Association Between Pain Distribution and Limitations in Basic and Instrumental Activities of Daily Living: A Cross-Sectional Study Based on the Survey of Health, Aging and Retirement in Europe on the Influence of Biopsychosocial Variables and Lifestyle
Abstract
Featured Application
Abstract
1. Introduction
- To analyze the associations between reporting more than one limitation in ADLs, both basic and instrumental, the presence of pain, and the extent of its distribution (LP vs. WP), in a population of retired, middle-aged, and older European adults. Additionally, to compare the proportions of individuals with more than one limitation in BADLs and IADLs according to pain presence and its distribution.
- To assess the number of limitations in BADLs and IADLs among retired, middle-aged, and older European adults based on the presence or absence of pain and its distribution (LP vs. WP).
- To identify, among sociodemographic, lifestyle, and biopsychosocial variables, the factors associated with the number of limitations through a Poisson regression model.
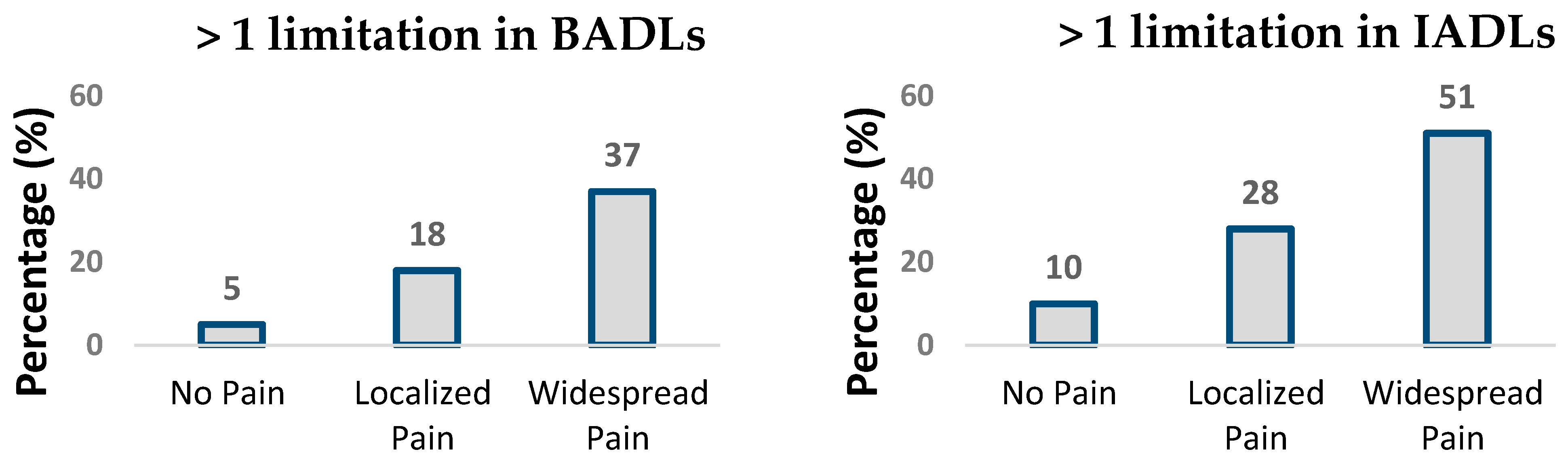
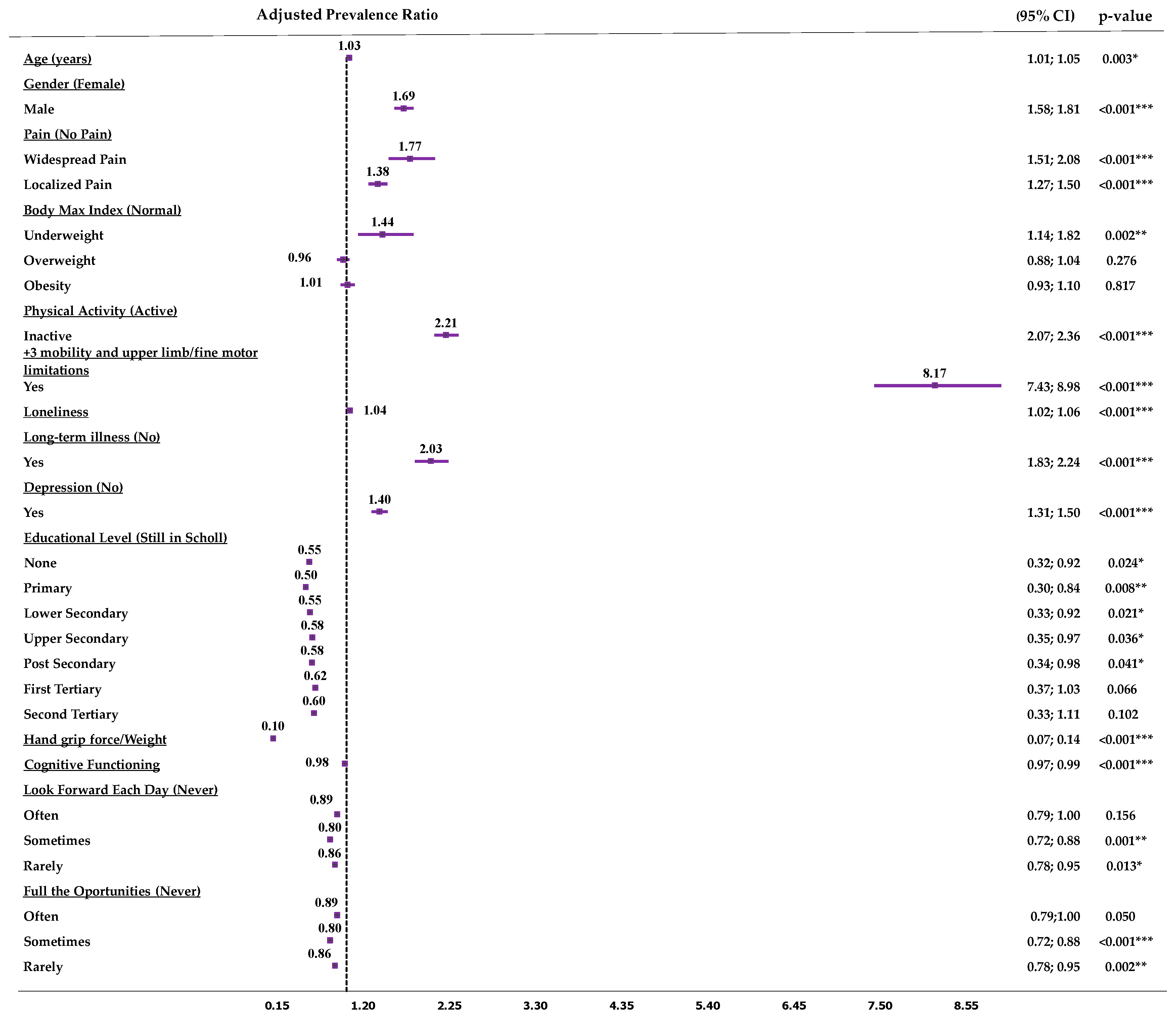
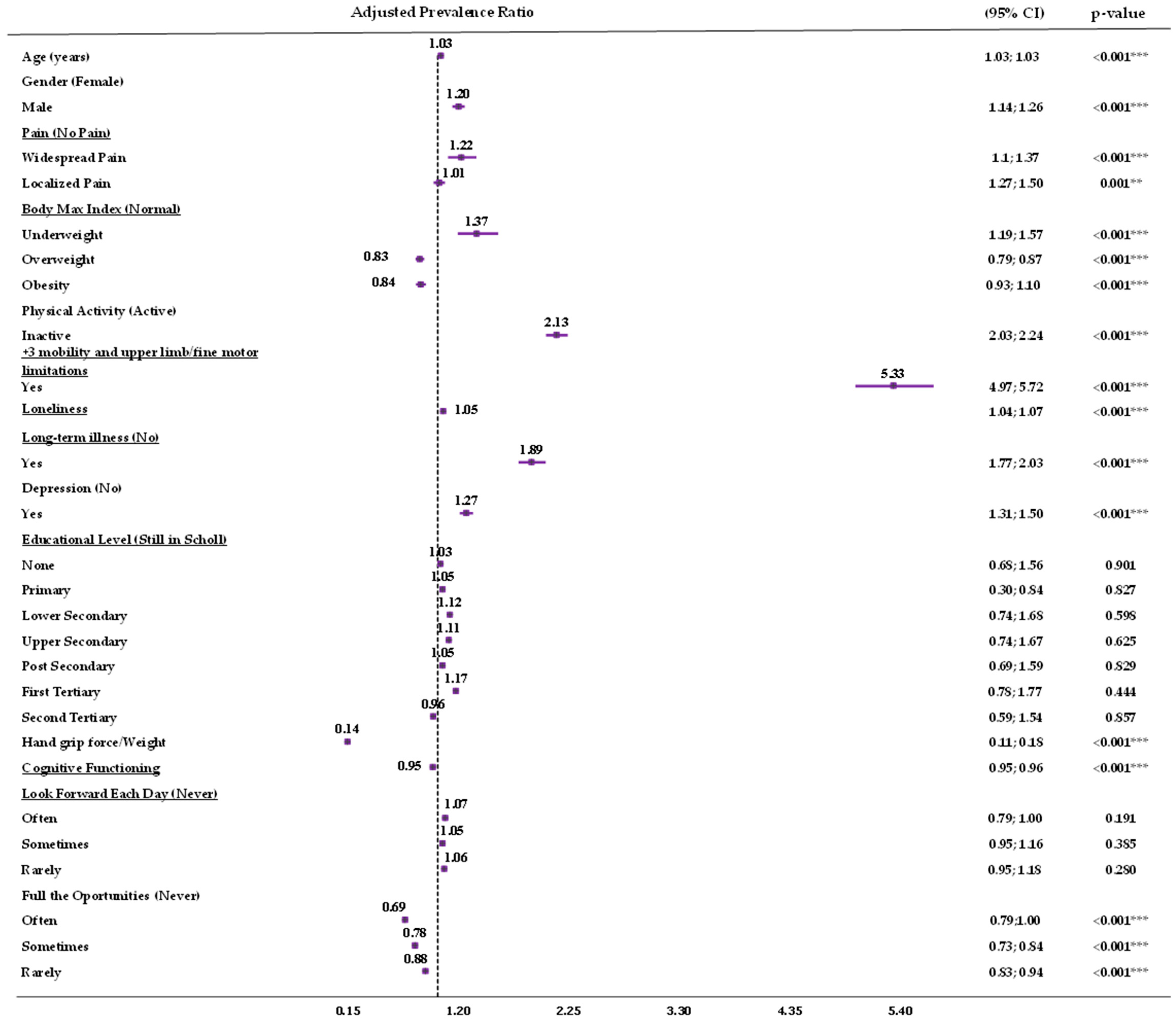
- In middle-aged and older retired Europeans, pain and its spread (LP vs. WP) are associated with the presence of more than one limitation in BADLs and IADLs.
