Metallomic Profiling of the Human Eye and Its Relevance to Ophthalmic Diseases
Abstract
1. Introduction
2. Metallomic Analysis of the Human Eye in Ophthalmic Diseases
2.1. Cataracts
2.1.1. Lens
2.1.2. Aqueous Humor
2.2. Glaucoma
2.3. Diabetic Retinopathy
2.4. Macular Degeneration
2.5. Other Ophthalmic Diseases
2.5.1. Cytomegalovirus (CMV) Retinitis
2.5.2. Druses
2.5.3. Corneal Dystrophy
2.5.4. Pterygium
3. Discussion
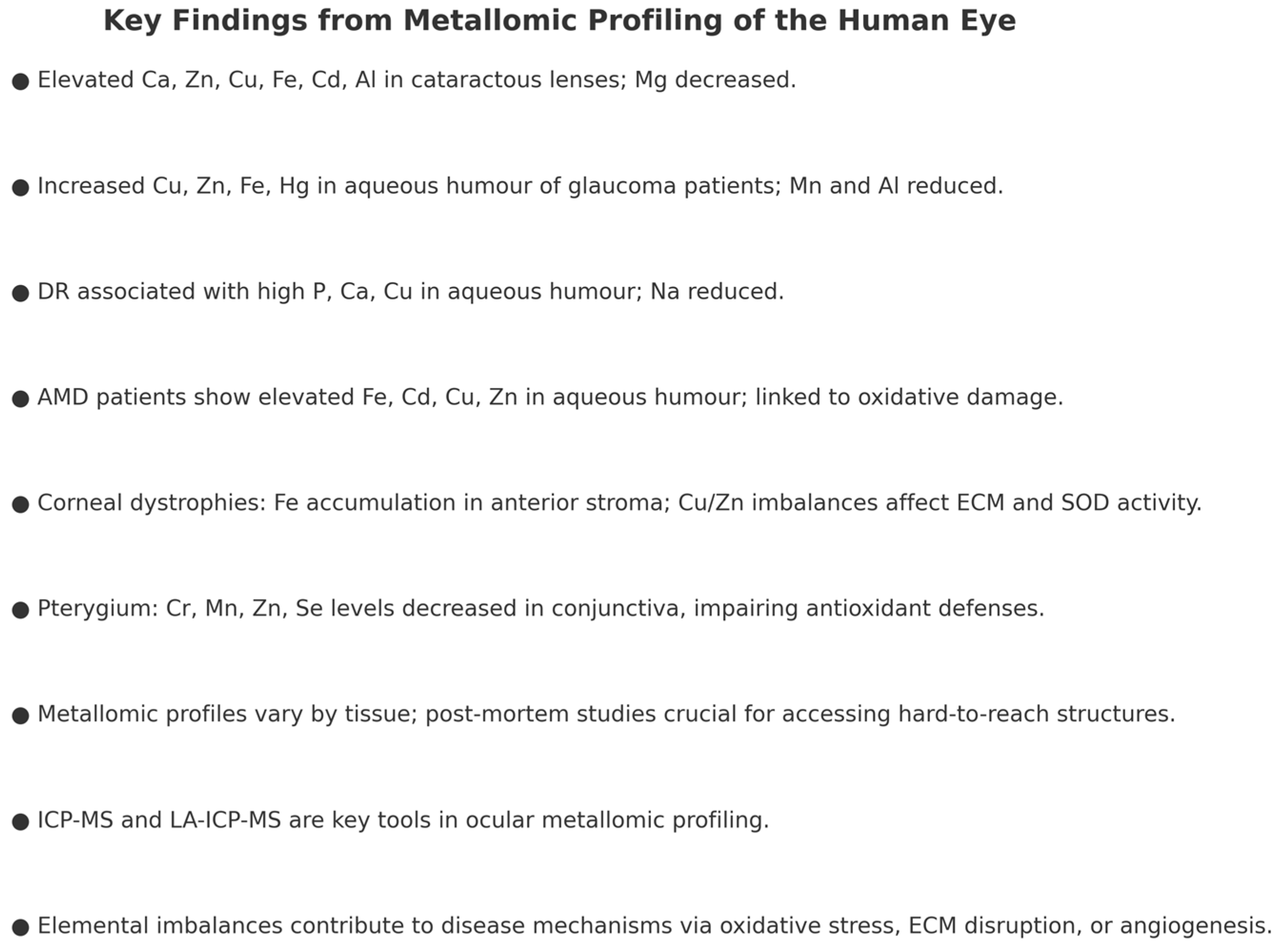
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| AAS | atomic absorption spectroscopy |
| ICP-AES | inductively coupled plasma atomic emission spectroscopy |
| ICP-MA | inductively coupled plasma mass spectrometry |
| LA-ICP-MS | laser ablation inductively coupled plasma mass spectrometry |
| ROS | reactive oxygen species |
References
- Haraguchi, H. Metallomics as Integrated Biometal Science. J. Anal. At. Spectrom. 2004, 19, 5–14. [Google Scholar] [CrossRef]
- Rayman, M.P. The Importance of Selenium to Human Health. Lancet 2000, 356, 233–241. [Google Scholar] [CrossRef]
- States, J.C.; Srivastava, S.; Chen, Y.; Barchowsky, A. Arsenic and Cardiovascular Disease. Toxicol. Sci. 2009, 107, 312–323. [Google Scholar] [CrossRef]
- Moksnes, M.R.; Hansen, A.F.; Wolford, B.N.; Thomas, L.F.; Rasheed, H.; Simic, A.; Bhatta, L.; Brantsaeter, A.L.; Surakka, I.; Zhou, W.; et al. A genome-wide association study provides insights into the genetic etiology of 57 essential and non-essential trace elements in humans. Commun. Biol. 2024, 7, 432. [Google Scholar] [CrossRef]
- Aalbers, T.G.; Houtman, J.P.; Makkink, B. Trace element concentrations in human autopsy tissue. Clin. Chem. 1987, 33, 2057–2064. [Google Scholar] [CrossRef] [PubMed]
- Stewart, T.J. Across the spectrum: Integrating multidimensional metal analytics for in situ metallomic imaging. Metallomics 2019, 11, 29–49. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, A.M. Elemental Analysis Using Atomic Absorption Spectroscopy. Eur. J. Eng. Technol. Res. 2021, 6, 48–51. [Google Scholar] [CrossRef]
- Michalke, B. Review about Powerful Combinations of Advanced and Hyphenated Sample Introduction Techniques with Inductively Coupled Plasma-Mass Spectrometry (ICP-MS) for Elucidating Trace Element Species in Pathologic Conditions on a Molecular Level. Int. J. Mol. Sci. 2022, 23, 6109. [Google Scholar] [CrossRef]
- Ciaralli, L.; Giordano, R.; Costantini, S.; Sepe, A.; Cruciani, F.; Moramarco, A.; Antonelli, B.; Balacco-Gabrieli, C. Element concentrations and cataract: An experimental animal model. J. Trace Elem. Med. Biol. 2001, 14, 205–209. [Google Scholar] [CrossRef]
- Micun, Z.; Falkowska, M.; Młynarczyk, M.; Kochanowicz, J.; Socha, K.; Konopińska, J. Levels of Trace Elements in the Lens, Aqueous Humour, and Plasma of Cataractous Patients-A Narrative Review. Int. J. Environ. Res. Public. Health 2022, 19, 376. [Google Scholar] [CrossRef]
- Eisma, J.H.; Dulle, J.E.; Fort, P.E. Current knowledge on diabetic retinopathy from human donor tissues. World J. Diabetes 2015, 6, 312–320. [Google Scholar] [CrossRef]
- Flieger, J.; Dolar-Szczasny, J.; Rejdak, R.; Majerek, D.; Tatarczak-Michalewska, M.; Proch, J.; Blicharska, E.; Flieger, W.; Baj, J.; Niedzielski, P.; et al. The Multi-Elemental Composition of the Aqueous Humor of Patients Undergoing Cataract Surgery, Suffering from Coexisting Diabetes, Hypertension, or Diabetic Retinopathy. Int. J. Mol. Sci. 2021, 22, 9413. [Google Scholar] [CrossRef] [PubMed]
- Forte, G.; Battagliola, E.T.; Malvasi, M.; Ruberti, N.; Daniele, P.; Mantovani, A.; Bocca, B.; Pacella, E. Trace Element Concentration in the Blood and Aqueous Humor of Subjects with Eye Cataract. Biol. Trace Elem. Res. 2025, 203, 684–693. [Google Scholar] [CrossRef] [PubMed]
- Moncaster, J.A.; Minaeva, O.; Lupoli, N.; Hua, N.; Goldstein, L.E. Mapping the Lens and Eye Metallome using Laser Ablation Inductively Coupled Plasma Mass Spectrometry (LA-ICP-MS). Investig. Ophthalmol. Vis. Sci. 2025, 66, 3270. [Google Scholar]
- Loh, A.; Hadziahmetovic, M.; Dunaief, J.L. Iron homeostasis and eye disease. Biochim. Biophys. Acta 2009, 1790, 637–649. [Google Scholar] [CrossRef]
- Xie, Q.; Peng, L.; Cai, F.; Ai, G.L.; Yang, K. Preliminary investigation of trace element in Pterygium using Synchrotron radiation micro-beam X-ray fluorescence analysis (-XRF). J. Instrum. 2013, 8, C07009. [Google Scholar] [CrossRef][Green Version]
