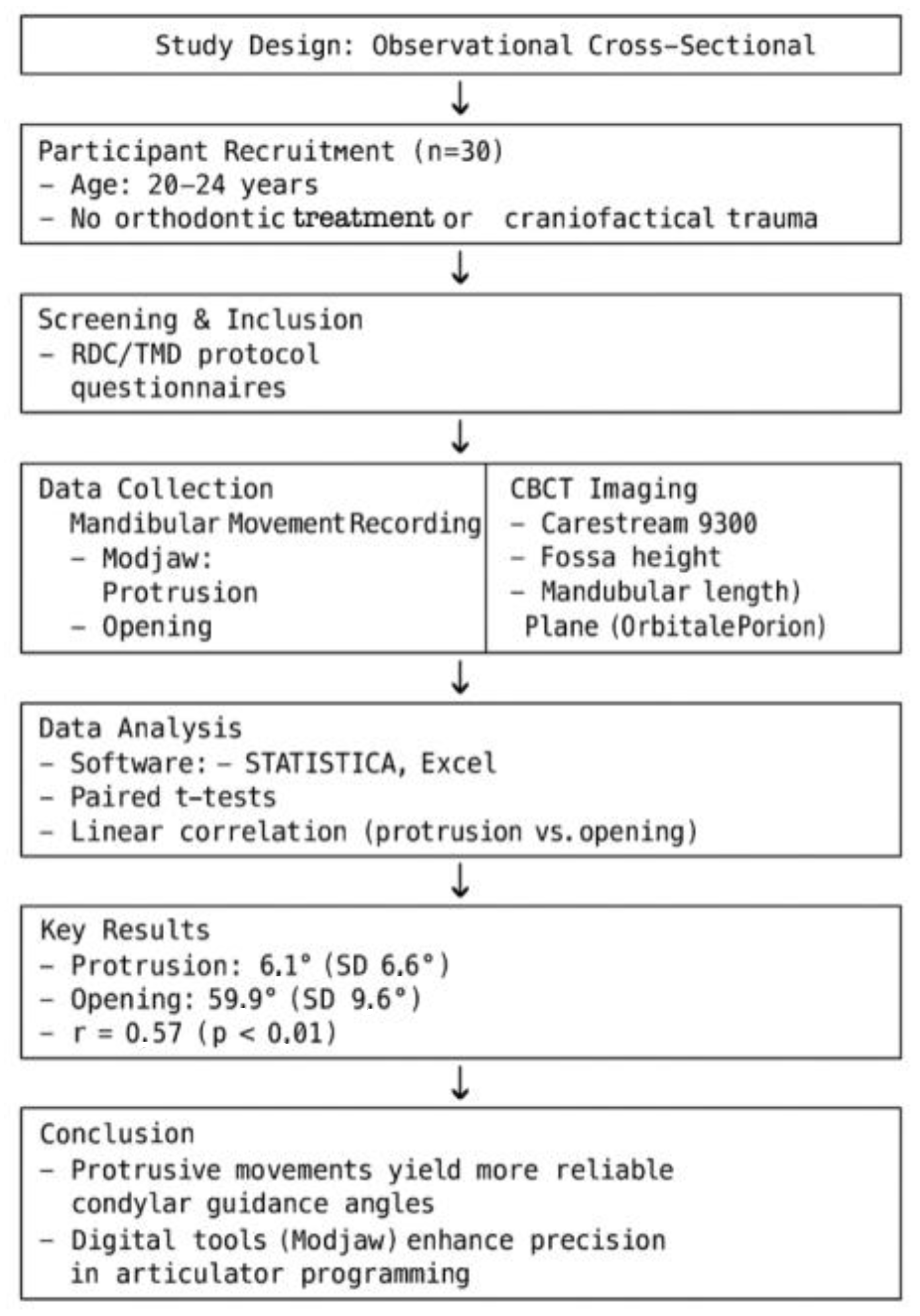
Comparison of Condylar Guidance in Opening and Protrusion Using Electronic Axiography and CBCT: An Observational Cross-Sectional Study
Abstract
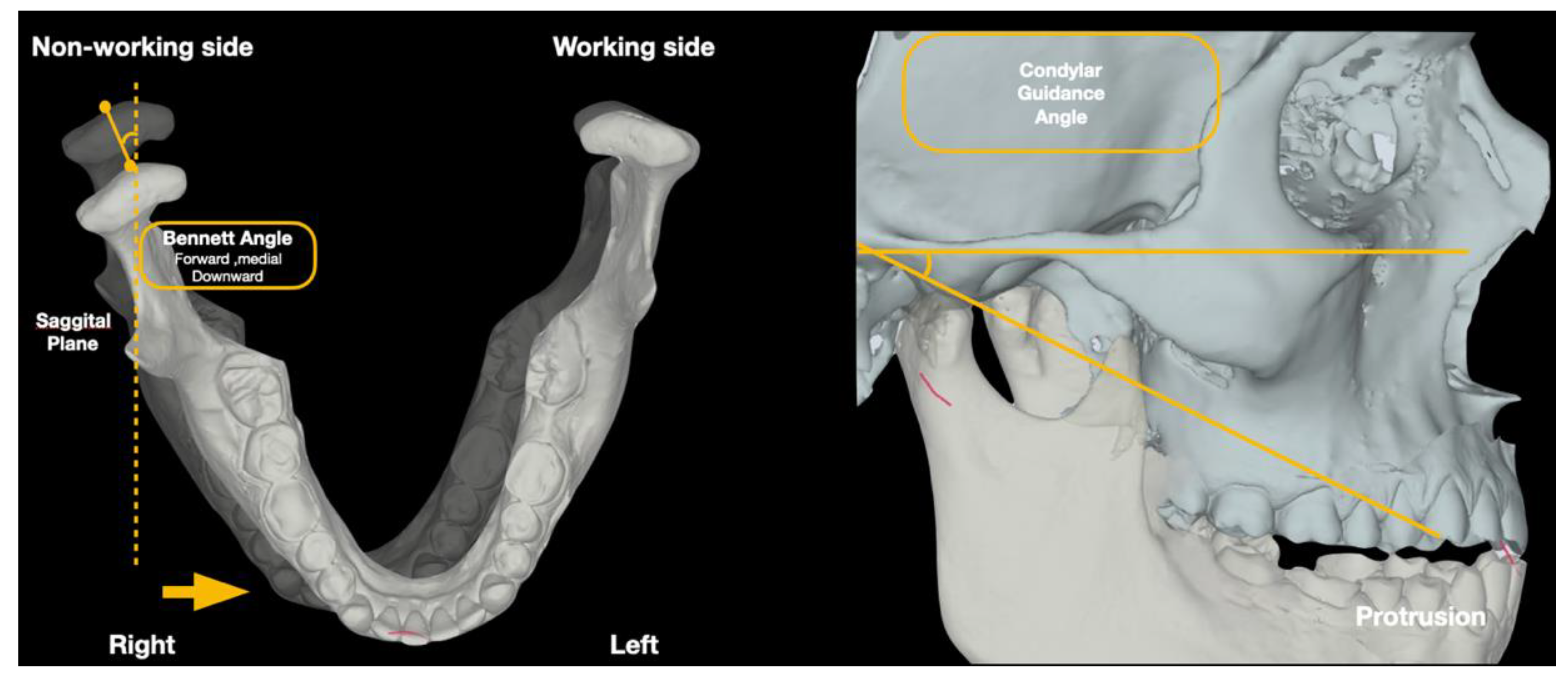
1. Introduction
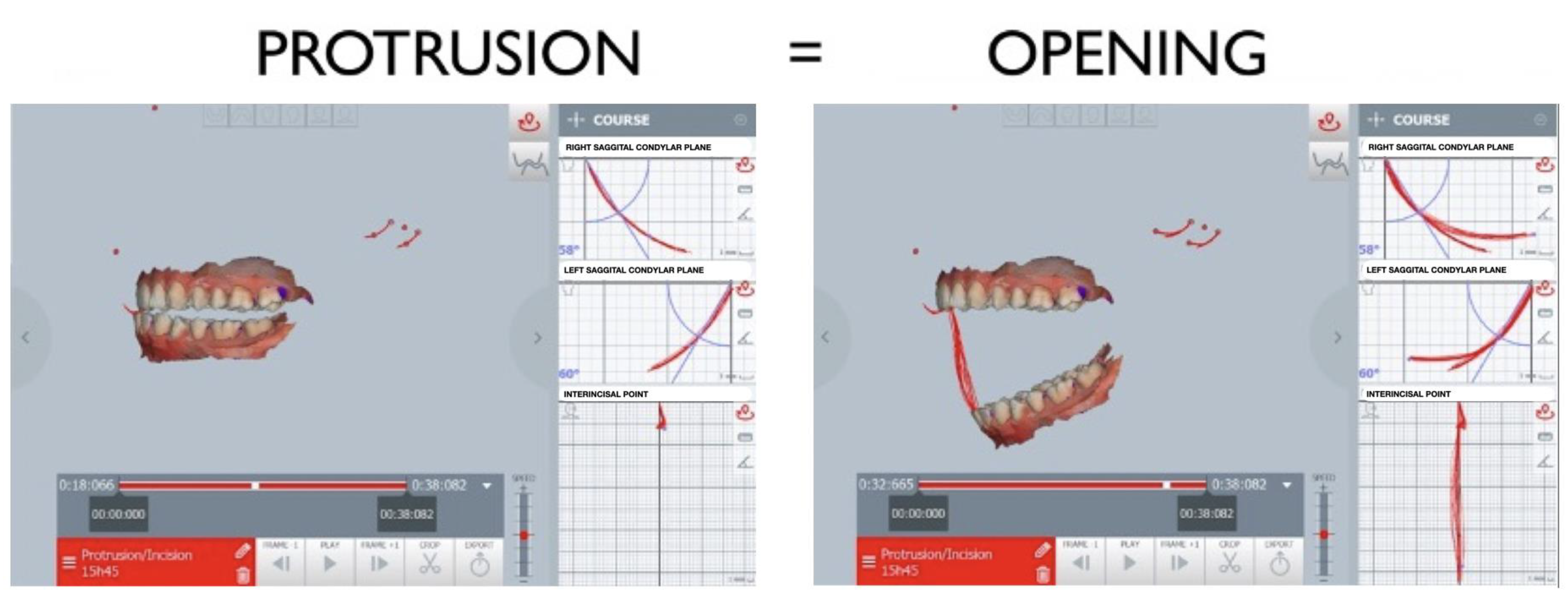
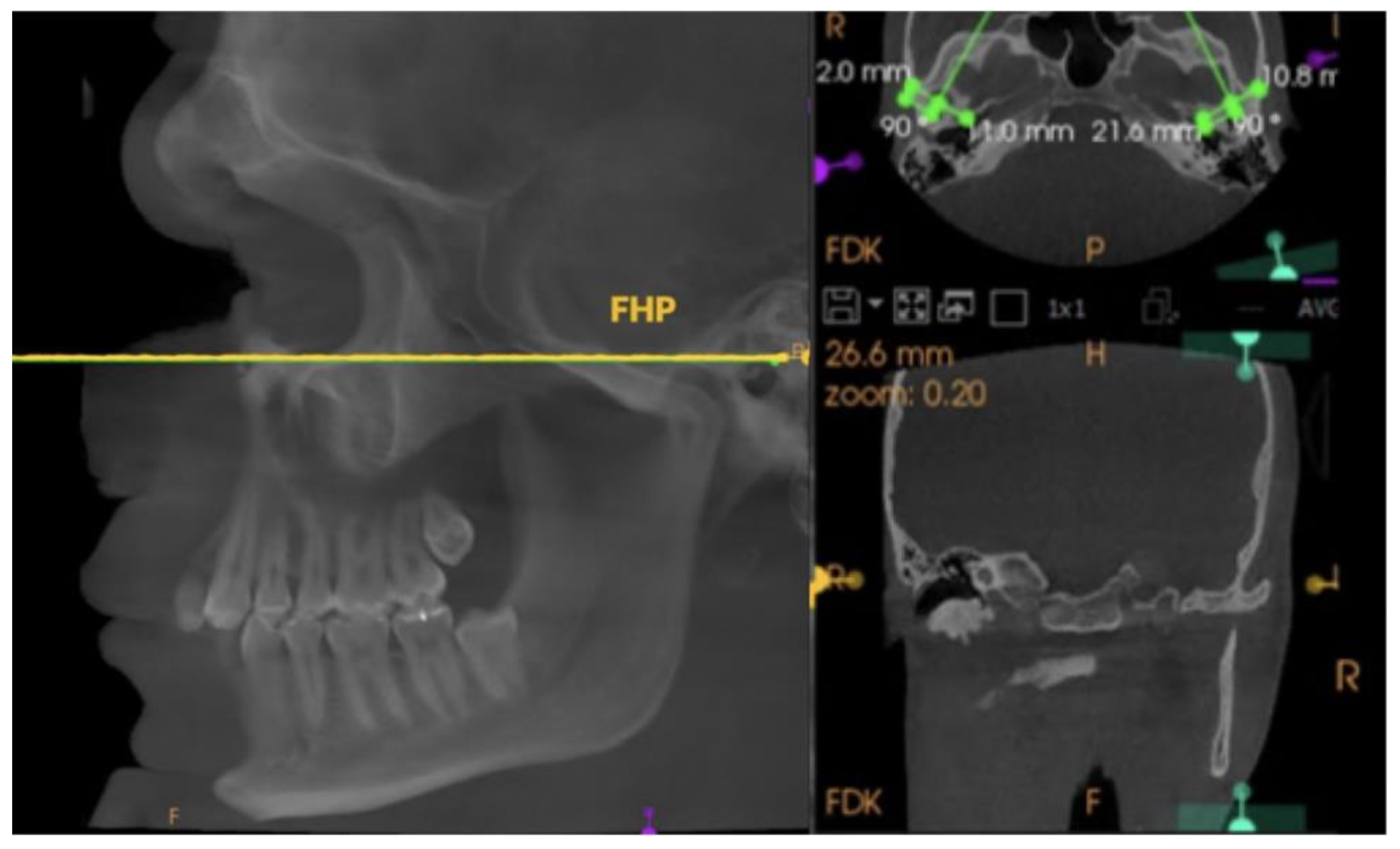
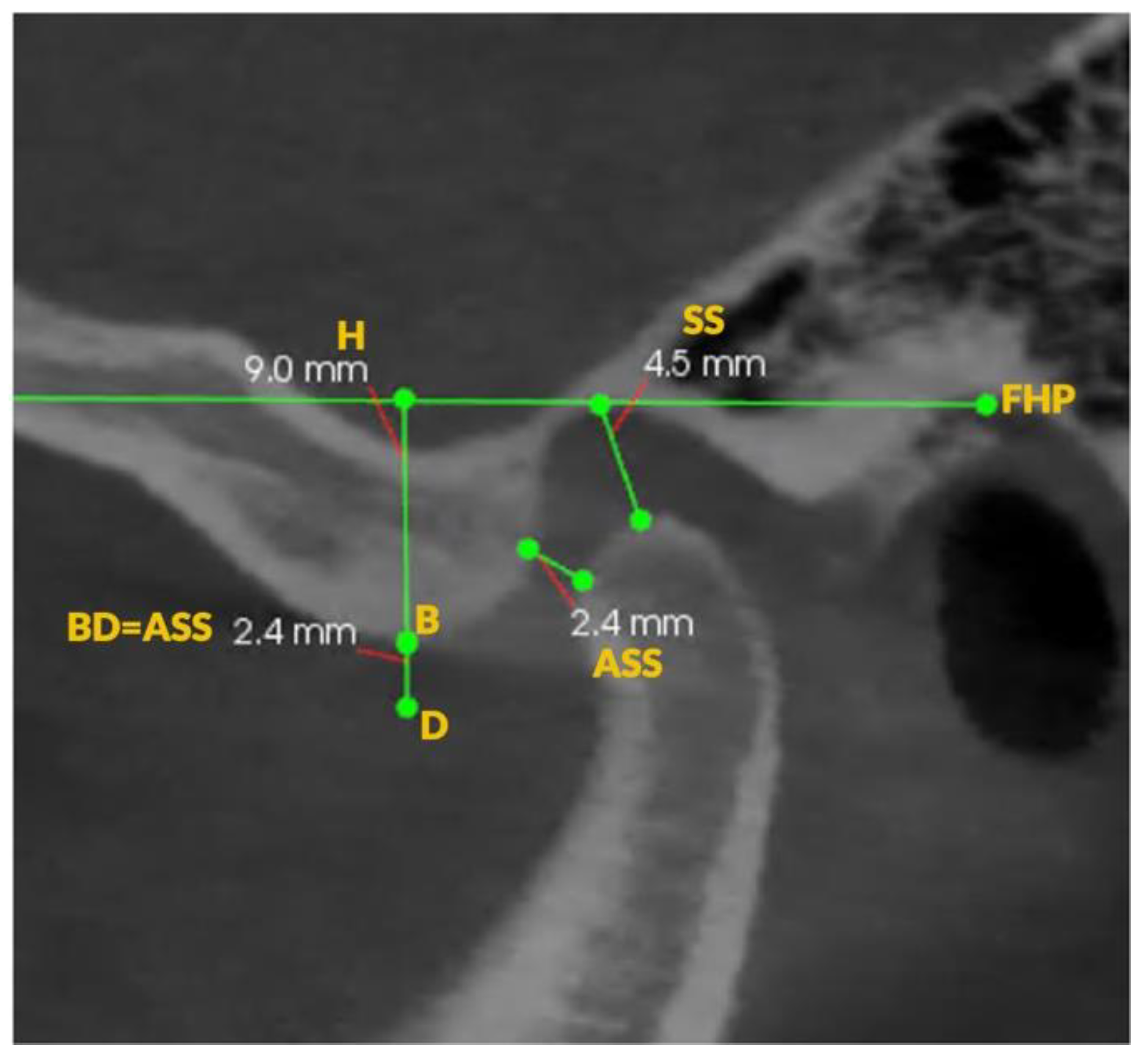
2. Materials and Methods
- -
- Repetitive mouth opening and closing;
- -
- Protrusive movements from maximum intercuspation (MIP);
- -
- Full mouth opening from MIP.
3. Results
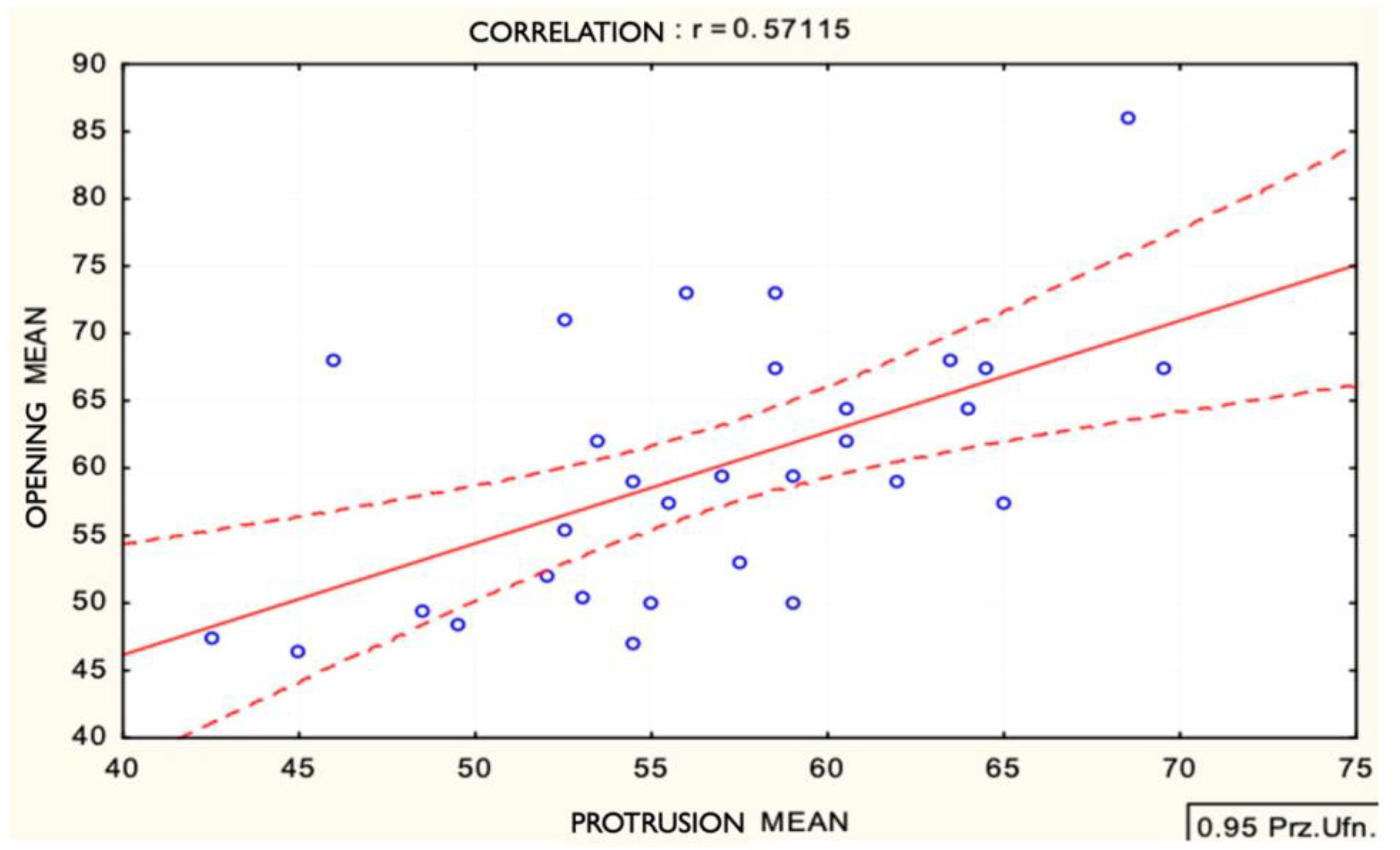
Correlation Between Protrusive and Opening Guidance Angles
4. Discussion
4.1. Correlation Between Protrusion and Mouth Opening
4.2. Clinical Implications of Movement Type
4.3. Methodological Considerations
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Iturriaga, V.; Bornhardt, T.; Velasquez, N. Temporomandibular Joint: Review of Anatomy and Clinical Implications. Dent. Clin. N. Am. 2023, 67, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Woodford, S.C.; Robinson, D.L.; Mehl, A.; Lee, P.V.S.; Ackland, D.C. Measurement of normal and pathological mandibular and temporomandibular joint kinematics: A systematic review. J. Biomech. 2020, 111, 109994. [Google Scholar] [CrossRef] [PubMed]
