Abstract
Background: The aesthetic performance of single-shade polymer-based restorative materials (SPRs) can be compromised by extrinsic stains. Understanding the effects of novel whitening interventions on SPRs is crucial. Objective: This in vitro study aimed to evaluate the effects of different whitening interventions, including a novel purple tooth serum and charcoal-based whitening toothpaste with and without in-office bleaching, on the color of a new coffee-stained SPR. Materials and Methods: Seventy disc-shaped SPR specimens were prepared, stained, and then divided into seven groups (n = 10). Three groups were subjected directly to 2500 cycles of brushing simulation with regular toothpaste (control), charcoal toothpaste, or purple tooth serum. The rest were divided into bleaching groups, and the four groups underwent a simulation of bleaching and then brushing with the three products. The color parameters were recorded at the stained baseline, after brushing, after bleaching, and after post-bleaching brushing. The color change (ΔE00) was calculated, and the data were analyzed statistically using the Kruskal–Wallis test and Dunn–Bonferroni pairwise comparisons (p < 0.05). Results: In-office bleaching without brushing had a statistically significantly higher ΔE00 value than all other groups (p < 0.001). Post hoc tests indicated that the ΔE00 values of the brushed specimens were not significantly different from each other when assessed with and without bleaching (p > 0.05). When using the charcoal toothpaste, the post-bleaching brushed specimens had a noticeable color change above the PT. Conclusions: Bleaching improved the stained SPR color initially, but other treatments may offer longer-lasting aesthetics. The charcoal toothpaste showed promising results when combined with bleaching. The purple serum showed limited effectiveness.
1. Introduction
Polymeric resin-based composite restorative materials (PRMs) have been used in dentistry for over 50 years and are frequently improved to meet high esthetic demands and clinical versatility [1,2]. PRMs consist of a resin matrix (most commonly Bisphenol A-glycidyl methacrylate (Bis-GMA)), inorganic fillers, silane coupling agents, pigments, inhibitors, additives, and initiators [3,4]. Recent advances in PRMs aim to simplify procedures and extend the lifespan of restorations, which often fail due to secondary caries, fractures, and/or esthetic deterioration [5]. Many dentists find it challenging to perfectly match the shade of a tooth with the PRM, often leaving a visible boundary [6]. Today, single-shade polymeric resin-based composite restorative materials (SPR) simplify shade matching procedures and enhance esthetics through their “smart shade technology” and “chameleon effect” [7,8]. New SPR formulations replace Bis-GMA with other monomers, such as urethane dimethacrylate (UDMA) and the low-viscosity triethylene glycol dimethacrylate (TEGDMA) to enhance their mechanical and esthetic properties and reduce the possibility of harmful bisphenol A (BPA) released from the set material [3,4]. The recently introduced Charisma Diamond One (Kulzer, Hanau, Germany) additionally contains bis(—acryloyloxymethyl) tricyclodecane (TCD-DI-HEA) to modify viscosity and reduce shrinkage [3]. SPRs contain uniformly sized spherical nano-fillers and color-producing particles that blend with surrounding hues to effectively restore the natural dental structure in a biomimetic approach [9,10]. Previous studies demonstrated the superior color-adjustment ability of SPRs against various background colors while reflecting wavelengths within the natural tooth’s color spectrum [7,11,12,13]. From a clinical perspective, the introduction of single-shade resin formulations can simplify shade-matching the restorative steps, decrease chair time, and improve cost-effectiveness [14,15].
Color stability of esthetic dental materials is a crucial factor in the clinical longevity of placed restorations [7]. Unfortunately, discoloration of PRMs is inevitable in the oral cavity due to intrinsic and extrinsic factors [7,16,17,18]. Intrinsic discoloration results from aging-mediated polymeric changes in the filler-matrix interface and within the resin matrix of the material. They are influenced by the degree of conversion and the properties of chemical components, including inorganic fillers, photoinitiators, pigments, and other organic matrix elements [7,18,19]. On the other hand, extrinsic discoloration results from staining media adhering to the restoration’s surface, worsened by poor oral hygiene practices, and eventually leading to the absorption of these superficial colorants through the material’s surface porosities [7,17]. These issues are mainly superficial and usually caused by exposure to non-dietary factors like smoking and other dietary substances like coffee, red wine, turmeric, and tea [12,17,20,21]. Therefore, the possibility of restoring the esthetic color of placed SPR-based restorations is a critical consideration in dental practice [18,22,23]. Although some clinicians prefer to replace the discolored restorations, more conservative management approaches are advocated in light of minimally invasive dentistry [14]. These include bleaching the restorations, brushing with whitening toothpaste, and the use of novel gels with stain-concealing properties [16,24,25].
External bleaching is a conservative treatment option that is typically used to enhance the color of teeth [11,12,13]. In-office peroxide-based bleaching offers the advantage of controlled application, with the possibility of an immediate effect observed by the patient [7,26]. Recent studies have found that this treatment option can potentially lighten the color of some SPRs affected by discoloration, but to varying extents and with questionable durability [7,12,16,27,28]. Color recovery of stained PRMs was found to be highly dependent on the frequency of bleaching applications, with multiple sessions typically being required to achieve clinically acceptable color changes [29,30]. On the other hand, bleaching may negatively impact the color match potential and surface characteristics of SPRs [31,32,33].
Over-the-counter whitening toothpastes are readily available but are primarily effective in removing surface stains [34]. They contain abrasives, such as hydrated silica and calcium carbonate, which polish enamel and remove food residues [35]. Whitening toothpastes with different formulations have been suggested in the recent literature to improve the color of PRMs and SPRs, with conflicting evidence regarding their effectiveness and the extent of improvement [11,36,37,38,39,40,41]. Hydrogen peroxide-based toothpastes have shown potential in improving the color of PRMs, particularly in terms of their lightness and whiteness by actively attacking stains [40]. However, the complete reversal of the staining effect in SPRs was not entirely attainable [39]. Charcoal-based products have gained significant attention in recent years [34]. Activated charcoal is a black powder made from heated organic materials, which is then incorporated into toothpastes to potentially adsorb pigments and mechanically remove surface stains [42]. Recent findings suggest that charcoal-containing toothpastes lead to a notable color change in PRMs and SPRs. However, they also lead to a greater deterioration in surface characteristics compared with regular toothpaste, while being less abrasive than powder toothpaste formulations [43].
Recently, toothpastes and gels containing water-soluble purple pigments have been introduced to improve the appearance of stained teeth by concealing and neutralizing their yellowish color [25,44,45]. The incorporated pigments would enhance the reflection of short visible-light wavelengths, resulting in brighter-looking teeth [25]. A novel highly water-soluble purple tooth serum (V34 Colour Corrector Serum™, Hismile, Burleigh, QLD, Australia) was introduced globally, containing high concentrations of two safe dyes, D&C Red No.33 and Brilliant Blue FCF (Blue 1) that bind to the pellicle. It was found to have a success rate of approximately 96.7%. % in improving tooth color in a controlled clinical trial [25]. Previous pigmented toothpaste formulations included blue covarine [11,46,47,48], but its use was limited due to its low solubility in water and restrictive FDA regulations in different countries [25]. Whitening toothpastes containing charcoal, blue covarine, and microbeads have been shown to induce a color change in SPRs [11,39,40,41,49,50]. However, the effects of the newly introduced purple tooth serum on discolored dental SPRs have not been investigated. An earlier study showed no significant color change associated with the use of blue covarine toothpaste [47]. On the other hand, a couple of recent studies found that blue covarine-, microbead abrasive-, and peroxide-based toothpastes produced a more pronounced whitening effect on teeth and dental restorations than charcoal-based variants [11,36]. Another study confirmed the greater color change in stained SPRs and PRMs after the use of blue covarine toothpaste [39], which could indicate a potential positive effect of new purple tooth serum formulae.
Despite the growing interest in innovative dental products, such as single-shade restoratives and over the counter (OTC) tooth whitening products, a notable gap remains in the literature regarding the efficacy of color-corrective toothpastes, serums, and foams, particularly the novel purple color-corrective serum, in comparison with traditional methods such as activated charcoal toothpaste and in-office bleaching with hydrogen peroxide. Specifically, it is unclear whether purple color corrective serum produces a more significant color change in stained single-shade polymer-based restorative materials. The main objective of the current study was to evaluate the response of a coffee-stained, single-shade composite resin to treatment with several conservative approaches for the management of discoloration. The null hypothesis was that there would be no difference in color change of a coffee-stained, single-shade polymeric resin-based restorative material (SPR) when subjected to various discoloration management techniques, such as brushing with a new color corrector serum and a charcoal-based toothpaste, with or without in-office bleaching.
2. Materials and Methods
2.1. Study Design
This study was approved by the Ethics Committee of the Faculty of Dentistry at King Abdulaziz University in Jeddah, Saudi Arabia (Proposal#203-11-24). Table 1 details the materials investigated in the current study.

Table 1.
Compositional information of the materials investigated in the study.
