Abstract
The adoption of healthcare technologies has grown significantly, with real-time location systems (RTLSs) gaining particular attention. Despite decades of research, gaps persist in understanding the current state of the field and its future directions. This scoping review, conducted by PRISMA guidelines, identified 1718 articles retrieved from six databases, from which 83 were included. The findings reveal a dominance of U.S.-based case studies and a lack of systematic literature reviews. While RFID is the most commonly used technology, alternative solutions are emerging, though few studies explore their combined use. The emergency department is the most studied setting, focusing on patient flow. However, case study quality varies, which affects replicability, and literature reviews often fail to justify technological choices adequately. RTLS benefits include improved efficiency, enhanced patient safety, and cost reduction, but challenges such as precision issues and signal interference persist. RTLS also serves as a foundation for digital twins, integrating AI and Industry 4.0 technologies for more sustainable healthcare operations. Technological advancements may shift perceptions of RTLS challenges and benefits, highlighting the need for analysis by technology type and release date. Additionally, current MeSH terms fail to adequately cover healthcare technologies, resulting in the exclusion of relevant studies.
1. Introduction
Healthcare is one of the primary sectors in modern society, accounting for a substantial portion of global investments and remaining a top priority on the agendas of various countries. Healthcare institutions and managers have faced several challenges, including the increasing pressure to enhance productivity, reduce costs, and improve resource management [1]. In this context, methodologies such as project management techniques, lean healthcare, Six Sigma, and implementing new technologies have emerged as potential solutions in scientific research and practice [2,3,4]. These approaches are directly associated with hospital operational excellence and are frequently combined with emerging technologies [5]. Furthermore, lean is a facilitator for implementing Industry 4.0 technologies, acting as a foundational step before technological adoption [6]. However, healthcare processes are inherently complex, involving multiple stakeholders and technical specificities that make their study challenging [7,8], making hospital operations a critical area of focus.
Despite the growing adoption of technology in healthcare, in some fields, it remains an underdeveloped sector compared to other industries [9]. For example, real-time location system (RTLS) development in hospitals is often hindered by high implementation costs, the need for customisation to diverse organisational structures, and the absence of a universally optimal sensor. Deployment also faces significant barriers, including limited infrastructure, staff resistance, patient privacy concerns, and low perceived usefulness by some healthcare providers, despite documented gains in operational efficiency and safety [10]. Various authors have highlighted the vast amounts of data generated in hospitals, often fraught with errors, gaps, lack of integration, and low reliability, hindering the use of advanced approaches like big data analytics and process mining [11]. Furthermore, when implementing improvement approaches such as lean healthcare, the lack of reliable data is a recurrent challenge [12]. In this context, by automatically collecting workflow data, RTLS can improve the quality of records while reducing the need for manual data entry and freeing up resources [13].
The emergence and popularisation of new technologies have opened doors for innovative data collection methods with higher accuracy, accessibility, and real-time data exchange. Real-time Location Systems (RTLSs) are a combination of sensors for the identification and tracking of the location of people or assets in real or almost real time [14]. The degree of real-time tracking depends on technological limitations and cost-effectiveness, as not all resources require data collection at millisecond intervals. For instance, tracking assets that move only within hourly intervals would result in unnecessary resource consumption [14,15]. This automatic data collection, combined with the ability to process and interpret it, enables detailed studies of patient, staff, and product flows, facilitating data-driven improvements with proven benefits to operations [10]. For instance, these technologies have been used to enhance the understanding of emergency departments by quantifying physicians’ time allocation and movements [16]. Furthermore, integrating RTLS with artificial intelligence, simulation techniques, cloud computing, and other Industry 4.0 technologies facilitates the creation of digital twins. These are virtual models that evolve in real time based on data from their real counterparts, enabling simulation and feedback to support decision making [17] , which can significantly enhance hospital operations management and more sustainable systems [17,18,19], by optimising resource utilisation, minimising redundancies, and supporting lean process improvements [20,21]. One of the challenges of digital twins is collecting diverse and unstructured data, which can be mitigated through the use of RTLS [18]. Nonetheless, current research appears not to reflect the opportunities this sector presents fully [9,10], highlighting the need to understand the state of research and the direction required for the broader adoption of RTLS in healthcare.
Thus, this article aims to characterise the current research on indoor location technologies in healthcare. This characterisation includes identifying the most commonly used technologies, the healthcare contexts in which they are applied, the methodological approaches adopted in literature, and the primary outcomes, barriers, and success factors reported. In addition, we analyse the first authors, countries, and institutions associated with the selected studies. This enables the identification of leading research groups, regional and institutional patterns, and broader trends in developing and applying indoor location technologies in healthcare. Understanding where and by whom the research is being conducted can offer valuable insights into the maturity and focus areas of the field across different contexts. The following research questions guide this scoping review:
- What are the characteristics and methodological approaches of existing research on indoor location technologies in healthcare? Who are the primary authors, and which countries and institutions contribute significantly to this topic?
- Which technologies are predominant, and in which healthcare context are they typically adopted?
- Do published works discuss factors contributing to success or failure? If so, what are these factors?
These research questions were selected because understanding the research landscape, technology adoption, and influencing factors is essential for guiding future development and implementation efforts. By concentrating on these core areas, this review aims to identify key trends, common application domains, and critical success factors, while also revealing gaps in the literature. Although other aspects of RTLS in healthcare, such as detailed technical specifications or economic evaluations, are important, they were not emphasised to maintain a comprehensive yet focused overview that facilitates targeted research and practical applications.
The following section will present the methodology of the review. This will be followed by the presentation and discussion of the results obtained from the analysis of the included articles, concluding with final remarks and considerations.
2. Materials and Methods
This scoping review was developed following the PRISMA extension for scoping reviews [22]. A scoping review was selected to comprehensively map the diverse and emerging literature on indoor location technologies in healthcare, enabling the identification of key concepts and research gaps in a field lacking extensive prior synthesis. The complete methodological approach adhered to the protocol established by Lopes et al. [23]. A summary of the key methodological steps is provided below to aid in understanding.
2.1. Search Strategy
The search strategy was designed by two researchers and reviewed by a third, adhering to the PRESS guidelines to ensure reliability [24]. Searches were conducted across six databases: PubMed, Cochrane, Scopus, Web of Science, Embase/MEDLINE, and Worldwide Science. The authors chose to include grey literature references, as these can make significant contributions to literature reviews and help mitigate publication bias and delays inherent to the traditional publication process [25]. The following Medical Subject Headings (MeSH) terms were combined using “AND” operators, the complete search strategy is available in the supplementary Material:
- (Hospitals OR Health Services OR Health Facilities).
- (Patient Identification Systems OR Geographic Information Systems OR Remote Sensing Technology).
- (Workflow OR Process Assessment, Health Care).
Additionally, non-indexed technological terms not included in the MeSH library were added to enhance the sensitivity of the search. Synonyms for MeSH terms and subcategories were also included, along with database-specific adjustments. The complete search strategy is available in Supplementary Table S1. After the initial searches, the authors chose not to apply filters related to time, study design, or source.
