Abstract
Post-surgical complications are common complications following saphenectomy surgery, and strategies to facilitate its resolution are essential for postoperative recovery. This study evaluated the effects of adhesive elastic taping on edema control in patients undergoing saphenectomy. A randomized controlled clinical trial was conducted with 40 patients of both sexes, divided into two groups: intervention (IG), which received taping immediately after surgery combined with standard compression, and a control group, which received standard treatment with compression stockings (CG). Assessments were performed preoperatively and seven days after surgery, including limb volume (indirect calculation), edema (dielectric constant analysis), Skin Elasticity Assessment (durometer), pain (Visual Analog Scale—VAS), limb functionality (Lower Extremity Functional Scale—LEFS), and ecchymosis area (Image J, version 1.51). Both groups showed a significant increase in edema postoperatively (IG: p = 0.003; CG: p = 0.001). The intervention group exhibited a trend toward volume reduction (p = 0.069), better functionality (p = 0.006)—skin elasticity was assessed using a durometer—and fewer ecchymoses (p = 0.002). Only the control group showed a significant increase in tissue firmness (p = 0.012). No significant difference in pain was observed between groups (p = 0.203). The application of taping demonstrated beneficial effects on postoperative functional recovery and ecchymosis control following saphenectomy.
1. Introduction
The post-surgical recovery of patients undergoing saphenectomy can be significantly affected by complications such as edema and ecchymosis, which delay rehabilitation and impact clinical outcomes [1,2]. Although compression therapy with stockings is considered the standard approach for managing these effects [3], new strategies are being investigated to enhance edema reduction and provide a more efficient postoperative recovery.
Functional elastic bandaging, also known as taping, emerges as an innovative and accessible alternative for surgical edema management, offering advantages in terms of cost-effectiveness, applicability, and patient tolerance. This technique, based on the application of an elastic adhesive cotton tape, is thermoactive and has elasticity similar to the skin, promoting a biomechanical effect that stimulates blood and lymphatic circulation by generating compression and decompression of capillaries during movement [4,5]. Additionally, it may modulate exaggerated inflammatory responses in the tissue, contributing to a more efficient healing process [6,7].
Taping has demonstrated beneficial effects, particularly in recovery control across various surgical contexts, including plastic surgeries [8], third molar extraction [9,10] orthopedic procedures [11], post-mastectomy lymphedema [12,13], and venous insufficiency symptoms [14]. Despite its growing use for different therapeutic purposes, its specific effectiveness in the post-saphenectomy recovery process has yet to be explored.
The objective of this study was to evaluate the impact of taping on post-saphenectomy recovery, analyzing its efficacy compared to conventional methods for postoperative event management. This study aims to expand the use of taping as a complementary resource in vascular disease recovery protocols, providing a practical and non-invasive alternative for patients suffering from chronic venous insufficiency.
2. Materials and Methods
2.1. Ethical Aspects
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Human Research Ethics Committee of the Faculty of Medicine of Ribeirão Preto—São Paulo—Brazil (FMRP/USP) under protocol number 5.596.054. Registered in Clinical Trials under number 12241. Informed consent was obtained from all subjects involved in the study.
2.2. Eligibility Criteria
Individuals of both sexes who underwent unilateral saphenectomy were included in the study, with a mean age of 42 years. Non-inclusion criteria comprised patients diagnosed with allergies, skin lesions, or ulcers in the limb being assessed.
2.3. Description of the Experiment
Participants were randomly allocated into two groups: one receiving standard compression therapy and the other undergoing compression taping immediately after surgery.
The clinical trial was conducted in accordance with the guidelines of the Consolidated Standards of Reporting Trials (CONSORT). One researcher was responsible for determining participant eligibility and conducting assessments using a standardized anamnesis form. A second researcher was in charge of randomizing participants into their respective groups and performing therapeutic procedures, while a third researcher analyzed the data, remaining blinded to group allocation.
Patients were randomly assigned in small blocks of 5:5, meaning that every five participants were allocated to each study group using sealed, opaque envelopes to ensure concealed allocation. Randomization was performed through a lottery draw of the envelopes.