- Hatcher, D.C. Anatomy of the Mandible, Temporomandibular Joint, and Dentition. Neuroimaging Clin. N. Am. 2022, 32, 749–761. [Google Scholar] [CrossRef]
- Starcke, E.N.; Engelmeier, R.L. The history of articulators: The wonderful world of “Grinders”. Part I. J. Prosthodont. 2006, 15, 129–140. [Google Scholar] [CrossRef]
- Kranjčić, J.; Hunt, D.; Kiršić, S.P.; Kovačić, I.; Vukšić, J.; Vojvodić, D. Articular Eminence Morphology of American Historic and Contemporary Populations. Acta Stomatol. Croat. 2021, 55, 397–405. [Google Scholar] [CrossRef]
- Sharpling, B. Semi-adjustable articulators. In Practical Procedures in Aesthetic Dentistry; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2017; pp. 60–66. [Google Scholar]
- Goldstein, G.; Goodacre, C. Selecting a Virtual Articulator: An Analysis of the Factors Available with Mechanical Articulators and their Potential Need for Inclusion with Virtual Articulators. J. Prosthodont. 2023, 32, 10–17. [Google Scholar] [CrossRef]
- Cabot, L.B. Using articulators to enhance clinical practice. Br. Dent. J. 1998, 184, 272–276. [Google Scholar] [CrossRef]