A total of seventy disc-shaped specimens were fabricated from a nano-hybrid TCD-containing SPR (Charisma Diamond One, Kulzer, Hanau, Germany). All specimens underwent staining through immersion in a coffee solution for 18 days, and baseline color readings were taken. The stained specimens were randomly assigned to seven groups (n = 10) based on the treatment that they would receive. The stained specimens were then divided into three main categories: the brushing groups, consisting of three groups depending on the toothpaste used without bleaching (BC, BP, BCH); the BL group, which received only bleaching and had immediate color assessment; and the bleaching then brushing groups, consisting of 3 groups, based on the toothpaste used after bleaching (BLC, BLP, BLCH). A color reading was finally taken for the 3 BR groups after 2500 brushing cycles. The BL group had its readings registered after bleaching, and then the 3 BLBR groups had their readings registered had their readings registered after 2500 cycles of brushing. The detailed study design is illustrated in Figure 1.
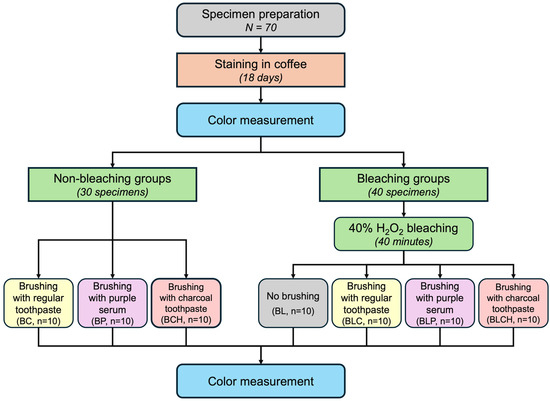
Figure 1.
Detailed study design, where BL is bleaching alone, BC is brushing with regular toothpaste, BP is brushing with purple tooth serum, BCH is brushing with charcoal toothpaste, BLC is bleaching and brushing with regular toothpaste, BLP is bleaching and brushing with purple serum, and BLCH is bleaching and brushing with charcoal toothpaste.
2.2. Specimen Fabrication
A custom mold was used to create disc-shaped specimens (8 × 2 mm). After spraying mold release solution on the mold, a glass slab was placed at the bottom of the mold, and the SPR material (Charisma One, Kulzer, Hanau, Germany) was packed into a designated circular space using a plastic filling instrument. The top surface was then covered with a mylar strip and a 1 mm thick glass slide, and gentle finger pressure was applied to extrude excess material and eliminate voids. The specimen preparation apparatus is demonstrated in Figure 2. Specimens were then cured using a light-emitting diode (LED) curing unit at 1200 mW cm−2 for 20 s (Mini LED Satelec, Satelec Acteon Group, Mérignac, France) according to the manufacturer’s instructions. Sof-Lex diamond polishing discs (3M ESPE, Solventum, Maplewood, MN, USA) attached to a straight handpiece rotating at a maximum of 12,000 rpm were used to polish the top surface of each specimen. A single operator performed all specimen preparation to maintain standardization between specimens. Each specimen was marked on the side that would not undergo color reading, denoting its group and number. All specimens were stored in a dark container in distilled water for 24 h before staining.
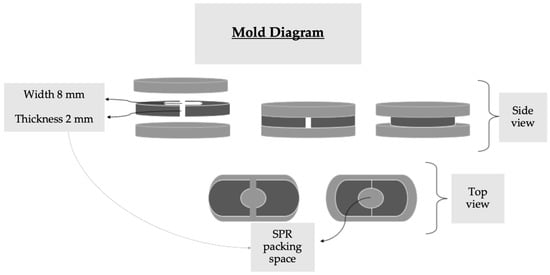
Figure 2.
Diagram representing the specimen fabrication apparatus, where SPR is the single-shade polymer-based restorative material.
2.3. Staining Procedures
All specimens were then placed in a coffee solution (Nescafé Classic instant coffee, Nestlé, Vevey, Switzerland) at room temperature. The solution was prepared beforehand by dissolving 2 g of the coffee grounds in 200 mL of boiled distilled water [53]. All specimens were stored in dark containers in an incubator at 37 °C for a total of 18 days. Storing specimens in coffee for 24 h is equivalent to storing them for approximately one month, assuming regular coffee consumption of about 3.2 cups per day, with an average duration of 15 min per cup [54]. Therefore, immersion for 18 days would represent 18 months of intra-oral use [29]. The beverage solutions were refreshed daily to ensure that there was no mold formation and to maintain the consistency of the coffee solution concentration, which varied throughout the day. After that, all specimens were randomly divided into seven groups (n = 10) according to the treatment that they received.
2.4. Color Parameter Measurement
All stained specimens were rinsed with deionized water for 5 min after staining and then gently dabbed dry with tissue paper before taking baseline color measurements. Baseline readings for all specimens were taken according to the CIE (Commission International de L’Eclairage [55]) L*, a*, and b* parameters using a lab-grade benchtop spectrophotometer (X-Rite ColorEye 7000A, X-Rite Inc., Grand Rapids, MI, USA), where L* represents lightness, with a value of 100 indicating white and zero indicating black; a* represents the red color axis (positive) and the green color axis (negative); and b* represents the yellow color axis (positive) and the blue color axis (negative). The spectrophotometric color measurement of each specimen was performed against a solid white background under an illuminating D65 light source. The spectrophotometer was calibrated before each measurement session. Baseline color measurements confirmed homogeneity of variance and no significant differences between groups, ensuring proper matching before interventions and allowing post-treatment differences to be attributed to experimental conditions rather than initial staining variations. The color parameters were recorded again after toothbrushing and/or bleaching. The color change (ΔE00) was determined using the stained specimen color readings as baseline measurements and applying the CIEDE 2000 color system guidelines [56,57]. The ΔE00 calculation was completed following the method published by Sharma et al. [58], in a Microsoft Excel sheet (Microsoft Office 365, Microsoft, Redmond, WA, USA) using the following formula, where x indicates the number of days of immersion in the beverage solution:
where x denotes the group; ΔL′ is the difference in lightness; ΔC′ is the difference in chroma; ΔH′ is the difference in hue, SL, SC, and SH refer to the weighting functions for lightness, chroma, and hue; kL, kC, and kH refer to the parametric weighting factors; and RT refers to the rotation term to account for chroma and hue interactions.
2.5. Non-Bleaching Group Assignment
Thirty stained specimens were randomly assigned to one of three groups: Group BC was regarded as a positive control group, with its ten specimens undergoing brushing with Colgate Regular toothpaste (Colgate-Palmolive, New York, NY, USA); Group BCH specimens were brushed using Colgate Optic White Charcoal Whitening Toothpaste (Colgate-Palmolive, New York, NY, USA); and Group BP specimens were brushed using the novel purple tooth serum (Hi Smile V34 Colour-Corrective tooth serum, Hi Smile, Gold Coast, Australia) (Group BC). Brushing simulations for 2500 cycles, as will be described in Section 2.6, were completed, after which color parameters were recorded according to the strategy mentioned in Section 2.4.
2.6. Brushing Simulation
Cylindrical acrylic blocks with a circular central well (Ecocryl cold, Protechno, Vilamalla, Spain) were produced using a silicone mold to hold the tested SPR specimens in place during the brushing simulation. Specimens were secured to the central wells of the acrylic blocks using vinyl polysiloxane impression material (Express XT Putty Soft, 3 M ESPE, Maplewood, MN, USA) and mounted to the test stations of the brushing simulation machine containing eight test stations (Toothbrush simulator ZM-3, SD Mechatronik GmbH, Feldkirchen-Westerham, Germany), as shown in Figure 3.

Figure 3.
Brushing simulation apparatus with 8 wells holding the SPR specimens inside.
A toothpaste slurry, prepared from the toothpaste assigned to each group and deionized water with a volume ratio of 1:3, was placed over the specimens, following previously published study protocols [59,60]. Toothbrushes (Tara Special Soft Toothbrush (soft bristles, medium-size, rectangular-shaped handle and head), Tara, Dammam, Saudi Arabia) were attached with a 1 N load, and the height and inclination of each toothbrush were adjusted so that the head was in contact with the specimen surface. The toothbrushes were subjected to a seven-day-long conditioning in deionized water at 37 °C, to remove residues, reduce variability, and ensure consistent bristle performance following ISO/TR 14569-1:2007 standard [61,62,63]. To run the simulation test, the machine was operated at a speed of 40 mm/s in a linear movement pattern for 2500 cycles, corresponding to 3 months of brushing intraorally [37,59,61]. Then, the acrylic blocks were removed from the test station and rinsed thoroughly under running water. The specimens were allowed to air-dry, and then color measurements were completed.
2.7. Bleaching Procedure and Bleaching Group Assignment
Forty stained specimens underwent external bleaching using in-office bleaching (40% Opalescence Boost bleaching gel, Ultradent, South Jordan, UT, USA). The two barrels of the bleaching formula (activator and bleaching gel) were mixed per the manufacturer’s instructions 25 times. A 1 mm thick layer of the mixed gel was applied to each specimen’s unmarked surface following the manufacturer’s instructions and allowed to remain for 20 min. The gel was then suctioned off, and once no gel was visible, the specimen was lightly rinsed with deionized water and allowed to air dry. Two cycles of bleaching were conducted, and the specimens were stored in deionized water for 24 h. Then, the color parameters were measured as described in Section 2.4, and ten bleached specimens were randomly assigned to Group BL.