- People with pain have a greater number of limitations in BADLs and IADLs than people without pain, with those with WP having the greatest number of limitations.
- Mobility limitations, long-term illnesses, and physical inactivity are the main factors associated with a greater number of limitations in ADLs and IADLs. Conversely, greater relative HGS is the main factor associated with fewer limitations.
2. Materials and Methods
2.1. Study Design, Data Collection, and Procedures
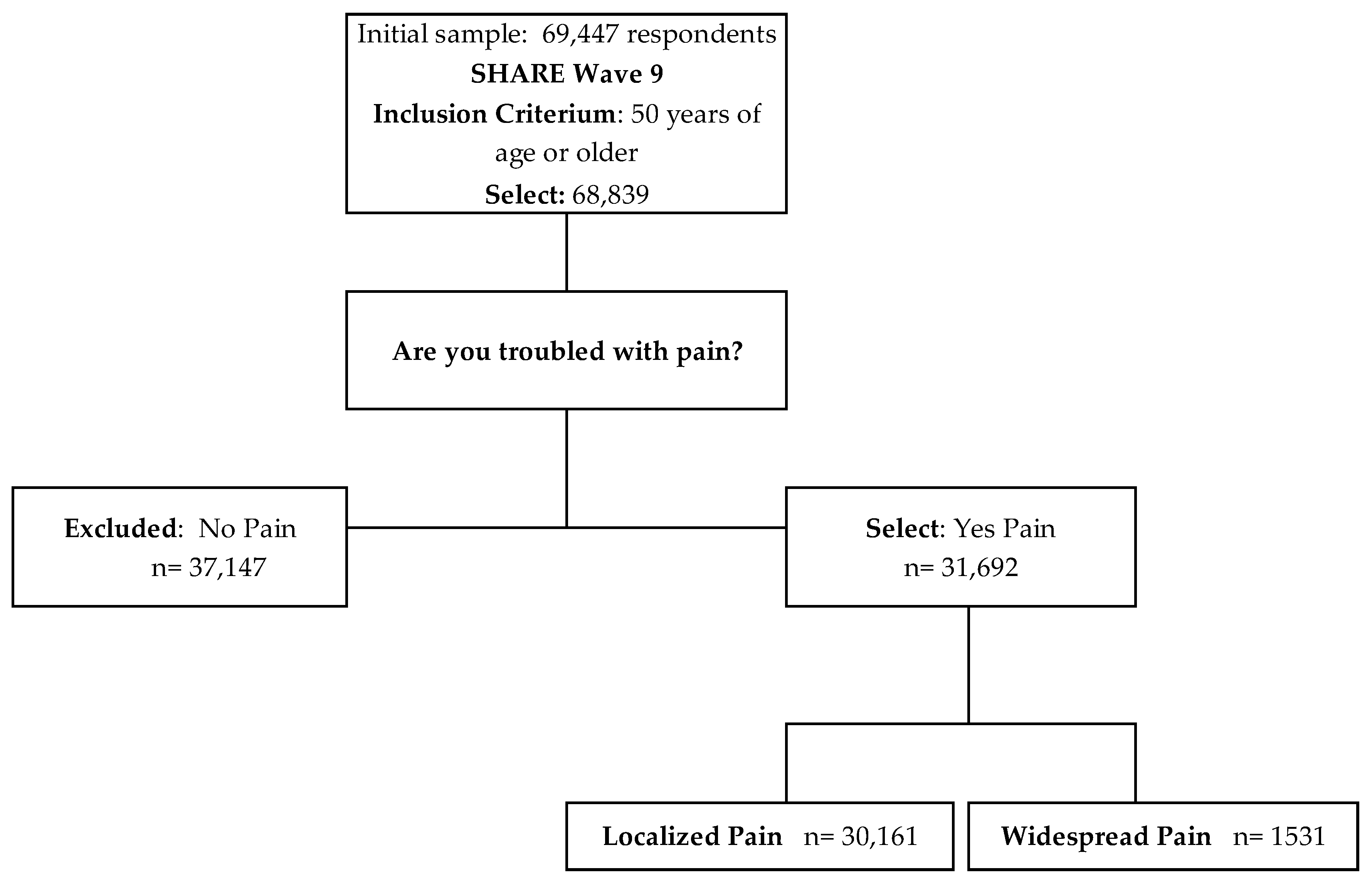
2.2. Sample
2.3. Grouping Criteria
2.4. Variables
2.4.1. Characterization Variables
2.4.2. Dependent Variables
2.5. Statistical Analysis
2.6. GenAI Declaration
3. Results
3.1. Descriptive Analysis
3.2. Pain Status and Basic Activities of Daily Living
3.3. Multiple Regression Models
3.3.1. Multivariate Poisson Regression Model of Limitations in Basic Activities of Daily Living
3.3.2. Multivariate Poisson Regression Model of Limitations in Instrumental Activities of Daily Living
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SHARE | The Survey of Health, Aging, and Retirement in Europe |
| OTFP-4 | Occupational Therapy Practice Framework (version 4) |
| ADLs | Activities of Daily Living |
| BADLs | Basic Activities of Daily Living |
| IADLs | Instrumental Activities of Daily Living |
| LP | Localized Pain |
| WP | Widespread Pain |
| HGS | Handgrip Strength |
References
- World Health Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 23 June 2025).
