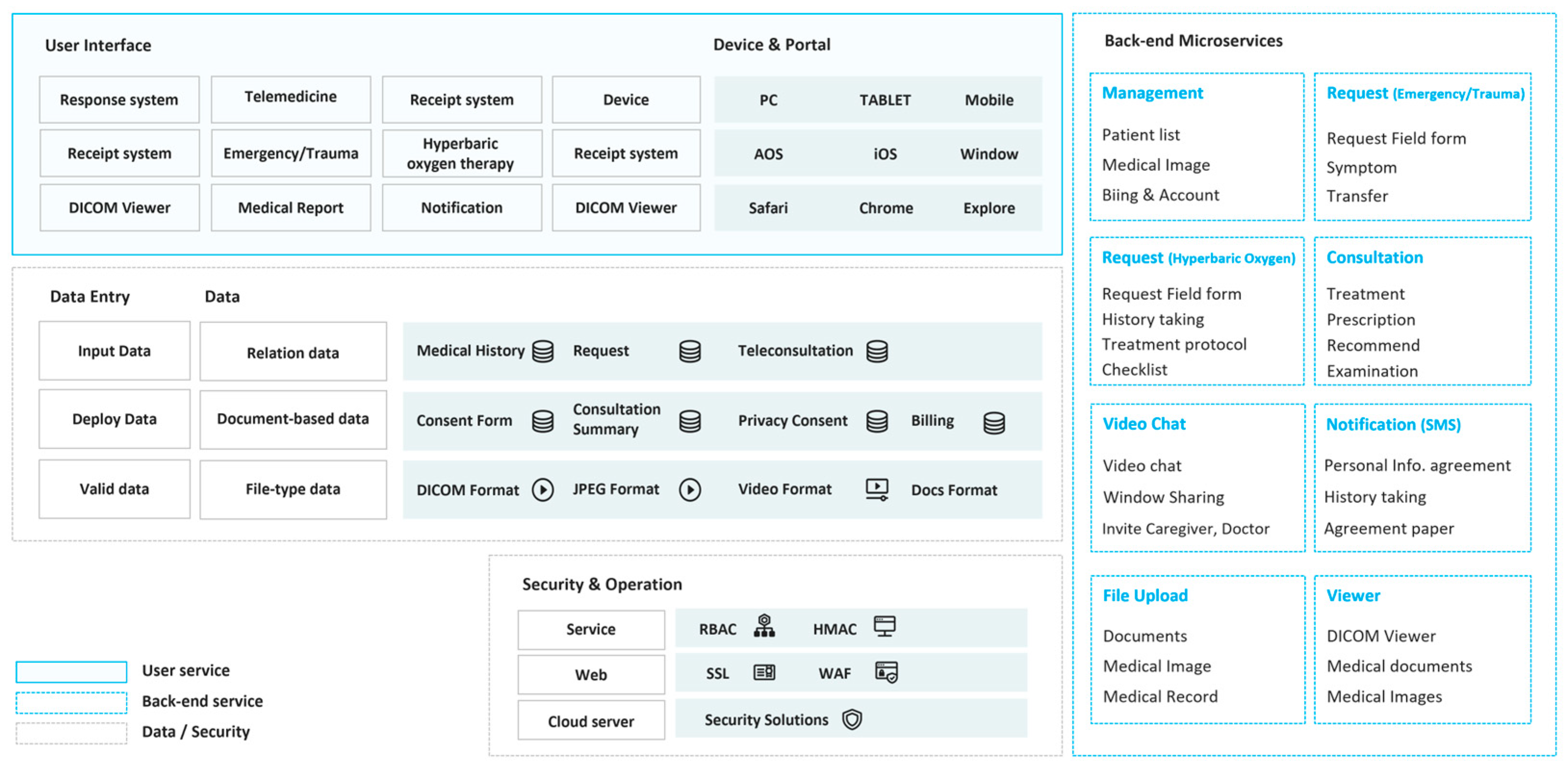
The platform follows a layered software architecture comprising the User Interface Layer, Client Data Entry Layer, Back-End Microservices Layer, and Data Persistence Layer, designed under the Zero Trust principle to secure all internal interactions (
Figure 2). It also employs an event-driven architecture that facilitates real-time asynchronous messaging across services during consultation requests, responses, and notification events, ensuring instantaneous user feedback.
