Effectiveness of Preformed Myofunctional Devices in the Treatment of Malocclusions: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
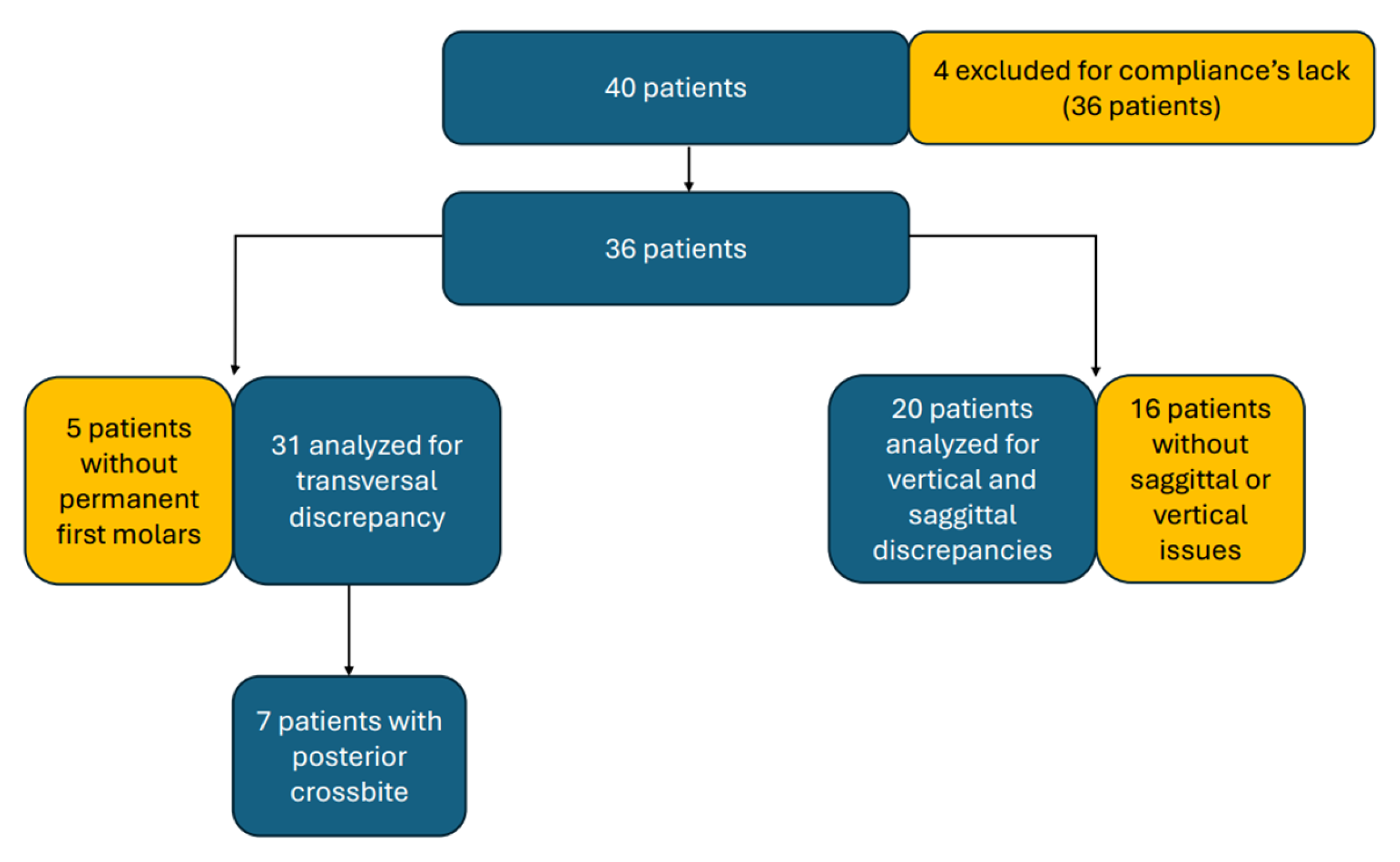
2.1. Study Participants