- Jones, C.H.; Dolsten, M. Healthcare on the Brink: Navigating the Challenges of an Aging Society in the United States. NPJ Aging 2024, 10, 22. [Google Scholar] [CrossRef] [PubMed]
- Kallestrup-Lamb, M.; Marin, A.O.K.; Menon, S.; Søgaard, J. Aging Populations and Expenditures on Health. J. Econ. Ageing 2024, 29, 100518. [Google Scholar] [CrossRef]
- Salive, M.E. Multimorbidity in Older Adults. Epidemiol. Rev. 2013, 35, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Ćwirlej-Sozańska, A.; Wiśniowska-Szurlej, A.; Wilmowska-Pietruszyńska, A.; Sozański, B. Determinants of ADL and IADL Disability in Older Adults in Southeastern Poland. BMC Geriatr. 2019, 19, 297. [Google Scholar] [CrossRef] [PubMed]
- Amuthavalli Thiyagarajan, J.; Mikton, C.; Harwood, R.H.; Gichu, M.; Gaigbe-Togbe, V.; Jhamba, T.; Pokorna, D.; Stoevska, V.; Hada, R.; Steffan, G.S.; et al. The UN Decade of Healthy Ageing: Strengthening Measurement for Monitoring Health and Wellbeing of Older People. Age Ageing 2022, 51, afac147. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo, M.; Merchant, R.A.; Morley, J.E.; Anker, S.D.; Aprahamian, I.; Arai, H.; Aubertin-Leheudre, M.; Bernabei, R.; Cadore, E.L.; Cesari, M.; et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. J. Nutr. Health Aging 2021, 25, 824–853. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- American Occupational Therapy Association. Occupational Therapy Practice Framework: Domain and Process—Fourth Edition. Am. J. Occup. Ther. 2020, 74, 7412410010p1–7412410010p87. [Google Scholar] [CrossRef] [PubMed]
- Balicki, P.; Sołtysik, B.K.; Borowiak, E.; Kostka, T.; Kostka, J. Activities of Daily Living Limitations in Relation to the Presence of Pain in Community-Dwelling Older Adults. Sci. Rep. 2025, 15, 15027. [Google Scholar] [CrossRef] [PubMed]
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.J.; Mogil, J.S.; Ringkamp, M.; Sluka, K.A.; et al. The Revised International Association for the Study of Pain Definition of Pain: Concepts, Challenges, and Compromises. Pain 2020, 161, 1976–1982. [Google Scholar] [CrossRef] [PubMed]
- Schofield, P.; Abdulla, A. Pain Assessment in the Older Population: What the Literature Says. Age Ageing 2018, 47, 324–327. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sánchez, I.; García-Esquinas, E.; Mesas, A.E.; Martín-Moreno, J.M.; Rodríguez-Mañas, L.; Rodríguez-Artalejo, F. Frequency, Intensity and Localization of Pain as Risk Factors for Frailty in Older Adults. Age Ageing 2019, 48, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Butera, K.A.; Roff, S.R.; Buford, T.W.; Cruz-Almeida, Y. The Impact of Multisite Pain on Functional Outcomes in Older Adults: Biopsychosocial Considerations. J. Pain Res. 2019, 12, 1115–1125. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.-W.; Kim, C.-W.; Jang, Y.-J.; Lee, C.-H.; Oh, M.-K.; Kim, K.-W.; Jang, H.-C.; Lim, J.-Y.; Chun, S.-W.; Lim, S.-K. Musculoskeletal Pain, Physical Activity, Muscle Mass, and Mortality in Older Adults: Results from the Korean Longitudinal Study on Health and Aging (KLoSHA). Medicina 2024, 60, 462. [Google Scholar] [CrossRef] [PubMed]
- Mcgrath, R.P.; Vincent, B.M.; Lee, I.-M.; Kraemer, W.J.; Peterson, M.D. Handgrip Strength, Function, and Mortality in Older Adults: A Time-Varying Approach. Med. Sci. Sports Exerc. 2018, 50, 2259–2266. [Google Scholar] [CrossRef] [PubMed]
- Vaishya, R.; Misra, A.; Vaish, A.; Ursino, N.; D’Ambrosi, R. Hand Grip Strength as a Proposed New Vital Sign of Health: A Narrative Review of Evidences. J. Health Popul. Nutr. 2024, 43, 7. [Google Scholar] [CrossRef] [PubMed]
- Pontes, V.D.C.B.; Santos, J.L.F.; Santos-Vilar, L.A.D.; Ferriolli, E. Handgrip Strength Predicts Disability in Older Emergency Department Patients: A Prospective Cohort Study. Geriatr. Gerontol. Aging 2024, 18, e0000142. [Google Scholar] [CrossRef]