2.2. Inclusion and Exclusion Criteria
The inclusion and exclusion criteria were defined before the searches were conducted using the PCC (Population, Concept, Context) framework. Table 1 summarises the details for each dimension.

Table 1.
Inclusion and exclusion criteria.
2.3. Data Analysis and Extraction
At least two independent researchers conducted all stages of data analysis and extraction. In cases of disagreement, a senior investigator was responsible for reviewing the paper and determining the appropriate course of action. Before starting this phase, an alignment meeting was held to review the research protocol, objectives, and key characteristics required to ensure consistency among reviewers. Additionally, all reviewers participated in a training session using a similar database and discussed the results.
Data analysis followed the same procedures, utilising a predefined spreadsheet to aid the process. The main findings were grouped qualitatively (e.g., the analysis of Hospital Areas followed the classification of Lima et al. [12]) for more straightforward presentation, and quantified to generate charts and quantitative indicators that provide an overview of the research landscape.
3. Results
The search strategy identified 1718 documents, which were systematically reviewed, leading to the inclusion of 83 articles. Figure 1 shows the PRISMA diagram for the search process, complemented by Supplementary Table S2, which summarises the articles included in the literature review.

Figure 1.
Prisma diagram for the scoping review.
While the inclusion of MeSH terms expanded the search parameters, it also yielded a substantial number of articles, many of which fell outside the scope of the study. The main reasons for exclusion were studies focused on outdoor location tracking, articles referring to patient monitoring or identification without attributes of time and location (e.g., remote monitoring of chronic patients), and articles that did not present detailed characteristics of the technology used in the full text.
3.1. General Characteristics
Although no time restriction was applied, the articles included in the analysis, after using the inclusion and exclusion criteria, were published between 2005 and 2022. The highest publication peak occurred between 2011 and 2013, with an average of nine articles published each year, as shown in Figure 2.
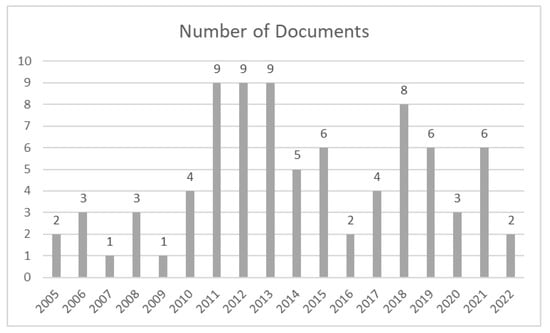
Figure 2.
Documents per year.
The average number of authors per article was 5.07, with a maximum of 13 authors and a minimum of 1. This relatively high average indicates that research on indoor location technologies in healthcare typically involves multidisciplinary collaboration, reflecting the complexity and the need for diverse expertise in this field. The median and mode were both four authors, totalling 421 contributors across the analysed studies. Indoor location technologies were applied in various hospital areas. Following the classification proposed by Lima et al. [12], the study areas were characterised as General Hospital/Non-specified (n = 25), Emergency Department (n = 15), and Surgery (n = 10). Other areas included Outpatient (n = 5), Trauma Department and Radiology (n = 4 each), Pathology and ICU (n = 3 each), and Primary Care, Ophthalmology, and Oncology (n = 2 each). The remaining areas had only one study each. A small number of studies have focused on more than one department [26,27,28,29]. There is a noticeable predominance of publications from the United States, with 36, followed by Taiwan and Germany, each with 5. The most published authors were James E. Stahl and Vimla L. Patel, with four articles each. Highlighting these key contributors helps identify influential researchers and research networks driving advancements in RTLS, which may guide future collaborations and indicate centres of expertise.
Most articles were classified as Case Studies (68), followed by Literature Reviews (12). There was also one System Development article without a technology application, one Framework Development article, and one Survey article. No scoping reviews were found. Most articles (77) were published in full text, while only six were published as abstracts. In the practical articles, the motivation for implementing RTLS and the characteristics of the institution involved in the case study are consistently reported; however, few justify the choice of a specific technology, lacking a comprehensive literature review on the available options.
3.2. Literature Reviews
None of the 12 documents classified as literature review (Supplementary Table S3) were scoping reviews. The documents were primarily non-systematic literature reviews with different objectives from the present scoping review. Considering the three systematic reviews, only one adhered to the PRISMA guidelines [30], and none conducted a quality analysis of the included articles. Supplementary Table S2 summarises the main characteristics of these documents.
3.3. Technologies and Workflows
Among the studies analysed, Radio Frequency Identification (RFID) was the most commonly used technology, appearing in 60 studies, followed by Bluetooth Low Energy (BLE), which was used in 9 articles. Over time, these technologies have maintained mainly RFID as the most popular choice, although new options are increasingly gaining traction. Of the 46 studies produced by 2014, 35 used RFID, and none employed BLE; only 4 studies used multiple technologies [31,32,33,34]. However, after 2014, 25 of the 37 studies employed RFID, 9 used BLE, and 6 used more than one technology [10,27,35,36,37,38]. This trend is illustrated in Figure 3, which displays the number of publications by year and technology for the main identified technologies.
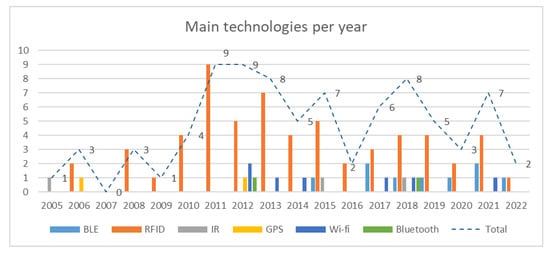
Figure 3.
Main technologies per year.
In terms of workflows, the majority of publications analyse patient flows (45), followed by staff (25), materials (13), and other flows (6). Only 19 studies examined multiple flows, the most common combination being patient and staff flows. The primary variables measured were geospatial location and time, occasionally supplemented with additional information to enhance the analysis.
Although many articles aim to improve workflows, most do not present the process before the technology implementation, making it difficult to understand the changes. The documents focus primarily on explaining the implementation methodology and the improvements in process metrics, such as waiting time.
3.4. Gains and Improvements
The most common benefits identified are related to efficiency, measured by Length of Stay (LOS) and waiting time, improved patient safety, and cost reduction [13,31,39,40,41,42,43,44,45]. Among the evaluated studies, several indicated that the technologies used were accurate and potentially viable for tracking resources, patients, and staff [13,14,29,30,32,36,37,39,41,44,46,47,48,49,50,51,52,53,54,55,56,57,58]. Notably, one study using BLE demonstrated precision above 99% in location accuracy at zone level, significantly increasing patient experience, safety, and operational efficiency [39]. While this was the only study providing such specific precision data, it exemplifies the potential performance levels achievable with these technologies. Additionally, most of these studies emphasised the benefits of improving workflows and patient care, which could provide valuable data for assessing service quality in the future [13,14,29,37,47,48,49,50,51,54,56,58,59].
