Modulating Effects of Urbanization and Age on Greenspace–Mortality Associations: A London Study Using Nighttime Light Data and Spatial Regression
Abstract
1. Introduction
- How does spatial accessibility to greenspaces associate with cause-specific mortality across London?
- Is there any spatial heterogeneity in this association related to urbanization levels and other socio-economic levels?
2. Materials and Methods
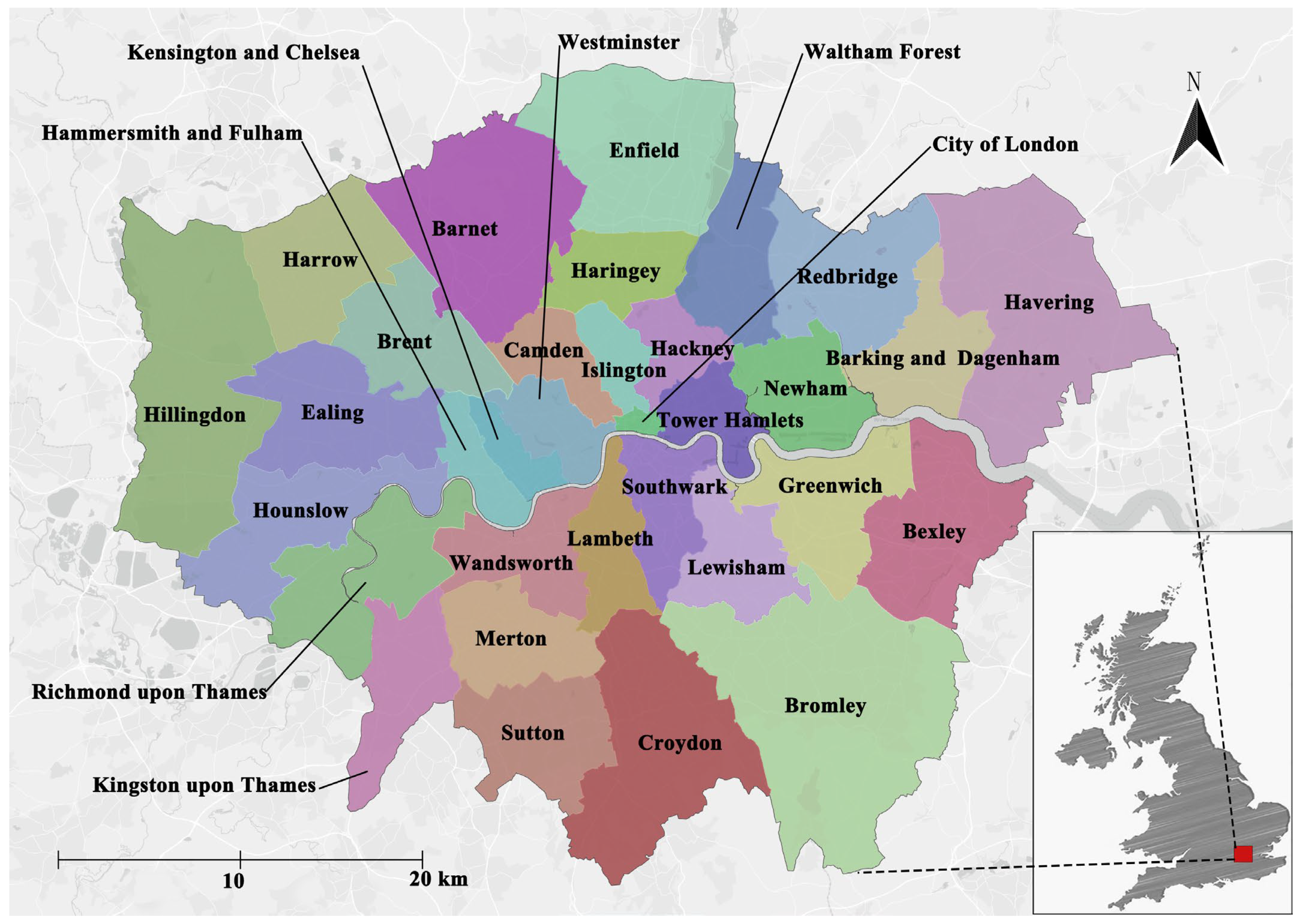
2.1. Study Area
2.2. Research Data
- (1)
- Chronic diseases mortality data
- (2)
- Greenspace data
- (3)
- Geo-spatial data
- (4)
- Socio-economic indicator
- (5)
- Nighttime light data
- (6)
- Air quality data
2.3. Methods
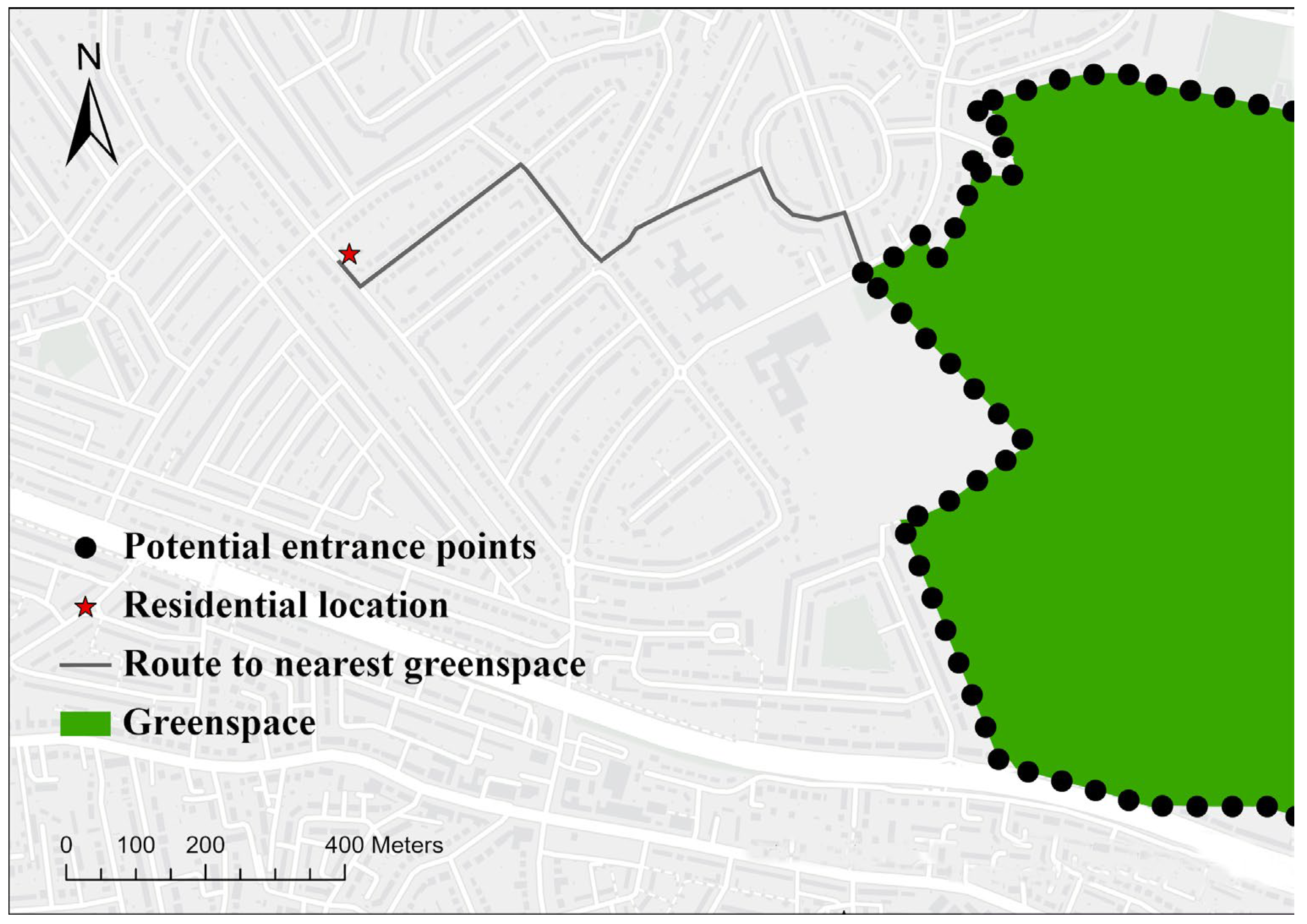
2.3.1. Greenspace Accessibility Measured by Shortest Road-Network Distance
| Algorithm 1 Dijkstra’s algorithm | |
| Step 1 (Initialization): In a directed graph G, divide all vertices into two sets: the set of vertices with determined shortest paths (S) and the set of vertices with undetermined shortest paths (V-S). Initially, S contains only the source vertex, and V-S contains all other vertices. | |
| Step 2 (loop): Find the vertex w closest to the source point in V-S and add it to S. | |
| Step 3 (update): For each vertex u in V-S, if there is an edge (w, u), update the shortest path length of u to: | |
