Effects of High-Intensity Interval Training on Functional Fitness in Older Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Considerations
2.2. Sample Description
2.3. Eligibility Criteria
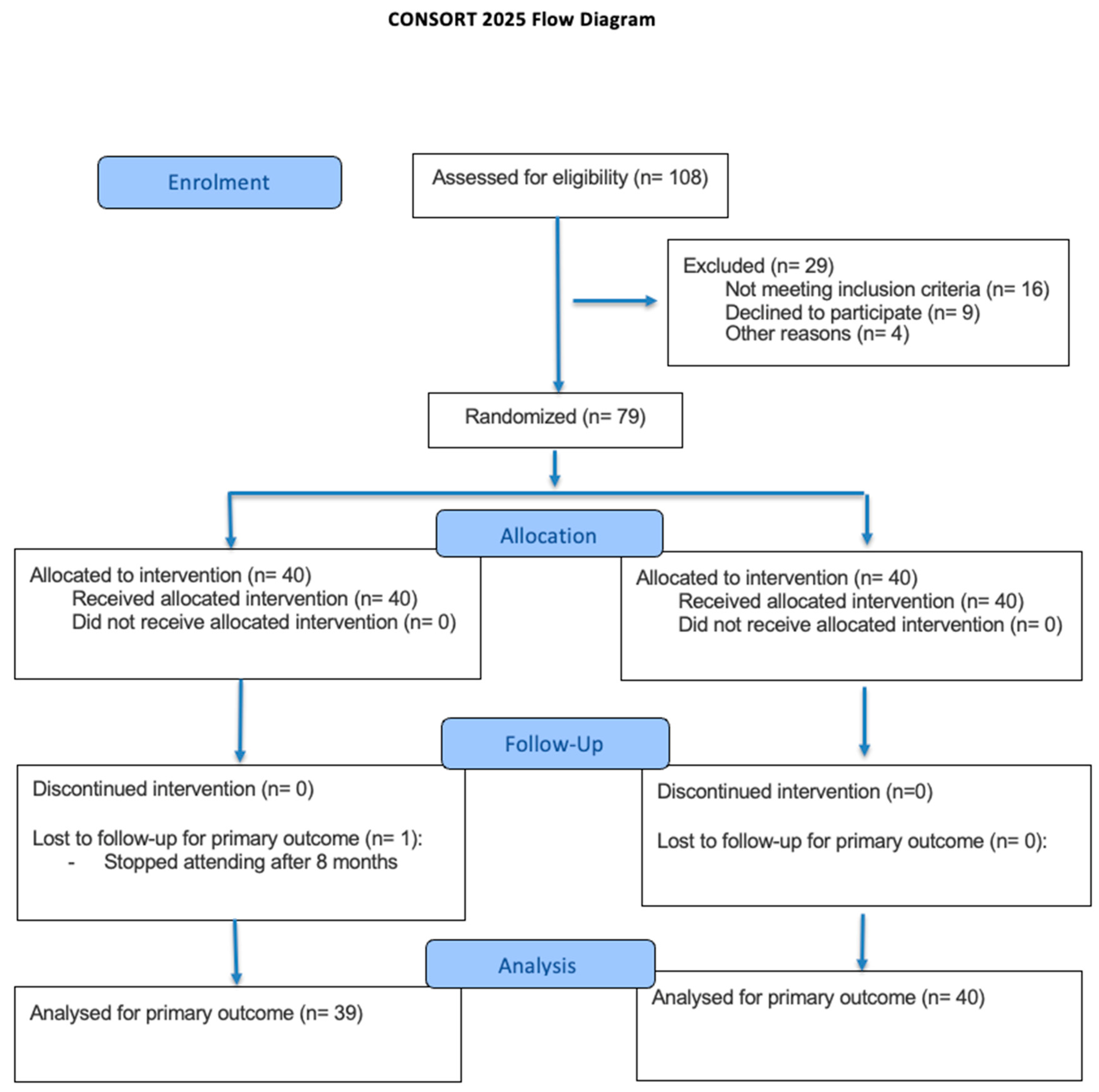
2.4. Recruitment and Randomization
2.5. Sample Size Calculation
2.6. Procedures
2.6.1. Anthropometry
2.6.2. Assessment of Functional Fitness
- Lower limb strength: Assessed using the 30 s Chair Stand Test, where participants were instructed to stand up and sit down from a standard chair as many times as possible within 30 s, with arms crossed over the chest. Only one trial was performed, and the number of correct repetitions was recorded.