2.8. Post-Bleaching Groups Assignment
The remaining thirty bleached specimens were randomly assigned to one of three groups depending on the toothpaste that would be used next (n = 10): Group BLC underwent brushing using a toothpaste slurry prepared from Colgate Regular toothpaste (Colgate-Palmolive, New York, NY, USA), Group BLCH specimens were brushed using Colgate Optic White Charcoal Whitening Toothpaste (Colgate-Palmolive, New York, NY, USA), and Group BLP specimens were brushed using the novel purple tooth serum (Hi Smile V34 Colour-Corrective toothpaste, Hi Smile, Gold Coast, Australia). Toothbrushing simulation was conducted as described previously in Section 2.6. The color parameters were recorded after the completion of 2500 cycles of brushing while following the steps described in Section 2.4.
2.9. Statistical Analysis
A total sample size of 70 specimens (n = 10 specimen per group) was selected after power calculation using G*Power software (version 3.1.9.6 for Mac OS, Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) for the study with an alpha error of 0.05, which was approximately 87% to detect differences (large effect f = 0.5) between groups.
Statistical analyses were conducted using R statistical software (Version 4.5.1, R Core Team (2025), Vienna, Austria) and DATAtab statistical calculator (DATAtab e.U., Graz, Austria). A Kolmogorov–Smirnov test of normality was conducted to confirm the normal distribution of the mean values for the color change measures (ΔE00 and ΔEab) within the groups. Levene’s Test was conducted to test the homogeneity of variances between the groups. The assumption of variance homogeneity for ΔE00 using Levene’s Test was violated. Therefore, Welch’s one-way analysis of variance (ANOVA) was conducted, followed by the Games-Howell post hoc test for pairwise comparisons. On the other hand, the homogeneity of variance was confirmed for the ΔEab values. Therefore, a one-way ANOVA test was performed, followed by Tukey’s HSD post hoc test. All statistical tests were conducted at p < 0.05.
3. Results
Results of Color Change
Group BL had the greatest color change (ΔE00, ΔEab) of all the test groups. Additionally, BLP had slightly greater ΔE00 and ΔEab than the other bleaching with brushing groups. BCH had a slightly greater ΔE00 and ΔEab than the other two brushing-only groups. Additionally, BL had the greatest change in lightness, followed by BLCH and BLC. The descriptive statistics of the color and lightness changes in the study groups are represented in Table 2 and Appendix A.

Table 2.
Descriptive statistical data on the color change (ΔE00, ΔEab), where BL is bleaching alone, BC is brushing with regular toothpaste, BP is brushing with purple tooth serum, BCH is brushing with charcoal tooth serum, BLC is bleaching and brushing with regular toothpaste, BLP is bleaching and brushing with purple tooth serum, and BLCH is bleaching and brushing with charcoal toothpaste.
The Welch’s one-way ANOVA and the standard one-way ANOVA tests revealed a significant difference between the groups in terms of the independent variable, TREATMENT, with respect to the dependent variables ΔE00 and ΔEab, respectively (p < 0.001). Thus, with the available data, the null hypothesis was rejected.
The Games-Howell test was used to compare the mean ΔE00 of the groups in pairs to find out which was significantly different (η2 = 0.92, Cohen’s d > 9). It revealed that the pairwise group comparisons of BC-BL, BP-BL, BCH-BL, BLC-BL, BLP-BL, and BLCH-BL had an adjusted p-value less than 0.001, and thus, based on the available data, it can be assumed that these groups were significantly different in pairs. Tukey’s HSD post hoc test was used to compare the mean ΔEab of the groups in pairs, and it revealed the same significant differences found in the ΔE00 results. The graphical representation of statistically significant pairwise comparison differences is represented in Figure 4, and the complete analysis is in Appendix B.
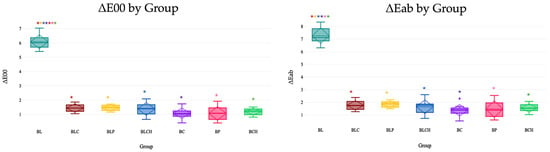
Figure 4.
Color change values of all groups with pairwise comparison results using Games-Howell and Tukey’s HSD post hoc tests for ΔE00 and ΔEab, respectively. Here, BL is bleaching alone, BC is brushing with regular toothpaste, BP is brushing with purple tooth serum, BCH is brushing with charcoal toothpaste, BLC is bleaching and brushing with regular toothpaste, BLP is bleaching and brushing with purple tooth serum, and BLCH is bleaching and brushing with charcoal toothpaste. Same color * represents statistically significant differences (p < 0.001).
4. Discussion
The increasing demand for esthetic dental treatments has led to a greater focus on polymer-based resin-composite restorative materials (PRMs) [64]. These materials are, however, known for their susceptibility to alterations in color stability and surface properties due to external factors such as bleaching agents and toothpastes. The aim of this study was to investigate the effects of bleaching and a novel purple color-correcting serum on the color of a stained single-shade polymer-based restorative material (SPR), which would affect both the longevity of restorations and patient satisfaction. The null hypothesis of the current study was that there would be no significant difference in the color change in the stained SPR between esthetic non-invasive treatments, including bleaching, brushing with charcoal-based whitening toothpaste, brushing with novel purple tooth serum, and a combination of bleaching and brushing. Based on the study results, the hypothesis was rejected.
4.1. Discussion and Justification of the Methodology Used
In the current study, the effect of a commonly used 40% in-office hydrogen peroxide bleaching gel was investigated. This concentration was selected for the study based on the literature, indicating its ability to induce structural and optical changes in PRMs by promoting oxidative degradation of the resin matrix and the filler/matrix interface [27,65,66]. Two cycles of bleaching were performed on each specimen to mimic clinical procedures according to the manufacturer’s instructions, which recommend completing two to three bleaching applications for satisfactory results [29].
According to the CAMBRA guidelines, a patient with a low risk of caries should visit the clinic for recall visits every 12–18 months [67]. Patients receiving bleaching treatments usually have restorations older than three years that show no signs of caries, classifying them in the low-caries-risk category [68]. Twenty-four hours of immersion in a coffee solution represents the equivalent of one month of intraoral use, according to Ertas et al. [54]. For these reasons, the staining period in the current study was selected to reflect 18 months of intraoral use. The exposure of SPRs to 18 months of coffee resulted in a significant color change, as determined in previous studies in the literature [18,22,69,70]. This duration includes patients who visit the clinic with complaints of discoloration and attend their 12- to 18-month recall appointments, during which they typically receive prophylactic tooth cleaning and scaling with ultrasonic and air-abrasion devices, which would remove superficially deposited stains [71,72]. During these visits, patients usually request dental whitening, oral hygiene advice, and other esthetic dental solutions.
A standard reference toothpaste with an RDA of 70 was used in this study, as its abrasivity falls within the acceptable clinical range [39,53]. An activated charcoal toothpaste with an RDA of 100 was included in this study due to its advertised dual mechanism of tooth whitening. The increasing use of activated charcoal in OTC dental products necessitates investigation of its effects on teeth and dental restorations [11]. Additionally, it was found previously that combining hydrogen peroxide with activated charcoal may accelerate color alteration in PRMs [22,40]. In the current study, a novel OTC purple tooth serum was investigated to complement or reduce the need for bleaching with hydrogen peroxide. It contains silica particles with an undisclosed RDA and dual water-soluble pigments to act in a similar manner to blue covarine, which was found to visually alter color perception instead of chemically changing the substrate [47,48]. As SPRs are increasingly used for their chameleon effect and aesthetic simplicity, evaluating their interaction with these widely advertised whitening agents is critical to understanding their potential in clinical practice [73].
Two thousand five hundred toothbrushing cycles were selected in the current study as this is reportedly equivalent to approximately three months of twice-daily brushing [37,59], which is a relevant duration for patients seeking dental consultation following bleaching treatment and a clinically translatable approximation of cumulative daily oral hygiene practices, offering insight into the durability and esthetic longevity of PRMs under simulated real-life conditions. In the study, soft-bristled toothbrushes with a low 1 N load were used for brushing simulation. This was conducted to simulate the gentle purple tooth serum application method recommended by the manufacturer while following ISO standard guidelines for toothbrushing simulation with toothpastes (ISO/TR 14569-1:2007) [63], which specify a load between 0.5 and 2.5 N for in vitro testing [61,62]. However, this brushing method still presents a deviation from the gentle cotton swab application of the serum. All specimens were rinsed gently after brushing to provide a standardized color testing surface for all treatment groups. This complied with the recommendations of the tooth serum and tested toothpaste manufacturers.
To assess color change in this study, a lab-grade benchtop spectrophotometer was selected due to its precision, objectivity, and widespread use in dental color evaluation, allowing the production of reliable, reproducible results that can be compared with the results in the previous literature. This colorimetric system quantifies color differences using three parameters—lightness (L*), the red-green axis (a*), and the yellow-blue axis (b*)—and has been extensively applied in previous studies investigating the effects of staining, aging, and bleaching on PRMs [7,16,17,73,74,75]. Forabosco et al. [33], Hasani et al. [76], and Telang et al. [77] employed the CIE L*a*b* system to objectively assess ΔE values, ensuring reproducible color change measurements over time. According to Luo [55], the CIE 1976 L*a*b* model continues to serve as the international standard for perceptual color comparisons in both scientific and clinical contexts. However, in dental research, the CIEDE 2000 color system for the calculation of color change produces more reliable and accurate data covering a wider spectrum of the color range seen in dental structures [56,57,58,78]. Therefore, its formula was utilized in the current study while following the guidelines of Sharma et al. [58]. Moreover, spectrophotometric evaluation overcomes the subjectivity associated with visual shade selection and enhances the reliability of color stability assessments.