- Doshi, K.N.; Sathe, S.; Dubey, S.A.; Bhoyar, A.; Dhamande, M.; Jaiswal, T. A Comprehensive Review on Virtual Articulators. Cureus 2024, 16, e52554. [Google Scholar] [CrossRef]
- Hobo, S.; Shillingburg, H.T.; Whitsett, L.D. Articulator selection for restorative dentistry. J. Prosthet. Dent. 1976, 36, 35–43. [Google Scholar] [CrossRef]
- Lepidi, L.; Galli, M.; Mastrangelo, F.; Venezia, P.; Joda, T.; Wang, H.L.; Li, J. Virtual Articulators and Virtual Mounting Procedures: Where Do We Stand? J. Prosthodont. 2021, 30, 24–35. [Google Scholar] [CrossRef]
- Lepidi, L.; Suriano, C.; Wang, H.L.; Granata, S.; Joda, T.; Li, J. Digital fixed complete-arch rehabilitation: From virtual articulator mounting to clinical delivery. J. Prosthet. Dent. 2022, 127, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Manziuc, M.M.; Dîrzu, A.; Almăşan, O.; Leucuţa, D.C.; Tăut, M.; Ifrim, C.; Berindean, D.; Kui, A.; Negucioiu, M.; Buduru, S. Cadiax Compact 2 and MODJAW comparative analysis of condylar inclination: Innovative digital approaches in dentistry. J. Prosthet. Dent. 2024, 133, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Tuppy, F.; Celar, R.M.; Celar, A.G.; Piehslinger, E.; Jäger, W. The reproducibility of condylar hinge axis positions in patients, by different operators, using the electronic mandibular position indicator. J. Orofac. Pain 1994, 8, 315–320. [Google Scholar] [PubMed]
