Predictability of ClinCheck in Overbite Correction with Aligners: A Systematic Review
Abstract
1. Introduction
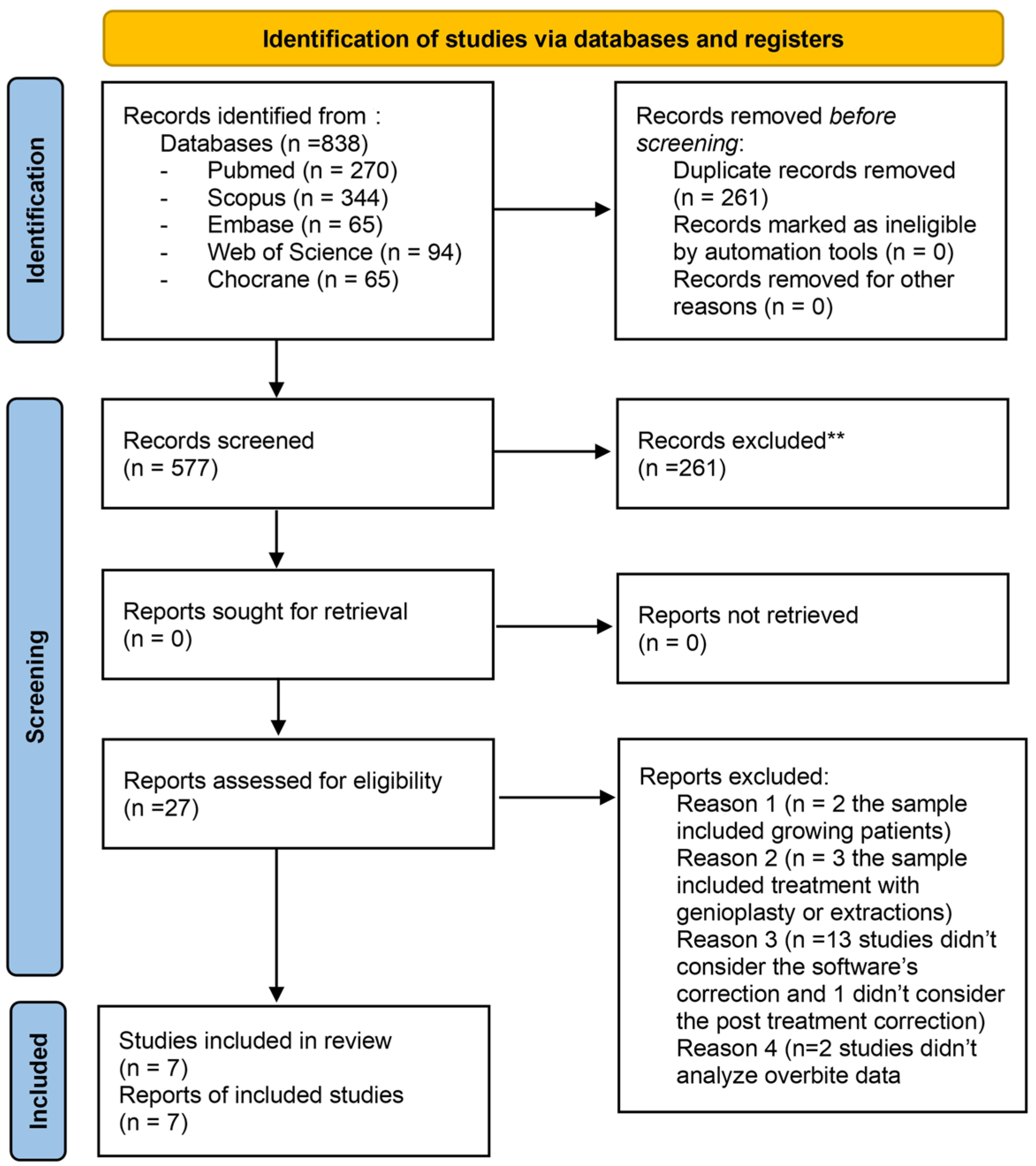
2. Materials and Methods
2.1. Eligibility Criteria
- Studies published in English;
- Patients aged ≥18 years;
- Patients treated with aligners;
- Patients without systemic diseases;
- Presence of permanent teeth, with involvement of the second molars;
- Patients with overbite measurements ≤2 mm or ≥2 mm;
- Orthodontic treatments involving both the maxillary and mandibular arches;
- Inclusion of a digital prediction of overbite correction generated by the software.
- Growing patients;
- Extractions;
- Temporomandibular disorders;
- Patients with bone metabolism disorders;
- Patients treated with orthognathic surgery;
- Loss of specimen.