4.2. Discussion of the Study Results
The findings of the current study demonstrated that the greatest color change occurred in the specimens immediately following bleaching with a 40% hydrogen peroxide gel. However, there were no significant differences in the color change between the other treatments, which included toothbrushing with different toothpastes, even when performed after bleaching. This demonstrated that while bleaching initially produced a significant improvement in color, this effect was not maintained after 2500 cycles of simulated toothbrushing using the different types of toothpastes, resulting in no eventual significant differences between the brushed and post-bleaching brushed groups. This suggests that the esthetic benefits of bleaching on the investigated SPR (Charisma Diamond One (CDO)) are transient and prone to relapse. This could indicate a possible dilution effect of the brushing after bleaching.
Even though the CDO contains staining-resistant, low-solubility UDMA monomers, it also includes low-viscosity, discoloration-susceptible TEGDMA, which could influence how the polymeric material responds to bleaching, whitening, and staining procedures [51]. Previously, it was reported that the color change in PRMs is inversely proportional to the TEGDMA content [79], partly explaining the limited color change effect of whitening treatments on the investigated SPR due to CDO’s low TEGDMA content. Swelling of the polymer network and water may reduce friction between polymer chains [80], causing a significantly different color change in bleached specimens during post-bleaching brushing, making them resemble the color of the non-bleached, brushed specimens. This chemical difference in the final resin matrix was consistently mentioned in the literature as a primary cause of discoloration owing to the water sorption tendency of the resin matrix [9,12,16]. However, this effect is standardized in the current investigation since one type of single shade composite was used.
In a recent study [33], it was found that bleaching teeth and SPRs together maintained the ability of the restorative material to match the new bleach shade without replacement, which could indicate the limited effect of bleaching on the restorative material, which is similar to the current study’s results. These results align with those of a study by Chen et al. [7], who reported that although bleaching initially altered the color of SPR materials, these changes were not stable over time, particularly after aging protocols. This reduction in bleaching effect after toothbrushing may be due to water sorption during brushing, causing a relapse of the bleaching effect [12]. The abrasiveness of the toothpastes and the silica particles present in the serum could have impacted the surface of the bleached SPR material. This interaction may have led to the removal of the most bleached surface layer, ultimately decreasing the retention of the color change attained by bleaching. Similarly, Forabosco et al. [33] found that bleaching had minimal long-term influence on the color matching of SPRs, highlighting the limited efficacy of bleaching on such materials. Furthermore, Aktu and Ulusoy [20] emphasized that bleaching procedures alone may not restore the original appearance.
While bleaching has been shown to effectively restore tooth enamel esthetics [65,81], its efficacy on PRMs, especially SPRs, appears to be limited. This discrepancy may be attributed to the differences in material composition, degree of conversion, and filler structure, as discussed in reviews by Ahmed et al. [10] and Alharbi et al. [82]. These highlighted that smart monochromatic SPRs rely heavily on light transmission and diffusion rather than intrinsic color, which may explain their reduced responsiveness to peroxide-based bleaching agents. The investigated SPR in the current study (CDO, with a degree of conversion up to 65% [3]) uses “adaptive light matching,” which determines the shade of the restoration by absorbing light waves reflected from the surrounding structures [80,83]. It contains UDMA, whose refractive index decreases as the size of the side alkyl chain increases, resulting in changes in translucency that are associated with the degree of conversion reached [84]. Further investigation into changes in translucency and degree of conversion associated with bleaching and brushing would be advisable, as it may shed light on the possible polymeric factors behind CDO’s response to bleaching and brushing.
The SPR color change produced by bleaching in the current study was around six, which is clearly noticeable as a different color to a lay observer and was statistically significantly greater than all other treatments (p < 0.001). Earlier research divided color changes into the following five categories according to how clear that change is: unnoticeable with a ΔE value below one, noticeable only by experienced observers when the change is up to two, noticeable by inexperienced observers when the change value is up to three and a half, clearly noticeable when the change reaches up to five, and clear differentiation of two colors when ΔE goes above five [85]. For dentistry, a ΔE00 value of 1.8 is generally considered the perceptibility threshold (PT), and 2.7 is the accepted threshold (AT) for acceptability [86,87]. All brushed specimens after bleaching showed a marginally greater ΔE00 and ΔEab than specimens that were only brushed, but it was not statistically significantly different (p > 0.05). This might indicate that bleaching might have maintained some of its positive effects even after brushing with the different toothpastes and the serum.
The color change produced by brushing with the novel purple tooth serum and the charcoal-based whitening toothpaste, with and without bleaching, was above one but below two, which means that the change would only be noticed by experienced dental personnel. This may suggest the abrasive removal of some of the adherent stain on the specimen surface, while also indicating a limitation in their color-related effects. Bleached specimens brushed with the color corrector serum exhibited a slightly greater, but not statistically or clinically significant, ΔE00 and ΔEab compared to other brushed groups. However, it slightly decreased the SPR’s lightness after bleaching as noted by the negative value of its ΔL, which could be attributed to the dark purple tint and the probably lower stain-removing abrasivity than toothpastes. Further investigation into the efficacy of toothbrushing with the novel purple tooth serum is advised to explore the possible effect of longer use. Brushing with charcoal-containing toothpaste lightened the specimens the most, followed by regular toothpaste, even though the color change was not statistically significant. A positive effect of charcoal-containing toothpaste was also reported by Forouzanfar et al. [36].
Within the limitations of the in vitro design of the study, the purple color-correcting tooth serum specimens did not have significantly different color change values compared to the other brushed SPR specimens, which could be attributed to their superficial and cosmetic concealer effect without actual change in the SPR material. The tooth serum was designed for a temporary concealing effect on teeth with gentle application and rinse before events [25,88] or brushing twice daily for 2 min [89], not as a toothpaste substitute. This would limit the direct comparison of its effects with toothpastes. Although positive effects were perceived on natural teeth after in vivo use of the product, as noted in a recent clinical trial by Pascolutti et al. [25], it must be noted that dental hard tissues differ drastically from restorative materials and, therefore, would respond differently to whitening and bleaching treatments. Additionally, that clinical trial included supervised application intraorally with no staining solutions, and positive subjective effects were also reported by study participants with both the placebo and the test serum, which could directly compare the study results.
The tested novel tooth serum contained two dyes, CI 17200 (D&C Red No. 33) and CI 42090 (FD&C Blue No. 1), resulting in a violet–purple coloration. The absorption of this highly water-soluble dye mixture into the salivary pellicle augments the reflection of violet light, masking yellow staining [25,90]. Since there was no exposure to saliva and, therefore, no pellicle on the SPR specimens, this could also explain why there was no statistically significant difference between brushing with it and brushing with standard toothpaste. Hashemikamangar et al. [46] investigated the effect of blue covarine-containing toothpaste on the color of resin-modified glass ionomers and other compounds and found no perceivable color differences, which is similar to what was found in the current study.
4.3. Limitations and Strengths of the Study
This study had several limitations. First, the simulated tooth brushing protocol was limited to 2500 cycles, which may not fully replicate the cumulative effects of long-term clinical brushing and, therefore, could limit the generalizability of the findings. Second, only one type of toothbrush bristle hardness and shape, and head size (soft, flat, medium size) was used, which may not represent the variability encountered in actual patient use with the wide variety of toothbrushes on the market.
When comparing the treatment groups, caution in interpreting the resulting color changes should be taken, given the deviations from the serum manufacturer’s protocol and the inherent differences between the tested materials. The tooth serum was marketed for daily esthetic use by gentle application on teeth, then wiping off or gently rinsing the excess material. Therefore, future research is recommended to compare different tinted tooth serums adhering more to the serum’s recommended application methods, like using cotton swabs or soft toothbrushes with gentler application loads. Additionally, testing a novel toothpaste that contains both the color-correcting serum and a toothpaste, compared to other whitening toothpastes, is recommended to provide direct comparative results.
The inherent nature of in vitro studies limits the ability to replicate all intraoral conditions, including the presence of saliva, temperature changes, dynamic forces, and other salivary factors. This includes the absence of salivary pellicle on the study’s specimens, necessary for the absorption of the color-correcting serum’s purple dye, which is yet another limitation of the study. Future in vitro and in vivo studies in the presence of saliva are recommended. This study focused on only one type of SPR, limiting the generalizability of the results. Therefore, comparing the SPR with other materials, as well as group shade PRMs with varying filler and monomer compositions, could provide additional valuable insights. Finally, the study utilized only extrinsic staining methods. In addition, it did not assess other optical and physical properties of the SPR material, such as translucency and gloss, surface roughness, microhardness and strength, and color match ability to a surrounding structure, which may also be influenced by bleaching and aging procedures and could further impact the material’s overall esthetic performance. In the current study, SPR specimens were tested, which are different than natural dental hard tissues, limiting comparison with the previous literature testing the toothpaste and tooth serum on natural teeth. Given the limitations of the study, caution is needed when interpreting the study findings and their implications for real-world scenarios.
The study presented several notable strengths that contribute to its validity and significance in the field of dental materials research. Firstly, it investigated a novel material (purple tooth serum) that had not been investigated for its effect on dental restorative materials. The current study utilized a controlled setting, enhancing the reliability of the findings. The power set for the current study (87%) was based on the detection of a large effect, which was confirmed by the detection of the large color change effect between the bleaching alone group and the other tested groups (η2 = 0.92, Cohen’s d > 9). However, future studies focusing on only toothbrushing effects, with a larger sample size, would be needed to detect smaller significant effects.