- Ogliari, G.; Ryg, J.; Andersen-Ranberg, K.; Scheel-Hincke, L.L.; Collins, J.T.; Cowley, A.; Di Lorito, C.; Booth, V.; Smit, R.A.J.; Akyea, R.K.; et al. Association between Pain Intensity and Depressive Symptoms in Community-Dwelling Adults: Longitudinal Findings from the Survey of Health, Ageing and Retirement in Europe (SHARE). Eur. Geriatr. Med. 2023, 14, 1111–1124. [Google Scholar] [CrossRef] [PubMed]
- Emerson, K.; Boggero, I.; Ostir, G.; Jayawardhana, J. Pain as a Risk Factor for Loneliness Among Older Adults. J. Aging Health 2018, 30, 1450–1461. [Google Scholar] [CrossRef] [PubMed]
- Bloomberg, M.; Bu, F.; Fancourt, D.; Steptoe, A. Trajectories of Loneliness, Social Isolation, and Depressive Symptoms before and after Onset of Pain in Middle-Aged and Older Adults. eClinicalMedicine 2025, 84, 103209. [Google Scholar] [CrossRef]
- Judge, S.T.; Clasey, J.L.; Crofford, L.J.; Segerstrom, S.C. Optimism and Pain Interference in Aging Women. Ann. Behav. Med. 2019, 54, 202–212. [Google Scholar] [CrossRef] [PubMed]
- Rivera, L.C.; Mancilla, I.A.; Bergstrom, J.; Thompson, S.; Molina, A.J. Relationships Between Self-Reported Pain and Optimism Among Community-Dwelling Older Adults. Int. J. Aging Hum. Dev. 2024, 99, 494–504. [Google Scholar] [CrossRef] [PubMed]
- Bell, T.R.; Sprague, B.N.; Ross, L.A. Longitudinal Associations of Pain and Cognitive Decline in Community-Dwelling Older Adults. Psychol. Aging 2022, 37, 715–730. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, M.; Börsch-Supan, A. SHARE Wave 8 Methodology: Collecting Cross-National Survey Data in Times of COVID-19; Munich Center for the Economics of Aging (MEA): Munich, Germany, 2021; ISBN 978-3-00-069877-4. [Google Scholar]
- Organisation for Economic Co-operation and Development. For E.C. and Classifying Educational Programmes—Manual for ISCED-97 Implementation in OECD Countries—1999 Edition; Organisation for Economic Co-operation and Development: Paris, France, 1999. [Google Scholar]
- Mohd Hairi, F.; Mackenbach, J.P.; Andersen-Ranberg, K.; Avendano, M. Does Socio-Economic Status Predict Grip Strength in Older Europeans? Results from the SHARE Study in Non-Institutionalised Men and Women Aged 50+. J. Epidemiol. Community Health 2010, 64, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Ogliari, G.; Ryg, J.; Andersen-Ranberg, K.; Scheel-Hincke, L.L.; Masud, T. Perceived Neighbourhood Environment and Falls among Community-Dwelling Adults: Cross-Sectional and Prospective Findings from the Survey of Health, Ageing and Retirement in Europe (SHARE). Eur. J. Ageing 2022, 19, 1121–1134. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.J.; Reischies, F.; Beekman, A.T.F.; Fuhrer, R.; Jonker, C.; Kivela, S.-L.; Lawlor, B.A.; Lobo, A.; Magnusson, H.; Fichter, M.; et al. Development of the EURO–D Scale—A European Union Initiative to Compare Symptoms of Depression in 14 European Centres. Br. J. Psychiatry 1999, 174, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Guerra, M.; Ferri, C.; Llibre, J.; Prina, A.M.; Prince, M. Psychometric Properties of EURO-D, a Geriatric Depression Scale: A Cross-Cultural Validation Study. BMC Psychiatry 2015, 15, 12. [Google Scholar] [CrossRef] [PubMed]
- Tomás, J.M.; Torres, Z.; Oliver, A.; Enrique, S.; Fernández, I. Psychometric Properties of the EURO-D Scale of Depressive Symptomatology: Evidence from SHARE Wave 8. J. Affect. Disord. 2022, 313, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Maskileyson, D.; Seddig, D.; Davidov, E. The EURO-D Measure of Depressive Symptoms in the Aging Population: Comparability Across European Countries and Israel. Front. Polit. Sci. 2021, 3, 665004. [Google Scholar] [CrossRef]
