Abstract
Background: This study aimed to evaluate the long-term stability of maxillary molar distalization in the treatment of Class II malocclusion. Methods: This study included 40 patients (31 males and 9 females) who received fixed orthodontic treatment after maxillary molar distalization. Orthodontic models and lateral cephalograms were evaluated at three time points: pre-treatment (T1), after orthodontic treatment (T2), and long-term follow-up (T3). The mean ages of the patients’ ages at T1, T2, and T3 were 13.02, 15.97, and 22.05 years, respectively. The statistical analysis included paired t-tests and Wilcoxon signed-rank tests. The statistical significance was set at p < 0.05. Results: The statistical analysis indicated no gender-related differences. A significant distalization of maxillary first molars was observed at T2 compared to T1 (p < 0.001). Despite a minor relapse, a statistically significant distalization was observed in T3-T1 (p < 0.001). The vertical skeletal angles, which increased during the treatment period, decreased at T3-T2. The molar relationship was almost maintained after long-term follow-up (p < 0.001). Conclusions: The maxillary molar distalization achieved in the Class II treatment was maintained in the long term. The vertical skeletal measurements decreased to their initial values in the long term. The Class I molar relationship did not change during the completion of the growth. This study hypothesized that the maxillary molar distalization achieved during fixed orthodontic treatment can be maintained in the long term without significant relapse.
1. Introduction
Congenital tooth absence, early loss of primary teeth, and interproximal caries can lead to the mesial movement of the maxillary first molars, resulting in dental Class II malocclusions. There are several techniques for treating this anteroposterior discrepancy, which is certainly influenced by the patient’s etiology, growth pattern, age, levels of cooperation, and, most importantly, chief complaint [1]. Most orthodontists tend to prefer nonextraction treatment when clinically appropriate; moreover, some patients completely refuse tooth extraction regardless of clinical recommendations [2,3,4].
Distalization of the maxillary teeth up to the molar, canine, and incisor Class I relationship is the treatment for Class II malocclusion with no major skeletal involvement. This treatment does not involve any skeletal changes or modifications in the vertical dimension, nor does it affect the mandibular arch by distalizing the maxillary molars [5,6]. Both extraoral [7,8,9] and intraoral [10,11,12] appliances are utilized to distalize molar teeth. Generally, distalization appliances seem to correct Class II molar relationships primarily by dentoalveolar modifications rather than through maxillary growth inhibition [13,14].
Although mesial migration is a physiological phenomenon, this situation may imply a decrease in the long-term stability of molar distalization outcomes [15]. Because molar distalization involves movement in the opposite direction to physiological drift, long-term stability issues may arise. While a few studies [1,10,16,17,18] have evaluated the effects and short-term results of distalization, limited data exist regarding the long-term outcomes following comprehensive fixed orthodontic treatment [15,19,20,21].
The aim of this study was to evaluate the long-term stability of Class II malocclusion treatment achieved through maxillary molar distalization by using orthodontic models and lateral cephalometric radiographs. Our hypothesis was that the dentoalveolar corrections obtained through maxillary molar distalization followed by fixed orthodontic treatment would remain stable in the long term, and no significant relapse would occur.
2. Materials and Methods
In this retrospective study, patients who were treated with maxillary molar distalization and fixed orthodontic treatment at the Department of Orthodontics, Ataturk University, Faculty of Dentistry, with recordings in the archive were identified and called for control. Forty individuals (9 males, 31 females) with a mean age of 13.02 years were included in this study at the beginning of treatment. All patients presented with Class II molar relationships and had no history of systemic disease or previous orthodontic treatment. The data were collected from a single institution with standardized treatment protocols. A summary of the patient characteristics is provided in Table 1. This study was approved by the Research Ethics Committee of the Faculty of Dentistry, Atatürk University, with the approval code 01/2014, and the date of approval was 14 January 2014. An informed consent form was obtained from all participants who were included in this study. Lateral cephalometric films were obtained from these individuals using orthodontic models and a Gendex Orthoralix 9200 DDE, Gendex Dental Systems-KaVo Kerr Group, Des Plaines, IL, USA (76 kVp, 7 mA) device.

Table 1.
Chronological ages of patients.