| where: | |
| denotes the shortest path length from the source vertex to vertex u | |
| denotes the shortest path length from the source vertex to vertex w | |
| denotes the weight of the edge from vertex w to vertex u | |
| Step 4 (repetition): Repeat steps 2 and 3 until V-S is empty. |
2.3.2. Geographically Weighted Regression
3. Results
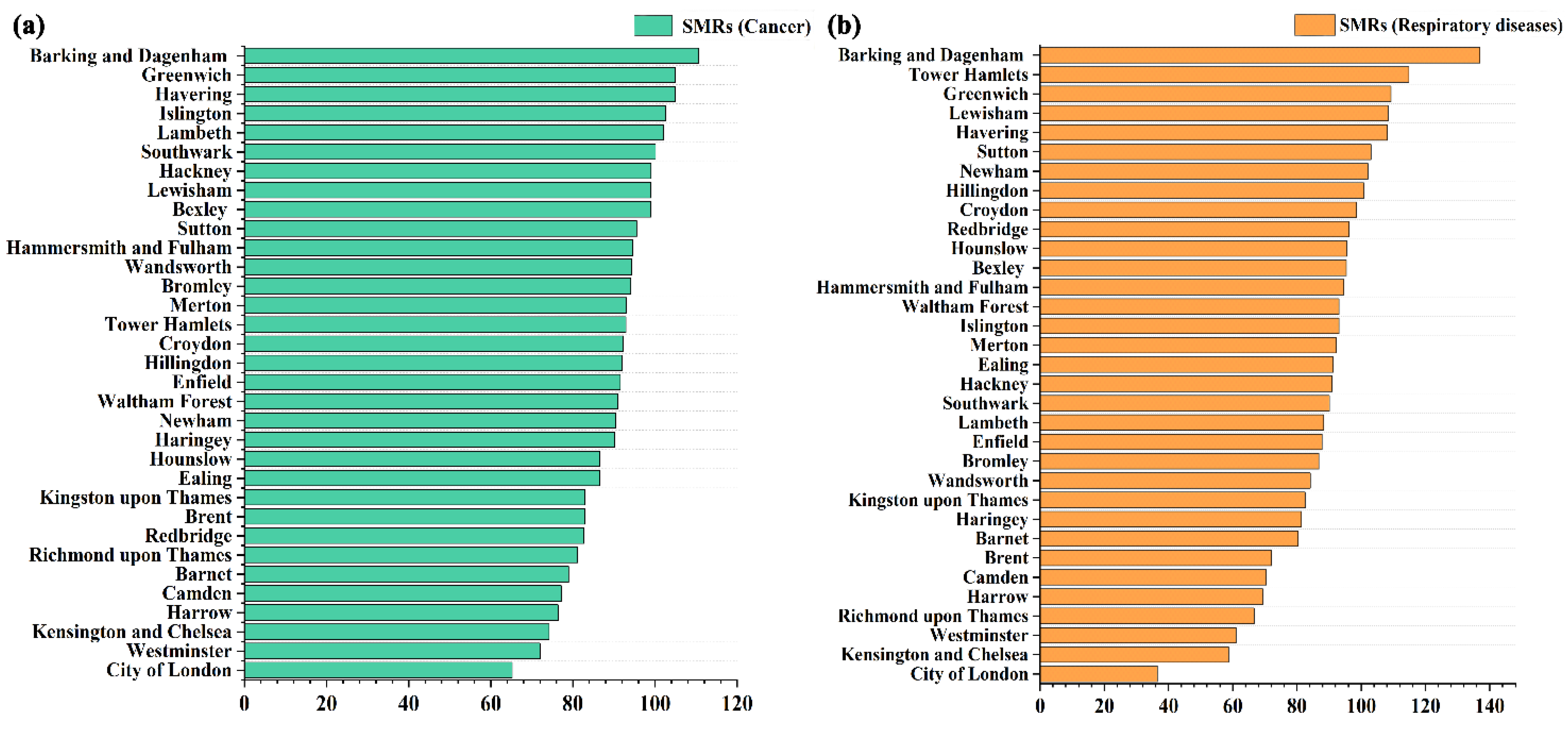
3.1. Descriptive Statistics for Chronic Diseases Mortality
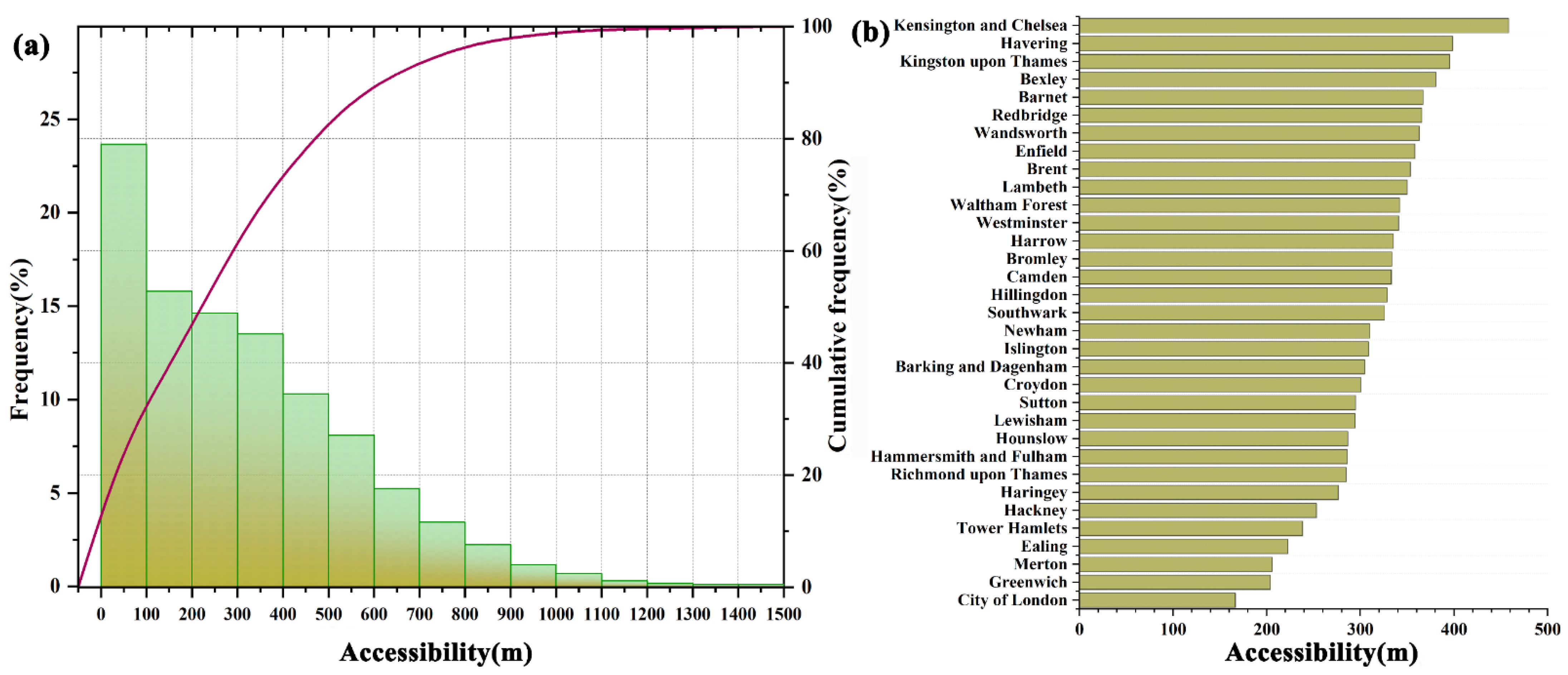
3.2. Greenspace Accessibility
3.3. Spatial Associations Between Greenspace Accessibility and Standardized Mortality Ratios
4. Discussion
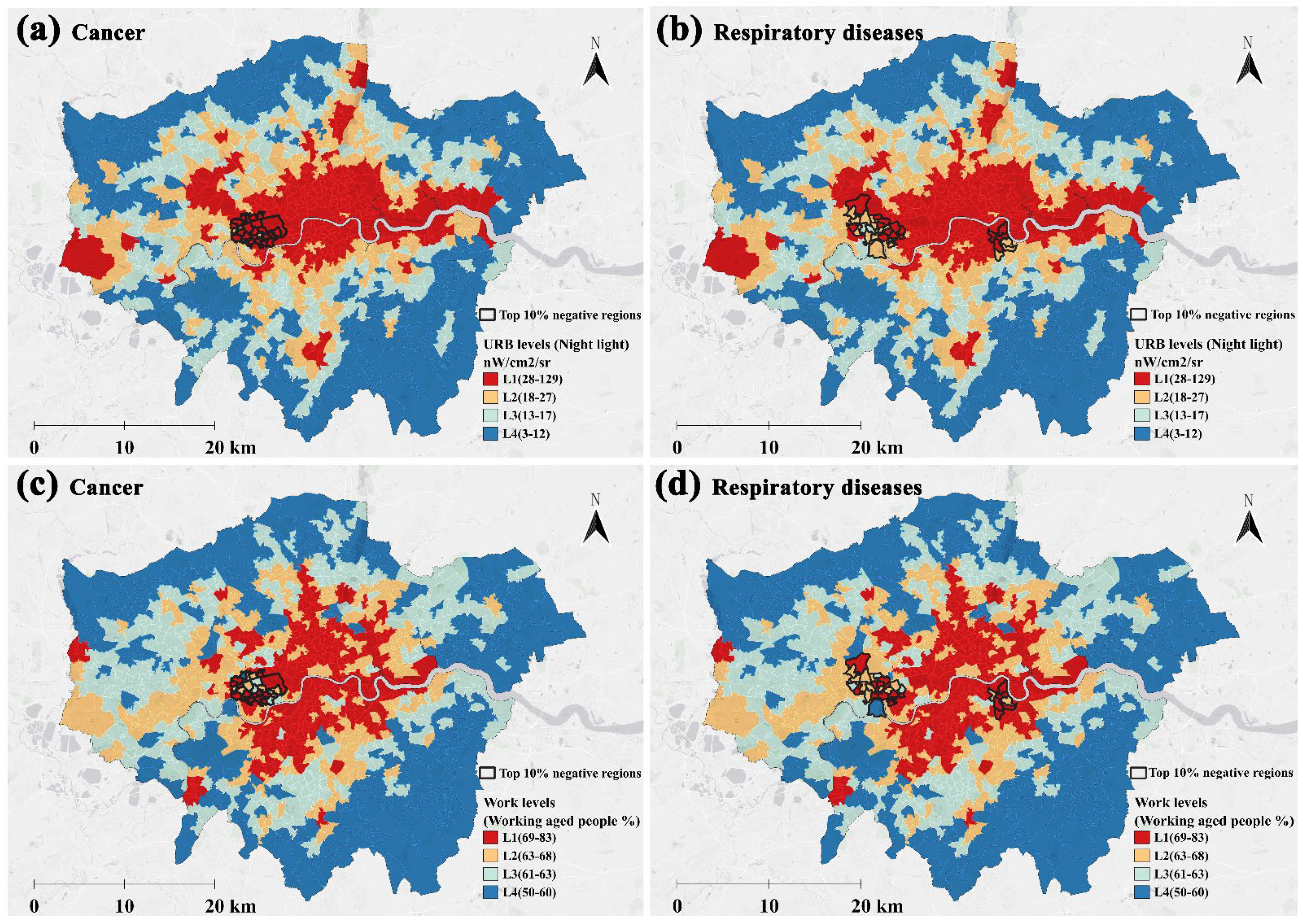
4.1. The Negative Impact of Greenspace Accessibility on Chronic Disease Mortality Is More Pronounced in Urban Central Areas
- Proximity advantages: High accessibility enables routine exposure, integrating nature contact into habitual activities [42].
- Microenvironmental mediation: Fine-grained urban greenery provides critical localized air quality improvements by filtering particulate matter and noxious gases [43]. This mechanism plausibly mitigates risks for pollution-sensitive conditions, including respiratory diseases and specific cancers—particularly lung cancer [82,83], but also emerging evidence links to prostate [84], skin, oral [85], breast [10], and rectal cancers [86].
- Variation in greenspace quality and function: A highly accessible greenspace in one area might be a well-maintained, multi-functional park encouraging physical activity and social cohesion, while in another area, it might be a less inviting, poorly maintained, or potentially unsafe space, explaining a neutral or even negative association [43,88].
- Unmeasured local environmental confounders: The spatial variation might capture the uneven distribution of environmental factors we could not measure at this scale, such as localized pollution sources beyond our air quality metrics [87], specific industrial histories, or stark differences in social cohesion [89] and crime rates within the greenspaces themselves [90]. For example, in areas where the environmental stressors overwhelm the restorative capacity of the available greenspace, the expected protective relationship may be diminished, nullified, or even reversed.
- Population characteristics: The GWR coefficient in a given area represents an average effect for that population. The mix of demographics, health behaviors, and cultural attitudes towards nature in one MSOA likely differs from that of its neighbor, modifying the average benefit derived from greenspace [25].
