Digital Medical X-ray Imaging, CAD in Lung Cancer and Radiomics in Colorectal Cancer: Past, Present and Future
Abstract
1. Introduction
2. Past
2.1. Digitization
2.2. From Analogic to Digital
- (1)
- Finding signs of disease on diagnostic images.
- (2)
- Helping in the operating room, locally or remotely, without tiredness or tremors.
- (3)
- Combining patient information in a way that is useful for diagnosis and research. In other words: big data, for predictive analysis of large amounts of information.
2.3. Beyond Digital
3. Present
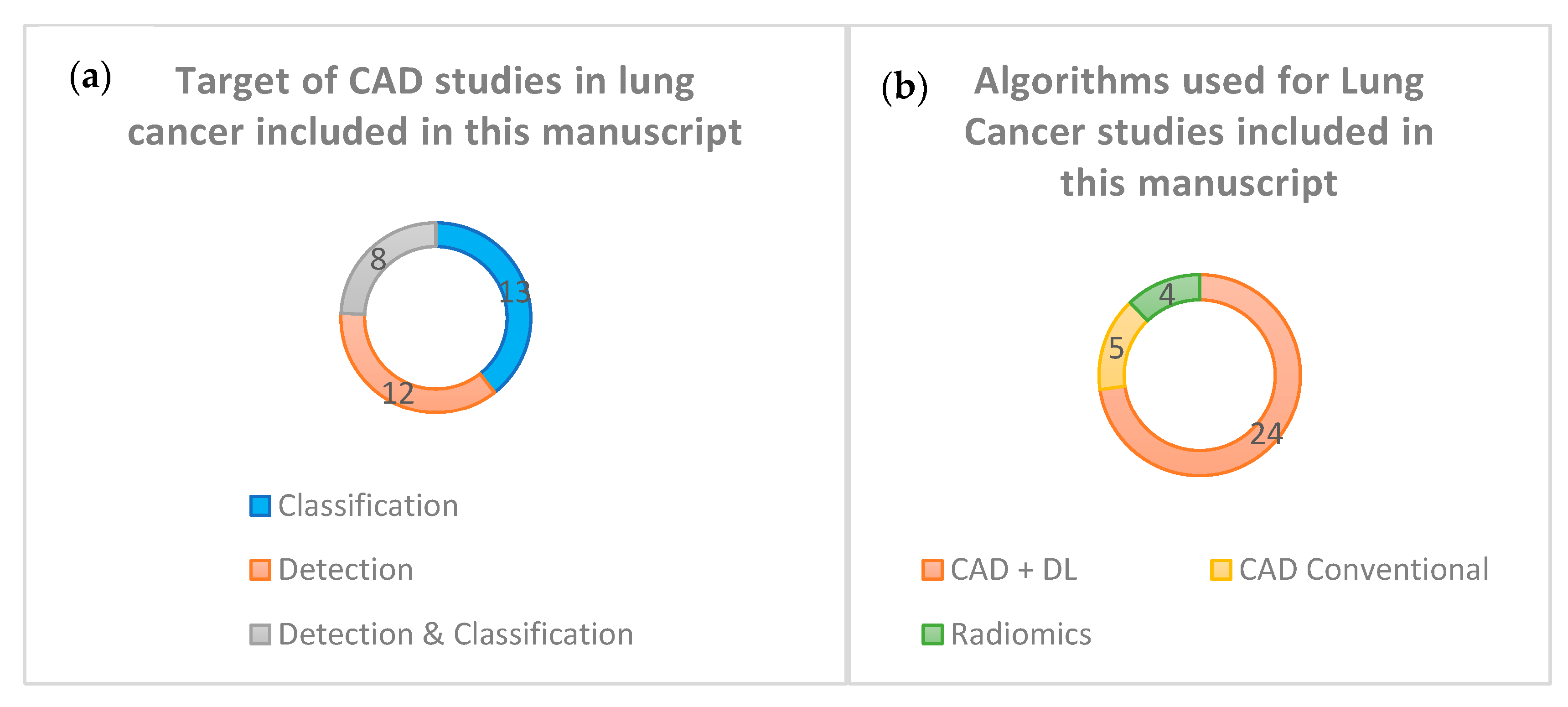
3.1. CAD in Lung Cancer Diagnosis
3.1.1. Algorithms Proposed for Nodular Detection
3.1.2. Algorithms Proposed for Nodular Classification
3.1.3. Algorithms Proposed for Detection and Nodular Classification
3.2. Radiomics and Personalized Medicine
3.2.1. Obtaining Images
3.2.2. Pre-Processing
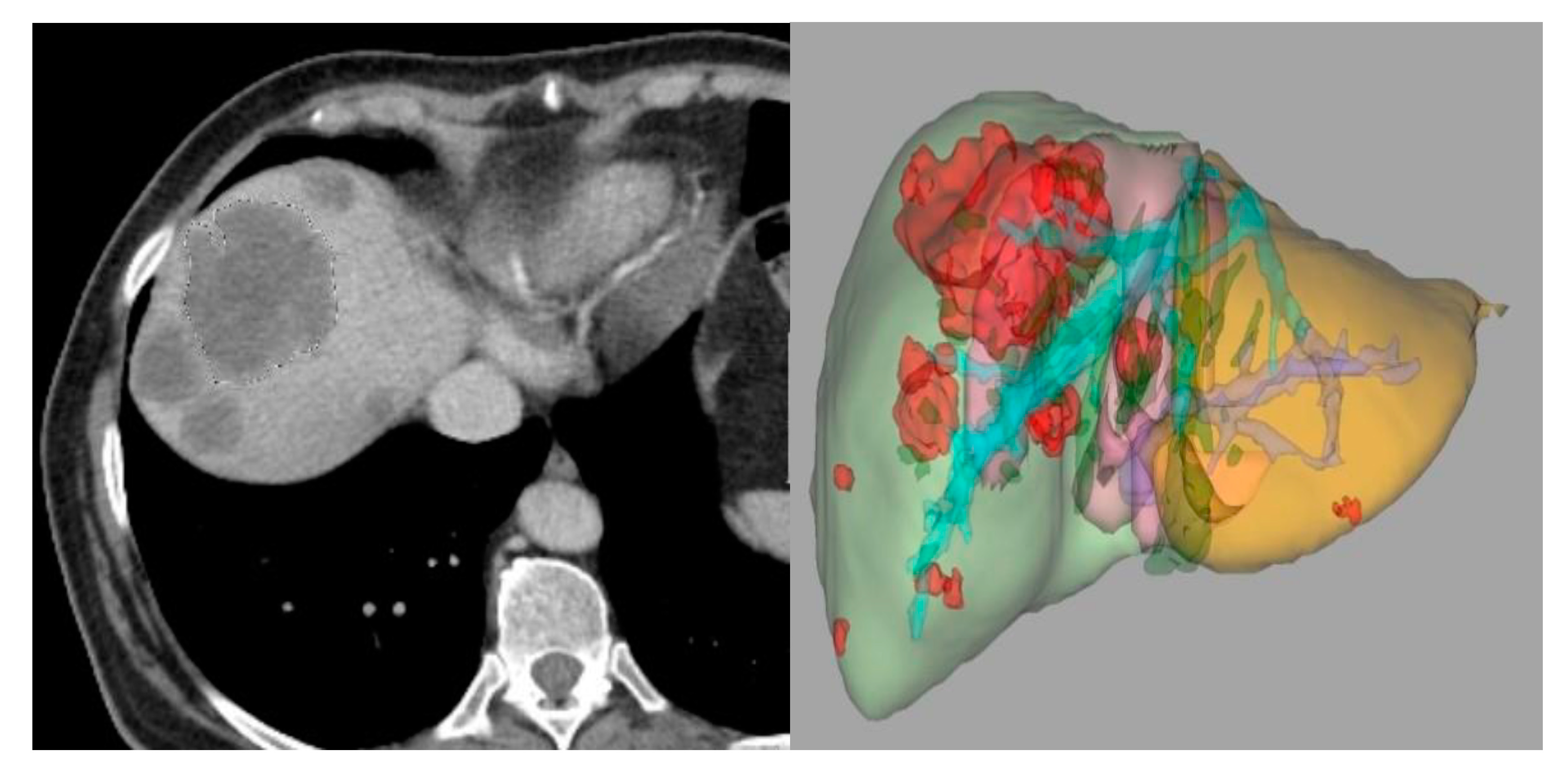
3.2.3. Segmentation
3.2.4. Feature Extraction and Classification
3.2.5. Analysis of Data
3.3. Radiomics and Radiogenomics in Colorectal Cancer
CT-Based Radiomics/Radiogenomics in Colorectal Cancer
4. Future
The Radiology Department of the Future
5. Discussion
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Souto, M. Sobre Imágenes y Máquinas: Medicina Digital del Siglo XXI; USC Ensaio: Santiago de Compostela, Spain, 2015; pp. 59–92, 128–162. [Google Scholar]
- Souto, M.; Malagari, K.S.; Tucker, D.; Tahoces, P.G.; Correa, J.; Benakis, V.S.; Roussos, C.; Strigaris, K.A.; Vidal, J.J.; Barnes, G.T.; et al. Digital radiograph of the chest: State of the art. Eur. Radiol. 1994, 4, 281–297. [Google Scholar]
- Suárez-Cuenca, J.J.; Tahoces, P.G.; Souto, M.; Lado, M.J.; Remy-Jardin, M.; Remy, J.; Vidal, J.J. Application of the iris filter for automatic detection of pulmonary nodules on computed tomography images. Comput. Biol. Med. 2009, 39, 921–933. [Google Scholar]
- Fraser, R.F.; Breatnach, E.; Barnes, G.T. Digital radiography of the chest: Clinical experience with a prototype unit. Radiology 1983, 148, 1–5. [Google Scholar]
- Barnes, G.T.; Sones, R.A.; Tesic, M.M. Digital chest radiography: Performance evaluation of a prototype unit. Radiology 1985, 154, 801–806. [Google Scholar]
- Fraser, R.G.; Sanders, C.; Barnes, G.T.; MacMahon, H.; Giger, M.L.; Doi, K.; Templeton, A.W.; Cox, G.G.; Dwyer, I.I.I.S.J.; Meritt, C.R.B.; et al. Digital imaging of the chest. Radiology 1989, 171, 297–307. [Google Scholar] [CrossRef]
- Yoshimura, H.; Giger, M.L.; Doi, K.; MacMahon, H.; Montner, S.M. Computerized scheme for the detection of pulmonary nodules. A nonlinear filtering technique. Investig. Radiol. 1992, 27, 124–129. [Google Scholar]
- Amer, H.M.; Abou-Chadi, F.E.; Kishk, S.S.; Obayya, M.I. A CAD System for the Early Detection of Lung Nodules Using Computed Tomography Scan Images. Int. J. Online Biomed. Eng. IJOE 2019, 15, 40–52. [Google Scholar]
- Gu, Y.; Lu, X.; Zhang, B.; Zhao, Y.; Yu, D.; Gao, L.; Cui, G.; Wu, L.; Zhou, T. Automatic lung nodule detection using multi-scale dot nodule-enhancement filter and weighted support vector machines in chest computed tomography. PLoS ONE 2019, 14, e0210551. [Google Scholar] [CrossRef]
- Wagner, A.-K.; Hapich, A.; Psychogios, M.N.; Teichgräber, U.; Malich, A.; Papageorgiou, I. Computer-Aided Detection of Pulmonary Nodules in Computed Tomography Using ClearReadCT. J. Med. Syst. 2019, 43, 58. [Google Scholar] [CrossRef]
- Huang, X.; Sun, W.; Tseng, T.L.B.; Li, C.; Qian, W. Fast and fully-automated detection and segmentation of pulmonary nodules in thoracic CT scans using deep convolutional neural networks. Comput. Med. Imaging Graph. 2019, 74, 25–36. [Google Scholar] [CrossRef]
- Huang, W.; Xue, Y.; Wu, Y. A CAD system for pulmonary nodule prediction based on deep three-dimensional convolutional neural networks and ensemble learning. PLoS ONE 2019, 14, e0219369. [Google Scholar] [CrossRef]
- Li, L.; Liu, Z.; Huang, H.; Lin, M.; Luo, D. Evaluating the performance of a deep learning-based computer-aided diagnosis (DL-CAD) system for detecting and characterizing lung nodules: Comparison with the performance of double reading by radiologists. Thorac. Cancer 2019, 10, 183–192. [Google Scholar] [CrossRef]
- Tang, H.; Kim, D.; Xie, X. Automated pulmonary nodule detection using 3D deep convolutional neural networks. Pattern Recognit. 2019, 85, 109–119. [Google Scholar]
- Zheng, S.; Guo, J.; Cui, X.; Veldhuis, R.N.J.; Oudkerk, M.; van Ooijen, P.M.A. Automatic Pulmonary Nodule Detection in CT Scans Using Convolutional Neural Networks Based on Maximum Intensity Projection. IEEE Trans. Med. Imaging 2020, 39, 797–805. [Google Scholar]
- Gong, L.; Jiang, S.; Yang, Z.; Zhang, G.; Wang, L. Automated pulmonary nodule detection in CT images using 3D deep squeeze-and-excitation networks. Int. J. Comput. Assist. Radiol. Surg. 2019, 14, 1969–1979. [Google Scholar] [CrossRef]
- Tan, J.; Huo, Y.; Liang, Z.; Li, L. Expert knowledge-infused deep learning for automatic lung nodule detection. J. X-ray Sci. Technol. 2019, 27, 17–35. [Google Scholar]
- Tran, G.S.; Nghiem, T.P.; Nguyen, V.T.; Luong, C.M.; Burie, J.-C. Improving Accuracy of Lung Nodule Classification Using Deep Learning with Focal Loss. J. Healthc. Eng. 2019, 2019, 5156416. [Google Scholar] [CrossRef]
- Tammemagi, M.; Ritchie, A.J.; Atkar-Khattra, S.; Dougherty, B.; Sanghera, C.; Mayo, J.R.; Yuan, R.; Manos, D.; McWilliams, A.M.; Schmidt, H.; et al. Predicting Malignancy Risk of Screen-Detected Lung Nodules-Mean Diameter or Volume. J. Thorac. Oncol. 2019, 14, 203–211. [Google Scholar] [CrossRef]
- Xie, Y.; Zhang, J.; Xia, Y. Semi-supervised adversarial model for benign-malignant lung nodule classification on chest CT. Med. Image Anal. 2019, 57, 237–248. [Google Scholar] [CrossRef]
- Zhao, X.; Qi, S.; Zhang, B.; Ma, H.; Qian, W.; Yao, Y.; Sun, J. Deep CNN models for pulmonary nodule classification: Model modification, model integration, and transfer learning. J. X-ray Sci. Technol. 2019, 27, 615–629. [Google Scholar]
- da Silva, G.; Silva, A.; de Paiva, A.; Gattass, M. Classification of malignancy of lung nodules in CT images using Convolutional Neural Network. In Anais do XVI Workshop de Informática Médica; SBC Porto Alegre: Porto Alegre, Brasil, 2016; pp. 2481–2489. [Google Scholar]
- Kailasam, S.P.; Sathik, M.M. A Novel Hybrid Feature Extraction Model for Classification on Pulmonary Nodules. Asian Pac. J. Cancer Prev. APJCP 2019, 20, 457–468. [Google Scholar]
- Wu, P.; Sun, X.; Zhao, Z.; Wang, H.; Pan, S.; Schuller, B. Classification of Lung Nodules Based on Deep Residual Networks and Migration Learning. Comput. Intell. Neurosci. 2020, 2020, 8975078. [Google Scholar] [CrossRef]
- Zhang, S.; Han, F.; Liang, Z.; Tan, J.; Cao, W.; Gao, Y.; Pomeroy, M.; Ng, K.; Hou, W. An investigation of CNN models for differentiating malignant from benign lesions using small pathologically proven datasets. Comput. Med. Imaging Graph. 2019, 77, 101645. [Google Scholar] [CrossRef]
- Liu, A.; Wang, Z.; Yang, Y.; Wang, J.; Dai, X.; Wang, L.; Lu, Y.; Xue, F. Preoperative diagnosis of malignant pulmonary nodules in lung cancer screening with a radiomics nomogram. Cancer Commun. 2020, 40, 16–24. [Google Scholar]
- Mao, L.; Chen, H.; Liang, M.; Li, K.; Gao, J.; Qin, P.; Ding, X.; Li, X.; Liu, X. Quantitative radiomic model for predicting malignancy of small solid pulmonary nodules detected by low-dose CT screening. Quant Imaging Med. Surg. 2019, 9, 263–272. [Google Scholar]
- Xu, Y.; Lu, L.; Lin, N.; Lian, W.; Yang, H.; Schwartz, L.H.; Yang, Z.H.; Zhao, B. Application of Radiomics in Predicting the Malignancy of Pulmonary Nodules in Different Sizes. AJR Am. J. Roentgenol. 2019, 213, 1213–1220. [Google Scholar]
- Zhou, Z.; Li, S.; Qin, G.; Folkert, M.; Jiang, S.; Wang, J. Multi-Objective-Based Radiomic Feature Selection for Lesion Malignancy Classification. IEEE J. Biomed. Health Inform. 2020, 24, 194–204. [Google Scholar] [CrossRef]
- Asuntha, A.; Srinivasan, A. Deep learning for lung Cancer detection and classification. Multimed. Tools Appl. 2020, 79, 7731–7762. [Google Scholar] [CrossRef]
- Bhandary, A.; Prabhu, G.A.; Rajinikanth, V.; Thanaraj, K.P.; Satapathy, S.C.; Robbins, D.E.; Shasky, C.; Zhang, Y.; Tavares, J.; Raja, N.M. Deep-learning framework to detect lung abnormality—A study with chest X-ray and lung CT scan images. Pattern Recognit Lett. 2020, 129, 271–278. [Google Scholar]
- Bansal, G.; Chamola, V.; Narang, P.; Kumar, S.; Raman, S. Deep3DSCan: Deep Residual Network And Morphological Descriptor Based Framework for Lung Cancer Classification And 3D Segmentation. IET Image Process. 2020, 14, 1217–1425. [Google Scholar] [CrossRef]
- El-Bana, S.; Al-Kabbany, A.; Sharkas, M. A Two-Stage Framework for Automated Malignant Pulmonary Nodule Detection in CT Scans. Diagnostics 2020, 10, 131. [Google Scholar] [CrossRef]
- Masood, A.; Yang, P.; Sheng, B.; Li, H.; Li, P.; Qin, J.; Lanfranchi, V.; Kim, J.; Feng, D.D. Cloud-Based Automated Clinical Decision Support System for Detection and Diagnosis of Lung Cancer in Chest CT. IEEE J Transl Eng Health Med. 2020, 8, 4300113. [Google Scholar] [CrossRef]
- Nasrullah, N.; Sang, J.; Alam, M.S.; Mateen, M.; Cai, B.; Hu, H. Automated Lung Nodule Detection and Classification Using Deep Learning Combined with Multiple Strategies. Sensors 2019, 19, 3722. [Google Scholar]
- Shanid, M.; Anitha, A. Lung cancer detection from ct images using salp-elephant optimization-based deep learning. Biomed. Eng. Appl. Basis Commun. 2020, 32, 2050001. [Google Scholar] [CrossRef]
- Zhang, C.; Sun, X.; Dang, K.; Li, K.; Guo, X.-W.; Chang, J.; Yu, Z.Q.; Huang, F.Y.; Wu, Y.S.; Liang, Z.; et al. Toward an Expert Level of Lung Cancer Detection and Classification Using a Deep Convolutional Neural Network. Oncologist 2019, 24, 1159–1165. [Google Scholar] [CrossRef]
- Gillies, R.J.; Kinahan, P.E.; Hricak, H. Radiomics: Images are more than pictures, they are data. Radiology 2016, 278, 563–577. [Google Scholar] [CrossRef]
- Bodalal, Z.; Trebeschi, S.; Nguyen-Kim, T.D.L.; Schats, W.; Beets-Tan, R. Radiogenomics: Bridging imaging and genomics. Abdom Radiol (NY) 2019, 44, 1960–1984. [Google Scholar]
- van Timmeren, J.E.; Cester, D.; Tanadini-Lang, S.; Alkadhi, H.; Baessler, B. Radiomics in medical imaging—“How-to” guide and critical reflection. Insights Imaging 2020, 11, 91. [Google Scholar]
- Badic, B.; Tixier, F.; Cheze Le Rest, C.; Hatt, M.; Visvikis, D. Radiogenomics in Colorectal Cancer. Cancers 2021, 13, 973. [Google Scholar] [CrossRef]
- Zwanenburg, A.; Vallières, M.; Abdalah, M.A.; Aerts, H.J.W.L.; Andrearczyk, V.; Apte, A.; Ashrafinia, S.; Bakas, S.; Beukinga, R.J.; Boellaard, R.; et al. The Image Biomarker Standardization Initiative: Standardized Quantitative Radiomics for High-Throughput Image-based Phenotyping. Radiology 2020, 295, 328–338. [Google Scholar]
- Xue, T.; Peng, H.; Chen, Q.; Li, M.; Duan, S.; Feng, F. A CT-Based Radiomics Nomogram in Predicting the Postoperative Prognosis of Colorectal Cancer: A Two-center Study. Acad. Radiol. 2022, 29, 1647–1660. [Google Scholar] [CrossRef]
- Huang, Y.; He, L.; Li, Z.; Chen, X.; Han, C.; Zhao, K.; Zhang, Y.; Qu, J.; Mao, Y.; Liang, C.; et al. Coupling radiomics analysis of CT image with diversification of tumor ecosystem: A new insight to overall survival in stage I-III colorectal cancer. Chin. J. Cancer Res. 2022, 34, 40–52. [Google Scholar] [CrossRef]
- Dercle, L.; Zhao, B.; Gönen, M.; Moskowitz, C.S.; Connors, D.E.; Yang, H.; Lu, L.; Reidy-Lagunes, D.; Fojo, T.; Karovic, S.; et al. An imaging signature to predict outcome in metastatic colorectal cancer using routine computed tomography scans. Eur. J. Cancer 2022, 161, 138–147. [Google Scholar] [CrossRef]
- Badic, B.; Desseroit, M.C.; Hatt, M.; Visvikis, D. Potential Complementary Value of Noncontrast and Contrast Enhanced CT Radiomics in Colorectal Cancers. Acad. Radiol. 2019, 26, 469–479. [Google Scholar] [CrossRef]
- Mühlberg, A.; Holch, J.W.; Heinemann, V.; Huber, T.; Moltz, J.; Maurus, S.; Jäger, N.; Liu, L.; Froelich, M.F.; Katzmann, A.; et al. The relevance of CT-based geometric and radiomics analysis of whole liver tumor burden to predict survival of patients with metastatic colorectal cancer. Eur. Radiol. 2021, 31, 834–846. [Google Scholar]
- Li, M.; Zhu, Y.Z.; Zhang, Y.C.; Yue, Y.F.; Yu, H.P.; Song, B. Radiomics of rectal cancer for predicting distant metastasis and overall survival. World J. Gastroenterol. 2020, 26, 5008–5021. [Google Scholar]
- Zhao, Y.; Yang, J.; Luo, M.; Yang, Y.; Guo, X.; Zhang, T.; Hao, J.; Yao, Y.; Ma, X. Contrast-Enhanced CT-based Textural Parameters as Potential Prognostic Factors of Survival for Colorectal Cancer Patients Receiving Targeted Therapy. Mol. Imaging Biol. 2021, 23, 427–435. [Google Scholar] [CrossRef]
- Ye, S.; Han, Y.; Pan, X.; Niu, K.; Liao, Y.; Meng, X. Association of CT-Based Delta Radiomics Biomarker With Progression-Free Survival in Patients With Colorectal Liver Metastases Undergo Chemotherapy. Front. Oncol. 2022, 12, 843991. [Google Scholar] [CrossRef]
- Rabe, E.; Cioni, D.; Baglietto, L.; Fornili, M.; Gabelloni, M.; Neri, E. Can the computed tomography texture analysis of colorectal liver metastases predict the response to first-line cytotoxic chemotherapy? World J. Hepatol. 2022, 14, 244–259. [Google Scholar]
- Cai, D.; Duan, X.; Wang, W.; Huang, Z.P.; Zhu, Q.; Zhong, M.E.; Lv, M.Y.; Li, C.H.; Kou, W.B.; Wu, X.J.; et al. A Metabolism-Related Radiomics Signature for Predicting the Prognosis of Colorectal Cancer. Front. Mol. Biosci. 2020, 7, 613918. [Google Scholar] [CrossRef]
- Defeudis, A.; Cefaloni, L.; Giannetto, G.; Cappello, G.; Rizzetto, F.; Panic, J.; Barra, D.; Nicoletti, G.; Mazzetti, S.; Vanzulli, A.; et al. Comparison of radiomics approaches to predict resistance to 1st line chemotherapy in liver metastatic colorectal cancer. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2021, 2021, 3305–3308. [Google Scholar]
- Lutsyk, M.; Gourevich, K.; Keidar, Z. Complete Pathologic Response Prediction by Radiomics Wavelets Features of Unenhanced CT Simulation Images in Locally Advanced Rectal Cancer Patients after Neoadjuvant Chemoradiation. ISR Med. Assoc. J. 2021, 23, 805–810. [Google Scholar]
- Bibault, J.E.; Giraud, P.; Housset, M.; Durdux, C.; Taieb, J.; Berger, A.; Coriat, R.; Chaussade, S.; Dousset, B.; Nordlinger, B.; et al. Deep Learning and Radiomics predict complete response after neo-adjuvant chemoradiation for locally advanced rectal cancer. Sci. Rep. 2018, 8, 12611. [Google Scholar] [CrossRef]
- Zhang, Z.; Yi, X.; Pei, Q.; Fu, Y.; Li, B.; Liu, H.; Han, Z.; Chen, C.; Pang, P.; Lin, H.; et al. CT radiomics identifying non-responders to neoadjuvant chemoradiotherapy among patients with locally advanced rectal cancer. Cancer Med. 2022. [Google Scholar] [CrossRef]
- Giannini, V.; Pusceddu, L.; Defeudis, A.; Nicoletti, G.; Cappello, G.; Mazzetti, S.; Sartore-Bianchi, A.; Siena, S.; Vanzulli, A.; Rizzetto, F.; et al. Delta-Radiomics Predicts Response to First-Line Oxaliplatin-Based Chemotherapy in Colorectal Cancer Patients with Liver Metastases. Cancers 2022, 14, 241. [Google Scholar] [CrossRef]
- Vandendorpe, B.; Durot, C.; Lebellec, L.; Le Deley, M.C.; Sylla, D.; Bimbai, A.M.; Amroun, K.; Ramiandrisoa, F.; Cordoba, A.; Mirabel, X.; et al. Prognostic value of the texture analysis parameters of the initial computed tomographic scan for response to neoadjuvant chemoradiation therapy in patients with locally advanced rectal cancer. Radiother. Oncol. 2019, 135, 153–160. [Google Scholar] [CrossRef]
- Zhuang, Z.; Liu, Z.; Li, J.; Wang, X.; Xie, P.; Xiong, F.; Hu, J.; Meng, X.; Huang, M.; Deng, Y.; et al. Radiomic signature of the FOWARC trial predicts pathological response to neoadjuvant treatment in rectal cancer. J. Transl. Med. 2021, 19, 256. [Google Scholar]
- Wang, F.; Tan, B.F.; Poh, S.S.; Siow, T.R.; Lim, F.L.W.T.; Yip, C.S.P.; Wang, M.L.C.; Nei, W.; Tan, H.Q. Predicting outcomes for locally advanced rectal cancer treated with neoadjuvant chemoradiation with CT-based radiomics. Sci. Rep. 2022, 12, 6167. [Google Scholar]
- Dercle, L.; Lu, L.; Schwartz, L.H.; Qian, M.; Tejpar, S.; Eggleton, P.; Zhao, B.; Peissevaux, H. Radiomics Response Signature for Identification of Metastatic Colorectal Cancer Sensitive to Therapies Targeting EGFR Pathway. J. Natl. Cancer Inst. 2020, 112, 902–912. [Google Scholar]
- Yuan, Z.; Frazer, M.; Zhang, G.G.; Latifi, K.; Moros, E.G.; Feygelman, V.; Felder, S.; Sanchez, J.; Dessureault, S.; Imanirad, I.; et al. CT-based radiomic features to predict pathological response in rectal cancer: A retrospective cohort study. J. Med. Imaging Radiat. Oncol. 2020, 64, 444–449. [Google Scholar]
- Bonomo, P.; Socarras Fernandez, J.; Thorwarth, D.; Casati, M.; Livi, L.; Zips, D.; Gani, C. Simulation CT-based radiomics for prediction of response after neoadjuvant chemo-radiotherapy in patients with locally advanced rectal cancer. Radiat. Oncol. 2022, 17, 84. [Google Scholar]
- Fan, S.; Cui, X.; Liu, C.; Li, X.; Zheng, L.; Song, Q.; Qi, J.; Ma, W.; Ye, Z. CT-Based Radiomics Signature: A Potential Biomarker for Predicting Postoperative Recurrence Risk in Stage II Colorectal Cancer. Front. Oncol. 2021, 11, 644933. [Google Scholar]
- Badic, B.; Da-Ano, R.; Poirot, K.; Jaouen, V.; Magnin, B.; Gagnière, J.; Pezet, D.; Hatt, M.; Visvikis, D. Prediction of recurrence after surgery in colorectal cancer patients using radiomics from diagnostic contrast-enhanced computed tomography: A two-center study. Eur. Radiol. 2022, 32, 405–414. [Google Scholar] [CrossRef]
- Hong, E.K.; Bodalal, Z.; Landolfi, F.; Bogveradze, N.; Bos, P.; Park, S.J.; Min-Lee, J.; Beets-Tan, R. Identifying high-risk colon cancer on CT an a radiomics signature improve radiologist’s performance for T staging? Abdom Radiol. (NY) 2022, 47, 2739–2746. [Google Scholar]
- Ge, Y.X.; Li, J.; Zhang, J.Q.; Duan, S.F.; Liu, Y.K.; Hu, S.D. Radiomics analysis of multicenter CT images for discriminating mucinous adenocarcinoma from nomucinous adenocarcinoma in rectal cancer and comparison with conventional CT values. J Xray Sci. Technol. 2020, 28, 285–297. [Google Scholar] [CrossRef]
- Hu, P.; Wang, J.; Zhong, H.; Zhou, Z.; Shen, L.; Hu, W.; Zhang, Z. Reproducibility with repeat CT in radiomics study for rectal cancer. Oncotarget 2016, 7, 71440–71446. [Google Scholar] [CrossRef]
- Dou, Y.; Liu, Y.; Kong, X.; Yang, S. T staging with functional and radiomics parameters of computed tomography in colorectal cancer patients. Medicine (Baltimore) 2022, 101, e29244. [Google Scholar]
- Liu, Q.; Li, J.; Xu, L.; Wang, J.; Zeng, Z.; Fu, J.; Huang, X.; Chu, Y.; Wang, J.; Zhang, H.Y.; et al. Individualized Prediction of Colorectal Cancer Metastasis Using a Radiogenomics Approach. Front. Oncol. 2021, 11, 620945. [Google Scholar]
- Huang, X.; Cheng, Z.; Huang, Y.; Liang, C.; He, L.; Ma, Z.; Chen, X.; Wu, X.; Li, Y.; Liang, C.; et al. CT-based Radiomics Signature to Discriminate High-grade From Low-grade Colorectal Adenocarcinoma. Acad. Radiol. 2018, 25, 1285–1297. [Google Scholar]
- Liang, C.; Huang, Y.; He, L.; Chen, X.; Ma, Z.; Dong, D.; Tian, J.; Liang, C.; Liu, Z. The development and validation of a CT-based radiomics signature for the preoperative discrimination of stage I-II and stage III-IV colorectal cancer. Oncotarget 2016, 7, 31401–31412. [Google Scholar]
- Badic, B.; Hatt, M.; Durand, S.; Jossic-Corcos, C.L.; Simon, B.; Visvikis, D.; Corcos, L. Radiogenomics-based cancer prognosis in colorectal cancer. Sci. Rep. 2019, 9, 9743. [Google Scholar] [CrossRef]
- Chu, Y.; Li, J.; Zeng, Z.; Huang, B.; Zhao, J.; Liu, Q.; Wu, H.; Fu, J.; Zhang, Y.; Cai, J.; et al. A Novel Model Based on CXCL8-Derived Radiomics for Prognosis Prediction in Colorectal Cancer. Front. Oncol. 2020, 10, 575422. [Google Scholar]
- Huang, Y.C.; Tsai, Y.S.; Li, C.I.; Chan, R.H.; Yeh, Y.M.; Chen, P.C.; Shen, M.R.; Lin, P.C. Adjusted CT Image-Based Radiomic Features Combined with Immune Genomic Expression Achieve Accurate Prognostic Classification and Identification of Therapeutic Targets in Stage III Colorectal Cancer. Cancers 2022, 14, 1895. [Google Scholar] [CrossRef]
- Hoshino, I.; Yokota, H.; Iwatate, Y.; Mori, Y.; Kuwayama, N.; Ishige, F.; Itami, M.; Uno, T.; Nakamura, Y.; Tatsumi, Y.; et al. Prediction of the differences in tumor mutation burden between primary and metastatic lesions by radiogenomics. Cancer Sci. 2022, 113, 229–239. [Google Scholar] [CrossRef]
- Yang, L.; Dong, D.; Fang, M.; Zhu, Y.; Zang, Y.; Liu, Z.; Zhang, H.; Ying, J.; Zhao, X.; Tian, J. Can CT-based radiomics signature predict KRAS/NRAS/BRAF mutations in colorectal cancer? Eur. Radiol. 2018, 28, 2058–2067. [Google Scholar]
- Shi, R.; Chen, W.; Yang, B.; Qu, J.; Cheng, Y.; Zhu, Z.; Gao, Y.; Wang, Q.; Liu, Y.; Li, Z.; et al. Prediction of KRAS, NRAS and BRAF status in colorectal cancer patients with liver metastasis using a deep artificial neural network based on radiomics and semantic features. Am. J. Cancer Res. 2020, 10, 4513–4526. [Google Scholar]
- González-Castro, V.; Cernadas, E.; Huelga, E.; Fernández-Delgado, M.; Porto, J.; Antunez, J.R.; Souto-Bayarri, M. CT Radiomics in Colorectal Cancer: Detection of KRAS Mutation Using Texture Analysis and Machine Learning. Appl. Sci. 2020, 10, 6214. [Google Scholar] [CrossRef]
- Wu, X.; Li, Y.; Chen, X.; Huang, Y.; He, L.; Zhao, K.; Huang, X.; Zhang, W.; Huang, Y.; Li, Y.; et al. Deep Learning Features Improve the Performance of a Radiomics Signature for Predicting KRAS Status in Patients with Colorectal Cancer. Acad. Radiol. 2020, 27, e254–e262. [Google Scholar]
- He, K.; Liu, X.; Li, M.; Li, X.; Yang, H.; Zhang, H. Noninvasive KRAS mutation estimation in colorectal cancer using a deep learning method based on CT imaging. BMC Med. Imaging 2020, 20, 59. [Google Scholar] [CrossRef]
- Hu, J.; Xia, X.; Wang, P.; Peng, Y.; Liu, J.; Xie, X.; Liao, Y.; Wan, Q.; Li, X. Predicting Kirsten Rat Sarcoma Virus Gene Mutation Status in Patients With Colorectal Cancer by Radiomics Models Based on Multiphasic CT. Front. Oncol. 2022, 12, 848798. [Google Scholar]
- Jang, B.S.; Song, C.; Kang, S.B.; Kim, J.S. Radiogenomic and Deep Learning Network Approaches to Predict KRAS Mutation from Radiotherapy Plan CT. Anticancer Res. 2021, 41, 3969–3976. [Google Scholar] [CrossRef]
- Xue, T.; Peng, H.; Chen, Q.; Li, M.; Duan, S.; Feng, F. Preoperative prediction of KRAS mutation status in colorectal cancer using a CT-based radiomics nomogram. Br. J. Radiol. 2022, 95, 20211014. [Google Scholar]
- Xue, T.; Peng, H.; Chen, Q.; Li, M.; Duan, S.; Feng, F. Preoperative Prediction of BRAF Mutation Status in Colorectal Cancer Using a Clinical-radiomics Model. Acad. Radiol. 2022, 29, 1298–1307. [Google Scholar]
- Negreros-Osuna, A.A.; Parakh, A.; Corcoran, R.B.; Pourvaziri, A.; Kambadakone, A.; Ryan, D.P.; Sahani, D.V. Radiomics Texture Features in Advanced Colorectal Cancer: Correlation with BRAF Mutation and 5-year Overall Survival. Radiol. Imaging Cancer 2020, 2, e190084. [Google Scholar] [CrossRef]
- Fan, S.; Li, X.; Cui, X.; Zheng, L.; Ren, X.; Ma, W.; Ye, Z. Computed Tomography-Based Radiomic Features Could Potentially Predict Microsatellite Instability Status in Stage II Colorectal Cancer: A Preliminary Study. Acad. Radiol. 2019, 26, 1633–1640. [Google Scholar]
- Li, Z.; Zhong, Q.; Zhang, L.; Wang, M.; Xiao, W.; Cui, F.; Yu, F.; Huang, C.; Feng, Z. Computed Tomography-Based Radiomics Model to Preoperatively Predict Microsatellite Instability Status in Colorectal Cancer: A Multicenter Study. Front. Oncol. 2021, 11, 666786. [Google Scholar] [CrossRef]
- Ying, M.; Pan, J.; Lu, G.; Zhou, S.; Fu, J.; Wang, Q.; Wang, L.; Hu, B.; Wei, Y.; Shen, J. Development and validation of a radiomics-based nomogram for the preoperative prediction of microsatellite instability in colorectal cancer. BMC Cancer 2022, 22, 524. [Google Scholar] [CrossRef]
- Chen, X.; He, L.; Li, Q.; Liu, L.; Li, S.; Zhang, Y.; Liu, Z.; Huang, Y.; Mao, Y.; Chen, X. Non-invasive prediction of microsatellite instability in colorectal cancer by a genetic algorithm-enhanced artificial neural network-based CT radiomics signature. Eur Radiol. 2022, 33, 11–22. [Google Scholar] [CrossRef]
- Pei, Q.; Yi, X.; Chen, C.; Pang, P.; Fu, Y.; Lei, G.; Chen, C.; Tan, F.; Gong, G.; Li, Q.; et al. Pre-treatment CT-based radiomics nomogram for predicting microsatellite instability status in colorectal cancer. Eur Radiol. 2022, 32, 714–724. [Google Scholar]
- Cao, Y.; Zhang, G.; Zhang, J.; Yang, Y.; Ren, J.; Yan, X.; Wang, Z.; Zhao, Z.; Huang, X.; Bao, H.; et al. Predicting Microsatellite Instability Status in Colorectal Cancer Based on Triphasic Enhanced Computed Tomography Radiomics Signatures: A Multicenter Study. Front. Oncol. 2021, 11, 687771. [Google Scholar] [CrossRef]
- Wu, J.; Zhang, Q.; Zhao, Y.; Liu, Y.; Chen, A.; Li, X.; Wu, T.; Li, J.; Guo, Y.; Liu, A. Radiomics Analysis of Iodine-Based Material Decomposition Images With Dual-Energy Computed Tomography Imaging for Preoperatively Predicting Microsatellite Instability Status in Colorectal Cancer. Front. Oncol. 2019, 9, 1250. [Google Scholar] [CrossRef]
- Golia Pernicka, J.S.; Gagniere, J.; Chakraborty, J.; Yamashita, R.; Nardo, L.; Creasy, J.M.; Petkovska, I.; Do, R.R.K.; Bates, D.D.B.; Paroder, V.; et al. Radiomics-based prediction of microsatellite instability in colorectal cancer at initial computed tomography evaluation. Abdom Radiol. (NY) 2019, 44, 3755–3763. [Google Scholar]
- Liu, Y.; Dou, Y.; Lu, F.; Liu, L. A study of radiomics parameters from dual-energy computed tomography images for lymph node metastasis evaluation in colorectal mucinous adenocarcinoma. Medicine (Baltimore) 2020, 99, e19251. [Google Scholar]
- Cheng, Y.; Yu, Q.; Meng, W.; Jiang, W. Clinico-Radiologic Nomogram Using Multiphase CT to Predict Lymph Node Metastasis in Colon Cancer. Mol Imaging Biol. 2022, 24, 798–806. [Google Scholar]
- Huang, Y.Q.; Liang, C.H.; He, L.; Tian, J.; Liang, C.S.; Chen, X.; Ma, Z.L.; Liu, Z.Y. Development and Validation of a Radiomics Nomogram for Preoperative Prediction of Lymph Node Metastasis in Colorectal Cancer. J. Clin. Oncol. 2016, 34, 2157–2164. [Google Scholar]
- Eresen, A.; Li, Y.; Yang, J.; Shangguan, J.; Velichko, Y.; Yaghmai, V.; Benson, A.B., 3rd; Zhang, Z. Preoperative assessment of lymph node metastasis in Colon Cancer patients using machine learning: A pilot study. Cancer Imaging 2020, 20, 30. [Google Scholar] [CrossRef]
- Li, M.; Jin, Y.; