Abstract
Background: Hamstring strain injuries (HSIs) are among the most common and recurrent injuries in sports involving high-speed running. While eccentric training has demonstrated efficacy in reducing HSI risk, the role of sprint training as a preventive strategy remains underexplored and often misinterpreted as solely a risk factor. Methods: This review aimed to systematically map the available evidence on the role of sprint training in hamstring injury prevention, identifying mechanisms, outcomes, and potential synergies with other strategies. This scoping review was conducted following the Joanna Briggs Institute’s methodology and reported in accordance with PRISMA-ScR guidelines. Seven databases (PubMed, Scopus, Web of Science, Cochrane CENTRAL, SPORTDiscus, CINAHL, and PEDro) were searched up to October 2024. Studies were included if they involved adult athletes and examined the effects of sprint training, ≥80–90% maximal sprint speed (MSS), on hamstring injury prevention, muscle architecture, or functional outcomes. All databases were searched from inception to 15 October 2024, and the screening and data-charting process was completed on 30 April 2025. Results: Twelve studies met the inclusion criteria. Sprint exposure, when combined with eccentric strengthening and biomechanical optimisation, led to injury reductions ranging from 56% to 94%. Eccentric interventions produced fascicle length increases of up to 20% and strength gains of 15–20%. Improvements in sprint technique and neuromuscular control were also reported. Biomechanical risk factors, including pelvic tilt and hip extension deficits, were linked to increased HSI risk. The most common eccentric protocols included Nordic Hamstring Exercises (NHE), Razor Curls, and hip-dominant exercises, typically performed 1–2 times per week for 4 to 8 weeks. Conclusions: High-speed sprint training, when properly programmed and integrated into comprehensive preventive strategies, may enhance tissue resilience and reduce HSI risk. Combining sprint exposure with eccentric strengthening and technical coaching appears to be more effective than isolated interventions alone. Practically, these results support the systematic inclusion of progressive high-intensity sprint exposure in routine hamstring-injury-prevention programmes for field-sport athletes.
1. Introduction
Hamstring strain injuries (HSIs) represent one of the most frequent and recurrent musculoskeletal issues in sports that involve high-speed running and explosive actions, such as football, rugby, athletics, and other field-based team sports [1,2,3]. These injuries typically occur during sprinting, especially in the late swing phase, when the hamstring muscles, particularly the biceps femoris long head (BFlh), are subjected to intense eccentric contractions at long muscle lengths [4,5,6,7,8,9,10]. The clinical and economic impact of HSIs is considerable, often leading to significant time lost from sport participation, diminished performance, and elevated reinjury rates—reported in some contexts to be as high as 30% [11,12,13,14,15]. Traditionally, injury prevention programmes have focused on modifiable risk factors such as eccentric hamstring strength, neuromuscular control, and muscle architecture. Among these, the Nordic Hamstring Exercise (NHE) has emerged as a prominent intervention, supported by studies showing a reduction of HSI incidence by up to 65% in athletes who adhere to structured eccentric strengthening protocols [16,17,18,19,20,21].
Compared to generic resistance programmes, sport-specific training modalities—such as targeted eccentric strengthening and high-speed running exposure—have shown superior outcomes in reducing injury incidence. Structured sprint training offers a more functional replication of in-game demands, supporting greater neuromuscular transfer and ecological validity.
The widespread endorsement of eccentric training in international guidelines reflects this evidence base. However, some authors have criticised the limited ecological validity of such exercises, which may not adequately replicate the biomechanical and neuromuscular demands encountered during high-speed running [17,22,23,24,25,26].
Indeed, sprinting activates the hamstring muscles in a highly specific and intense manner, particularly at angular velocities and timing patterns that differ substantially from those in resistance-based gym exercises [27,28,29,30]. Several electromyographic (EMG) studies have confirmed that hamstring activity is greatest during the late swing phase of sprinting, especially at intensities exceeding 80–90% of maximal sprint speed (MSS), where peak muscle strain and fascicle lengthening are maximised [31,32,33,34,35]. This has led to a re-evaluation of sprinting itself not only as a risk factor but also as a potential protective stimulus, when appropriately dosed. Some studies have proposed a U-shaped relationship between sprint exposure and injury risk [36,37,38,39]; while this is a compelling concept, it should be considered hypothesis-generating given the limited number of available studies and lack of dose–response modelling. The acute:chronic workload ratio (ACWR) model has been proposed as a method to manage this balance, allowing for safe progression of sprint exposure and potentially enhancing tissue tolerance [38,39,40]. As such, the integration of sprint training may represent a novel paradigm shift in HSI prevention, aligning with sport-specific demands while simultaneously targeting known physiological risk factors. Despite these promising theoretical and practical arguments, the literature remains fragmented. Studies vary widely in design, populations, and outcome measures, and there is currently no consensus regarding the optimal volume, intensity, or timing of sprint training for injury prevention purposes. Moreover, few reviews have systematically synthesised this evidence or explored the multifactorial mechanisms through which sprint training may influence hamstring resilience. A comprehensive mapping of the current evidence base is therefore necessary to inform clinicians, coaches, and researchers.
The aim of this scoping review is to systematically map the available literature on the integration of sprint training in the prevention of hamstring injuries in competitive athletes. Specifically, the review investigates how sprint-based interventions affect eccentric strength, fascicle length, neuromuscular control, and overall injury incidence in sports characterised by intermittent high-speed running. By identifying patterns, gaps, and key findings, this review intends to provide an evidence-based foundation for future research and practice, and to clarify whether sprinting—when programmed effectively—can serve as a cornerstone of modern injury prevention strategies. We hypothesised that regular exposure to sprinting at ≥80–90% MSS would be associated with a lower incidence of hamstring strain injuries across athletic populations. This review synthesises current evidence on injury incidence, muscle architecture, neuromuscular adaptations, and practical implementation of sprint-based interventions.