The patient selection criteria were established based on the following parameters:
Inclusion Criteria:
- Skeletal Class I and dental Class II molar relationship;
- Pretreatment chronological age between 11 and 17 years;
- Normal vertical growth pattern;
- Patients with complete orthodontic models in the archive;
- Patients with complete and good-quality radiographs in the archive;
Exclusion Criteria:
- Any tooth loss both at the beginning and during the follow-up period;
- Tooth agenesis;
- Treatment records with inadequate-quality cephalometric radiographs of the patients;
- Dentofacial deformity.
2.1. Measurements
Three serial lateral cephalometric radiographs were obtained from each patient for evaluations at 3 different observation periods: pre-treatment (T1), after fixed orthodontic treatment following maxillary molar distalization (T2), and post-treatment long term (T3). Lateral cephalometric films obtained at T1, T2, and T3 were transferred to the Dolphin Imaging 11.8 Premium program (Dolphin Imaging & Management Solutions, Los Angeles, CA, USA) (Patterson Dental Supply, Inc., St. Paul, MN, USA), calibrated, and custom-analyzed (Figure 1 and Figure 2).
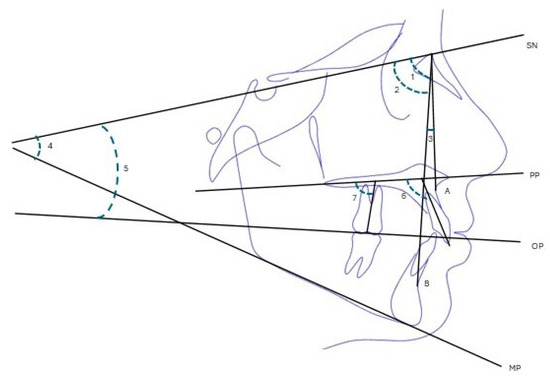
Figure 1.
Cephalometric angular measurements: (1) SNA°, sella–nasion–A point; (2) SNB°, sella–nasion–B point; (3) ANB°, A point–nasion–B point; (4) SN-MP°, sella–nasion–mandibular plane; (5) SN-OP°, sella–nasion–occlusal plane; (6) U1-PP°, maxillary central incisor–palatal plane; (7) U6-PP°, maxillary first molar–palatal plane.
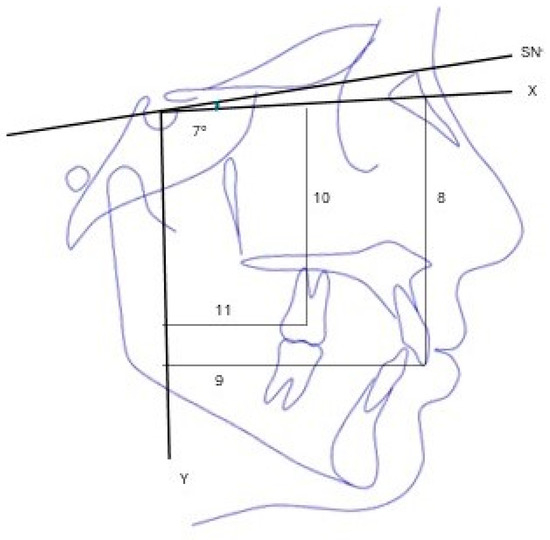
Figure 2.
Cephalometric linear measurements: 7°: Angle between SN plane and X plane; (8) U1-X (mm), distance from maxillary central incisor to X plane; (9) U1-Y (mm), distance from maxillary central incisor to Y plane; (10) U6-X (mm), distance from maxillary first molar to X plane; (11) U6-Y (mm), distance from maxillary first molar to Y plane.
In this study, the horizontal reference plane (X plane), which makes a 7° angle clockwise from the sella point to the SN plane, was used according to Kalra et al. [22] The plane (Y plane) drawn at an angle of 90° from the sella point to the X plane was used as the vertical reference plane (Figure 2). We preferred the “corrected Sella-Nasion Plane”, which was described by Burstone et al. [23], because the plane of the SN is least affected by growth and development-dependent changes and is reproducible when assigned.
The midpoint of the line connecting the widest mesio-distal dimensions of the maxillary first molar tooth was used in the cephalometric measurements because the crown is least impacted by distal tipping [10,24,25,26]. The incisal edge was used as a landmark to evaluate the movement of the upper incisor. To evaluate changes in the tooth axis inclinations, the long axes were established by the line passing through the center point and furcation point of the molar tooth and the incisor tooth’s incisal edge and root apex [15,17,24]. The angle of the long axes of the teeth with the palatal plane was measured [17].