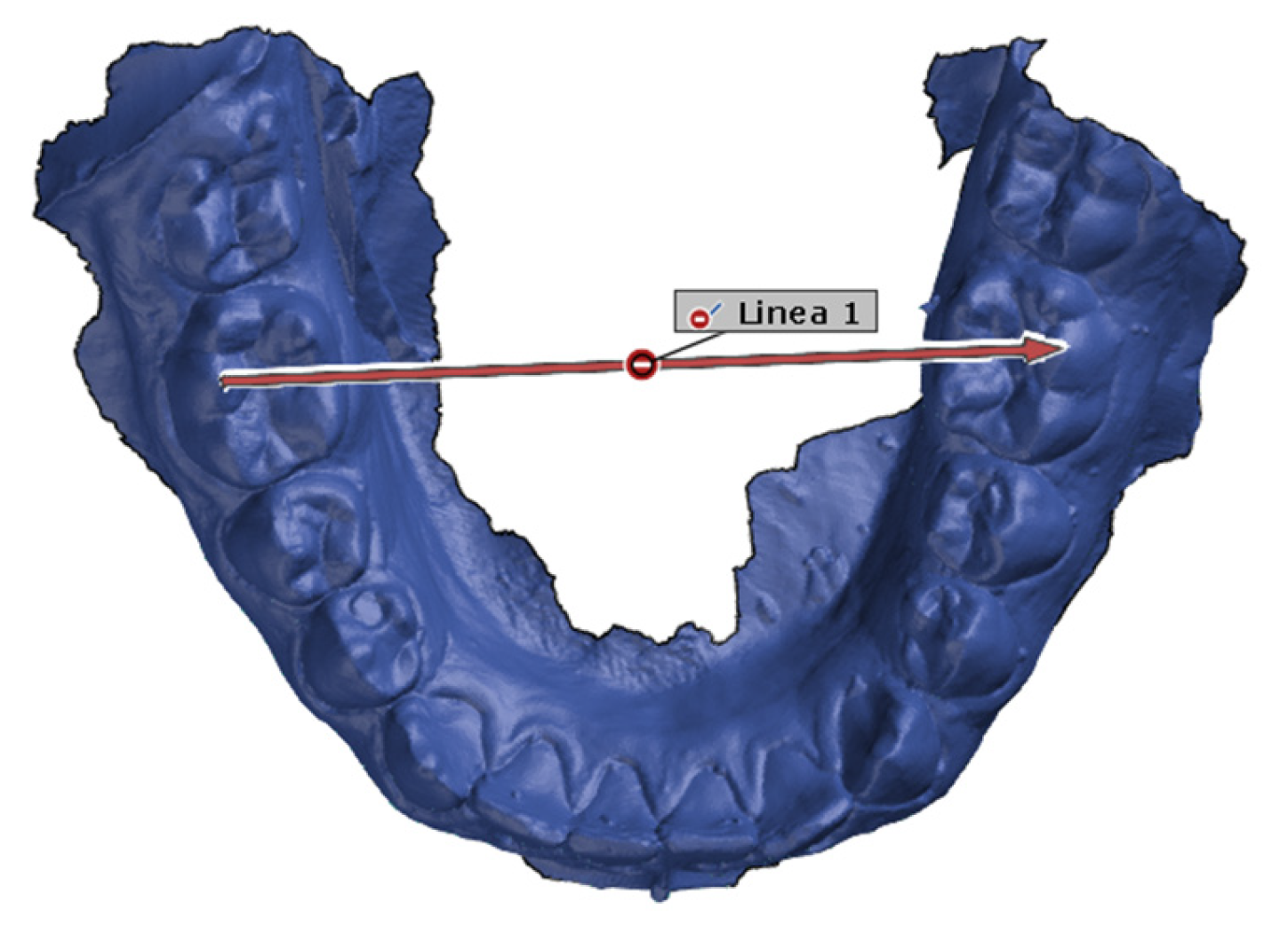
2.2. Study Design
- Presence of diagnosed malocclusion and oral dysfunction;
- Patient in mixed dentition;
- Patient without any previous orthodontic treatment.
