Effects of a Pneumatic External Abdominal Pressure Assist Belt on Trunk and Lower Limb Muscle Activity and Joint Kinematics During Lifting Tasks
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Conditions
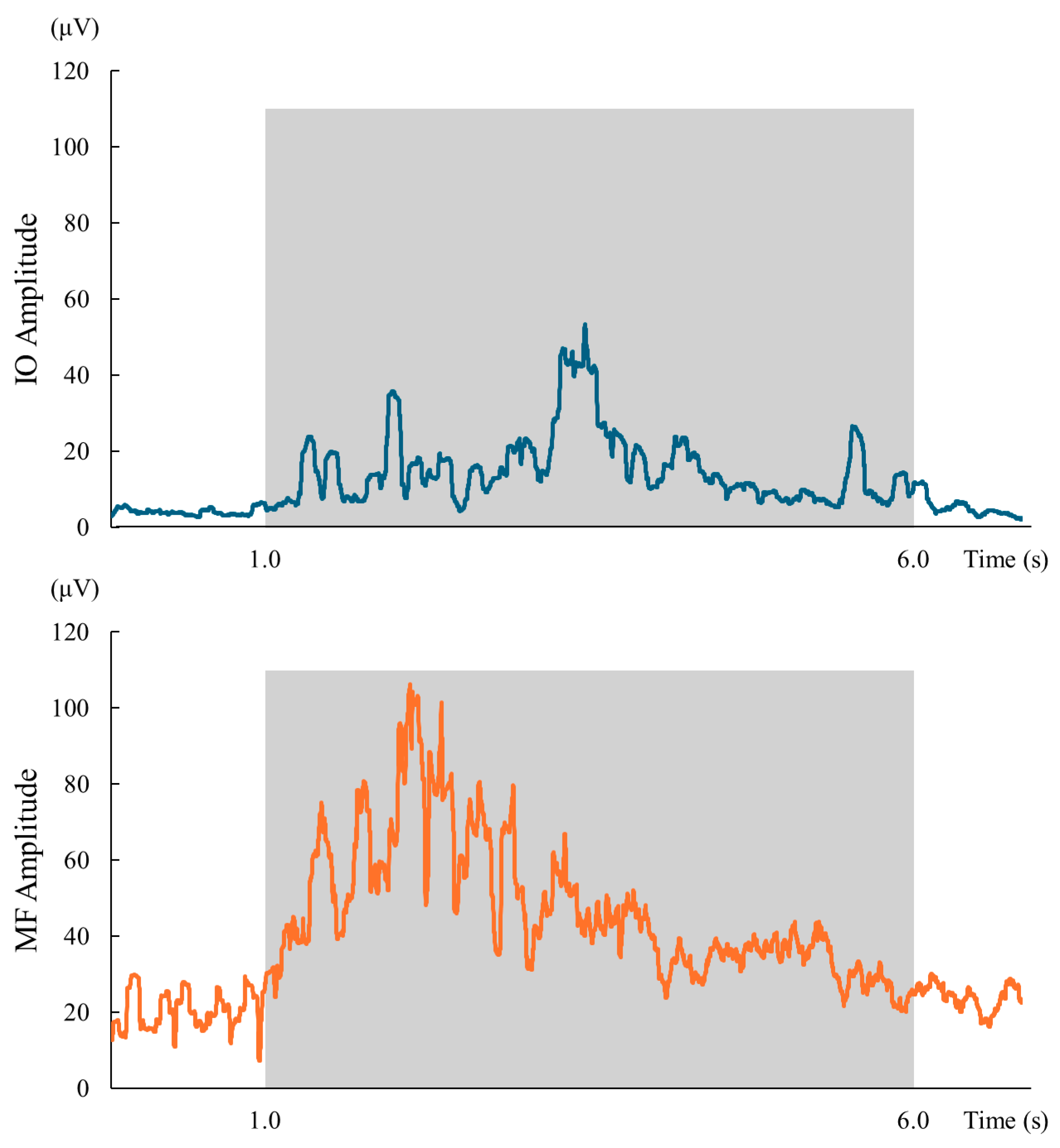
2.3. Muscle Activity
2.4. Joint Angle
2.5. Specifications of the Abdominal Pressure Assist Device
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Heneweer, H.; Staes, F.; Aufdemkampe, G.; van Rijn, M.; Vanhees, L. Physical activity and low back pain: A systematic review of recent literature. Eur. Spine J. 2011, 20, 826–845. [Google Scholar] [CrossRef] [PubMed]
- Marras, W.S.; Lavender, S.A.; Leurgans, S.E.; Rajulu, S.L.; Allread, W.G.; Fathallah, F.A.; Ferguson, S.A. The role of dynamic three-dimensional trunk motion in occupationally-related low back disorders. The effects of workplace factors, trunk position, and trunk motion characteristics on risk of injury. Spine 1993, 18, 617–628. [Google Scholar] [CrossRef] [PubMed]
- Cholewicki, J.; Juluru, K.; McGill, S.M. Intra-abdominal pressure mechanism for stabilizing the lumbar spine. J. Biomech. 1999, 32, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W.; Eriksson, A.E.; Shirley, D.; Gandevia, S.C. Intra-abdominal pressure increases stiffness of the lumbar spine. J. Biomech. 2005, 38, 1873–1880. [Google Scholar] [CrossRef]
- Bojairami, I.E.; Driscoll, M. Coordination Between Trunk Muscles, Thoracolumbar Fascia, and Intra-Abdominal Pressure Toward Static Spine Stability. Spine 2022, 47, E423–E431. [Google Scholar] [CrossRef]
- Stokes, I.A.; Gardner-Morse, M.G.; Henry, S.M. Abdominal muscle activation increases lumbar spinal stability: Analysis of contributions of different muscle groups. Clin. Biomech. 2011, 26, 797–803. [Google Scholar] [CrossRef]
- Hodges, P.W.; Richardson, C.A. Feedforward contraction of transversus abdominis is not influenced by the direction of arm movement. Exp. Brain Res. 1997, 114, 362–370. [Google Scholar] [CrossRef]
- Yamane, M.; Aoki, M.; Sasaki, Y.; Hayashi, T. Feedforward coactivation of trunk muscles during rapid shoulder movements. JSES Int. 2022, 6, 660–668. [Google Scholar] [CrossRef]
- Cholewicki, J.; Juluru, K.; Radebold, A.; Panjabi, M.M.; McGill, S.M. Lumbar spine stability can be augmented with an abdominal belt and/or increased intra-abdominal pressure. Eur. Spine J. 1999, 8, 388–395. [Google Scholar] [CrossRef]
- DeBeliso, M.; Sevene, T.; Adams, K.J.; Harris, C.; Climstein, M.; Berning, J.M. The Effects of a Back-Belt on Lumbar Disc Deformation During Stoop Type Lifting. Sci. Eng. Investig. 2013, 16, 21613-01. [Google Scholar]