The maxilla was superimposed on the ANS-PNS planes to evaluate the change in positions of the U6 and U1 (Figure 3) [1,16,24]. In this study, to evaluate the movements of the maxillary teeth, the palatal plane connecting the ANS and PNS points was used, and superimposition was performed by overlapping this plane locally from the ANS point.
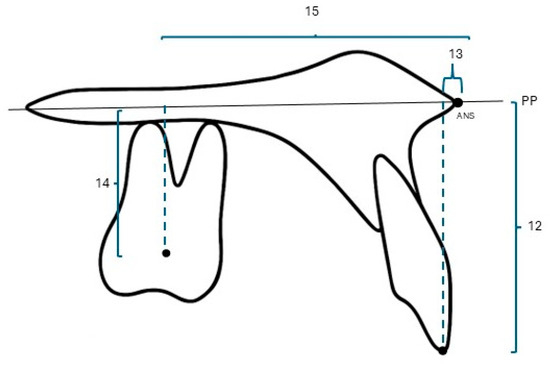
Figure 3.
Measurements in superimposition of the maxilla. (12) U1-PP (mm), distance from maxillary incisor tip to palatal plane; (13) U1-ANS (mm), distance from maxillary incisor to anterior nasal spina; (14) U6-PP (mm), distance from maxillary first molar to palatal plane; (15) U6-ANS (mm), distance from maxillary first molar to anterior nasal spina.
Orthodontic models were created by taking upper and lower jaw measurements from each individual at T1, T2, and T3. The overjet, overbite, arch length, irregularity index, right and left molar relationship (the horizontal distance between the tip of the mesio-buccal cusp of the upper first molar and the median sulcus of the lower first molar) were made in the model analysis (Figure 4) [19,27,28]. A digital caliper with a 0.01 mm precision was used to take the measurements.
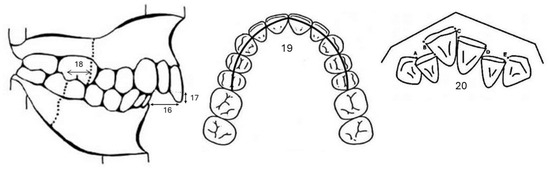
Figure 4.
Measurements on the orthodontic model: (16) overjet (mm); (17) overbite (mm); (18) molar relationship (mm); (19) maxillary arc length (mm); (20) maxillary irregularity index (mm).
2.2. Statistical Analysis
The study data’s conformity to normal distribution was evaluated with the Kolmogorov–Smirnov test. The paired t-test was used for normal distribution and the Wilcoxon signed-rank test was used for non-normal distribution to compare the changes during the periods examined. The Mann–Whitney U test was conducted to assess the significance of the gender differences. Because there were no gender-specific differences in most measurements examined, males and females were combined and statistically evaluated. Statistical significance was set at p < 0.05.
The minimum number of subjects was determined using G*Power 3 (Düsseldorf, Germany), applying a significance level of p < 0.05 and a power of 95%, referencing a study that indicated 2.0 mm of mesial movement following distalization with the Pendulum appliance [19].
2.3. Method Error
To test the intra-examiner reliability, measurements of 15 randomly selected cephalograms from 120 records belonging to 40 individuals were repeated at 1-month intervals, which showed high reliability (intraclass correlation coefficient range: 0.917–0.997).
3. Results
This study tested the hypothesis that maxillary first molar distalization achieved through orthodontic treatment can be maintained in the long term, and that dentoalveolar measurements remain stable after treatment. The mean and standard deviation values of the chronological ages of the individuals included in this study at T1, T2, and T3 are presented in Table 1. The average treatment period was 3.0 years, and the long-term follow-up period was 6.1 years. The values for the T1, T2, and T3 periods are shown in Table 2. The mean and standard deviations with changes in the cephalometric and model measurements relative to T2-T1, T3-T2, and T3-T1 are summarized in Table 3.

Table 2.
Mean cephalometric and model measurements at T1, T2, and T3.

Table 3.
Changes in cephalometric and model measurements at T2-T1, T3-T2, and T3-T1 a.
3.1. Changes in Cephalometric Measurements
Statistically significant increases occurred in the SNA and SNB skeletal measurements at T2-T1, T3-T2, and T3-T1. (p < 0.001). The maxillomandibular relationship did not significantly change during these periods.
When the T2-T1 period was examined, increases were observed in the SN-MD (p < 0.001) and SN-OP measurements. During the post-treatment period (T3-T2), there was a statistically significant decrease in the SN-MP and SN-OP angular measurements (p < 0.001). The craniofacial growth pattern remained unchanged by the applied mechanics, as indicated by the SN-MP measurements, which showed no significant alterations from T1 to T3. After the distalization of the maxillary molars and the fixed orthodontic treatment, clockwise rotation of the mandibular region caused a significant increase in the SN-MP measurement. The value decreased from T3 to T1 after treatment and returned to the initial value.
During the T2-T1 period, the distalization and fixed therapy resulted in a 1.76 mm increase in the U6-ANS distance. Although a 0.31 mm relapse was reported between T3 and T2, the maintenance of a distalization of 1.45 mm throughout the whole follow-up period can be considered an important result. This relapse can be explained by the teeth’s associated mesialization tendency and the approximately 2° mesial inclination of the maxillary first molar crowns compared to the baseline. No significant change in the U6-Y distance was observed, suggesting that the sagittal growth of the maxilla continued naturally despite the distalizing forces. Significant increases were observed in the U6-PP angle (1.63°), which indicates the inclination of the first molar, and in the U6-X (3.04 mm) and U6-PP (1.33 mm) distances, which indicate the amount of vertical direction position.
Statistically significant increases were observed in the U6-X (1.25 mm), U6-Y (1.5 mm), and U6-PP (0.39 mm) (p < 0.001) dimensional measurements and U6-PP (0.42°) (p < 0.001) angular measurement in the post-treatment period (T3-T2). The measurements indicate the sagittal and vertical displacement of the maxillary molars and changes in their axial inclination.
Upper incisors remained relatively vertically stable in the post-treatment phase, indicating favorable long-term control of the anterior tooth position. No significant change was observed in the U1-PP measurement, which shows the buccal inclination of the upper incisors, or the U1-ANS measurement, which shows the sagittal position, during the treatment period (T2-T1) and in the long term after treatment (T3-T2). The increase in the U1-X and U1-Y measurements is associated with craniofacial growth in the vertical and sagittal directions.
3.2. Changes in Model Measurements
During orthodontic treatment, there were statistically significant reductions in the overbite, overjet, index of irregularity, and right and left molar relationship measurements, as well as an increase in the arch length (p < 0.001).
In the long term after treatment, a 0.3 mm increase in the overjet, a 0.65 mm decrease in the arch length, and a 2.61 mm increase in the irregularity index were observed. The changes observed in these parameters reveal the presence of mild irregularities in the long-term follow-up. Although there was no significant change in the left molar relationship and overbite, a 0.28 mm change was observed in the right molar relationship.
4. Discussion
In the management of dental Class II malocclusion, the two primary treatment modalities traditionally include maxillary molar distalization and the extraction of two premolars in the upper arch. However, in recent years, there has been a noticeable decline in the frequency of extraction-based treatments—particularly those involving four premolars or even just two maxillary premolars in Class II cases. This trend is largely attributed to increasing esthetic demands and the growing adoption of alternative orthodontic strategies, such as maxillary expansion techniques, distalization appliances, temporary anchorage devices (TADs), and the more frequent application of interproximal enamel reduction [29]. In addition, maxillary molar distalization holds a significant role in clear aligner therapy due to its high level of predictability [30].
Despite being a commonly employed procedure in orthodontics with various available techniques, maxillary molar distalization lacks sufficient long-term follow-up research in the literature. A recent systematic review [31] confirmed this scarcity, identifying only nine relevant articles, of which only five included follow-up periods of at least four years and just three involved more than 20 distalization patients. In the present study, long-term outcomes were assessed in 40 patients who completed fixed orthodontic treatment following maxillary molar distalization, with an average post-treatment follow-up period of 6.1 years.