- Castro-Costa, E.; Dewey, M.; Stewart, R.; Banerjee, S.; Huppert, F.; Mendonca-Lima, C.; Bula, C.; Reisches, F.; Wancata, J.; Ritchie, K.; et al. Prevalence of Depressive Symptoms and Syndromes in Later Life in Ten European Countries: The SHARE Study. Br. J. Psychiatry 2007, 191, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Trucharte, A.; Calderón, L.; Cerezo, E.; Contreras, A.; Peinado, V.; Valiente, C. Three-Item Loneliness Scale: Psychometric Properties and Normative Data of the Spanish Version. Curr. Psychol. 2023, 42, 7466–7474. [Google Scholar] [CrossRef] [PubMed]
- Daniel, F.; Espírito-Santo, H.; Lemos, L.; Guadalupe, S.; Barroso, I.; Gomes Da Silva, A.; Ferreira, P.L. Measuring Loneliness: Psychometric Properties of the Three-Item Loneliness Scale among Community-Dwelling Adults. Heliyon 2023, 9, e15948. [Google Scholar] [CrossRef] [PubMed]
- Katz, S. Studies of Illness in the Aged: The Index of ADL: A Standardized Measure of Biological and Psychosocial Function. JAMA 1963, 185, 914. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Plantinga, L.C.; Bowling, C.B.; Pearce, B.D.; Hoge, C.; Dunlop-Thomas, C.; Lim, S.S.; Katz, P.P.; Yazdany, J. Limitations in Activities of Daily Living Among Individuals with Systemic Lupus Erythematosus. Arthritis Care Res. 2025, 77, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Lozano, M.; Mundo-López, A.; San-Sebastian, A.P.; Galiano-Castillo, N.; Fernandez-Lao, C.; Cantarero-Villanueva, I.; Arroyo-Morales, M.; Ocón-Hernández, O.; Artacho-Cordón, F. Limitations in Activities of Daily Living Among Spanish Women Diagnosed with Endometriosis. Am. J. Occup. Ther. 2021, 75, 7506205050. [Google Scholar] [CrossRef] [PubMed]
- Powell, V.D.; Abedini, N.C.; Galecki, A.T.; Kabeto, M.; Kumar, N.; Silveira, M.J. Unwelcome Companions: Loneliness Associates with the Cluster of Pain, Fatigue, and Depression in Older Adults. Gerontol. Geriatr. Med. 2021, 7, 2333721421997620. [Google Scholar] [CrossRef] [PubMed]
- Nicolson, P.J.A.; Williamson, E.; Morris, A.; Sanchez-Santos, M.T.; Bruce, J.; Silman, A.; Lamb, S.E. Musculoskeletal Pain and Loneliness, Social Support and Social Engagement among Older Adults: Analysis of the Oxford Pain, Activity and Lifestyle Cohort. Musculoskelet. Care 2021, 19, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Fillingim, R.B.; King, C.D.; Ribeiro-Dasilva, M.C.; Rahim-Williams, B.; Riley, J.L. Sex, Gender, and Pain: A Review of Recent Clinical and Experimental Findings. J. Pain 2009, 10, 447–485. [Google Scholar] [CrossRef] [PubMed]
- Mills, S.E.E.; Nicolson, K.P.; Smith, B.H. Chronic Pain: A Review of Its Epidemiology and Associated Factors in Population-Based Studies. Br. J. Anaesth. 2019, 123, e273–e283. [Google Scholar] [CrossRef] [PubMed]
- Sorge, R.E.; Totsch, S.K. Sex Differences in Pain. J. Neurosci. Res. 2017, 95, 1271–1281. [Google Scholar] [CrossRef] [PubMed]
- McVinnie, D.S. Obesity and Pain. Br. J. Pain 2013, 7, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Tang, H.; Lin, J.; Zeng, R. Causal Relationships of Obesity on Musculoskeletal Chronic Pain: A Two-Sample Mendelian Randomization Study. Front. Endocrinol. 2022, 13, 971997. [Google Scholar] [CrossRef] [PubMed]
- Núñez-Cortés, R.; Cruz-Montecinos, C.; López-Bueno, R.; Andersen, L.L.; Calatayud, J. Physical Inactivity Is the Most Important Unhealthy Lifestyle Factor for Pain Severity in Older Adults with Pain: A SHARE-Based Analysis of 27,528 Cases from 28 Countries. Musculoskelet. Sci. Pract. 2025, 76, 103270. [Google Scholar] [CrossRef] [PubMed]
- Fanning, J.; Brooks, A.K.; Robison, J.T.; Irby, M.B.; Ford, S.; N’Dah, K.; Rejeski, W.J. Associations between Patterns of Physical Activity, Pain Intensity, and Interference among Older Adults with Chronic Pain: A Secondary Analysis of Two Randomized Controlled Trials. Front. Aging 2023, 4, 1216942. [Google Scholar] [CrossRef] [PubMed]