- Bai, J.; Hua, A.; Weng, D.; Wang, N.; Wang, J. Effects of non-extensible lumbar belts on static and dynamic postural stability. BMC Musculoskelet. Disord. 2023, 24, 362. [Google Scholar] [CrossRef]
- Van Duijvenbode, I.C.; Jellema, P.; van Poppel, M.N.; van Tulder, M.W. Lumbar supports for prevention and treatment of low back pain. Cochrane Database Syst. Rev. 2008, 2008, CD001823. [Google Scholar] [CrossRef]
- Chen, Z.; Zhang, M.; Zhang, X.; Liu, C.; Wang, H. Understanding the User Experience of Lumbar-Support-Assistive Devices in Lower-Back Pain Patients: Design Recommendations. Appl. Sci. 2024, 14, 7495. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Walter, T.; Stutzig, N.; Siebert, T. Active exoskeleton reduces erector spinae muscle activity during lifting. Front. Bioeng. Biotechnol. 2023, 11, 1143926. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Murakami, H.; Demura, S.; Yoshioka, K.; Shinmura, K.; Yokogawa, N.; Igarashi, T.; Yonezawa, N.; Shimizu, T.; Tsuchiya, H. Abdominal trunk muscle weakness and its association with chronic low back pain and risk of falling in older women. BMC Musculoskelet. Disord. 2019, 20, 273. [Google Scholar] [CrossRef] [PubMed]
- Nakai, Y.; Usumoto, Y.; Takeshita, Y. The Effects of Regional Muscle Strength and Mass on Standing Long Jump Performance. Muscles 2024, 3, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Alemi, M.M.; Geissinger, J.; Simon, A.A.; Chang, S.E.; Asbeck, A.T. A passive exoskeleton reduces peak and mean EMG during symmetric and asymmetric lifting. J. Electromyogr. Kinesiol. 2019, 47, 25–34. [Google Scholar] [CrossRef]
- De Luca, C.J. The Use of Surface Electromyography in Biomechanics. J. Appl. Biomech. 1997, 13, 135–163. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Cram, J.R.; Kasman, G.S.; Holtz, J. Introduction to Surface Electromyography; Aspen Publishers: New York, NY, USA, 1998. [Google Scholar]
- Criswell, E.; Cram, J.R. Cram’s Introduction to Surface Electromyography, 2nd ed.; Jones and Bartlett: Boston, MA, USA, 2011; p. 21. 412p. [Google Scholar]
- Kendall, F.P. Muscles: Testing and Function with Posture and Pain, 5th ed.; Lippincott Williams & Wilkins: Ambler, PA, USA, 2005. [Google Scholar]
- Prisco, G.; Pirozzi, M.A.; Santone, A.; Esposito, F.; Cesarelli, M.; Amato, F.; Donisi, L. Validity of Wearable Inertial Sensors for Gait Analysis: A Systematic Review. Diagnostics 2024, 15, 36. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: New York, NY, USA, 1988. [Google Scholar]
