Retrospective Analysis of Full-Arch Zirconia Rehabilitations on Dental Implants: Clinical Outcomes and Patient Satisfaction
Abstract
1. Introduction
- Zirconia–titanium hybrid ISFCDPs: a monolithic zirconia prosthesis (Katana YML 1050 MPa, Kuraray Noritake, Tokyo, Japan) is glued on a titanium framework and acts as the esthetic and functional portion of the prosthesis, while a titanium framework provides elasticity and force dissipation to the system. The prosthesis is usually screwed directly on the implants or on Multi-Unit Abutments (MUAs), depending on the implant orientation.
- Progressive monolithic zirconia ISFCDPs: a monolithic zirconia prosthesis (Katana HTML 1200 MPa, Kuraray Noritake) is glued on dedicated components and screwed directly on the implants, without the use of a titanium framework. The progressive nature of zirconia is provided by layers with a different yttria molarity, with the more esthetic zirconia on the external section of the prosthesis and stronger zirconia at the core.
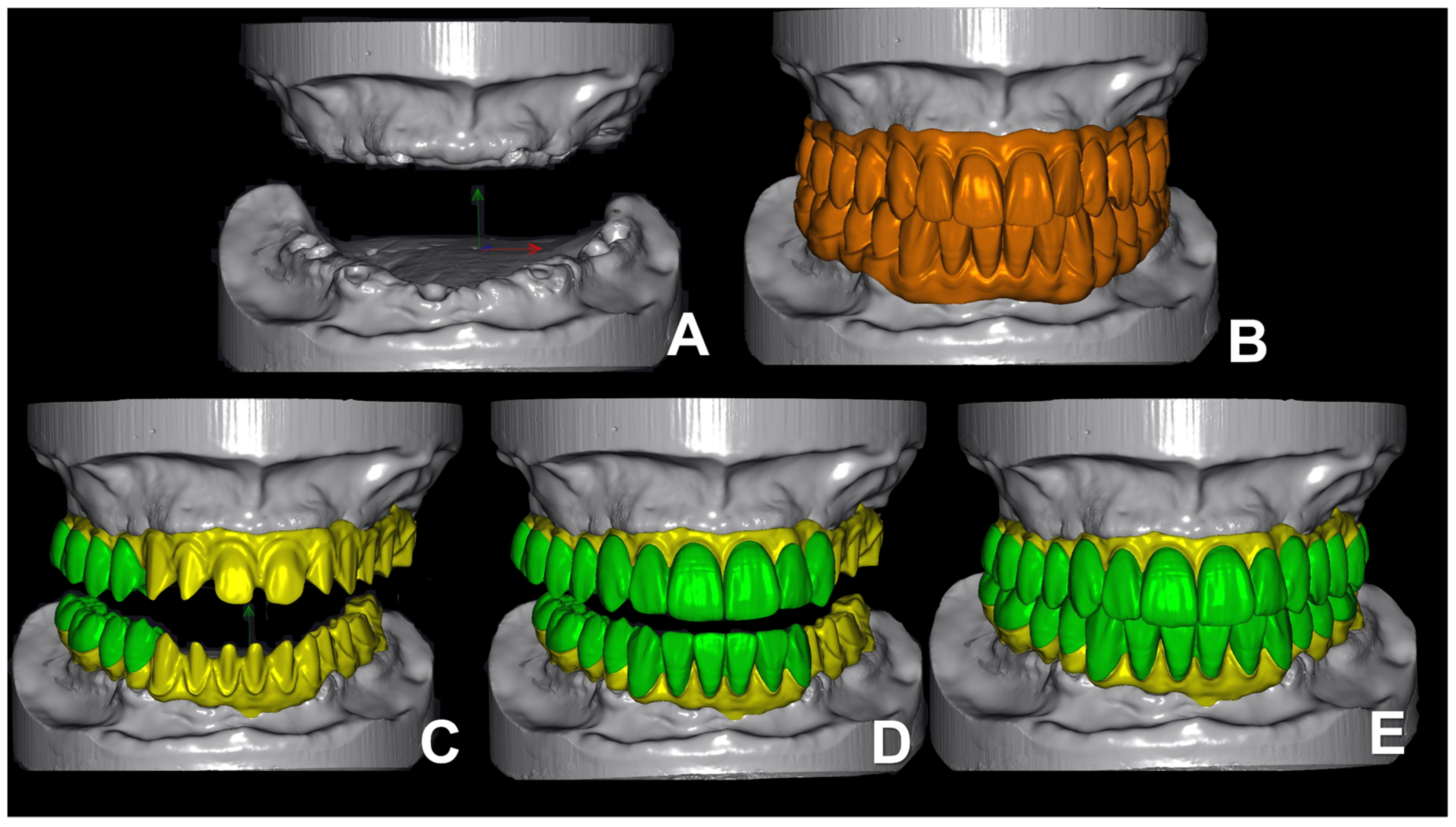
- Zirconia-on-zirconia (Zirc-on-Zirc) ISFCDPs are produced with a protocol in which a high-strength and opaque zirconia framework (Katana HTML 1200 Mpa, Kuraray Noritake) is glued on dedicated components to screw it directly on the implants, while highly esthetic zirconia crowns (Katana STML 750 MPa, Kuraray Noritake) are cemented on the zirconia framework using a fluid ceramic fused at high temperatures.