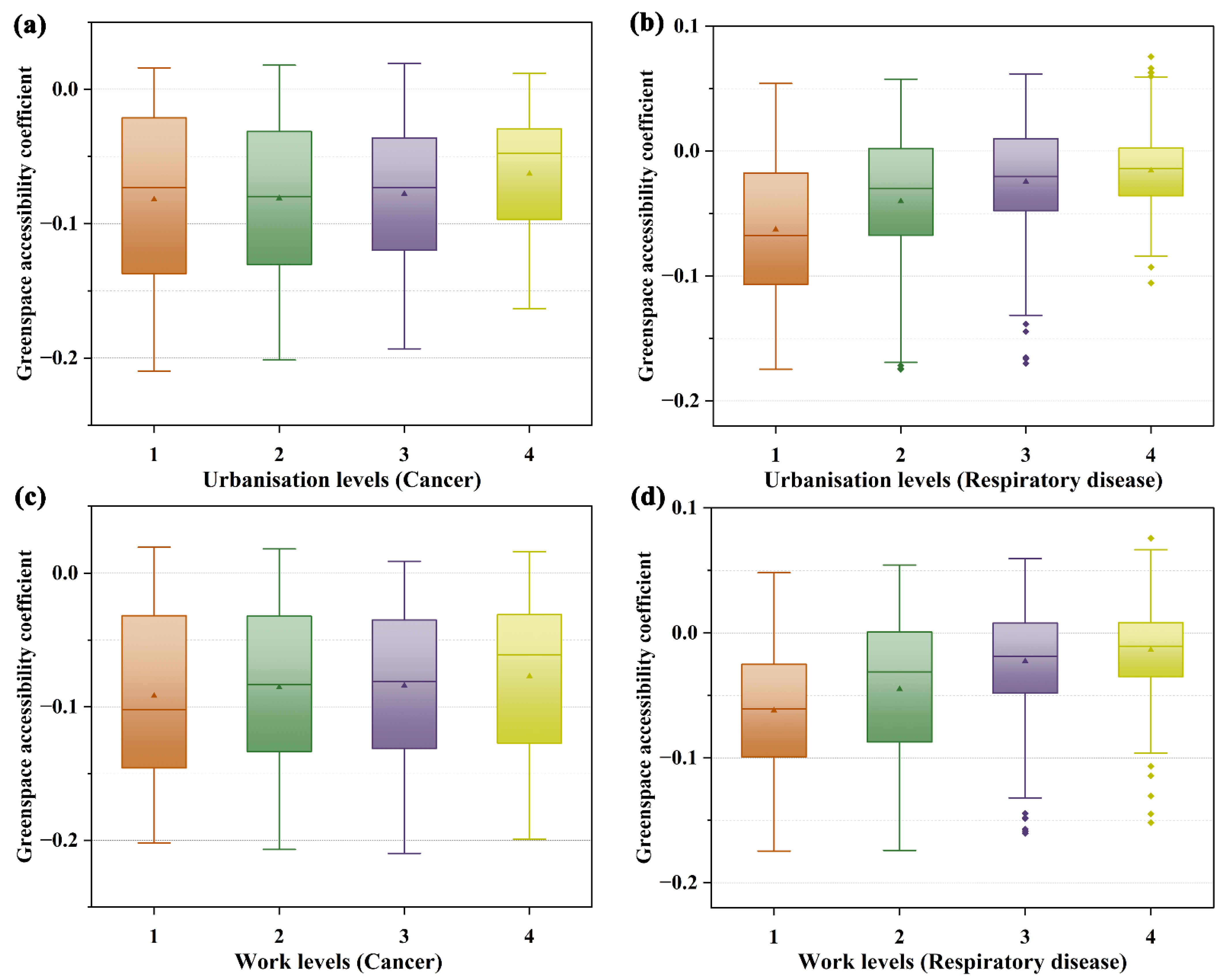
4.2. The Inhibitory Effect of Greenspace Accessibility on Chronic Disease Mortality Becomes Stronger as Urbanization Levels and the Proportion of the Working Population Increase
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhou, Q.; Liao, Y.; Wang, J. Mapping global urban greenspace: An analysis based on open land-cover data. Urban For. Urban Green. 2022, 74, 127638. [Google Scholar] [CrossRef]
- Seyler, B.C.; Luo, H.; Wang, X.; Zuoqiu, S.; Xie, Y.; Wang, Y. Assessing the impact of urban greenspace on physical health: An empirical study from Southwest China. Front. Public Health 2023, 11, 1148582. [Google Scholar] [CrossRef] [PubMed]
- Asri, A.K.; Lee, H.-Y.; Wu, C.-D.; Spengler, J.D. How does the presence of greenspace related to physical health issues in Indonesia? Urban For. Urban Green. 2022, 74, 127667. [Google Scholar] [CrossRef]
- World Health Organization. Urban Green Spaces and Health: A Review of Evidence; World Health Organization: Copenhagen, Denmark, 2016. [Google Scholar]
- Public Health England. Improving Access to Greenspace: A New Review for 2020; Care, D.H.S., Ed.; Public Health England: London, UK, 2020. [Google Scholar]
- Zhang, J.; Lim, Y.-H.; Chen, J.; Hyman, S.; Cole-Hunter, T.; Tuffier, S.; Napolitano, G.; Bergmann, M.; Mortensen, L.H.; Brandt, J.; et al. Residential greenspace and COVID-19 morbidity and mortality: A nationwide cohort study in Denmark. Environ. Int. 2024, 194, 109173. [Google Scholar] [CrossRef]
- Dong, R.; Yuan, H.; Xu, G.; Li, Y.; Xu, Y.; Fu, C. Impact of Different Greenspace Metrics on Cardiovascular Disease Incidence in Urban Settings: A Comparative Analysis. J. Urban Health 2025, 102, 274–289. [Google Scholar] [CrossRef]
- Godina, S.L.; Rosso, A.L.; Hirsch, J.A.; Besser, L.M.; Lovasi, G.S.; Donovan, G.H.; Garg, P.K.; Platt, J.M.; Fitzpatrick, A.L.; Lopez, O.L.; et al. Neighborhood greenspace and cognition: The cardiovascular health study. Health Place 2023, 79, 102960. [Google Scholar] [CrossRef]
- Mueller, W.; Milner, J.; Loh, M.; Vardoulakis, S.; Wilkinson, P. Exposure to urban greenspace and pathways to respiratory health: An exploratory systematic review. Sci. Total Environ. 2022, 829, 154447. [Google Scholar] [CrossRef]
- Odebeatu, C.C.; Darssan, D.; Roscoe, C.; Ahmed, M.; Reid, S.; Osborne, N.J. Greenspace and risk of obesity-related cancer in the UK Biobank cohort: An analysis of private residential gardens and other greenspace types. Sci. Total Environ. 2024, 943, 173833. [Google Scholar] [CrossRef]
- Mayne, S.L.; Kelleher, S.; Hannan, C.; Kelly, M.K.; Powell, M.; Dalembert, G.; McPeak, K.; Jenssen, B.P.; Fiks, A.G. Neighborhood Greenspace and Changes in Pediatric Obesity During COVID-19. Am. J. Prev. Med. 2023, 64, 33–41. [Google Scholar] [CrossRef]
- Cui, W.; Xu, J.; Tang, F.; Gao, M.M.; Zheng, Y.; Zhou, D.; Yang, S.; Han, Z.R. Perceived Greenspace Exposure and Children’s Emotional Well-Being in Daily Life: Comparisons between Children Living in Urban and Rural Areas. J. Happiness Stud. 2025, 26, 65. [Google Scholar] [CrossRef]
- He, Q.; Liu, L.; Zhang, H.; Chen, R.; Dong, G.; Yan, L.; Zeng, Y.; Kim, Y.; Ji, J.S. Environmental greenspace, subjective well-being, and all-cause mortality in elderly Chinese: Association and mediation study in a prospective cohort. Environ. Res. 2023, 227, 115732. [Google Scholar] [CrossRef] [PubMed]
- Houlden, V.; Albuquerque, J.P.d.; Weich, S.; Jarvis, S. Does nature make us happier? A spatial error model of greenspace types and mental wellbeing. Environ. Plan. B Urban Anal. City Sci. 2021, 48, 655–670. [Google Scholar] [CrossRef]
- Elbakidze, M.; Teitelbaum, S.; Dawson, L. Urban greenspace to support social integration of immigrants? Case studies across Sweden. Urban For. Urban Green. 2025, 111, 128868. [Google Scholar] [CrossRef]
- Clarke, M.; Cadaval, S.; Wallace, C.; Anderson, E.; Egerer, M.; Dinkins, L.; Platero, R. Factors that enhance or hinder social cohesion in urban greenspaces: A literature review. Urban For. Urban Green. 2023, 84, 127936. [Google Scholar] [CrossRef]
- Li, J.; Xie, Y.; Xu, J.; Zhang, C.; Wang, H.; Huang, D.; Li, G.; Tian, J. Association between greenspace and cancer: Evidence from a systematic review and meta-analysis of multiple large cohort studies. Environ. Sci. Pollut. Res. 2023, 30, 91140–91157. [Google Scholar] [CrossRef]
- Gao, Y.; Pa, K.; Li, H.; Zhao, B. Greenspace Exposure with Chronic Obstructive Pulmonary Disease: A Systematic Review. Forest 2024, 15, 634. [Google Scholar] [CrossRef]
- Frank, L.D.; Wali, B. Treating two pandemics for the price of one: Chronic and infectious disease impacts of the built and natural environment. Sustain. Cities Soc. 2021, 73, 103089. [Google Scholar] [CrossRef]
- Wali, B.; Frank, L.D.; Chapman, J.; Fox, E.H. Role of Walkability, Bike Infrastructure, and Greenspace in Combatting Chronic Diseases: A Heterogeneous Ecological Analysis in the United States. Sustain. Cities Soc. 2024, 113, 105550. [Google Scholar] [CrossRef]
- Li, R.; Liu, M.; Song, J.; Xu, Y.; He, A.; Hu, X.; Yang, S.; Ding, G.; Chen, M.; Jin, C. Association between residential greenspace and mental health among cancer survivors in Shanghai, China. Environ. Res. Lett. 2023, 238, 117155. [Google Scholar] [CrossRef]
- Venter, Z.S.; Krog, N.H.; Barton, D.N. Linking green infrastructure to urban heat and human health risk mitigation in Oslo, Norway. Sci. Total Environ. 2020, 709, 136193. [Google Scholar] [CrossRef]
- Sun, S.; Sarkar, C.; Kumari, S.; James, P.; Cao, W.; Lee, R.S.-Y.; Tian, L.; Webster, C. Air pollution associated respiratory mortality risk alleviated by residential greenness in the Chinese Elderly Health Service Cohort. Environ. Res. Lett. 2020, 183, 109139. [Google Scholar] [CrossRef]
- Bauwelinck, M.; Casas, L.; Nawrot, T.S.; Nemery, B.; Trabelsi, S.; Thomas, I.; Aerts, R.; Lefebvre, W.; Vanpoucke, C.; Nieuwenhuyse, A.V.; et al. Residing in urban areas with higher green space is associated with lower mortality risk: A census-based cohort study with ten years of follow-up. Environ. Int. 2021, 148, 106365. [Google Scholar] [CrossRef]
- Houlden, V.; Albuquerque, J.P.d.; Weich, S.; Jarvis, S. A spatial analysis of proximate greenspace and mental wellbeing in London. Appl. Geogr. 2019, 109, 102036. [Google Scholar] [CrossRef]