2.4.1. User Interface Layer
The user interface layer, which forms the uppermost part of the Dr. LINK platform, was developed using Vue.js, a progressive JavaScript framework for building responsive and interactive web interfaces. This layer provides a user-friendly clinical interface that supports key functions such as consultation requests, response management, and real-time inter-hospital communication. By adopting a single-page application (SPA) architecture, the system allows data to update seamlessly without full-page reloads, thereby improving responsiveness and usability during time-sensitive consultations. The interface consists of modular components corresponding to clinical tasks—such as patient data entry, feedback exchange, and notification management—to ensure scalability and maintainability. Real-time communication between clinicians is supported by server push technology, enabling instant updates on consultation progress and alerts. This architecture ultimately enhances the speed and efficiency of collaborative clinical decision-making in remote and emergency care settings.
2.4.2. Client Data Entry & Interaction Layer
The client input layer is designed to systematically capture structured data entered by medical personnel and ensure its reliable and consistent transmission within the system. It was developed using Vue.js, a lightweight JavaScript framework that enables dynamic and interactive data input through web-based forms. Each field undergoes real-time validation to prevent input errors, and the collected data are automatically formatted into a standardized structure for secure transfer to the backend server. Asynchronous communication protocols are employed to transmit validated data efficiently and securely, supporting essential clinical workflows such as initiating consultation requests, submitting expert feedback, and exchanging clinical notes. By simplifying the data entry process and reducing the cognitive load on users, this layer enhances data accuracy, workflow efficiency, and the timeliness of remote clinical consultations.
2.4.3. Back-End Microservices Layer
The Back-end Microservices Layer of Dr. LINK is composed of several independent microservices, each designed to manage specific functionalities essential for the platform’s operation. These microservices enable the platform to handle diverse aspects of telemedicine consultations, ensuring seamless and efficient operations across various processes.
Consultation Request Management: This module facilitates the registration and management of new consultation requests and supports associated processes such as fee billing and reconciliation.
Emergency/Trauma Consultation Service: This service enables the creation and upload of emergency and trauma medical records, ensuring timely documentation for critical cases.
Hyperbaric Oxygen Consultation Service: This service manages the intake process for hyperbaric oxygen therapy consultations, including initial form submission, adaptation assessments, protocol sharing, and pre-treatment checklist completion.
Consultation Response Service: This module allows clinicians to input clinical opinions and response notes in reply to consultation requests.
Telemedicine Service: This service provides real-time video communication capabilities, facilitating remote consultations between healthcare providers and patients.
Notification Service: This system sends automated notifications regarding key events, such as the submission of new consultation requests and the receipt of responses.
File Upload Service: This service supports the uploading of medical images and documents in various formats, including DICOM and PDF files, to ensure comprehensive information sharing.
File Viewer: This module enables the viewing of a wide range of medical record formats, such as DICOM images, JPG files, and AVI videos, within the platform.
2.4.4. Data Persistence Layer
The data generated during the consultation request and response process is stored and managed using MSSQL and PostgreSQL databases. All data is encrypted to ensure security, and sensitive information is pseudonymized for further protection. This includes relational data such as patient medical history, personal details, consultation requests, and responses. Additionally, document-based data, including telemedicine consent forms, privacy consent forms, and consultation summaries, are stored. Lastly, media files, such as medical records (documents), PDFs, medical images (DICOM), JPG, PNG, and AVI files, are also stored.
2.4.5. Security and Operations Layer
As shown in
Table 1, the Dr. LINK platform was designed in compliance with the ‘Zero Trust Guideline 2.0’ containing the Zero Trust Architecture (ZTA) principles distributed by the Korea Internet & Security Agency (KISA) [
15]. It is strengthened to enhance security across its entire system, incorporating SSL encryption and a Web Application Firewall (WAF). User management is handled through an ID lifecycle management system, which includes processes for creating, updating, and deleting user accounts, while also verifying user identities based on additional credentials, such as medical license numbers and copies. Access control is finely segmented using Role-Based Access Control (RBAC), ensuring that users have access only to the resources necessary for their roles. Furthermore, the platform employs an Intrusion Detection System (IDS) within the cloud infrastructure to provide continuous, 24/7 security monitoring and response capabilities, with established protocols for handling any incidents or system failures.
2.5. Data Processing and Communication
The Dr. LINK platform supports emergency teleconsultations by enabling medical staff to initiate consultation requests, which are then processed by the system on the server. Following processing, the results are sent back to the staff through real-time notifications, and consultation fees are generated for billing purposes. The main data flow within the platform is divided into three key stages: (1) consultation request input, (2) consultation response and action tracking, and (3) integration with hospital information systems (HIS) and event-driven notifications.
2.5.1. Consultation Request Input
A doctor from affiliated hospitals, mainly in medically underserved areas, entered patient data and submitted consultation requests through the Dr. LINK platform while treating patients. This will ensure that what you enter within the platform is serialized into JSON format on the client side. This data is then transmitted to the back-end microservices layer via an asynchronous API request. Upon receipt, the request is stored in a cloud database and assigned a unique consultation request ID, which sets its status to “pending.” The request is automatically routed to the designated medical institution selected in advance. An alert is sent to the doctors affiliated with the receiving institution via Dr. LINK’s integrated notification service. This ensures that the relevant clinical staff are notified in real-time, allowing for prompt review and response.