Since the evaluated group consisted of growing individuals, the significant increases observed in both the SNA and SNB angles during the treatment and follow-up periods can be attributed more to the ongoing craniofacial growth of the mandible and maxilla rather than the direct effect of the treatment itself [32]. Notably, the ANB angle remained unchanged in our study, indicating that the correction of Class II malocclusion was largely due to dentoalveolar compensation rather than skeletal change. This finding aligns with studies by Angelieri et al. [17], Caprioglio et al. [19], and Chou et al. [21], who reported similar patterns of limited skeletal changes and the preservation of the maxillomandibular skeletal relationship.
Although the distalization mechanics temporarily increased the SN-MP angle during treatment, this returned to baseline post-treatment. This finding closely aligns with the earlier results of Caprioglio et al. [19]. It has also been claimed that the distalization mechanics did not change the vertical craniofacial growth pattern [17]. In the study by Song et al. [20], it was observed that the lower anterior facial height decreased significantly as a result of maxillary arch distalization and remained relatively constant throughout the retention period. However, these findings may not be directly comparable to our results due to methodological differences. In particular, the inclusion of adult patients in their study and the use of a different distalization protocol may explain the inconsistency in the vertical skeletal changes.
In this study, it was expected that both during the distalization phase and throughout the follow-up period, the maxilla and mandible, along with their associated dentition, would move anteriorly as a whole. Indeed, the fact that the distance from the maxillary molar to the vertical reference plane (U6–Y) did not significantly change—and even increased slightly—in the records taken immediately after distalization suggests that the effects of distalization were masked by concurrent growth. However, the average increase of 1.76 mm in the distance between the maxillary molars and the ANS, along with an approximately 2.5 mm improvement in the molar relationship following distalization, indicates that the maxillary molars were substantially distalized.
During the fixed orthodontic treatment and subsequent follow-up period, as the maxilla and mandible continued to move anteriorly, a relapse of 0.31 mm occurred. As a result, the remaining net distalization was reduced to 1.45 mm. Nonetheless, the improvement in the molar relationship was largely maintained throughout the entire observation period. One possible explanation for this stability is that, after achieving a Class I molar relationship during treatment, dentoalveolar compensation mechanisms helped preserve this occlusal relationship during the period of maxillomandibular growth [19]. Again, this has been linked to the correct intercuspation and the skeletal growth pattern [33,34].
Furthermore, the statistically significant extrusion of upper first molars observed during and after treatment, and the increase in the U6-X axis distance, are in line with the vertical changes previously reported by Ngantung et al. [10] and Angelieri et al. [17]. These changes underscore the need for careful vertical control, particularly in hyperdivergent patients.
The incisor region remained relatively stable throughout, with minor inclination and extrusion changes, suggesting that anterior dental changes were primarily growth-driven.
During the T2–T1 period, there was a statistically significant increase in the arch length and significant decreases in the overjet, overbite, irregularity index, and both right and left molar relationship measurements. In the long-term follow-up treatment, some relapse was observed in the overjet, arch length, irregularity index, and right molar relationship. However, the improvements achieved during treatment were largely maintained. These findings were generally consistent with those reported in similar studies in the literature [10,13,16,21,35].
Clinically, our findings emphasize the importance of overcorrection strategies, retention protocols, and growth guidance for achieving long-term stability following distalization. The small relapse values in the overjet, arch length, and molar relationship measurements support the conclusions from multiple studies indicating that, when performed with well-planned biomechanics and patient compliance, distalization is a viable long-term option for selected Class II cases. However, this study has several limitations. The absence of a control group limits the ability to distinguish treatment effects from natural craniofacial development. Additionally, the reliance on two-dimensional imaging restricts the evaluation of the three-dimensional skeletal and dental adaptations. Future studies utilizing CBCT and larger, more diverse samples are necessary to further elucidate the full effects of distalization over time.
5. Conclusions
Long-term evaluations have demonstrated that maxillary molar distalization provides stable treatment outcomes. Although minor relapse may occur due to continued maxillomandibular growth following orthodontic treatment, it does not appear to significantly affect either the molar relationship or the overall amount of distalization. Additionally, the vertical craniofacial changes observed during treatment were found to be temporary, with the maxillomandibular relationship remaining generally stable over time in Class II malocclusion cases.