- James, P.; Hart, J.E.; Banay, R.F.; Laden, F. Exposure to Greenness and Mortality in a Nationwide Prospective Cohort Study of Women. Environ. Health Perspect. 2016, 124, 1344–1352. [Google Scholar] [CrossRef]
- Labib, S.M.; Lindley, S.; Huck, J.J. Estimating multiple greenspace exposure types and their associations with neighbourhood premature mortality: A socioecological study. Sci. Total Environ. 2021, 789, 147919. [Google Scholar] [CrossRef]
- Klompmaker, J.O.; Hoek, G.; Bloemsma, L.D.; Marra, M.; Wijga, A.H.; Brink, C.v.d.; Brunekreef, B.; Lebret, E.; Gehring, U.; Janssen, N.A.H. Surrounding green, air pollution, traffic noise exposure and non-accidental and cause-specific mortality. Environ. Int. 2020, 134, 105341. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuijsen, M.J.; Gascon, M.; Martinez, D.; Ponjoan, A.; Blanch, J.; Garcia-Gil, M.d.M.; Ramos, R.; Foraster, M.; Mueller, N.; Espinosa, A.; et al. Air Pollution, Noise, Blue Space, and Green Space and Premature Mortality in Barcelona: A Mega Cohort. Int. J. Environ. Res. Public Health 2018, 15, 2405. [Google Scholar] [CrossRef] [PubMed]
- Kabisch, N.; Strohbach, M.; Haase, D.; Kronenberg, J. Urban green space availability in European cities. Ecol. Indic. 2016, 70, 586–596. [Google Scholar] [CrossRef]
- Ryan, S.C.; Sugg, M.M.; Runkle, J.D.; Thapa, B. Advancing Understanding on Greenspace and Mental Health in Young People. GeoHealth 2024, 8, e2023GH000959. [Google Scholar] [CrossRef]
- Baka, A.; Mabon, L. Assessing equality in neighbourhood availability of quality greenspace in Glasgow, Scotland, United Kingdom. Landsc. Res. 2022, 47, 584–597. [Google Scholar] [CrossRef]
- Ye, Y.; Xiang, Y.; Qiu, H.; Li, X. Revealing urban greenspace accessibility inequity using the carrying capacity-based 3SFCA method and location big data. Sustain. Cities Soc. 2024, 108, 105513. [Google Scholar] [CrossRef]
- Zhang, J.; Yu, Z.; Zhao, B.; Sun, R.; Vejre, H. Links between green space and public health: A bibliometric review of global research trends and future prospects from 1901 to 2019. Environ. Res. Lett. 2020, 15, 063001. [Google Scholar] [CrossRef]
- Viinikka, A.; Paloniemi, R.; Assmuth, T. Mapping the distributive environmental justice of urban waters. Fenn. Int. J. Geogr. 2018, 196, 9–23. [Google Scholar] [CrossRef]
- Mears, M.; Brindley, P.; Jorgensen, A.; Maheswaran, R. Population-level linkages between urban greenspace and health inequality: The case for using multiple indicators of neighbourhood greenspace. Health Place 2020, 62, 102284. [Google Scholar] [CrossRef] [PubMed]
- Koliotsis, P.T.A.; Papadopoulou, M.P. Spatial Analysis of the Accessibility of Urban Greenspace at the City Level. Eur. J. Environ. Sci. 2020, 10, 15–21. [Google Scholar] [CrossRef]
- Barber, A.; Haase, D.; Wolff, M. Permeability of the city—Physical barriers of and in urban green spaces in the city of Halle, Germany. Ecol. Indic. 2021, 125, 107555. [Google Scholar] [CrossRef]
- Tannous, H.O.; Major, M.D.; Furlan, R. Accessibility of green spaces in a metropolitan network using space syntax to objectively evaluate the spatial locations of parks and promenades in Doha, State of Qatar. Urban For. Urban Green. 2021, 58, 126892. [Google Scholar] [CrossRef]
- World Health Organization. Urban Green Spaces: A Brief for Action; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Natural England. Green Infrastructure Standards for England—Summary; Natural England: London, UK, 2023. [Google Scholar]
- Roscoe, C.; Mackay, C.; Gulliver, J.; Hodgson, S.; Cai, Y.; Vineis, P.; Fecht, D. Associations of private residential gardens versus other greenspace types with cardiovascular and respiratory disease mortality: Observational evidence from UK Biobank. Environ. Int. 2022, 167, 107427. [Google Scholar] [CrossRef]
- Wang, R.; Feng, Z.; Pearce, J. Neighbourhood greenspace quantity, quality and socioeconomic inequalities in mental health. Cites 2022, 129, 103815. [Google Scholar] [CrossRef]
- Jalkanen, J.; Fabritius, H.; Vierikko, K.; Moilanen, A.; Toivonen, T. Analyzing fair access to urban green areas using multimodal accessibility measures and spatial prioritization. Appl. Geogr. 2020, 124, 102320. [Google Scholar] [CrossRef]
- Markevych, I.; Schoierer, J.; Hartig, T.; Chudnovsky, A.; Hystad, P.; Dzhambov, A.M.; Vries, S.d.; Triguero-Mas, M.; Brauer, M.; Nieuwenhuijsen, M.J.; et al. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ. Res. 2017, 158, 301–317. [Google Scholar] [CrossRef] [PubMed]
- Moran, M.R.; Bilal, U.; Dronova, I.; Ju, Y.; Gouveia, N.; Caiaffa, W.T.; Friche, A.A.d.L.; Moore, K.; Miranda, J.J.; Rodríguez, D.A. The equigenic effect of greenness on the association between education with life expectancy and mortality in 28 large Latin American cities. Health Place 2021, 72, 102703. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.; Popham, F. Effect of exposure to natural environment on health inequalities: An observational population study. Lancet 2008, 372, 1655–1660. [Google Scholar] [CrossRef] [PubMed]
- Hartig, T.; Astell-Burt, T.; Bergsten, Z.; Amcoff, J.; Mitchell, R.; Feng, X. Associations between greenspace and mortality vary across contexts of community change: A longitudinal ecological study. J. Epidemiol. Community Health 2020, 74, 534–540. [Google Scholar] [CrossRef]
- Schinasi, L.H.; Kondo, M.C.; Edwards, J.; Clougherty, J.E.; Roos, A.J.D.; Bilal, U. Does Urban Greenspace Reduce Mortality Inequalities Based on Poverty, Race, or Both in Philadelphia, PA? J. Urban Health 2023, 100, 686–695. [Google Scholar] [CrossRef]
- Maas, J.; Verheij, R.A.; Vries, S.d.; Spreeuwenberg, P.; Schellevis, F.G.; Groenewegen, P.P. Morbidity is related to a green living environment. J. Epidemiol. Community Health 2009, 63, 967–973. [Google Scholar] [CrossRef]
- Orioli, R.; Antonucci, C.; Scortichini, M.; Cerza, F.; Marando, F.; Ancona, C.; Manes, F.; Davoli, M.; Michelozzi, P.; Forastiere, F.; et al. Exposure to residential greenness as a predictor of cause-specific mortality and stroke incidence in the rome longitudinal study. Environ. Health Perspect. 2019, 127, 027002. [Google Scholar] [CrossRef]
