Optimizing Printing Temperature and Post-Curing Time for Enhanced Mechanical Property and Fabrication Reproducibility of 3D-Printed Dental Photopolymer Resins
Abstract
1. Introduction
2. Materials and Methods
2.1. Pilot Test
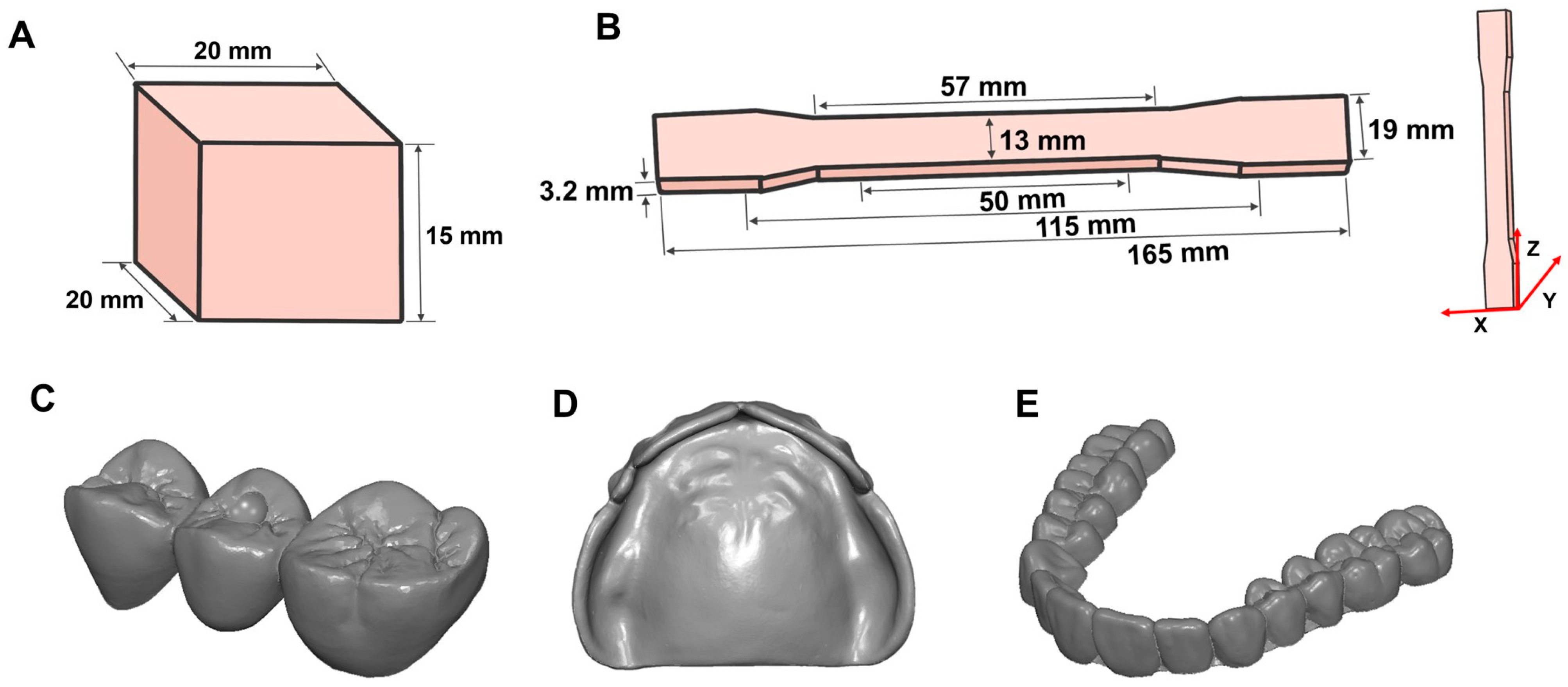
2.2. Specimen Preparation
2.3. Evaluation of Double-Bond Conversion
2.4. Evaluation of Tensile Strength
2.5. Evaluation of Fabrication Reproducibility
2.5.1. Temporary Crowns
2.5.2. Denture Bases
2.5.3. Clear Aligners
2.6. Statistical Analysis
3. Results
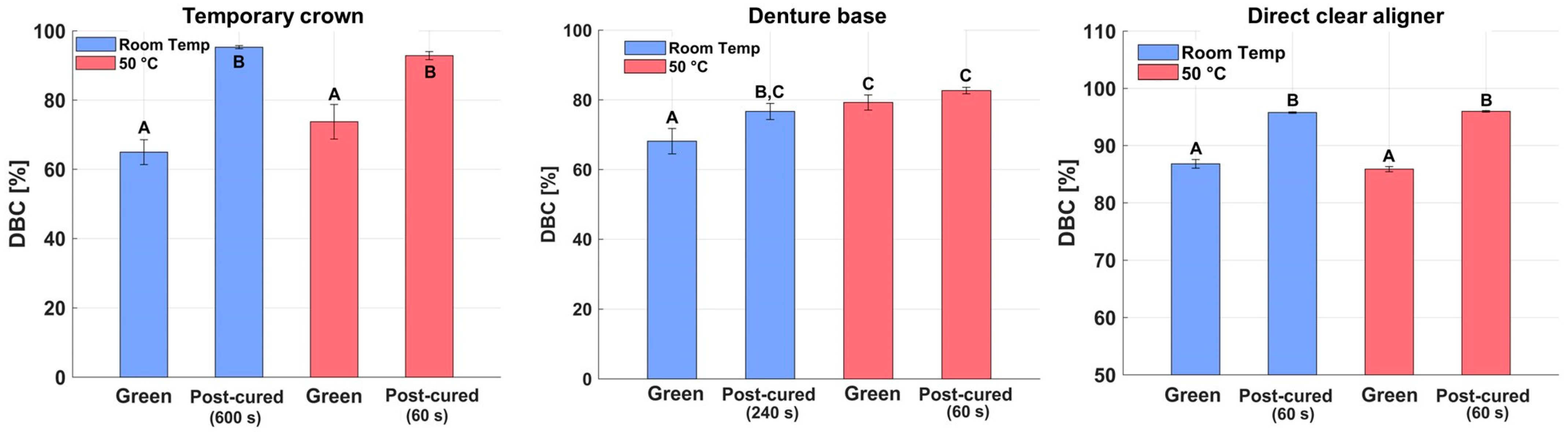
3.1. Results of Double-Bond Conversion
3.1.1. Results of DBC Test for Temporary Crown Resin
3.1.2. Results of DBC Test for Denture Base Resin
3.1.3. DBC of Direct Clear Aligner Resin
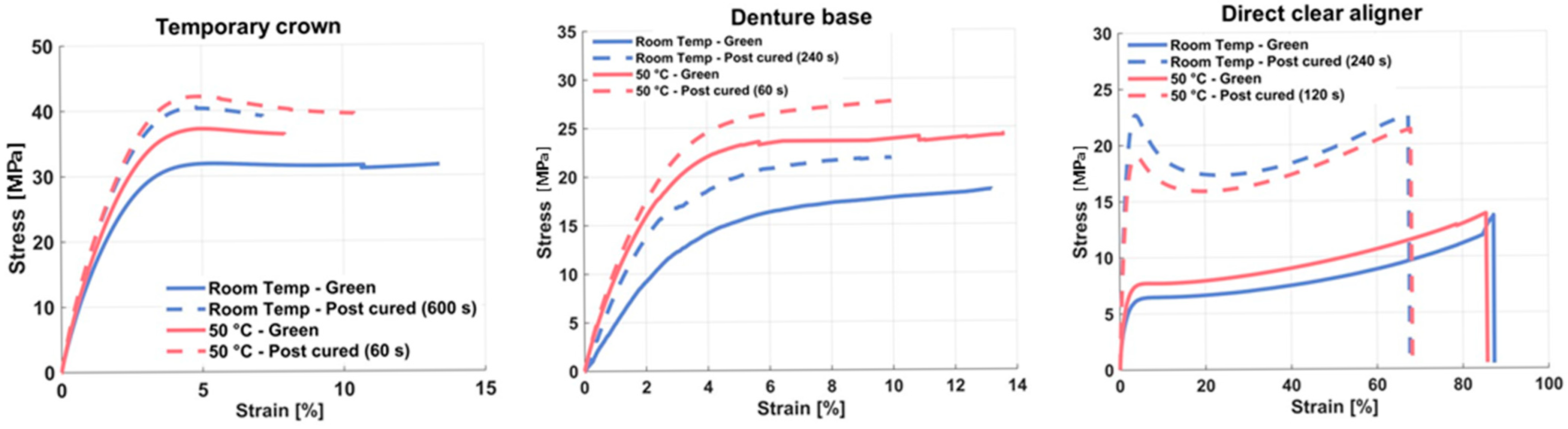
3.2. Results of Tensile Test
3.2.1. Results of Tensile Test for Temporary Crown Resin
3.2.2. Results of Tensile Test for Denture Base Resin
3.2.3. Results of Tensile Test for Direct Clear Aligner Resin
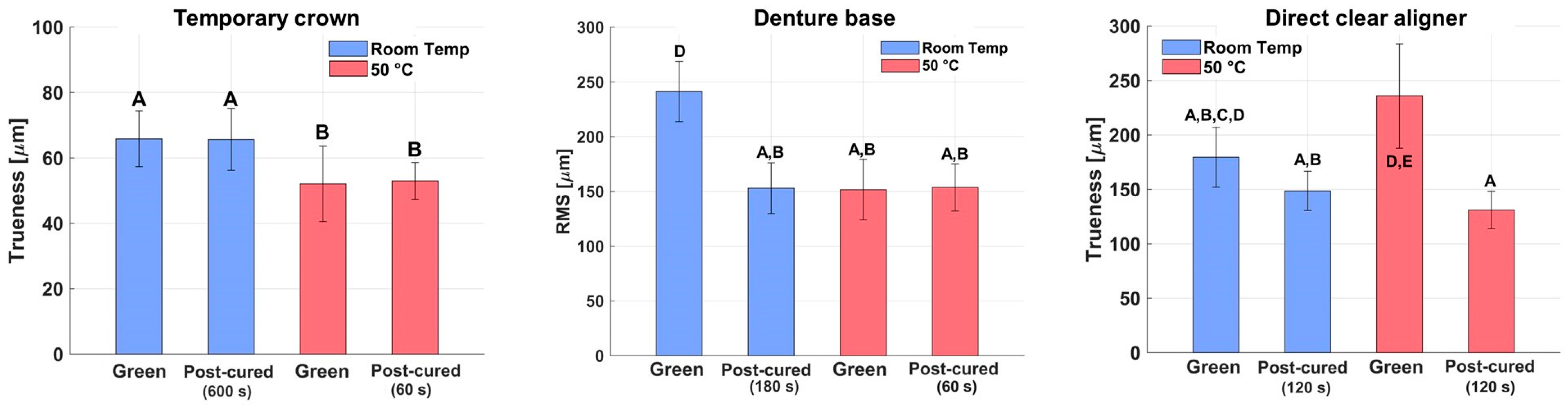
3.3. Results of Fabrication Reproducibility
3.3.1. Results of Fabrication Reproducibility for Temporary Crown Resin
3.3.2. Results of Fabrication Reproducibility for Denture Base Resin
3.3.3. Results of Fabrication Reproducibility for Direct Clear Aligner Resin
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tichá, D.; Tomášik, J.; Oravcová, Ľ.; Thurzo, A. Three-Dimensionally-Printed Polymer and Composite Materials for Dental Applications with Focus on Orthodontics. Polymers 2024, 16, 3151. [Google Scholar] [CrossRef]