Several studies reported time savings in hospital activities, including shorter waiting times [43,45,58,60,61], reduced delays in medical care and locating equipment [26,42,48], and faster test completion [45]. One study used RFID to track laboratory samples, reducing sample identification time and contamination risk since [33].
Additionally, studies highlighted the benefits of indoor location technologies for patient or staff safety [9,13,30,38,39,40,41,61,62,63,64], and some mentioned cost reduction advantages in hospital activities [42,65,66,67]. However, safety is typically not a direct outcome but an assumed improvement resulting from enhanced workflows and operational efficiency.
3.5. Limitations and Risks
A significant portion of the studies did not explicitly address the main limitations and risks related to technology use, instead highlighting recurring challenges identified in the literature, which limits the analysis of this topic. However, the most cited difficulty was the lack of precision and sensitivity of the technologies or their intrinsic limitations [9,27,31,55,58,62,66,68]. Also, the lack of infrastructure (physical or technological) in locations where the technologies were applied and signal interference from medical equipment, materials such as metal or liquids, and even between tags was reported in some articles [9,13,27,62,65,67,69,70,71].
Implementation and hardware costs were obstacles reported [9,44,49,55,60,61,65,72,73]. However, these focus primarily on implementation and do not discuss maintenance costs. User acceptance [41,49,59], both by patients and healthcare staff, and the need for adequate training were described as limitations in some references [62,63,74], in addition to other user-related issues, including the Hawthorne effect [43,56,75], limited sample space and time [48,56,58,60,76], and experimental or controlled environments impacting the technology’s actual effectiveness.
Lastly, articles mentioned difficulties in processing and analysing the data collected and privacy and data security risks [44,60,62,65,67,73,77]. A lack of comparison with other geolocation methods was also cited as a limitation in two articles [50,78] and two papers noted that the lack of patient satisfaction evaluation was a limitation [45,46].
4. Discussion
The use of digital technologies in healthcare has emerged as a prominent area of practice, utilising routine and innovative technologies to meet health-related needs [79]. Specifically, indoor positioning technologies have the potential to provide real-time, accurate data collection, thereby improving operational efficiency [39,41,61,80]. However, despite publications dating back to 2005, notable gaps remain in the scientific development of this topic.
Most of the identified reviews were non-systematic, focusing on presenting technologies and discussing their benefits rather than answering a specific question. This highlights a gap in comparative studies, making it challenging for healthcare organisations to select the most suitable technology for implementation. This is evident from the large number of case studies, many of which lack a robust literature review to justify their decisions. Many studies are driven by the feasibility of the technology itself, aiming to validate a preselected tool rather than conducting a thorough comparative analysis [33,78,80]. Additionally, there appears to be significant variability in the quality of the articles, with structures that are often dissimilar and do not adhere to the case report or literature review guidelines commonly adopted in health studies [81]. In this regard, it would be beneficial for the authors of future publications to consider adapting quality checklists when structuring their work.
RFID has been the dominant choice regarding the technologies themselves, primarily due to its low cost and ease of implementation, with numerous solutions already available on the market. However, industrial advancements seem to have driven a shift in recent years, with the rise of BLE starting in 2015. One point of concern is the limited number of publications exploring the combined use of different technologies, a strategy employed in other contexts to address precision and cost issues, for example. Although some manufacturers have started incorporating this approach into their offerings, the studies do not yet reflect this trend, possibly due to the time required for scientific publications. Precision has become a significant challenge [27,31,55,62,66,68], which can be mitigated by applying multiple positioning technologies in conjunction with probabilistically mapped movement models. Given the specificities of each workflow and the implementation environment, no generic solution fits all cases, making tailored implementations essential. Costs appear to be decreasing, driven by the increasing popularity and emergence of new technologies.
The diversity of possible applications for indoor positioning is evident from the various hospital areas studied and the different types of workflows analysed (Supplementary Table S2). The emergency department and surgery stand out, aligning with the lean healthcare literature [12]. However, there is a noticeable gap in studies examining different hospital areas and their interactions, which could be an area for future research, as this is one of the potential improvements proposed by RTLS. In terms of workflows, patient flows are given priority, likely reflecting value-based healthcare concepts [82]. Staff flows are also frequently considered, but material flows receive less attention, presenting opportunities for further research. This gap represents a significant operational disadvantage, as the efficiency of hospital care depends on several factors and characteristics [83]. The lack of comprehensive studies encompassing all logistical aspects of the hospital environment limits the implementation of more integrated and effective hospital management solutions
As presented in the results, the main benefits identified were improved efficiency (measured by LOS and waiting time), enhanced patient safety, and cost reduction [13,31,39,40,41,42,43,44,45]. Challenges include data accuracy, user acceptance, and signal interference. However, some of these benefits and challenges are contradictory across different studies, making it essential to analyse them within the context of the technology used and the publication date, as advancements in the field are ongoing. For example, accuracy is sometimes cited as a limitation [31,55,68], while, in other instances, it is regarded as a benefit [67]. These differing perspectives often depend on the specific implementation of the technology and the period in which the study was conducted, highlighting the need for a nuanced approach when interpreting the results. While costs have been highlighted, there is a lack of comparative studies on implementation, maintenance, and long-term savings, leaving the real advantage and feasibility of RTLS use open to debate. One point of concern is that a significant portion of the studies do not present the initial workflows or propose modelling improvements or process enhancements. This may indicate an opportunity for further research, suggesting that these activities could be enhanced following the implementation of RTLS, potentially combined with other approaches such as process mining.
Finally, a critical issue identified in the research is the limited scope of existing studies on indoor positioning systems in hospital settings, which primarily focus on applying a single pre-selected technology without a deeper analysis or justification for this choice. This compromises the replicability and usefulness of these studies for future similar applications and limits the overall results, which is especially significant as few articles address the challenges of maintaining RTLS systems and integrating them with other approaches. This review intends to address this gap by systematically mapping the key technologies employed, their application contexts, and the factors influencing their adoption. This provides insights into technological trends and supports more informed decision making in future research and implementation.
Real-Time Location Systems (RTLSs) are among the key technologies enabling the development of digital twins (DTs), models that integrate with reality and exchange data in real time [17,19,84,85]. Although this research primarily focuses on location systems, many publications related to DTs do not explicitly use the term, instead referring to concepts such as the Internet of Things (IoT) or Cyber–Physical Systems [17]. In this context, overcoming the challenges associated with RTLS can drive the advancement of DTs, unlocking benefits such as improved workflows, data-driven decision making, and enhanced patient experiences, all of which contribute to more sustainable systems [17,86]. Addressing these challenges to facilitate data collection is a key enabler of digital twins and a fundamental step toward integrating advanced technologies in hospital operations management, such as artificial intelligence and big data analytics, ultimately driving the development of smart hospitals [18,19,86,87].
This study has some limitations. The results are constrained by the search strategy and the databases selected, which may have excluded relevant studies. Industry research was not included, as it is often excluded from academic publications due to patent-related secrecy. Additionally, a formal bibliometric analysis to identify potential biases from recurring groups of researchers was not conducted; this will be explored in a future publication.
