Abstract
Background: The aim of this retrospective study was to conduct an in vivo evaluation of the accuracy of surgical guides obtained via 3D printing technology that were used to transfer the 3D software-planned position and axis during palatal miniscrew placement. Methods: Twenty-four Caucasian subjects with permanent dentition underwent a CBCT examination to plan palatal skeletal anchorage using two miniscrews in the anterior palatal arch. A specific software function capable of identifying and displaying all CBCT scans passing through the planned miniscrew axis was used to identify the scan showing the maximum discrepancy between the planned and final miniscrew placement. The maximum insertion angle discrepancy and the maximum linear difference between the head and tip of the miniscrew were measured on the overlaid 3D STL models of the planned miniscrew position at CBCT with the final clinical position of the miniscrew. Results: Descriptive and inferential statistics were performed. On average, there was a discrepancy between the planned insertion axis and the final insertion axis of 2.95° (SD ± 1.13°), with a 10 mm miniscrew length. Conclusion: Three-dimensional I.-printed surgical guides for palatal miniscrew placement show a mean deviation of 2.95° from the planned position, indicating good but improvable accuracy in placement.
1. Introduction
In recent years, the integration of digital workflows in orthodontics has profoundly transformed clinical protocols, enabling more precise diagnosis, treatment planning, and appliance fabrication. Among these innovations, the use of three-dimensional (3D) printing technology for the fabrication of surgical guides has significantly enhanced the accuracy and predictability of miniscrew-assisted anchorage procedures [1,2,3].
The concept of skeletal anchorage in the palate was initially introduced through the clinical application of osseointegrated palatal implants, which are specifically designed to meet orthodontic anchorage requirements [4].
Although effective, these systems required invasive surgical protocols and were limited by the necessity of osseointegration.
Nearly a decade later, the introduction of non-osseointegrated palatal miniscrews, also referred to as temporary anchorage devices (TADs), represented a major advancement in anchorage management. These devices allowed for less invasive placement and greater clinical versatility, particularly in hybrid protocols such as the palatal Hyrax expander [5].
However, the clinical application of palatal TADs is challenged by significant interindividual anatomical variability in the palatal vault.
Several studies have investigated this region, analyzing total bone depth, as well as cortical and mucosal thickness [6,7]. These data have been essential in defining guidelines for optimal insertion sites. Nevertheless, high standard deviations in reported measurements underscore substantial anatomical heterogeneity [8,9].
In certain patients, palatal bone thickness at commonly recommended insertion zones may fall below 8 mm, which is the minimum length of commercially available palatal miniscrews [6,7] This increases the risk of nasal floor perforation, even when using the shortest screws available.
Given these anatomical variations and associated risks, preoperative assessment using cone-beam computed tomography (CBCT) is considered essential for the accurate estimation of available bone volume and personalized treatment planning [10,11].
Advanced digital technologies, such as virtual guided planning and additive manufacturing via 3D printing, enable the precise three-dimensional reconstruction of individual bone anatomy. This facilitates the simulation of ideal miniscrew placement, optimizing angulation and depth based on patient-specific morphology. The production of patient-specific surgical guides through 3D printing ensures the faithful clinical transfer of the virtual plan, thereby minimizing the risk of nasal floor perforation and soft tissue injury [8].
The integration of these technologies thus represents an advanced strategy to enhance the safety, accuracy, and efficacy of minimally invasive orthodontic procedures, effectively addressing challenges related to anatomical heterogeneity [12]. Surgical guides are typically fabricated using 3D printing technology with biocompatible resins that comply with international standards, such as ISO 10993-1:2018 (Biological evaluation of medical devices—Part 1: Evaluation and testing within a risk management process. International Organization for Standardization: Geneva, Switzerland), for the biological evaluation of medical devices. These resins are specifically certified for surgical applications, ensuring adequate mechanical properties, sterilizability, and cytocompatibility, thereby minimizing the risk of adverse tissue reactions and guaranteeing patient safety during clinical use (e.g., Class I or IIa medical devices under the Medical Device Regulation—MDR 2017/745/EU). While the implementation of 3D-printed surgical guides in palatal miniscrew placement has been documented in the orthodontic literature, there remains a lack of quantitative in vivo studies that directly compare the actual clinical position of miniscrews to their preoperative virtual planning. Similar investigations in the broader field of dental implantology have demonstrated that guided surgical protocols significantly enhance placement accuracy and reduce clinical complications compared to conventional freehand techniques [13,14].
The accurate transfer of the virtual plan is particularly critical in orthodontic miniscrew placement because it helps avoid risks such as nasal floor perforation, root damage, and soft tissue injury, which can negatively impact device stability and overall treatment success [15]. Recent advancements in CBCT-based virtual planning, combined with 3D printing patient-specific surgical guides, have shown promising improvements in precision and surgical outcomes in dental applications [15,16]. However, these benefits have not yet been comprehensively validated for the unique anatomical and biomechanical challenges posed by palatal miniscrew insertion.