- Hue, O. The Sagittal Condylar Paths in Edentulous Patients: Analysis with Computerized Axiography. Int. J. Prosthodont. 2016, 29, 11–16. [Google Scholar] [CrossRef]
- Gsellmann, B.; Schmid-Schwap, M.; Piehslinger, E.; Slavicek, R. Lengths of condylar pathways measured with computerized axiography (CADIAX) and occlusal index in patients and volunteers. J. Oral Rehabil. 1998, 25, 146–152. [Google Scholar] [CrossRef]
- Hüe, O. Condylar paths during protrusion in edentulous patients: Analysis with electronic axiography. J. Prosthodont. 2011, 20, 294–298. [Google Scholar] [CrossRef]
- Lewandowska, A.; Mańka-Malara, K.; Kostrzewa-Janicka, J. Sagittal Condylar Inclination and Transversal Condylar Inclination in Different Skeletal Classes. J. Clin. Med. 2022, 11, 2664. [Google Scholar] [CrossRef]
- Bapelle, M.; Dubromez, J.; Savoldelli, C.; Tillier, Y.; Ehrmann, E. Update on the parameters influencing the adjustment of the sagittal and transversal condylar inclination of dental articulators. Quintessence Int. 2022, 53, 78–88. [Google Scholar]
- Caro, A.J.; Peraire, M.; Martinez-Gomis, J.; Anglada, J.M.; Samsó, J. Reproducibility of lateral excursive tooth contact in a semi-adjustable articulator depending on the type of lateral guidance. J. Oral Rehabil. 2005, 32, 174–179. [Google Scholar] [CrossRef]
- Amarnath, G.S.; Kumar, U.; Hilal, M.; Muddugangadhar, B.C.; Anshuraj, K.; Shruthi, C.S. Comparison of Cone Beam Computed Tomography, Orthopantomography with Direct Ridge Mapping for Pre-Surgical Planning to Place Implants in Cadaveric Mandibles: An Ex-Vivo Study. J. Int. Oral Health 2015, 7 (Suppl. S1), 38. [Google Scholar]
- Aljohani, A.O.; Sghaireen, M.G.; Abbas, M.; Alzarea, B.K.; Srivastava, K.C.; Shrivastava, D.; Issrani, R.; Mathew, M.; Alsharari, A.H.L.; Alsharari, M.A.D.; et al. Comparative Evaluation of Condylar Guidance Angles Measured Using Arcon and Non-Arcon Articulators and Panoramic Radiographs—A Systematic Review and Meta-Analysis. Life 2023, 13, 1352. [Google Scholar] [CrossRef] [PubMed]
- Bapelle, M.; Dubromez, J.; Savoldelli, C.; Tillier, Y.; Ehrmann, E. Modjaw® device: Analysis of mandibular kinematics recorded for a group of asymptomatic subjects. Cranio J. Craniomandib. Sleep Pract. 