MeSH (Medical Subject Headings) terms are an important tool for finding specific information in databases. The absence of MeSH terms related to these technologies, especially newer ones, appears to be a limitation, as relevant articles may be excluded, thereby narrowing the scope of searches. This limitation was likely overlooked, given that few of the analysed articles were reviews, and only one explicitly mentioned the lack of MeSH terms as a restriction [88]. Of all the articles used in the research, 12 were review articles; of these, only 3 posed well-defined research questions. This suggests that researchers may not have recognised the absence of MeSH terms as a potential barrier to the development of these studies.
5. Conclusions
This work consisted of a scoping review of documents related to indoor RTLS in healthcare, enabling the identification of the current state and gaps in academic knowledge on the topic.
Despite the considerable number of publications on the subject, no prior review like this one has been identified. Current research lacks robust examples of technology application across various hospital areas, with a clear focus on emergency departments and patient flows. It is necessary to explore the hospital environment as a whole. While RFID dominates the field, there is a need to investigate the combined use of different technologies, which could enhance benefits and overcome obstacles. Further studies are needed on the costs involved, not only in the implementation but also in the long-term maintenance of equipment. Finally, the existing MeSH terms may be insufficient to adequately detail research on healthcare technologies, and the inclusion of new terms in indexing is suggested.
The main benefits identified relate to operational improvements, reflected in metrics such as LOS and waiting time. However, implementation challenges are rarely presented in detail or discussed thoroughly. Furthermore, technological advances have led to the evolution of advantages, barriers, and technologies over the years, necessitating that comparisons account for factors such as publication date and the technologies employed. Overcoming these challenges is an essential step in enabling the development of digital twins, which supports data collection and the integration of artificial intelligence and other technologies. In this context, with current data protection laws, security and privacy are emerging as key challenges in using real-time patient tracking systems.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app15116231/s1, Table S1: Search Strategy; Table S2: Papers General Characteristics; Table S3: Identified Literature Reviews. References cited in the Supplementary Materials are also included in this reference list to ensure all sources are properly acknowledged [89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112].
Author Contributions
Conceptualisation, E.T.L., D.C.L., S.E.S.F., and R.M.L.; methodology, E.T.L., D.C.L., S.E.S.F., and R.M.L.; validation, B.S.G., S.E.S.F., and R.M.L.; formal analysis, E.T.L., D.C.L., G.P., I.O.A., G.A.K., and P.H.S.d.M.; investigation, E.T.L., D.C.L., G.P., I.O.A., G.A.K., and P.H.S.d.M.; writing—original draft preparation, E.T.L., G.P., I.O.A., G.A.K., and P.H.S.d.M.; writing—review and editing, E.T.L., D.C.L., B.S.G., S.E.S.F., and R.M.L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was partially supported by FCT—Fundação para a Ciência e Tecnologia within the R&D Units Project Scope UIDB/00319/2023. This research received funding from the Scientific Initiation Program of the School of Health Sciences—PIC/ESCS through the funds of the Foundation for Teaching and Research in Health Sciences—FEPECS.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| MeSH | Medical Subject Headings |
References
- Figueroa, C.A.; Harrison, R.; Chauhan, A.; Meyer, L. Priorities and challenges for health leadership and workforce management globally: A rapid review. BMC Health Serv. Res. 2019, 19, 239. [Google Scholar] [CrossRef] [PubMed]
- Lopes, E.T.; Lopes, D.C.; Souza, T.A.; Lima, R.M.; Souza, A.L.A.C. Project Management in Hospital Environments: A 5-Year Systematic Literature Review. Springer Proc. Math. Stat. 2023, 431, 275–287. [Google Scholar] [CrossRef]
- Santos, A.C.d.S.G.d.; Reis, A.d.C.; de Souza, C.G.; Santos, I.L.; Ferreira, L.A.F.; Senna, P. Measuring the current state-of-the-art in lean healthcare literature from the lenses of bibliometric indicators. Benchmarking 2023, 30, 3508–3533. [Google Scholar] [CrossRef]
- Wahyuni, S.; Pranata, S.; Setiaprabhawa, F.B.; Maftuchah, L. Exploring the Trend of Technology Use and Innovation in Health Care Service in Hospitals through a Bibliometric Analysis. Babcock Univ. Med. J. 2024, 7, 51–63. [Google Scholar] [CrossRef]
- Hoefsmit, P.C.; Heuvel, J.v.D.; Zandbergen, R.; Does, R. Operational excellence in hospitals. Int. J. Lean Six Sigma 2024, 15, 957–964. [Google Scholar] [CrossRef]
- Bittencourt, V.L.; Alves, A.; Leão, C.P. Industry 4.0 triggered by Lean Thinking: Insights from a systematic literature review. Int. J. Prod. Res. 2021, 59, 1496–1510. [Google Scholar] [CrossRef]
- Rebuge, Á.; Ferreira, D.R. Business process analysis in healthcare environments: A methodology based on process mining. Inf. Syst. 2012, 37, 99–116. [Google Scholar] [CrossRef]
- Lima, R.M.; Lopes, E.T.; Lopes, D.C.; Gonçalves, B.S.; Cunha, P.G. Hospital operations management—Characterising patients’ process flows in emergency departments. Bus. Process Manag. J. 2024, 30, 207–231. [Google Scholar] [CrossRef]
- Yao, W.; Chu, C.-H.; Li, Z. The adoption and implementation of RFID technologies in healthcare: A literature review. J. Med. Syst. 2012, 36, 3507–3525. [Google Scholar] [CrossRef]
- Bazo, R.; da Costa, C.A.; Seewald, L.A.; da Silveira, L.G.; Antunes, R.S.; Righi, R.d.R.; Rodrigues, V.F. A Survey About Real-Time Location Systems in Healthcare Environments. J. Med. Syst. 2021, 45, 35. [Google Scholar] [CrossRef]
- Mans, R.S.; Van Der Aalst, W.M.P.; Vanwersch, R.J.B. Process Mining in Healthcare Evaluating and Exploiting Operational Healthcare Processes, 1st ed.; Springer: Cham, Switzerland, 2015. [Google Scholar] [CrossRef]
- Lima, R.M.; Dinis-Carvalho, J.; Souza, T.A.; Vieira, E.; Gonçalves, B. Implementation of lean in health care environments: An update of systematic reviews. Int. J. Lean Six Sigma 2021, 12, 399–431. [Google Scholar] [CrossRef]