- Whitlock, E.L.; Diaz-Ramirez, L.G.; Glymour, M.M.; Boscardin, W.J.; Covinsky, K.E.; Smith, A.K. Association Between Persistent Pain and Memory Decline and Dementia in a Longitudinal Cohort of Elders. JAMA Intern. Med. 2017, 177, 1146–1153. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Li, G.; Chen, Z.; Hu, Z.; Wang, Q.; Huang, G.; Luo, Q. Trajectories of Pain and Their Associations with Long-Term Cognitive Decline in Older Adults: Evidence from Two Longitudinal Cohorts. Age Ageing 2024, 53, afae183. [Google Scholar] [CrossRef] [PubMed]
- IsHak, W.W.; Wen, R.Y.; Naghdechi, L.; Vanle, B.; Dang, J.; Knosp, M.; Dascal, J.; Marcia, L.; Gohar, Y.; Eskander, L.; et al. Pain and Depression: A Systematic Review. Harv. Rev. Psychiatry 2018, 26, 352–363. [Google Scholar] [CrossRef] [PubMed]
- Thompson, T.; Correll, C.U.; Gallop, K.; Vancampfort, D.; Stubbs, B. Is Pain Perception Altered in People with Depression? A Systematic Review and Meta-Analysis of Experimental Pain Research. J. Pain 2016, 17, 1257–1272. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Wu, J.; Bair, M.J.; Krebs, E.E.; Damush, T.M.; Tu, W. Reciprocal Relationship between Pain and Depression: A 12-Month Longitudinal Analysis in Primary Care. J. Pain 2011, 12, 964–973muhplalozan. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, T.; Rashid, M.; Zanwar, P.P. Examining the Association of Pain and Pain Frequency with Self-Reported Difficulty in Activities of Daily Living and Instrumental Activities of Daily Living Among Community-Dwelling Older Adults: Findings From the Longitudinal Aging Study in India. J. Gerontol. Ser. B 2023, 78, 1545–1554. [Google Scholar] [CrossRef] [PubMed]
- United Nations. In Proceedings of The United Nations Conference on Sustainable Development (UNCSD or “Rio+20”), Rio de Janeiro, Brazil, 20–22 June 2012. Available online: https://www.un.org/en/conferences/environment/rio2012 (accessed on 16 July 2025).
| Terminology Used in the SHARE Project | Correspondence with the Terminological Update Based on the OTPF-4 |
|---|---|
| Basic Activities of Daily Living | |
| Dressing, including putting on socks and shoes Walking across a room Bathing or showering Eating (e.g., cutting up food) Getting up or lying down Toileting (including sitting down and standing up) | Dressing Home mobility (functional mobility) Bathing, showering Eating Transferring (functional mobility) Toileting and toilet hygiene |
| Instrumental Activities of Daily Living | |
| Preparing a hot meal Shopping for groceries Making a phone call Taking medication Using a map to orient oneself in unfamiliar places Doing house or garden work Managing money (e.g., paying bills and keeping accounts) Using public transportation Doing laundry | Meal preparation Shopping Communication management Medication management * Driving and community mobility Housekeeping (home establishment and management) Financial management Using public transportation Doing laundry (home establishment and management) |
| No Pain | Localized Pain | Widespread Pain | |||||
|---|---|---|---|---|---|---|---|
| n (37,147) | n (30,161) | n (1531) | |||||
| Median | (IQR) | Median | (IQR) | Median | (IQR) | p-Value | |
| Age | 68 | (14) | 71 | (15) | 72 | (16) | <0.001 *** |
| Loneliness | 3 | (1) | 4 | (2) | 4 | (3) | <0.001 *** |
| Hand Grip Ratio (kg/Weight) | 0.4 | (0.2) | 0.4 | (0.2) | 0.3 | (0.2) | <0.001 *** |
| Cognitive Functioning | 18 | (6) | 17 | (6) | 16 | (8) | <0.001 *** |
| n | (%) | n | (%) | n | (%) | ||
| Sex | |||||||
| Men | 1762 | 48% | 11,243 | 37% | 453 | 30% | <0.001 *** |
| Female | 19,385 | 52% | 18,918 | 63% | 1078 | 70% | |
| Body Mass Index | |||||||
| Underweight | 420 | 1% | 391 | 1% | 44 | 3% | <0.001 *** |
| Normal | 13,144 | 37% | 8620 | 30% | 464 | 33% | |
| Overweight | 15,265 | 42% | 11,442 | 39% | 521 | 38% | |
| Obese | 7141 | 20% | 8642 | 29% | 363 | 26% | |
| Depression | |||||||
| No | 29,978 | 83% | 17,646 | 61% | 500 | 38% | <0.001 *** |
| Yes | 6028 | 17% | 11,355 | 39% | 810 | 62% | |
| Long-term illness | |||||||
| No | 22,619 | 61% | 8150 | 27% | 214 | 14% | <0.001 *** |
| Yes | 14,449 | 39% | 21,994 | 73% | 1313 | 86% | |