Author Contributions
Conceptualization, F.U. and A.K.; methodology, F.U. and A.K.; software, F.U.; validation, F.U. and A.K.; formal analysis, F.U. and A.K.; investigation, F.U.; resources, F.U.; data curation, F.U. and A.K.; writing—original draft preparation, F.U.; writing—review and editing, F.U.; visualization, F.U.; supervision, F.U. and A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Research Ethics Committee of the Faculty of Dentistry, Atatürk University (protocol code 01/2014 and the date of approval was 14 January 2014).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Patel, M.P.; Henriques, J.F.; Freitas, K.M.; Grec, R.H. Cephalometric effects of the Jones Jig appliance followed by fixed appliances in Class II malocclusion treatment. Dent. Press J. Orthod. 2014, 19, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Hichijo, N.; Sato, M.; Mino, A.; Tamamura, N.; Iwata, M.; Tanaka, E. Long-term stability of maxillary group distalization with interradicular miniscrews in a patient with a Class II Division 2 malocclusion. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 912–922. [Google Scholar] [CrossRef] [PubMed]
- Luppanapornlarp, S.; Johnston, L.E., Jr. The effects of premolar-extraction: A long-term comparison of outcomes in “clear-cut” extraction and nonextraction Class II patients. Angle Orthod. 1993, 63, 257–272. [Google Scholar] [CrossRef] [PubMed]
- Bowman, S.J.; Johnston, L.E., Jr. The esthetic impact of extraction and nonextraction treatments on Caucasian patients. Angle Orthod. 2000, 70, 3–10. [Google Scholar] [CrossRef]
- Cetlin, N.M.; Ten Hoeve, A. Nonextraction treatment. J. Clin. Orthod. 1983, 17, 396–413. [Google Scholar]
- Moyers, R.E.; Riolo, M.L.; Guire, K.E.; Wainright, R.L.; Bookstein, F.L. Differential diagnosis of class II malocclusions. Part 1. Facial types associated with class II malocclusions. Am. J. Orthod. 1980, 78, 477–494. [Google Scholar] [CrossRef]
- Firouz, M.; Zernik, J.; Nanda, R. Dental and orthopedic effects of high-pull headgear in treatment of Class II, division 1 malocclusion. Am. J. Orthod. Dentofac. Orthop. 1992, 102, 197–205. [Google Scholar] [CrossRef]
- Ucem, T.T.; Yuksel, S. Effects of different vectors of forces applied by combined headgear. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 316–323. [Google Scholar] [CrossRef]
- Bilbo, E.E.; Marshall, S.D.; Southard, K.A.; Allareddy, V.; Holton, N.; Thames, A.M.; Otsby, M.S.; Southard, T.E. Long-term skeletal effects of high-pull headgear followed by fixed appliances for the treatment of Class II malocclusions. Angle Orthod. 2018, 88, 530–537. [Google Scholar] [CrossRef]
- Ngantung, V.; Nanda, R.S.; Bowman, S.J. Posttreatment evaluation of the distal jet appliance. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 178–185. [Google Scholar] [CrossRef]
- Keles, A.; Erverdi, N.; Sezen, S. Bodily distalization of molars with absolute anchorage. Angle Orthod. 2003, 73, 471–482. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Kim, Y.; Park, J.H.; Lee, N.K.; Kim, S.H.; Kook, Y.A. Long-term evaluation of maxillary molar position after distalization using modified C-palatal plates in patients with and without second molar eruption. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 853–861. [Google Scholar] [CrossRef]
- Burkhardt, D.R.; McNamara, J.A., Jr.; Baccetti, T. Maxillary molar distalization or mandibular enhancement: A cephalometric comparison of comprehensive orthodontic treatment including the pendulum and the Herbst appliances. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Bondemark, L.; Kurol, J. Distalization of maxillary first and second molars simultaneously with repelling magnets. Eur. J. Orthod. 1992, 14, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Bechtold, T.E.; Park, Y.C.; Kim, K.H.; Jung, H.; Kang, J.Y.; Choi, Y.J. Long-term stability of miniscrew anchored maxillary molar distalization in Class II treatment. Angle Orthod. 2020, 90, 362–368. [Google Scholar] [CrossRef]