Consequently, this retrospective study aims to evaluate the in vivo accuracy of 3D-printed surgical guides in faithfully transferring the digitally planned three-dimensional position and angulation of palatal miniscrews. Such data are essential for validating guided protocols and ultimately improving clinical predictability and patient safety in orthodontic anchorage procedures.
2. Materials and Methods
This retrospective cross-sectional CBCT study was conducted according to the principles of the Declaration of Helsinki. Its protocol was reviewed and approved by the Ethics Committee of Messina (prot. 33-2020).
The University clinic’s database was searched, and records of patients showing the following criteria were selected: Caucasian subjects with permanent dentition (excluding third molars) who had undergone a CBCT exam for planning skeletal palatal anchorage with two miniscrews placed in the anterior palatine vault, aged between 14 and 22 y.o., with no history of previous orthodontic treatment, as well as the absence of craniofacial abnormalities or congenital syndromes, such as cleft lip and palate, cysts, or maxillary tumors. Moreover, the included subjects had the following records in their folders: digital models obtained with an intra-oral scanner, a supplementary maxillary scan taken for scan body position registration, and a CBCT scan of the maxilla stored as a DICOM file.
Twenty-four cases met the inclusion criteria; their records were checked for quality and integrity, and they were included in this investigation. Patients were stratified by gender and ordered by age within each group. A random sequence generator was used to create two lists of randomized numbers, each with 11 and 13 units.
The final sample size was determined through a preliminary power analysis, using data obtained from the first 10 patients included in the study. To ensure the robustness of the results, an additional evaluation was carried out based on studies available in the literature. The parameters considered for the analysis are as follows: 0° (planned miniscrew angulation), 2.3° (maximum angular discrepancy between the planned and final miniscrew axis), and 2.6 (common standard deviation). The power level was set at 0.8, and the significance level was set at 5%. The results of the analysis indicated that a sample of 21 cases would be sufficient to achieve the desired statistical power. To minimize the risk of false negative results, the sample size was increased to 24 subjects (12 females and 12 males). Case enrollment was performed using a balanced randomization system based on patient gender. The final sample included 24 subjects (mean age 18.4 ± 3.15 years), with 12 male subjects (mean age 17.7 ± 3.06 years) and 12 female subjects (mean age 19 ± 3.56 years). The overall sample included 8 subjects with skeletal Class I, 10 subjects with skeletal Class II, and 6 subjects with skeletal Class III. CBCT and lateral cephalogram records were generated using the Kavo OP 3D Pro CBCT scanner (Kavo Dental Technologies, Imaging Sciences International, Hatfield, PA, USA). The CBCT scans were acquired with a voxel size of 0.3 mm and a field of view (FOV) of 8 × 9 cm. The acquisition parameters for the CBCT examinations were set as follows: 90 kV, 6.3–8 mA, and an exposure time ranging from 5 to 8 s. Lateral cephalometric radiographs were performed using the following settings: 90 kV, 10 mA, and an exposure time of 16 s.
Digital maxillary models were obtained using an intraoral scanner (Medit i500, Medit, Seoul, Republic of Korea) and exported in STL file format with a resolution of 20 µm.
DICOM files and a maxillary digital model were imported into a specific software used for planning the 3-dimensional position of miniscrews (BlueSkyPlan software version 4.7, Blue Sky Bio, LLC, Grayslake, IL, USA).
Subsequently, Blue Sky Plan software was used to superimpose maxillary digital models and CBCT volumes (Figure 1). The software (internationally registered as a medical device) used an algorithm to automatically superimpose the digital maxillary model and the CBCT volume scan. Blue Sky Plan software was also used to design the surgical guide.
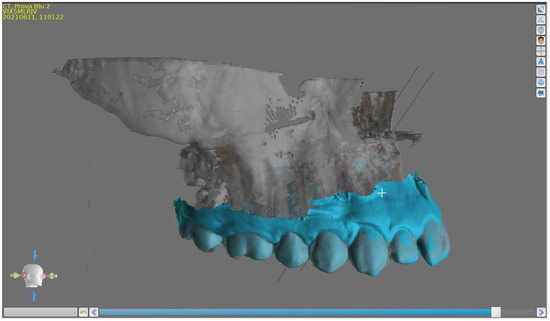
Figure 1.
BlueSky Plan Software interface, overlaying digital maxillary models and CBCT volumes.