- Narongdej, P.; Hassanpour, M.; Alterman, N.; Rawlins-Buchanan, F.; Barjasteh, E. Advancements in Clear Aligner Fabrication: A Comprehensive Review of Direct-3D Printing Technologies. Polymers 2024, 16, 371. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Alghauli, M.A.; Aljohani, M.H.A.; Zafar, M.S. Advanced Additive Manufacturing in Implant Dentistry: 3D Printing Technologies, Printable Materials, Current Applications and Future Requirements. Bioprinting 2024, 42, e00356. [Google Scholar] [CrossRef]
- Azab, A.; Abdelhady, W.A.; Elwakeel, E.; Ashraf, M.; Wally, R.; Soliman, A.; Mohamed, M.A.; Abozaid, D. Systematic Review and Meta-Analysis of Mechanical Properties of 3D Printed Denture Bases Compared to Milled and Conventional Materials. Sci. Rep. 2025, 15, 29207. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.H.; Majeed, M.A. Milling Versus Printing: The Effect of Fabrication Technique on the Trueness and Fitness of Fabricated Crowns (A Comparative In Vitro Study). Prosthesis 2025, 7, 107. [Google Scholar] [CrossRef]
- Kirby, S.; Pesun, I.; Nowakowski, A.; França, R. Effect of Different Post-Curing Methods on the Degree of Conversion of 3D-Printed Resin for Models in Dentistry. Polymers 2024, 16, 549. [Google Scholar] [CrossRef]
- Aktug Karademir, S.; Atasoy, S.; Akarsu, S.; Karaaslan, E. Effects of Post-Curing Conditions on Degree of Conversion, Microhardness, and Stainability of 3D Printed Permanent Resins. BMC Oral Health 2025, 25, 304. [Google Scholar] [CrossRef]