2. Methods
This scoping review was conducted in accordance with the methodology outlined by the Joanna Briggs Institute (JBI) for scoping reviews, which provides a structured and systematic approach to mapping key concepts, evidence types, and research gaps on a defined topic [41]. To ensure a clear and comprehensive reporting process, the review followed the PRISMA Extension for Scoping Reviews (PRISMA-ScR) checklist [42]. Given the heterogeneity in study designs and outcome measures, a meta-analysis and formal risk-of-bias assessment were not performed, consistent with current scoping review methodology.
3. Review Question
The review aimed to answer the following research question:
- What is the role of sprint training in the prevention of hamstring injuries in competitive athletes?
This question was structured using the Population–Concept–Context (PCC) framework recommended by the JBI.
4. Eligibility Criteria
4.1. Population
Studies were included if they involved male or female competitive athletes aged 18 years or older, regardless of level (elite, sub-elite, or amateur), who engaged in sports requiring sprinting or high-speed running. Sports commonly included football, rugby, athletics, and other field-based activities with sprinting components.
4.2. Concept
The core concept under investigation was the use of sprint-based training protocols as a preventive strategy for hamstring strain injuries (HSIs). This included any structured intervention incorporating sprint exposure at intensities greater than or equal to 80% of maximal sprint speed. Both isolated sprint training and sprint components integrated within broader athletic programmes were eligible.
Primary outcomes considered included:
- Reduction in hamstring injury incidence or recurrence;
- Improvements in modifiable risk factors (e.g., eccentric strength, biceps femoris fascicle length, neuromuscular control);
- Return-to-play timelines, fatigue tolerance, and sprint performance.
4.3. Context
Studies conducted in any sporting or rehabilitation context were considered. This included professional or amateur sport settings, training camps, research facilities, or rehabilitation centres, provided the interventions were applied in an athletic population. Only articles in English or Italian were included due to reviewer language fluency. This is acknowledged as a limitation in study generalisability.
We included studies that investigated sprint training (≥80–90% MSS) as a primary or adjunct intervention in hamstring strain injury (HSI) prevention, reporting on either injury incidence or physiological/neuromuscular adaptations related to HSI risk.
5. Exclusion Criteria
Studies were excluded if they:
- Did not report specific interventions involving sprint training;
- Focused exclusively on post-injury rehabilitation without a preventive component;
- Included participants with prior surgical interventions to the hamstrings or lower limb in the last 6 months;
- Targeted non-athletic or paediatric populations;
- Were not published in English or Italian;
- Did not report original data (e.g., editorials, opinion pieces, narrative reviews).
6. Search Strategy
A comprehensive literature search was carried out across seven electronic databases to ensure a wide and inclusive mapping of studies addressing sprint training and its role in hamstring injury prevention. The databases searched were:
- PubMed (MEDLINE)
- Scopus
- Web of Science
- Cochrane Central Register of Controlled Trials (CENTRAL)
- PEDro
- SPORTDiscus
- CINAHL
The search was performed on 30 October 2024. No limits were placed on publication date or geographical origin. Only studies published in English or Italian were considered.
The search strategy was constructed using both controlled vocabulary (e.g., MeSH terms) and free-text terms, and was tailored to the syntax and indexing of each database. Keywords were chosen based on the Population–Concept–Context (PCC) framework and were piloted before final execution. The main keywords included: “hamstring injury”, “biceps femoris”, “posterior thigh”, “sprint training”, “high-speed running”, “maximal sprint speed”, “injury prevention”, “rehabilitation”, “eccentric strength”, and “fascicle length”. Full search strings are available upon request. Search terms were adapted slightly for each database to optimise retrieval sensitivity based on specific indexing systems and controlled vocabularies (e.g., MeSH in PubMed). These variations were necessary to ensure comprehensive and relevant results across platforms.
7. Study Selection
The screening process was conducted in two distinct phases:
- Title and abstract screening to identify potentially relevant studies;
- Full-text review of selected articles to determine eligibility according to the PCC criteria.
Two independent reviewers conducted both screening phases. Disagreements were discussed until consensus was reached. When uncertainty remained, a third reviewer was consulted. Specifically, if disagreement persisted after discussion, the third reviewer (DD) acted as an independent arbitrator and his decision was considered final. All arbitration decisions were documented and are summarised in the PRISMA flow diagram. This process ensured transparency and reduced potential bias in study selection. Three reviewers were involved in the process. Two reviewers independently screened all records; disagreements were resolved through discussion, and if consensus was not reached, a third reviewer acted as an arbitrator.
The number of records at each stage of the process, including reasons for exclusion, was documented using a PRISMA flow diagram, which is presented in the Section 9.