The focus on the Charisma One SPR allowed for targeted insights into the performance of specific materials used in dental restorations. Additionally, the study’s examination of color change under various treatment conditions provided a glimpse into the interactions between the in-office bleaching agents, OTC toothpastes, novel OTC tooth serum, and SPR materials. By comparing multiple treatments, including charcoal-containing toothpaste and the novel purple color-corrective tooth serum, the study offers valuable insights into the effectiveness of these options for maintaining the esthetic qualities of dental restorations.
5. Conclusions
Within the limitations of the current study, it can be concluded that the efficacy of bleaching with or without whitening toothpastes in treating discoloration in single-shade polymer-based restorative materials (SPRs) raises some concerns. The novel purple tooth serum could not improve the color of the SPR compared with other toothpastes. The study results showed that bleaching caused a noticeable color change immediately after treatment, but this effect diminished after simulated tooth brushing, resulting in no significant differences among groups. This suggests that the initial whitening from bleaching may be temporary, and the tested SPR would only have limited responsiveness to bleaching. Therefore, it would be advisable for clinicians to consider other options, including potentially resurfacing/repairing, veneering, or even replacing the stained restoration, rather than relying on bleaching and OTC products as a long-term solution for esthetic enhancement after discoloration. However, further studies are needed in order to investigate the effect on different formulations of single-shade resin composites, the response to different bleaching techniques, other types of toothpastes, and other color corrector formulations, as well as the effect of prolonged brushing.
Author Contributions
Conceptualization, H.E.Y., F.A.H., H.M.N. and R.A.; data curation, H.E.Y., W.H.M. and Y.M.A.; formal analysis, H.E.Y., W.H.M. and Y.M.A.; investigation, H.E.Y., W.H.M. and Y.M.A.; methodology, H.E.Y., F.A.H., H.M.N. and R.A.; project administration, H.E.Y., F.A.H., R.A. and H.M.N.; resources, H.E.Y., F.A.H., W.H.M. and Y.M.A.; software, H.E.Y. and F.A.H.; supervision, H.E.Y.; validation, H.E.Y. and F.A.H., visualization, H.E.Y., F.A.H., W.H.M. and Y.M.A.; writing—original draft preparation, W.H.M., Y.M.A. and H.E.Y.; writing—review and editing, H.E.Y., F.A.H., W.H.M., Y.M.A., H.M.N. and R.A. All authors have read and agreed to the published version of the manuscript.
Funding
The Deanship of Scientific Research (DSR) at King Abdulaziz University (KAU), Jeddah, Saudi Arabia has funded this project under grant no. (G:507-165-1443).
Institutional Review Board Statement
This study was approved by the Ethics Committee of the Faculty of Dentistry at King Abdulaziz University in Jeddah, Saudi Arabia (Proposal#203-11-24).
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request.
Acknowledgments
The authors acknowledge the Advanced Technology Dental Research Laboratory (ATDRL), Faculty of Dentistry, King Abdulaziz University, with thanks for their technical support.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A. Descriptive Statistics of the Change in Color Parameters for All Tested Groups

Table A1.
Descriptive statistics of the change in color parameters (dL, da, db, dL′/k_L/S_L, dC′/k_C/S_C, dH′/k_H/S_H) for all tested groups.
Table A1.
Descriptive statistics of the change in color parameters (dL, da, db, dL′/k_L/S_L, dC′/k_C/S_C, dH′/k_H/S_H) for all tested groups.
| Group | Frequency | Mean | Std. Deviation | Minimum | Maximum | |
| dL | BL | 10 | 7.11 | 0.64 | 6.07 | 8.27 |
| BLC | 10 | 0.5 | 0.76 | −0.71 | 1.55 | |
| BLP | 10 | −0.45 | 0.65 | −1.36 | 0.63 | |
| BLCH | 10 | 0.67 | 0.47 | 0.07 | 1.48 | |
| BC | 10 | −0.22 | 0.59 | −1.07 | 0.77 | |
| BP | 10 | −0.36 | 0.68 | −1.46 | 0.71 | |
| BCH | 10 | −0.06 | 0.64 | −1.13 | 0.95 | |
| Group | Frequency | Mean | Std. Deviation | Minimum | Maximum | |
| da | BL | 10 | 0.31 | 0.15 | 0.1 | 0.58 |
| BLC | 10 | −0.5 | 0.2 | −0.86 | −0.26 | |
| BLP | 10 | −0.47 | 0.2 | −0.68 | −0.1 | |
| BLCH | 10 | −0.46 | 0.17 | −0.7 | −0.25 | |
| BC | 10 | −0.35 | 0.18 | −0.7 | −0.09 | |
| BP | 10 | −0.31 | 0.24 | −0.73 | −0.06 | |
| BCH | 10 | −0.38 | 0.15 | −0.62 | −0.19 | |
| Group | Frequency | Mean | Std. Deviation | Minimum | Maximum | |
| db | BL | 10 | 1.01 | 1.13 | −1.91 | 2.1 |
| BLC | 10 | −1.41 | 0.43 | −2.21 | −0.76 | |
| BLP | 10 | −1.58 | 0.31 | −2.1 | −1.21 | |
| BLCH | 10 | −1.35 | 0.56 | −2.49 | −0.55 | |
| BC | 10 | −1.18 | 0.41 | −1.98 | −0.5 | |
| BP | 10 | −1.24 | 0.59 | −2.32 | −0.57 | |
| BCH | 10 | −1.36 | 0.38 | −1.97 | −0.66 | |
| Group | Frequency | Mean | Std. Deviation | Minimum | Maximum | |
| dL′/k_L/S_L | BL | 10 | −5.98 | 0.51 | −6.99 | −5.26 |
| BLC | 10 | 0.4 | 0.62 | −0.6 | 1.21 | |
| BLP | 10 | −0.36 | 0.52 | −1.1 | 0.5 | |
| BLCH | 10 | 0.53 | 0.37 | 0.06 | 1.18 | |
| BC | 10 | −0.17 | 0.49 | −0.86 | 0.64 | |
| BP | 10 | −0.29 | 0.54 | −1.12 | 0.57 | |
| BCH | 10 | −0.04 | 0.52 | −0.89 | 0.81 | |
| Group | Frequency | Mean | Std. Deviation | Minimum | Maximum | |
| dC′/k_C/S_C | BL | 10 | −0.71 | 0.75 | −1.45 | 1.21 |
| BLC | 10 | −0.97 | 0.3 | −1.51 | −0.55 | |
| BLP | 10 | −1.09 | 0.21 | −1.45 | −0.84 | |
| BLCH | 10 | −0.92 | 0.39 | −1.69 | −0.35 | |
| BC | 10 | −0.83 | 0.29 | −1.4 | −0.36 | |
| BP | 10 | −0.85 | 0.38 | −1.43 | −0.39 | |
| BCH | 10 | −0.94 | 0.27 | −1.37 | −0.45 | |
| Group | Frequency | Mean | Std. Deviation | Minimum | Maximum | |
| dH′/k_H/S_H | BL | 10 | 0.45 | 0.2 | 0.17 | 0.9 |
| BLC | 10 | 0.71 | 0.4 | 0.24 | 1.32 | |
| BLP | 10 | 0.7 | 0.29 | 0.18 | 1.08 | |
| BLCH | 10 | 0.8 | 0.31 | 0.45 | 1.24 | |
| BC | 10 | 0.46 | 0.27 | 0.06 | 0.95 | |
| BP | 10 | 0.33 | 0.25 | 0.04 | 0.71 | |
| BCH | 10 | 0.48 | 0.26 | 0.02 | 0.81 |
Appendix B. Change of Color Pairwise Comparison Results for Delta Eab and Delta E00

Table A2.
Change of color pairwise comparison results for delta Eab and delta E00 using Tukey’s HSD and Games-Howell tests.
Table A2.