- Aksoy, M.; Topsakal, K.G.; Süküt, Y.; Duran, G.S. Post-Curing Protocols and Dimensional Accuracy of 3D-Printed Resin Materials. Clin. Investig. Orthod. 2025, 2025, 1–8. [Google Scholar] [CrossRef]
- Hassanpour, M.; Narongdej, P.; Alterman, N.; Moghtadernejad, S.; Barjasteh, E. Effects of Post-Processing Parameters on 3D-Printed Dental Appliances: A Review. Polymers 2024, 16, 2795. [Google Scholar] [CrossRef] [PubMed]
- Steyrer, B.; Busetti, B.; Harakály, G.; Liska, R.; Stampfl, J. Hot Lithography vs. Room Temperature DLP 3D-Printing of a Dimethacrylate. Addit. Manuf. 2018, 21, 209–214. [Google Scholar] [CrossRef]
- Kim, H.; Han, S.; Seo, Y. Novel Dual-Curing Process for a Stereolithographically Printed Part Triggers a Remarkably Improved Interlayer Adhesion and Excellent Mechanical Properties. Langmuir 2020, 36, 9250–9258. [Google Scholar] [CrossRef]
- Lee, J.-M.; Son, K.; Lee, K.-B. Evaluation of Photopolymer Resins for Dental Prosthetics Fabricated via the Stereolithography Process at Different Polymerization Temperatures—Part I: Conversion Rate and Mechanical Properties. J. Prosthet. Dent. 2024, 131, 166.e1–166.e9. [Google Scholar] [CrossRef] [PubMed]
- Sahrir, C.D.; Lin, W.-S.; Wang, C.-S.; Lin, H.-E.; Wang, C.-W.; Lin, W.-C. Effects of 3D-Printers and Manufacturer-Specified Post-Curing Units on the Dimensional Accuracy, Compressive Strength, and Degree of Conversion of Resin for Fixed Dental Prostheses. J. Dent. Sci. 2025, 20, 1699–1708. [Google Scholar] [CrossRef]
- ASTM D638; Standard Test Method for Tensile Properties of Plastics. ASTM International: West Conshohocken, PA, USA, 2022.