2.2. Search Strategy and Selection Process
2.3. Data Collection and Data Items
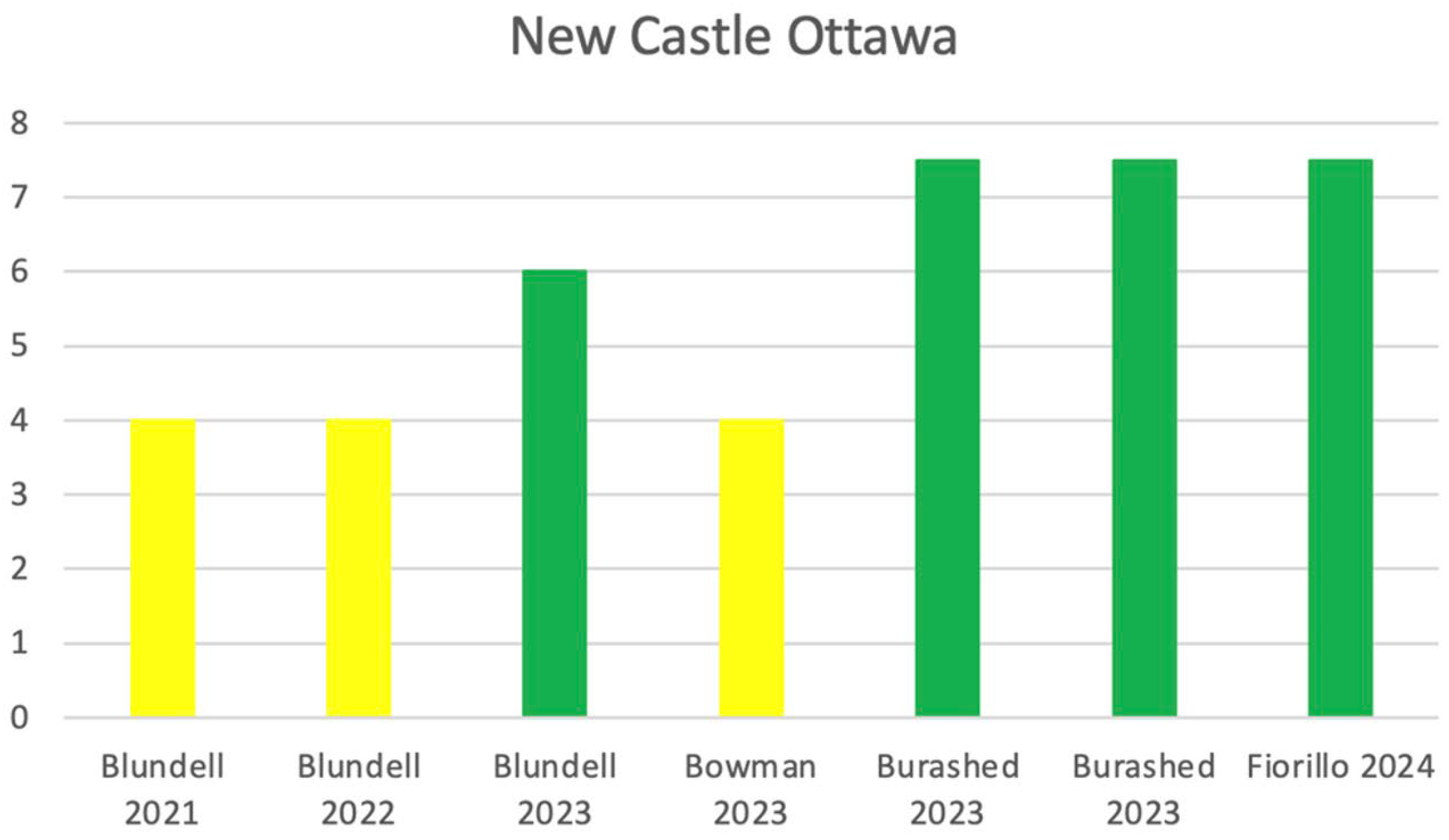
2.4. Quality Assesment in Individual Studies
- -
- Selection of study groups
- -
- Comparability between groups
- -
- Assessment of exposure/outcome
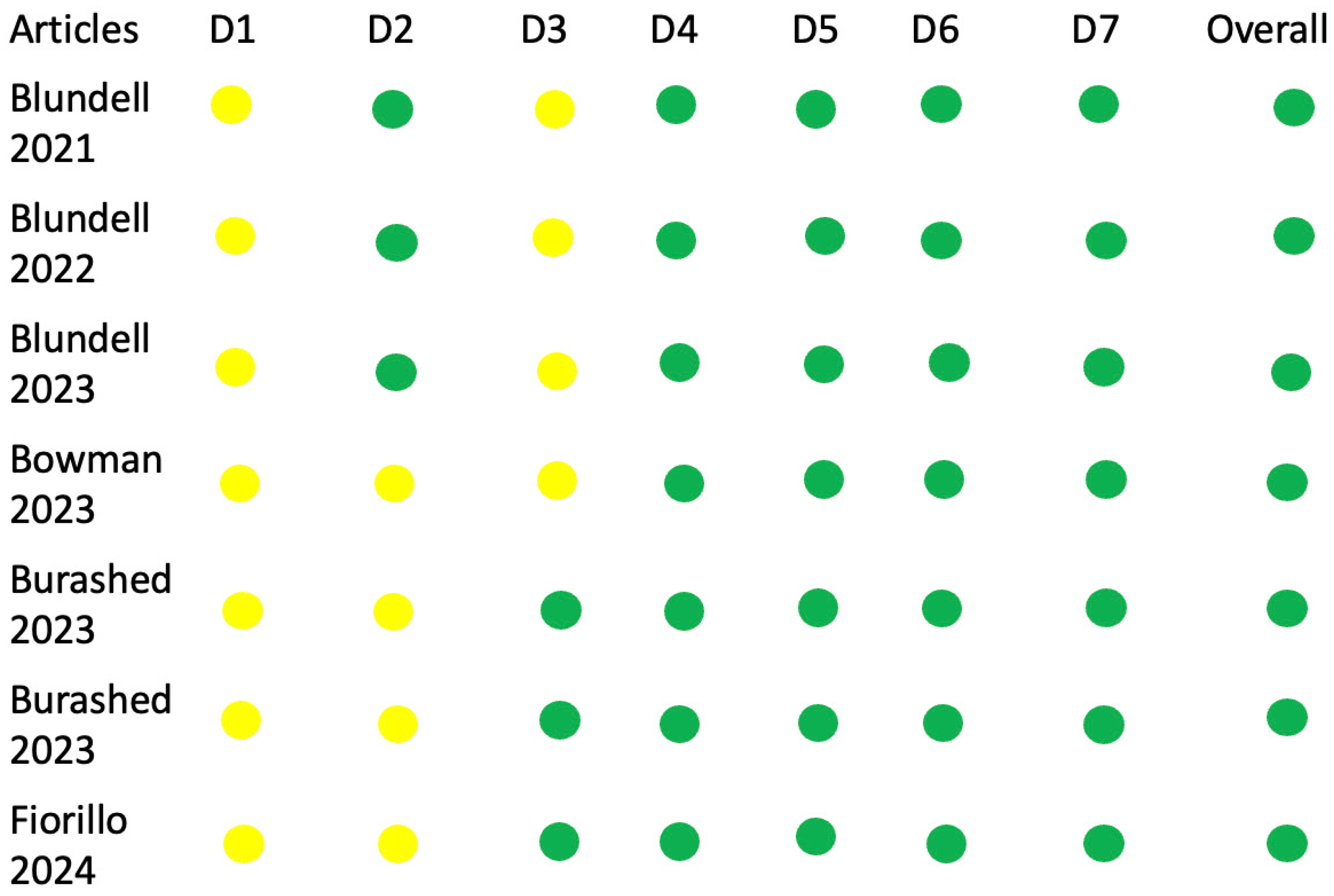
2.5. Risk of Bias Assesment
- -