2.4. Conventional Postoperative Treatment
Patients assigned to the conventional treatment group underwent seven days of compressive bandaging following surgery. Subsequently, they were instructed to wear 7/8-length elastic compression stockings with moderate compression (20–30 mmHg) for 24 h per day over a 7-day period. This approach aligns with standard postoperative protocols aimed at minimizing edema, hematoma formation, and improving venous circulation.
2.5. Taping Application
The experimental group received taping applied to the lower limb immediately post-surgery. The technique involved elastic bandages measuring 20 cm and 15 cm, arranged in a fish-scale pattern to optimize lymphatic and blood flow, using AKTive Tape® (Suzhou SunMed, Suzhou, China). The active tension applied in the functional region of the bandage was set at 80%, whereas the base and anchor sections (5 cm) were placed without tension to allow physiological adaptation (Figure 1).

Figure 1.
Image of the lower limb in the post-operative period of saphenectomy with taping application.
2.5.1. Evaluation Criteria
Both groups were monitored for postoperative edema, pain levels, and functional recovery using validated assessment scales and imaging techniques. Measurements were taken at baseline (pre-surgery) and at 7-day follow-up to compare the efficacy of both treatments.
2.5.2. Edema Assessment
For edema assessment, a non-invasive method for quantifying water content at different tissue depths was employed using the MoistureMeter D® (Delfin Technologies, Kuopio, Finland). The dielectric constant (DC) of the skin generated a high-frequency electromagnetic (EM) wave at 300 MHz, which was transmitted to the coaxial probe model S15. This probe provides information related to the dermis, with a measurement depth ranging from 1.5 mm to 3 mm [15]. The DC of the tissue is proportional to water content, meaning that higher readings indicate greater hydration levels [15,16].
Participants remained at rest for 5 min in a supine position on an examination table in a temperature-controlled room (24 °C) before the procedure. The probe was positioned perpendicularly to the skin with stable pressure, taking measurements at five points along the medial region of the lower limbs.
Lower limb perimetry was performed by the same evaluator, using a graduated measuring tape in centimeters, with the participant in a supine position [17]. Measurements were taken at the dorsum of the foot, ankle, and from this joint, five additional measurements were recorded every 10 cm up to the inguinal region.
The limb volume was calculated based on perimetry data using an indirect method, summing the approximate volume of six truncated cones according to the following formula [18]: volume = (h) (C1 × C2 + C12 + C22)/12π
2.5.3. Skin Elasticity Assessment
Skin elasticity was assessed using the ElastiMeter® (Delfin Technologies, Kuopio, Finland), a device that enables instantaneous measurements of elastic properties and biophysical changes in the skin. For each evaluation point, five consecutive measurements were performed, and the mean value of these readings was used to determine the Elastic Support Index (ESI), expressed in N/m. Assessments were conducted at five distinct points on the medial region of the lower limbs, with 10 cm spacing between them.
2.5.4. Pain Assessment
Pain was quantified using the Numerical Visual Scale (NVS), where a score of 0 represented no pain and a score of 10 indicated the worst imaginable pain [19]. The scale was applied on the seventh postoperative day.
2.5.5. Lower Limb Functionality Assessment
The functionality of the lower limbs was assessed using the Lower Extremity Functional Scale—LEFS [20], which measures musculoskeletal dysfunctions in this region. The scale consists of 20 items, each scored on a scale from zero to four, with a maximum possible score of 80. Patients completed the questionnaire, and the total score was obtained by summing the responses to all 20 items. A minimum score of 0 indicates a reduced functional level, while a maximum score of 80 represents high functionality [20,21]. The scale was applied on the seventh postoperative day.
2.5.6. Ecchymosis Area Analysis
The ecchymosis area was assessed using Image J (Wayne Rasband at the National Institutes of Health—NIH, Bethesda, MD, USA), version 1.51, 2018, an advanced image analysis software that enables precise quantification of lesion dimensions. The tool allowed for accurate measurement of the affected region by analyzing digital images and detecting the boundaries of the ecchymoses. This methodology ensured objective evaluation, minimizing potential biases and enhancing the reliability of the data collected.