The surgical guides were digitally designed using BlueSkyPlan software (version 4.7, Blue Sky Bio, LLC, Grayslake, IL, USA), a CE-certified medical software for 3D orthodontic planning and surgical guide design. The final guide models were exported in STL file format and processed using CHITUBOX software (version 64, Shenzhen CBD Technology Co., Ltd., Shenzhen, China) to generate the printing file. The guides were printed using a Form 2 stereolithography 3D printer (Formlabs, Millbury, OH, USA) with a layer thickness of 50 µm, employing a CE-certified Surgical Guide Resin (Formlabs). The printing process was performed according to the manufacturer’s guidelines. After printing, the guides underwent post-processing, including a 10 min isopropyl alcohol wash to remove residual resin, support removal, manual polishing, and a final 5 min light-curing cycle in a Form Cure unit (Formlabs, Millbury, OH, USA) at 60 °C. The surgical guides were designed to incorporate metal bushings provided by the miniscrew manufacturer (HDC, Thiene, VI, Italy), enabling precise coupling with a dedicated pick-up driver for controlled miniscrew insertion. Following the administration of local infiltration anesthesia with articaine 4% without vasoconstrictor (Ubistesin, 3M ESPE, Seefeld, Germany) to the palatal mucosa adjacent to the planned insertion sites, a pilot osteotomy was performed using a stainless steel lance drill (Ø 1.1 mm, HDC, Thiene, VI, Italy) at a rotational speed of 1500 rpm under continuous sterile saline irrigation. Predrilling was carried out to ensure controlled cortical perforation, reduce insertion torque, and improve the positional accuracy of the miniscrew.
Subsequently, palatal miniscrews (Regular Plus Konic, HDC, Thiene, VI, Italy) with a length of 10 mm and a diameter of 2.0 mm were inserted manually through the metal sleeves of the surgical guide using a dedicated pick-up driver provided by the manufacturer. Insertion was performed under strict aseptic conditions, with each screw advanced until its collar reached the guide sleeve surface, ensuring appropriate primary stability and optimal axial positioning. The insertion torque was manually controlled using a mechanical torque gauge and maintained within a range of 10–15 Ncm, following clinical safety recommendations for palatal miniscrew placement.
Once the orthodontic miniscrews were positioned, two dedicated scan bodies (HDC, Thiene, VI, Italy) made of medical-grade polyether ether ketone (PEEK) and measuring 5 mm in height were attached to the miniscrews. The position and angulation of the miniscrews were then registered by acquiring a new intraoral scan using a Medit i500 intraoral scanner (Medit, Seoul, Republic of Korea). The scanning protocol included a high-resolution setting with a scan resolution of 20 µm, starting from the occlusal surfaces of the maxillary teeth and extending to the palatal area, ensuring the optimal acquisition of the scan bodies’ profiles for precise digital superimposition (Figure 2).
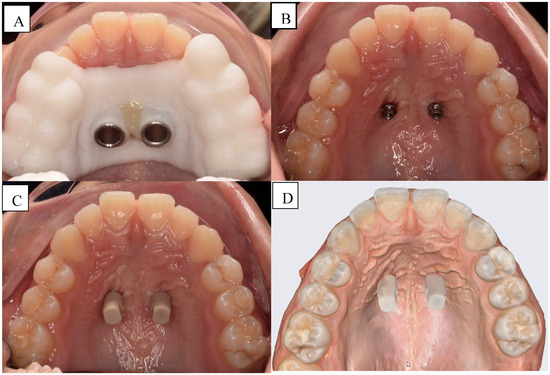
Figure 2.
(A) Testing of the template; (B) Miniscrew inserted; (C) Analogous application; (D) Intraoral scan with analogs inserted.
The post-insertion intraoral scan was used to digitally position two virtual analogs of the miniscrews in correspondence with the recorded scan body positions. These virtual analogs were then superimposed onto the preoperative planned miniscrew positions using the superimposition tool of BlueSkyPlan Software (version 4.7, Blue Sky Bio, LLC, Grayslake, IL, USA). The superimposition was performed using a best-fit surface-based alignment protocol on the surrounding palatal anatomy to ensure precise registration of pre- and post-operative datasets. Outcome measurements were performed bilaterally on both the right and left sides of each patient. The primary outcome, which was the maximum insertion angle discrepancy (MAD), was determined by visualizing and measuring the angular deviation between the long axis of the planned miniscrew and the actual inserted analog on the matched 3D models within the software interface. Angular measurements were expressed in degrees (°) and recorded for both sides of each case (Figure 3).
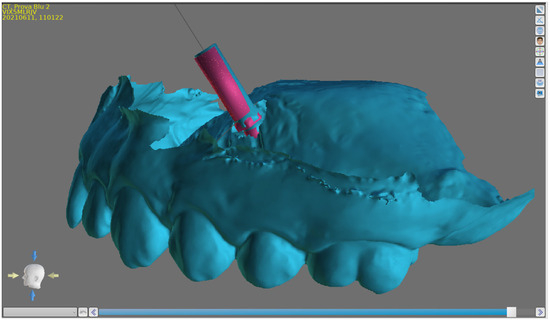
Figure 3.
Discrepancy between the planned and inserted miniscrew on 3D models.
A specific software function able to identify and show all the CBCT scans passing through the miniscrew axis of the planned miniscrew was used to identify the scan that showed the maximum discrepancy between the planned and final miniscrew placement. (Figure 4).
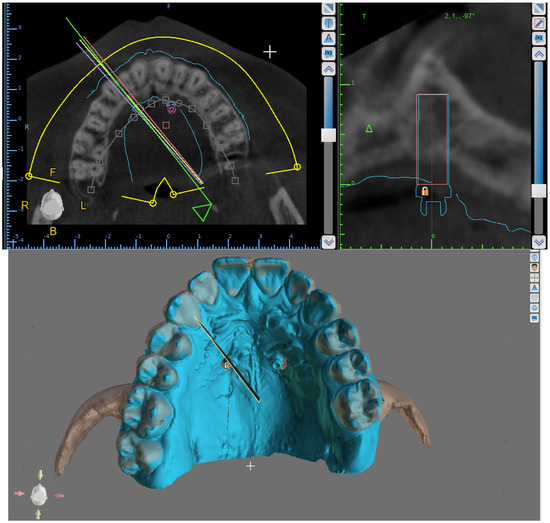
Figure 4.
Software interface: the maximum discrepancy between the placement of the planned miniscrew and the final miniscrew.
This scan was used to measure all the outcomes evaluated in this study: the maximum angular discrepancy (MAD); maximum vertical tip distance (VTD); maximum linear distance between the profiles of the planned and final miniscrews measured on lines parallel to the miniscrew axis (Figure 5); maximum horizontal tip discrepancy (HTDmax) perpendicular to the miniscrew axis; minimum horizontal tip discrepancy (HTDmin) (Figure 6); maximum vertical head distance (VHD); maximum horizontal head discrepancy (HHDmax); and minimum horizontal head discrepancy (HHDmin) (Figure 7).
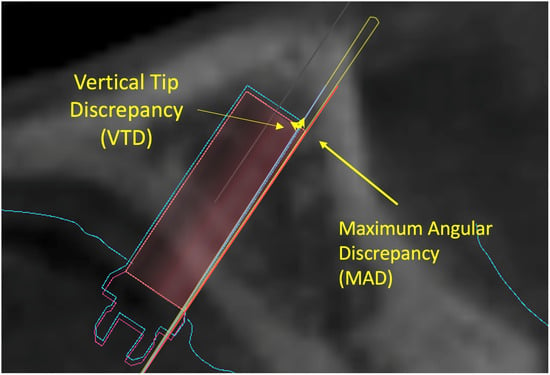
Figure 5.
Software interface: the identified maximum angular discrepancy (MAD), maximum vertical tip distance (VTD), and maximum linear distance between planned and final miniscrew profiles measured on lines parallel to the miniscrew axis.
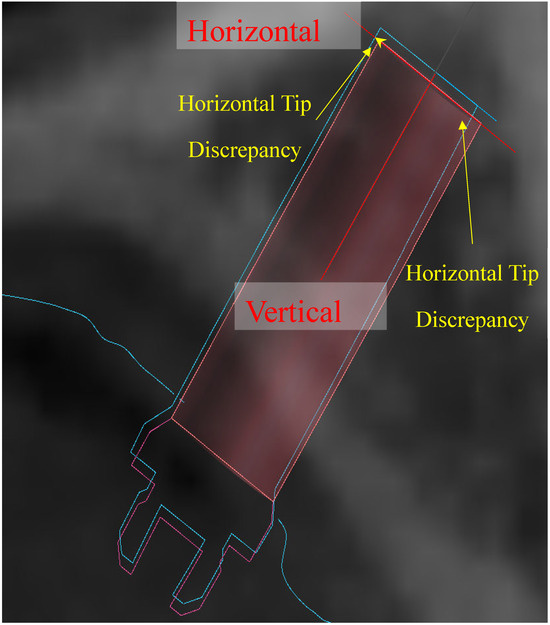
Figure 6.
Software interface: maximum horizontal tip discrepancy (HTDmax) and minimum horizontal tip discrepancy (HTDmin).
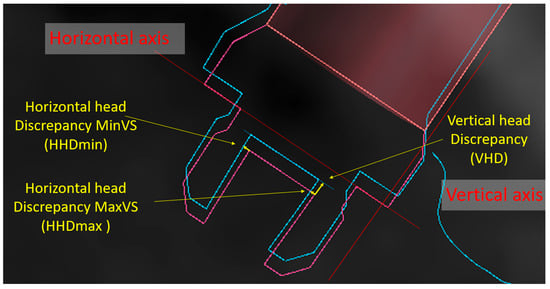
Figure 7.
Software interface: the maximum vertical head distance (VHD), maximum horizontal head discrepancy (HHDmax), and minimum horizontal head discrepancy (HHDmin).
3. Statistical Analysis
All measurements were performed by two orthodontists with at least ten years of clinical experience and advanced expertise in digital orthodontic technologies. To assess inter-operator consistency, a reproducibility analysis was conducted using the intraclass correlation coefficient (ICC), which demonstrated high agreement and confirmed excellent measurement reliability.
The statistical analysis included both descriptive and inferential methods. Descriptive statistics were calculated for each outcome variable, including the mean, standard deviation, and minimum and maximum values (Table 1). The normality of the angular deviation data between the planned and actual miniscrew insertion axes was verified using the Shapiro–Wilk test, which confirmed a normal distribution.

Table 1.
Descriptive statistics. Means, standard deviations, and minimum and maximum mean values.
Accordingly, a paired t-test was applied to assess whether the discrepancies between planned and actual positions were statistically significant (Table 2). No significant differences were observed between the right and left sides for any of the evaluated variables. As a result, the analysis was conducted on the entire sample without distinguishing between sides, focusing solely on the spatial reference points. All analyses were conducted in Stata software (version 17; StataCorp, College Station, TX, USA).

Table 2.
Inferential statistics. t-test Comparison between linear discrepancies with p = 0.05 and Spearman’s R = 0.05.
4. Results
A total of 24 patients underwent the bilateral insertion of palatal miniscrews, resulting in 48 screws analyzed. All measurements were performed on postoperative CBCT images and compared with the virtual insertion plan. The analysis revealed measurable discrepancies between the planned and actual positions; the mean angular deviation (MAD) between the planned and actual screw axes was 2.95° ± 1.13°, with a range of 0.9° to 5.19° (Figure 8). In terms of linear discrepancies, the mean horizontal deviation at the head level (Hor Head Dmax) was 0.30 mm ± 0.16 mm, whereas at the tip level (Hor Tip Dmax), it increased to 0.66 mm ± 0.21 mm; similarly, vertical deviations of 0.35 mm ± 0.21 mm at the head and 0.67 mm ± 0.67 mm at the tip were observed, confirming that deviations increase with the distance from the surgical guide, since the tip is geometrically farther from the fixed reference point. A paired t-test analysis showed that the discrepancies between the head and tip on the horizontal plane were significant on both the right and left sides (p < 0.05), indicating a systematic translation of the tip relative to the planned trajectory, while no significant differences were found between the right and left sides at the tip or the head, justifying the aggregation of bilateral data. Furthermore, the vertical discrepancy between the head and tip (VHD vs. VTD) was also significant (p < 0.05), indicating a three-dimensional inclination in the deviation. Spearman’s correlation analysis did not reveal statistically significant relationships between angular deviation (MAD) and linear discrepancies, either horizontal or vertical, at the head or tip levels, except for a weak but significant correlation between VHD and MAD (R < 0.05), suggesting that greater angular deviation may be associated with a slight increase in vertical head discrepancy.
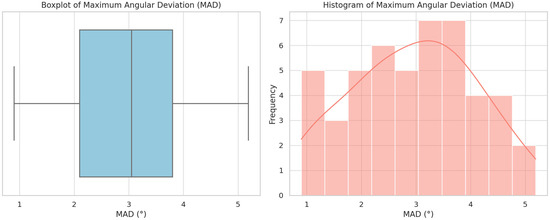
Figure 8.
Distribution of maximum angular deviations (MADs) between planned and actual miniscrew positions. The boxplot (left) illustrates the median, interquartile range, and potential outliers, highlighting the variability in insertion angles. The histogram (right), with an overlaid density curve, shows the frequency distribution of MAD values across the sample (n = 48), indicating a near-normal distribution with a slight right skew.
Despite the observed deviations, the data confirm that the use of customized surgical guides produced by 3D printing, combined with standardized protocols and the potential development of more rigid guiding systems to minimize mechanical tolerance, allows for a general improvement in accuracy compared to conventional techniques.
5. Discussion
The insertion site for orthodontic miniscrews is influenced by several clinical factors, including the direction of intended tooth movement, anchorage requirements, and anatomical limitations. Although the anterior palate is a commonly preferred site due to its favorable bone quality and thickness, several studies have highlighted its high anatomical variability. For this reason, a preliminary evaluation using cone beam computed tomography (CBCT) is strongly recommended to ensure accurate and safe placement, particularly in cases involving impacted teeth or narrow maxillary arches [17,18,19,20].
The use of 3D-printed surgical guides has been proposed to enhance the accuracy and reproducibility of miniscrew insertion. Numerous authors have compared traditional free-hand placement with guided insertion using 3D templates, reporting significantly better outcomes in terms of angular and linear deviations when surgical guides are employed [21,22,23].
These guides have proven effective not only in palatal insertions but also in more challenging anatomical regions such as the infrazygomatic crest and interradicular space [21,24,25].
Quantitative assessments using pre- and postoperative CBCT scans have confirmed the improved precision of guided insertion techniques, which reduces the risk of iatrogenic damage to adjacent roots or the maxillary sinus [23,26].
Two different studies conducted on cadavers [27] and phantoms [28] showed that miniscrew-assisted placement with a surgical guide is more accurate than free-hand placement in terms of both angular deviation and mesiodistal deviation in the coronal and apical miniscrew areas [27,28].
A recent study by Pozzan et al. [22] analyzed the accuracy of palatal miniscrew placement in a digital workflow, assessing errors at multiple stages, from virtual planning to laboratory model fabrication and clinical insertion. They highlighted how even small deviations during the lab phase (mean angular error ~2.12°) could contribute to cumulative inaccuracies that compromise the final clinical outcome, particularly in protocols requiring high-precision insertion.
Discrepancies between planned and achieved miniscrew positions may result from several factors, including patient-specific bone morphology, operator experience, and procedural inconsistencies [29,30].
Although digital scanners have demonstrated high reliability in the literature [29], operator skill and environmental conditions can still affect scan accuracy. Therefore, standardized protocols and the precise execution of each step in the digital workflow are essential for optimizing outcomes.
In the context of single-visit protocols, accurate digital planning followed by predrilling using a surgical guide ensures optimal screw angulation and minimizes undercuts. This facilitates the insertion of TADs and the immediate fit of orthodontic appliances, ultimately reducing chair time and enhancing clinical efficiency [31].
The present study aimed to evaluate the real-world accuracy of 3D-printed surgical guides for palatal miniscrew insertion by comparing the digitally planned position with the actual postoperative outcome. Through the superimposition of STL models from the planning phase and the final clinical scan, discrepancies in the insertion angle and spatial deviation were measured at both the screw head and tip.
The results revealed greater horizontal and vertical discrepancies at the tip than at the head, which is consistent with the geometric amplification of angular deviations as distance increases. The mean angular deviation between the planned and final screw insertion axes was 2.95° (SD ± 1.13°), which is lower than that reported by Pozzan et al. (5.7° ± 3.42°), possibly due to the exclusion of the laboratory-derived errors in the current workflow. These findings underscore the clinical relevance of each step in the digital protocol and reinforce the value of surgical guides in improving insertion precision.
Future Research Directions and Possible Applications
The findings of this study indicate that customized surgical guides, digitally planned and fabricated through 3D printing, allow for the effective clinical transfer of the virtually defined 3D position of palatal miniscrews. Nonetheless, the angular and linear discrepancies observed—although limited—highlight the need for the further refinement of each phase within the digital workflow. The greater deviations noted at the screw tip, likely due to the cumulative effect of mechanical tolerances and inherent limitations of printing and component coupling, underscore the importance of standardizing clinical–digital protocols. Looking ahead, future developments may include the integration of artificial intelligence algorithms to predict deviation risk and the adoption of dynamic navigation or robotic systems to enhance placement accuracy. Clinically, personalized guides may prove especially valuable in patients with unfavorable palatal anatomy because they improve insertion safety and the biomechanical reliability of skeletal anchorage. Long-term studies will be necessary to determine whether the detected deviations have a significant impact on primary stability or the functional longevity of miniscrews in vivo.
6. Conclusions
The use of 3D-printed surgical guides for palatal miniscrew insertion resulted in a mean angular deviation of 2.95° (SD ± 1.13°), demonstrating a clear improvement in placement accuracy compared with free-hand techniques. However, even small apex-level discrepancies may compromise the efficacy of single-visit protocols, where miniscrew insertion and appliance attachment are completed during a single appointment.
Guided insertion proved particularly beneficial in anatomically challenging scenarios—such as narrow palatal vaults, transverse maxillary dysplasia, impacted teeth, or infrazygomatic sites—by reducing the risk of root or nasal cavity perforation.
An integrated digital–laboratory workflow combining CBCT-based planning, intra-oral scanning, and the use of scan bodies enables the precise registration of miniscrew positions for the fabrication of customized palatal appliances. This approach obviates the need for conventional impressions, enhances patient comfort, and streamlines clinical procedures.
To further reduce cumulative errors, clinicians should rigorously standardize each step of the digital workflow (imaging, planning, guide fabrication, and insertion) and undertake dedicated training in 3D planning software and guided surgery protocols. A pre-operative CBCT is recommended in cases of limited bone volume or complex anatomy to verify the planned trajectory.
Prospective, randomized comparisons of different guided systems are now warranted to confirm these findings and optimize single-visit protocols for palatal miniscrew placement.
Author Contributions
Conceptualization, A.M.B., E.C. and S.B.; data curation, A.M.B., E.C. and S.B.; formal analysis, A.M.B., E.C., M.P. and D.A.; funding acquisition, A.M.B. and R.N.; investigation, A.M.B., E.C., S.B. and D.A.; methodology, A.M.B., E.C., S.B. and D.A.; project administration, D.A. and R.N.; resources, A.M.B., E.C., S.B., D.A. and R.N.; software, D.A. and R.N.; supervision, D.A., A.M. and R.N.; validation, D.A. and R.N.; visualization, M.P. and R.N.; roles/writing—original draft, A.M.B. and R.N.; writing—review and editing, A.M.B., D.A. and R.N. All authors have read and agreed to the published version of the manuscript.
Funding
This work was partially supported by the European Union (NextGeneration EU) through the MUR-PNRR project SAMOTHRACE (ECS00000022).
Institutional Review Board Statement
The study proposal received joint approval by the Ethics Committee of Messina (prot. 33-2020).
Data Availability Statement
All raw data are publicly available upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Stursa, L.; Wendl, B.; Jakse, N.; Pichelmayer, M.; Weiland, F.; Antipova, V.; Kirnbauer, B. Accuracy of Palatal Orthodontic Mini-Implants Placed Using Fully Digital Planned Insertion Guides: A Cadaver Study. J. Clin. Med. 2023, 12, 6782. [Google Scholar] [CrossRef] [PubMed]
- Santmartí-Oliver, M.; Jorba-García, A.; Moya-Martínez, T.; de-la-Rosa-Gay, C.; Camps-Font, O. Safety and Accuracy of Guided Interradicular Miniscrew Insertion: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 7697. [Google Scholar] [CrossRef] [PubMed]
- Schwärzler, A.; Ludwig, B.; Chitan, P.; Lettner, S.; Sagl, B.; Jonke, E. Transfer accuracy of 3D printed versus CAD/CAM milled surgical guides for temporary orthodontic implants: A preclinical micro CT study. J. Dent. 2024, 146, 105060. [Google Scholar] [CrossRef] [PubMed]
- Antoszewska-Smith, J.; Sarul, M.; Łyczek, J.; Konopka, T.; Kawala, B. Effectiveness of orthodontic miniscrew implants in anchorage reinforcement during en-masse retraction: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 440–455. [Google Scholar] [CrossRef]
- Di Leonardo, B.; Ludwig, B.; Lisson, J.A.; Contardo, L.; Mura, R.; Hourfar, J. Insertion torque values and success rates for paramedian insertion of orthodontic mini-implants: A retrospective study. J. Orofac. Orthop. 2018, 79, 109–115. [Google Scholar] [CrossRef]
- Faegheh, G.; Khosravifard, N.; Maleki, D.; Hosseini, S.K. Evaluation of Palatal Bone Thickness and Its Relationship with Palatal Vault Depth for Mini-Implant Insertion Using Cone Beam Computed Tomography Images. Turk. J. Orthod. 2022, 35, 120–126. [Google Scholar] [CrossRef]
- Nucera, R.; Costa, S.; Bellocchio, A.M.; Barbera, S.; Drago, S.; Silvestrini, A.; Migliorati, M. Evaluation of palatal bone depth, cortical bone, and mucosa thickness for optimal orthodontic miniscrew placement performed according to the third palatal ruga clinical reference. Eur. J. Orthod. 2022, 44, 530–536. [Google Scholar] [CrossRef]
- Negrisoli, S.; Angelieri, F.; Gonçalves, J.R.; da Silva, H.D.P.; Maltagliati, L.; Raphaelli Nahás-Scocate, A.C. Assessment of the bone thickness of the palate on cone-beam computed tomography for placement of miniscrew-assisted rapid palatal expansion appliances. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 849–857. [Google Scholar] [CrossRef]
- Blasi, A.; Nucera, R.; Ronsivalle, V.; Candida, E.; Grippaudo, C. Asymmetry index for the photogrammetric assessment of facial asymmetry. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 394–402. [Google Scholar] [CrossRef]
- Sánchez-Riofrío, D.; Viñas, M.J.; Ustrell-Torrent, J.M. CBCT and CAD-CAM technology to design a minimally invasive maxillary expander. BMC Oral. Health 2020, 20, 303. [Google Scholar] [CrossRef]
- Aiello, D.; Nucera, R.; Costa, S.; Figliuzzi, M.M.; Paduano, S. A Simplified Digital Approach to the Treatment of a Postpuberty Patient with a Class III Malocclusion and Bilateral Crossbite. Case Rep. Dent. 2021, 2021, 3883187. [Google Scholar] [CrossRef] [PubMed]
- Burak, K.; Hilmi, B.M. Evaluating palatal mucosal thickness in orthodontic miniscrew sites using cone-beam computed tomography. BMC Oral. Health 2024, 24, 1153. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Schneider, D.; Ganeles, J.; Wismeijer, D.; Zwahlen, M.; Hämmerle, C.H.; Tahmaseb, A. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral. Maxillofac. Implant. 2009, 24, 92–109. [Google Scholar]
- D’Haese, J.; Van De Velde, T.; Komiyama, A.; Hultin, M.; De Bruyn, H. Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: A review of the literature. Clin. Implant. Dent. Relat. Res. 2012, 14, 321–335. [Google Scholar] [CrossRef]
- Poggio, P.M.; Incorvati, C.; Velo, S.; Carano, A. “Safe zones”: A guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 2006, 76, 191–197. [Google Scholar] [CrossRef]
- Kim, T.; Lee, S.; Kim, G.B.; Hong, D.; Kwon, J.; Park, J.W.; Kim, N. Accuracy of a simplified 3D-printed implant surgical guide. J. Prosthet. Dent. 2020, 124, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Baumgaertel, S. Quantitative investigation of palatal bone depth and cortical bone thickness for mini-implant placement in adults. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 104–108. [Google Scholar] [CrossRef]
- Hourfar, J.; Ludwig, B.; Bister, D.; Braun, A.; Kanavakis, G. The most distal palatal ruga for placement of orthodontic mini-implants. Eur. J. Orthod. 2015, 37, 373–378. [Google Scholar] [CrossRef]
- Nucera, R.; Ciancio, E.; Maino, G.; Barbera, S.; Imbesi, E.; Bellocchio, A.M. Evaluation of bone depth, cortical bone, and mucosa thickness of palatal posterior supra-alveolar insertion site for miniscrew placement. Prog. Orthod. 2022, 23, 18. [Google Scholar] [CrossRef]
- Maino, B.G.; Paoletto, E.; Lombardo, L., 3rd; Siciliani, G. A Three-Dimensional Digital Insertion Guide for Palatal Miniscrew Placement. J. Clin. Orthod. 2016, 50, 12–22. [Google Scholar]
- Su, L.; Song, H.; Huang, X. Accuracy of two orthodontic mini-implant templates in the infrazygomatic crest zone: A prospective cohort study. BMC Oral. Health 2022, 22, 252. [Google Scholar] [CrossRef] [PubMed]
- Pozzan, L.; Migliorati, M.; Dinelli, L.; Riatti, R.; Torelli, L.; Di Lenarda, R.; Contardo, L. Accuracy of the digital workflow for guided insertion of orthodontic palatal TADs: A step-by-step 3D analysis. Prog. Orthod. 2022, 23, 27. [Google Scholar] [CrossRef] [PubMed]
- Wilmes, B.; Vasudavan, S.; Drescher, D. CAD-CAM-fabricated mini-implant insertion guides for the delivery of a distalization appliance in a single appointment. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.C.; Huang, J.N.; Zhao, S.F.; Xu, X.J.; Xie, Z.J. Radiographic and surgical template for placement of orthodontic microimplants in interradicular areas: A technical note. Int. J. Oral. Maxillofac. Implant. 2006, 21, 629–634. [Google Scholar]
- Yuan, L.; Zhao, R.; Liu, J.; Tang, R.; Bai, S.; Liu, X. The success rate of infrazygomatic mini-implants placed with and without surgical guides: A historical control study. BMC Oral. Health 2025, 25, 124. [Google Scholar] [CrossRef]
- Cantarella, D.; Savio, G.; Grigolato, L.; Zanata, P.; Berveglieri, C.; Lo Giudice, A.; Isola, G.; Del Fabbro, M.; Moon, W. A New Methodology for the Digital Planning of Micro-Implant-Supported Maxillary Skeletal Expansion. Med. Devices 2020, 13, 93–106. [Google Scholar] [CrossRef]
- Bae, M.J.; Kim, J.Y.; Park, J.T.; Cha, J.Y.; Kim, H.J.; Yu, H.S.; Hwang, C.J. Accuracy of miniscrew surgical guides assessed from cone-beam computed tomography and digital models. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 893–901. [Google Scholar] [CrossRef]
- Qiu, L.; Haruyama, N.; Suzuki, S.; Yamada, D.; Obayashi, N.; Kurabayashi, T.; Moriyama, K. Accuracy of orthodontic miniscrew implantation guided by stereolithographic surgical stent based on cone-beam CT-derived 3D images. Angle Orthod. 2012, 82, 284–293. [Google Scholar] [CrossRef]
- Melo, A.C.; Andrighetto, A.R.; Hirt, S.D.; Bongiolo, A.L.; Silva, S.U.; Silva, M.A. Risk factors associated with the failure of miniscrews—A ten-year cross sectional study. Braz. Oral. Res. 2016, 30, e124. [Google Scholar] [CrossRef]
- Crismani, A.G.; Bertl, M.H.; Celar, A.G.; Bantleon, H.P.; Burstone, C.J. Miniscrews in orthodontic treatment: Review and analysis of published clinical trials. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 108–113. [Google Scholar] [CrossRef]
- Maino, B.G.; Paoletto, E.; Cremonini, F.; Liou, E.; Lombardo, L. Tandem Skeletal Expander and MAPA Protocol for Palatal Expansion in Adults. J. Clin. Orthod. 2020, 54, 690–704. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).