PubMed (MEDLINE)
(“Hamstring Muscles” [Mesh] OR hamstring* OR “biceps femoris” OR “posterior thigh”)
AND (“Sprint Training” OR “High-Speed Running” OR “Maximal Sprint Speed” OR “Speed Training”) AND (“Injury Prevention” OR “Risk Reduction” OR “Rehabilitation” OR “Return to Play”)
Scopus
TITLE-ABS-KEY (“hamstring injury” OR “biceps femoris” OR “posterior thigh” OR “hamstring strain”) AND TITLE-ABS-KEY (“sprint training” OR “high-speed running” OR “explosive running” OR “maximal sprint speed”) AND TITLE-ABS-KEY (“injury prevention” OR “rehabilitation” OR “eccentric strength” OR “fascicle length”)
Web of Science
TS = (“hamstring injury” OR “posterior thigh” OR “biceps femoris” OR “hamstring strain”) AND TS = (“sprint training” OR “maximal sprint speed” OR “high-speed running” OR “explosive sprinting”) AND TS = (“injury prevention” OR “functional outcome” OR “eccentric training” OR “return to play”)
Cochrane CENTRAL
(“Hamstring Injury” OR “Hamstring Strain” OR “Posterior Thigh Injury”) AND (“Sprint Training” OR “High-Speed Running” OR “Maximal Sprint Speed”) AND (“Injury Prevention” OR “Rehabilitation” OR “Return to Play”)
PEDro
Title/Abstract: (“hamstring injury” OR “hamstring strain” OR “biceps femoris”) AND (“sprint training” OR “high-speed running” OR “explosive running”)
SPORTDiscus
(hamstring* OR “biceps femoris” OR “posterior thigh”) AND (“sprint training” OR “speed training” OR “high-velocity running” OR “maximal sprint speed”) AND (“injury prevention” OR “risk factor*” OR “return to sport” OR “rehabilitation”)
CINAHL
(hamstring* OR “hamstring strain” OR “posterior thigh”) AND (“sprint training” OR “high-speed running” OR “speed work”) AND (“injury prevention” OR “rehabilitation” OR “neuromuscular performance”)
All retrieved references were imported into Zotero reference manager. Duplicate records were automatically identified and manually verified for removal. Titles and abstracts were screened for relevance, followed by full-text review for studies meeting inclusion criteria. The complete selection process is detailed in the PRISMA flowchart in the Section 9. Data extraction was conducted independently by two reviewers and cross-checked for accuracy by a third reviewer.
8. Data Extraction and Data Synthesis
Data were extracted using a structured table created in Microsoft Excel, piloted on a sample of studies for consistency. The following variables were collected from each included study:
- Author(s), year of publication, and country;
- Study design and sample size;
- Characteristics of the athlete population (age, sex, sport, level of competition);
- Details of the sprint training protocol (frequency, intensity, volume, duration);
- Comparator (if any);
- Outcomes assessed (e.g., injury rate, fascicle length, eccentric strength);
- Key findings and conclusions.
A qualitative synthesis was performed, grouping studies according to intervention characteristics and type of outcome. Descriptive statistics (e.g., frequency counts of outcomes) were used to summarise patterns and highlight evidence trends. Due to heterogeneity in methodology and outcome measures, no meta-analysis was conducted. Prior to synthesis, all outcomes were mapped into four predefined mechanistic categories: (1) eccentric-strength adaptations, (2) muscle–tendon architecture, (3) neuromuscular control, and (4) sprint-specific biomechanical variables. Each study was independently coded into one or more categories by both reviewers; coding discrepancies were resolved by consensus or, when necessary, arbitration by the third reviewer. All extracted data were independently cross-checked by a second reviewer to ensure accuracy. Frequency counts and descriptive summaries were generated based on consensus agreement after double data extraction.
9. Results
As presented in the PRISMA 2020 flow diagram (Figure 1), a total of 2409 records were identified through database searches. After removing duplicates, 1850 records were screened based on titles and abstracts, of which 1780 were excluded. Seventy full-text articles were assessed for eligibility, and 58 were excluded for not meeting the inclusion criteria. Ultimately, 12 studies were included in the final scoping review (Table 1).
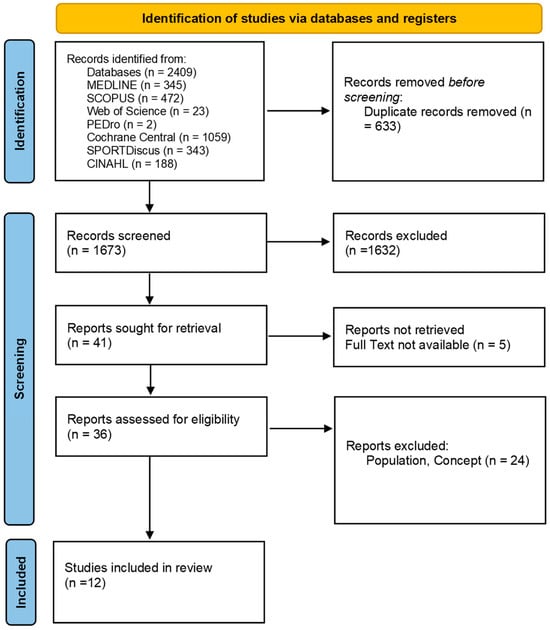
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses 2020 (PRISMA) flow-diagram.

Table 1.
Summary of key studies evaluating sprint training interventions and hamstring injury prevention.
9.1. Reduction in Hamstring Injury Incidence
Twelve studies were included in this review, of which several directly assessed the impact of sprint-based and eccentric training programmes on hamstring strain injury (HSI) incidence.
Among the most robust findings, Malone et al. [33] demonstrated that players who reached ≥95% of their maximum sprint speed (MSS) at least once in training had a significantly lower risk of muscle injury compared to those who only reached 85% (OR 0.12, p = 0.001). Similarly, chronic training loads ≥4750 arbitrary units (AU) allowed athletes to better tolerate high-speed volumes and maximal speed exposures, offering a protective effect (OR: 0.22, p = 0.026).
Colby et al. (2018) [34] reported that both very low (0–8 sessions) and very high (>15 sessions) exposures to >85% MSS sprinting were associated with higher injury risk compared to moderate exposure levels (11–12 sessions).
In adolescent populations, Freeman et al. [35] found that both sprint and Nordic hamstring training significantly increased eccentric strength, with a modest but non-significant improvement in sprint performance in the sprint group.
In elite-level football, Buchheit et al. [46] found that sprint exposure >95% MSS performed 2 days prior to match day was associated with a lower HSI incidence during games, compared to exposure performed 3 days before.