2024, 42, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Lassmann, Ł.; Nowak, Z.; Orthlieb, J.D.; Żółtowska, A. Complicated Relationships between Anterior and Condylar Guidance and Their Clinical Implications—Comparison by Cone Beam Computed Tomography and Electronic Axiography—An Observational Cohort Cross-Sectional Study. Life 2023, 13, 335. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral. Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Chae, J.M.; Park, J.H.; Tai, K.; Mizutani, K.; Uzuka, S.; Miyashita, W.; Seo, H.Y. Evaluation of condyle-fossa relationships in adolescents with various skeletal patterns using cone-beam computed tomography. Angle Orthod. 2020, 90, 224–232. [Google Scholar] [CrossRef]
- Oancea, L.; Stegaroiu, R.; Cristache, C.M. The influence of temporomandibular joint movement parameters on dental morphology. Ann. Anat.-Anat. Anz. 2018, 218, 49–58. [Google Scholar] [CrossRef]
- Price, R.B.; Kolling, J.N.; Clayton, J.A. Effects of changes in articulator settings on generated occlusal tracings Part I: Condylar inclination progressive side shift settings. J. Prosthet. Dent. 1991, 65, 237–243. [Google Scholar] [CrossRef]
- Price, R.B.; Kolling, J.N.; Clayton, J.A. Effects of changes in articulator settings on generated occlusal tracings Part II: Immediate side shift intercondylar distance rear top wall settings. J. Prosthet. Dent. 1991, 65, 377–382. [Google Scholar] [CrossRef]

| Patient | Protrusion | Opening | ||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| 1 | 53 | 53 | 50 | 51 |
| 2 | 63 | 66 | 64 | 71 |
| 3 | 48 | 70 | 49 | 51 |
| 4 | 71 | 66 | 83 | 89 |
| 5 | 53 | 59 | 69 | 77 |
| 6 | 68 | 56 | 70 | 48 |
| 7 | 64 | 64 | 65 | 64 |
| 8 | 59 | 59 | 61 | 58 |
| 9 | 59 | 58 | 68 | 78 |
| 10 | 57 | 52 | 61 | 57 |
| 11 | 64 | 63 | 65 | 71 |
| 12 | 70 | 69 | 69 | 66 |
| 13 | 59 | 62 | 64 | 65 |
| 14 | 48 | 51 | 46 | 51 |
| 15 | 65 | 65 | 62 | 53 |
| 16 | 53 | 44 | 56 | 43 |
| 17 | 49 | 58 | 60 | 64 |
| 18 | 57 | 57 | 60 | 59 |
| 19 | 47 | 45 | 72 | 64 |
| 20 | 57 | 52 | 49 | 45 |
| 21 | 60 | 61 | 57 | 67 |
| 22 | 53 | 62 | 54 | 52 |
| 23 | 59 | 58 | 70 | 65 |
| 24 | 43 | 42 | 51 | 44 |
| 25 | 55 | 50 | 71 | 71 |
| 26 | 56 | 55 | 61 | 54 |
| 27 | 51 | 54 | 56 | 55 |
| 28 | 54 | 56 | 53 | 47 |
| 29 | 48 | 42 | 51 | 42 |
| 30 | 55 | 49 | 54 | 50 |
| Variables X and Y | Number of Cases | Mean | Standard Deviation | r(X,Y) | r2 | p |
|---|---|---|---|---|---|---|
| Protrusion Mean | 30 | 56.6000 | 6.6299 | 0.571147 | 0.326209 | 0.000979 |