- Yan, Y.; Ge, M.; Ma, R.; Zhao, H.; Wang, D.; Hu, C.; Wang, J.; Chen, W.; Zhang, C. A candidate reference method for serum calcium measurement by inductively coupled plasma mass spectrometry. Clin. Chim. Acta 2016, 461, 141–145. [Google Scholar] [CrossRef]
- Hou, X.W.; Wang, Y.; Pan, C.W. Metabolomics in Age-Related Macular Degeneration: A Systematic Review. Investig. Ophthalmol. Vis. Sci. 2020, 61, 13. [Google Scholar] [CrossRef]
- Yildirim, Z.; Ucgun, N.I.; Kilic, N.; Gursel, E.; Sepici-Dincel, A. Pseudoexfoliation syndrome and trace elements. Ann. N. Y. Acad. Sci. 2007, 1100, 207–212. [Google Scholar] [CrossRef]
- Hohberger, B.; Chaudhri, M.A.; Michalke, B.; Lucio, M.; Nowomiejska, K.; Schlötzer-Schrehardt, U.; Grieb, P.; Rejdak, R.; Jünemann, A.G.M. Levels of aqueous humor trace elements in patients with open-angle glaucoma. J. Trace Elem. Med. Biol. 2018, 45, 150–155. [Google Scholar] [CrossRef]
- Zhou, Y.; Hong, F.; Wang, X.; Feng, J.; Zhu, D.; Xu, Y.; Tao, Y. Abnormal Levels of Aqueous Humor Trace Elements in Patients with Cytomegalovirus Retinitis. Eye 2019, 33, 1606–1612. [Google Scholar] [CrossRef] [PubMed]
- Dolar-Szczasny, J.; Święch, A.; Flieger, J.; Tatarczak-Michalewska, M.; Niedzielski, P.; Proch, J.; Majerek, D.; Kawka, J.; Mackiewicz, J. Levels of Trace Elements in the Aqueous Humor of Cataract Patients Measured by the Inductively Coupled Plasma Optical Emission Spectrometry. Molecules 2019, 24, 4127. [Google Scholar] [CrossRef]
- Zeimer, R.; Weinreb, A.; Loewinger, E.; Kalman, Z.H.; Belkin, M. Detection and analysis of metals in the eye by x-ray spectrometry. Med. Phys. 1974, 1, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Erie, J.C.; Butz, J.A.; Good, J.A.; Erie, E.A.; Burritt, M.F.; Cameron, J.D. Heavy metal concentrations in human eyes. Am. J. Ophthalmol. 2005, 139, 888–893. [Google Scholar] [CrossRef] [PubMed]
- Czarnek, K.; Siwicki, A.K. Influence of chromium (III), cobalt (II) and their mixtures on cell metabolic activity. Curr. Issues Pharm. Med. Sci. 2021, 34, 87–93. [Google Scholar] [CrossRef]
- Czarnek, K.; Tatarczak-Michalewska, M.; Dreher, P.; Rajput, V.D.; Wójcik, G.; Gierut-Kot, A.; Szopa, A.; Blicharska, E. UV-C Seed Surface Sterilization and Fe, Zn, Mg, Cr Biofortification of Wheat Sprouts as an Effective Strategy of Bioelement Supplementation. Int. J. Mol. Sci. 2023, 24, 10367. [Google Scholar] [CrossRef]
- Czarnek, K.; Terpilowska, S.; Siwicki, A.K. Genotoxicity and mutagenicity of nickel(ii) and iron(iii) and interactions between these microelements. Trace Elem. Electrolytes 2019, 36, 17–24. [Google Scholar] [CrossRef]
- Zhu, X.; Lu, Y. Selenium supplementation can slow the development of naphthalene cataract. Curr. Eye Res. 2012, 37, 163–169. [Google Scholar] [CrossRef]
- de Vega, R.G.; García, M.; Fernández-Sánchez, M.L.; González-Iglesias, H.; Sanz-Medel, A. Protective effect of selenium supplementation following oxidative stress mediated by glucose on retinal pigment epithelium. Metallomics 2018, 10, 83–92. [Google Scholar] [CrossRef]
- Miceli, M.V.; Tate, D.J., Jr.; Alcock, N.W.; Newsome, D.A. Zinc deficiency and oxidative stress in the retina of pigmented rats. Investig. Ophthalmol. Vis. Sci. 1999, 40, 1238–1244. [Google Scholar]
- Chandorkar, A.G.; Bulakh, P.M.; Albal, M.V. Electrolyte composition in normal and cataractous lenses. Indian. J. Ophthalmol. 1980, 28, 135–138. [Google Scholar]
- Bonanno, J.A. Molecular mechanisms underlying the corneal endothelial pump. Exp. Eye Res. 2012, 95, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Baj, J.; Forma, A.; Kowalska, B.; Teresiński, G.; Buszewicz, G.; Majerek, D.; Flieger, W.; Maciejewski, R.; Karakuła, K.; Flieger, M.; et al. Multi-Elemental Analysis of Human Optic Chiasm—A New Perspective to Reveal the Pathomechanism of Nerve Fibers’ Degeneration. Int. J. Environ. Res. Public. Health 2022, 19, 4420. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Liang, Y.; Jiang, G.; Gan, Q.; Yang, T.; Liao, P.; Liang, H. Global, regional, and national burden of cataract: A comprehensive analysis and projections from 1990 to 2021. PLoS ONE 2025, 20, e0326263. [Google Scholar] [CrossRef] [PubMed]
- Nizami, A.A.; Gurnani, B.; Gulani, A.C. Cataract; Updated 27 February 2024, January 2025; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK539699/ (accessed on 20 July 2025).