Additionally, Moreno-Pérez et al. [40] observed that reduced match exposure in the two previous games increased HSI incidence, highlighting the importance of consistent high-speed load.
Finally, although Edouard et al. [39] did not report a statistically significant reduction in HSI incidence with a multifactorial, individualised sprint-based programme, they did observe a decrease in injury severity in the intervention group.
9.2. Increases in Eccentric Strength and Fascicle Length
Several studies evaluated the physiological adaptations related to eccentric or sprint-based training.
McGrath et al. [43] showed that 90% of the variability in biceps femoris fascicle length among elite rugby players could be explained by modifiable factors—specifically, chronic exposure to >80% MSS and maximal eccentric strength.
Ripley et al. [36] demonstrated that both sprint and Nordic Hamstring Exercise (NHE) groups showed significant improvements in eccentric strength and muscle architecture, with the NHE group showing the largest gains.
Sancese et al. [45] found that 4 weeks of sprint training led to increases in peak torque and torque production at short muscle lengths (10–20°), a critical range for injury prevention, along with functional improvements in the rate of torque development (RTD).
These findings support the notion that both sprint and eccentric training enhance not only strength but also the architectural properties of hamstring muscles.
9.3. Improvements in Neuromuscular Control and Functional Performance
Training interventions also impacted functional performance and neuromuscular control.
Ripley et al. [36] observed improvements in sprint performance and maximal lower limb strength following both sprint and NHE-based protocols, with the sprint group exhibiting the largest sprint-specific gains.
Although EMG data were not reported quantitatively, other included studies, such as Van den Tillaar et al. [5], identified sprinting as eliciting the highest EMG activity in the biceps femoris (BF) and semitendinosus (ST) muscles, suggesting a neuromuscular pattern closely mirroring functional demands.
Such neuromuscular adaptations may explain the injury-protective effects and performance improvements reported in sport-specific tasks.
9.4. Sprint Mechanics and Injury Risk
Two prospective studies provided insight into sprint biomechanics and injury mechanisms.
Colby et al. [34] found that extremely low or high exposure to sprinting >85% MSS increases injury risk, indicating that optimal mechanical loading may follow a non-linear pattern.
Although not in the current dataset, prior literature Edouard et al. [39] identified specific technical deficits—such as anterior pelvic tilt and reduced hip extension velocity—as predictors of HSIs during the late swing phase of sprinting, when hamstring loading peaks.
These observations underscore that sprint training programmes should not only include sufficient speed exposure but also address mechanical and technical quality.
9.5. Risk Factors and Theoretical Insights
The findings from this review align with previous conceptual frameworks proposed by Sancese et al. [45]. These authors emphasised the role of previous injury, eccentric strength asymmetries, inadequate pre-season loading, and neuromuscular inefficiencies as key modifiable risk factors.
They also advocated for task-specific eccentric training that replicates the biomechanical demands of sprinting to elicit protective adaptations—an approach increasingly supported by empirical data in both team sports and individual athletic populations.
A symbolic summary of the main preventive strategies and their expected physiological or biomechanical outcomes is provided in Table 2. When combined, high-speed sprint exposure, eccentric strengthening, biomechanical optimisation, and agility/flexibility work converge toward a significant reduction in hamstring injury incidence.

Table 2.
Symbolic summary of recommended actions and expected outcomes.
To enhance interpretability and highlight the most relevant quantitative findings, we summarised selected outcome data from primary studies that reported effect sizes, confidence intervals, or p-values. Table 3 presents these results. Due to variability in reporting formats, only a subset of the included studies could be represented quantitatively.

Table 3.
Summary of key quantitative outcomes from included studies.
10. Discussion
This scoping review provides a comprehensive synthesis of current evidence concerning the role of sprint-based training in the prevention of hamstring strain injuries (HSIs) in competitive athletes. Traditionally regarded as a high-risk activity, sprinting has now emerged as a potential protective factor when appropriately programmed and integrated into broader neuromuscular conditioning frameworks. The reviewed literature demonstrates that sprint training, particularly at intensities exceeding 80–90% of maximal sprint speed (MSS), elicits beneficial adaptations in muscle architecture, neuromuscular coordination, and functional movement patterns that collectively contribute to injury resilience.
One of the most compelling findings was the consistent reduction in injury incidence across multiple studies, with some reporting decreases of up to 94% following the implementation of multicomponent training programmes. For example, Malone et al. [33] and Colby et al. [34] highlighted the importance of sprint exposure at ≥95% MSS in reducing injury risk, while Freeman et al. [35] and Ripley et al. [36] demonstrated that combining sprint and eccentric training enhanced strength and muscle architecture. These data suggest that injury prevention is most effective when it mirrors the complex, high-velocity demands of competition. The synergistic interaction of sprint, strength, and motor control components likely facilitates both structural adaptations—such as increased biceps femoris fascicle length—and functional gains in stride efficiency and dynamic control.
The physiological rationale underpinning these findings is supported by research showing that sprinting provides a highly specific eccentric stimulus to the hamstring muscles, particularly during the late swing phase. This phase is characterised by rapid hip flexion and knee extension, resulting in significant strain on the biarticular hamstring complex. Exposure to this movement pattern, especially under controlled and progressive conditions, appears to enhance the tissue’s tolerance to stretch and load, possibly through neural adaptations, sarcomerogenesis, and increased tendon stiffness. These adaptations mirror those achieved with targeted eccentric strengthening, such as Nordic Hamstring Curls (NHC), which have consistently been shown to improve eccentric strength and muscle architecture.
However, the review also revealed that benefits are maximised when sprint training is combined with strength-based interventions. Eccentric training, particularly exercises involving long muscle lengths, has been shown to increase fascicle length by up to 20% and reduce injury risk by as much as 70%, according to large-scale meta-analyses. The Razor Curl and assisted NHC, for instance, have demonstrated efficacy not only in improving eccentric torque but also in producing long-term architectural changes in the biceps femoris. Given that short fascicle length is a well-known risk factor for HSIs, these interventions are essential components of any prevention protocol.