- Frisby, J.; Smith, V.; Traub, S.; Patel, V.L. Contextual Computing : A Bluetooth based approach for tracking healthcare providers in the emergency room. J. Biomed. Inform. 2017, 65, 97–104. [Google Scholar] [CrossRef]
- Kamel Boulos, M.N.; Berry, G. Real-time locating systems (RTLS) in healthcare: A condensed primer. Int. J. Health Geogr. 2012, 11, 25. Available online: http://www.ij-healthgeographics.com/content/11/1/25 (accessed on 15 August 2024). [CrossRef] [PubMed]
- Sivadevuni, S.S.; Ravichandran, S.K. Systematic Literature Review—IoT-Based Supply Chain Management in Industry 4.0. In Intelligent Cyber Physical Systems and Internet of Things: ICoICI 2022; Springer: Cham, Switzerland, 2023; pp. 291–302. [Google Scholar]
- Huguet, M.; Pehlivan, C.; Ballereau, F.; Dodane-Loyenet, A.; Fontanili, F.; Garaix, T.; Yordanov, Y.; Augusto, V.; Tazarourte, K.; Redjaline, A. Indoor positioning systems provide insight into emergency department systems enabling proposal of designs to improve workflow. Commun. Med. 2025, 5, 72. [Google Scholar] [CrossRef]
- Han, Y.; Li, Y.; Li, Y.; Yang, B.; Cao, L. Digital twinning for smart hospital operations: Framework and proof of concept. Technol. Soc. 2023, 74, 102317. [Google Scholar] [CrossRef]
- Sun, T.; He, X.; Song, X.; Shu, L.; Li, Z. The Digital Twin in Medicine: A Key to the Future of Healthcare? Front. Med. 2022, 9, 907066. [Google Scholar] [CrossRef]
- Shaikh, T.A.; Rasool, T.; Verma, P. Machine intelligence and medical cyber-physical system architectures for smart healthcare: Taxonomy, challenges, opportunities, and possible solutions. Artif. Intell. Med. 2023, 146, 102692. [Google Scholar] [CrossRef]
- Nowotarski, P.; Pasławski, J.; Skrzypczak, M.; Krygier, R. RTLS systems as a Lean Management tool for productivity improvement. In Proceedings of the 34th International Symposium on Automation and Robotics in Construction (ISARC 2017), Taipei, Taiwan, 28 June–1 July 2017. [Google Scholar]
- Musser, J.A.; Cho, J.; Cohn, A.; Niziol, L.M.; Ballouz, D.; Burke, D.T.; Newman-Casey, P.A. Measuring impact of a quality improvement initiative on glaucoma clinic flow using an automated real-time locating system. BMC Ophthalmol. 2022, 22, 283. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Lopes, E.T.; Lopes, D.C.; Pedrozo, G.; Alves, I.O.; Käfer, G.A.; Medeiros, P.H.S.; de Gonçalves, B.S.; Fernandes, S.E.S.; Lima, R.M. Use of indoor location technologies in healthcare contexts: A scoping review protocol. Comun. Ciências Saúde 2024, 35, 1–18. Available online: https://revistaccs.escs.edu.br (accessed on 15 August 2024).
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J. Clin. Epidemiol. 2016, 75, 40–46. [Google Scholar] [CrossRef]
- Paez, A. Gray literature: An important resource in systematic reviews. J. Evid.-Based Med. 2017, 10, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Moatari-Kazerouni, A.; Bendavid, Y. Improving logistics processes of surgical instruments: Case of RFID technology. Bus. Process Manag. J. 2017, 23, 448–466. [Google Scholar] [CrossRef]
- Yoo, S.; Kim, S.; Kim, E.; Jung, E.; Lee, K.-H.; Hwang, H. Real-time location system-based asset tracking in the healthcare field: Lessons learned from a feasibility study. BMC Med. Inform. Decis. Mak. 2018, 18, 80. [Google Scholar] [CrossRef]
- Meyer, M.; Fairbrother, P.; Egan, M.; Chueh, H.; Sandberg, W.S. Using Location Tracking Data to Assess Efficiency in Established Clinical Workflows. AMIA Symp. 2006, 2006, 1031. [Google Scholar]
- Vankipuram, M.; Kahol, K.; Cohen, T.; Patel, V.L. Visualization and Analysis of Activities in Critical Care Environments. AMIA Symp. 2009, 2009, 662–666. [Google Scholar]
- Overmann, K.M.; Wu, D.T.; Xu, C.T.; Bindhu, S.S.; Barrick, L. Real-time locating systems to improve healthcare delivery: A systematic review. J. Am. Med. Inform. Assoc. 2021, 28, 1308–1317. [Google Scholar] [CrossRef] [PubMed]
- Issom, D.Z.; Hagry, C.; Wodia Mendo, L.; Seng, H.; Ehrler, F.; Lovis, C. Challenges and issues of geolocation in clinical environment. Stud. Health Technol. Inform. 2012, 180, 447–451. [Google Scholar] [CrossRef]
- Liu, J.; Rao, R. A coordinator loss-tolerant zigbee mesh network with region detection using RFID for the real-time indoor positioning system. In Proceedings of the 2011 3rd International Conference on Multimedia Information Networking and Security (MINES), Shanghai, China, 4–6 November 2011; pp. 472–476. [Google Scholar] [CrossRef]
- Shim, H.; Uh, Y.; Lee, S.H.; Yoon, Y.R. A new specimen management system using RFID technology. J. Med. Syst. 2011, 35, 1403–1412. [Google Scholar] [CrossRef]
- Gao, T.; White, D. A next generation electronic triage to aid mass casualty emergency medical response. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, New York, NY, USA, 30 August–3 September 2006; pp. 6501–6504. [Google Scholar] [CrossRef]
- Muhammad, S.U.-R.; Rabie, T.; Suleiman, S. A Novel Wireless Mesh Network for Indoor Robotic Navigation. In Proceedings of the 5th International Conference on Electronic Devices, Systems and Applications (ICEDSA), Ras Al Khaimah, United Arab Emirates, 6–8 December 2016. [Google Scholar]
- Vakili, S.; Pandit, R.; Singman, E.L.; Appelbaum, J.; Boland, M.V. A comparison of commercial and custom-made electronic tracking systems to measure patient flow through an ambulatory clinic. Int. J. Health Geogr. 2015, 14, 32. [Google Scholar] [CrossRef]
- Prater, A.; Bowen, M.; Pavich, E.; Hawkins, C.M.; Safdar, N.; Fountain, J.; Anderson, A.; Frankel, M.; Dehkharghani, S. Enhancing Workflow Analysis in Acute Stroke Patients Using Radiofrequency Identification and Infrared-based Real-Time Location Systems. J. Am. Coll. Radiol. 2017, 14, 231–234. [Google Scholar] [CrossRef]
- Rosen, M.A.; Dietz, A.S.; Lee, N.; Wang, I.-J.; Markowitz, J.; Wyskiel, R.M.; Yang, T.; Priebe, C.E.; Sapirstein, A.; Gurses, A.P.; et al. Sensor-based measurement of critical care nursing workload: Unobtrusive measures of nursing activity complement traditional task and patient level indicators of workload to predict perceived exertion. PLoS ONE 2018, 13, e0204819. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Tang, G.; Chamber, E.; Gillespie, J.; Wallace, C.; Chiu, T.; Pompos, A.; Godley, A.; Timmerman, R.; Jiang, S.; et al. An Indoor Real-Time Location System (RTLS) to Improve Patient Safety and Clinical Workflow of Radiation Therapy. In Proceedings of the AAPM 63rd Annual Meeting & Exhibition, Online, 25–29 July 2021; Available online: https://w4.aapm.org/meetings/2021AM/programInfo/programAbs.php?sid=9374&aid=58497 (accessed on 15 August 2024).