- Absence of compliance;
- Patients under 5y;
- Patients with previous therapy.
2.3. Statistical Analysis
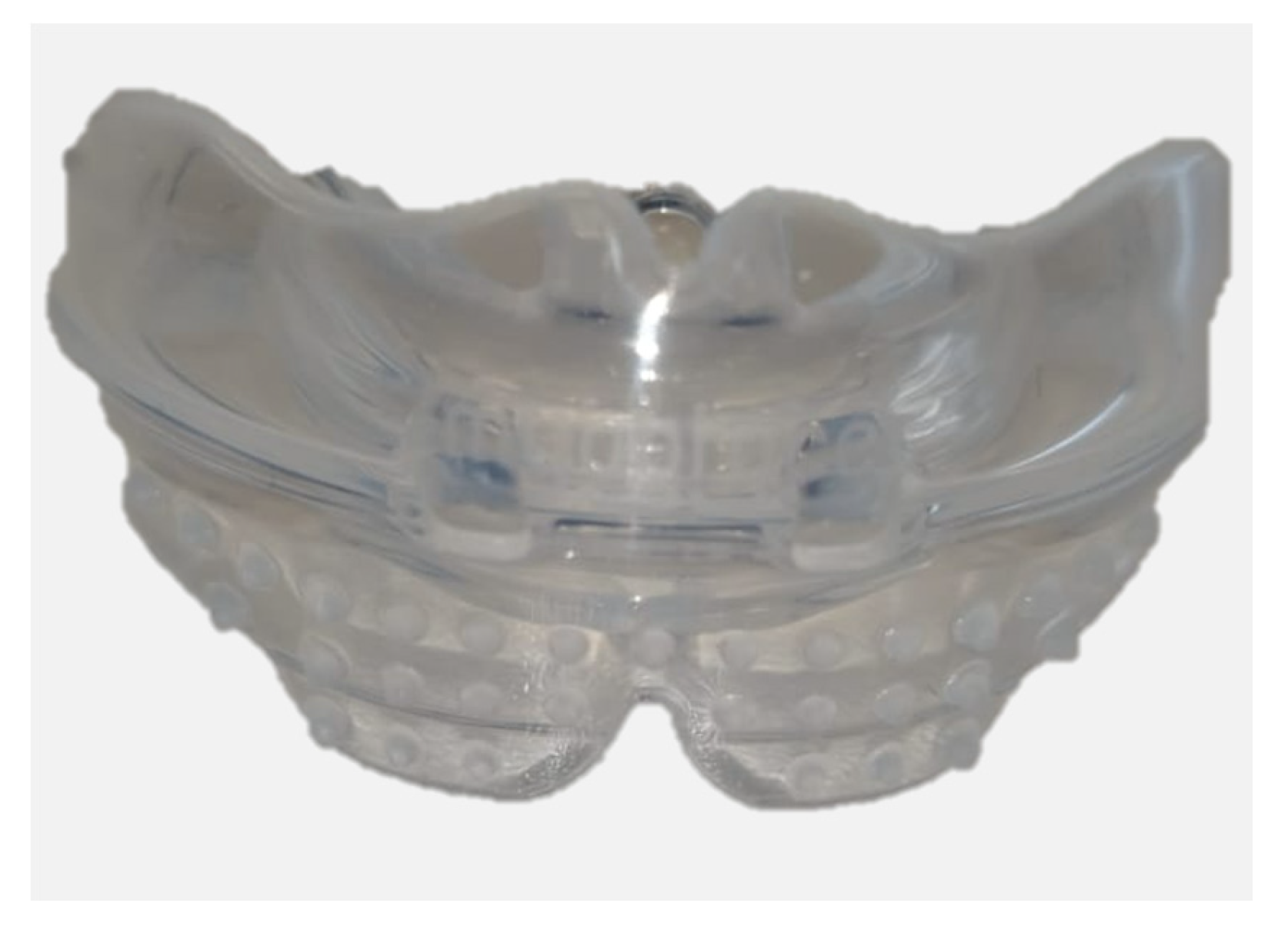
2.4. Device Description
- K (Kids) Series: For the mixed-dentition stage, around ages 6 to 10. It is particularly effective for treating dental crowding and correcting open or deep bites due to oral dysfunction habits.