- D1: Bias due to confounding factors
- -
- D2: Bias due to participant selection
- -
- D3: Bias in intervention classification
- -
- D4: Bias due to deviations from the planned interventions
- -
- D5: Bias due to missing data
- -
- D6: Bias in data measurement
- -
- D7: Bias in selection of reported outcomes
3. Results
- -
- -
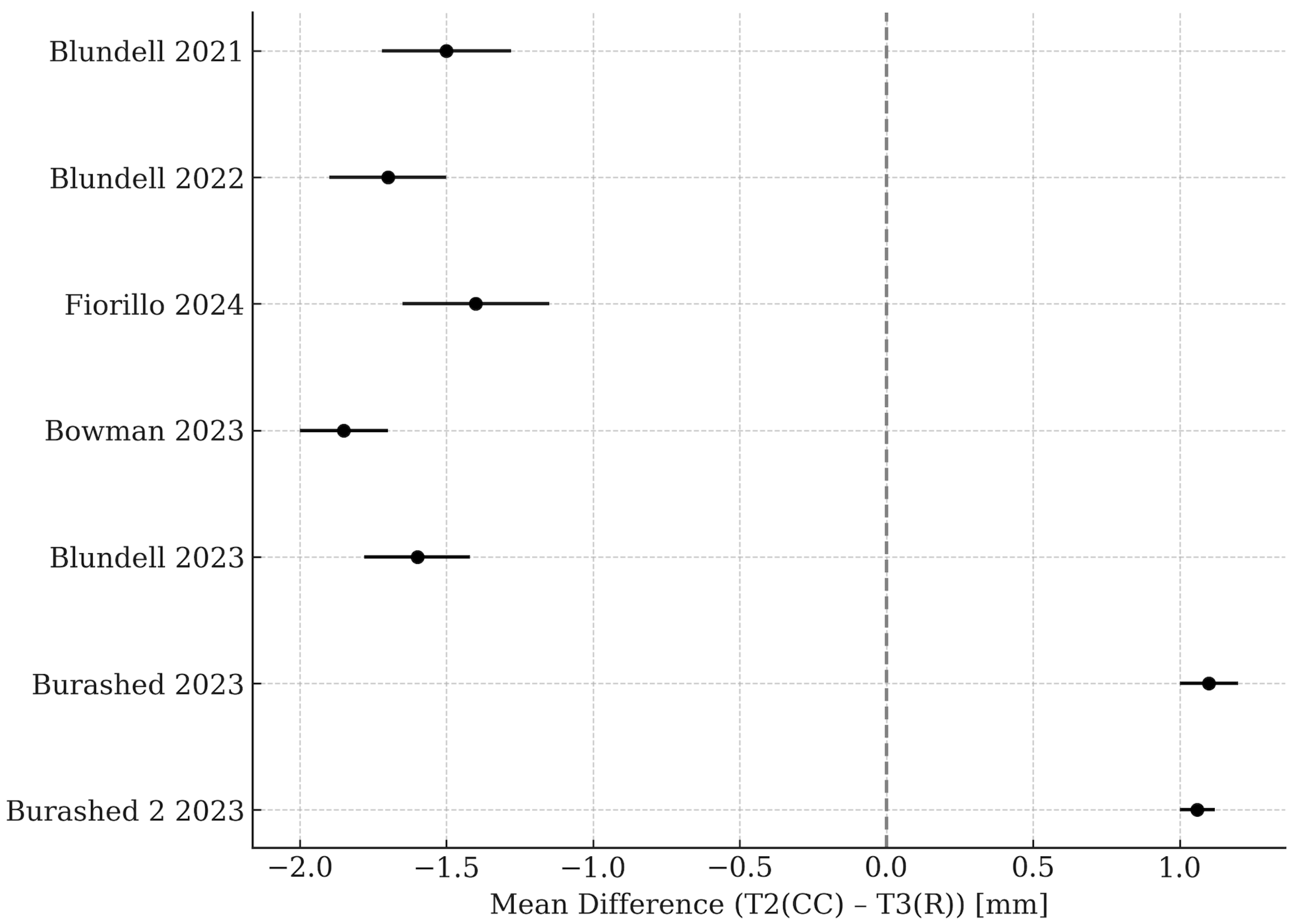
3.1. Meta-Analysis
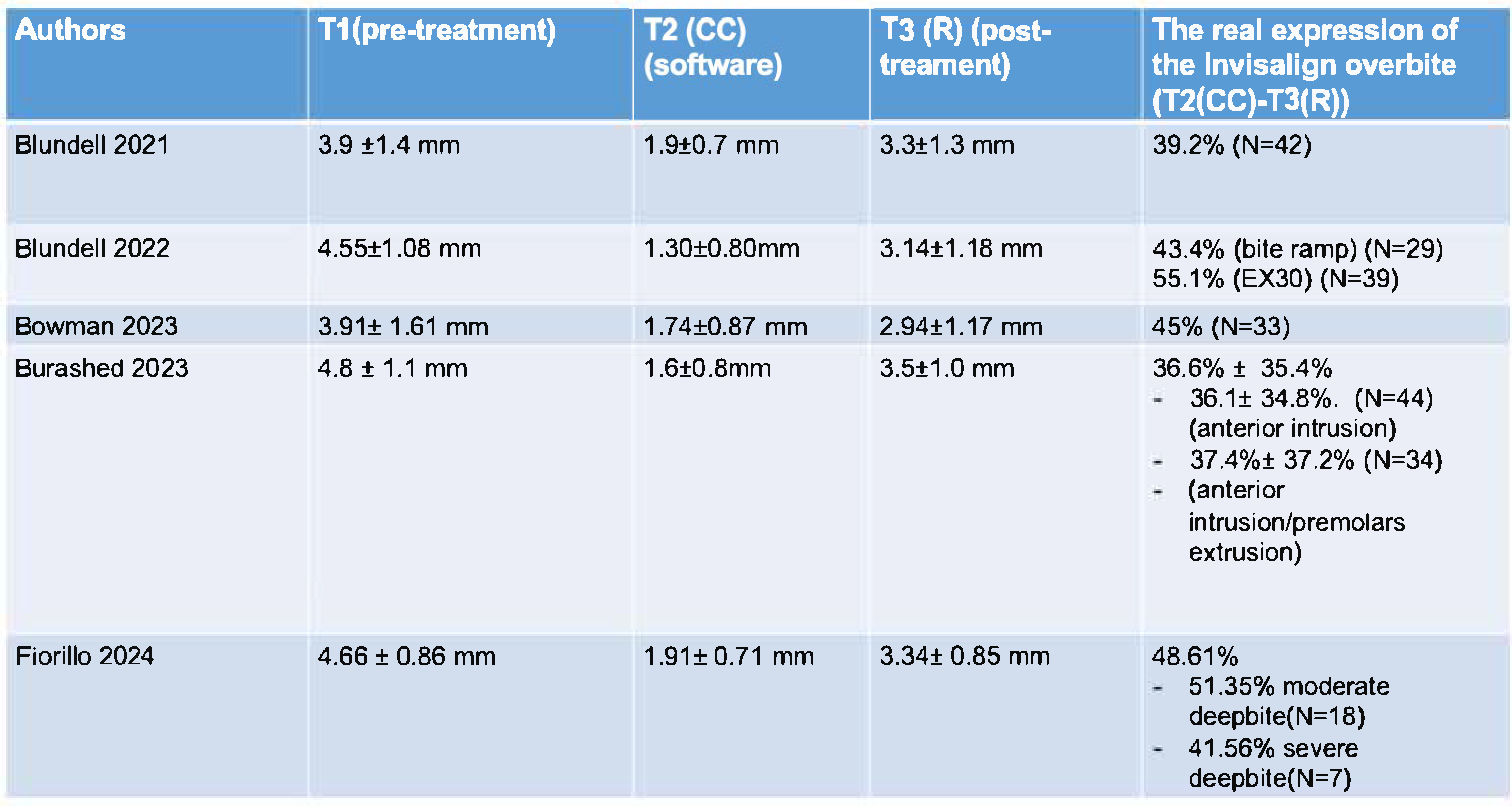
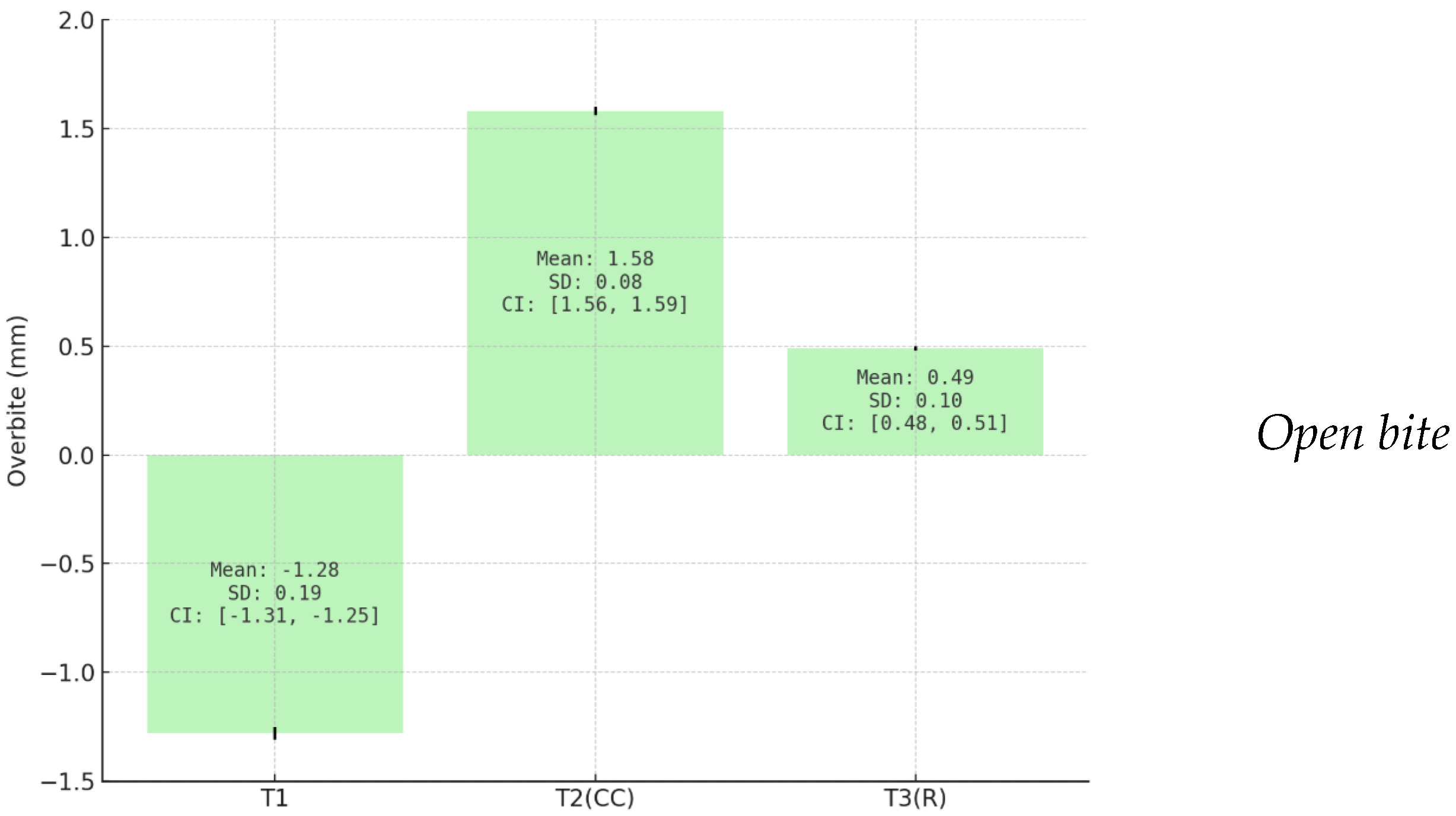
3.2. Quantitative Assessment of Overbite Correction
- -
- T1: 4.39 mm (SD: 0.37; 95%; CI: 4.34–4.44 mm);
- -
- T2(CC): 1.62 mm (SD: 0.25; 95%, CI: 1.59–1.65 mm);
- -
- T3(R): 3.24 mm (SD: 0.18; 95%, CI: 3.21–3.26 mm).