- Yeung, C.; Kwok, S.; Mui, H. An Investigation of an RFID-based Patient-tracking and Mobile Alert System. Int. J. Eng. Bus. Manag. 2011, 3, 50–56. [Google Scholar] [CrossRef]
- Ku, H.; Wang, P.; Su, M.; Liu, C.C.; Hwang, W. Application of Radio-frequency Identification in Perioperative Care. AORN J. 2011, 94, 158–172. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Hawthorne, H.; Pasupathy, K.; Hallbeck, S.; Sir, M.; Nestler, D.; Herbst, K.; Koening, K.; Blocker, R.; Gifford, S.; et al. Cost Savings Generated by a Radio Frequency Identification (RFID) Search System. Ann. Emerg. Med. 2016, 68, S44. [Google Scholar] [CrossRef]
- Stübig, T.; Zeckey, C.; Min, W.; Janzen, L.; Citak, M.; Krettek, C.; Hüfner, T.; Gaulke, R. Effects of a WLAN-based real time location system on outpatient contentment in a Level I trauma center. Int. J. Med. Inform. 2014, 83, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-S.; Kim, J.; Kim, S.-H.; Yoo, S.K. Design of RFID based the Patient Management and Tracking System in Hospital. In Proceedings of the 2008 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Vancouver, BC, Canada, 20–25 August 2008; pp. 1459–1461. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Lee, H.-J.; Byeon, N.-S.; Kim, H.-C.; Ha, K.-S.; Chung, C.-Y. Development and impact of radio-frequency identification-based workflow management in health promotion center: Using interrupted time-series analysis. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 935–940. [Google Scholar] [CrossRef]
- Stübig, T.; Suero, E.; Zeckey, C.; Min, W.; Janzen, L.; Citak, M.; Krettek, C.; Hüfner, T.; Gaulke, R. Improvement in the workflow efficiency of treating non-emergency outpatients by using a WLAN-based real-time location system in a level I trauma center. J. Am. Med. Inform. Assoc. 2013, 20, 1132–1136. [Google Scholar] [CrossRef]
- Browning, L.; White, K.; Siiankoski, D.; Colling, R.; Roskell, D.; Fryer, E.; Hemsworth, H.; Roberts-Gant, S.; Roelofsen, R.; Rittscher, J.; et al. RFID analysis of the complexity of cellular pathology workflow—An opportunity for digital pathology. Front. Med. 2022, 9, 933933. [Google Scholar] [CrossRef]
- Ohashi, K.; Ota, S.; Ohno-Machado, L.; Tanaka, H. Smart medical environment at the point of care: Auto-tracking clinical interventions at the bed side using RFID technology. Comput. Biol. Med. 2010, 40, 545–554. [Google Scholar] [CrossRef]
- Guo, B.; Documet, J.; Lee, J.; Liu, B.; King, N.; Shrestha, R.; Wang, K.; Huang, H.; Grant, E.G. Experiences With a Prototype Tracking and Verification System Implemented Within an Imaging Center. Acad. Radiol. 2007, 14, 270–278. [Google Scholar] [CrossRef]
- Bostwick, D.G. Radiofrequency identification specimen tracking in anatomical pathology: Pilot study of 1067 consecutive prostate biopsies. Ann. Diagn. Pathol. 2013, 17, 391–402. [Google Scholar] [CrossRef]
- Weng, S.-J.; Tsai, M.-C.; Tsai, Y.-T.; Gotcher, D.F.; Chen, C.-H.; Liu, S.-C.; Xu, Y.-Y.; Kim, S.-H. Improving the efficiency of an emergency department based on activity-relationship diagram and radio frequency identification technology. Int. J. Environ. Res. Public Health 2019, 16, 4478. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.A.; Seim, A.R.; Fairbrother, P.; Egan, M.T.; Sandberg, W.S. Automatic Time-Motion Study of a Multistep Preoperative Process. Anesthesiology 2008, 108, 1109–1116. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Maeda, H. Robust Indoor Positioning Method using BLE and Wireless Mesh Network. In Proceedings of the 2022 IEEE International Conference on Dependable, Autonomic and Secure Computing, Falerna, Italy, 12–15 September 2022. [Google Scholar] [CrossRef]
- Bahlman, D.T.; Johnson, F.C. Using technology to improve and support communication and workflow processes. AORN J. 2005, 82, 65–73. [Google Scholar] [CrossRef]
- Stahl, J.E.; Drew, M.A.; Leone, D.; Crowley, R.S. Measuring process change in primary care using real-time location systems: Feasibility and the results of a natural experiment. Technol. Health Care 2011, 19, 415–421. [Google Scholar] [CrossRef]
- Ward, D.R.; Ghali, W.A.; Graham, A.; Lemaire, J.B. A real-time locating system observes physician time-motion patterns during walk-rounds: A pilot study. BMC Med. Educ. 2014, 14, 37. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, R.; Abreu, E.; Henriques, C.; Gil, T.; Lopes, S.; Morgado, A.; Oliveira, L.; Serra, A.; Vieira, A.; Moura, J. Using smart RFID solutions to improve RBC units stock management, transfusion safety and blood unit traceability with clear benefits to the patient. Vox Sang. 2021, 116, 5–188. [Google Scholar] [CrossRef]
- Lin, Y.C.; Padman, R. Process visibility analysis in ambulatory care: A simulation study with RFID data. Stud. Health Technol. Inform. 2013, 192, 768–772. [Google Scholar] [CrossRef]
- Lam, S. Practical Considerations in Implementing RFID for the Blood Supply. Vox Sang. 2018, 113, 20. [Google Scholar] [CrossRef]
- Stahl, J.E.; Drew, M.A. Face Time Versus Test Ordering: Is There a trade off? Am. J. Manag. Care 2013, 19, SP362–SP368. [Google Scholar]
- Huang, Y.-C.; Chu, C.-P. RFID Applications in Hospitals-A Case Study for Emergency Department. J. Commun. Comput. 2011, 8, 70–75. [Google Scholar]
- Harry, T.; Taylor, M.; Fletcher, R.L.; Mundt, A.J.; Pawlicki, T. Passive tracking of linac clinical flow using radiofrequency identification technology. Pract. Radiat. Oncol. 2014, 4, e85–e90. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.C.; Chang, C.-H.; Su, M.-C.; Chu, H.-T.; Hung, S.-H.; Wong, J.-M.; Wang, P.-C. RFID-initiated workflow control to facilitate patient safety and utilization efficiency in operation theater. Comput. Methods Programs Biomed. 2011, 104, 435–442. [Google Scholar] [CrossRef]