- Jarvis, I.; Gergel, S.; Koehoorn, M.; Bosch, M.v.d. Greenspace access does not correspond to nature exposure: Measures of urban natural space with implications for health research. Landsc. Urban Plan. 2020, 194, 103686. [Google Scholar] [CrossRef]
- Browning, M.H.E.M.; Rigolon, A.; McAnirlin, O.; Yoon, H.V. Where greenspace matters most: A systematic review of urbanicity, greenspace, and physical health. Landsc. Urban Plan. 2022, 217, 104233. [Google Scholar] [CrossRef]
- Cao, Y.; Yu, W.; Li, C.; Chu, Z.; Guo, B.; Wang, H.; Ma, W.; Xu, X.; Liu, Q.; Zhao, Q. Association between greenspace morphology and dengue fever in China. Parasites Vectors 2025, 18, 115. [Google Scholar] [CrossRef]
- Helbich, M.; Blüml, V.; Jong, T.d.; Plener, P.L.; Kwan, M.-P.; Kapusta, N.D. Urban–rural inequalities in suicide mortality: A comparison of urbanicity indicators. Int. J. Health Geogr. 2017, 16, 39. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Shi, K.; Wu, Y.; Chang, Z. Remotely sensed nighttime lights reveal China’s urbanization process restricted by haze pollution. Build. Environ. 2021, 206, 108350. [Google Scholar] [CrossRef]
- Zheng, Q.; Seto, K.C.; Zhou, Y.; You, S.; Weng, Q. Nighttime light remote sensing for urban applications: Progress, challenges, and prospects. ISPRS J. Photogramm. Remote Sens. 2023, 202, 125–141. [Google Scholar] [CrossRef]
- Li, T.; Guo, Z.; Ma, C. Dynamic Characteristics of Urbanization Based on Nighttime Light Data in China’s “Plain–Mountain Transition Zone”. Int. J. Environ. Res. Public Health 2022, 19, 9230. [Google Scholar] [CrossRef]
- World Health Organization. Healthy Cities: Effective Approach to a Rapidly Changing World; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Greater London Authority. MSOA Atlas. Available online: https://data.london.gov.uk/dataset/msoa-atlas/ (accessed on 2 April 2023).
- Office for Health Improvement and Disparities. Public Health Profiles. Available online: https://fingertips.phe.org.uk/profile/health-profiles (accessed on 25 February 2025).
- Brousmiche, D.; Lanier, C.; Occelli, F.; Pochet, L.; Degezelle, S.; Genin, M.; Deram, A.; Cuny, D. Spatial scale and spatial effects: Shedding light on how a change of scale can affect the characterization of environmental health inequalities. Environ. Sci. Policy 2023, 144, 20–30. [Google Scholar] [CrossRef]
- Lachowycz, K.; Jones, A.P. Does walking explain associations between access to greenspace and lower mortality? Soc. Sci. Med. 2014, 107, 9–17. [Google Scholar] [CrossRef]
- Greenspace Information for Greater London CIC. Our Data Holdings. Available online: https://www.gigl.org.uk/our-data-holdings/ (accessed on 9 February 2023).
- Cao, X.; Onishi, A.; Chen, J.; Imura, H. Quantifying the cool island intensity of urban parks using ASTER and IKONOS data. Landsc. Urban Plan. 2010, 96, 224–231. [Google Scholar] [CrossRef]
- Zhang, F.; Qian, H. A comprehensive review of the environmental benefits of urban green spaces. Environ. Res. Lett. 2024, 252, 118837. [Google Scholar] [CrossRef]
- Ordnance Survey. OS Open Roads Data. Available online: https://docs.os.uk/os-downloads/networks/os-open-roads/os-open-roads-overview/os-open-roads-data (accessed on 19 November 2024).
- OpenStreetMap. OSM Buildings Data. Available online: https://cesium.com/platform/cesium-ion/content/cesium-osm-buildings/ (accessed on 9 May 2024).
- Noble, S.; McLennan, D.; Noble, M.; Plunkett, E.; Gutacker, N.; Silk, M.; Wright, G. The English Indices of Deprivation 2019 Research Report Ministry of Housing; Ministry of Housing, Communities & Local Government: London, UK, 2019.
- Yang, Z.; Kwan, M.-P.; Liu, D.; Huang, J. How objective and subjective greenspace, combined with air and noise pollution, impacts mental health through the mediation of physical activity. Urban For. Urban Green. 2025, 105, 128683. [Google Scholar] [CrossRef]
- Viinikka, A.; Tiitu, M.; Heikinheimo, V.; Halonen, J.I.; Nyberg, E.; Vierikko, K. Associations of neighborhood-level socioeconomic status, accessibility, and quality of green spaces in Finnish urban regions. Appl. Geogr. 2023, 157, 102973. [Google Scholar] [CrossRef]
- Weeks, W.B.; Chang, J.E.; Pagán, J.A.; Aerts, A.; Weinstein, J.N.; Ferres, J.L. An observational, sequential analysis of the relationship between local economic distress and inequities in health outcomes, clinical care, health behaviors, and social determinants of health. Int. J. Equity Health 2023, 22, 181. [Google Scholar] [CrossRef]
- Cheng, J.; Cui, Y.; Wang, X.; Wang, Y.; Feng, R. Spatial characteristics of health outcomes and geographical detection of its influencing factors in Beijing. Front. Public Health 2024, 12, 1424801. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.H.; Kwon, Y.D. Patterns of health literacy and influencing factors differ by age: A cross-sectional study. BMC Public Health 2025, 25, 1556. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Liu, Y.; Zhang, Y.; Liu, Y.; Wang, B.; Zhang, G. Spatially Varying Relationships between Land Subsidence and Urbanization: A Case Study in Wuhan, China. Remote Sens. 2022, 14, 291. [Google Scholar] [CrossRef]
- Yuan, X.; Li, Y.; Song, Y.; Lu, H.; Wang, Y.; Ge, B.; Wang, J. Spatial Distribution Characteristics and Driving Factors of 777 Traditional Villages in Yunnan Province: A Study Based on GWR Model and Geodetector. Land 2024, 13, 2004. [Google Scholar] [CrossRef]
- Yang, C.; Li, R.; Sha, Z. Exploring the Dynamics of Urban Greenness Space and Their Driving Factors Using Geographically Weighted Regression: A Case Study in Wuhan Metropolis, China. Land 2020, 9, 500. [Google Scholar] [CrossRef]
- Huang, B.; Wu, B.; Barry, M. Geographically and temporally weighted regression for modeling spatio-temporal variation in house prices. Int. J. Geogr. Inf. Sci. 2010, 24, 383–401. [Google Scholar] [CrossRef]
- Kupfer, J.A.; Farris, C.A. Incorporating spatial non-stationarity of regression coefficients into predictive vegetation models. Landsc. Ecol. 2007, 22, 837–852. [Google Scholar] [CrossRef]
- Wang, H.; Qin, F.; Xu, C.; Li, B.; Guo, L.; Wang, Z. Evaluating the suitability of urban development land with a Geodetector. Ecol. Indic. 2021, 123, 107339. [Google Scholar] [CrossRef]
- Greater London Authority. Access to Public Open Space and Nature by Ward; Greater London Authority: London, UK, 2012.