- Caprioglio, A.; Cozzani, M.; Fontana, M. Comparative evaluation of molar distalization therapy with erupted second molar: Segmented versus Quad Pendulum appliance. Prog. Orthod. 2014, 15, 49. [Google Scholar] [CrossRef][Green Version]
- Angelieri, F.; Almeida, R.R.; Almeida, M.R.; Fuziy, A. Dentoalveolar and skeletal changes associated with the pendulum appliance followed by fixed orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 520–527. [Google Scholar] [CrossRef]
- Mossaz, C.F.; Byloff, F.K.; Kiliaridis, S. Cervical headgear vs pendulum appliance for the treatment of moderate skeletal Class II malocclusion. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 616–623. [Google Scholar] [CrossRef]
- Caprioglio, A.; Fontana, M.; Longoni, E.; Cozzani, M. Long-term evaluation of the molar movements following Pendulum and fixed appliances. Angle Orthod. 2013, 83, 447–454. [Google Scholar] [CrossRef]
- Song, B.-J.; Lee, K.-J.; Cha, J.-Y.; Lee, J.-S.; Mo, S.-S.; Yu, H.-S. Stability of the Maxillary and Mandibular Total Arch Distalization Using Temporary Anchorage Devices (TADs) in Adults. Appl. Sci. 2022, 12, 2898. [Google Scholar] [CrossRef]
- Chou, A.H.K.; Park, J.H.; Shoaib, A.M.; Lee, N.K.; Lim, H.J.; Abdulwhab, A.A.; Alfawaz, F.; Kook, Y.A. Total maxillary arch distalization with modified C-palatal plates in adolescents: A long-term study using cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 470–479. [Google Scholar] [CrossRef] [PubMed]
- Kalra, V.; Burstone, C.J.; Nanda, R. Effects of a fixed magnetic appliance on the dentofacial complex. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 467–478. [Google Scholar] [CrossRef] [PubMed]
- Burstone, C.J.; James, R.B.; Legan, H.; Murphy, G.A.; Norton, L.A. Cephalometrics for orthognathic surgery. J. Oral. Surg. 1978, 36, 269–277. [Google Scholar] [PubMed]
- Ghosh, J.; Nanda, R.S. Evaluation of an intraoral maxillary molar distalization technique. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 639–646. [Google Scholar] [CrossRef]
- Byloff, F.K.; Darendeliler, M.A. Distal molar movement using the pendulum appliance. Part 1: Clinical and radiological evaluation. Angle Orthod. 1997, 67, 249–260. [Google Scholar] [CrossRef]
- Bussick, T.J.; McNamara, J.A., Jr. Dentoalveolar and skeletal changes associated with the pendulum appliance. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 333–343. [Google Scholar] [CrossRef]
- Rosa, W.G.N.; de Almeida-Pedrin, R.R.; Oltramari, P.V.P.; de Castro Conti, A.C.F.; Poleti, T.; Shroff, B.; de Almeida, M.R. Total arch maxillary distalization using infrazygomatic crest miniscrews in the treatment of Class II malocclusion: A prospective study. Angle Orthod. 2023, 93, 41–48. [Google Scholar] [CrossRef]
- Burns, A.; Dowling, A.H.; Garvey, T.M.; Fleming, G.J. The reliability of Little’s Irregularity Index for the upper dental arch using three dimensional (3D) digital models. J. Dent. 2014, 42, 1320–1326. [Google Scholar] [CrossRef]
- Dardengo Cde, S.; Fernandes, L.Q.; Capelli Junior, J. Frequency of orthodontic extraction. Dent. Press J. Orthod. 2016, 21, 54–59. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Xie, Z.; Xu, H.; Tian, Y.; Han, X. Long-term stability of maxillary molar distalization in the treatment of Angle Class II malocclusion: A systematic review and meta-analysis. Clin. Oral. Investig. 2025, 29, 277. [Google Scholar] [CrossRef] [PubMed]
- Riolo, M.L.; Moyers, R.; McNamara, J.A.; Hunter, W.S. An Atlas of Craniofacial Growth: Cephalometric Standards from the University School Growth Study; Center for Human Growth and Development, University of Michigan: Ann Arbor, MI, USA, 1974. [Google Scholar]
- Melsen, B. Effects of cervical anchorage during and after treatment: An implant study. Am. J. Orthod. 1978, 73, 526–540. [Google Scholar] [CrossRef] [PubMed]
- Gianelly, A.A. Distal movement of the maxillary molars. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Chiu, P.P.; McNamara, J.A., Jr.; Franchi, L. A comparison of two intraoral molar distalization appliances: Distal jet versus pendulum. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 353–365. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).