- Upper limb strength: Evaluated using the Arm Curl Test, in which participants lifted a dumbbell (2.3 kg for females, 3.6 kg for males) with the dominant arm while seated. The number of complete repetitions performed in 30 s was recorded. One trial was conducted.
- Lower limb flexibility: Measured using the Chair Sit-and-Reach Test. Participants extended one leg forward and reached toward the toes, holding the final position. The best result from two attempts was recorded.
- Upper limb flexibility: Assessed using the Back Scratch Test, recording the distance between the middle fingers of both hands placed behind the back. The best of two trials was noted.
- Agility and dynamic balance: Evaluated with the Timed Up and Go (TUG) test. Participants stood up from a chair, walked three meters, turned around, returned, and sat down. The fastest time of two trials was recorded in seconds.
- Cardiorespiratory endurance: Assessed using the 2-Minute Step Test (2MST). Participants marched in place for two minutes, raising their knees to a height midway between the patella and iliac crest. Only the number of times the right knee reached the required height was counted. One trial was performed.
2.6.3. Handgrip Strength
2.6.4. High Intensity Interval Training Program
- Warm-up (10 min): Included joint mobility drills, dynamic stretching, and low-intensity aerobic movements to gradually increase heart rate and prepare the body for exercise.
- HIIT Core (30 min): Comprised repeated cycles of high-intensity functional movements (30–60 s)—such as stationary marching, high knees, jumping jacks, butt kicks, and modified burpees—interspersed with active recovery periods (60–90 s) using light movements or slow-paced marching. Each session included 6 to 10 work-recovery intervals, with progressive increases in volume and intensity throughout the program.
- Aerobic Functional Segment (10 min): Focused on reinforcing cardiovascular endurance through moderate-paced rhythmic movements and coordination tasks aimed at improving agility and motor control. Exercises included step taps, lateral steps, and multi-directional walking patterns.
- Cool-down (10 min): Consisted of static stretching for major muscle groups and guided breathing exercises to support recovery and return to baseline.
2.6.5. Timeline of Assessments
- M1 (PRE): Conducted prior to the initiation of the high-intensity interval training program.
- M2 (MID): Conducted at the midpoint of the 65-week intervention.
- M3 (POST): Conducted upon completion of the training program.
2.7. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Global Report on Ageism. Available online: https://www.who.int/publications/i/item/9789240016866 (accessed on 11 September 2025).
- Ismail, Z.; Ahmad, W.I.W.; Hamjah, S.H.; Astina, I.K. The Impact of Population Ageing: A Review. Iran. J. Public Health 2021, 50, 2451–2460. [Google Scholar] [CrossRef] [PubMed]
- Guillemot, J.; Zhang, X.; Warner, M. Population Aging and Decline Will Happen Sooner Than We Think. Soc. Sci. 2024, 13, 190. [Google Scholar] [CrossRef]
- Liougas, M.P.; Fortino, A.; Brozowski, K.; McMurray, J. Social Inclusion Programming for Older Adults Living in Age-Friendly Cities: A Scoping Review. 2025. Available online: https://bmjopen.bmj.com/content/15/1/e088439.info (accessed on 11 September 2025).