- Pang, Z.; Xie, B.; An, Z.; Wang, L. Spatial and moderating effects of greenspace on the association between air pollution and lung cancer incidence. Appl. Geogr. 2024, 164, 103207. [Google Scholar] [CrossRef]
- Tan, L.Y.; Wang, Y.; Yang, L.; Chen, C.-S.; Zhang, F.; Yua, M.-T.; Guo, P.; Zhang, Q.-Y. Residing in areas with high residential greenspace is associated with increased COPD risk and decreased lung function of adults in eastern China. Heart Lung 2025, 70, 329–338. [Google Scholar] [CrossRef]
- Cao, Z.; Xu, C.; Li, S.; Wang, Y.; Yang, H. Residential greenspace and risk of cancer: A prospective cohort study from the UK Biobank. Sci. Total Environ. 2023, 871, 162145. [Google Scholar] [CrossRef] [PubMed]
- Datzmann, T.; Markevych, I.; Trautmann, F.; Heinrich, J.; Schmitt, J.; Tesch, F. Outdoor air pollution, green space, and cancer incidence in Saxony: A semi-individual cohort study. BMC Public Health 2018, 18, 715. [Google Scholar] [CrossRef] [PubMed]
- Sakhvidi, M.J.Z.; Yang, J.; Siemiatycki, J.; Dadvand, P.; Hoogh, K.d.; Vienneau, D.; Goldberg, M.; Zins, M.; Lequy, E.; Jacquemin, B. Greenspace exposure and cancer incidence: A 27-year follow-up of the French GAZEL cohort. Sci. Total Environ. 2021, 787, 15. [Google Scholar] [CrossRef] [PubMed]
- Douglas, J.A.; Archer, R.S.; Alexander, S.E. Ecological determinants of respiratory health: Examining associations between asthma emergency department visits, diesel particulate matter, and public parks and open space in Los Angeles, California. Prev. Med. Rep. 2019, 14, 100855. [Google Scholar] [CrossRef]
- Wang, R.; Feng, Z.; Pearce, J.; Zhou, S.; Zhang, L.; Liu, Y. Dynamic greenspace exposure and residents’ mental health in Guangzhou, China: From over-head to eye-level perspective, from quantity to quality. Landsc. Urban Plan. 2021, 215, 104230. [Google Scholar] [CrossRef]
- Wilson, B.; Neale, C.; Roe, J. Urban green space access, social cohesion, and mental health outcomes before and during COVID-19. Cities 2024, 152, 105173. [Google Scholar] [CrossRef]
- Ambrey, C.L.; Shahni, T.J. Greenspace and wellbeing in Tehran: A relationship conditional on a neighbourhood’s crime rate. Urban For. Urban Green. 2017, 27, 155–161. [Google Scholar] [CrossRef]
- Milà, C.; Ranzani, O.; Sanchez, M.; Ambrós, A.; Bhogadi, S.; Kinra, S.; Kogevinas, M.; Dadvand, P.; Tonne, C. Land-Use Change and Cardiometabolic Risk Factors in an Urbanizing Area of South India: A Population-Based Cohort Study. Environ. Health Perspect. 2020, 128, 47003. [Google Scholar] [CrossRef]
- Fong, K.C.; Hart, J.E.; James, P. A Review of Epidemiologic Studies on Greenness and Health: Updated Literature Through 2017. Curr. Environ. Health Rep. 2018, 5, 77–78. [Google Scholar] [CrossRef]
- Krabbendam, L.; Vugt, M.v.; Conus, P.; Söderström, O.; Empson, L.A.; Os, J.v.; Fett, A.-K.J. Understanding urbanicity: How interdisciplinary methods help to unravel the effects of the city on mental health. Psychol. Med. 2021, 51, 1099–1110. [Google Scholar] [CrossRef]
- Dzhambov, A.M.; Browning, M.H.E.M.; Markevych, I.; Hartig, T.; Lercher, P. Analytical approaches to testing pathways linking greenspace to health: A scoping review of the empirical literature. Environ. Res. Lett. 2020, 186, 109613. [Google Scholar] [CrossRef]
- Vukomanovic, J.; Singh, K.K.; Vogler, J.B.; Meentemeyer, R.K. Protection status and proximity to public-private boundaries influence land use intensification near U.S. parks and protected areas. Conserv. Sci. Pract. 2020, 2, e190. [Google Scholar] [CrossRef]
- Rigolon, A. A complex landscape of inequity in access to urban parks: A literature review. Landsc. Urban Plan. 2016, 153, 160–169. [Google Scholar] [CrossRef]
- Smith, A. Beyond the pale: Fencing off parks for festivals. Urban Stud. 2023, 60, 2763–2778. [Google Scholar] [CrossRef]
- Xie, X.; Zhou, H.; Gou, Z.; Yi, M. Spatiotemporal Patterns of the Use of Green Space by White-Collar Workers in Chinese Cities: A Study in Shenzhen. Land 2021, 10, 1006. [Google Scholar] [CrossRef]
- Zhou, Y.; Lu, Y. Health effects of greenspace morphology: Large, irregular-shaped, well-connected, and close-clustered greenspaces may reduce mortality risks, especially for neighborhoods with higher aging levels. Environ. Res. Lett. 2024, 263, 120095. [Google Scholar] [CrossRef] [PubMed]
- Astell-Burt, T.; Feng, X. Association of Urban Green Space With Mental Health and General Health Among Adults in Australia. JAMA Netw. Open 2019, 2, e198209. [Google Scholar] [CrossRef]
- He, Q.; Liu, L.; Chang, H.-T.; Wu, C.-D.; Ji, J.S. Residential green space structures and mortality in an elderly prospective longitudinal cohort in China. Environ. Res. Lett. 2021, 16, 094003. [Google Scholar] [CrossRef]
- Zhou, W.; Wang, Q.; Kadier, A.; Wang, W.; Zhou, F.; Li, R.; Ling, L. The role of residential greenness levels, green land cover types and diversity in overweight/obesity among older adults: A cohort study. Environ. Res. Lett. 2023, 217, 114854. [Google Scholar] [CrossRef]
- Creed, C.; Carvalho, J.S. Exploring the user experience, quality, and provision of urban greenspace: A mixed-method approach. Urban For. Urban Green. 2024, 100, 128470. [Google Scholar] [CrossRef]
- Dawson, L.; Elbakidze, M.; Ermel, L.E.K.v.; Olsson, U.; Ongena, Y.P.; Schaffer, C.; Johansson, K.-E. Why don’t we go outside?—Perceived constraints for users of urban greenspace in Sweden. Urban For. Urban Green. 2023, 82, 127865. [Google Scholar] [CrossRef]
- Cheng, J.; Lu, M.; Sun, H.; Mao, Y. A survival analysis of patients with an acute exacerbation of chronic obstructive pulmonary disease discharged from the respiratory intensive care unit. Ann. Palliat. Med. 2020, 9, 1812–1820. [Google Scholar] [CrossRef]
- Sakhvidi, M.J.Z.; Yang, J.; Mehrparvar, A.H.; Dzhambov, A.M.; Ebrahimi, A.; Dadvand, P.; Jacquemin, B. Exposure to greenspace and cancer incidence, prevalence, and mortality: A systematic review and meta-analyses. Sci. Total Environ. 2022, 838, 156180. [Google Scholar] [CrossRef]
- Dong, P.-P.; Chen, G.; Wen, Y.; Heinrich, J.; Fuertes, E.; Zhao, T.; Idrose, N.S.; Lin, L.-Z.; Gui, Z.-H.; Qin, X.; et al. Greenspace and respiratory diseases and symptoms in Chinese children: A large-scale study exploring joint associations with ozone. Sustain. Cities Soc. 2025, 124, 106329. [Google Scholar] [CrossRef]