- Chen, S.P.; Woreta, F.; Chang, D.F. Cataracts: A Review. JAMA 2025, 333, 2093–2103. [Google Scholar] [CrossRef]
- Congdon, N.; West, S.K.; Buhrmann, R.R.; Kouzis, A.; Muñoz, B.; Mkocha, H. Prevalence of the different types of age-related cataract in an African population. Investig. Ophthalmol. Vis. Sci. 2001, 42, 2478–2482. [Google Scholar]
- Hashemi, H.; Pakzad, R.; Yekta, A.; Aghamirsalim, M.; Pakbin, M.; Ramin, S.; Khabazkhoob, M. Global and regional prevalence of age-related cataract: A comprehensive systematic review and meta-analysis. Eye 2020, 34, 1357–1370. [Google Scholar] [CrossRef]
- Goel, N. Christmas tree cataract. Saudi J. Ophthalmol. 2016, 30, 210–211. [Google Scholar] [CrossRef]
- Midha, N.K.; Garg, M.K.; Kumar, D.; Meena, D.S.; Bohra, G.K. Rapidly Developing Cataract in Young Adult Patients: Always a Matter for Further Evaluation. Cureus 2021, 13, e17312. [Google Scholar] [CrossRef]
- Li, X.; Xie, J.; Xu, J.; Deng, L.; Cao, G.; Huang, S.; Zeng, C.; Liu, C.; Zhu, S.; He, G.; et al. Long-Term Exposure to Ambient PM2.5 and Age-Related Cataracts among Chinese Middle-Aged and Older Adults: Evidence from Two National Cohort Studies. Environ. Sci. Technol. 2023, 57, 11792–11802. [Google Scholar] [CrossRef]
- Tan, J.S.; Wang, J.J.; Younan, C.; Cumming, R.G.; Rochtchina, E.; Mitchell, P. Smoking and the Long-Term Incidence of Cataract: The Blue Mountains Eye Study. Ophthalmic Epidemiol. 2008, 15, 155–161. [Google Scholar] [CrossRef]
- Lindblad, B.E.; Håkansson, N.; Philipson, B.; Wolk, A. Alcohol Consumption and Risk of Cataract Extraction: A Prospective Cohort Study of Women. Ophthalmology 2007, 114, 680–685. [Google Scholar] [CrossRef]
- Jaga, K.; Dharmani, C. Ocular toxicity from pesticide exposure: A recent review. Environ Health Prev Med 2006, 11, 102–107. [Google Scholar] [CrossRef]
- Collman, G.W.; Shore, D.L.; Shy, C.M.; Checkoway, H.; Luria, A.S. Sunlight and Other Risk Factors for Cataracts: An Epidemiologic Study. Am. J. Public. Health 1988, 78, 1459–1462. [Google Scholar] [CrossRef] [PubMed]
- Ainsbury, E.A.; Bernard, S.; Bright, S.; Dalke, C.; Jarrin, M.; Kunze, S.; Tanner, R.; Dynlacht, J.R.; Quinlan, R.A.; Graw, J.; et al. Ionizing Radiation-Induced Cataracts: Recent Biological and Mechanistic Developments and Perspectives for Future Research. Mutat. Res. Mol. Mech. Mutagen. 2016, 770, 238–261. [Google Scholar] [CrossRef] [PubMed]
- Urban, R.C., Jr.; Cotlier, E. Corticosteroid-Induced Cataracts. Surv. Ophthalmol. 1986, 31, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Jacques, P.F.; Chylack, L.T., Jr.; McGandy, R.B.; Hartz, S.C. Antioxidant status in persons with and without senile cataract. Arch. Ophthalmol. 1988, 106, 337–340. [Google Scholar] [CrossRef]
- Obrosova, I.G.; Chung, S.S.; Kador, P.F. Diabetic Cataracts: Mechanisms and Management. Diabetes Metab. Res. Rev. 2010, 26, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Berthoud, V.M.; Beyer, E.C. Oxidative Stress, Lens Gap Junctions, and Cataracts. Antioxid. Redox Signal. 2009, 11, 339–353. [Google Scholar] [CrossRef]
- Bell, S.J.; Oluonye, N.; Harding, P.; Moosajee, M. Congenital Cataract: A Guide to Genetic and Clinical Management. Ther. Adv. Rare Dis. 2020, 1, 2633004020938061. [Google Scholar] [CrossRef]
- Kang, M.J.; Yim, H.B.; Hwang, H.B. Two Cases of Myotonic Dystrophy Manifesting Various Ophthalmic Findings with Genetic Evaluation. Indian. J. Ophthalmol. 2016, 64, 535–537. [Google Scholar] [CrossRef]
- Armentano, M.; Lucchino, L.; Alisi, L.; Chicca, A.V.; Di Martino, V.; Miraglia, E.; Iannetti, L.; Comberiati, A.M.; Giustini, S.; Lambiase, A.; et al. Ophthalmic Manifestation in Neurofibromatosis Type 2. Appl. Sci. 2023, 13, 6304. [Google Scholar] [CrossRef]
- Lambert, S.R.; Drack, A.V. Infantile Cataracts. Surv. Ophthalmol. 1996, 40, 427–458. [Google Scholar] [CrossRef] [PubMed]
- Garrity, J.A.; Liesegang, T.J. Ocular Complications of Atopic Dermatitis. Can. J. Ophthalmol. 1984, 19, 21–24. [Google Scholar]
- Jun, G.; Guo, H.; Klein, B.E.K.; Klein, R.; Wang, J.J.; Mitchell, P.; Miao, H.; Lee, K.E.; Joshi, T.; Buck, M.; et al. EPHA2 Is Associated with Age-Related Cortical Cataract in Mice and Humans. PLoS Genet. 2009, 5, e1000584. [Google Scholar] [CrossRef]
- Shiels, A.; Hejtmancik, J.F. Inherited Cataracts: Genetic Mechanisms and Pathways New and Old. Exp. Eye Res. 2021, 209, 108662. [Google Scholar] [CrossRef]
- Berry, V.; Francis, P.; Kaushal, S.; Moore, A.; Bhattacharya, S. Missense Mutations in MIP Underlie Autosomal Dominant ‘Polymorphic’ and Lamellar Cataracts Linked to 12q. Nat. Genet. 2000, 25, 15–17. [Google Scholar] [CrossRef] [PubMed]
- Bu, L.; Jin, Y.; Shi, Y.; Chu, R.; Ban, A.; Eiberg, H.; Andres, L.; Jiang, H.; Zheng, G.; Qian, M.; et al. Mutant DNA-Binding Domain of HSF4 Is Associated with Autosomal Dominant Lamellar and Marner Cataract. Nat. Genet. 2002, 31, 276–278. [Google Scholar] [CrossRef]
- Pras, E.; Levy-Nissenbaum, E.; Bakhan, T.; Lahat, H.; Assia, E.; Geffen-Carmi, N.; Frydman, M.; Goldman, B.; Pras, E. A Missense Mutation in the LIM2 Gene Is Associated with Autosomal Recessive Presenile Cataract in an Inbred Iraqi Jewish Family. Am. J. Hum. Genet. 2002, 70, 1363–1367. [Google Scholar] [CrossRef]
- Graw, J. Genetics of Crystallins: Cataract and Beyond. Exp. Eye Res. 2009, 88, 173–189. [Google Scholar] [CrossRef]
- Jakobs, P.M.; Hess, J.F.; FitzGerald, P.G.; Kramer, P.; Weleber, R.G.; Litt, M. Autosomal-dominant congenital cataract associated with a deletion mutation in the human beaded filament protein gene BFSP2. Am. J. Hum. Genet. 2000, 66, 1432–1436. [Google Scholar] [CrossRef]
- Valleix, S.; Niel, F.; Nedelec, B.; Algros, M.P.; Schwartz, C.; Delbosc, B.; Delpech, M.; Kantelip, B. Homozygous nonsense mutation in the FOXE3 gene as a cause of congenital primary aphakia in humans. Am. J. Hum. Genet. 2006, 79, 358–364. [Google Scholar] [CrossRef]
- Fernandez, M.M.; Afshari, N.A. Nutrition and the prevention of cataracts. Curr. Opin. Ophthalmol. 2008, 19, 66–70. [Google Scholar] [CrossRef]
- Shichi, H. Cataract formation and prevention. Expert. Opin. Investig. Drugs 2004, 13, 691–701. [Google Scholar] [CrossRef]
- Wu, F.; Wang, S.; Zhu, J.; Rutgard, J.; Yan, Y.B.; Zhang, K.; Zhao, L. Public impact, prevention, and treatment of cataracts. Sci. China Life Sci. 2015, 58, 1157–1159. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Burge, W.E. Analysis of the ash of the normal and the cataractous lens. Arch. Ophthalmol. 1909, 38, 435–450. [Google Scholar][Green Version]
- Tang, D.; Borchman, D.; Yappert, M.C.; Vrensen, G.F.J.M.; Rasi, V. Influence of Age, Diabetes, and Cataract on Calcium, Lipid-Calcium, and Protein-Calcium Relationships in Human Lenses. Investig. Ophthalmol. Vis. Sci. 2003, 44, 2059–2066. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, L.E.; Johnson, F.B. Calcium Oxalate Crystals within Ocular Tissues: A Clinicopathologic and Histochemical Study. AMA Arch. Ophthalmol. 1958, 60, 372–383. [Google Scholar] [CrossRef]
- Harding, C.V.; Chylack, L.T., Jr.; Susan, S.R.; Lo, W.K.; Bobrowski, W.F. Calcium-Containing Opacities in the Human Lens. Investig. Ophthalmol. Vis. Sci. 1983, 24, 1194–1202. [Google Scholar]
- Kashani, M.R.; Yousefi, R.; Akbarian, M.; Alavianmehr, M.M.; Ghasemi, Y. Structure, Chaperone Activity, and Aggregation of Wild-Type and R12C Mutant αB-Crystallins in the Presence of Thermal Stress and Calcium Ion—Implications for Role of Calcium in Cataract Pathogenesis. Biochemistry 2016, 81, 122–134. [Google Scholar] [CrossRef]
- Ringvold, A.; Sagen, E.; Bjerve, K.S.; Følling, I. The calcium and magnesium content of the human lens and aqueous humour. A study in patients with hypocalcemic and senile cataract. Acta Ophthalmol. 1988, 66, 153–156. [Google Scholar] [CrossRef]