Change of color pairwise comparison results for delta Eab and delta E00 using Tukey’s HSD and Games-Howell tests.
| Delta Eab Tukey’s HSD Pairwise Comparisons | Mean Diff. | p | 95% CI Lower Limit | 95% CI Upper Limit |
| BL-BLC | 5.5 | <0.001 | 4.82 | 6.19 |
| BL-BLP | 5.43 | <0.001 | 4.74 | 6.12 |
| BL-BLCH | 5.62 | <0.001 | 4.93 | 6.31 |
| BL-BC | 5.9 | <0.001 | 5.21 | 6.58 |
| BL-BP | 5.8 | <0.001 | 5.12 | 6.49 |
| BL-BCH | 5.71 | <0.001 | 5.03 | 6.4 |
| BLC-BLP | 0.08 | 1 | −0.61 | 0.76 |
| BLC-BLCH | 0.11 | 0.999 | −0.57 | 0.8 |
| BLC-BC | 0.39 | 0.597 | −0.3 | 1.08 |
| BLC-BP | 0.3 | 0.835 | −0.39 | 0.99 |
| BLC-BCH | 0.21 | 0.967 | −0.48 | 0.9 |
| BLP-BLCH | 0.19 | 0.979 | −0.5 | 0.88 |
| BLP-BC | 0.47 | 0.383 | −0.22 | 1.15 |
| BLP-BP | 0.38 | 0.641 | −0.31 | 1.06 |
| BLP-BCH | 0.28 | 0.868 | −0.4 | 0.97 |
| BLCH-BC | 0.28 | 0.881 | −0.41 | 0.96 |
| BLCH-BP | 0.19 | 0.982 | −0.5 | 0.87 |
| BLCH-BCH | 0.09 | 1 | −0.59 | 0.78 |
| BC-BP | 0.09 | 1 | −0.6 | 0.78 |
| BC-BCH | 0.18 | 0.983 | −0.5 | 0.87 |
| BP-BCH | 0.09 | 1 | −0.6 | 0.78 |
| Delta E00 Games-Howell Pairwise Comparisons | Adjusted p-Value | Estimate Mean Difference | 95% CI Lower limit | 95% CI Upper Limit |
| BC-BCH | 0.980 | 0.117 | −0.364 | 0.597 |
| BC-BL | <0.0001 | 5.010 | 4.350 | 5.670 |
| BC-BLC | 0.263 | 0.368 | −0.144 | 0.880 |
| BC-BLCH | 0.677 | 0.307 | −0.326 | 0.940 |
| BC-BLP | 0.124 | 0.392 | −0.071 | 0.855 |
| BC-BP | 1.000 | −0.005 | −0.662 | 0.652 |
| BCH-BL | <0.0001 | 4.890 | 4.280 | 5.510 |
| BCH-BLC | 0.461 | 0.251 | −0.170 | 0.672 |
| BCH-BLCH | 0.909 | 0.190 | −0.388 | 0.769 |
| BCH-BLP | 0.167 | 0.275 | −0.068 | 0.618 |
| BCH-BP | 0.991 | −0.122 | −0.729 | 0.485 |
| BL-BLC | <0.0001 | −4.640 | −5.280 | −4.010 |
| BL-BLCH | <0.0001 | −4.700 | −5.430 | −3.980 |
| BL-BLP | <0.0001 | −4.620 | −5.220 | −4.020 |
| BL-BP | <0.0001 | −5.020 | −5.760 | −4.280 |
| BLC-BLCH | 1.000 | −0.061 | −0.662 | 0.540 |
| BLC-BLP | 1.000 | 0.024 | −0.374 | 0.422 |
| BLC-BP | 0.448 | −0.373 | −1.000 | 0.254 |
| BLCH-BLP | 0.998 | 0.085 | −0.482 | 0.652 |
| BLCH-BP | 0.774 | −0.312 | −1.030 | 0.404 |
| BLP-BP | 0.305 | −0.397 | −0.993 | 0.200 |
References
- Ferracane, J.L. A Historical Perspective on Dental Composite Restorative Materials. J. Funct. Biomater. 2024, 15, 173. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Nassar, M.; Elsayed, M.A.; Jameel, D.B.; Ahmad, T.T.; Rahman, M.M. In Vitro Optical and Physical Stability of Resin Composite Materials with Different Filler Characteristics. Polymers 2023, 15, 2121. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz Atalı, P.; Doğu Kaya, B.; Manav Özen, A.; Tarçın, B.; Şenol, A.A.; Tüter Bayraktar, E.; Korkut, B.; Bilgin Göçmen, G.; Tağtekin, D.; Türkmen, C. Assessment of Micro-Hardness, Degree of Conversion, and Flexural Strength for Single-Shade Universal Resin Composites. Polymers 2022, 14, 4987. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Rocha, L.; Gonçalves, V.M.F.; Cunha, S.C.; Fernandes, J.O.; Pinho, T.; Tiritan, M.E. Evaluation of BPA and Bis-GMA Release from Recent Dental Composite Materials by LC-MS/MS. Separations 2023, 10, 455. [Google Scholar] [CrossRef]
- Pfeifer, C.S. Polymer-Based Direct Filling Materials. Dent. Clin. N. Am. 2017, 61, 733–750. [Google Scholar] [CrossRef]
- AlHamdan, E.M.; Bashiri, A.; Alnashmi, F.; Al-Saleh, S.; Al-shahrani, K.; Al-shahrani, S.; Alsharani, A.; Alzahrani, K.M.; Alqarawi, F.K.; Vohra, F.; et al. Evaluation of Smart Chromatic Technology for a Single-Shade Dental Polymer Resin: An In Vitro Study. Appl. Sci. 2021, 11, 10108. [Google Scholar] [CrossRef]
- Chen, S.; Zhu, J.; Yu, M.; Jin, C.; Huang, C. Effect of aging and bleaching on the color stability and surface roughness of a recently introduced single-shade composite resin. J. Dent. 2024, 143, 104917. [Google Scholar] [CrossRef]
- Leal, C.d.F.C.; Miranda, S.B.; Alves Neto, E.L.d.; Freitas, K.; de Sousa, W.V.; Lins, R.B.E.; de Andrade, A.K.M.; Montes, M.A.J.R. Color Stability of Single-Shade Resin Composites in Direct Restorations: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Polymers 2024, 16, 2172. [Google Scholar] [CrossRef]
- Turkistani, A.; Yeslam, H.E. Comparative Evaluation of Color Stability in Bioactive and Conventional Resin Cements Under Thermal Stress Conditions. Biomimetics 2025, 10, 432. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Jouhar, R.; Khurshid, Z. Smart Monochromatic Composite: A Literature Review. Int. J. Dent. 2022, 2022, 2445394. [Google Scholar] [CrossRef]
- Vaz, V.T.P.; Jubilato, D.P.; Oliveira, M.R.M.; Bortolatto, J.F.; Floros, M.C.; Dantas, A.A.R.; Oliveira Junior, O.B. Whitening toothpaste containing activated charcoal, blue covarine, hydrogen peroxide or microbeads: Which one is the most effective? J. Appl. Oral. Sci. 2019, 27, e20180051. [Google Scholar] [CrossRef]
- Tepe, H.; Celiksoz, O.; Yaman, B.C. Evaluation of color stability in single-shade composite resins using spectrophotometer and cross-polarized mobile photography. BMC Oral Health 2025, 25, 280. [Google Scholar] [CrossRef]
- Pereira Sanchez, N.; Powers, J.M.; Paravina, R.D. Instrumental and visual evaluation of the color adjustment potential of resin composites. J. Esthet. Restor. Dent. 2019, 31, 465–470. [Google Scholar] [CrossRef]
- Chaple Gil, A.; Caviedes, R.; Bersezio, C.; Martín, J.; Fernández, E.; Angel, P. Color Matching and Stability of Single-Shade Chameleon Dental Composites: A Systematic Review. J. Esthet. Restor. Dent. 2025, 37, 1838–1847. [Google Scholar] [CrossRef]
- Forabosco, E.; Josic, U.; Consolo, U.; Generali, L.; D’Alessandro, C.; Breschi, L.; Checchi, V. Color Match of Single-Shade Versus Multi-Shade Resin Composites: A Systematic Review With Meta-Analysis. J. Esthet. Restor. Dent. 2025, 37, 1443–1451. [Google Scholar] [CrossRef] [PubMed]
- AlHabdan, A.; Alsuhaibani, A.; Alomran, L.; Almutib, L. Effect of Staining and External Bleaching on the Color Stability and Surface Roughness of Universal-Shade Resin-Based Composite. Clin. Cosmet. Investig. Dent. 2025, 17, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Checchi, V.; Forabosco, E.; Della Casa, G.; Kaleci, S.; Giannetti, L.; Generali, L.; Bellini, P. Color Stability Assessment of Single- and Multi-Shade Composites Following Immersion in Staining Food Substances. Dent. J. 2024, 12, 285. [Google Scholar] [CrossRef] [PubMed]
- Hasanain, F.A. Effect of Ageing, Staining and Polishing on the Colour Stability of a Single, a Group Shade and Nano Fill Dental Composite: An In-vitro Study. J. Clin. Diagn. Res. 2022, 16, 26–30. [Google Scholar] [CrossRef]
- Barutcigil, Ç.; Yıldız, M. Intrinsic and extrinsic discoloration of dimethacrylate and silorane based composites. J. Dent. 2012, 40, e57–e63. [Google Scholar] [CrossRef]
- Aktu, A.; Ulusoy, N. Effect of Polishing Systems on the Surface Roughness and Color Stability of Aged and Stained Bulk-Fill Resin Composites. Materials 2024, 17, 3576. [Google Scholar] [CrossRef]
- Yeslam, H.E.; Bakhsh, A.F. Impact of kombucha, coffee, and turmeric beverages on the color stability of a single-shade versus a multi-shade resin-based composite. PeerJ 2025, 13, e19759. [Google Scholar] [CrossRef] [PubMed]
- Gamal, W.; Safwat, A.; Abdou, A. Effect of Coloring Beverages on Color Stability of Single Shade Restorative Material: An In Vitro Study. Open Access Maced. J. Med. Sci. 2022, 10, 28–32. [Google Scholar] [CrossRef]
- Şahin, H.C.; Korkut, B. Color adjustment of single-shade composites following staining, repolishing, and bleaching procedures. BMC Oral Health 2025, 25, 248. [Google Scholar] [CrossRef] [PubMed]
- Mariano da Rocha, B.G.P.; Ruiz-Lopez, J.; Perez, M.M.; Gaidarji, B.; Frasson, G.T.; Durand, L.B. Effectiveness and one-year whiteness stability of different in-office bleaching agents and alternative protocols. J. Prosthet. Dent. 2024, 133, 857–864. [Google Scholar] [CrossRef]
- Pascolutti, M.; Tomic, A.; Milleman, K.R.; Milleman, J.L.; Walsh, L.J. Safety and Effectiveness of a Novel Color Corrector Serum for Causing Temporary Changes to Tooth Shade: A Randomized Controlled Clinical Study. Dent. J. 2024, 12, 197. [Google Scholar] [CrossRef]
- Castro, G.G.; Pinto, P.A.; Favoreto, M.W.; Reis, A.; Viviana-Mora, M.; de Miranda, R.d.C.M.; Cardenas, A.F.M.; Loguercio, A.D.; Tavarez, R.R.d.J. Bleaching efficacy of in-office bleaching with violet light using low-concentration hydrogen peroxide nanoparticulate photocatalyst gel: A randomized controlled trial. Photodiagn. Photodyn. Ther. 2024, 50, 104410. [Google Scholar] [CrossRef]