- -
- T1: −1.28 mm (SD: 0.19; 95%,CI: −1.31, −1.25 mm)
- -
- T2(CC): 1.58 mm (SD: 0.08; 95%, CI: 1.56 −1.59 mm)
- -
- T3 (R): 0.49 mm (SD: 0.10; 95%, CI: 0.48 −0.51 mm).
4. Discussion
5. Conclusions
- -
- The correction of deep bite predicted by the ClinCheck software overestimates the correction achieved clinically.
- -
- There is a concordance between the ClinCheck prediction and the actual outcomes for open bite correction.
- -
- The application of posterior occlusal bite blocks and traditional attachments appears to exert minimal influence on the success of open bite closure.
- -
- The lack of standardized protocols for staging and biomechanics likely contributes to the variability observed in deep bite treatment outcomes. Overengineering the final set up and incorporating planned overcorrections may be necessary to reduce the discrepancy between the virtual plans and the clinical results.
6. Limitations
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kesling, H. The philosophy of the tooth positioning appliance. Am. J. Orthod. Oral Surg. 1945, 31, 297–304. [Google Scholar] [CrossRef]
- Walton, D.K.; Fields, H.W.; Johnston, W.M.; Rosenstiel, S.F.; Firestone, A.R.; Christensen, J.C. Orthodontic appliance preferences of children and adolescents. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 698.e1–698.e12. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Fields, H.W.; Sarver, D.M. Contemporary Orthodontics, 4th ed.; Mosby: St. Louis, MO, USA, 2007; pp. 7–9. [Google Scholar]
- Ghafari, J.G.; Macari, A.T.; Haddad, R.V. Deep bite: Treatment options and challenges. Semin. Orthod. 2013, 19, 253–266. [Google Scholar] [CrossRef]
- Gu, D.; Leroux, B.; Finkleman, S.; Todoki, L.; Greenlee, G.; Allareddy, V.; Jolley, C.; Vermette, M.; Shin, K.; Kau, C.H.; et al. Anterior openbite malocclusion in adults. Angle Orthod. 2021, 92, 27–35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Burstone, C.R. Deep overbite correction by intrusion. Am. J. Orthod. 1977, 72, 1–22. [Google Scholar] [CrossRef]
- Burford, D.; Noar, J.H. The Causes, diagnosis and treatment of anterior open bite. Dent. Update 2003, 30, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Steadman, S.R. Predetermining the overbite and overjet. Angle Orthod. 1949, 19, 101–105. [Google Scholar]
- Weir, T. Clear aligners in orthodontic treatment. Aust. Dent. J. 2017, 62 (Suppl. 1), 58–62. [Google Scholar] [CrossRef] [PubMed]
- Blundell, H.L.; Weir, T.; Byrne, G. Predictability of overbite control with the Invisalign appliance comparing SmartTrack with precision bite ramps to EX30. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e71–e81. [Google Scholar] [CrossRef]
- Bichu, Y.M.; Alwafi, A.; Liu, X.; Andrews, J.; Ludwig, B.; Bichu, A.Y.; Zou, B. Advances in orthodontic clear aligner materials. Bioact. Mater. 2022, 22, 384–403. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Moshiri, M.; Nicozisis, J.; Miller, S. Mechanical considerations for deep-bite correction with aligners. Semin. Orthod. 2020, 26, 134–138. [Google Scholar] [CrossRef]
- Henick, D.; Dayan, W.; Dunford, R.; Warunek, S.; Al-Jewair, T. Effects of Invisalign (G5) with virtual bite ramps for skeletal deep overbite malocclusion correction in adults. Angle Orthod. 2021, 91, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.; Ojima, K.; Dan, C.; Upadhyay, M.; Alshehri, A.; Kuo, C.-L.; Mu, J.; Uribe, F.; Nanda, R. Evaluation of open bite closure using clear aligners: A retrospective study. Prog. Orthod. 2020, 21, 23. [Google Scholar] [CrossRef] [PubMed]
- Tai, S. Clear Aligner Technique; Quintessence Publishing: Hanover Park, IL, USA, 2020; Chapter 8: Deep Bite; pp. 95–112. [Google Scholar]
- Kravitz, N.D.; Hansa, I.; Vaid, N.R.; Moshiri, M.; Adel, S.M. Does age influence deep overbite correction with Invisalign? A prospective study evaluating mandibular incisor intrusion in adolescents vs adults. Angle Orthod. 2023, 94, 145–150. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Haouili, N.; Kravitz, N.D.; Vaid, N.R.; Ferguson, D.J.; Makki, L. Has Invisalign improved? A prospective follow-up study on the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 420–425. [Google Scholar] [CrossRef]
- Khosravi, R.; Cohanim, B.; Hujoel, P.; Daher, S.; Neal, M.; Liu, W.; Huang, G. Management of overbite with the Invisalign appliance. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 691–699.e2. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Kusnoto, B.; BeGole, E.; Obrez, A.; Agran, B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 27–35. [Google Scholar] [CrossRef]
- Blundell, H.L.; Weir, T.; Kerr, B.; Freer, E. Predictability of overbite control with the Invisalign appliance. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 725–731. [Google Scholar] [CrossRef]
- Tai, S. Clear Aligner Technique; Quintessence Publishing: Hanover Park, IL, USA, 2020; Chapter 9: Anterior Open Bite; pp. 113–130. [Google Scholar]
- Guarneri, M.P.; Oliverio, T.; Silvestre, I.; Lombardo, L.; Siciliani, G. Open bite treatment using clear aligners. Angle Orthod. 2013, 83, 913–919. [Google Scholar] [CrossRef]
- Schupp, W.; Haubrich, J.; Neumann, I. Treatment of anterior open bite with the Invisalign system. J. Clin. Orthod. 2010, 44, 501–507. [Google Scholar]
- Rask, H.; English, J.D.; Colville, C.; Kasper, F.K.; Gallerano, R.; Jacob, H.B. Cephalometric evaluation of changes in vertical dimension and molar position in adult non-extraction treatment with clear aligners and traditional fixed appliances. Dent. Press J. Orthod. 2021, 26, e2119360. [Google Scholar] [CrossRef] [PubMed]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.V.; Chen, J. The Invisalign System; Tuncay, O.C., Ed.; Quintessence Publishing Company, Ltd.: New Malden, UK, 2016; Chapter 14; pp. 12–32. [Google Scholar]