- T Series (Teens): For the development of permanent teeth, generally between ages 11 and 15. This device helps encourage the correct development of dental arches and tooth alignment.
2.5. The Myobrace System
3. Results
4. Discussion
Limits of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Paglia, L. Interceptive orthodontics: Awareness and prevention is the first cure. Eur. J. Paediatr. Dent. 2023, 24, 5. [Google Scholar] [CrossRef]
- Lin, T.H.; Hughes, T.; Meade, M.J. The genetic and environmental contributions to variation in the permanent dental arch form: A twin study. Eur. J. Orthod. 2023, 45, 868–874. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grippaudo, C.; Paolantonio, E.G.; Antonini, G.; Saulle, R.; La Torre, G.; Deli, R. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngol. Ital. 2016, 36, 386–394. [Google Scholar] [CrossRef] [PubMed]
- Katib, H.S.; Aljashash, A.A.; Albishri, A.F.; Alfaifi, A.H.; Alduhyaman, S.F.; Alotaibi, M.M.; Otayf, T.S.; Bashikh, R.A.; Almadani, J.A.; Thabet, A.M.; et al. Influence of Oral Habits on Pediatric Malocclusion: Etiology and Preventive Approaches. Cureus 2024, 16, e72995. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sinha, S.P.; Bajracharya, M.; Huang, C.S.; Ko, E.W. Does cleft lip and palate affect the severity of malocclusion? Clin. Oral Investig. 2023, 27, 7557–7567. [Google Scholar] [CrossRef] [PubMed]
- Paolantonio, E.G.; Ludovici, N.; Saccomanno, S.; La Torre, G.; Grippaudo, C. Association between oral habits, mouth breathing and malocclusion in Italian preschoolers. Eur. J. Paediatr. Dent. 2019, 20, 204–208. [Google Scholar] [CrossRef]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dental Press J. Orthod. 2018, 23, 40.e1–40.e10, Erratum in Dental Press J. Orthod. 2019, 24, 113. [Google Scholar] [CrossRef]
- De Ridder, L.; Aleksieva, A.; Willems, G.; Declerck, D.; de Llano-Pérula, M.C. Prevalence of Orthodontic Malocclusions in Healthy Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 7446. [Google Scholar] [CrossRef]
- Moeller, J.L.; Paskay, L.C.; Gelb, M.L. Myofunctional therapy: A novel treatment of pediatric sleep-disordered breathing. Sleep Med. Clin. 2014, 9, 235–243. [Google Scholar] [CrossRef]
- Mills, C.S. International Association of Orofacial Myology History: Origin—Background—Contributors. Int. J. Orofac. Myol. 2011, 37, 5–25. [Google Scholar] [CrossRef] [PubMed]
- Alhasyimi, A.A.; Syahfik, I. Growth Modification of Developing Class II Division 1 Malocclusion Using Myofunctional Appliances. Case Rep. Dent. 2023, 2023, 8201195. [Google Scholar] [CrossRef] [PubMed]
- Rusli, R.O.; Achmad, H.; Kuandinata, W.; Fatimah, I.; Nurwahidah, A.; Halid, S.; La Mente, N.H. Myobrace versus twin block in the treatment of class II malocclusion in Children: A systematic review. Saudi Dent. J. 2024, 36, 661–664. [Google Scholar] [CrossRef] [PubMed]