- Althaqafi, K.A.; Alshabib, A. Effect of Bleaching Agents on Discoloured Resin-Based Composites for Direct Restorations: A Systematic Review. J. Pharm. Bioallied Sci. 2023, 15 (Suppl. S1), S1–S10. [Google Scholar] [CrossRef]
- Rosa, E.; Silva, L.; Silva, P.F.D.; Silva, A. Color matching and color recovery in large composite restorations using single-shade or universal composites. Braz. Dent. J. 2024, 35, e245665. [Google Scholar] [CrossRef]
- Yeslam, H.E.; AlZahrani, S.J. Time-dependent effect of intense capsule-coffee and bleaching on the color of resin-infiltrated enamel white spot lesions: An in vitro study. PeerJ 2022, 10, e14135. [Google Scholar] [CrossRef]
- Gul, P.; Harorli, O.; Ocal, I.B.; Ergin, Z.; Barutcugil, Ç. Color recovery effect of different bleaching systems on a discolored composite resin. Niger. J. Clin. Pract. 2017, 20, 1226. [Google Scholar] [CrossRef]
- Akarslan, E.; Hocaoglu, F.O.; Ucun, I. Classification of disc damage status by discovering knowledge from experimental data in marble cutting process. Proc. Inst. Mech. Eng. Part C–J. Mech. Eng. Sci. 2017, 231, 2407–2416. [Google Scholar] [CrossRef]
- Miranda, S.B.; Leal, C.d.F.C.; Lins, R.B.E.; Montes, M.A.J.R. Clinical Implications of Color Adjustment in Single-Shade Resins Post-Dental Bleaching: A Systematic Review. J. Clin. Med. 2025, 14, 3194. [Google Scholar] [CrossRef] [PubMed]
- Forabosco, E.; Consolo, U.; Mazzitelli, C.; Kaleci, S.; Generali, L.; Checchi, V. Effect of bleaching on the color match of single-shade resin composites. J. Oral Sci. 2023, 65, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Bardellini, E.; Marchetti, S.; Bordanzi, A.; Zanini, S.; Majorana, A.; Conti, G. Effectiveness of Activated Charcoal Toothpaste vs. 6% Hydrogen Peroxide Whitening Pen—An In Vitro Study. Dent. J. 2025, 13, 216. [Google Scholar] [CrossRef]
- Vranić, E.; Lacević, A.; Mehmedagić, A.; Uzunović, A. Formulation ingredients for toothpastes and mouthwashes. Bosn. J. Basic Med. Sci. 2004, 4, 51–58. [Google Scholar] [CrossRef]
- Forouzanfar, A.; Hasanpour, P.; Yazdandoust, Y.; Bagheri, H.; Mohammadipour, H.S. Evaluating the Effect of Active Charcoal-Containing Toothpaste on Color Change, Microhardness, and Surface Roughness of Tooth Enamel and Resin Composite Restorative Materials. Int. J. Dent. 2023, 2023, 6736623. [Google Scholar] [CrossRef]
- Turkistani, A.; Hasanain, F.A. Investigating the impact of whitening toothpastes on bioactive resin-based restorative materials: A comparative analysis. BMC Oral Health 2024, 24, 1527. [Google Scholar] [CrossRef]
- Ebrahimzadeh, F.; Fakhar, H.; Akbari, H.; Mosharraf, R.; Farzad, A. Effect of Two Whitening Toothpastes on Composite Resin Restorations Discolored by 0.2% Chlorhexidine Mouthwash. Front. Dent. 2022, 19, 38. [Google Scholar] [CrossRef]
- Colak, G.; Katirci, G. In Vitro evaluation of the effects of whitening toothpastes on the color and surface roughness of different composite resin materials. BMC Oral Health 2023, 23, 580. [Google Scholar] [CrossRef]
- Mehrgan, S.; Kermanshah, H.; Omrani, L.R.; Ahmadi, E.; Rafeie, N. Comparison the effect of charcoal-containing, hydrogen peroxide-containing, and abrasive whitening toothpastes on color stability of a resin composite; an in vitro study. BMC Oral Health 2021, 21, 594. [Google Scholar] [CrossRef]
- Gömleksiz, S.; Okumuş, Ö.F. The effect of whitening toothpastes on the color stability and surface roughness of stained resin composite. BMC Oral Health 2024, 24, 860. [Google Scholar] [CrossRef]
- Palandi, S.; Kury, M.; Zaghi Dal Picolo, M.; Coelho, C.; Cavalli, V. Effects of activated charcoal powder combined with toothpastes on enamel color change and surface properties. J. Esthet. Restor. Dent. 2020, 32, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Campolina, M.G.; de Souza, P.A.N.; Dietrich, L.; Soares, C.J.; Carvalho, C.N.; Carlo, H.L.; Silva, G.R. Can charcoal-based dentifrices change the color stability and roughness of bleached tooth enamel and resin composites? J. Clin. Exp. Dent. 2025, 17, e149–e159. [Google Scholar] [CrossRef] [PubMed]
- British Dental Journal. A beautiful, healthy smile for less. Br. Dent. J. 2023, 234, 831. [Google Scholar] [CrossRef]
- Vilhena, F.V.; Frederico de Oliveira Graeff, C.; Svizero, N.D.R.; D’Alpino, P.H.P. Effectiveness of Experimental Whitening Toothpastes Containing Colorants on the Optical Properties of Enamel. Sci. World J. 2022, 2022, 4576912. [Google Scholar] [CrossRef]
- Hashemikamangar, S.S.; Hoseinpour, F.; Kiomarsi, N.; Dehaki, M.G.; Kharazifard, M.J. Effect of an Optical Whitening Toothpaste on Color Stability of Tooth-Colored Restorative Materials. Eur. J. Dent. 2020, 14, 85–91. [Google Scholar] [CrossRef]
- Philpotts, C.J.; Cariddi, E.; Spradbery, P.S.; Joiner, A. In vitro evaluation of a silica whitening toothpaste containing blue covarine on the colour of teeth containing anterior restoration materials. J. Dent. 2017, 67S, S29–S33. [Google Scholar] [CrossRef]
- Tao, D.; Smith, R.N.; Zhang, Q.; Sun, J.N.; Philpotts, C.J.; Ricketts, S.R.; Naeeni, M.; Joiner, A. Tooth whitening evaluation of blue covarine containing toothpastes. J. Dent. 2017, 67S, S20–S24. [Google Scholar] [CrossRef]
- Tomás, D.B.M.; Pecci-Lloret, M.P.; Guerrero-Gironés, J. Effectiveness and abrasiveness of activated charcoal as a whitening agent: A systematic review of in vitro studies. Ann. Anat. 2023, 245, 151998. [Google Scholar] [CrossRef]
- Kim, S.; Chung, S.H.; Yamaguchi, S.; Arima, T.; Park, Y.S. Current evidence on the impact of whitening toothpastes on dental restorative materials: A comprehensive review. J. Prosthodont. Res. 2025. online ahead of print. [Google Scholar] [CrossRef]
- Krajangta, N.; Angkananuwat, C.; Leelaponglit, S.; Saelor, P.; Ngamjarrussriwichai, N.; Klaisiri, A. The Effect of Whitening and Daily Dentifrices on Red Wine Staining in Different Types of Composite Resins. Appl. Sci. 2024, 14, 12030. [Google Scholar] [CrossRef]
- Koc, U.; Bagdatli, Z.; Yilmaz, A.E.; Çakır, F.; Altundaşar, E.; Gurgan, S. Effects of charcoal-based whitening toothpastes on human enamel in terms of color, surface roughness, and microhardness: An in vitro study. Clin. Oral Investig. 2021, 25, 5977–5985. [Google Scholar] [CrossRef]
- Hazar, A.; Hazar, E. Effects of Whitening Dentifrices on the Enamel Color, Surface Roughness, and Morphology. Odovtos—Int. J. Dent. Sci. 2022, 25, 225–234. [Google Scholar] [CrossRef]
- Ertas, E.; Guler, A.U.; Yucel, A.C.; Koprulu, H.; Guler, E. Color stability of resin composites after immersion in different drinks. Dent. Mater. J. 2006, 25, 371–376. [Google Scholar] [CrossRef]
- Luo, M.R. CIE Chromatic Adaptation; Comparison of von Kries, CIELAB, CMCCAT97 and CAT02. In Encyclopedia of Color Science and Technology; Luo, R., Ed.; Springer: Berlin/Heidelberg, Germany, 2014; pp. 1–7. [Google Scholar]
- Gomez-Polo, C.; Portillo Munoz, M.; Lorenzo Luengo, M.C.; Vicente, P.; Galindo, P.; Martin Casado, A.M. Comparison of the CIELab and CIEDE2000 color difference formulas. J. Prosthet. Dent. 2016, 115, 65–70. [Google Scholar] [CrossRef]
- Paravina, R.D.; Ghinea, R.; Herrera, L.J.; Bona, A.D.; Igiel, C.; Linninger, M.; Sakai, M.; Takahashi, H.; Tashkandi, E.; Perez Mdel, M. Color difference thresholds in dentistry. J. Esthet. Restor. Dent. 2015, 27 (Suppl. S1), S1–S9. [Google Scholar] [CrossRef]
- Sharma, G.; Wu, W.; Dalal, E.N. The CIEDE2000 color-difference formula: Implementation notes, supplementary test data, and mathematical observations. Color Res. Appl. 2005, 30, 21–30. [Google Scholar] [CrossRef]
- Turkistani, A.; Hasanain, F.A. Surface roughness and gloss retention of bioactive resin composite after simulated toothbrush abrasion. Mater. Res. Express 2024, 11, 055401. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, J.; Hill, R.; Baysan, A. Evaluation of toothpastes for treating root carious lesions—A laboratory-based pilot study. BMC Oral Health 2024, 24, 484. [Google Scholar] [CrossRef]
- Büyükgöze Dindar, M.; Tekbas-Atay, M. The Effect of Brushing Force on The Surface Properties and Color Stability of Dental Enamel. NEU Dent. J. 2023, 5, 167–172. [Google Scholar] [CrossRef]
- Mohd Fathoni, F.; Kassim, Z.H.M.; Ab Ghani, S.M. Effect of a locally manufactured toothbrushing simulator on the monomer elution of CAD/CAM resin composite block—A pilot study. J. Health Transl. Med. 2024, 332. [Google Scholar] [CrossRef]
- ISO/TR 14569-1:2007(en); Dental Materials—Guidance on Testing of Wear—Part 1: Wear by Toothbrushing. The International Organization for Standardization: Geneva, Switzerland, 2007.