- Tateuchi, H.; Taniguchi, M.; Mori, N.; Ichihashi, N. Balance of hip and trunk muscle activity is associated with increased anterior pelvic tilt during prone hip extension. J. Electromyogr. Kinesiol. 2012, 22, 391–397. [Google Scholar] [CrossRef]
- McGill, S.M.; Norman, R.W.; Sharratt, M.T. The effect of an abdominal belt on trunk muscle activity and intra-abdominal pressure during squat lifts. Ergonomics 1990, 33, 147–160. [Google Scholar] [CrossRef]
- Cholewicki, J.; Reeves, N.P.; Everding, V.Q.; Morrisette, D.C. Lumbosacral orthoses reduce trunk muscle activity in a postural control task. J. Biomech. 2007, 40, 1731–1736. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, D.A.; Moseley, G.L.; Hodges, P.W. The lumbar multifidus: Does the evidence support clinical beliefs? Man. Ther. 2006, 11, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Van den Tillaar, R.; Andersen, V.; Saeterbakken, A.H. Comparison of muscle activation and kinematics during free-weight back squats with different loads. PLoS ONE 2019, 14, e0217044. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, T.; Brechue, W.F.; Fujita, T.; Sato, Y.; Abe, T. Muscle activation during low-intensity muscle contractions with varying levels of external limb compression. J. Sports Sci. Med. 2008, 7, 467–474. [Google Scholar] [PubMed]
- Caneiro, J.P.; O’Sullivan, P.; Smith, A.; Ovrebekk, I.R.; Tozer, L.; Williams, M.; Teng, M.L.W.; Lipp, O.V. Physiotherapists implicitly evaluate bending and lifting with a round back as dangerous. Musculoskelet. Sci. Pract. 2019, 39, 107–114. [Google Scholar] [CrossRef]
- Nolan, D.; O’Sullivan, K.; Stephenson, J.; O’Sullivan, P.; Lucock, M. How do manual handling advisors and physiotherapists construct their back beliefs, and do safe lifting posture beliefs influence them? Musculoskelet. Sci. Pract. 2019, 39, 101–106. [Google Scholar] [CrossRef]
- McGill, S.M. The biomechanics of low back injury: Implications on current practice in industry and the clinic. J. Biomech. 1997, 30, 465–475. [Google Scholar] [CrossRef]
- McGill, S.M.; Hughson, R.L.; Parks, K. Changes in lumbar lordosis modify the role of the extensor muscles. Clin. Biomech. 2000, 15, 777–780. [Google Scholar] [CrossRef]
- Gagnon, D.; Plamondon, A.; Larivière, C. A comparison of lumbar spine and muscle loading between male and female workers during box transfers. J. Biomech. 2018, 81, 76–85. [Google Scholar] [CrossRef]