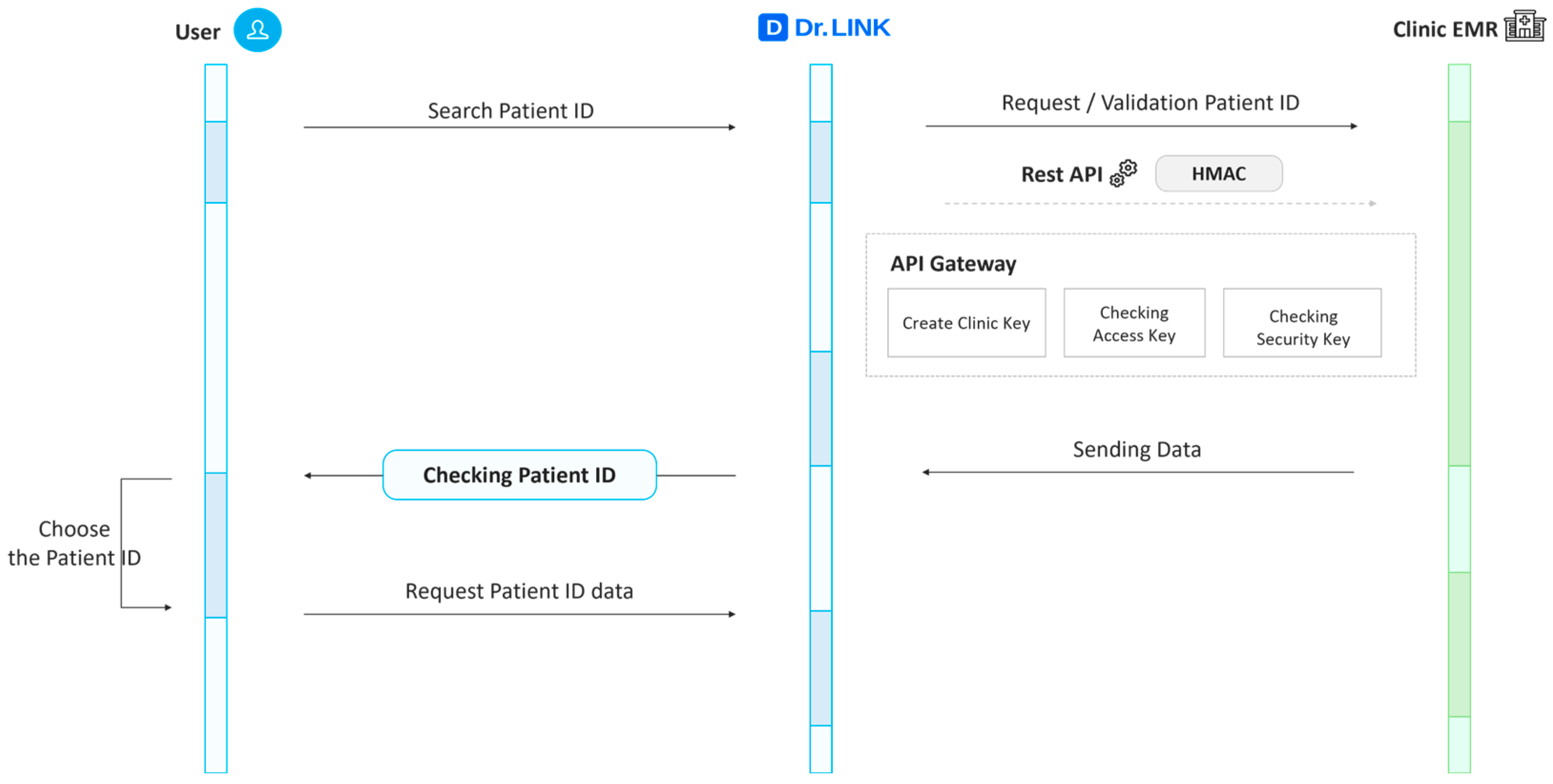
2.5.2. Consultation Response and Action Tracking
Once the receiving doctor reviews the consultation request, they submit a response, which is linked to the original consultation ID, updating its status accordingly. The requesting doctor is then notified of the response, and the consultation process is marked as complete. If the receiving institution is unable to accept the consultation, the platform allows for dynamic consultation transfer to an alternate institution. This feature ensures that no consultation request goes unanswered, facilitating seamless coordination between medical institutions (
Figure 3).