- Takashima, M.D.; Grimwood, K.; Vilcins, D.; Knibbs, L.D.; Sly, P.D.; Lambert, S.B. Association of antenatal and early childhood air pollution and greenspace exposures with respiratory pathogen upper airway acquisitions and respiratory health outcomes. Int. J. Environ. Health Res. 2024, 34, 3147–3160. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Piedrahita, C.; Roscoe, C.J.; Howe, C.; Fecht, D.; Nazelle, A.d. Holistic approach to assess the association between the synergistic effect of physical activity, exposure to greenspace, and fruits and vegetable intake on health and wellbeing: Cross-sectional analysis of UK Biobank. Front. Public Health 2022, 10, 886608. [Google Scholar] [CrossRef] [PubMed]
- Barbey, C.; Bonvallot, N.; Clerc, F. Health Outcomes Related to Multiple Exposures in Occupational Settings: A Review. Saf. Health Work. 2024, 15, 382–395. [Google Scholar] [CrossRef]
- Biernacka, M.; Kronenberg, J.; Łaszkiewicz, E. An integrated system of monitoring the availability, accessibility and attractiveness of urban parks and green squares. Appl. Geogr. 2020, 116, 102152. [Google Scholar] [CrossRef]


| Dataset | Source | Description | Time Range (Year) |
|---|---|---|---|
| Chronic diseases mortality data | Office for National Statistics (ONS) | Includes indirect standardized mortality ratios for cancer and respiratory diseases in Greater London. For ethical considerations, the data do not include personal privacy characteristics or medical records. | 2016–2020 |
| Greenspace data | Greenspace Information for Greater London (GiGL) | Providing geo-spatial data on more than 20,000 greenspaces in Greater London. | 1986–2008 |
| Geo-spatial data (road network and residential area) | Ordnance Survey/OpenStreetMap | Providing road-network data and residential area data for Greater London. | 2025 |
| Socio-economic indicator (IMD 2019) | Ministry of Housing, Communities and Local Government | Provides socio-economic data for various areas within London, including seven different dimensions: income, employment, educational attainment, health, crime, barriers to housing and services, and living conditions. | 2019 |
| Nighttime light data | Google Earth Engine (GEE) | Used to measure the level of urbanization in Greater London | 2019 |
| Air quality data | The Greater London Authority (GLA) and Transport for London (TFL) | Includes emissions at grid level for NOx, PM2.5, and CO2 in tonnes/year, for all sources. | 2019 |
| Variables | Description | |
|---|---|---|
| Dependent variables | Cancer SMRs | Indirect standardized mortality ratios for cancer |
| Respiratory disease SMRs | Indirect standardized mortality ratios for respiratory diseases | |
| Core independent variable | Greenspace accessibility | Greenspace accessibility measured by shortest road-network distance |
| Covariates | Income | The proportion of the population in an area experiencing deprivation relating to low income |
| Education | The proportion of the population lacking attainment and skills | |
| Employment | The proportion of the working-age population in an area involuntarily excluded from the labor market | |
| Crime | The risk of personal and material victimization at local level | |
| Housing | The physical and financial accessibility of housing and local services | |
| Health | The risk of premature death and the impairment of quality of life through poor physical or mental health. | |
| Built environment | The quality of the local environment | |
| Air quality | Emissions at grid level for NOx, PM2.5, and CO2 in tonnes/year | |
| Variables | Definition |
|---|---|
| Predicted value of the standardized mortality ratio (cancer and respiratory diseases) at position i | |
| Coordinates of point i | |
| Intercept | |
| Regression coefficient of the kth independent variable on point i; can be obtained using the weight function approach | |
| Error term at position i | |
| Value of the independent variable (including greenspace accessibility and other socio-economic factors) at position i |
| Cancer | L1 * | L2 * | L3 * | L4 * |
|---|---|---|---|---|
| URB | 92.8 | 92.6 | 89.4 | 90.2 |
| IMD | 80.8 | 86.7 | 94.0 | 103.5 |
| CHI | 97.6 | 90.5 | 88.8 | 88.1 |
| OLD | 84.4 | 87.8 | 96.4 | 96.3 |
| Work | 92.0 | 91.4 | 91.4 | 90.2 |
| Respiratory diseases | ||||
| URB | 92.6 | 89.5 | 92.5 | 89.2 |
| IMD | 72.8 | 84.0 | 96.8 | 110.2 |
| CHI | 105.7 | 92.2 | 85.8 | 80.1 |
| OLD | 78.9 | 87.9 | 96.8 | 100.2 |
| Work | 87.3 | 92.4 | 95.5 | 88.6 |
| Variables | Cancer | Respiratory Diseases | ||||
|---|---|---|---|---|---|---|
| Coefficient (β) | p-Value | R2 | Coefficient (β) | p-Value | R2 | |
| Greenspace accessibility | −0.1265 | 0.0001 | 0.0144 | −0.1233 | 0.0001 | 0.0115 |
| Greenspace accessibility with other six variables | −0.0499 | 0.0394 | 0.3013 | −0.0486 | 0.0142 | 0.2920 |
| Variables | Cancer | Respiratory Diseases | ||||
|---|---|---|---|---|---|---|
| Coefficient (β) | p-Value | R2 | Coefficient (β) | p-Value | R2 | |
| Greenspace accessibility | −0.1342 | <0.001 | 0.2274 | −0.1102 | <0.001 | 0.2458 |
| Greenspace accessibility with other six variables | −0.0759 | <0.001 | 0.4654 | −0.0358 | <0.001 | 0.4978 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, L.; Chen, W. Modulating Effects of Urbanization and Age on Greenspace–Mortality Associations: A London Study Using Nighttime Light Data and Spatial Regression. Appl. Sci. 2025, 15, 9328. https://doi.org/10.3390/app15179328
Fan L, Chen W. Modulating Effects of Urbanization and Age on Greenspace–Mortality Associations: A London Study Using Nighttime Light Data and Spatial Regression. Applied Sciences. 2025; 15(17):9328. https://doi.org/10.3390/app15179328
Chicago/Turabian StyleFan, Liwen, and Wei Chen. 2025. "Modulating Effects of Urbanization and Age on Greenspace–Mortality Associations: A London Study Using Nighttime Light Data and Spatial Regression" Applied Sciences 15, no. 17: 9328. https://doi.org/10.3390/app15179328
APA StyleFan, L., & Chen, W. (2025). Modulating Effects of Urbanization and Age on Greenspace–Mortality Associations: A London Study Using Nighttime Light Data and Spatial Regression. Applied Sciences, 15(17), 9328. https://doi.org/10.3390/app15179328