2.5.7. Statistical Analysis
The sample size calculation was processed using SPSS software, version 20 (IBM, Armonk, NY, USA). The sample size was determined based on the study conducted by Aguilar-Ferrándiz et al. [14], considering the effect of taping on edema as the primary outcome variable. A statistical power of 80%, a significance level of 5%, and potential sample losses were accounted for, resulting in a required sample size of 20 volunteers per group.
Statistical analysis was performed using SPSS software (version 20), applying non-parametric statistical tests due to the nature of the data and the observed distribution. For comparisons between more than two groups, the Kruskal-Walli’s test was applied. For paired comparisons, the Wilcoxon test was used, while the Mann-Whitney test was employed for comparisons between independent groups. The adopted significance level was 5% (p < 0.05).
3. Results
The following flow chart (Figure 2) presents the stages of the clinical trial, detailing the process of participant selection, intervention, and analysis.
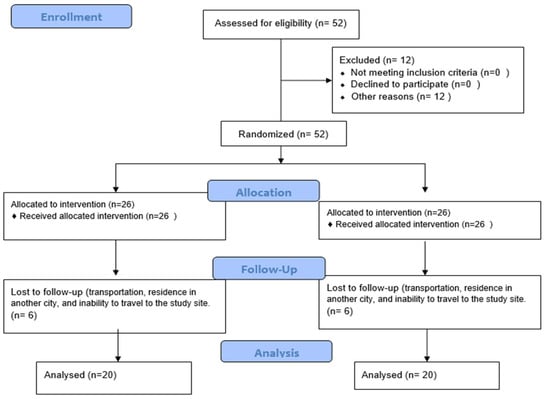
Figure 2.
Study flow chart.
In Table 1, the analysis of tissue hydration in the lower limbs (MoistureMeter), shows no statistically significant difference was observed between the Intervention group (IG) and Control group (CG) at any of the evaluated time points (pre- and post-operative), both in the limb where saphenectomy was performed (p = 0.387 and p = 0.285, respectively) and in the limbs without saphenectomy (p = 0.745 and p = 0.839).

Table 1.
Comparison of lower limb tissue hydration between the Intervention group (IG) and Control group (CG) at pre- and post-operative time points.
Similarly, the comparison of lower limb volume in Table 2 also showed no significant differences between the groups at any of the analyzed time points (p > 0.05).

Table 2.
Lower limb volume—comparisons between groups in the preoperative and postoperative periods.
Table 2 showed a significant increase in postoperative edema in both groups (Intervention Group: p = 0.003; Control Group: p = 0.001), with no significant differences between them in the preoperative (p = 0.387) and postoperative periods (p = 0.285). Regarding lower limb volumetry, as presented in Table 3, there was a trend toward a reduction in lower limb volume in the intervention group (IG) between the pre- and post-intervention periods (p = 0.069), although without statistical significance. In the remaining analyses, no significant intragroup differences were observed. Intergroup analyses also did not reveal relevant statistical differences between the pre- and post-intervention periods (p > 0.05).

Table 3.
Instantaneous sin elasticity between GT and GC group at preoperative and postoperative time points.
The analysis of instantaneous skin elasticity using the Elastimeter (Table 3) showed no significant differences between the Intervention group (IG) and Control group (CG) in the preoperative and postoperative periods, both in limbs that underwent saphenectomy (p = 0.117 and p = 0.387, respectively) and in those that did not (p = 0.417 and p = 0.262).
Table 4 presents the intergroup analysis of the variables ecchymosis, visual analog scale (VAS) for pain, and lower extremity functional scale (LEFS). Regarding the presence of postoperative ecchymosis in the limb subjected to saphenectomy, a significant difference was observed between groups (p = 002), with the intervention group (IG) showing a lower mean ecchymosis value (0.085) compared to the control group (CG)—0.174.

Table 4.
Comparison of the presence of ecchymosis, pain scale (VAS), and power extremity functional scale (LEFS) between the intervention (IG) and control (CG) groups in the postoperative period of saphenectomy.