- Ramirez-Bello, V.; Martinez-Seoane, J.; Fernández-Silva, A.; Amero, C. Zinc and Copper Ions Induce Aggregation of Human β-Crystallins. Molecules 2022, 27, 2970. [Google Scholar] [CrossRef]
- Cumurcu, T.; Mendil, D.; Etikan, I. Levels of zinc, iron, and copper in patients with pseudoexfoliative cataract. Eur. J. Ophthalmol. 2006, 16, 548–553. [Google Scholar] [CrossRef] [PubMed]
- Nagai, N.; Fukuhata, T.; Ito, Y. Effect of Magnesium Deficiency on Intracellular ATP Levels in Human Lens Epithelial Cells. Biol. Pharm. Bull. 2007, 30, 6–10. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cekić, O. Effect of Cigarette Smoking on Copper, Lead and Cadmium Accumulation in Human Lens. Br. J. Ophthalmol. 1998, 82, 186–188. [Google Scholar] [CrossRef] [PubMed]
- Garner, B.; Roberg, K.; Qian, M.; Eaton, J.W.; Truscott, R.J. Distribution of ferritin and redox-active transition metals in normal and cataractous human lenses. Exp. Eye Res. 2000, 71, 599–607. [Google Scholar] [CrossRef]
- Garner, B.; Davies, M.J.; Truscott, R.J. Formation of hydroxyl radicals in the human lens is related to the severity of nuclear cataract. Exp. Eye Res. 2000, 70, 81–88. [Google Scholar] [CrossRef]
- Tweeddale, H.J.; Hawkins, C.L.; Janmie, J.F.; Truscott, R.J.; Davies, M.J. Cross-linking of lens crystallin proteins induced by tryptophan metabolites and metal ions: Implications for cataract development. Free. Radic. Res. 2016, 50, 1116–1130. [Google Scholar] [CrossRef]
- Cumurcu, T.; Mendil, D.; Erkorkmaz, U. Aqueous humor and serum levels of chromium in cataract patients with and without diabetes mellitus. Ophthalmologica 2008, 222, 324–328. [Google Scholar] [CrossRef]
- Kim, C.J.; Choi, S.K. Analysis of aqueous humor calcium and phosphate from cataract eyes with and without diabetes mellitus. Korean J. Ophthalmol. 2007, 21, 90–94. [Google Scholar] [CrossRef]
- Schmeling, M.; Gaynes, B.I.; Tidow-Kebritchi, S. Heavy metal analysis in lens and aqueous humor of cataract patients by total reflection X-ray fluorescence spectrometry. Powder Diffr. 2014, 29, 155–158. [Google Scholar] [CrossRef][Green Version]
- Tham, Y.-C.; Li, X.; Wong, T.Y.; Quigley, H.A.; Aung, T.; Cheng, C.-Y. Global prevalence of glaucoma and pro-jections of glaucoma burden through 2040. Ophthalmology 2014, 121, 2081–2090. [Google Scholar] [CrossRef]
- Vision Loss Expert Group of the Global Burden of Disease Study; The GBD 2019 Blindness and Vision Impairment Collaborators. Global estimates on the number of people blind or visually impaired by glaucoma: A meta-analysis from 2000 to 2020. Eye 2024, 38, 2036–2046. [Google Scholar] [CrossRef]
- Foster, P.J.; Buhrmann, R.; Quigley, H.A.; Johnson, G.J. The definition and classification of glaucoma in prevalence surveys. Br. J. Ophthalmol. 2002, 86, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Quigley, H.A.; Broman, A.T. The number of people with glaucoma worldwide in 2010 and 2020. Br. J. Ophthalmol. 2006, 90, 262–267. [Google Scholar] [CrossRef]
- Pasquale, L.R.; Kang, J.H. Lifestyle, nutrition, and glaucoma. J. Glaucoma 2009, 18, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Saccà, S.C.; Izzotti, A. Oxidative stress and glaucoma: Injury in the anterior segment of the eye. Prog. Brain Res. 2008, 173, 385–407. [Google Scholar] [CrossRef] [PubMed]
- Shu, D.Y.; Chaudhary, S.; Cho, K.S.; Lennikov, A.; Miller, W.P.; Thorn, D.C.; Yang, M.; McKay, T.B. Role of Oxidative Stress in Ocular Diseases: A Balancing Act. Metabolites 2023, 13, 187. [Google Scholar] [CrossRef]
- Leske, M.C.; Heijl, A.; Hussein, M.; Bengtsson, B.; Hyman, L.; Komaroff, E. Factors for glaucoma progression and the effect of treatment: The early manifest glaucoma trial. Arch. Ophthalmol. 2003, 121, 48–56. [Google Scholar] [CrossRef]
- Armaly, M.F. Effect of Corticosteroids on Intraocular Pressure and Fluid Dynamics. II. The Effect of Dexamethasone in the Glaucomatous Eye. Arch. Ophthalmol. 1963, 70, 492–499. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, W.; Huang, W.; Zhang, X. Diabetes mellitus as a risk factor for open-angle glaucoma: A systematic review and meta-analysis. PLoS ONE 2014, 9, e102972. [Google Scholar] [CrossRef]
- Chung, H.J.; Hwang, H.B.; Lee, N.Y. The Association between Primary Open-Angle Glaucoma and Blood Pressure: Two Aspects of Hypertension and Hypotension. Biomed. Res. Int. 2015, 2015, 827516. [Google Scholar] [CrossRef]
- Gordon, M.O.; Beiser, J.A.; Brandt, J.D.; Heuer, D.K.; Higginbotham, E.J.; Johnson, C.A.; Keltner, J.L.; Miller, J.P.; Parrish, R.K.; Wilson, M.R.; et al. The Ocular Hypertension Treatment Study: Baseline Factors That Predict the Onset of Primary Open-Angle Glaucoma. Arch. Ophthalmol. 2002, 120, 714–720. [Google Scholar] [CrossRef]
- Marcus, M.W.; de Vries, M.M.; Montolio, F.G.J.; Jansonius, N.M. Myopia as a Risk Factor for Open-Angle Glaucoma: A Systematic Review and Meta-Analysis. Ophthalmology 2011, 118, 1989–1994.e2. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Hu, C.C.; Ho, J.D.; Chiu, H.W.; Lin, H.C. Obstructive Sleep Apnea and Increased Risk of Glaucoma: A Population-Based Matched-Cohort Study. Ophthalmology 2013, 120, 1559–1564. [Google Scholar] [CrossRef] [PubMed]
- Lascaratos, G.; Shah, A.; Garway-Heath, D.F. The Genetics of Pigment Dispersion Syndrome and Pigmentary Glaucoma. Surv. Ophthalmol. 2013, 58, 164–175. [Google Scholar] [CrossRef] [PubMed]
- Gedde, S.J.; Herndon, L.W.; Brandt, J.D.; Budenz, D.L.; Feuer, W.J.; Schiffman, J.C.; Tube Versus Trabeculectomy Study Group. Postoperative complications in the Tube Versus Trabeculectomy (TVT) study during five years of follow-up. Am. J. Ophthalmol. 2012, 153, 804–814. [Google Scholar] [CrossRef]
- American Academy of Ophthalmology. Primary Open-Angle Glau-coma. In Preferred Practice Pattern® Guidelines; American Academy of Ophthalmology: San Francisco, CA, USA, 2020. [Google Scholar]
- Coleman, A.L.; Kodama, T.; Moroi, S.E. The epidemiology of glaucoma: An update. Ann. Acad. Med. Singap. 2008, 37, 493–500. [Google Scholar]
- Kravchik, M.V.; Novikov, I.A.; Petrov, S.Y.; Avetisov, S.E. Bioinorganic chemistry of open-angle glaucoma: A review. J. Trace Elem. Med. Biol. 2020, 62, 126652. [Google Scholar] [CrossRef]
- Bussel, I.I.; Aref, A.A. Dietary factors and the risk of glaucoma: A review. Ther. Adv. Chronic. Dis. 2014, 5, 188–194. [Google Scholar] [CrossRef]
- Ramdas, W.D. The relation between dietary intake and glaucoma: A systematic review. Acta Ophthalmol. 2018, 96, 550–556. [Google Scholar] [CrossRef] [PubMed]
- Cekiç, O.; Bardak, Y.; Totan, Y.; Kavakli, S.; Akyol, O.; Ozdemir, O.; Karel, F. Nickel, chromium, manganese, iron and aluminum levels in human cataractous and normal lenses. Ophthalmic Res. 1999, 31, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Jünemann, A.G.; Stopa, P.; Michalke, B.; Chaudhri, A.; Reulbach, U.; Huchzermeyer, C.; Schlötzer-Schrehardt, U.; Kruse, F.E.; Zrenner, E.; Rejdak, R.; et al. Levels of aqueous humor trace elements in patients with non-exsudative age-related macular degeneration: A case-control study. PLoS ONE 2013, 8, e56734. [Google Scholar] [CrossRef] [PubMed]
- Helin-Toiviainen, M.; Rönkkö, S.; Kaarniranta, K.; Puustjärvi, T.; Rekonen, P.; Ollikainen, M.; Uusitalo, H. Oxidized low-density lipoprotein, lipid and calcium aggregates reveal oxidative stress and inflammation in the conjunctiva of glaucoma patients. Acta Ophthalmol. 2017, 95, 378–385. [Google Scholar] [CrossRef]
- McElnea, E.M.; Quill, B.; Docherty, N.G.; Irnaten, M.; Siah, W.F.; Clark, A.F.; O’Brien, C.J.; Wallace, D.M. Oxidative stress, mitochondrial dysfunction and calcium overload in human lamina cribrosa cells from glaucoma donors. Mol. Vis. 2011, 17, 1182–1191. [Google Scholar] [PubMed] [PubMed Central]