- Tollaro, I.; Baccetti, T.; Franchi, L.; Tanasescu, C.D. Role of posterior transverse interarch discrepancy in Class II, Division 1 malocclusion during the mixed dentition phase. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Levrini, L.; Persano, R.; Piantanida, S.; Carganico, A.; Deppieri, A.; Naboni, G.; Mastrapasqua, R.F.; Saran, S. The Effects of the Myobrace® System on Peripheral Blood Oxygen Saturation (SpO2) in Patients with Mixed Dentition with Oral Dysfunction. Dent. J. 2023, 11, 191. [Google Scholar] [CrossRef]
- Fichera, G.; Martina, S.; Palazzo, G.; Musumeci, R.; Leonardi, R.; Isola, G.; Giudice, A.L. New Materials for Orthodontic Interceptive Treatment in Primary to Late Mixed Dentition. A Retrospective Study Using Elastodontic Devices. Materials 2021, 14, 1695. [Google Scholar] [CrossRef]
- Giudice, A.L.; Ronsivalle, V.; Santonocito, S.; Lucchese, A.; Venezia, P.; Marzo, G.; Leonardi, R.; Quinzi, V. Digital analysis of the occlusal changes and palatal morphology using elastodontic devices. A prospective clinical study including Class. II subjects in mixed dentition. Eur. J. Paediatr. Dent. 2022, 23, 275–280. [Google Scholar] [CrossRef]
- Giudice, A.L.; Ronsivalle, V.; Conforte, C.; Marzo, G.; Lucchese, A.; Leonardi, R.; Isola, G. Palatal changes after treatment of functional posterior cross-bite using elastodontic appliances: A 3D imaging study using deviation analysis and surface-to-surface matching technique. BMC Oral Health 2023, 23, 68. [Google Scholar] [CrossRef]
- Johnson, J.S.; Satyaprasad, S.; Chandra, H.S.; Havaldar, K.S.; Raj, A.; Suresh, N. A Comparative Evaluation of the Dentoskeletal Treatment Effects Using Twin Block Appliance and Myobrace System on Class II Division I Malocclusion. Int. J. Clin. Pediatr. Dent. 2021, 14 (Suppl. 1), S10. [Google Scholar] [CrossRef]
- Büyükbayraktar, Z.Ç.; Camcı, H. Dentoalveolar, skeletal, pharyngeal airway, cervical posture, hyoid bone position, and soft palate changes with Myobrace and Twin-block: A retrospective study. BMC Oral Health 2023, 23, 53. [Google Scholar] [CrossRef]
- Madian, A.M.; Elfouly, D. Cephalometric changes in pharyngeal airway dimensions after functional treatment with twin block versus myobrace appliances in developing skeletal class II patients: A randomized clinical trial. BMC Oral Health 2023, 23, 998. [Google Scholar] [CrossRef]
- Rodríguez-Olivos, L.H.G.; Chacón-Uscamaita, P.R.; Quinto-Argote, A.G.; Pumahualcca, G.; Pérez-Vargas, L.F. Deleterious oral habits related to vertical, transverse and sagittal dental malocclusion in pediatric patients. BMC Oral Health. 2022, 22, 88. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maspero, C.; Prevedello, C.; Giannini, L.; Galbiati, G.; Farronato, G. Atypical swallowing: A review. Minerva Stomatol. 2014, 63, 217–227. [Google Scholar] [PubMed]