2. Materials and Methods
- Patients treated with a zirconia ISFCDP.
- Patients following a periodontal maintenance program with at least one recall visit per year.
- Minimum follow-up of 1 year after prosthetic delivery.
- Patient treated with implant-supported fixed partial prosthesis.
- Patients with uncontrolled systemic diseases, were under treatment with medication that could interfere with bone metabolism, or who received radiation treatment in neck or head area.
- Patients not following a periodontal maintenance program.
- Patients affected by untreated periodontal disease.
- Heavy smokers (>10 cigarettes per day).
- Buccal soft tissue dehiscence: presence of implant threads clinically visible.
- Implant threads exposure: exposure of implant threads, both in presence of a buccal soft tissue dehiscence or covered by soft tissue (presence of a dark shade under the soft tissue in a position corresponding to an implant).
- Chipping of the esthetic part of the ISCFPDs: presence and position of one or more partial fractures of the pink ceramic.
- Past or present fracture of the framework or functional structure: full framework fracture, cracks or fractures related to the functional part of the ISFCDPs, requiring in-lab repairment.
- Past or present unscrewing of the ISCFPD: requirement of screw tightening during one of the follow-up visits.
- Pocket probing depth (PPD) at implant level: probing was performed using a 15 mm UNC-15 probe (Hu-Friedy) on six sites around each implant (two vestibular, two lingual/palatal and two interproximal, one mesial and one distal). A probing depth of more than 6 mm was considered a sign of peri-implantitis.
- Bleeding on probing at implant level: present in case of bleeding after gentle probing in a nearby site. The presence of bleeding on probing was considered a sign of peri-implantitis.
- Purulent discharge: present in case of purulent discharge appearing after probing, which is considered a sign of peri-implantitis.
- Local signs of inflammation: present in case of clear signs of swelling, redness, pain on probing or spontaneous pain corresponding to an implant; all considered signs of peri-implantitis.