- Akyol, N.; Değer, O.; Keha, E.E.; Kiliç, S. Aqueous humour and serum zinc and copper concentrations of patients with glaucoma and cataract. Br. J. Ophthalmol. 1990, 74, 661–662. [Google Scholar] [CrossRef]
- NikhalaShree, S.; George, R.J.; Shantha, B.; Vijaya, L.; Sulochana, K.N.; Coral, K. Copper, Lysyl Oxidase Activity, and Collagen in Aqueous Humour of Primary Glaucoma: An Association with Clinical Parameters. Ophthalmic Res. 2023, 66, 949–957. [Google Scholar] [CrossRef]
- Wörn, M.; Lämmer, R.; Lucio, M.; Michalke, B.; Rühl, E.; Hohberger, B. The influence of trace elements on the therapeutic success of suprachoroidal draining devices. J. Trace Elem. Med. Biol. 2023, 78, 127195. [Google Scholar] [CrossRef] [PubMed]
- Bocca, B.; Forte, G.; Pisano, A.; Farace, C.; Giancipoli, E.; Pinna, A.; Dore, S.; Madeddu, R. A pilot study to evaluate the levels of aqueous humor trace elements in open-angle glaucoma. J. Trace Elem. Med. Biol. 2020, 61, 126560. [Google Scholar] [CrossRef]
- Yau, J.W.Y.; Rogers, S.L.; Kawasaki, R.; Lamoureux, E.L.; Kowalski, J.W.; Bek, T.; Chen, S.-J.; Dekker, J.M.; Fletcher, A.; Grauslund, J.; et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 2012, 35, 556–564. [Google Scholar] [CrossRef]
- Teo, Z.L.; Tham, Y.-C.; Yu, M.; Chee, M.L.; Rim, T.H.; Cheung, N.; Bikbov, M.M.; Wang, Y.X.; Tang, Y.; Lu, Y.; et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: A systematic review and meta analysis. Ophthalmology 2021, 128, 1580–1591. [Google Scholar] [CrossRef]
- Lopes de Faria, J.B.; Silva, K.C.; Lopes de Faria, J.M. The Contribution of Hypertension to Diabetic Nephropathy and Retinopathy: The Role of Inflammation and Oxidative Stress. Hypertens. Res. 2011, 34, 413–422. [Google Scholar] [CrossRef]
- Qian, H.; Ripps, H. Neurovascular Interaction and the Pathophysiology of Diabetic Retinopathy. Exp. Diabetes Res. 2011, 2011, 693426. [Google Scholar] [CrossRef]
- van Leiden, H.A.; Dekker, J.M.; Moll, A.C.; Nijpels, G.; Heine, R.J.; Bouter, L.M.; Stehouwer, C.D. Blood Pressure, Lipids, and Obesity Are Associated with Retinopathy: The Hoorn Study. Diabetes Care 2002, 25, 1320–1325. [Google Scholar] [CrossRef]
- Ting, D.S.W.; Cheung, G.C.M.; Wong, T.Y. Diabetic Retinopathy: Global Prevalence, Major Risk Factors, Screening Practices and Public Health Challenges: A Review. Clin. Exp. Ophthalmol. 2016, 44, 260–277. [Google Scholar] [CrossRef] [PubMed]
- DCCT Research Group. The Effect of Intensive Treatment of Diabetes on the Development and Pro-gression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N. Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Stratton, I.M.; Kohner, E.M.; Aldington, S.J.; Turner, R.C.; Holman, R.R.; Manley, S.E.; Matthews, D.R. UKPDS 50: Risk factors for incidence and progression of retinopathy in Type II diabetes over 6 years from diagnosis. Diabetologia 2001, 44, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Chew, E.Y.; Klein, M.L.; Ferris, F.L., 3rd; Remaley, N.A.; Murphy, R.P.; Chantry, K.; Hoogwerf, B.J.; Miller, D. Association of Elevated Serum Lipid Levels with Retinal Hard Exudate in Diabetic Retinopathy. Early Treatment Diabetic Retinopathy Study (ETDRS) Report 22. Arch. Ophthalmol. 1996, 114, 1079–1084. [Google Scholar] [CrossRef] [PubMed]
- Orsi, E.; Solini, A.; Bonora, E.; Vitale, M.; Garofolo, M.; Fondelli, C.; Trevisan, R.; Vedovato, M.; Cavalot, F.; Zerbini, G.; et al. Retinopathy as an Independent Predictor of All-Cause Mortality in Individuals with Type 2 Diabetes. Diabetes Metab. 2023, 49, 101413. [Google Scholar] [CrossRef]
- Abhary, S.; Hewitt, A.W.; Burdon, K.P.; Craig, J.E. A Systematic Meta-Analysis of Genetic Association Studies for Diabetic Retinopathy. Diabetes 2009, 58, 2137–2147. [Google Scholar] [CrossRef]
- Rippin, J.D.; Patel, A.; Bain, S.C. Genetics of Diabetic Nephropathy. Best. Pract. Res. Clin. Endocrinol. Metab. 2001, 15, 345–358. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.; Sobrin, L. Genetics of Diabetic Retinopathy. Curr. Diabetes Rep. 2014, 14, 515. [Google Scholar] [CrossRef]
- Aiello, L.P.; Avery, R.L.; Arrigg, P.G.; Keyt, B.A.; Jampel, H.D.; Shah, S.T.; Pasquale, L.R.; Thieme, H.; Iwamoto, M.A.; Park, J.E.; et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N. Engl. J. Med. 1994, 331, 1480–1487. [Google Scholar] [CrossRef]
- Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for Diabetic Macular Edema: Early Treatment Diabetic Retinopathy Study Report No. 4. Int. Ophthalmol. Clin. 1987, 27, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Cheung, N.; Mitchell, P.; Wong, T.Y. Diabetic retinopathy. Lancet 2010, 376, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Aydin, E.; Cumurcu, T.; Özugurlu, F.; Özyurt, H.; Sahinoglu, S.; Mendil, D.; Hasdemir, E. Levels of Iron, Zinc, and Copper in Aqueous Humor, Lens, and Serum in Nondiabetic and Diabetic Patients: Their Relation to Cataract. Biol. Trace Elem. Res. 2005, 108, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Kayiklik, A.; Sukgen, E.A. Biochemical analysis of aqueous humor in diabetic and non-diabetic patients with cataracts. Ophthalmol. J. 2019, 4, 1–6. [Google Scholar] [CrossRef]
- Wong, W.L.; Su, X.; Li, X.; Cheung, C.M.G.; Klein, R.; Cheng, C.-Y.; Wong, T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and me-ta-analysis. Lancet Glob. Health 2014, 2, e106–e116. [Google Scholar] [CrossRef]
- Ferris, F.L., 3rd; Wilkinson, C.P.; Bird, A.; Chakravarthy, U.; Chew, E.; Csaky, K.; Sadda, S.R. Clinical classification of age-related macular degeneration. Ophthalmology 2013, 120, 844–851. [Google Scholar] [CrossRef]
- Thornton, J.; Edwards, R.; Mitchell, P.; Harrison, R.A.; Buchan, I.; Kelly, S.P. Smoking and age-related macular degeneration: A review of association. Eye 2005, 19, 935–944. [Google Scholar] [CrossRef]
- Chakravarthy, U.; Wong, T.Y.; Fletcher, A.; Piault, E.; Evans, C.; Zlateva, G.; Buggage, R.; Pleil, A.; Mitchell, P. Clinical risk factors for age-related macular degeneration: A systematic review and meta-analysis. BMC Ophthalmol. 2010, 10, 31. [Google Scholar] [CrossRef]
- Fritsche, L.G.; Fariss, R.N.; Stambolian, D.; Abecasis, G.R.; Curcio, C.A.; Swaroop, A. Age-related macular degeneration: Genetics and biology coming together. Annu. Re.v Genom. Hum. Genet. 2014, 15, 151–171. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, P.J.; Brown, D.M.; Heier, J.S.; Boyer, D.S.; Kaiser, P.K.; Chung, C.Y.; Kim, R.Y.; Group, M.S. Ranibizumab for neovascular age-related macular degeneration. N. Engl. J. Med. 2006, 355, 1419–1431. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Miller, J.W.; Sickenberg, M.; Laqua, H.; Barbazetto, I.; Gragoudas, E.S.; Zografos, L.; Piguet, B.; Pournaras, C.J.; Donati, G.; et al. Photodynamic Therapy with Verteporfin for Choroidal Neovascularization Caused by Age-Related Macular Degeneration: Results of Retreatments in a Phase 1 and 2 Study. Arch. Ophthalmol. 1999, 117, 1177–1187, Erratum in Arch. Ophthalmol. 2000, 118, 488. [Google Scholar] [CrossRef] [PubMed]
- Age-Related Eye Disease Study 2 Research Group. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: The Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA 2013, 309, 2005–2015. [Google Scholar] [CrossRef]
- Stopa, P.; Rejdak, R.; Michalke, B.; Chaudhri, A.; Schlotzer-Schrehardt, U.; Kruse, F.E.; Zrenner, E.; Junemann, A.G. Levels of Aqueous Humour Trace Elements in Patients with Age-Related Macular Degeneration. Investig. Ophthalmol. Vis. Sci. 2010, 51, 4109. [Google Scholar]
- Medscape Reference. Cytomegalovirus (CMV) Retinitis. eMedicine. Available online: https://emedicine.medscape.com/article/1227228-overview (accessed on 3 July 2025).