- Paradowska-Stolarz, A.; Wezgowiec, J.; Malysa, A.; Wieckiewicz, M. Effects of Polishing and Artificial Aging on Mechanical Properties of Dental LT Clear® Resin. J. Funct. Biomater. 2023, 14, 295. [Google Scholar] [CrossRef]
- Bayarsaikhan, E.; Lim, J.-H.; Shin, S.-H.; Park, K.-H.; Park, Y.-B.; Lee, J.-H.; Kim, J.-E. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef]
- Niu, C.; Li, D.; Zhang, Y.; Wang, Y.; Ning, S.; Zhao, G.; Ye, Z.; Kong, Y.; Yang, D. Prospects for 3D-Printing of Clear Aligners—A Narrative Review. Front. Mater. 2024, 11, 1438660. [Google Scholar] [CrossRef]
- Katheng, A.; Kanazawa, M.; Iwaki, M.; Minakuchi, S. Evaluation of Dimensional Accuracy and Degree of Polymerization of Stereolithography Photopolymer Resin under Different Postpolymerization Conditions: An In Vitro Study. J. Prosthet. Dent. 2021, 125, 695–702. [Google Scholar] [CrossRef]
- Klein-Júnior, C.A.; Zander-Grande, C.; Amaral, R.; Stanislawczuk, R.; Garcia, E.J.; Baumhardt-Neto, R.; Meier, M.M.; Loguercio, A.D.; Reis, A. Evaporating Solvents with a Warm Air-Stream: Effects on Adhesive Layer Properties and Resin–Dentin Bond Strengths. J. Dent. 2008, 36, 618–625. [Google Scholar] [CrossRef]
- Schmalz, G.; Hickel, R.; van Landuyt, K.L.; Reichl, F.-X. Scientific Update on Nanoparticles in Dentistry. Int. Dent. J. 2018, 68, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Alifui-Segbaya, F.; Varma, S.; Lieschke, G.J.; George, R. Biocompatibility of Photopolymers in 3D Printing. 3D Print. Addit. Manuf. 2017, 4, 185–191. [Google Scholar] [CrossRef]
- Shirey, N.; Mendonca, G.; Groth, C.; Kim-Berman, H. Comparison of Mechanical Properties of 3-Dimensional Printed and Thermoformed Orthodontic Aligners. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 720–728. [Google Scholar] [CrossRef]
- Kusum, P.; Sharma, S.; Jha, S. Comparative Evaluation of Mechanical Properties of Clear Aligner Biosheet Materials—An In Vitro Study. J. Pharm. Bioallied Sci. 2025, 17, S1616. [Google Scholar] [CrossRef]
- Bagheri, A.; Jin, J. Photopolymerization in 3D Printing. ACS Appl. Polym. Mater. 2019, 1, 593–611. [Google Scholar] [CrossRef]
- Šimunović, L.; Brenko, L.; Marić, A.J.; Meštrović, S.; Haramina, T. Rheology of Dental Photopolymers for SLA/DLP/MSLA 3D Printing. Polymers 2025, 17, 2706. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-Y.; Kim, H.; Kim, H.-J.; Chung, C.-J.; Choi, Y.-J.; Kim, S.-J.; Cha, J.-Y. Thermo-Mechanical Properties of 3D-Printed Photocurable Shape Memory Resin for Clear Aligners. Sci. Rep. 2022, 12, 6246. [Google Scholar] [CrossRef]
- Choi, J.-Y.; Kim, H.; Kim, S.-H.; Kim, S.-J.; Cha, J.-Y.; Lee, S.-Y.; Lee, J.; Min, J.; Jang, S.; Khan, T.A.; et al. Mechanical and Viscoelastic Properties of a Temperature-Responsive Photocurable Resin for 3D-Printed Orthodontic Clear Aligners. Sci. Rep. 2025, 15, 23530. [Google Scholar] [CrossRef] [PubMed]