- Oladele, I.O.; Omotosho, T.F.; Adediran, A.A. Polymer-Based Composites: An Indispensable Material for Present and Future Applications. Int. J. Polym. Sci. 2020, 2020, 8834518. [Google Scholar] [CrossRef]
- Abu-saq Al Yami, A.; Al Qahtani, S.; Shokair, N.; Al Ghamdi, M.; Al Bouni, R. Effect of home and in-office bleaching systems on the nanomechanical properties of tooth enamel. Saudi Dent. J. 2020, 32, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Mourouzis, P.; Koulaouzidou, E.A.; Helvatjoglu-Antoniades, M. Effect of in-office bleaching agents on physical properties of dental composite resins. Quintessence Int. 2013, 44, 295–302. [Google Scholar] [PubMed]
- Featherstone, J.D.B.; Crystal, Y.O.; Alston, P.; Chaffee, B.W.; Doméjean, S.; Rechmann, P.; Zhan, L.; Ramos-Gomez, F. Evidence-Based Caries Management for All Ages-Practical Guidelines. Front. Oral Health 2021, 2, 657518. [Google Scholar] [CrossRef]
- Alqahtani, M.Q. Tooth-bleaching procedures and their controversial effects: A literature review. Saudi Dent. J. 2014, 26, 33–46. [Google Scholar] [CrossRef]
- Ersöz, B.; Karaoğlanoğlu, S.; Oktay, E.A.; Aydin, N. Resistance of Single-shade Composites to Discoloration. Oper. Dent. 2022, 47, 686–692. [Google Scholar] [CrossRef]
- Rohym, S.; Tawfeek, H.E.M.; Kamh, R. Effect of coffee on color stability and surface roughness of newly introduced single shade resin composite materials. BMC Oral Health 2023, 23, 236. [Google Scholar] [CrossRef]
- Fee, P.A.; Riley, P.; Worthington, H.V.; Clarkson, J.E.; Boyers, D.; Beirne, P.V. Recall intervals for oral health in primary care patients. Cochrane Database Syst. Rev. 2020, 10, Cd004346. [Google Scholar]
- Cobb, C.M.; Daubert, D.M.; Davis, K.; Deming, J.; Flemmig, T.F.; Pattison, A.; Roulet, J.F.; Stambaugh, R.V. Consensus Conference Findings on Supragingival and Subgingival Air Polishing. Compend. Contin. Educ. Dent. 2017, 38, e1–e4. [Google Scholar]
- Anwar, R.S.; Hussein, Y.F.; Riad, M. Optical behavior and marginal discoloration of a single shade resin composite with a chameleon effect: A randomized controlled clinical trial. BDJ Open 2024, 10, 11. [Google Scholar] [CrossRef]
- Mazzitelli, C.; Paolone, G.; Sabbagh, J.; Scotti, N.; Vichi, A. Color Stability of Resin Cements after Water Aging. Polymers 2023, 15, 655. [Google Scholar] [CrossRef]
- Andreucci, A.; Baroudi, K.; Freitas, M.; Amaral, M.; Aguiar, F.; Zanatta, R.; Liporoni, P. Color Stability and Degree of Conversion of Light-cured Resin Cements. Open Dent. J. 2023, 17, E187421062305150. [Google Scholar] [CrossRef]
- Hasani, E.; Baghban, A.A.; Sheikh-Al-Eslamian, S.M.; Sadr, A. Effect of bleaching on color change of composite after immersion in chlorhexidine and coffee. J. Conserv. Dent. 2019, 22, 529–532. [Google Scholar] [CrossRef]
- Telang, A.; Narayana, I.H.; Madhu, K.S.; Kalasaiah, D.; Ramesh, P.; Nagaraja, S. Effect of Staining and Bleaching on Color stability and Surface Roughness of Three Resin Composites: An in vitro study. Contemp. Clin. Dent. 2018, 9, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman, T.A.; Rodgers, B.; Suliman, A.A.; Johnston, W.M. Color and translucency stability of contemporary resin-based restorative materials. J. Esthet. Restor. Dent. 2021, 33, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Sensi, L.; Winkler, C.; Geraldeli, S. Accelerated aging effects on color stability of potentially color adjusting resin-based composites. Oper. Dent. 2021, 46, 188–196. [Google Scholar] [CrossRef]
- Ipek, İ.; Bilge, K. The effect of different liquids on the surface roughness and color stability of single shade and nanohybrid resin composites: An AFM and SEM analysis. Microsc. Res. Tech. 2024, 87, 2063–2071. [Google Scholar] [CrossRef]
- Vieira, I.; Vieira-Junior, W.F.; Pauli, M.C.; Theobaldo, J.D.; Aguiar, F.H.; Lima, D.A.; Leonardi, G.R. Effect of in-office bleaching gels with calcium or fluoride on color, roughness, and enamel microhardness. J. Clin. Exp. Dent. 2020, 12, e116–e122. [Google Scholar] [CrossRef]
- Alharbi, G.; Al Nahedh, H.N.A.; Al-Saud, L.M.; Shono, N.; Maawadh, A. Flexural strength and degree of conversion of universal single shade resin-based composites. Heliyon 2024, 10, e32557. [Google Scholar] [CrossRef]
- Altınışık, H.; Özyurt, E. Instrumental and visual evaluation of the color adjustment potential of different single-shade resin composites to human teeth of various shades. Clin. Oral Investig. 2023, 27, 889–896. [Google Scholar] [CrossRef]
- Zhu, J.; Chen, S.; Anniwaer, A.; Xu, Y.; Huang, C. Effects of background color and restoration depth on color adjustment potential of a new single-shade resin composite versus multi-shade resin composites. Front. Bioeng. Biotechnol. 2023, 11, 1328673. [Google Scholar] [CrossRef]
- Mokrzycki, W.; Tatol, M. Colour difference ∆E—A survey. Mach. Graph. Vis. 2011, 20, 383–411. [Google Scholar]
- Paravina, R.D.; Perez, M.M.; Ghinea, R. Acceptability and perceptibility thresholds in dentistry: A comprehensive review of clinical and research applications. J. Esthet. Restor. Dent. 2019, 31, 103–112. [Google Scholar] [CrossRef]
- Al-khazraji, K.; Sleibi, A. Analysis of Colour Differences Obtained by Acceptability and Perceptibility Threshold (Visual Method):-Review. Mustansiria Dent. J. 2023, 19, 280–289. [Google Scholar] [CrossRef]
- HiSmile V34 Colour Corrector Serum. Available online: https://hismile.online/en/products/v34-color-correcting-serum?srsltid=AfmBOoqjCTNr2u583svIKKAOvTnebA3gE7At63OBpoUFfYjVDOG36O1y (accessed on 1 May 2025).
- Adorebeuty Hismile V34 Colour Corrector Serum. Available online: https://www.adorebeauty.com.au/p/hismile/hismile-v34-colour-corrector.html (accessed on 1 May 2025).
- Tarver, J.G. Dye Compositions and Methods for Whitening Teeth Using Same. U.S. Patent No. 6,030,222, 29 February 2000. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).