- Trafimow, J.H.; Schipplein, O.D.; Novak, G.J.; Andersson, G.B. The effects of quadriceps fatigue on the technique of lifting. Spine 1993, 18, 364–367. [Google Scholar] [CrossRef]
- Saraceni, N.; Campbell, A.; Kent, P.; Ng, L.; Straker, L.; O’Sullivan, P. Exploring lumbar and lower limb kinematics and kinetics for evidence that lifting technique is associated with LBP. PLoS ONE 2021, 16, e0254241. [Google Scholar] [CrossRef]
- Cholewicki, J.; Panjabi, M.M.; Khachatryan, A. Stabilizing function of trunk flexor-extensor muscles around a neutral spine posture. Spine 1997, 22, 2207–2212. [Google Scholar] [CrossRef]
- Van Dieën, J.H.; Reeves, N.P.; Kawchuk, G.; van Dillen, L.R.; Hodges, P.W. Analysis of Motor Control in Patients With Low Back Pain: A Key to Personalized Care? J. Orthop. Sports Phys. Ther. 2019, 49, 380–388. [Google Scholar] [CrossRef]


| Variable | Total (n = 24) | Male (n = 12) | Female (n = 12) |
|---|---|---|---|
| Age (years) | 20.8 ± 2.2 | 20.7 ± 0.6 | 21.0 ± 3.0 |
| Height (cm) | 166.1 ± 6.1 | 170.2 ± 4.2 | 162.1 ± 4.8 |
| Body weight (kg) | 57.2 ± 7.7 | 60.6 ± 7.8 | 53.7 ± 5.9 |
| Abdominal pressure (kPa) | 13.3 ± 4.5 | 15.1 ± 3.5 | 11.5 ± 4.6 |
| Handgrip strength (kg) | 33.5 ± 6.8 | 37.9 ± 5.9 | 29.1 ± 4.3 |
| Knee extensor strength (N) | 460.1 ± 101.8 | 496.2 ± 94.8 | 424.0 ± 95.6 |
| Lower leg length (cm) | 37.3 ± 2.3 | 37.5 ± 1.6 | 37.2 ± 2.8 |
| Knee extension torque (Nm) | 172.3 ± 40.3 | 186.2 ± 36.7 | 158.4 ± 38.9 |
| Muscle | A70 | A40 | A0 | NA | p | Effect Size | Post-Hoc Comparisons |
|---|---|---|---|---|---|---|---|
| EO | 17.1 ± 7.2 | 18.4 ± 10.2 | 19.2 ± 10.9 | 18.1 ± 8.9 | 0.208 | 0.007 (very small) | – |
| RA | 4.2 (2.6–4.9) | 4.2 (2.6–4.9) | 4.2 (2.6–4.9) | 4.2 (2.6–4.9) | 0.637 | 0.024 (very small) | – |
| IO | 22.7 (16.2–36.1) | 22.7 (16.2–36.1) | 22.7 (16.2–36.1) | 22.7 (16.2–36.1) | <0.001 | 0.344 (moderate) | A40 < A0 ***, A40 < NA *** |
| ES | 43.7 ± 15.9 | 43.0 ± 14.5 | 46.2 ± 16.6 | 49.7 ± 16.6 | <0.001 | 0.028 (small) | NA > A0 **, NA > A40 **, NA > A70 ***; A0 > A40 *, A0 > A70 * |
| MF | 44.5 ± 21.1 | 45.0 ± 20.7 | 42.4 ± 18.1 | 41.0 ± 18.8 | 0.005 | 0.007 (very small) | A40 > A0 *, A40 > NA ** |
| RF | 9.1 ± 5.3 | 8.4 ± 4.3 | 8.1 ± 4.5 | 6.8 ± 3.9 | 0.001 | 0.032 (small) | A0 > NA **, A40 > NA ***, A70 > NA *** |
| VL | 28.5 ± 12.4 | 29.6 ± 14.5 | 26.9 ± 13.0 | 24.8 ± 11.5 | 0.001 | 0.020 (small) | A40 > NA **, A70 > NA **, A40 > A0 * |
| BF | 27.5 ± 12.3 | 27.4 ± 12.8 | 27.7 ± 12.2 | 29.5 ± 13.1 | 0.041 | 0.005 (very small) | NA > A40 *, NA > A70 ** |