- Iuga, I.C.; Nerişanu, R.A.; Iuga, H. The impact of healthcare system quality and economic factors on the older adult population: A health economics perspective. Front. Public Health 2024, 12, 1454699. [Google Scholar] [CrossRef]
- Sun, X.; Li, X. (Eds.) Aging and chronic disease: Public health challenge and education reform. Front. Public Health 2023, 11, 1175898. [Google Scholar]
- Prince, M.J.; Wu, F.; Guo, Y.; Gutierrez Robledo, L.M.; O’Donnell, M.; Sullivan, R.; Yusuf, S. The burden of disease in older people and implications for health policy and practice. Lancet 2015, 385, 549–562. [Google Scholar] [CrossRef]
- Gianfredi, V.; Nucci, D.; Pennisi, F.; Maggi, S.; Veronese, N.; Soysal, P. Aging, longevity, and healthy aging: The public health approach. Aging Clin. Exp. Res. 2025, 37, 125. [Google Scholar] [CrossRef]
- Eckstrom, E.; Neukam, S.; Kalin, L.; Wright, J. Physical Activity and Healthy Aging. Clin. Geriatr. Med. 2020, 36, 671–683. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.; Durstine, J.L. Physical activity, exercise, and chronic diseases: A brief review. Sports Med. Health Sci. 2019, 1, 3–10. [Google Scholar] [CrossRef]
- Stern, G.; Psycharakis, S.G.; Phillips, S.M. Effect of High-Intensity Interval Training on Functional Movement in Older Adults: A Systematic Review and Meta-analysis. Sports Med.—Open 2023, 9, 5. [Google Scholar] [CrossRef]
- Oliveira, A.; Fidalgo, A.; Farinatti, P.; Monteiro, W. Effects of high-intensity interval and continuous moderate aerobic training on fitness and health markers of older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2024, 124, 105451. [Google Scholar] [CrossRef]
- Sert, H.; Gulbahar Eren, M.; Gurcay, B.; Koc, F. The effectiveness of a high-intensity interval exercise on cardiometabolic health and quality of life in older adults: A systematic review and meta-analysis. BMC Sports Sci. Med. Rehabil. 2025, 17, 128. [Google Scholar] [CrossRef]
- Atakan, M.M.; Li, Y.; Koşar, Ş.N.; Turnagöl, H.H.; Yan, X. Evidence-Based Effects of High-Intensity Interval Training on Exercise Capacity and Health: A Review with Historical Perspective. Int. J. Environ. Res. Public Health 2021, 18, 7201. [Google Scholar] [CrossRef]
- Mateo-Gallego, R.; Madinaveitia-Nisarre, L.; Giné-Gonzalez, J.; María Bea, A.; Guerra-Torrecilla, L.; Baila-Rueda, L.; Perez-Calahorra, S.; Civeira, F.; Lamiquiz-Moneo, I. The effects of high-intensity interval training on glucose metabolism, cardiorespiratory fitness and weight control in subjects with diabetes: Systematic review a meta-analysis. Diabetes Res. Clin. Pract. 2022, 190, 109979. [Google Scholar] [CrossRef] [PubMed]
- Niyazi, A.; Mir, E.; Ghasemi Kahrizsangi, N.; Mohammad Rahimi, N.; Fazolahzade Mousavi, R.; Setayesh, S.; Hoseinpour, A.N.; Rahimi, F.M.; Rahimi, G.R.M. The effect of functional exercise program on physical functioning in older adults aged 60 years or more: A systematic review and meta-analysis of randomized controlled trials. Geriatr. Nurs. 2024, 60, 548–559. [Google Scholar] [CrossRef]
- Distefano, G.; Goodpaster, B.H. Effects of Exercise and Aging on Skeletal Muscle. Cold Spring Harb. Perspect. Med. 2018, 8, a029785. [Google Scholar] [CrossRef]
- Liu, J.-D.; Quach, B.; Chung, P.-K. Further understanding of the Senior Fitness Test: Evidence from community-dwelling high function older adults in Hong Kong. Arch. Gerontol. Geriatr. 2019, 82, 286–292. [Google Scholar] [CrossRef]
- de Lima, T.R.; Silva, D.A.S.; Kovaleski, D.F.; González-Chica, D.A. Associação da força muscular com fatores sociodemográficos e estilo de vida em adultos e idosos jovens no Sul do Brasil. Ciênc. Saúde Coletiva 2018, 23, 3811–3820. [Google Scholar] [CrossRef] [PubMed]
- Dodds, R.M.; Syddall, H.E.; Cooper, R.; Benzeval, M.; Deary, I.J.; Dennison, E.M.; Der, G.; Gale, C.R.; Inskip, H.M.; Jagger, C. Grip Strength across the Life Course: Normative Data from Twelve British Studies. PLoS ONE 2014, 9, e113637. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, R.; Gough, A.; Loudon, K. The SPIRIT Checklist—Lessons from the experience of SPIRIT protocol editors. Trials 2022, 23, 359. [Google Scholar] [CrossRef]
- Boutron, I.; Altman, D.G.; Moher, D.; Schulz, K.F.; Ravaud, P.; CONSORT NPT Group. CONSORT Statement for Randomized Trials of Nonpharmacologic Treatments: A 2017 Update and a CONSORT Extension for Nonpharmacologic Trial Abstracts. Ann. Intern. Med. 2017, 167, 40–47. [Google Scholar] [CrossRef]
- Overview of R and RStudio|SpringerLink. Available online: https://link.springer.com/chapter/10.1007/978-3-030-80519-7_2 (accessed on 20 December 2024).