- Bowen, M.E.; Wingrave, C.A.; Klanchar, A.; Craighead, J. Tracking technology: Lessons learned in two health care sites. Technol. Health Care 2013, 21, 191–197. [Google Scholar] [CrossRef]
- Stübig, T.; Zeckey, C.; Min, W.; Citak, M.; Krettek, C.; Hüfner, T.; Gaulke, R. Development of a WLAN-based real time localization system for patient tracking in a Level I Trauma center. Technol. Health Care 2012, 20, 317–327. [Google Scholar] [CrossRef]
- Ariffin, F.N.H.; Wan, A.T.; Suhaili, W.S.H. Psychiatric Patients Monitoring Using RFID: An Affordable Approach. In Proceedings of the 2015 IEEE International Conference on Computer and Communications (ICCC), Chengdu, China, 10–11 October 2015; pp. 181–185. [Google Scholar] [CrossRef]
- Jones, T.L. Radiofrequency identification: Exploiting an old technology for measuring nurse time and motion. CIN Comput. Inform. Nurs. 2012, 30, 463–472. [Google Scholar] [CrossRef] [PubMed]
- Okoniewska, B.; Graham, A.; Gavrilova, M.; Wah, D.; Gilgen, J.; Coke, J.; Burden, J.; Nayyar, S.; Kaunda, J.; Yergens, D.; et al. Multidimensional evaluation of a radio frequency identification wi-fi location tracking system in an acute-care hospital setting. J. Am. Med. Inform. Assoc. 2012, 19, 674–679. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chang, Y.-T.; Syed-Abdul, S.; Tsai, C.-Y.; Li, Y.-C. A novel method for inferring RFID tag reader recordings into clinical events. Int. J. Med. Inform. 2011, 80, 872–880. [Google Scholar] [CrossRef]
- Ohashi, K.; Ota, S.; Ohno-Machado, L.; Tanaka, H. Comparison of RFID Systems for Tracking Clinical Interventions at the Bedside. AMIA Symp. 2008, 2008, 525–529. [Google Scholar]
- Surian, D.; Kim, V.; Menon, R.; Dunn, A.G.; Sintchenko, V.; Coiera, E. Tracking a moving user in indoor environments using Bluetooth low energy beacons. J. Biomed. Inform. 2019, 98, 103288. [Google Scholar] [CrossRef]
- Newman-Casey, P.A.; Musser, J.; Niziol, L.M.; Shedden, K.; Burke, D.; Cohn, A. Designing and validating a low-cost real time locating system to continuously assess patient wait times. J. Biomed. Inform. 2020, 106, 103428. [Google Scholar] [CrossRef]
- Ajami, S.; Carter, M.W. The advantages and disadvantages of Radio Frequency Identification (RFID) in Health-care Centers; approach in Emergency Room (ER). Pak. J. Med. Sci. 2013, 29, 3552. [Google Scholar] [CrossRef]
- Stahl, J.E.; Drew, M.A.; Kimball, A.B. Patient-clinician concordance, face-time and access. Int. J. Health Care Qual. Assur. 2014, 27, 664–671. [Google Scholar] [CrossRef]
- Castner, J.; Suffoletto, H. Emergency Department Crowding and Time at the Bedside: A Wearable Technology Feasibility Study. J. Emerg. Nurs. 2018, 44, 624–631.e2. [Google Scholar] [CrossRef] [PubMed]
- Dey, A.; Vijayaraman, B.; Choi, J.H. RFID in US hospitals: An exploratory investigation of technology adoption. Manag. Res. Rev. 2016, 39, 399–424. [Google Scholar] [CrossRef]
- Vankipuram, A.; Traub, S.; Patel, V.L. A method for the analysis and visualization of clinical workflow in dynamic environments. J. Biomed. Inform. 2018, 79, 20–31. [Google Scholar] [CrossRef]
- Marchand-Maillet, F.; Debes, C.; Garnier, F.; Dufeu, N.; Sciard, D.; Beaussier, M. Accuracy of Patient’s Turnover Time Prediction Using RFID Technology in an Academic Ambulatory Surgery Center. J. Med. Syst. 2015, 39, 12. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening. 2019. Available online: https://www.who.int/publications/i/item/9789241550505 (accessed on 15 August 2024).
- Guédon, A.C.P.; Wauben, L.S.G.L.; de Korne, D.F.; Overvelde, M.; Dankelman, J.; Dobbelsteen, J.J.v.D. A RFID Specific Participatory Design Approach to Support Design and Implementation of Real-Time Location Systems in the Operating Room. J. Med. Syst. 2015, 39, 168. [Google Scholar] [CrossRef]
- UK Equator Centre. Enhancing the QUAlity and Transparency of Health Research; Equator Network; UK Equator Centre: Oxford, UK, 2024. [Google Scholar]
- Porter, M.E. What Is Value in Health Care? N. Engl. J. Med. 2010, 363, 2477–2481. [Google Scholar] [CrossRef]
- Doshmangir, L.; Khabiri, R.; Jabbari, H.; Arab-Zozani, M.; Kakemam, E.; Gordeev, V.S. Strategies for utilisation management of hospital services: A systematic review of interventions. Glob. Health 2022, 18, 53. [Google Scholar] [CrossRef]
- Katsoulakis, E.; Wang, Q.; Wu, H.; Shahriyari, L.; Fletcher, R.; Liu, J.; Achenie, L.; Liu, H.; Jackson, P.; Xiao, Y.; et al. Digital twins for health: A scoping review. NPJ Digit. Med. 2024, 7, 77. [Google Scholar] [CrossRef] [PubMed]
- Armeni, P.; Polat, I.; De Rossi, L.M.; Diaferia, L.; Meregalli, S.; Gatti, A. Digital Twins in Healthcare: Is It the Beginning of a New Era of Evidence-Based Medicine? A Critical Review. J. Pers. Med. 2022, 12, 1255. [Google Scholar] [CrossRef] [PubMed]
- Elkefi, S.; Asan, O. Digital Twins for Managing Health Care Systems: Rapid Literature Review. J. Med. Internet Res. 2022, 24, e37641. [Google Scholar] [CrossRef]
- Cellina, M.; Cè, M.; Alì, M.; Irmici, G.; Ibba, S.; Caloro, E.; Fazzini, D.; Oliva, G.; Papa, S. Digital Twins: The New Frontier for Personalized Medicine? Appl. Sci. 2023, 13, 7940. [Google Scholar] [CrossRef]
- van der Togt, R.; Bakker, P.J.; Jaspers, M.W.M. A framework for performance and data quality assessment of Radio Frequency IDentification (RFID) systems in health care settings. J. Biomed. Inform. 2011, 44, 372–383. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, Z.; Luo, D.; Henry, P.; Kazemifar, S.; Rozario, T.; Yan, Y.; Westover, K.; Lu, W.; Nguyen, D.; Long, T.; et al. Accurate real time localization tracking in a clinical environment using Bluetooth Low Energy and deep learning. PLoS ONE 2018, 13, e0205392. [Google Scholar] [CrossRef]