- Zhao, Q.; Li, N.N.; Chen, Y.X.; Zhao, X.Y. Clinical features of Cytomegalovirus retinitis in patients with acquired immunodeficiency syndrome and efficacy of the current therapy. Front. Cell Infect. Microbiol. 2023, 13, 1107237. [Google Scholar] [CrossRef]
- Ferreira Tátá, C.; Ramires, T.; Piteira, M.; Matono, R.; Guz, C. Cytomegalovirus Retinitis as a Sole Manifestation of HIV Infection. Cureus 2021, 13, e18642. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ganciclovir. Australian Medicines Handbook; AMH Pty Ltd.: Wirlinga, Australia, 2024. [Google Scholar]
- Razonable, R.R.; Humar, A.; AST Infectious Diseases Community of Practice. Cytomegalovirus in Solid Organ Transplantation. Am. J. Transplant. 2013, 13 (Suppl. 4), 93–106. [Google Scholar] [CrossRef] [PubMed]
- Silvestri, G.; Williams, M.A.; McAuley, C.; Oakes, K.; Sillery, E.; Henderson, D.C.; Ferguson, S.; Silvestri, V.; Muldrew, K.A. Drusen prevalence and pigmentary changes in Caucasians aged 18–54 years. Eye 2012, 26, 1357–1362. [Google Scholar] [CrossRef]
- Wang, J.J.; Rochtchina, E.; Lee, A.J.; Chia, E.M.; Smith, W.; Cumming, R.G.; Mitchell, P. Ten-year incidence and progression of age-related maculopathy: The Blue Mountains Eye Study. Ophthalmology 2007, 114, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Zweifel, S.A.; Spaide, R.F.; Curcio, C.A.; Malek, G.; Imamura, Y. Reticular pseudodrusen are subretinal drusenoid deposits. Ophthalmology 2010, 117, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Hageman, G.S.; Anderson, D.H.; Johnson, L.V.; Hancox, L.S.; Taiber, A.J.; Hardisty, L.I.; Hageman, J.L.; Stockman, H.A.; Borchardt, J.D.; Gehrs, K.M.; et al. A common haplotype in the complement regulatory gene factor H (CFH) predisposes individuals to age-related macular degeneration. Proc. Natl. Acad. Sci. USA 2005, 102, 7227–7232. [Google Scholar] [CrossRef] [PubMed]
- Guymer, R.H.; Wu, Z.; Hodgson, L.A.B.; Caruso, E.; Brassington, K.H.; Tindill, N.; Aung, K.Z.; McGuinness, M.B.; Fletcher, E.L.; Chen, F.K.; et al. Subthreshold Nanosecond Laser Intervention in Age-Related Macular Degeneration: The LEAD Randomized Controlled Clinical Trial. Ophthalmology 2019, 126, 829–838. [Google Scholar] [CrossRef]
- van Kuijk, E.F.; Linkous, D.H.; Lengyel, I.; Frederickson, C.J.; Cano, K.E.; Jones, B.F.; Flinn, J.M. Trace Elements in Drusen. Investig. Ophthalmol. Vis. Sci. 2006, 47, 858. [Google Scholar]
- Aiello, F.; Gallo Afflitto, G.; Ceccarelli, F.; Cesareo, M.; Nucci, C. Global Prevalence of Fuchs Endothelial Corneal Dystro-phy in Adult Population: A Systematic Review and Meta Analysis. J. Ophthalmol. 2022, 2022, 3091695. [Google Scholar] [CrossRef]
- Li, W.; Qu, N.; Li, J.K.; Li, Y.X.; Han, D.M.; Chen, Y.X.; Tian, L.; Shao, K.; Yang, W.; Wang, Z.S.; et al. Evaluation of the Genetic Variation Spectrum Related to Corneal Dystrophy in a Large Cohort. Front. Cell Dev. Biol. 2021, 9, 632946. [Google Scholar] [CrossRef]
- Weiss, J.S.; Rapuano, C.J.; Seitz, B.; Busin, M.; Kivelä, T.T.; Bouheraoua, N.; Bredrup, C.; Nischal, K.K.; Chawla, H.; Borderie, V.; et al. IC3D Classification of Corneal Dystrophies—Edition 3. Cornea 2024, 43, 466–527. [Google Scholar] [CrossRef]
- Cho, E.H.; Lee, M.; Ki, C.-S.; Seol, C.A.; Jang, M.-A. Genetic epidemiology of epithelial-stromal TGFBI dystrophies in a large Korean population. Sci. Rep. 2025, 15, 25360. [Google Scholar] [CrossRef]
- Chan, C. Innovations in the Treatment of Corneal Dystrophies. Ophthalmology Times, 16 April 2023; Volume 48. [Google Scholar]
- Viola, P.; Neri, E.; Testa, V.; Parekh, M.; Cian, R.; Grassetto, A.; Romano, V. Clinical Outcomes of Preloaded Descemet Membrane Endothelial Keratoplasty with Endothelium Inward: A 24-Month Comparative Analysis Between Fuchs Endothelial Corneal Dystrophy and Bullous Keratopathy. Cornea 2023, 42, 1133–1139. [Google Scholar] [CrossRef]
- Akagi, Y.; Yamanaka, A.; Ohmoto, Y.; Sato, H.; Tsubota, K. Histochemical detection of iron and other metals in granular and lattice corneal dystrophies. Br. J. Ophthalmol. 1998, 82, 697–701. [Google Scholar]
- Kaya, S.G.; Inanc-Surer, S.; Cakan-Akdogan, G.; Oktay, G.; Utine, C.A.; Kalyoncu, S. Roles of matrix metalloproteinases in the cornea: A special focus on macular corneal dystrophy. Medicine in Drug Discovery 2021, 11, 100095. [Google Scholar] [CrossRef]
- Wojcik, K.A.; Kaminska, A.; Blasiak, J.; Szaflik, J.; Szaflik, J.P. Oxidative Stress in the Pathogenesis of Keratoconus and Fuchs En-dothelial Corneal Dystrophy. Int. J. Mol. Sci. 2013, 14, 19294–19308. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wu, W.; Wang, Z.; Zhai, C.; Deng, B.; Alzogool, M.; Wang, Y. Novel Corneal Protein Biomarker Candidates Reveal Iron Metabolic Disturbance in High Myopia Eyes. Front. Cell Dev. Biol. 2021, 9, 689917. [Google Scholar] [CrossRef]
- Seitz, B.; Behrens, A.; Fischer, M.; Langenbucher, A.; Naumann, G.O. Morphometric Analysis of Deposits in Granular and Lattice Corneal Dystrophy: Histopathologic Implications for Phototherapeutic Keratectomy. Cornea 2004, 23, 380–385. [Google Scholar] [CrossRef]
- Behndig, A.; Karlsson, K.; Johansson, B.O.; Brännström, T.; Marklund, S.L. Superoxide Dismutase Isoenzymes in the Normal and Diseased Human Cornea. Investig. Ophthalmol. Vis. Sci. 2001, 42, 2293–2296. [Google Scholar]
- Liu, L.; Wu, J.; Geng, J.; Yuan, Z.; Huang, D. Geographical prevalence and risk factors for pterygium: A systematic review and meta-analysis. BMJ Open 2013, 3, e003787. [Google Scholar] [CrossRef]
- Pan, Z.; Cui, J.; Shan, G.; Chou, Y.; Pan, L.; Sun, Z.; Cui, Z.; Sun, J.; Cao, Y.; Zhao, J.; et al. Prevalence and Risk Factors for Pterygium: A Cross-Sectional Study in Han and Manchu Ethnic Populations in Hebei, China. BMJ Open 2019, 9, e02572. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saw, S.M.; Tan, D. Pterygium: Prevalence, demography and risk factors. Ophthalmic Epidemiol. 1999, 6, 219–228. [Google Scholar] [CrossRef]
- Anguria, P.; Kitinya, J.; Ntuli, S.; Carmichael, T. The role of heredity in pterygium development. Int. J. Ophthalmol. 2014, 7, 532–537. [Google Scholar] [CrossRef]
- Altiparmak, U.E.; Katircioğlu, Y.A.; Yağci, R.; Yalniz, Z.; Duman, S. Mitomycin C and Conjunctival Autograft for Recurrent Pterygium. Int. Ophthalmol. 2007, 27, 339–343. [Google Scholar] [CrossRef]
- Better Health Channel. Pterygium: Prevention May Include Wearing UV-Protecting Sunglasses and a Hat in Areas with Strong Sunlight. Department of Health, State Government of Victoria, Australia; 2024. Available online: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pterygium (accessed on 3 July 2025).