2.5.3. Integration with Hospital Information System (HIS) and Event-Driven Notifications
Dr. LINK seamlessly integrates with the hospital information systems (HIS) of two affiliated medical centers (Wonju, and Yeongwol) and one public health center (Goseong), via a standardized RESTful API. During the process of retrieving patient data from each institution’s EMR into Dr. LINK, institution-specific identification keys are defined, and an HMAC (Hash-based Message Authentication Code) based on an API access key and a security key is applied to verify the integrity of server-to-server communication. This integration ensures that essential patient data, such as demographics and clinical history, is retrieved efficiently during consultation requests, eliminating the need for duplicate manual input. The data is displayed in a structured format within the platform, enhancing consultation accuracy. Real-time event-driven notifications are also sent to the involved parties, ensuring immediate response and coordination (
Figure 4).
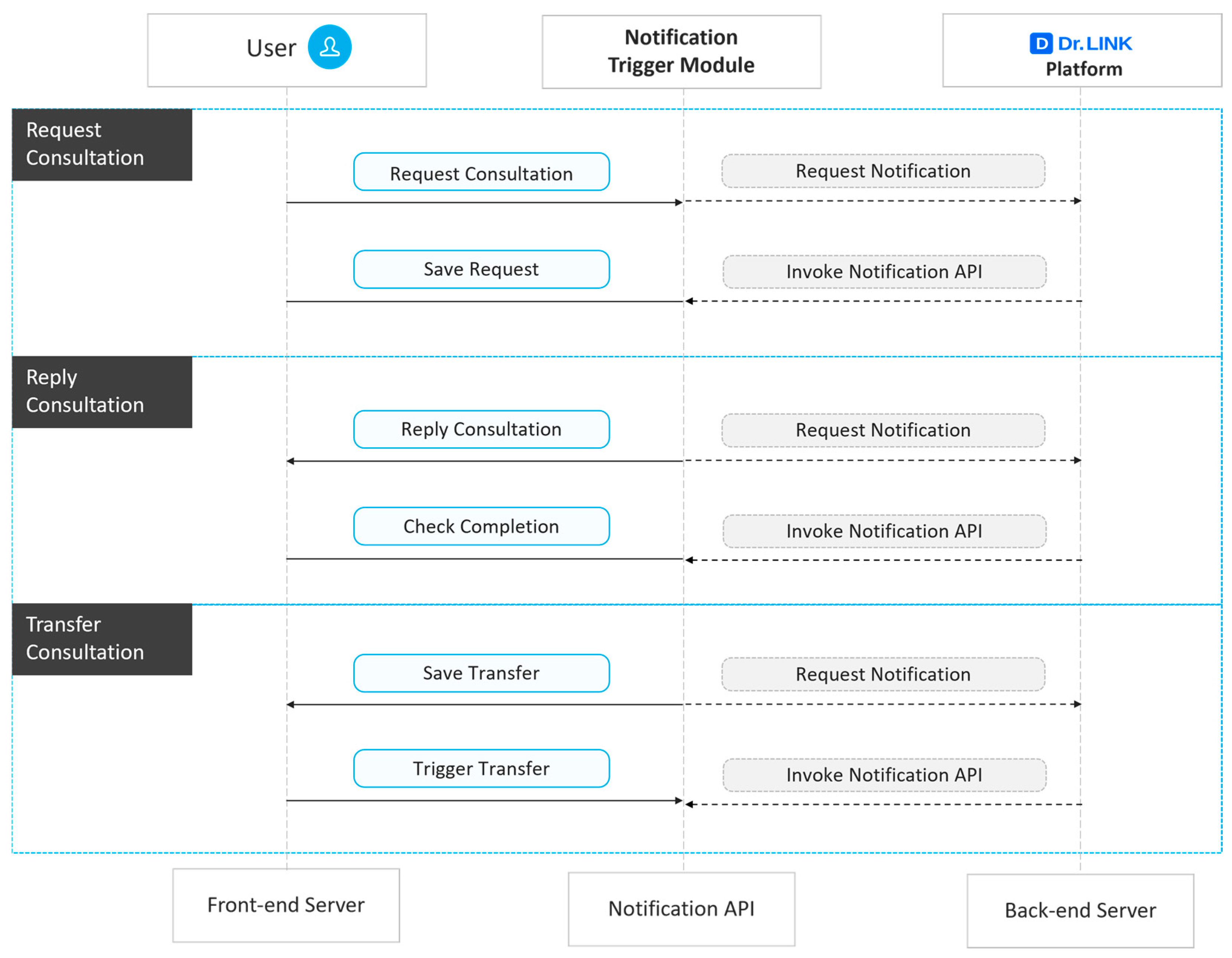
For key events such as consultation request creation, response submission, and consultation transfer, Dr. LINK promptly sends alerts to users via SMS or email using notification API of the commercial cloud platform (NAVER Cloud Platform
®, NAVER Cloud Corp., Seongnam, Republic of Korea), ensuring reliable message delivery (
Figure 5). These alerts are template-based and tailored to the specific event type, with all external communications secured via HTTPS. Moreover, logs are maintained to track delivery status, including success/failure flags and timestamps.