- Paoloni, V.; Giuntini, V.; Lione, R.; Nieri, M.; Barone, V.; Merlo, M.M.; Mazza, F.; Passaleva, S.; Cozza, P.; Franchi, L. Comparison of the dento-skeletal effects produced by Leaf expander versus rapid maxillary expander in prepubertal patients: A two-center randomized controlled trial. Eur. J. Orthod. 2022, 44, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S.; Dawson, D.; Southard, K.A.; Lee, A.N.; Casko, J.S.; Southard, T.E. Transverse molar movements during growth. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 615–624. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, L. Oral dysfunction as a cause of malocclusion. Orthod. Craniofacial Res. 2019, 22 (Suppl. 1), 43–48. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pavlow, S.S.; McGorray, S.P.; Taylor, M.G.; Dolce, C.; King, G.J.; Wheeler, T.T. Effect of early treatment on stability of occlusion in patients with Class II malocclusion. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 235–244. [Google Scholar] [CrossRef]
- Al Nimri, K.; Richardson, A. Interceptive orthodontics in the real world of community dentistry. Int. J. Paediatr. Dent. 2000, 10, 99–108. [Google Scholar] [CrossRef]
- Hanoun, A.A.; Rao, G.K.; Khamis, M.F.; Mokhtar, N. Efficacy of the Prefabricated Myofunctional Appliance T4FTM in Comparison to Twin Block Appliance for Class II Division 1 Malocclusion Treatment: A Randomized Clinical Trial. Malays. J. Med. Health Sci. 2020, 16, 307–316. [Google Scholar]
- Idris, G.; Hajeer, M.Y.; Al-Jundi, A. Soft- and hard-tissue changes following treatment of Class II division 1 malocclusion with Activator versus Trainer: A randomized controlled trial. Eur. J. Orthod. 2019, 41, 21–28. [Google Scholar] [CrossRef]
- Elhamouly, Y.; El-Housseiny, A.A.; Ismail, H.A.; El Habashy, L.M. Myofunctional Trainer versus Twin Block in Developing Class II Division I Malocclusion: A randomized comparative clinical trial. Dent. J. 2020, 8, 44. [Google Scholar] [CrossRef]
- Xie, L.; Wang, P.; Wu, J. Soft and Hard Tissue Changes Following Treatment of Class II Division 1 Malocclusion with Twin-Block and Myofunctional Appliance: A Pilot Study. Chin. J. Plast. Reconstr. Surg. 2020, 2, 217–227. [Google Scholar] [CrossRef]

| OVJ T0 (mm) | OVJ T1 (mm) | OVB T0 (mm) | OVB T1 (mm) | |
|---|---|---|---|---|
| 1. | 3.3 | 1.4 | 2.5 | 1.1 |
| 2. | 4.1 | 1 | 1.3 | 2 |
| 3. | 4.4 | 2.8 | 2.3 | −0.7 |
| 4. | 2.8 | 1.1 | 2.9 | 1.6 |
| 5. | 5.2 | 2.1 | 3.4 | 2.4 |
| 6. | 3.6 | 1.6 | 1.1 | 2.2 |
| 7. | 3.4 | 2 | 3.5 | 2.1 |
| 8. | 2.3 | 1.7 | 3.2 | 3.3 |
| 9. | 2.8 | 2.6 | 3.7 | 2.5 |
| 10. | 9.6 | 1.6 | 3.6 | 0.9 |
| 11. | 3.1 | 1.9 | 1.2 | 1 |
| 12. | 4.5 | 1.5 | 2 | 0.9 |
| 13. | 2.7 | 1.5 | −1 | 0.3 |
| 14. | 2.8 | 1.5 | 3.1 | 2.4 |
| 15. | 2.5 | 2.2 | 2.3 | 3 |
| 16. | 3.7 | 1.7 | 2.7 | 1.5 |
| 17. | 3.4 | 2.6 | 6.4 | 4 |