- Ghori, M.; Wan, T.-C.; Sodhy, G. Bluetooth Low Energy 5 Mesh Based Hospital Communication Network (B5MBHCN). In Proceedings of the International Conference on Advances in Cyber Security 2019, Penang, Malaysia, 30 July–1 August 2019; pp. 247–261. [Google Scholar] [CrossRef]
- Tu, Y.; Chi, H.; Zhou, W.; Kapoor, G.; Eryarsoy, E.; Piramuthu, S. Critical evaluation of RFID applications in healthcare. In Proceedings of the 2019 International Conference on Future Network Systems and Security, Melbourne, Australia, 27–29 November 2019; pp. 240–248. [Google Scholar] [CrossRef]
- Lee, C.K.M.; Palaniappan, S. Effective Asset Management For Hospitals with RFID. In Proceedings of the 2014 IEEE International Technology Management Conference, Chicago, IL, USA, 12-15 June 2014. [Google Scholar] [CrossRef]
- Hamilton, D. Handling the demands of a population boom. Using RTLS to improve patient care and workflows. Health Manag Technol. 2015, 36, 14–15. [Google Scholar]
- Pawlicki, T.; Harry, T.; Taylor, M.; Fletcher, R.; Mundt, A. Investigation of RFID-based Workflow Analysis. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 543. [Google Scholar] [CrossRef]
- Hayden, G.; Ku, B.; Pugliese, R.; Grzywinski, M.; Faircloth, B.; Carlisle, S. Mapping Hospital Environments: Doctors and Architects Working Together to Design Better Emergency Departments. Acad. Emerg. Med. 2018; 25, S285–S298. [Google Scholar] [CrossRef][Green Version]
- Fry, E.A.; Lenert, L.A. MASCAL: RFID Tracking of Patients, Staff and Equipment to Enhance Hospital Response to Mass Casualty Events. In Proceedings of the American Medical Informatics Association Annual Symposium 2015 (AMIA 2015), San Francisco, CA, USA, 14–18 November 2015; pp. 261–265. [Google Scholar]
- Koenig, K.R.; Pasupathy, K.S.; Hellmich, T.R.; Hawthorne, H.J.; Karalius, V.P.; Sir, M.; Das, D.; Heaton, H.A.; Nestler, D.M. Measuring Sensitivity and Precision of Real-Time Location Systems (RTLS): Definition, Protocol and Demonstration for Clinical Relevance. J. Med. Syst. 2021, 45, 15. [Google Scholar] [CrossRef]
- Musa, A.; Yusuf, Y. MEWARE: Enhanced workflow automation, reliability and efficiency in medical establishments. In Proceedings of the 2012 Colloquium in Information Science and Technology, Fez, Morocco, 22–24 October 2012; pp. 112–116. [Google Scholar] [CrossRef]
- Vankipuram, A.; Patel, V.L.; Traub, S.; Shortliffe, E.H. Overlaying multiple sources of data to identify bottlenecks in clinical workflow. J. Biomed. Inform. 2019. [Google Scholar] [CrossRef]
- Arunachalam, S.P.; Albertson, S.M.; Sir, M.Y.; Nestler, D.M.; Heaton, H.A.; Marisamy, G.; Pasupathy, K.S. Patient satisfaction in the emergency department is influenced by total length of stay: A RFID based feasibility study. In Proceedings of the 2020 Design of Medical Devices Conference, Minneapolis, MN, USA, 6–9 April 2020. [Google Scholar] [CrossRef]
- Fernández-Llatas, C.; Benedi, J.M.; García-Gómez, J.M.; Traver, V. Process mining for individualized behavior modeling using wireless tracking in nursing homes. Sensors (Switzerland) 2013, 13, 15434–15451. [Google Scholar] [CrossRef]
- Nagy, P.; George, I.; Bernstein, W.; Caban, J.; Klein, R.; Mezrich, R.; Park, A. Radio frequency identification systems technology in the surgical setting. Surg. Innov. 2006, 13, 61. [Google Scholar] [CrossRef] [PubMed]
- Kranzfelder, M.; Schneider, A.; Fiolka, A.; Ing, D.; Schwan, E.; Gillen, S.; Wilhelm, D.; Schirren, R.; Reiser, S.; Jensen, B.; et al. Real-time instrument detection in minimally invasive surgery using radiofrequency identification technology. J. Surg. Res. 2013, 185, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Oude Weernink, C.E.; Felix, E.; Verkuijlen, P.J.E.M.; Dierick-van Daele, A.T.M.; Kazak, J.K.; van Hoof, J. Real-time location systems in nursing homes: State of the art and future applications. J Enabling. Technol. 2018, 12, 45–56. [Google Scholar] [CrossRef]
- Hussian, F.; Durrani, S.; Farooqi, J.; Mahmood, H.; Junjua, G.; Jattala, I.; Ikram, N. RFID & WSN based integrated maternity ward monitoring system. In Proceedings of the 16th International Multi Topic Conference, Lahore, Pakistan, 19–20 December 2013; pp. 43–48. [Google Scholar] [CrossRef]
- Southard, P.B.; Chandra, C.; Kumar, S. RFID in healthcare: A Six Sigma DMAIC and simulation case study. Int. J. Health Care. Qual. Assur. 2012, 25, 291–321. [Google Scholar] [CrossRef] [PubMed]
- Frisch, P.H. RFID in Today’s Intelligent Hospital Enhancing Patient Care & Optimizing Hospital Operations. In Proceedings of the 2019 IEEE International Conference on RFID Technology and Applications, Pisa, Italy, 25–27 September 2019; pp. 458–463. [Google Scholar] [CrossRef]
- Kato-Lin, Y.C.; Padman, R. RFID technology-enabled Markov reward process for sequencing care coordination in ambulatory care: A case study. Int. J. Inf. Manag. 2019, 48, 12–21. [Google Scholar] [CrossRef]
- Kumar, S.; Livermont, G.; McKewan, G. Stage implementation of RFID in hospitals. Technol. Health Care 2010, 18, 31–46. [Google Scholar] [CrossRef]
- Han, G.; Klinker, G.J.; Ostler, D.; Schneider, A. Testing a proximity-based location tracking system with Bluetooth Low Energy tags for future use in the OR. In Proceedings of the 17th International Conference on e-Health Networking, Applications and Services (Healthcom), Boston, MA, USA, 14–17 October 2015; pp. 17–21. [Google Scholar]
- Stahl, J.E.; Holt, J.K.; Gagliano, N.J. Understanding performance and behavior of tightly coupled outpatient systems using RFID: Initial experience. J. Med. Syst. 2011, 35, 291–297. [Google Scholar] [CrossRef]
- Patel, B.; Vilendrer, S.; Kling, S.M.R.; Brown, I.; Ribeira, R.; Eisenberg, M.; Sharp, C. Using a real-time locating system to evaluate the impact of telemedicine in an emergency department during COVID-19: Observational study. J. Med. Internet. Res. 2021, 23, e29240. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).