2.6. Design of Empirical Research
Using the Dr. LINK platform, an empirical study has been designed to evaluate the effectiveness of a remote collaborative care system in emergency medicine and hyperbaric oxygen therapy settings, particularly in underserved areas. The study was conducted over a three-month period from June to August 2024 across two affiliated medical centers (Wonju, and Yeongwol) and one public health center (Goseong), during which data on remote consultations were continuously collected and analyzed. This study focused on emergency (trauma and non-trauma) care and hyperbaric oxygen therapy (HBOT), which requires rapid multidisciplinary decision-making. The inclusion criteria were all patients (acute trauma/non-trauma patients presenting to the emergency room, HBOT patients) in need of treatment who visited hospitals in medically underserved areas and decided to participate after hearing an explanation about this study. Exclusion criteria included patients not consenting to participate or if the medical staff deemed them unsuitable to participate in this study. This service is often concentrated in tertiary hospitals, and access to trauma specialists and HBOT rooms is limited in medically underserved areas. Therefore, two medical centers and one public health center in medically underserved areas were recruited to participate in this study. Especially, one public health center was selected because of the significant need for HBOT among residents engaged in plain diving and fisheries. Dr. LINK is designed to improve timely decision support in these highly dependent clinical areas by facilitating telemedicine collaboration between medical providers in these underserved areas and tertiary hospitals. It will analyze the utility and clinical benefits of remote collaboration for patients and medical staff in these settings. The study was approved by the Institutional Review Board of Wonju Christian Hospital (IRB approval no.: CR324057; approval date: 8 August 2024) and the Clinical Research Information Service of the Korea Disease Control and Prevention Agency (Trial registration no.: KCT0010592; registration date: 5 June 2025). This clinical study will be conducted in compliance with the International Conference on Harmonization (ICH) Guidelines and the principles of the Declaration of Helsinki, and will adhere to the Korean Good Clinical Practice (KGCP) and related regulations, taking into account the rights and safety of the subjects. All participants provided written informed consent prior to participation in the study.
2.6.1. Evaluation Metrics
The evaluation method utilized the Telehealth Usability Questionnaire (TUQ) for assessing the usability of remote consultation [
17]. The questionnaire was reviewed by three emergency medicine specialists and used to assess patient (and caregiver) satisfaction in this study. To address concerns regarding the reliability of responses that could be skewed by participants choosing extreme or middle values on a 5-point Likert scale, the scale was revised to a 7-point Likert scale [
18]. The questionnaire consisted of 18 items, categorized into five evaluation criteria as shown in
Table 2: (1) the usefulness of remote consultation, (2) ease of use and learnability of remote consultation, (3) the quality of the remote consultation platform, (4) the quality of interaction during remote consultation, and (5) the trustworthiness of remote consultation.
2.6.2. Statistical Analysis
The statistical analysis for this study will be conducted using IBM SPSS Statistics Version 29.0 (IBM Corp., Armonk, NY, USA). Nominal variables will be analyzed using frequency distributions and percentages, and differences between groups will be tested using chi-square or Fisher’s exact tests. For continuous variables, normality will be assessed using Kolmogorov–Smirnov or Shapiro–Wilk tests, and depending on the data’s distribution, differences will be analyzed using t-tests or Mann–Whitney U tests, with a significance level set at 0.05. In addition to p-values, effect sizes were calculated to evaluate the practical significance of observed differences. Cohen’s d was computed for continuous variables, and Cramer’s V for categorical variables, following conventional interpretive thresholds. These statistical methods will ensure robust, reliable results, providing meaningful insights into the effectiveness and practicality of the remote collaborative care system.
3. Results
3.1. Comparison with Existing Digital Health Platforms
Digital healthcare platforms have been developed to address different aspects of patient care. The Lifelog Big Data Platform focuses on enhancing healthcare services by integrating individualized lifelogs with clinical data. Its goal is to build a sustainable digital healthcare ecosystem through standardized data management and analysis systems [
19]. Furthermore, the MEDBIZ platform focuses on monitoring patient conditions through real-time data collection and analysis, and developing digital therapeutics and medical services based on this data. Its strength lies in its self-management capabilities, which leverage wearable devices and mobile apps [
20].