| Degree | |||||||
| Hip flexion | 113.1 ± 12.6 | 113.0 ± 12.3 | 111.8 ± 12.5 | 108.1 ± 12.5 | 0.002 | 0.027 (small) | A70 > NA *, A40 > NA *, A0 > NA * |
| Knee flexion | 85.2 ± 16.3 | 84.3 ± 15.4 | 82.8 ± 16.2 | 79.1 ± 15.6 | 0.002 | 0.022 (small) | A70 > NA **, A40 > NA **, A0 > NA * |
| Ankle dorsiflexion | 22.9 ± 8.9 | 23.0 ± 8.8 | 22.7 ± 8.7 | 21.3 ± 8.6 | 0.231 | 0.007 (very small) | – |
| Muscle | A70 | A40 | A0 | NA | p | Effect Size | Post-Hoc Comparisons |
|---|---|---|---|---|---|---|---|
| EO | 12.7 ± 5.5 | 12.8 ± 6.6 | 13.8 ± 8.0 | 13.2 ± 6.7 | 0.309 | 0.004 (very small) | – |
| RA | 3.4 (2.7–4.4) | 2.8 (1.9–4.0) | 2.7 (1.7–4.2) | 2.7 (1.8–3.6) | 0.001 | 0.322 (moderate) | A70 > NA **, A70 > A40 **, A70 > n *** |
| IO | 15.8 (12.5–22.6) | 16.3 (11.9–28.9) | 17.9 (12.8–32.1) | 20.2 (15.3–28.4) | 0.001 | 0.285 (moderate) | A40 < NA ***, A0 < NA**, A70 < NA * |
| ES | 42.8 ± 16.7 | 43.1 ± 15.2 | 44.5 ± 16.4 | 42.4 ± 16.3 | 0.241 | 0.003 (very small) | – |
| MF | 39.3 ± 19.1 | 39.9 ± 20.2 | 37.8 ± 18.5 | 35.1 ± 17.5 | 0.040 | 0.010 (very small) | (no pairwise survived correction) |
| RF | 4.9 (3.5–6.8) | 4.9 (4.0–6.3) | 4.8 (3.2–7.8) | 4.6 (3.2–5.7) | 0.011 | 0.160 (small) | A70 > NA *, A40 > NA * |
| VL | 18.6 ± 9.3 | 18.2 ± 8.5 | 19.2 ± 9.4 | 17.5 ± 8.3 | 0.254 | 0.005 (very small) | – |
| BF | 29.2 (19.6–43.2) | 31.4 (23.1–38.9) | 31.9 (19.0–40.7) | 32.9 (20.1–40.4) | 0.759 | 0.016 (very small) | – |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakai, Y.; Takeshita, Y. Effects of a Pneumatic External Abdominal Pressure Assist Belt on Trunk and Lower Limb Muscle Activity and Joint Kinematics During Lifting Tasks. Appl. Sci. 2025, 15, 10897. https://doi.org/10.3390/app152010897
Nakai Y, Takeshita Y. Effects of a Pneumatic External Abdominal Pressure Assist Belt on Trunk and Lower Limb Muscle Activity and Joint Kinematics During Lifting Tasks. Applied Sciences. 2025; 15(20):10897. https://doi.org/10.3390/app152010897
Chicago/Turabian StyleNakai, Yuki, and Yasufumi Takeshita. 2025. "Effects of a Pneumatic External Abdominal Pressure Assist Belt on Trunk and Lower Limb Muscle Activity and Joint Kinematics During Lifting Tasks" Applied Sciences 15, no. 20: 10897. https://doi.org/10.3390/app152010897
APA StyleNakai, Y., & Takeshita, Y. (2025). Effects of a Pneumatic External Abdominal Pressure Assist Belt on Trunk and Lower Limb Muscle Activity and Joint Kinematics During Lifting Tasks. Applied Sciences, 15(20), 10897. https://doi.org/10.3390/app152010897