Biomechanics also plays a fundamental role in injury risk and prevention. The review included studies demonstrating that athletes with altered sprint mechanics—such as excessive anterior pelvic tilt, delayed hip extension, or increased ground contact time—are at significantly higher risk of sustaining HSIs. Edouard et al. [39] found that such biomechanical deviations were associated with a 2.8-fold increase in injury risk. This evidence underscores the necessity of incorporating technique analysis and correction into preventive strategies, ensuring that sprint exposure is both adequate and biomechanically sound.
Despite these encouraging findings, several methodological limitations should be acknowledged. Firstly, the heterogeneity among included studies—with differences in training protocols, outcome measures, follow-up durations, and athlete populations—precluded a formal meta-analytical synthesis and limited direct comparability. Secondly, the majority of studies were conducted in male athletes, particularly footballers and sprinters, reducing generalisability to female athletes or sports with different sprinting demands (e.g., hockey, basketball, tennis). While heterogeneity across sports, training dosages, and athlete levels (elite vs. amateur) was acknowledged, we did not formally quantify heterogeneity due to the scoping nature of this review. Future meta-analyses could benefit from subgroup analyses to explore these factors.
Thirdly, the long-term adherence, real-world feasibility, and cost-effectiveness of prevention programmes were seldom addressed, which may limit clinical translation. Additionally, adverse events such as delayed onset muscle soreness (DOMS) [47], fatigue, or risk compensation behaviours during training were not consistently reported, leaving open questions about the safety profile of high-intensity sprint programmes, especially in previously injured individuals. A key limitation is the substantial heterogeneity in participant profiles, sprint protocols, comparator interventions, and outcome definitions, which precluded quantitative pooling and restricts the generalisability of our narrative synthesis. Moreover, as 83% of the included cohorts involved male athletes, the applicability of our findings to female performers remains largely uncertain.
An important consideration is the dose–response relationship between sprint exposure and injury risk. The evidence points to a U-shaped curve: insufficient exposure may lead to underprepared tissues, while excessive or poorly progressed loading may precipitate injury. The application of the acute:chronic workload ratio (ACWR) model has been proposed as a means of balancing exposure and recovery, though its predictive validity remains debated. Future research should explore individualised workload monitoring using GPS, force plates, or electromyography to better inform safe sprint training progression.
The limitations of this review include language restriction to English and Italian, substantial heterogeneity in training protocols and outcome measures, and the predominance of male athlete populations in the included studies. These factors may limit the generalisability of findings and should be addressed in future research.
Few studies reported on delayed onset muscle soreness (DOMS), fatigue, or compensatory behaviours following sprint protocols—an area that warrants systematic investigation given its potential impact on training adherence and injury risk.
Finally, theoretical contributions from authors such as Sancese et al. [45] emphasise the value of specificity in preventive interventions. Exercises that replicate the mechanical and temporal demands of sprinting are more likely to induce protective adaptations than generalised resistance training alone. This conceptual shift supports a paradigm in which sprinting is not simply tolerated in training but actively prescribed as part of injury prevention.
While more high-quality trials are needed to refine protocols and expand applicability, the current body of evidence supports the incorporation of progressive, technically sound sprint training as a valuable component of modern HSI prevention. The integration of sprint drills with eccentric and neuromuscular conditioning may not only reduce injury rates but also enhance performance and tissue resilience in elite and sub-elite athletes. Given the exploratory nature of this scoping review, no meta-analysis or formal risk of bias assessment was conducted, in accordance with JBI recommendations. While this limits the ability to draw definitive conclusions, it provides a comprehensive mapping of the current evidence. Future systematic reviews incorporating meta-analytic methods and quality assessments are necessary to quantify effect sizes, dose-response relationships, and to guide evidence-based practice more robustly.
10.1. Synergistic Effects with Distal Kinetic-Chain Interventions
Forces generated during ground contact propagate along the entire lower-limb kinetic chain. Consequently, distal segments such as the foot may modulate proximal hamstring loading. Emerging evidence indicates that impaired foot biomechanics—e.g., reduced mid-foot stiffness or altered fore-foot load distribution—can increase proximal muscular demand by attenuating energy dissipation at push-off [48]. Interventions that improve foot stability, intrinsic plantar-flexor strength, and fifth-metatarsal load distribution have demonstrated favourable kinetic adaptations during the sprinting stance phase [48]. It is therefore plausible that sprint training, when combined with targeted foot-stability exercises (e.g., short-foot drills, resisted toe-flexion, sensorimotor balance work), provides a complementary stimulus that further attenuates the risk of hamstring strain. Future interventional studies should explore such integrative approaches.
10.2. Clinical Practice Implications
The findings of this review offer practical recommendations for sports medicine and performance professionals aiming to reduce hamstring injury risk in competitive athletes. Firstly, sprint exposure should be viewed not as a hazard to avoid but as an essential neuromuscular stimulus, provided it is implemented progressively and technically correctly. Training sessions should incorporate repeated sprint efforts at intensities ≥90% of MSS, with careful attention to weekly sprint load and acute:chronic ratio progression.
Secondly, sprint training must not occur in isolation. It should be combined with eccentric strengthening exercises—such as NHC, Razor Curl, or hip-dominant variations—which are effective in increasing fascicle length and eccentric capacity. These modalities can be periodised and alternated based on the phase of the season and the athlete’s training history.
Thirdly, attention to sprint mechanics is essential. Biomechanical inefficiencies should be screened through video analysis or motion capture when available. Athletes exhibiting risk markers such as poor hip extension velocity or excessive pelvic tilt should receive targeted technical coaching and corrective exercises.