| 18. | 3.4 | 0 | 1.9 | 0 |
| 19. | 2.1 | 1.9 | 3.7 | 2.5 |
| 20. | 2.2 | 2.8 | 0.7 | 1.7 |
| Maxillary Intermolar Width T0 (mm) | Maxillary Intermolar Width T1 (mm) | |
|---|---|---|
| 1. | 38.2 | 44.2 |
| 2. | 44.8 | 45.6 |
| 3. | 43.3 | 45.9 |
| 4. | 40.9 | 46.3 |
| 5. | 43.4 | 44.3 |
| 6. | 43.6 | 45.1 |
| 7. | 39.1 | 43.9 |
| 8. | 48.9 | 49.4 |
| 9. | 42.1 | 43.6 |
| 10. | 46.6 | 47.1 |
| 11. | 47.4 | 50.6 |
| 12. | 43.9 | 44.5 |
| 13. | 42.4 | 43.7 |
| 14. | 45.3 | 46.5 |
| 15. | 43.5 | 48.9 |
| 16. | 43.7 | 47 |
| 17. | 43.8 | 48.2 |
| 18. | 49.7 | 53.5 |
| 19. | 37.2 | 44 |
| 20. | 42 | 46.4 |
| 21. | 45.9 | 47.6 |
| 22. | 44.8 | 45.8 |
| 23. | 45.6 | 46 |
| 24. | 40.1 | 46.9 |
| 25. | 43.5 | 46.3 |
| 26. | 41.9 | 45.5 |
| 27. | 45.1 | 44.9 |
| 28. | 47.1 | 47.9 |
| 29. | 40.5 | 44.3 |
| 30. | 49 | 53.5 |
| 31. | 45.1 | 49.2 |
| PTID T0 (mm) | PTID T1 (mm) | |
|---|---|---|
| 1. | 4.72 | −0.6 |
| 2. | 5.8 | 1.7 |
| 3. | 7.9 | 2.7 |
| 4. | 7.5 | 3.7 |
| 5. | 4.6 | 0 |
| 6. | 6.5 | 3.9 |
| 7. | 3.9 | 0.4 |
| N | Minimum (mm) | Maximum (mm) | Average (mm) | SD (mm) | Sign. | |
|---|---|---|---|---|---|---|
| OVJ (T0) | 20 | 2.10 | 9.60 | 3.5950 | 1.63143 | p = 0.000 |
| OVJ (T1) | 20 | 0.00 | 2.80 | 1.7750 | 0.66797 | |
| OVB (T0) | 20 | −1.00 | 6.40 | 2.5250 | 1.51167 | p = 0.008 |
| OVB (T1) | 20 | −0.70 | 4.00 | 1.7350 | 1.14858 | |
| Maxillary Intermolar Width (T0) | 31 | 37.2000 | 49.7000 | 43.8193 | 3.0395 | p = 0.000 |
| Maxillary Intermolar Width (T1) | 31 | 43.6 | 53.5 | 46.665 | 2.5691 | |
| PTID T0 | 7 | 3.90 | 7.90 | 5.8457 | 1.52708 | p = 0.000 |
| PTID T1 | 7 | −0.60 | 3.90 | 1.6857 | 1.81239 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Levrini, L.; Giorgino, V.; Giannotta, N.; Carganico, A.; Deppieri, A.; Giorgino, S.; Saran, S. Effectiveness of Preformed Myofunctional Devices in the Treatment of Malocclusions: A Pilot Study. Appl. Sci. 2025, 15, 11153. https://doi.org/10.3390/app152011153
Levrini L, Giorgino V, Giannotta N, Carganico A, Deppieri A, Giorgino S, Saran S. Effectiveness of Preformed Myofunctional Devices in the Treatment of Malocclusions: A Pilot Study. Applied Sciences. 2025; 15(20):11153. https://doi.org/10.3390/app152011153
Chicago/Turabian StyleLevrini, Luca, Vincenzo Giorgino, Nicola Giannotta, Andrea Carganico, Alessandro Deppieri, Silvia Giorgino, and Stefano Saran. 2025. "Effectiveness of Preformed Myofunctional Devices in the Treatment of Malocclusions: A Pilot Study" Applied Sciences 15, no. 20: 11153. https://doi.org/10.3390/app152011153
APA StyleLevrini, L., Giorgino, V., Giannotta, N., Carganico, A., Deppieri, A., Giorgino, S., & Saran, S. (2025). Effectiveness of Preformed Myofunctional Devices in the Treatment of Malocclusions: A Pilot Study. Applied Sciences, 15(20), 11153. https://doi.org/10.3390/app152011153