As shown in
Table 3, the Dr. LINK platform distinguishes itself through its focus on real-time, high-fidelity telecollaboration for critical and specialized care while sharing certain technological foundations with existing digital health platforms. Dr. LINK emphasizes urgent clinician-to-clinician interaction for trauma, emergency, and hyperbaric oxygen therapy, whereas the Lifelog Bigdata Platform is oriented toward long-term preventive health and MEDBIZ toward precision medicine and chronic disease management. Despite these differing priorities, all three platforms leverage digital technologies to enhance clinical decision-making and patient care.
Dr. LINK integrates medical imaging, vital signs, and clinical records, complementing Lifelog Bigdata platform’s wearable and EMR-derived datasets and MEDBIZ platform’s IoMT-collected patient data. Standardization approaches differ with HIS APIs for Dr. LINK, unified keys for Lifelog, and HL7 and FHIR for MEDBIZ, yet all platforms aim to ensure interoperability and structured data exchange. Data processing is performed on cloud infrastructure across the platforms with Dr. LINK employing microservices for low-latency collaboration, Lifelog using data warehouse analytics for longitudinal insights, and MEDBIZ combining real-time streaming with batch processing.
Security measures vary with Dr. LINK implementing a Zero Trust framework, Lifelog following ISO and CSAP standards [
21,
22], and MEDBIZ relying on encryption and de-identification protocols. Analytically, Dr. LINK prioritizes real-time alerts and status monitoring while Lifelog provides health statistics and MEDBIZ offers AI-driven predictive analytics, yet all provide actionable insights to improve care. Service offerings differ in scope with Dr. LINK supporting multi-party teleconsultation, Lifelog offering personalized health management, and MEDBIZ integrating multiple digital interfaces. Scalability is addressed in all three platforms with Dr. LINK focusing on multi-hospital expansion, Lifelog on multi-institutional and long-term data aggregation, and MEDBIZ on modular cloud-native growth. Each platform’s strengths reflect its primary purpose with Dr. LINK delivering ultra-low latency secure telecollaboration, Lifelog excelling in longitudinal multi-source integration, and MEDBIZ providing continuous IoMT-driven insights.
3.2. Usability Assessment of Remote Consultation
As shown in
Table 4, a total of 42 patients who had experienced consecutively remote consultation through the Dr. LINK platform participated in the usability assessment. The overall mean age was 68.2 ± 17.0 years, with subgroup means of 43.8 ± 17.4 years for emergency care patients and 74.0 ± 10.8 years for HBOT patients. The sex distribution was 35 males (83.3%) and 7 females (16.7%), with 3 males (37.5%) and 5 females (62.5%) in the emergency care group, and 32 males (94.1%) and 2 females (5.9%) in the HBOT group. Regarding socioeconomic and lifestyle factors, 8 participants (19.0%) were economically active (6/8 in emergency care, 2/34 in HBOT), while 34 (81.0%) were not. Three participants (7.1%) reported current smoking (all in the emergency care group), and four (9.5%) reported alcohol consumption (all in the emergency care group). Participants were recruited from medically underserved regions, and prior exposure to telemedicine or digital tools was minimal, reflecting the target population for the Dr. LINK platform. As this study was designed as an exploratory usability evaluation rather than a hypothesis-driven efficacy trial, no a priori power analysis was performed. Nonetheless, the sample size of 42 was considered sufficient to provide stable descriptive and nonparametric analyses, consistent with prior usability research demonstrating that 30–50 participants typically yield reliable results [
23].
The Telehealth Usability Questionnaire (TUQ) was administered immediately after each participant completed a remote consultation session to assess real-time user experiences and satisfaction with the system. Although patients did not directly operate the Dr. LINK platform, they experienced remote consultations as local clinicians at underserved hospitals performed teleconsultations with specialists at the tertiary hospital. Because the local clinicians were not specialists in the patients’ clinical domains, they relied on guidance from the tertiary hospital specialists to support patient care. Therefore, the TUQ responses reflect patients’ indirect experience of system usability, including perceived workflow, communication, and overall effectiveness during actual consultations.
Table 5 presents the TUQ results for patients who used the Dr. LINK remote collaborative care platform. Overall, participants reported strongly positive perceptions of system usability, with mean scores across all domains ranging from 6.71 to 6.83 on the 7-point scale. These results indicate consistently favorable user responses, although it should be noted that the TUQ does not include standardized cut-off values for defining “high” or “low” usability. Therefore, these findings should be interpreted as relatively high levels of user agreement rather than absolute benchmarks of satisfaction.
Subgroup comparisons revealed meaningful differences between emergency care patients (n = 8) and HBOT patients (n = 34). The HBOT group consistently reported higher usability ratings, with mean scores approaching the upper limit of the scale (e.g., 6.97 ± 0.17), whereas emergency care patients showed greater variability and slightly lower averages.