Fourthly, foot biomechanics should be optimised. Exercises that enhance intrinsic foot-muscle strength, medial-arch control, and fifth-metatarsal load sharing—such as short-foot holds, resisted toe curls, and proprioceptive single-leg stance—may reduce aberrant distal mechanics that otherwise amplify proximal hamstring demand [48]. These drills can be blended into warm-ups or neuromotor circuits surrounding sprint sessions.
Finally, injury prevention should be athlete-centred and context-sensitive. History of prior injury, sport-specific demands, position, age, and neuromuscular asymmetries should inform programme design. Integrating monitoring technologies (e.g., GPS, sprint timing systems, muscle function tests) into regular assessments may allow practitioners to detect overload or maladaptation before injuries occur.
Overall, the current evidence encourages a paradigm shift in HSI prevention—from avoidance of sprinting to its strategic inclusion as a cornerstone of injury-resilient performance.
11. Conclusions
This scoping review highlights the preventive value of sprint-based training in reducing hamstring injuries among competitive athletes. When progressively and technically implemented, sprint exposure—especially at ≥90% of the maximal sprint speed—can serve as both a performance enhancer and an injury mitigation strategy. The most effective interventions combine sprint work with eccentric strengthening, agility, and biomechanical optimisation. Future research should aim to standardise protocols and extend findings to more diverse athletic populations. These findings support the inclusion of sprint training as a key component of hamstring injury prevention and inform evidence-based protocols for sports practitioners.
Author Contributions
R.T. and F.G. conceptualised and designed the study and were responsible for data acquisition. R.T. drafted the manuscript. F.G. and D.D. provided supervision and guidance throughout the study. F.G. performed the editing of the manuscript. R.T. reviewed the manuscript and curated the methodology. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ekstrand, J.; Hägglund, M.; Waldén, M. Injury Incidence and Injury Patterns in Professional Football: The UEFA Injury Study. Br. J. Sports Med. 2011, 45, 553–558. [Google Scholar] [CrossRef]
- Liu, H.; Garrett, W.E.; Moorman, C.T.; Yu, B. Injury Rate, Mechanism, and Risk Factors of Hamstring Strain Injuries in Sports: A Review of the Literature. J. Sport Health Sci. 2012, 1, 92–101. [Google Scholar] [CrossRef]
- Arnason, A.; Andersen, T.E.; Holme, I.; Engebretsen, L.; Bahr, R. Prevention of Hamstring Strains in Elite Soccer: An Intervention Study. Scand. J. Med. Sci. Sports 2008, 18, 40–48. [Google Scholar] [CrossRef]
- Aiello, F.; Di Claudio, C.; Fanchini, M.; Impellizzeri, F.M.; McCall, A.; Sharp, C.; Brown, S.J. Do Non-Contact Injuries Occur during High-Speed Running in Elite Football? Preliminary Results from a Novel GPS and Video-Based Method. J. Sci. Med. Sport 2023, 26, 465–470. [Google Scholar] [CrossRef] [PubMed]
- van den Tillaar, R.; Solheim, J.A.B.; Bencke, J. Comparison of Hamstring Muscle Activation During High-Speed Running and Various Hamstring Strengthening Exercises. Int. J. Sports Phys. Ther. 2017, 12, 718–727. [Google Scholar] [CrossRef]
- Kalema, R.N.; Duhig, S.J.; Williams, M.D.; Donaldson, A.; Shield, A.J. Sprinting Technique and Hamstring Strain Injuries: A Concept Mapping Study. J. Sci. Med. Sport 2022, 25, 209–215. [Google Scholar] [CrossRef]
- Woods, C.; Hawkins, R.; Maltby, S.; Hulse, M.; Thomas, A.; Hodson, A. The Football Association Medical Research Programme: An Audit of Injuries in Professional Football—Analysis of Hamstring Injuries. Br. J. Sports Med. 2004, 38, 36–41. [Google Scholar] [CrossRef]
- Jonkers, I.; Stewart, C.; Spaepen, A. The Complementary Role of the Plantarflexors, Hamstrings and Gluteus Maximus in the Control of Stance Limb Stability during Gait. Gait Posture 2003, 17, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Higashihara, A.; Nagano, Y.; Ono, T.; Fukubayashi, T. Differences in Activation Properties of the Hamstring Muscles during Overground Sprinting. Gait Posture 2015, 42, 360–364. [Google Scholar] [CrossRef]
- Dorn, T.W.; Schache, A.G.; Pandy, M.G. Muscular Strategy Shift in Human Running: Dependence of Running Speed on Hip and Ankle Muscle Performance. J. Exp. Biol. 2012, 215, 1944–1956. [Google Scholar] [CrossRef]
- Schache, A.G.; Dorn, T.W.; Blanch, P.D.; Brown, N.A.T.; Pandy, M.G. Mechanics of the Human Hamstring Muscles during Sprinting. Med. Sci. Sports Exerc. 2012, 44, 647–658. [Google Scholar] [CrossRef] [PubMed]