- R: The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 11 September 2025).
- Nuttall, F.Q. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr. Today 2015, 50, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Zierle-Ghosh, A.; Jan, A. Physiology, Body Mass Index; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK535456/ (accessed on 19 July 2025).
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut Off Points; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK541070/ (accessed on 19 July 2025).
- Langhammer, B.; Stanghelle, J.K. The Senior Fitness Test. J. Physiother. 2015, 61, 163. [Google Scholar] [CrossRef]
- Hesseberg, K.; Bentzen, H.; Bergland, A. Reliability of the senior fitness test in community-dwelling older people with cognitive impairment. Physiother. Res. Int. J. Res. Clin. Phys. Ther. 2015, 20, 37–44. [Google Scholar] [CrossRef]
- Cossio-Bolaños, M.; Vidal-Espinoza, R.; Villar-Cifuentes, I.; de Campos, L.F.C.C.; de Lázari, M.S.R.; Urra-Albornoz, C.; Sulla-Torres, J.; Gomez-Campos, R. Functional fitness benchmark values for older adults: A systematic review. Front. Public Health 2024, 12, 1335311. [Google Scholar] [CrossRef]
- Kemala Sari, N.; Stepvia, S.; Ilyas, M.F.; Setiati, S.; Harimurti, K.; Fitriana, I. Handgrip strength as a potential indicator of aging: Insights from its association with aging-related laboratory parameters. Front. Med. 2025, 12, 1491584. [Google Scholar] [CrossRef]
- Marriott, C.F.S.; Petrella, A.F.M.; Marriott, E.C.S.; Boa Sorte Silva, N.C.; Petrella, R.J. High-Intensity Interval Training in Older Adults: A Scoping Review. Sports Med.—Open 2021, 7, 49. [Google Scholar] [CrossRef]
- Grummt, M.; Hafermann, L.; Claussen, L.; Herrmann, C.; Wolfarth, B. Rating of Perceived Exertion: A Large Cross-Sectional Study Defining Intensity Levels for Individual Physical Activity Recommendations. Sports Med.—Open 2024, 10, 71. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhu, Y.; Wong, W.K. Statistical tests for homogeneity of variance for clinical trials and recommendations. Contemp. Clin. Trials Commun. 2023, 33, 101119. [Google Scholar] [CrossRef]
- Ghasemi, A.; Zahediasl, S. Normality Tests for Statistical Analysis: A Guide for Non-Statisticians. Int. J. Endocrinol. Metab. 2012, 10, 486–489. [Google Scholar] [CrossRef] [PubMed]
- Di Leo, G.; Sardanelli, F. Statistical significance: P value, 0.05 threshold, and applications to radiomics—Reasons for a conservative approach. Eur. Radiol. Exp. 2020, 4, 18. [Google Scholar] [CrossRef]
- Siegel, A.F. Chapter 16—Nonparametrics: Testing with Ordinal Data or Nonnormal Distributions. In Practical Business Statistics—6th Edition; Siegel, A.F., Ed.; Academic Press: Boston, MA, USA, 2012; pp. 491–506. Available online: https://www.sciencedirect.com/science/article/pii/B978012385208300016X (accessed on 19 July 2025).
- Brunner, E.; Domhof, S.; Langer, F. Nonparametric Analysis of Longitudinal Data in Factorial Experiments; Wiley: New York, NY, USA, 2002. [Google Scholar]
- Glynn, D.; Nikolaidis, G.; Jankovic, D.; Welton, N.J. Constructing Relative Effect Priors for Research Prioritization and Trial Design: A Meta-epidemiological Analysis. Med. Decis. Mak. 2023, 43, 553–563. [Google Scholar] [CrossRef]
- Hothorn, T.; Bretz, F.; Westfall, P.; Heiberger, R.M.; Schuetzenmeister, A.; Scheibe, S. multcomp: Simultaneous Inference in General Parametric Models. 2025. Available online: https://cran.r-project.org/web/packages/multcomp/index.html (accessed on 19 July 2025).