Independent-samples t-tests (with Welch correction when variances were unequal) and Mann–Whitney U tests were conducted to examine group differences. Levene’s test indicated violations of variance homogeneity for several variables, so non-parametric analyses were additionally performed to address potential deviations from normality. The results showed statistically significant between-group differences for most items (p < 0.05), except SFT-2, suggesting that these patterns are robust and consistent across statistical methods.
Across all domains, including Usefulness (UFN), Ease of Use & Learnability (ELA), Interface Quality (IFQ), Interaction Quality (IAQ), Reliability (RLA), and Satisfaction (SFT), HBOT patients consistently reported higher scores. In the Usefulness domain, UFN-1 (p = 0.021) and UFN-2 (p = 0.037) were significantly higher in the HBOT group, while UFN-3 approached significance (p = 0.055). For Ease of Use & Learnability, all items (ELA-1 to ELA-3) showed significant differences (p < 0.05), indicating that HBOT patients found the system easier to use and learn. Interface Quality (IFQ-1 to IFQ-4) and Interaction Quality (IAQ-1 to IAQ-4) also demonstrated significant differences (p = 0.009–0.055), suggesting superior design, responsiveness, and engagement among HBOT patients. Reliability scores were higher in the HBOT group (RLA-1: p = 0.007; RLA-2: p = 0.021), indicating greater perceived system dependability. In the Satisfaction domain, SFT-1 differed significantly (p = 0.047), whereas SFT-2 did not (p = 0.070), suggesting that while overall satisfaction was high, some aspects may vary by patient context. Importantly, these differences corresponded to large practical effect sizes: Cohen’s d values ranged from approximately 0.94 to 1.80 (most items > 1.1), indicating medium-to-very-large practical differences in perceived usefulness, ease of use, interaction quality, reliability, and overall satisfaction in favor of HBOT patients. For example, the reliability item (RLA-1) showed a very large effect (d ≈ 1.80), and interaction quality (IAQ-2) also showed a very large effect (d ≈ 1.77).
These findings suggest that HBOT patients who undergo scheduled, repeated, and relatively stable procedures may experience and evaluate the platform more favorably, whereas emergency/trauma encounters, characterized by urgent, unpredictable, and high-pressure conditions, may limit the perceived usefulness or ease of use of the system. Given the small emergency subgroup (n = 8), these effect size estimates should be interpreted cautiously; nevertheless, the magnitude of d values supports the practical relevance of the observed group differences beyond statistical significance alone.
4. Discussion
The Dr. LINK platform offers a distinct technical advantage through its specialization in real-time, high-fidelity telecollaboration for critical and specialized medical care. Its implementation represents a significant advancement in mitigating healthcare disparities in medically underserved regions, particularly in trauma care and hyperbaric oxygen therapy (HBOT). By leveraging cloud-native architecture, real-time communication, and seamless integration with existing hospital information systems (HIS), Dr. LINK enables efficient collaboration between local primary care providers and urban specialists. This design aligns with evidence supporting the efficacy of telemedicine in improving healthcare delivery and outcomes in resource-limited settings [
24].
In contrast to MEDBIZ, which emphasizes continuous IoMT-based patient monitoring and AI-driven predictive analytics for precision medicine, Dr. LINK is optimized for synchronous, clinician-to-clinician interaction, making it particularly effective for emergency response, trauma management, and specialized treatments such as HBOT [
19]. Compared with the Lifelog Bigdata Platform, which focuses on aggregating and analyzing long-term, multi-source health datasets for preventive and population-level research, Dr. LINK delivers immediate clinical impact by bridging geographical and institutional gaps in care [
20]. By prioritizing urgent, collaborative workflows, Dr. LINK serves as a critical enabler of equitable access to advanced medical expertise, especially in underserved or remote regions. To clarify the scope of this comparison, it should be noted that the evaluation of Dr. LINK relative to Lifelog and MEDBIZ is purely conceptual. Empirical validation of Dr. LINK against these existing platforms has not yet been performed, and future studies are planned to systematically assess comparative performance and clinical outcomes.
Our findings align with prior studies that emphasize the benefits of multidisciplinary telemedicine platforms in optimizing patient care pathways. For instance, Greenhalgh et al. highlighted the importance of platform adaptability and end-user involvement in the success of remote care models [
12]. Similarly, the integration of AI and IoMT technologies into telemedicine infrastructure has been shown to improve diagnostic accuracy and treatment decision-making, as demonstrated in recent global case studies [
25]. While prior studies have reported that tele-emergency systems reduced unnecessary patient transfers and improved clinical outcomes, our study did not empirically evaluate such effects. The current findings are limited to usability and satisfaction metrics, and further research is needed to assess clinical and operational impact. Notably, Dr. LINK addresses a critical limitation observed in earlier telehealth solutions—namely, the lack of support for ongoing, team-based care management. Prior platforms often facilitated one-time consultations without enabling sustained interdisciplinary collaboration or integration into clinical workflows [
26]. In contrast, Dr. LINK’s event-driven microservices and EHR integration ensure continuity of care and reduce the burden of redundant data entry, both of which have been cited as barriers to provider adoption in telemedicine [
27].