- Hegyi, A.; Gonçalves, B.A.M.; Finni, T.; Cronin, N.J. Individual Region- and Muscle-Specific Hamstring Activity at Different Running Speeds. Med. Sci. Sports Exerc. 2019, 51, 2274–2285. [Google Scholar] [CrossRef] [PubMed]
- Morin, J.-B.; Gimenez, P.; Edouard, P.; Arnal, P.; Jiménez-Reyes, P.; Samozino, P.; Brughelli, M.; Mendiguchia, J. Sprint Acceleration Mechanics: The Major Role of Hamstrings in Horizontal Force Production. Front. Physiol. 2015, 6, 404. [Google Scholar] [CrossRef] [PubMed]
- Ernlund, L.; Vieira, L.d.A. Hamstring Injuries: Update Article. Rev. Bras. Ortop. 2017, 52, 373–382. [Google Scholar] [CrossRef]
- Dalton, S.L.; Kerr, Z.Y.; Dompier, T.P. Epidemiology of Hamstring Strains in 25 NCAA Sports in the 2009–2010 to 2013–2014 Academic Years. Am. J. Sports Med. 2015, 43, 2671–2679. [Google Scholar] [CrossRef]
- Kerkhoffs, G.M.; van den Bekerom, M.; Elders, L.A.M.; van Beek, P.A.; Hullegie, W.A.M.; Bloemers, G.M.F.M.; de Heus, E.M.; Loogman, M.C.M.; Rosenbrand, K.C.J.G.M.; Kuipers, T.; et al. Diagnosis, Treatment and Prevention of Ankle Sprains: An Evidence-Based Clinical Guideline. Br. J. Sports Med. 2012, 46, 854–860. [Google Scholar] [CrossRef]
- Timmins, R.G.; Bourne, M.N.; Shield, A.J.; Williams, M.D.; Lorenzen, C.; Opar, D.A. Short Biceps Femoris Fascicles and Eccentric Knee Flexor Weakness Increase the Risk of Hamstring Injury in Elite Football (Soccer): A Prospective Cohort Study. Br. J. Sports Med. 2016, 50, 1524–1535. [Google Scholar] [CrossRef]
- Martin, R.L.; Cibulka, M.T.; Bolgla, L.A.; Koc, T.A.; Loudon, J.K.; Manske, R.C.; Weiss, L.; Christoforetti, J.J.; Heiderscheit, B.C. Hamstring Strain Injury in Athletes. J. Orthop. Sports Phys. Ther. 2022, 52, CPG1–CPG44. [Google Scholar] [CrossRef]
- Crow, J.; Semciw, A.; Couch, J.; Pizzari, T. Does a Recent Hamstring Muscle Injury Affect the Timing of Muscle Activation during High Speed Overground Running in Professional Australian Football Players? Phys. Ther. Sport 2020, 43, 188–194. [Google Scholar] [CrossRef]
- Gabbe, B.J.; Bennell, K.L.; Finch, C.F.; Wajswelner, H.; Orchard, J.W. Predictors of Hamstring Injury at the Elite Level of Australian Football. Scand. J. Med. Sci. Sports 2006, 16, 7–13. [Google Scholar] [CrossRef]
- Engebretsen, A.H.; Myklebust, G.; Holme, I.; Engebretsen, L.; Bahr, R. Intrinsic Risk Factors for Hamstring Injuries among Male Soccer Players: A Prospective Cohort Study. Am. J. Sports Med. 2010, 38, 1147–1153. [Google Scholar] [CrossRef] [PubMed]
- Croisier, J.-L.; Ganteaume, S.; Binet, J.; Genty, M.; Ferret, J.-M. Strength Imbalances and Prevention of Hamstring Injury in Professional Soccer Players: A Prospective Study. Am. J. Sports Med. 2008, 36, 1469–1475. [Google Scholar] [CrossRef] [PubMed]
- Mendiguchia, J.; Garrues, M.A.; Schilders, E.; Myer, G.D.; Dalmau-Pastor, M. Anterior Pelvic Tilt Increases Hamstring Strain and Is a Key Factor to Target for Injury Prevention and Rehabilitation. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Duhig, S.; Shield, A.J.; Opar, D.; Gabbett, T.J.; Ferguson, C.; Williams, M. Effect of High-Speed Running on Hamstring Strain Injury Risk. Br. J. Sports Med. 2016, 50, 1536–1540. [Google Scholar] [CrossRef]
- Suarez-Arrones, L.; Nakamura, F.Y.; Maldonado, R.A.; Torreno, N.; Di Salvo, V.; Mendez-Villanueva, A. Applying a Holistic Hamstring Injury Prevention Approach in Elite Football: 12 Seasons, Single Club Study. Scand. J. Med. Sci. Sports 2021, 31, 861–874. [Google Scholar] [CrossRef]
- Tedeschi, R.; Platano, D.; Giorgi, F. Stepping towards Relief: A Scoping Review on the Impact of Unstable Footwear in Chronic Low Back Pain Management. J. Sports Med. Phys. Fitness 2025, 65, 247–254. [Google Scholar] [CrossRef]
- Green, B.; Bourne, M.N.; van Dyk, N.; Pizzari, T. Recalibrating the Risk of Hamstring Strain Injury (HSI): A 2020 Systematic Review and Meta-Analysis of Risk Factors for Index and Recurrent Hamstring Strain Injury in Sport. Br. J. Sports Med. 2020, 54, 1081–1088. [Google Scholar] [CrossRef]
- Bramah, C.; Tawiah-Dodoo, J.; Rhodes, S.; Elliott, J.D.; Dos’Santos, T. The Sprint Mechanics Assessment Score: A Qualitative Screening Tool for the In-Field Assessment of Sprint Running Mechanics. Am. J. Sports Med. 2024, 52, 1608–1616. [Google Scholar] [CrossRef]
- Haugen, T.; Tønnessen, E.; Hisdal, J.; Seiler, S. The Role and Development of Sprinting Speed in Soccer. Int. J. Sports Physiol. Perform. 2014, 9, 432–441. [Google Scholar] [CrossRef]
- Lacome, M.; Avrillon, S.; Cholley, Y.; Simpson, B.M.; Guilhem, G.; Buchheit, M. Hamstring Eccentric Strengthening Program: Does Training Volume Matter? Int. J. Sports Physiol. Perform. 2020, 15, 81–90. [Google Scholar] [CrossRef]