- Konietschke, F.; Noguchi, K.; Rubarth, K. nparcomp: Multiple Comparisons and Simultaneous Confidence Intervals. 2019. Available online: https://cran.r-project.org/web/packages/nparcomp/index.html (accessed on 19 July 2025).
- Lin, S.-C.; Lee, J.-Y.; Yang, Y.; Fang, C.-C.; Fang, H.-L.; Hou, T.-H. Exploring the Design of Upper Limb Strength Training Through High-Intensity Interval Training Combined with Exergaming: Usability Study. JMIR Serious Games 2024, 12, e51730. [Google Scholar] [CrossRef]
- Ballesta-García, I.; Martínez-González-Moro, I.; Rubio-Arias, J.; Carrasco-Poyatos, M. High-Intensity Interval Circuit Training Versus Moderate-Intensity Continuous Training on Functional Ability and Body Mass Index in Middle-Aged and Older Women: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 4205. [Google Scholar] [CrossRef] [PubMed]
- Villafaina, S.; Giménez-Guervós Pérez, M.J.; Fuentes-García, J.P. Comparative Effects of High-Intensity Interval Training vs. Moderate-Intensity Continuous Training in Phase III of a Tennis-Based Cardiac Rehabilitation Program: A Pilot Randomized Controlled Trial. Sustainability 2020, 12, 4134. [Google Scholar] [CrossRef]
- Duan, Y.; Wang, Y.; Liang, W.; Wong, H.-S.; Baker, J.S.; Yang, S. Feasibility and effects of high-intensity interval training in older adults with mild to moderate depressive symptoms: A pilot cluster-randomized controlled trial. J. Exerc. Sci. Fit. 2025, 23, 246–251. [Google Scholar] [CrossRef]
- Schneider, A.; Leite, L.B.; Teixeira, J.; Forte, P.; Barbosa, T.M.; Monteiro, A.M. Multicomponent Exercise and Functional Fitness: Strategies for Fall Prevention in Aging Women. Sports 2025, 13, 159. [Google Scholar] [CrossRef] [PubMed]
- Valentim-Silva, J.R.; Costa, M.L.; de Oliveira, G.L.; de Oliveira, T.A.P.; de Conceição, M.C.S.C.; Dantas, E.H.M. High Intensity Exercise and Flexibility of the Lower Limbs: Dose-Effect Study. Rev. Bras. Med. Esporte 2016, 22, 311–314. [Google Scholar] [CrossRef]
- Bottaro, M.; Machado, S.; Nogueira, W.; Scales, R.; Veloso, J. Effect of high versus low-velocity resistance training on muscular fitness and functional performance in older men. Eur. J. Appl. Physiol. 2007, 99, 257–264. [Google Scholar] [CrossRef]
- Khushnood, K.; Burki, Y.K.; Ejaz, A.; Sultan, N.; Mehmood, R. Effects of high intensity interval training on mobility and fitness outcomes in stroke. Rehabil. J. 2024, 8, 22–28. [Google Scholar] [CrossRef]

| Group (n) | Age (Mean ± SD) | Median | Min./Max. Age | BMI (Mean ± SD) | Median | Min./Max. BMI | p-Value |
|---|---|---|---|---|---|---|---|
| Control (40) | 69.2 ± 4.3 | 70 | 62/76 | 28.8 ± 4.9 kg/m2 | 27.9 | 22.4/36.7 | 0.61 |
| High Intensity Interval Training (39) | 68.7 ± 5.1 | 69 | 60/78 | 27.5 ± 5.3 kg/m2 | 26.8 | 21.1/35.9 | 0.44 |
| Group (n) | Variable | M1 Mean (±SD) [CI 95%] | M2 Mean (±SD) [CI 95%] | M3 Mean (±SD) [CI 95%] | RTE |
|---|---|---|---|---|---|
| High Intensity Interval Training (39) | Back Scratch (cm) | −2.44 (11.23) [−6.08, 1.2] | 0.56 (10.51) [−2.84, 3.97] | 2.67 (11.18) [−0.95, 6.3] | 0.53 |