Another notable contribution of this study lies in the empirical evaluation of the platform through real-world application in trauma and hyperbaric oxygen therapy (HBOT) settings. Trauma care in rural and remote areas often suffers from delayed interventions due to the lack of immediate access to specialized medical personnel. Few telemedicine systems have been evaluated in these specialized domains, despite growing evidence of their importance in emergency response scenarios [
28]. Telemedicine platforms have been shown to mitigate these challenges by enabling remote consultations and real-time decision-making. For instance, the use of telepresence in trauma surgery has been associated with improved initial evaluations and treatment plans, leading to better patient outcomes and reduced costs [
29]. Dr. LINK’s integration of real-time video communication and structured data exchange supports these findings, offering a scalable solution to enhance trauma care in underserved regions. In addition, HBOT requires specialized equipment and trained personnel, which are often unavailable in remote areas. Telemedicine platforms can bridge this gap by facilitating remote assessments and consultations. Recent studies have highlighted the potential of HBOT in improving neurocognitive functions and reducing fatigue in patients with post-COVID-19 conditions, indicating broader applications of this therapy [
30]. Dr. LINK’s capability to manage HBOT consultations, including protocol sharing and pre-treatment assessments, ensures that patients in underserved areas can access this therapy with guidance from specialists, thereby expanding the reach of HBOT services.
The success of telemedicine platforms hinges on their usability and acceptance by healthcare providers. The Telehealth Usability Questionnaire (TUQ) employed in this study offers a comprehensive assessment of user satisfaction, encompassing factors such as usefulness, ease of use, and trustworthiness [
16]. While the TUQ serves as a valuable and widely used instrument, it does not establish fixed thresholds for interpreting absolute satisfaction levels. Therefore, the present findings should be viewed as indicative of relatively high perceived usability within the scale’s range rather than as definitive categorical ratings. Dr. LINK’s user-centric design and real-time feedback mechanisms are likely to foster similar levels of engagement and satisfaction among medical staff.
However, the study also acknowledges several limitations. First, the empirical evaluation involved a relatively small sample size (n = 42) across three affiliated institutions in South Korea. Therefore, the results should be interpreted as preliminary evidence of feasibility rather than definitive proof of clinical effectiveness Second, the study did not include a control or comparison group, making it impossible to assess the platform’s impact relative to standard care. Future large-scale evaluations involving a broader range of participants and institutions are warranted to confirm the generalizability of these findings across diverse healthcare settings with differing infrastructure or regulatory environments. Lastly, while the platform was designed for scalability, further stress-testing in higher-demand environments is necessary. Lastly, future studies should explore the integration of patient-reported outcomes and long-term health impact assessments to comprehensively evaluate the platform’s clinical utility.
During the implementation period of the Dr. LINK platform, no adverse events, communication errors, data breaches, or delays in patient management were reported. To ensure patient safety, the platform incorporated multiple safeguards, including encrypted data transmission, real-time alert systems, and 24/7 security monitoring. These mechanisms were designed to detect and respond to potential risks promptly. Although safety was not a primary focus of this study, as it centered on usability, future research should include formal safety assessments to further validate the platform’s reliability in emergency and trauma care settings.
5. Conclusions
This study demonstrates that the Dr. LINK platform, as a cloud-native teleconsultation system, effectively enhances access to emergency and hyperbaric oxygen therapy (HBOT) in medically underserved areas by enabling structured, real-time, and interdisciplinary collaboration. By overcoming geographic and infrastructural barriers, the platform offers a scalable, secure, and adaptable digital health solution suitable for a variety of clinical settings.
The successful implementation and empirical validation of Dr. LINK would be provided not only a practical framework for future remote collaborative care platforms but also contributes meaningfully to ongoing efforts to reduce healthcare disparities. As digital health technologies continue to advance, platforms like Dr. LINK could be poised to play a pivotal role in driving the transformation toward more equitable, efficient, and sustainable models of healthcare delivery.
Ultimately, Dr. LINK exemplifies the transformative potential of telemedicine in bridging critical gaps in specialized care, particularly in trauma and HBOT, across underserved regions. Continued refinement and rigorous evaluation will be essential to fully realize its long-term impact on healthcare equity and outcomes.