- Howard, R.M.; Conway, R.; Harrison, A.J. Muscle Activity in Sprinting: A Review. Sports Biomech. 2018, 17, 1–17. [Google Scholar] [CrossRef]
- Mendiguchia, J.; Conceição, F.; Edouard, P.; Fonseca, M.; Pereira, R.; Lopes, H.; Morin, J.-B.; Jiménez-Reyes, P. Sprint versus Isolated Eccentric Training: Comparative Effects on Hamstring Architecture and Performance in Soccer Players. PLoS ONE 2020, 15, e0228283. [Google Scholar] [CrossRef] [PubMed]
- Malone, S.; Roe, M.; Doran, D.A.; Gabbett, T.J.; Collins, K. High Chronic Training Loads and Exposure to Bouts of Maximal Velocity Running Reduce Injury Risk in Elite Gaelic Football. J. Sci. Med. Sport 2017, 20, 250–254. [Google Scholar] [CrossRef] [PubMed]
- Colby, M.J.; Dawson, B.; Peeling, P.; Heasman, J.; Rogalski, B.; Drew, M.K.; Stares, J. Improvement of Prediction of Noncontact Injury in Elite Australian Footballers With Repeated Exposure to Established High-Risk Workload Scenarios. Int. J. Sports Physiol. Perform. 2018, 13, 1130–1135. [Google Scholar] [CrossRef] [PubMed]
- Freeman, B.W.; Young, W.B.; Talpey, S.W.; Smyth, A.M.; Pane, C.L.; Carlon, T.A. The Effects of Sprint Training and the Nordic Hamstring Exercise on Eccentric Hamstring Strength and Sprint Performance in Adolescent Athletes. J. Sports Med. Phys. Fitness 2019, 59, 1119–1125. [Google Scholar] [CrossRef]
- Ripley, N.J.; Cuthbert, M.; Comfort, P.; McMahon, J.J. Effect of Additional Nordic Hamstring Exercise or Sprint Training on the Modifiable Risk Factors of Hamstring Strain Injuries and Performance. PLoS ONE 2023, 18, e0281966. [Google Scholar] [CrossRef]
- Tedeschi, R. Case Study: Gait Assessment of a Patient with Hallux Rigidus Before and After Plantar Modification. Int. J. Surg. Case Rep. 2024, 114, 109197. [Google Scholar] [CrossRef]
- Lee, J.W.Y.; Mok, K.-M.; Chan, H.C.K.; Yung, P.S.H.; Chan, K.-M. Eccentric Hamstring Strength Deficit and Poor Hamstring-to-Quadriceps Ratio Are Risk Factors for Hamstring Strain Injury in Football: A Prospective Study of 146 Professional Players. J. Sci. Med. Sport 2018, 21, 789–793. [Google Scholar] [CrossRef]
- Edouard, P.; Lahti, J.; Fleres, L.; Ahtiainen, J.; Ulvila, J.-J.; Lehtinen, T.; Virtanen, N.; Taipale, T.; Bellver, M.; Peltonen, V.; et al. A Musculoskeletal Multifactorial Individualised Programme for Hamstring Muscle Injury Risk Reduction in Professional Football: Results of a Prospective Cohort Study. BMJ Open Sport Exerc. Med. 2024, 10, e001866. [Google Scholar] [CrossRef]
- Moreno-Pérez, V.; Del Coso, J.; López-Del Campo, R.; Resta, R.; Romero-Sangüesa, J.; Courel-Ibáñez, J.; Méndez-Villanueva, A. Reduced Match Exposure in the Previous 2 Matches Accounts for Hamstring Muscle Injury Incidence in Professional Football Players. Sports Health 2024, 16, 109–114. [Google Scholar] [CrossRef]
- Peters: Joanna Briggs Institute Reviewer’s Manual, JBI—Google Scholar. Available online: https://scholar-google-com.ezproxy.unibo.it/scholar_lookup?hl=en&publication_year=2020&author=MDJ+Peters&author=C+Godfrey&author=P+McInerney&author=Z+Munn&author=AC+Tricco&author=H+Khalil&title=Joanna+Briggs+Institute+Reviewer%27s+Manual%2C+JBI (accessed on 9 June 2022).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- McGrath, T.M.; Hulin, B.T.; Pickworth, N.; Clarke, A.; Timmins, R.G. Determinants of Hamstring Fascicle Length in Professional Rugby League Athletes. J. Sci. Med. Sport 2020, 23, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.; Collins, K.; Macgregor, L.J. The Influence of Weekly Sprint Volume and Maximal Velocity Exposures on Eccentric Hamstring Strength in Professional Football Players. Sports 2022, 10, 125. [Google Scholar] [CrossRef] [PubMed]
- Sancese, A.; Taylor, L.; Walsh, G.; Byrd, E.; Delextrat, A. Effects of Sprint versus Strength Training on Risk Factors for Hamstring Injury in Football Players. J. Sports Med. Phys. Fitness 2023, 63, 580–587. [Google Scholar] [CrossRef]
- Buchheit, M.; Settembre, M.; Hader, K.; McHugh, D. Exposures to Near-to-Maximal Speed Running Bouts during Different Turnarounds in Elite Football: Association with Match Hamstring Injuries. Biol. Sport 2023, 40, 1057–1067. [Google Scholar] [CrossRef]
- Tedeschi, R. Delayed Onset Muscle Soreness in Neurological Rehabilitation: An Overlooked Challenge. Acta Neurol. Belg. 2025, 125, 585–586. [Google Scholar] [CrossRef]
- Zhou, H.; Xu, D.; Quan, W.; Gao, Z.; Xiang, L.; Gu, Y. Are There Changes in the Foot Biomechanics during the before and after Fifth Metatarsal Fracture Running Stance Phase? iScience 2025, 28, 112432. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).