- Statistical methods and sample size
3. Results
4. Discussion
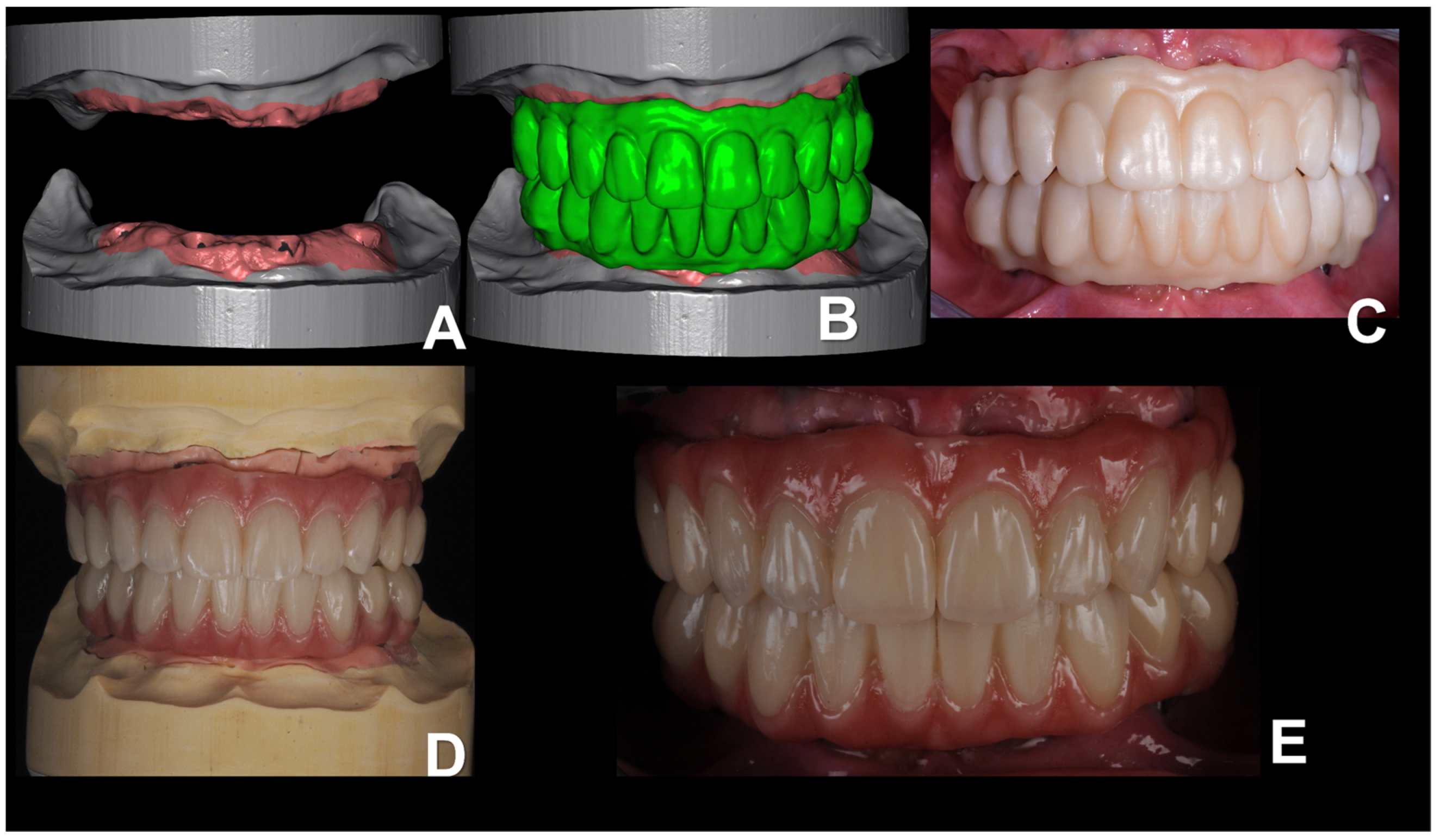
- Zirconia–titanium hybrid ISFCDPs (Figure 1)
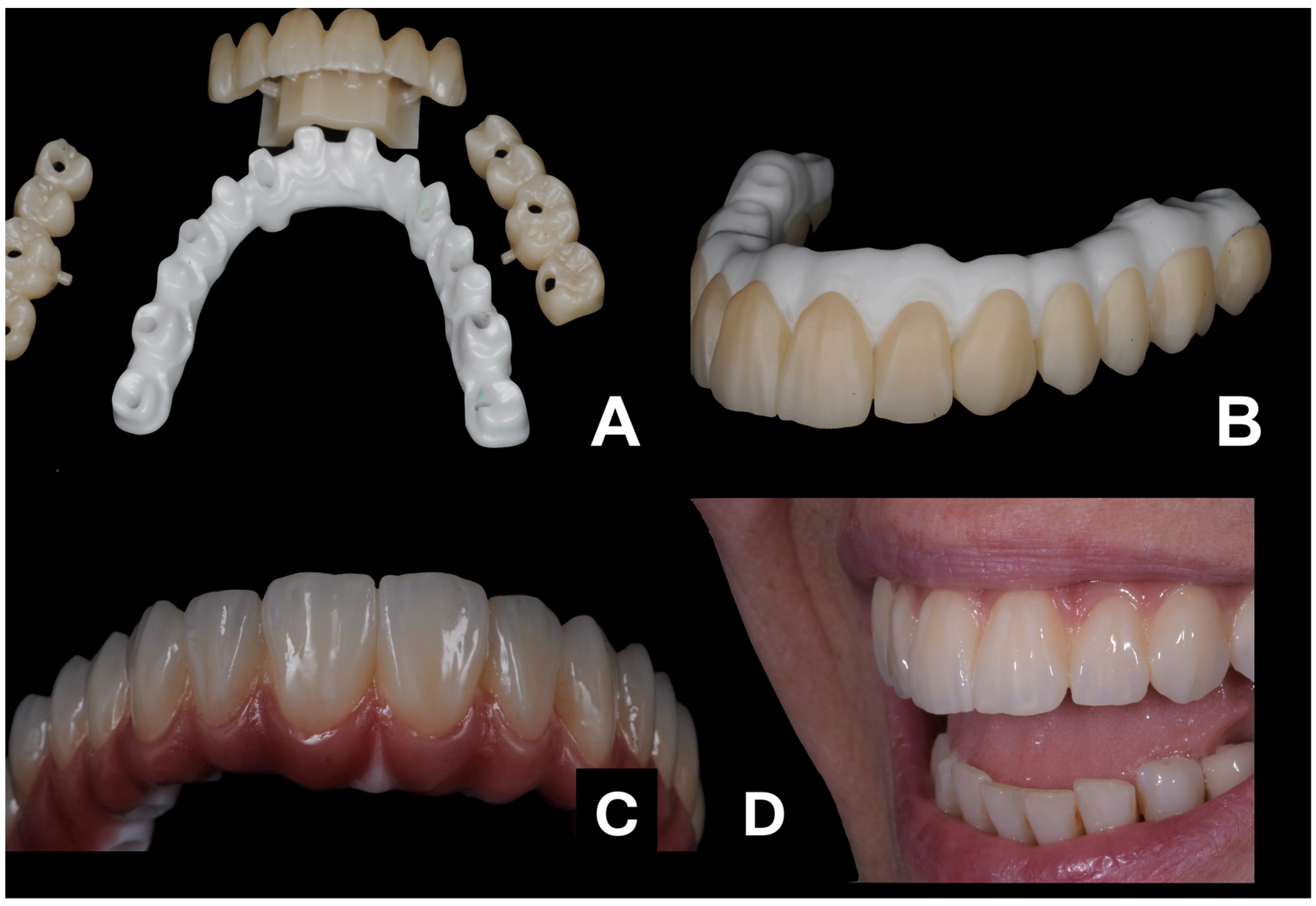
- Progressive (or multi-layer) Zirconia ISFCDPs (Figure 2)
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Madfa, A.; Al-Sanabani, F.; Al-Qudami, N.; Al-Sanabani, J.; Amran, A. Use of Zirconia in Dentistry: An Overview. Open Biomater. J. 2014, 5, 1–9. [Google Scholar] [CrossRef]
- Ghodsi, S.; Jafarian, Z. A Review on Translucent Zirconia. Eur. J. Prosthodont. Restor. Dent. 2018, 26, 62–74. [Google Scholar]
- Cesar, P.F.; Miranda, R.B.P.; Santos, K.F.; Scherrer, S.S.; Zhang, Y. Recent advances in dental zirconia: 15 years of material and processing evolution. Dent. Mater. 2024, 40, 824–836. [Google Scholar] [CrossRef]
- Zarb, G.A.; Schmitt, A. The edentulous predicament. I: A prospective study of the effectiveness of implant-supported fixed prostheses. J. Am. Dent. Assoc. 1996, 127, 59–65. [Google Scholar] [CrossRef]
- Carlsson, G.E. Facts and fallacies: An evidence base for complete dentures. Dent. Update 2006, 33, 134–142. [Google Scholar] [CrossRef]
- Fueki, K.; Kimoto, K.; Ogawa, T.; Garrett, N.R. Effect of implant-supported or retained dentures on masticatory performance: A systematic review. J. Prosthet. Dent. 2007, 98, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Limmer, B.; Sanders, A.E.; Reside, G.; Cooper, L.F. Complications and patient-centered outcomes with an implant-supported monolithic zirconia fixed dental prosthesis: 1 year results. J. Prosthodont. 2014, 23, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Cooper, L.F. The current and future treatment of edentulism. J. Prosthodont. 2009, 18, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Felton, D.A. Edentulism and comorbid factors. J. Prosthodont. 2009, 18, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Cinquini, C.; Alfonsi, F.; Marchio, V.; Gallo, F.; Zingari, F.; Bolzoni, A.R.; Romeggio, S.; Barone, A. The Use of Zirconia for Implant-Supported Fixed Complete Dental Prostheses: A Narrative Review. Dent. J. 2023, 11, 144. [Google Scholar] [CrossRef]