- Son, K.; Son, Y.-T.; Lee, J.-M.; Lee, K.-B. Marginal and Internal Fit and Intaglio Surface Trueness of Interim Crowns Fabricated from Tooth Preparation of Four Finish Line Locations. Sci. Rep. 2021, 11, 13947. [Google Scholar] [CrossRef]
- Son, K.; Lee, S.; Kang, S.H.; Park, J.; Lee, K.-B.; Jeon, M.; Yun, B.-J. A Comparison Study of Marginal and Internal Fit Assessment Methods for Fixed Dental Prostheses. J. Clin. Med. 2019, 8, 785. [Google Scholar] [CrossRef]
- Wang, C.; Shi, Y.-F.; Xie, P.-J.; Wu, J.-H. Accuracy of Digital Complete Dentures: A Systematic Review of In Vitro Studies. J. Prosthet. Dent. 2021, 125, 249–256. [Google Scholar] [CrossRef]
- Katheng, A.; Kanazawa, M.; Komagamine, Y.; Iwaki, M.; Namano, S.; Minakuchi, S. Effect of Post-Rinsing Time and Method on Accuracy of Denture Base Manufactured with Stereolithography. J. Adv. Prosthodont. 2022, 14, 45–55. [Google Scholar] [CrossRef]
- McCarty, M.C.; Chen, S.J.; English, J.D.; Kasper, F. Effect of Print Orientation and Duration of Ultraviolet Curing on the Dimensional Accuracy of a 3-Dimensionally Printed Orthodontic Clear Aligner Design. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Venezia, P.; Ronsivalle, V.; Rustico, L.; Barbato, E.; Leonardi, R.; Lo Giudice, A. Accuracy of Orthodontic Models Prototyped for Clear Aligners Therapy: A 3D Imaging Analysis Comparing Different Market Segments 3D Printing Protocols. J. Dent. 2022, 124, 104212. [Google Scholar] [CrossRef] [PubMed]
| Resin Type | Printing Temperature | Post- Processing Time (s) | Mean | SD | 95% Confidence Interval | Partial η2 | F | p | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Temporary crown | RT | Green | 65.0 A | 7.2 | 56.0 | 73.9 | 0.762 | 15.378 | <0.001 * |
| 60 | 69.8 A | 2.3 | 67.0 | 72.6 | |||||
| 120 | 71.8 A | 6.3 | 64.0 | 79.7 | |||||
| 180 | 71.5 A | 20.1 | 46.6 | 96.5 | |||||
| 240 | 92.5 B | 2.3 | 89.6 | 95.4 | |||||
| 600 | 95.3 B | 0.9 | 94.2 | 96.4 | |||||
| 50 °C | Green | 73.8 A | 10.0 | 61.3 | 86.2 | ||||
| 60 | 92.9 B | 2.3 | 90.0 | 95.7 | |||||
| 120 | 94.2 B | 0.4 | 93.7 | 94.6 | |||||
| 180 | 97.7 B | 0.9 | 96.5 | 98.9 | |||||
| 240 | 97.1 B | 0.6 | 96.4 | 97.9 | |||||
| Denture base | RT | Green | 68.2 A | 3.7 | 63.6 | 72.7 | 0.748 | 12.893 | <0.001 * |
| 60 | 71.6 AB | 1.6 | 69.7 | 73.6 | |||||
| 120 | 70.9 AB | 1.7 | 68.8 | 73.0 | |||||
| 180 | 70.8 AB | 1.3 | 69.2 | 72.4 | |||||
| 240 | 76.7 BC | 2.3 | 73.8 | 79.5 | |||||
| 600 | 76.5 BC | 5.6 | 69.6 | 83.4 | |||||
| 50 °C | Green | 79.2 C | 2.2 | 76.5 | 82.0 | ||||
| 60 | 82.7 C | 0.9 | 81.5 | 83.8 | |||||
| 120 | 82.2 C | 2.6 | 78.9 | 85.5 | |||||
| 180 | 82.1 C | 3.0 | 78.4 | 85.9 | |||||
| 240 | 80.5 C | 2.4 | 77.5 | 83.5 | |||||
| Direct clear aligner | RT | Green | 86.8 A | 0.8 | 85.9 | 87.8 | 0.992 | 526.463 | <0.001 * |
| 60 | 95.8 B | 0.1 | 95.6 | 95.9 | |||||
| 120 | 96.7 BCD | 0.7 | 95.9 | 97.5 | |||||
| 180 | 96.0 B | 0.2 | 95.8 | 96.3 | |||||
| 240 | 97.0 DE | 0.3 | 96.7 | 97.4 | |||||
| 600 | 100.0 G | 0.0 | 100.0 | 100.0 | |||||
| 50 °C | Green | 85.9 A | 0.4 | 85.3 | 86.4 | ||||
| 60 | 96.0 B | 0.1 | 95.8 | 96.2 | |||||
| 120 | 97.4 EF | 0.7 | 96.5 | 98.2 | |||||
| 180 | 96.4 BC | 0.4 | 95.9 | 96.9 | |||||
| 240 | 98.1 F | 0.2 | 97.8 | 98.4 | |||||
| Resin Type | Printing Temperature | Post- Processing Time (s) | Mean | SD | 95% Confidence Interval | Partial η2 | F | p | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Tensile strength (MPa) | RT | Green | 31.8 A | 1.4 | 30.4 | 33.3 | 0.910 | 47.812 | <0.001 * |
| 60 | 31.3 A | 1.8 | 29.4 | 33.2 | |||||
| 120 | 31.3 A | 0.9 | 30.4 | 32.3 | |||||
| 180 | 35.6 B | 0.9 | 34.6 | 36.6 | |||||
| 240 | 35.5 B | 0.7 | 34.8 | 36.2 | |||||
| 600 | 38.7 C | 1.6 | 37.0 | 40.4 | |||||
| 50 °C | Green | 35.9 B | 2.2 | 33.6 | 38.2 | ||||
| 60 | 40.5 C | 0.6 | 39.9 | 41.1 | |||||
| 120 | 38.9 C | 0.6 | 38.3 | 39.5 | |||||
| 180 | 39.6 C | 0.5 | 39.0 | 40.1 | |||||
| 240 | 39.0 C | 0.9 | 38.0 | 40.0 | |||||
| Elongation (%) | RT | Green | 13.7E | 3.0 | 9.9 | 17.5 | 0.800 | 17.585 | <0.001 * |
| 60 | 12.7 E | 1.8 | 10.4 | 14.9 | |||||
| 120 | 12.1 DE | 1.8 | 9.8 | 14.3 | |||||
| 180 | 10.5 CDE | 1.5 | 8.6 | 12.3 | |||||
| 240 | 4.9A | 1.7 | 2.8 | 7.0 | |||||
| 600 | 4.7 A | 0.9 | 3.6 | 5.8 | |||||
| 50 °C | Green | 8.9 BCD | 1.2 | 7.4 | 10.4 | ||||
| 60 | 7.9 ABC | 1.9 | 5.5 | 10.3 | |||||
| 120 | 8.6 BCD | 1.5 | 6.7 | 10.5 | |||||
| 180 | 8.5 BC | 0.7 | 7.7 | 9.4 | |||||
| 240 | 5.5 AB | 0.8 | 4.5 | 6.4 | |||||
| Elastic modulus (MPa) | RT | Green | 1444.9 A | 144.6 | 1265.4 | 1624.4 | 0.953 | 88.377 | <0.001 * |
| 60 | 1748.4 B | 25.3 | 1717.0 | 1779.9 | |||||
| 120 | 1811.6 B | 45.1 | 1755.6 | 1867.7 | |||||
| 180 | 2162.1 C | 48.5 | 2101.9 | 2222.4 | |||||
| 240 | 2221.3 CDE | 16.7 | 2200.6 | 2242.1 | |||||
| 600 | 2341.9 DEF | 103.1 | 2213.9 | 2469.9 | |||||
| 50 °C | Green | 2176.3 CD | 129.6 | 2015.3 | 2337.3 | ||||
| 60 | 2508.4 F | 55.9 | 2439.0 | 2577.8 | |||||
| 120 | 2363.2 EF | 98.9 | 2240.3 | 2486.0 | |||||
| 180 | 2489.0 F | 44.3 | 2434.0 | 2544.0 | |||||
| 240 | 2457.4 F | 77.9 | 2360.7 | 2554.0 | |||||
| Resin Type | Printing Temperature | Post- Processing Time (s) | Mean | SD | 95% Confidence Interval | Partial η2 | F | p | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Tensile strength (MPa) | RT | Green | 18.5 A | 0.9 | 17.4 | 19.7 | 0.963 | 50.083 | <0.001 * |
| 60 | 19.3 AB | 1.0 | 18.1 | 20.5 | |||||
| 120 | 19.2 AB | 1.2 | 17.8 | 20.7 | |||||
| 180 | 19.5 AB | 0.4 | 19.0 | 20.0 | |||||
| 240 | 21.6 BC | 1.1 | 20.2 | 23.0 | |||||
| 600 | 21.7 BC | 0.8 | 20.7 | 22.6 | |||||
| 50 °C | Green | 23.8 C | 1.3 | 22.3 | 25.4 | ||||
| 60 | 27.7 D | 0.3 | 27.3 | 28.1 | |||||
| 120 | 27.9 D | 0.5 | 27.3 | 28.6 | |||||
| 180 | 27.9 D | 0.5 | 27.3 | 28.5 | |||||
| 240 | 27.9 D | 0.4 | 27.4 | 28.4 | |||||
| Elongation (%) | RT | Green | 14.2 C | 3.2 | 10.3 | 18.2 | 0.382 | 6.055 | <0.001 * |
| 60 | 10.5 ABC | 3.1 | 6.7 | 14.3 | |||||
| 120 | 9.7 ABC | 2.1 | 7.1 | 12.3 | |||||
| 180 | 8.2 A | 2.7 | 4.9 | 11.5 | |||||
| 240 | 8.5 AB | 1.4 | 6.7 | 10.3 | |||||
| 600 | 6.6 A | 1.2 | 5.1 | 8.2 | |||||
| 50 °C | Green | 13.4 BC | 2.0 | 10.9 | 15.8 | ||||
| 60 | 10.3 ABC | 3.6 | 5.9 | 14.7 | |||||
| 120 | 10.3 ABC | 1.6 | 8.3 | 12.3 | |||||
| 180 | 6.7 A | 2.0 | 4.3 | 9.1 | |||||
| 240 | 6.3 A | 2.2 | 3.5 | 9.1 | |||||
| Elastic modulus (MPa) | RT | Green | 692.5 A | 41.0 | 641.6 | 743.4 | 0.949 | 81.98 | <0.001 * |
| 60 | 776.9 A | 56.3 | 707.1 | 846.8 | |||||
| 120 | 811.9 A | 96.6 | 691.9 | 931.8 | |||||
| 180 | 951.2 B | 28.5 | 915.8 | 986.6 | |||||
| 240 | 1022.4 BC | 73.8 | 930.8 | 1114.1 | |||||
| 600 | 1081.1 CD | 61.9 | 1004.3 | 1157.9 | |||||
| 50 °C | Green | 1187.9 D | 97.4 | 1067.0 | 1308.9 | ||||
| 60 | 1316.7 E | 55.7 | 1247.6 | 1385.9 | |||||
| 120 | 1322.5 E | 22.6 | 1294.5 | 1350.5 | |||||
| 180 | 1319.0 E | 29.6 | 1282.3 | 1355.7 | |||||
| 240 | 1321.5 E | 18.5 | 1298.5 | 1344.5 | |||||
| Resin Type | Printing Temperature | Post- Processing Time (s) | Mean | SD | 95% Confidence Interval | Partial η2 | F | p | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Tensile strength (MPa) | RT | Green | 13.6 AB | 0.6 | 12.9 | 14.4 | 0.972 | 154.509 | <0.001 * |
| 60 | 14.8 B | 0.8 | 13.9 | 15.8 | |||||
| 120 | 18.0 C | 0.2 | 17.8 | 18.3 | |||||
| 180 | 19.9 D | 0.6 | 19.1 | 20.7 | |||||
| 240 | 21.8 F | 0.4 | 21.3 | 22.4 | |||||
| 600 | 21.0 DEF | 1.0 | 19.8 | 22.2 | |||||
| 50 °C | Green | 13.4 A | 0.7 | 12.6 | 14.2 | ||||
| 60 | 14.8 B | 0.5 | 14.2 | 15.5 | |||||
| 120 | 20.9 DEF | 0.4 | 20.0 | 21.0 | |||||
| 180 | 21.2 EF | 0.3 | 20.8 | 21.5 | |||||
| 240 | 20.2 DE | 0.6 | 19.4 | 20.9 | |||||
| Elongation (%) | RT | Green | 86.9 E | 17.2 | 65.6 | 108.3 | 0.637 | 7.719 | <0.001 * |
| 60 | 84.4 CDE | 2.4 | 81.4 | 87.4 | |||||
| 120 | 76.8 ABCDE | 3.9 | 72.0 | 81.7 | |||||
| 180 | 74.0 ABCD | 4.8 | 68.0 | 79.9 | |||||
| 240 | 66.5 A | 1.5 | 64.6 | 68.3 | |||||
| 600 | 73.4 ABCD | 2.1 | 70.8 | 76.0 | |||||
| 50 °C | Green | 85.9 DE | 4.2 | 80.6 | 91.1 | ||||
| 60 | 80.1 BCDE | 3.2 | 76.1 | 84.0 | |||||
| 120 | 68.1 AB | 2.5 | 64.9 | 71.2 | |||||
| 180 | 67.1 A | 1.5 | 65.3 | 69.0 | |||||
| 240 | 72.7 ABC | 3.7 | 68.1 | 77.3 | |||||
| Elastic modulus (MPa) | RT | Green | 427.0 A | 50.5 | 364.2 | 489.7 | 0.972 | 151.697 | <0.001 * |
| 60 | 757.3 B | 65.4 | 676.1 | 838.5 | |||||
| 120 | 1094.9 C | 174.6 | 878.0 | 1311.7 | |||||
| 180 | 1301.1 D | 114.6 | 1158.8 | 1443.4 | |||||
| 240 | 1663.1 EF | 37.1 | 1617.0 | 1709.2 | |||||
| 600 | 1509.9 E | 103.8 | 1381.0 | 1638.8 | |||||
| 50 °C | Green | 554.0 A | 19.0 | 530.4 | 577.7 | ||||
| 60 | 1041.4 C | 41.9 | 989.4 | 1093.5 | |||||
| 120 | 1538.6 E | 77.1 | 1442.9 | 1634.3 | |||||
| 180 | 1728.5 F | 48.8 | 1667.9 | 1789.1 | |||||
| 240 | 1493.8 E | 34.2 | 1451.3 | 1536.3 | |||||