- Namuslu, M.; Balci, M.; Coşkun, M.; Yağci, R.; Cimen, B.; Çetin, A.; Ayyildiz, A.; Erdamar, H.; Yiğitoğlu, R. Investigation of trace elements in pterygium tissue. Curr. Eye Res. 2013, 38, 526–530. [Google Scholar] [CrossRef]
- Gupta, P.D.; Johar, K.; Nagpal, K.; Vasavada, A.R. Causative and preventive action of calcium in cataractogenesis. Acta Phar-macol. Sin. 2004, 25, 1250–1256. [Google Scholar]
- Minogue, P.J.; Rodriguez, S.H.; Berthoud, V.M.; Beyer, E.C. Pediatric cataracts of different etiologies contain insoluble, calcified particles. Front. Ophthalmol. 2023, 3, 1213359. [Google Scholar] [CrossRef] [PubMed]
- Langford-Smith, A.; Tilakaratna, V.; Lythgoe, P.R.; Clark, S.J.; Bishop, P.N.; Day, A.J. Age and Smoking Related Changes in Metal Ion Levels in Human Lens: Implications for Cataract Formation. PLoS ONE 2016, 11, e0147576. [Google Scholar] [CrossRef] [PubMed]
- Zawadzka, I.; Młynarczyk, M.; Falkowska, M.; Socha, K.; Konopińska, J. Dietary Patterns; Serum Concentrations of Selenium, Copper, and Zinc; Copper/Zinc Ratio; and Total Antioxidant Status in Patients with Glaucoma. PLoS ONE 2024, 19, e0301511. [Google Scholar] [CrossRef]
- Kamińska, A.; Romano, G.L.; Rejdak, R.; Zweifel, S.; Fiedorowicz, M.; Rejdak, M.; Bajka, A.; Amato, R.; Bucolo, C.; Avitabile, T.; et al. Influence of Trace Elements on Neurodegenerative Diseases of The Eye-The Glaucoma Model. Int. J. Mol. Sci. 2021, 22, 4323. [Google Scholar] [CrossRef]
- Francis, B.A.; Du, L.T.; Najafi, K.; Murthy, R.; Kurumety, U.; Rao, N.; Minckler, D.S. Histopathologic Features of Conjunctival Filtering Blebs. Arch. Ophthalmol. 2005, 123, 166–170. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Balbaba, M.; Ulaş, F.; Erdağ, M.; Yıldırım, H.; Çeliker, Ü.; Aydın, S. Evaluation of Aqueous Humor and Serum Cortistatin Levels in Diabetic Patients with and without Diabetic Retinopathy. Eur. J. Ophthalmol. 2021, 31, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Bleich, S.; Roedl, J.; Von Ahsen, N.; Schlötzer-Schrehardt, U.; Reulbach, U.; Beck, G.; Kruse, F.E.; Naumann, G.O.; Kornhuber, J.; Jünemann, A.G. Elevated Homocysteine Levels in Aqueous Humor of Patients with Pseudoexfoliation Glaucoma. Am. J. Ophthalmol. 2004, 138, 162–164. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Jung, J.H.; Park, T.K.; Moon, C.E.; Han, K.; Lee, J.; Lee, H.K.; Ji, Y.W.; Kim, C.Y. Proteome alterations in the aqueous humor reflect structural and functional phenotypes in patients with advanced normal-tension glaucoma. Sci. Rep. 2022, 12, 1221. [Google Scholar] [CrossRef] [PubMed]
- Hartness, E.M.; Shevalye, H.; Skeie, J.M.; Eggleston, T.; Field, M.G.; Schmidt, G.A.; Phruttiwanichakun, P.; Salem, A.K.; Greiner, M.A. Iron-Sulfur Clusters and Iron Responsive Element Binding Proteins Mediate Iron Accumulation in Corneal Endothelial Cells in Fuchs Dystrophy. Investig. Ophthalmol. Vis. Sci. 2025, 66, 23. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.; Clay, S.M.; Oldenburg, C.E.; Rose-Nussbaumer, J.; Hwang, D.G.; Chan, M.F. Overexpression of MMPs in Corneas Requiring Penetrating and Deep Anterior Lamellar Keratoplasty. Investig. Ophthalmol. Vis. Sci. 2019, 60, 1734–1747. [Google Scholar] [CrossRef] [PubMed]
- Harding, J.J. Cataract: Biochemistry, Epidemiology and Pharmacology, 1st ed.; Springer: Dordrecht, The Netherlands, 1991; X+334p, ISBN 978-0412360503. [Google Scholar]
- Kushwah, N.; Bora, K.; Maurya, M.; Pavlovich, M.C.; Chen, J. Oxidative Stress and Antioxidants in Age-Related Macular Degeneration. Antioxidants 2023, 12, 1379. [Google Scholar] [CrossRef]
- Ekici, F.; Korkmaz, Ş.; Karaca, E.E.; Sül, S.; Tufan, H.A.; Aydın, B.; Dileköz, E. The Role of Magnesium in the Pathogenesis and Treatment of Glaucoma. Int. Sch. Res. Not. 2014, 2014, 745439. [Google Scholar] [CrossRef]
- Duarte, J.N. Neuroinflammatory Mechanisms of Mitochondrial Dysfunction and Neurodegeneration in Glaucoma. J. Ophthalmol. 2021, 2021, 4581909. [Google Scholar] [CrossRef]
- Ghaffarieh, A.; Ciolino, J.B. Potential of Application of Iron Chelating Agents in Ophthalmic Diseases. Semin. Ophthalmol. 2021, 36, 157–161. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Melachuri, S.; Lim, C.C.; Winters, J. Optic neuropathy in iron overload and iron chelation therapy. Am. J. Hematol. 2022, 97, 670–672. [Google Scholar] [CrossRef]
- He, E.; Feng, Y.; Xiang, W.; Lin, Z.; Li, Y.; Hu, W.; Liu, K.; Tao, S.; Shu, Q.; Wang, J.; et al. Ferroptosis Contributes to Retinal Ganglion Cell Loss in GLAST Knockout Mouse Model of Normal Tension Glaucoma. Investig. Ophthalmol. Vis. Sci. 2025, 66, 26. [Google Scholar] [CrossRef]
- Kowluru, R.A.; Chan, P.S. Oxidative stress and diabetic retinopathy. J. Diabetes Res. 2007, 2007, 43603. [Google Scholar] [CrossRef]
- Duh, E.J.; Sun, J.K.; Stitt, A.W. Diabetic retinopathy: Current understanding, mechanisms, and treatment strategies. JCI Insight 2017, 2, e93751. [Google Scholar] [CrossRef]
- Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supple-mentation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch. Ophthalmol. 2001, 119, 1417–1436. [Google Scholar] [CrossRef]
- Vishwanathan, R.; Chung, M.; Johnson, E.J. A Systematic Review on Zinc for the Prevention and Treatment of Age-Related Macular Degeneration. Investig. Ophthalmol. Vis. Sci. 2013, 54, 3985–3998. [Google Scholar] [CrossRef] [PubMed]
- Buonfiglio, F.; Korb, C.A.; Stoffelns, B.; Pfeiffer, N.; Gericke, A. Recent Advances in Our Understanding of Age-Related Macular Degeneration: Mitochondrial Dysfunction, Redox Signaling, and the Complement System. Aging Dis. 2024, 16, 1535–1575. [Google Scholar] [CrossRef] [PubMed]
- Combs, J.A.; Norton, E.B.; Saifudeen, Z.R.; Bentrup, K.H.Z.; Katakam, P.V.; Morris, C.A.; Myers, L.; Kaur, A.; Sullivan, D.E.; Zwezdaryk, K.J. Human Cytomegalovirus Alters Host Cell Mitochondrial Function during Acute Infection. J. Virol. 2020, 94, e01183-19. [Google Scholar] [CrossRef] [PubMed]