- Fischer, K.; Stenberg, T. Prospective 10-year cohort study based on a randomized, controlled trial (RCT) on implant-supported full-arch maxillary prostheses. part II: Prosthetic outcomes and maintenance. Clin. Implant. Dent. Relat. Res. 2013, 15, 498–508. [Google Scholar] [CrossRef] [PubMed]
- Morton, D.; Gallucci, G.; Lin, W.S.; Pjetursson, B.; Polido, W.; Roehling, S.; Sailer, I.; Aghaloo, T.; Albera, H.; Bohner, L.; et al. Group 2 ITI Consensus Report: Prosthodontics and implant dentistry. Clin. Oral. Implants Res. 2018, 29 (Suppl. S16), 215–223. [Google Scholar] [CrossRef]
- Abdulmajeed, A.A.; Lim, K.G.; Närhi, T.O.; Cooper, L.F. Complete-arch implant-supported monolithic zirconia fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2016, 115, 672–677.e671. [Google Scholar] [CrossRef]
- Churruca, K.; Pomare, C.; Ellis, L.A.; Long, J.C.; Henderson, S.B.; Murphy, L.E.D.; Leahy, C.J.; Braithwaite, J. Patient-reported outcome measures (PROMs): A review of generic and condition-specific measures and a discussion of trends and issues. Health Expect 2021, 24, 1015–1024. [Google Scholar] [CrossRef]
- Larsson, C.; Vult von Steyern, P.; Nilner, K. A prospective study of implant-supported full-arch yttria-stabilized tetragonal zirconia polycrystal mandibular fixed dental prostheses: Three-year results. Int. J. Prosthodont. 2010, 23, 364–369. [Google Scholar]
- Pjetursson, B.E.; Sailer, I.; Zwahlen, M.; Hämmerle, C.H. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: Single crowns. Clin. Oral. Implants Res. 2007, 18 (Suppl. S3), 73–85. [Google Scholar] [CrossRef]
- Delucchi, F.; De Giovanni, E.; Pesce, P.; Bagnasco, F.; Pera, F.; Baldi, D.; Menini, M. Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies. Materials 2021, 14, 3251. [Google Scholar] [CrossRef] [PubMed]
- Tiossi, R.; Gomes, É.A.; Faria, A.C.L.; Rodrigues, R.C.S.; Ribeiro, R.F. Biomechanical behavior of titanium and zirconia frameworks for implant-supported full-arch fixed dental prosthesis. Clin. Implant. Dent. Relat. Res. 2017, 19, 860–866. [Google Scholar] [CrossRef]
- Pelekanos, S.; Ntovas, P.; Rizou, V.; Pozzi, A. Translucent monolithic zirconia titanium-supported FP1 full-arch prosthesis: A novel proof of concept to address esthetic, functional, and biologic challenges. J. Esthet. Restor. Dent. 2024, 36, 197–206. [Google Scholar] [CrossRef]
- Mijiritsky, E.; Elad, A.; Krausz, R.; Ivanova, V.; Zlatev, S. Clinical performance of full-arch implant-supported fixed restorations made of monolithic zirconia luted to a titanium bar: A retrospective study with a mean follow-up of 16 months. J. Dent. 2023, 137, 104675. [Google Scholar] [CrossRef]
- Kolgeci, L.; Mericske, E.; Worni, A.; Walker, P.; Katsoulis, J.; Mericske-Stern, R. Technical complications and failures of zirconia-based prostheses supported by implants followed up to 7 years: A case series. Int. J. Prosthodont. 2014, 27, 544–552. [Google Scholar] [CrossRef] [PubMed]


| Sample Characteristics | Number |
|---|---|
| Number of Patients | 14 |
| Males | 5 |
| Females | 9 |
| Mean Age | 64 |
| Number of ISFCDPs | 14 |
| Maxillary ISFCDPs | 10 |
| Mandibular ISFCDPs | 4 |
| Maxillary Zirc-on-Zirc ISFCDPs | 3 |
| Mandibular Zirc-on-Zirc ISFCDPs | 2 |
| Maxillary Progressive Monolithic Zirconia ISFCDPs | 3 |
| Mandibular Progressive Monolithic Zirconia ISFCDPs | 0 |
| Maxillary Zirconia-on-Titanium ISFCDPs | 4 |
| Mandibular Zirconia-on-Titanium ISFCDPs | 2 |
| Number of Implants | 86 |
| Mean Follow-up Time (Months) | 36 |
| Complications | Number (%) |
|---|---|
| Implants showing purulent discharge | 3 (3.49%) |
| Sites with PPD > 3 mm but <5 mm | 15 (2.7%) |
| Sites with swelling and redness | 2 (0.3%) |
| Sites with bleeding on probing (BoP) | 26 (4.7%) |
| Chipping | 1 (pink gingiva) (7.1%) |
| Patients with at least one implant spire exposure. | 6 (42.86%) |
| Complications | Zirc-on-Zirc ISFCDPs | Progressive Zirconia ISFCDPs | Zirconia-on-Titanium ISFCDPs |
|---|---|---|---|
| Presence of purulent discharge (over total n° of ISFCDPs) | 1/5 | 0/3 | 0/6 |
| Presence of sites with PPD >3 mm but <5 mm (over total n° of ISFCDPs) | 2/5 | 2/3 | 0/6 |
| Presence of sites with swelling and redness (over total n° of ISFCDPs) | 2/5 | 2/3 | 0/6 |
| Sites with bleeding on probing (over total n° of ISFCDPs) | 2/5 | 2/3 | 0/6 |
| Chipping (over total n° of ISFCDPs) | 1/5 | 0/3 | 0/3 |
| Presence of at least one implant spire exposure (over total n° of ISFCDPs) | 2/5 | 2/3 | 2/6 |
| Satisfaction | Percentage |
|---|---|
| Completely satisfied | 78.57% |
| Very satisfied | 14.53% |
| Satisfied | 7.14% |
| Not satisfied | 0% |
| Would recommend treatment with ISFCDPs | 100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marchio, V.; Cinquini, C.; Alfonsi, F.; Romeggio, S.; Stoppaccioli, M.; Zingari, F.; Priami, M.; Barone, A. Retrospective Analysis of Full-Arch Zirconia Rehabilitations on Dental Implants: Clinical Outcomes and Patient Satisfaction. Appl. Sci. 2025, 15, 416. https://doi.org/10.3390/app15010416
Marchio V, Cinquini C, Alfonsi F, Romeggio S, Stoppaccioli M, Zingari F, Priami M, Barone A. Retrospective Analysis of Full-Arch Zirconia Rehabilitations on Dental Implants: Clinical Outcomes and Patient Satisfaction. Applied Sciences. 2025; 15(1):416. https://doi.org/10.3390/app15010416
Chicago/Turabian StyleMarchio, Vincenzo, Chiara Cinquini, Fortunato Alfonsi, Stefano Romeggio, Marco Stoppaccioli, Francesco Zingari, Mattia Priami, and Antonio Barone. 2025. "Retrospective Analysis of Full-Arch Zirconia Rehabilitations on Dental Implants: Clinical Outcomes and Patient Satisfaction" Applied Sciences 15, no. 1: 416. https://doi.org/10.3390/app15010416
APA StyleMarchio, V., Cinquini, C., Alfonsi, F., Romeggio, S., Stoppaccioli, M., Zingari, F., Priami, M., & Barone, A. (2025). Retrospective Analysis of Full-Arch Zirconia Rehabilitations on Dental Implants: Clinical Outcomes and Patient Satisfaction. Applied Sciences, 15(1), 416. https://doi.org/10.3390/app15010416