For pain assessment, the IG also exhibited a lower mean score (1.25) than the CG (1.65), although this difference was not statistically significant (p = 0.203).
Finally, functional assessment of the lower limbs demonstrated a significant difference between groups (p = 0.006), with the IG achieving a higher mean functional score (66.20) compared to the CG (58.60), suggesting better functional recovery in patients who received taping intervention.
In the comparison between the IG and CG groups, as shown in Table 5, no significant difference was observed in pain intensity (VAS) between the groups (p = 0.203), although the IG group showed a slightly lower mean (1.25 ± 1.62) compared to the CG group (1.65 ± 1.35). On the other hand, lower extremity functionality, as measured by the Lower Extremity Functional Scale (LEFS), was significantly higher in the IG group (66.20 ± 18.64) than in the CG group (58.60 ± 11.82), with p = 0.006.

Table 5.
Comparison between IG and CG groups on VAS and LEFS scales in the postoperative period.
4. Discussion
This study aimed to evaluate the effect of taping on the recovery of lower limbs following unilateral saphenectomy. Studies have indicated that taping may assist in the reorganization of tissue pressures and improvement of lymphatic circulation, thereby supporting the management of postoperative complications [8,22,23,24,25]. However, its specific effects in the postoperative period of saphenectomy are still not well established.
No significant differences were observed between the groups undergoing unilateral saphenectomy in terms of edema control. This finding is likely due to the fact that both groups received standard compression therapy, which is widely recognized for its efficacy in managing postoperative edema [26,27]. Unlike compression stockings, taping primarily exerts elastic traction forces rather than circumferential pressure or direct compression.
The absence of significant differences between groups regarding edema control with the use of elastic adhesive bandaging was an expected finding, given the well-established evidence supporting the superiority of conventional compression therapy. Compression garments exert continuous circumferential pressure, which facilitates venous return, reduces capillary filtration, and promotes lymphatic drainage, mechanisms widely documented in the literature as effective in managing postoperative edema [28]. A clinical trial [29] comparing elastic adhesive bandaging with compression stockings in patients with chronic venous disease demonstrated that compression was significantly more effective in reducing edema, whereas taping showed more modest effects. Furthermore, a systematic review on the use of taping for edema control found that studies reporting positive outcomes are few, methodologically weak, and present notable limitations.
Although elastic adhesive bandaging is often perceived as a supportive intervention for edema control due to its elastic traction, its mechanism of action differs substantially from that of compression stockings [11]. Unlike the latter, bandaging does not provide uniform circumferential pressure and instead relies on localized tension, which may be insufficient to counteract the hemodynamic forces driving edema formation, particularly in the acute postoperative phase
The analysis of instantaneous skin elasticity, measured by the Elastimeter, also did not reveal significant differences between the intervention group (IG) and the control group (CG), either in the operated or non-operated limbs, across the pre- and postoperative periods. However, although statistical results did not reach the conventional significance threshold (p < 0.05), the p-value (0.052) suggests a trend toward significance that warrants further investigation. A significant difference was observed after seven days (p = 0.012).
The relatively small sample size (20 participants per group) may have limited the ability to detect moderate effects, as suggested by near-significant p-values like 0.052 for skin elasticity. This raises the possibility of a type II error, underscoring the need for future studies with larger cohorts to confirm the clinical benefits of taping after saphenectomy.
The presence of edema seven days after saphenectomy remains a common and clinically relevant occurrence. Even after the initial recovery period, interstitial fluid accumulation may persist due to lymphatic injury, transient venous dysfunction, and local inflammatory responses triggered by surgery [30]. This edema, even when subclinical, can alter tissue biomechanics by increasing interstitial volume and compromising the integrity of the extracellular matrix (ECM), thereby reducing its density and elasticity [31].
It is also important to consider additional hypotheses, such as the influence of individual factors like pre-existing vascular conditions. Chronic venous insufficiency is one of the leading causes of lower limb edema, resulting from increased capillary hydrostatic pressure and vascular permeability, which facilitate fluid buildup in the interstitial space. The severity of edema may vary according to individual clinical profiles, with venous hypertension being a key determinant [32,33].
In the present study, a significant reduction in ecchymosis was observed seven days after surgery, consistent with previous findings in other surgical contexts that reported positive outcomes related to ecchymosis modulation through taping [34]. These findings reinforce the potential of taping in the reabsorption of blood extravasation, even though its effects appear more peripheral than central in the affected area, corroborating the clinical trial results.
Although this study did not show statistically significant results regarding pain reduction, Aguillar-Ferrandiz et al. [14] suggested that taping may exert a placebo effect on pain. Therefore, taping is considered a promising therapeutic strategy in postoperative rehabilitation, particularly for pain relief and improved functionality both observed in the current study.
The improvements in LEFS scores and subcutaneous hemorrhage suggest clinically meaningful effects of taping. The LEFS changes approach the established MCID of nine points [20], and prior studies support taping’s role in reducing postoperative edema and ecchymosis [8,35].
Another study also reported reductions in pain and increases in knee flexion range in patients undergoing total knee arthroplasty, although the evidence quality remains low [36]. A similar effect was seen in post-thoracotomy patients [37], where taping significantly reduced pain, improved respiratory function, and decreased analgesic consumption compared to the control group. It was also effective in reducing pain and enhancing physical tolerance in postoperative laparoscopic abdominal surgery, further supporting its role as an adjunct in functional recovery. The timing of the postoperative period may also influence the outcomes of this study. Significant improvements in ecchymosis, edema, and pain were observed in liposuction patients at 7, 14, and 21 days postoperatively [8].
The findings of this study are limited to the acute phase of the inflammatory and edematous process, which prevents assessment of tissue response progression in later repair stages, suggesting the need for further research.
Evaluating therapeutic effects within the first seven days after saphenectomy carries strong clinical relevance, as this period marks the peak of the acute inflammatory response and postoperative edema formation. During this window, hemodynamic changes, increased vascular permeability, and interstitial fluid accumulation can directly affect limb mobility and raise the risk of secondary complications such as wound dehiscence and infection. Investigating interventions capable of modulating this process early on is therefore strategically valuable not only to accelerate functional recovery but also to reduce postoperative care costs. Further studies are needed to evaluate the progression of effects during later stages of tissue repair, as well as to investigate how comorbidities and age-related physiological differences may influence the effectiveness of taping in postoperative recovery.
A limitation of this study was the inability to blind participants and therapists due to the nature of the intervention, which may have affected subjective outcomes such as pain. To minimize this bias, we employed concealed allocation through randomization and standardized procedures, along with validated instruments for outcome assessment.
5. Conclusions
The study demonstrated significant effects of taping following saphenectomy, including reduced ecchymosis and improved skin elasticity and lower limb functionality. However, no statistically significant result was observed in relation to edema control.
Author Contributions
Conceptualization, E.C.d.O.G. and R.M.G.; methodology, E.C.d.O.G. and R.M.G., software, R.M.G.; validation, E.C.d.O.G. and R.M.G.; formal analysis, R.M.G. and C.C.Z.; investigation, R.M.G.; resources, E.C.d.O.G.; data curation, R.M.G. and C.C.Z.; writing—original draft preparation, R.M.G.; writing—review and editing, R.M.G., E.C.d.O.G. and A.N.; visualization, R.M.G., E.C.d.O.G., E.H.S.Z., C.C.Z. and A.N.; supervision, E.C.d.O.G. All authors have read and agreed to the published version of the manuscript.
Funding
This study was financed in part by the Coordination for the Improvement of Higher Education Personnel (CAPES), Brazil–Finance Code 001.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee Research Ethics Committee of the University Hospital, Ribeirão Preto Medical School–University of São Paulo (CAAE: 59928122.2.0000.5440) on 22 August 2022.
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest. Furthermore, this study has not been submitted to any other journal.
References
- Mik, S.M.L.; Stubenrouch, F.E.; Dink, A.; Legemate, D.A.; Balm, R.; Ubbink, D.T. Treatment of varicose veins, international consensus on which major complications to discuss with the patient: A Delphi study. Phlebology 2019, 34, 201–207. [Google Scholar] [CrossRef]
- Da Silva, E.M.; Hochman, B.; Ferreira, L.M. Perioperative corticosteroids for preventing complications following facial plastic surgery. Cochrane Database Syst. Rev. 2014, 6, CD009697. [Google Scholar] [CrossRef] [PubMed]
- Mariani, F.; Marone, E.M.; Gasbarro, G.; Bucalossi, M.; Spelta, S.; Amsler, F.; Agnati, M.; Chiesa, R. Multicenter randomized trial comparing compression with elastic stocking versus bandage after surgery for varicose veins. J. Vasc. Surg. 2011, 53, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.Y.; Lee, H.R.; Lee, D.C. The use of elastic adhesive tape to promote lymphatic flow in the rabbit hind leg. Yonsei Med. J. 2003, 44, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Ristow, O.; Pautke, C.; Kehl, V.; Koerdt, S.; Hahnefeld, L.; Hohlweg-Majert, B. Kinesiologic taping reduces morbidity after oral and maxillofacial surgery: A pooled analysis. Physiother. Theory Pract. 2014, 30, 390–398. [Google Scholar] [CrossRef]
- Beidler, S.K.; Douillet, C.D.; Berndt, D.F.; Keagy, B.A.; Rich, P.B.; Marston, W.A. Inflammatory cytokine levels in chronic venous insufficiency ulcer tissue before and after compression therapy. J. Vasc. Surg. 2009, 49, 1013–1020. [Google Scholar] [CrossRef]
- Frangogiannis, N.G. The inflammatory response in myocardial injury, repair, and remodeling. Nat. Rev. Cardiol. 2017, 14, 254–272. [Google Scholar] [CrossRef]
- Zingaretti, N.; Albanese, R.; Pisano, G.; Isola, M.; Giusti, A.; De Martino, M.; De Francesco, F.; Riccio, M.; Parodi, P.C. Evaluation of Kinesio Taping for Edema, Ecchymosis, and Pain After Liposuction: A Prospective Pilot Study. Aesthet. Surg. J. 2023, 43, NP787–NP796. [Google Scholar] [CrossRef]
- Jarón, A.; Jedliński, M.; Grzywacz, E.; Mazur, M.; Trybek, G. Kinesiology Taping as an Innovative Measure against Post-Operative Complications after Third Molar Extraction—Systematic Review. J. Clin. Med. 2020, 9, 3988. [Google Scholar] [CrossRef]
- Tatli, U.; Benlidayi, I.C.; Salimov, F.; Guzel, R. Effectiveness of kinesio taping on postoperative morbidity after impacted mandibular third molar surgery: A prospective, randomized, placebo-controlled clinical study. J. Appl. Oral Sci. 2020, 28, e20200159. [Google Scholar] [CrossRef]
- Hörmann, J.; Vach, W.; Jakob, M.; Seghers, S.; Saxer, F. Kinesiotaping for postoperative oedema—What is the evidence? A systematic review. BMC Sports Sci. Med. Rehabil. 2020, 12, 14. [Google Scholar] [CrossRef]
- Pop, T.B.; Karczmarek-Borowska, B.; Tymczak, M.; Hałas, I.; Banaś, J. The influence of Kinesiology Taping on the reduction of lymphoedema among women after mastectomy-preliminary study. Contemp. Oncol. 2014, 18, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Torres-Lacomba, M.; Navarro-Brazález, B.; Prieto-Gómez, V.; Ferrandez, J.C.; Bouchet, J.Y.; Romay-Barrero, H. Effectiveness of four types of bandages and kinesio-tape for treating breast-cancer-related lymphoedema: A randomized, single-blind, clinical trial. Clin. Rehabil. 2020, 34, 1230–1241. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Ferrándiz, M.E.; Castro-Sánchez, A.M.; Matarán-Peñarrocha, G.A.; Guisado-Barrilao, R.; García-Ríos, M.C.; Moreno-Lorenzo, C.A. A randomized controlled trial of a mixed Kinesio taping–compression technique on venous symptoms, pain, peripheral venous flow, clinical severity and overall health status in postmenopausal women with chronic venous insufficiency. Clin. Rehabil. 2014, 28, 69–81. [Google Scholar] [CrossRef] [PubMed]
- Miettinen, M.; Mönkkönen, J.; Lahtinen, M.R.; Nuutinen, J.; Lahtinen, T. Measurement of oedema in irritant-exposed skin by a dielectric technique. Skin Res. Technol. 2006, 12, 235–240. [Google Scholar]
- Alanen, E.; Nuutinen, J.; Nicklén, K.; Lahtinen, T.; Mönkkönen, J. Measurement of hydration in the stratum corneum with the MoistureMeter and comparison with the Corneometer. Skin Res. Technol. 2004, 10, 32–37. [Google Scholar] [CrossRef]
- Bertelli, D.F.; de Oliveira, P.; Gimenes, A.S.; Moreno, M.A. Postural drainage and manual lymphatic drainage for lower limb edema in women with morbid obesity after bariatric surgery: A randomized controlled trial. Am. J. Phys. Med. Rehabil. 2013, 92, 697–703. [Google Scholar] [CrossRef]
- Brorson, H.; Svensson, B.; Ohlin, K. Volume measurements and follow-up. In Lymphedema: Presentation, Diagnosis, and Treatment; Greene, A.K., Slavin, S.A., Brorson, H., Eds.; Springer: Cham, Switzerland, 2015; pp. 115–122. [Google Scholar] [CrossRef]
- Heller, G.; Manuguerra, M.; Chow, R. How to analyze the Visual Analogue Scale: Myths, truths and clinical relevance. Scand. J. Pain 2016, 13, 67–75. [Google Scholar] [CrossRef]
- Binkley, J.M.; Stratford, P.W.; Lott, S.A.; Riddle, D.L. The Lower Extremity Functional Scale (LEFS): Scale development, measurement properties, and clinical application. Phys. Ther. 1999, 79, 371–383. [Google Scholar] [CrossRef]
- Pereira, L.M.; Dias, J.M.; Mazuquin, B.F.; Castanhas, L.G.; Menacho, M.O.; Cardoso, J.R. Translation, cross-cultural adaptation and analysis of the psychometric properties of the lower extremity functional scale (LEFS): LEFS-BRAZIL. Braz. J. Phys. Ther. 2013, 17, 272–280. [Google Scholar] [CrossRef]
- Rezende, V.J.; Carvalho, L.C.; Yanagihara, G.; Rocha, C.B.J.; Maia, P.R.; Marino, L.d.S.; Iunes, D.H. Effect of kinesio-taping on the acute phase of the post-operative reconstruction of the anterior cruciate ligament: A randomized controlled trial. J. Bodyw. Mov. Ther. 2023, 35, 320–325. [Google Scholar] [CrossRef]
- Labianca, L.; Andreozzi, V.; Princi, G.; Princi, A.A.; Calderaro, C.; Guzzini, M.; Ferretti, A. The effectiveness of Kinesio Taping in improving pain and edema during early rehabilitation after Anterior Cruciate Ligament Reconstruction: A prospective, randomized, controlled study. Acta Biomed. 2022, 92, e2021336. [Google Scholar] [CrossRef]
- Cakmak, M.; Cigdem-Karacay, B. The effect of kinesio taping on edema, pain, and functionality after total knee arthroplasty: A randomised sham-controlled double blinded clinical study. J. Orthop. Sci. 2023, 29, 983–989. [Google Scholar] [CrossRef] [PubMed]
- Sobiech, M.; Czępińska, A.; Zieliński, G.; Zawadka, M.; Gawda, P. Does application of lymphatic drainage with kinesiology taping have any effect on the extent of edema and range of motion in early postoperative recovery following primary endoprosthetics of the knee joint? J. Clin. Med. 2022, 11, 3456. [Google Scholar] [CrossRef] [PubMed]
- Belczak, C.E.Q.; Godoy, J.M.P.; Ramos, R.N.; Belczak, S.Q.; Caffaro, R.A. Is the wearing of elastic stockings for half a day as effective as wearing them for the entire day? Phlebology 2009, 24, 21–25. [Google Scholar] [CrossRef]
- Gloviczki, P.; Comerota, A.J.; Dalsing, M.C.; Eklof, B.G.; Gillespie, D.L.; Gloviczki, M.L.; Lohr, J.M.; McLafferty, R.B.; Meissner, M.H.; Murad, M.H.; et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J. Vasc. Surg. 2011, 53, 2S–48S. [Google Scholar] [CrossRef]
- De Moraes Silva, M.A.; Nelson, A.; Bell-Syer, S.E.; Jesus-Silva, S.G.; Miranda, F., Jr. Compression for preventing recurrence of venous ulcers. Cochrane Database Syst. Rev. 2024, 3, CD002303. [Google Scholar] [CrossRef]
- Baha, N.; Ozyilmaz, S.; Aygutalp, N.; Demir, R.; Baltaci, G.; Yigit, Z. Effects of Kinesio Taping and compression stockings on pain, edema, functional capacity and quality of life in patients with chronic venous disease: A randomized controlled trial. Clin. Rehabil. 2020, 34, 783–793. [Google Scholar] [CrossRef]
- Terada, Y.; Fukuda, S.; Tohda, E.; Kigawa, I.; Wanibuchi, Y.; Mitsui, T. Venous function and delayed leg swelling following saphenectomy in coronary artery bypass grafting. Jpn. J. Thorac. Cardiovasc. Surg. 1999, 47, 559–562. [Google Scholar] [CrossRef]
- Subramani, R.; Izquierdo-Alvarez, A.; Bhattacharya, P.; Meerts, M.; Moldenaers, P.; Ramon, H.; Van Oosterwyck, H. The influence of swelling on elastic properties of polyacrylamide hydrogels. Front. Mater. 2020, 7, 212. [Google Scholar] [CrossRef]
- Santa Cruz, M.; Singh, N.; Poltiyelova, E.; Marks, N.; Ascher, E.; Hingorani, A. Seasonal variation in swelling of lower extremity edema in patients with chronic venous insufficiency. J. Vasc. Surg. Venous Lymphat. Disord. 2023, 11, 498–501. [Google Scholar] [CrossRef]
- Ortega, M.A.; Fraile-Martínez, O.; García-Montero, C.; Álvarez-Mon, M.A.; Chaowen, C.; Ruiz-Grande, F.; Pekarek, L.; Monserrat, J.; Asúnsolo, A.; García-Honduvilla, N.; et al. Understanding Chronic Venous Disease: A Critical Overview of Its Pathophysiology and Medical Management. J. Clin. Med. 2021, 10, 3239. [Google Scholar] [CrossRef]
- Vercelli, S.; Colombo, C.; Tolosa, F.; Moriondo, A.; Bravini, E.; Ferriero, G.; Francesco, S. The effects of kinesio taping on the color intensity of superficial skin hematomas: A pilot study. Phys. Ther. Sport 2017, 25, 24–29. [Google Scholar] [CrossRef]
- Bruno, A.; Vigliano, T.; Foti, R. The role of taping in early recovery after abdominoplasty: A comprehensive review and proposal of a standardized protocol. Aesthetic Plast. Surg. 2025, 49, 112–120. [Google Scholar] [CrossRef]
- Ickert, E.C.; Griswold, D.; Ross, O.; Dudash, S.; Duchon, C.; Learman, K. Effects of kinesiotaping during early post-operative rehabilitation in individuals who underwent a total knee arthroplasty: A systematic review and meta-analysis of randomized control trials. Clin. Rehabil. 2024, 38, 345–356. [Google Scholar] [CrossRef]
- Aksu, N.T.; Erdoğan, M.; Erdoğan, A. The effect of kinesio taping on pain, respiratory function, and muscle strength after thoracotomy. Turk. Gogus Kalp Damar Cerrahisi Derg. 2023, 31, 507–516. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).