- Suh, H.; Garnett, B.S.; Mahood, K.; Mahjoub, N.; Boyd, R.L.; Oh, H. Treatment of anterior open bites using non-extraction clear aligner therapy in adult patients. Korean J. Orthod. 2022, 52, 210–219. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Masella, R.S.; Meister, M. Current concepts in the biology of orthodontic tooth movement. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 458–468. [Google Scholar] [CrossRef]
- van der Bie, R.M.; Bos, A.; Bruers, J.J.M.; Jonkman, R.E.G. Patient adherence in orthodontics: A protocol for a scoping review. BDJ Open 2024, 10, 62. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Chamberland, S.; Nataf, N. Noninvasive conservative management of anterior open bite treated with TADs versus clear aligner therapy. Clin Oral Investig. 2024, 28, 236. [Google Scholar] [CrossRef] [PubMed]
- Meade, M.J.; Weir, T. Predicted and achieved overjet and overbite measurements with the Invisalign appliance: A retrospective study. Angle Orthod. 2024, 94, 3–9. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shahabuddin, N.; Kang, J.; Jeon, H.H. Predictability of the deep overbite correction using clear aligners. Am. J. Orthod. Dentofacial Orthop. 2023, 163, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Moshiri, S.; Araújo, E.A.; McCray, J.F.; Thiesen, G.; Kim, K.B. Cephalometric evaluation of adult anterior open bite non-extraction treatment with Invisalign. Dental Press J. Orthod. 2017, 22, 30–38. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Greco, M.; Rombolà, A. Precision bite ramps and aligners: An elective choice for deep bite treatment. J. Orthod. 2022, 49, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Gong, B.; Xie, X.; Cao, L.; Gu, Y.; Sun, Y.; Bai, Y. The effectiveness of clear aligners in levelling the curve of Spee and related maxillofacial factors in patients with a deep overbite. Australas. Orthod. J. 2024, 40, 169–177. [Google Scholar] [CrossRef]
- Finkleman, S.; Cohanim, B.; Tai, S.K.; Khosravi, R.; Huang, G. Does planned molar intrusion with aligners assist with closure of anterior open bite? Am. J. Orthod. Dentofac. Orthop. 2024, 166, 330–349.e1. [Google Scholar] [CrossRef] [PubMed]
- Fujiyama, K.; Yujin, S.; Tanikawa, C.; Yamashiro, T.; Guo, X.; Deguchi, T. Comparison of clinical outcomes between Invisalign and conventional fixed appliance therapies in adult patients with severe deep overbite treated with nonextraction. AJO-DO 2022, 161, 542–547. [Google Scholar] [CrossRef]
- Garnett, B.S.; Mahood, K.; Nguyen, M.; Al-Khateeb, A.; Liu, S.; Boyd, R.; Oh, H. Cephalometric comparison of adult anterior open bite treatment using clear aligners and fixed appliances. Angle Orthod. 2019, 89, 3–9. [Google Scholar] [CrossRef]
- Husain, F.; Warunek, S.; Gurav, A.; Giangreco, T.; Tanberg, W.; Al-Jewair, T. Influence of Invisalign precision bite ramp utilization on deep bite correction and root length in adults. Angle Orthod. 2024, 94, 488–495. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karalikkattil, T.L.; Batra, N.; Vivek, C.R.; Reddy, V.; Manimegalan, P.; Tom, A. Effectiveness of Invisalign Treatment on Open Bite Correction. J. Pharm. Bioallied Sci. 2024, 16 (Suppl. 1), S850–S852. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meade, M.J.; Blundell, H.; Weir, T. Predicted overbite and overjet changes with the Invisalign appliance: A validation study. Angle Orthod. 2024, 94, 10–16. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moradinejad, M.; Harrell, R.E.; Mousavi, S.M.; Alavi, M.; Basseri, A.D.; Feiz, A.; Daryanavard, H.; Rakhshan, V. Effects of clear aligners on the vertical position of the molar teeth and the vertical and sagittal relationships of the face: A preliminary retrospective before-after clinical trial. BMC Oral Health 2024, 24, 234. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Steele, B.P.; Pandis, N.; Darendeliler, M.A.; Papadopoulou, A.K. A comparative assessment of the dentoskeletal effects of clear aligners vs miniplate-supported posterior intrusion with fixed appliances in adult patients with anterior open bite. A multicenter, retrospective cohort study. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 214–228.e4. [Google Scholar] [CrossRef] [PubMed]
- Blundell, H.L.; Weir, T.; Byrne, G. Predictability of anterior open bite treatment with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2023, 164, 674–681. [Google Scholar] [CrossRef] [PubMed]
- Bowman, E.; Bowman, P.; Weir, T.; Dreyer, C.W.; Meade, M.J. Evaluation of the predicted vs. achieved occlusal outcomes with the Invisalign® appliance: A retrospective investigation of adult patients. Int. Orthod. 2023, 21, 100746. [Google Scholar] [CrossRef] [PubMed]
- Burashed, H. The efficacy of anterior open bite closure when using Invisalign’s optimized extrusion versus conventional attachments. J. World Fed. Orthod. 2023, 12, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Burashed, H.; El Sebai, R. Quantifying the efficacy of overbite reduction in patients treated with clear aligners using optimized versus conventional attachments. J. World Fed. Orthod. 2023, 12, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, G.; Campobasso, A.; Garrisi, L.; Battista, G.; D’aNtò, V.; Mandelli, A.; Mandelli, G.; Ambrosi, A.; Gastaldi, G. The accuracy of biomechanical mechanisms for dental deep bite correction using the Invisalign system. Australas. Orthod. J. 2024, 40, 87–95. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, G.D.; Sterne, A.C.J. Cochrane Handbook for Systematic Review of Intervention Version 5.1.0 [Updated March 2011]. The Chocrane Collaboration. 2011. Available online: www.handbook.cochrane.org (accessed on 1 January 2025).
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Arat, M.; Iseri, H. Orthodontic and orthopaedic approach in the treatment of skeletal open bite. Eur. J. Orthod. 1992, 14, 207–215. [Google Scholar] [CrossRef]
- Morton, J.; Derakhshan, M.; Kaza, S.; Li, C. Design of the Invisalign system performance. Semin. Orthod. 2017, 23, 3–11. [Google Scholar] [CrossRef]
- Charalampakis, O.; Iliadi, A.; Ueno, H.; Oliver, D.R.; Kim, K.B. Accuracy of clear aligners: A retrospective study of patients who needed refinement. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 47–54. [Google Scholar] [CrossRef]
- Hamilton, P. Comparison of Open Bite Closure Outcomes: Clear Aligners vs. Skeletal Anchorage Molar Intrusion. Master’s Thesis, University of North Carolina Chapel Hill, Chapel Hill, NC, USA, 2020. [Google Scholar]
- Grünheid, T.; Loh, C.; Larson, B.E. How accurate is Invisalign in non extraction cases? Are predicted tooth positions achieved? Angle Orthod. 2017, 87, 809–815. [Google Scholar] [CrossRef]
- Bates, M.T.; Shroff, B.; Carrico, C.K.; Kheirandish, N.; Lindauer, S.J. Perceived efficacy of extrusion of maxillary lateral incisors with aligners. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Savignano, R.; Valentino, R.; Razionale, A.V.; Michelotti, A.; Barone, S.; D’aNtò, V. Biomechanical Effects of Different Auxiliary-Aligner Designs for the Extrusion of an Upper Central Incisor: A Finite Element Analysis. J. Health Eng. 2019, 2019, 9687127. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nucera, R.; Dolci, C.; Bellocchio, A.M.; Costa, S.; Barbera, S.; Rustico, L.; Farronato, M.; Militi, A.; Portelli, M. Effects of Composite Attachments on Orthodontic Clear Aligners Therapy: A Systematic Review. Materials 2022, 15, 533. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jamilian, A.; Emami, M.S.; Showkatbakhsh, A. The effect of anterior inclined plane treatment on the dentoskeletal of Class II division 1 patients. Saudi J. Kidney Dis. Transplant. 2007, 25, 130–132. [Google Scholar] [CrossRef] [PubMed]
- Pasciuti, E.; Coloccia, G.; Inchingolo, A.D.; Patano, A.; Ceci, S.; Bordea, I.R.; Cardarelli, F.; Di Venere, D.; Inchingolo, F.; Dipalma, G. Deep Bite Treatment with Aligners: A New Protocol. Appl. Sci. 2022, 12, 6709. [Google Scholar] [CrossRef]
- Liu, Y.; Hu, W. Force changes associated with different intrusion strategies for deep-bite correction by clear aligners. Angle Orthod. 2018, 88, 771–778. [Google Scholar] [CrossRef]
- Galan-Lopez, L.; Barcia-Gonzalez, J.; Plasencia, E. A systematic review of the accuracy and efficiency of dental movements with Invisalign®. Korean J. Orthod. 2019, 49, 140–149. [Google Scholar] [CrossRef]
- Yan, X.; Zhang, X.; Ren, L.; Yang, Y.; Wang, Q.; Gao, Y.; Jiang, Q.; Jian, F.; Long, H.; Lai, W. Effectiveness of clear aligners in achieving proclination and intrusion of incisors among Class II division 2 patients: A multivariate analysis. Prog. Orthod. 2023, 24, 12. [Google Scholar] [CrossRef]

| Articles | Reason of Exclusion |
|---|---|
| [31] | The authors analyze overbite in a heterogeneous sample considering patients who underwent extraction and genioplasty |
| [32] | The authors analyze extraction cases |
| [33] | Two of the 24 patients included in the sample underwent extraction of four premolars |
| [34] | Patients <18 years old are also analysed from a cephalometric perspective between T1 and T2, without considering the data provided by ClinCheck |
| [35] | Patients <18 years old and evaluation of deep bite in terms of the IMPA value |
| [16] | The authors consider only the value of intrusion and do not report overbite values |
| [36] | The authors evaluate the leveling of the Spee curve, but the overbite data is not analyzed |
| [37] | There is a loss of the sample at T3. At T1, 36 patients are analyzed, and at T3, only 14 remain. Additionally, there is no evaluation of overbite through ClinCheck (T2) |
| [38] | The study compares two groups, but it does not analyze the correction of overbite through the ClinCheck software (T2) |
| [39] | Cephalometric evaluation between two groups of patients treated with two different devices in hyperdivergent patients, without considering the correction of overbite through software (T2) in patients treated with aligners |
| [14] | The correction of overbite at T2 through ClinCheck is not considered |
| [13] | The correction of overbite at T2 through ClinCheck is not considered |
| [40] | The correction of overbite at T2 through ClinCheck is not considered |
| [41] | The correction of overbite at T2 through ClinCheck is not considered |
| [18] | The correction of overbite at T2 through ClinCheck is not considered |