- Ramkumar, H.L.; Zhang, J.; Chan, C.C. Retinal ultrastructure of murine models of dry age-related macular degeneration (AMD). Prog. Retin. Eye Res. 2010, 29, 169–190. [Google Scholar] [CrossRef]
- Di Girolamo, N.; Wakefield, D.; Coroneo, M.T. UVB-Mediated Induction of Cytokines and Growth Factors in Pterygium Epithelial Cells Involves Cell Surface Receptors and Intracellular Signaling. Investig. Ophthalmol. Vis. Sci. 2006, 47, 2430–2437. [Google Scholar] [CrossRef]
- Chui, J.; Di Girolamo, N.; Wakefield, D.; Coroneo, M.T. The pathogenesis of pterygium: Current concepts and their thera-peutic implications. Ocul. Surf. 2008, 6, 24–43. [Google Scholar] [CrossRef]
- Erie, J.C.; Good, J.A.; Butz, J.A.; Pulido, J.S. Reduced Zinc and Copper in the Retinal Pigment Epithelium and Choroid in Age-Related Macular Degeneration. Am. J. Ophthalmol. 2009, 147, 276–282.e1. [Google Scholar] [CrossRef]
- Li, M.; Gende, M.; Tovar, A.; Schmeling, M.; Tidow-Kebritchi, S.; Gaynes, B.I. Assessing Chronic Heavy Metal Exposure by Analysis of Human Cataract Specimens and the Relationship to Metabolic Profiles. Curr. Eye Res. 2025, 50, 264–275. [Google Scholar] [CrossRef]
- Di Girolamo, N.; Coroneo, M.T.; Wakefield, D. UVB-Elicited Induction of MMP-1 Expression in Human Ocular Surface Epithelial Cells Is Mediated through the ERK1/2 MAPK-Dependent Pathway. Investig. Ophthalmol. Vis. Sci. 2003, 44, 4705–4714. [Google Scholar] [CrossRef]
| Analytical Technique | Advantages | Limitations | Applications in Ocular Studies |
|---|---|---|---|
| ICP-MS (Inductively Coupled Plasma Mass Spectrometry) | High sensitivity (ppt level); multi-element detection; isotopic analysis possible | Expensive instrumentation; complex sample prep; potential contamination | Widely used for aqueous humor, lens, and retina; enables trace metal profiling |
| AAS (Atomic Absorption Spectroscopy) | Relatively simple and cost-effective; good for single-element quantification | Low throughput; less sensitive than ICP-MS; cannot do multi-element at once | Used in postmortem retina and optic nerve studies (e.g., Al, Fe, Zn levels) |
| TXRF (Total Reflection X-ray Fluorescence) | Minimal sample prep; simultaneous multi-element detection; non-destructive | Lower sensitivity than ICP-MS; matrix effects can interfere | Applied in conjunctival tissue (e.g., Cr, Zn, Se in pterygium) |
| LA-ICP-MS (Laser Ablation ICP-MS) | Enables spatial mapping of elements; minimal sample digestion | Requires solid samples; calibration challenges; semi-quantitative | Used for retina and cornea to map metal distribution (e.g., Fe in AMD) |
| Decade | Milestone/Advancement | Notes | Key References |
|---|---|---|---|
| 1970s | Early trace metal studies in the eye | Atomic absorption spectroscopy (AAS) used to quantify basic elements (e.g., Cu, Zn) in cataractous lenses. | [9,10] |
| 1980s | Postmortem lens and retina analysis expands | Focus on Fe and Al in senile and diabetic retinopathy tissues. | [11] |
| 1990s | Introduction of ICP-AES and ICP-MS | Higher sensitivity and multielement capability applied to aqueous humor and vitreous samples. | [12,13] |
| 2000s | Laser Ablation ICP-MS (LA-ICP-MS) | Enabled spatial elemental mapping in cornea, retina, and lens tissue sections. | [14,15] |
| 2010s | SR-XRF applications | Synchrotron Radiation X-ray Fluorescence (SR-XRF) and microbeam XRF used to visualize metal distribution in ocular tissues at cellular resolution. | [16] |
| 2020s | Integrated multi-omics and biometal imaging | Studies correlate metallomics with genomics and proteomics; non-invasive sampling explored (e.g., tears). | [17,18] |
| Disease | Part of the Eye | Concentrations of Elements | Ref. | |
|---|---|---|---|---|
| Increase | Decrease | |||
| Cataracts | Lens | Ca, Zn, Cu, Cd, Al, V, Fe, Cr, Mn, Ba | Mg | [22,67,68,69,70,71,72,75,76,77,78,79,81,83] |
| Aqueous humor | P *, Ni, Ca, Cs, K, Mg, Na, P, Rb, Tl, Te, Pb, Al | ND | [22,82,83] | |
| Glaucoma | Lens | Fe, Ni | Cr, Al, Mn | [105,106,109,110,111] |
| Aqueous humor | Cu, Zn, Fe, Hg | Fe | ||
| Conjunctival stroma | Ca | ND | ||
| Diabetic retinopathy | Lens | Cu | ND | [128,129] |
| Aqueous humor | P, Ca, Cl | Na | ||
| Macular degeneration | Aqueous humor | Cd, Co, Fe, Zn | ND | [138] |
| Pterygium | Pterygium conjunctiva | ND | Cr, Mn, Zn, Se | [168] |
| Study/Author(s) | Sample Source | Tissue Analyzed | Analytical Method | Key Findings |
|---|---|---|---|---|
| [9] | Cataract surgery (lens) | Lens | ICP-OES | ↑ Ca, Cu, Zn in cataractous lenses |
| [180] | Cataract surgery (lens) | Lens | ICP-MS | ↓ Mg, ↑ Ca in nuclear cataracts |
| [181] | Postmortem (retina) | Retina | SR-XRF | ↑ Zn, Cu in AMD retinas |
| [105] | Postmortem (retina) | Retina | LA-ICP-MS | ↑ Fe in AMD retinas (LA-ICP-MS mapping) |
| [182] | Aqueous humor (AMD patients) | Aqueous Humor | ICP-MS | ↑ Fe, Cd, Cu, Zn in AMD; oxidative damage |
| [16] | Conjunctival tissue (pterygium excision) | Conjunctiva | TXRF | ↓ Cr, Mn, Zn, Se in pterygium |
| [15] | Corneal stroma (keratoconus surgery) | Cornea | LA-ICP-MS | ↑ Fe in anterior corneal stroma |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forma, A.; Torbicz, A.; Teresiński, G.; Maciejewski, R.; Baj, J. Metallomic Profiling of the Human Eye and Its Relevance to Ophthalmic Diseases. Appl. Sci. 2025, 15, 8934. https://doi.org/10.3390/app15168934
Forma A, Torbicz A, Teresiński G, Maciejewski R, Baj J. Metallomic Profiling of the Human Eye and Its Relevance to Ophthalmic Diseases. Applied Sciences. 2025; 15(16):8934. https://doi.org/10.3390/app15168934
Chicago/Turabian StyleForma, Alicja, Andrzej Torbicz, Grzegorz Teresiński, Ryszard Maciejewski, and Jacek Baj. 2025. "Metallomic Profiling of the Human Eye and Its Relevance to Ophthalmic Diseases" Applied Sciences 15, no. 16: 8934. https://doi.org/10.3390/app15168934
APA StyleForma, A., Torbicz, A., Teresiński, G., Maciejewski, R., & Baj, J. (2025). Metallomic Profiling of the Human Eye and Its Relevance to Ophthalmic Diseases. Applied Sciences, 15(16), 8934. https://doi.org/10.3390/app15168934