| Resin Type | Printing Temperature | Post- Processing Time (s) | Mean | SD | 95% Confidence Interval | Partial η2 | F | p | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Temporary crown | RT | Green | 65.9 A | 8.5 | 56.9 | 74.8 | 0.404 | 3.206 | 0.003 * |
| 60 | 50.8 B | 8.8 | 41.6 | 60.0 | |||||
| 120 | 65.4 A | 11.8 | 52.9 | 77.8 | |||||
| 180 | 64.5 AC | 9.4 | 54.6 | 74.4 | |||||
| 240 | 55.9 ABC | 6.5 | 49.0 | 62.7 | |||||
| 600 | 65.7 A | 9.5 | 55.8 | 75.6 | |||||
| 50 °C | Green | 52.1 B | 11.5 | 40.0 | 64.2 | ||||
| 60 | 53.0 B | 5.6 | 47.1 | 58.9 | |||||
| 120 | 51.7 B | 9.5 | 41.6 | 61.7 | |||||
| 180 | 51.3 B | 7.6 | 43.4 | 59.2 | |||||
| 240 | 54.0 BC | 7.8 | 45.9 | 62.2 | |||||
| Denture base | RT | Green | 241.3 D | 27.5 | 207.2 | 275.4 | 0.752 | 13.378 | <0.001 * |
| 60 | 218.9 CD | 22.9 | 190.5 | 247.4 | |||||
| 120 | 173.6 ABC | 19.7 | 149.2 | 198.0 | |||||
| 180 | 153.1 AB | 23.2 | 124.3 | 181.9 | |||||
| 240 | 162.7 AB | 19.8 | 138.1 | 187.3 | |||||
| 600 | 135.5 A | 22.2 | 107.9 | 163.1 | |||||
| 50 °C | Green | 151.7 AB | 27.7 | 117.3 | 186.2 | ||||
| 60 | 153.7 AB | 21.5 | 127.0 | 180.5 | |||||
| 120 | 167.4 AB | 24.8 | 136.6 | 198.2 | |||||
| 180 | 199.1 BCD | 20.7 | 173.5 | 224.8 | |||||
| 240 | 241.2 D | 20.3 | 216.0 | 266.4 | |||||
| Direct clear aligner | RT | Green | 179.6 ABCD | 27.4 | 145.5 | 213.7 | 0.860 | 26.942 | <0.001 * |
| 60 | 231.6 CDE | 25.2 | 200.4 | 262.9 | |||||
| 120 | 148.7 AB | 18.0 | 126.3 | 171.0 | |||||
| 180 | 203.8 BCD | 15.7 | 184.2 | 223.3 | |||||
| 240 | 228.3 CDE | 17.8 | 206.2 | 250.4 | |||||
| 600 | 179.2 ABC | 31.1 | 140.5 | 217.8 | |||||
| 50 °C | Green | 235.8 DE | 47.9 | 176.4 | 295.2 | ||||
| 60 | 278.6 EF | 21.6 | 251.8 | 305.5 | |||||
| 120 | 131.1 A | 17.2 | 109.7 | 152.4 | |||||
| 180 | 149.6 AB | 33.6 | 107.9 | 191.3 | |||||
| 240 | 334.2 F | 12.5 | 318.7 | 349.8 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-M.; Son, K.; Lee, K.-B. Optimizing Printing Temperature and Post-Curing Time for Enhanced Mechanical Property and Fabrication Reproducibility of 3D-Printed Dental Photopolymer Resins. Appl. Sci. 2025, 15, 11552. https://doi.org/10.3390/app152111552
Lee J-M, Son K, Lee K-B. Optimizing Printing Temperature and Post-Curing Time for Enhanced Mechanical Property and Fabrication Reproducibility of 3D-Printed Dental Photopolymer Resins. Applied Sciences. 2025; 15(21):11552. https://doi.org/10.3390/app152111552
Chicago/Turabian StyleLee, Ji-Min, Keunbada Son, and Kyu-Bok Lee. 2025. "Optimizing Printing Temperature and Post-Curing Time for Enhanced Mechanical Property and Fabrication Reproducibility of 3D-Printed Dental Photopolymer Resins" Applied Sciences 15, no. 21: 11552. https://doi.org/10.3390/app152111552
APA StyleLee, J.-M., Son, K., & Lee, K.-B. (2025). Optimizing Printing Temperature and Post-Curing Time for Enhanced Mechanical Property and Fabrication Reproducibility of 3D-Printed Dental Photopolymer Resins. Applied Sciences, 15(21), 11552. https://doi.org/10.3390/app152111552