| +3 Mobility and upper limb/fine motor limitations | |||||||
| No | 32,676 | 88% | 16,482 | 55% | 496 | 33% | <0.001 *** |
| Yes | 4374 | 12% | 13,656 | 45% | 1027 | 67% | |
| Physical Activity | |||||||
| Inactive | 3473 | 9% | 5333 | 18% | 543 | 36% | <0.001 *** |
| Active | 33,592 | 91% | 24,794 | 82% | 979 | 64% | |
| Education level | |||||||
| None | 729 | 2% | 963 | 3% | 98 | 6% | <0.001 *** |
| Pre-primary | 3491 | 9% | 4398 | 15% | 350 | 23% | |
| Primary | 5211 | 14% | 5462 | 18% | 298 | 20% | |
| Lower secondary | 15,232 | 41% | 11,735 | 39% | 525 | 34% | |
| Upper secondary | 1912 | 5% | 1450 | 5% | 44 | 3% | |
| Post-secondary non-tertiary | 10,006 | 27% | 5838 | 19% | 198 | 13% | |
| First stage of tertiary education | 380 | 1% | 193 | 1% | 9 | 0% | |
| Still in school | 11 | 0% | 15 | 0% | 2 | 0% | |
| Dispositional optimism: | |||||||
| Look forward to each day | |||||||
| Often | 24,798 | 68% | 17,111 | 58% | 648 | 48% | <0.001 *** |
| Sometimes | 8273 | 23% | 8456 | 29% | 406 | 30% | |
| Rarely | 2348 | 7% | 2818 | 10% | 186 | 14% | |
| Never | 890 | 3% | 922 | 3% | 104 | 8% | |
| Full of opportunities | |||||||
| Often | 15,938 | 44% | 8298 | 28% | 308 | 23% | <0.001 *** |
| Sometimes | 13,984 | 39% | 11,845. | 41% | 487 | 36% | |
| Rarely | 5193 | 14% | 6974 | 24% | 342 | 26% | |
| Never | 1144 | 3% | 2147 | 7% | 208 | 16% | |
| Mdn | (IQR) | Mdn | (SD) | H | df | p-Value | Post Hoc U | p-Value | |
|---|---|---|---|---|---|---|---|---|---|
| Basic Activities of Daily Living Limitations | |||||||||
| No Pain (1) | 0 | (0.0) | 0.1 | (0.6) | 4569.4 | 2 | <0.001 | ||
| 1 vs. 2 | <0.001 *** | ||||||||
| Localized Pain (2) | 0 | (0.0) | 0.4 | (1.1) | 1 vs. 3 | <0.001 *** | |||
| 2 vs. 3 | <0.001 *** | ||||||||
| Widespread Pain (3) | 0 | (2.0) | 1.2 | (1.9) | |||||
| Instrumental Activities of Daily Living Limitations | |||||||||
| No Pain (1) | 0 | (0.0) | 0.3 | (1.3) | 3731.4 | 2 | <0.001 | ||
| 1 vs. 2 | <0.001 *** | ||||||||
| Localized Pain (2) | 0 | (1.0) | 0.8 | (1.8) | 1 vs. 3 | <0.001 *** | |||
| 2 vs. 3 | <0.001 *** | ||||||||
| Widespread Pain (3) | 1 | (4.0) | 2.2 | (3.0) | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salas-Gómez, D.; Denche-Zamorano, Á.; Mendoza-Holgado, C.; Barrios-Fernandez, S. Association Between Pain Distribution and Limitations in Basic and Instrumental Activities of Daily Living: A Cross-Sectional Study Based on the Survey of Health, Aging and Retirement in Europe on the Influence of Biopsychosocial Variables and Lifestyle. Appl. Sci. 2025, 15, 8026. https://doi.org/10.3390/app15148026
Salas-Gómez D, Denche-Zamorano Á, Mendoza-Holgado C, Barrios-Fernandez S. Association Between Pain Distribution and Limitations in Basic and Instrumental Activities of Daily Living: A Cross-Sectional Study Based on the Survey of Health, Aging and Retirement in Europe on the Influence of Biopsychosocial Variables and Lifestyle. Applied Sciences. 2025; 15(14):8026. https://doi.org/10.3390/app15148026
Chicago/Turabian StyleSalas-Gómez, Diana, Ángel Denche-Zamorano, Cristina Mendoza-Holgado, and Sabina Barrios-Fernandez. 2025. "Association Between Pain Distribution and Limitations in Basic and Instrumental Activities of Daily Living: A Cross-Sectional Study Based on the Survey of Health, Aging and Retirement in Europe on the Influence of Biopsychosocial Variables and Lifestyle" Applied Sciences 15, no. 14: 8026. https://doi.org/10.3390/app15148026
APA StyleSalas-Gómez, D., Denche-Zamorano, Á., Mendoza-Holgado, C., & Barrios-Fernandez, S. (2025). Association Between Pain Distribution and Limitations in Basic and Instrumental Activities of Daily Living: A Cross-Sectional Study Based on the Survey of Health, Aging and Retirement in Europe on the Influence of Biopsychosocial Variables and Lifestyle. Applied Sciences, 15(14), 8026. https://doi.org/10.3390/app15148026