| Control (40) | Back Scratch (cm) | −1.79 (14.25) [−6.34, 2.77] | −3.21 (14.29) [−7.78, 1.36] | −4.81 (14.31) [−9.39, −0.23] | 0.48 |
| High Intensity Interval Training (39) | Hand Grip (Kg) | 24.69 (7.45) [22.27, 27.1] | 24.27 (6.95) [22.02, 26.53] | 25.63 (6.97) [23.37, 27.89] | 0.54 |
| Control (40) | Hand Grip (Kg) | 22.79 (8.9) [19.94, 25.63] | 22.19 (8.94) [19.33, 25.05] | 21.58 (8.91) [18.73, 24.43] | 0.47 |
| High Intensity Interval Training (39) | Arm Curl (reps) | 21.92 (5.16) [20.25, 23.6] | 24.0 (4.48) [22.55, 25.45] | 27.05 (4.29) [25.66, 28.44] | 0.62 |
| Control (40) | Arm Curl (reps) | 19.95 (5.38) [18.23, 21.67] | 19.42 (5.14) [17.78, 21.07] | 18.7 (5.12) [17.06, 20.34] | 0.40 |
| High Intensity Interval Training (39) | 30s Chair Stand Reps | 6.48 (1.24) [6.02, 6.93] | 6.47 (1.42) [6.01, 6.94] | 6.4 (1.11) [6.03, 6.77] | 0.52 |
| Control (40) | 30s Chair Stand Reps | 9.81 (3.25) [8.77, 10.85] | 10.2 (3.26) [9.15, 11.24] | 10.46 (3.24) [9.43, 11.5] | 0.50 |
| High Intensity Interval Training (39) | 2 Minutes Step Test (reps) | 26.08 (4.77) [24.53, 27.62] | 26.18 (5.11) [24.52, 27.84] | 26.74 (5.5) [24.96, 28.53] | 0.57 |
| Control (40) | 2 Minutes Step Test (reps) | 26.8 (7.19) [24.5, 29.1] | 26.02 (7.51) [23.62, 28.43] | 25.48 (7.61) [23.04, 27.91] | 0.42 |
| High Intensity Interval Training (39) | Chair Sit and Reach (cm) | 196.38 (40.65) [183.21, 209.56] | 202.79 (44.19) [188.47, 217.12] | 209.46 (42.8) [195.59, 223.33] | 0.58 |
| Control (40) | Chair Sit and Reach (cm) | 182.38 (50.33) [166.28, 198.47] | 179.15 (48.25) [163.72, 194.58] | 176.78 (47.05) [161.73, 191.82] | 0.43 |
| High Intensity Interval Training (39) | TUG (s) | −7.13 (12.4) [−11.15, −3.11] | −6.25 (9.62) [−9.37, −3.13] | −4.05 (10.07) [−7.32, −0.79] | 0.39 |
| Control (40) | TUG (s) | −12.52 (12.93) [−16.65, −8.38] | −12.96 (12.83) [−17.06, −8.86] | −13.28 (12.79) [−17.37, −9.19] | 0.61 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schneider, A.; Leite, L.B.; Santos, F.; Teixeira, J.; Forte, P.; Barbosa, T.M.; Monteiro, A.M. Effects of High-Intensity Interval Training on Functional Fitness in Older Adults. Appl. Sci. 2025, 15, 10745. https://doi.org/10.3390/app151910745
Schneider A, Leite LB, Santos F, Teixeira J, Forte P, Barbosa TM, Monteiro AM. Effects of High-Intensity Interval Training on Functional Fitness in Older Adults. Applied Sciences. 2025; 15(19):10745. https://doi.org/10.3390/app151910745
Chicago/Turabian StyleSchneider, André, Luciano Bernardes Leite, Fernando Santos, José Teixeira, Pedro Forte, Tiago M. Barbosa, and António Miguel Monteiro. 2025. "Effects of High-Intensity Interval Training on Functional Fitness in Older Adults" Applied Sciences 15, no. 19: 10745. https://doi.org/10.3390/app151910745
APA StyleSchneider, A., Leite, L. B., Santos, F., Teixeira, J., Forte, P., Barbosa, T. M., & Monteiro, A. M. (2025). Effects of High-Intensity Interval Training on Functional Fitness in Older Adults. Applied Sciences, 15(19), 10745. https://doi.org/10.3390/app151910745