| Opening Mean | 59.8833 | 9.5923 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lassmann, Ł.; Żółtowska, A.; Teślak-Piesyk, M.; Yar, R. Comparison of Condylar Guidance in Opening and Protrusion Using Electronic Axiography and CBCT: An Observational Cross-Sectional Study. Appl. Sci. 2025, 15, 5993. https://doi.org/10.3390/app15115993
Lassmann Ł, Żółtowska A, Teślak-Piesyk M, Yar R. Comparison of Condylar Guidance in Opening and Protrusion Using Electronic Axiography and CBCT: An Observational Cross-Sectional Study. Applied Sciences. 2025; 15(11):5993. https://doi.org/10.3390/app15115993
Chicago/Turabian StyleLassmann, Łukasz, Agata Żółtowska, Monika Teślak-Piesyk, and Riaz Yar. 2025. "Comparison of Condylar Guidance in Opening and Protrusion Using Electronic Axiography and CBCT: An Observational Cross-Sectional Study" Applied Sciences 15, no. 11: 5993. https://doi.org/10.3390/app15115993
APA StyleLassmann, Ł., Żółtowska, A., Teślak-Piesyk, M., & Yar, R. (2025). Comparison of Condylar Guidance in Opening and Protrusion Using Electronic Axiography and CBCT: An Observational Cross-Sectional Study. Applied Sciences, 15(11), 5993. https://doi.org/10.3390/app15115993