| [42] | The authors compare whether there are differences between the ClinCheck software and Geomagic Control X software in predicting the correction of overbite in open-bite subjects. However, they do not analyze the actual correction after treatment (T3) |
| [43] | The correction of overbite at T2 through ClinCheck is not considered |
| [24] | The correction of overbite at T2 through ClinCheck is not considered in the comparison between a group of patients treated with fixed appliances and a group treated with aligners |
| [27] | The correction of overbite at T2 through ClinCheck is not considered |
| [44] | The correction of overbite at T2 through ClinCheck is not considered |
| Parameter | Blundell et al., 2022 [10] | Blundell et al., 2021 [20] | Blundell et al., 2023 [45] | Bowman et al., 2023 [46] | Burashed et al., 2023 [47] | Burashed et al., 2023 [48] | Fiorillo et al., 2024 [49] |
|---|---|---|---|---|---|---|---|
| Study design | Retrospective | Retrospective | Retrospective | Retrospective | Retrospective cohort | Retrospective cohort | Retrospective |
| Sample size | 68 | 42 | 76 | 33 | 86 | 78 | 25 |
| Sex | / | / | 53 F 23 M | 21 F 12 M | 57 F 29 M | 29 M 49 F | 12 M 13 F |
| Age | ≥18 y | ≥18 y | 35 ± 2 y | 32.7 y | 31.8 ± 10.1 y | 34.9 ± 14.3 y | 32.28 y |
| CA system | Invisalign | Invisalign | Invisalign | Invisalign | Invisalign | Invisalign | Invisalign |
| No. of CA | ≥14 | ≥14 | ≥14 | / | 25.0 ± 10.8 | 29.8 ± 12.9 | ≥14 |
| Material | N = 29 Smart track + bite ramp N = 39 EX30 | Smart track | Smart track | Smart track | Smart track | Smart track | Smart track |
| Presence of second molars | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Biteramp, biteblock and attachments | (N = 29) bite ramp | / | POBBs | / | A (n = 42) Conventional attachments B (n = 44) Optimized attachments | A (n = 42) Conventional attachments B (n = 36) Optimized attachments (G5) | Conventional attachment (3 mm, 1.5 mm) 0.20 ± 0.05 mm vertical jump |
| Elastics | / | / | / | / | / | / | / |
| TADs | / | / | / | / | / | / | / |
| Software | Geomagic Control X software (3DSystem Rock Hill SC) version 2017.0.3 | Geomagic Control X software (3DSystem Rock Hill SC) version 2017.0.3 | Geomagic Control X software (3DSystem Rock Hill SC) version 2017.0.3 | Geomagic Control X software (3DSystem Rock Hill SC) version 2017.0.3 | ClinCheck software version 2023 | ClinCheck software version 2023 | Geomagic Control X software (3DSystem Rock Hill SC) version 2017.0.3 |
| Measure | Vertical distance between the mid-point of the incisal edge of the upper left central incisor and the mid-point between the incisal edges of the lower left central and lateral incisors | Vertical distance between the midpoint of the incisal edge of the upper left central incisor and the midpoint between the incisal edges of the lower left central and lateral incisors | Vertical distance between the midpoint of the incisal edge of the upper left central incisor and the midpoint between the incisal edges of the lower left central and lateral incisors | Vertical distance between the midpoint of the incisal edge of the upper left central incisor and the midpoint between the incisal edges of the lower left central and lateral incisors | / | / | Distance between the marginal edges of the upper and lower incisors |
| Type of malocclusion | Deep bite | Deep bite | Open bite | Deep bite | Open bite | Deep bite | Deep bite |
| Skeletal pattern | / | / | / | / | / | / | / |
| Treatment duration | / | / | 16.4 months | / | / | / | / |
| CA change regime | 2 weeks | 2 weeks | 2 weeks | 2 weeks | 10 days | 10 days | / |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boccuzzi, M.; Cosola, S.; Butera, A.; Genovesi, A.; Laborante, T.; Castaldo, A.; Zizza, A.; Oldoini, G.; Nota, A.; Tecco, S. Predictability of ClinCheck in Overbite Correction with Aligners: A Systematic Review. Appl. Sci. 2025, 15, 7268. https://doi.org/10.3390/app15137268
Boccuzzi M, Cosola S, Butera A, Genovesi A, Laborante T, Castaldo A, Zizza A, Oldoini G, Nota A, Tecco S. Predictability of ClinCheck in Overbite Correction with Aligners: A Systematic Review. Applied Sciences. 2025; 15(13):7268. https://doi.org/10.3390/app15137268
Chicago/Turabian StyleBoccuzzi, Michela, Saverio Cosola, Andrea Butera, Annamaria Genovesi, Teresa Laborante, Attilio Castaldo, Agostino Zizza, Giacomo Oldoini, Alessandro Nota, and Simona Tecco. 2025. "Predictability of ClinCheck in Overbite Correction with Aligners: A Systematic Review" Applied Sciences 15, no. 13: 7268. https://doi.org/10.3390/app15137268
APA StyleBoccuzzi, M., Cosola, S., Butera, A., Genovesi, A., Laborante, T., Castaldo, A., Zizza, A., Oldoini, G., Nota, A., & Tecco, S. (2025). Predictability of ClinCheck in Overbite Correction with Aligners: A Systematic Review. Applied Sciences, 15(13), 7268. https://doi.org/10.3390/app15137268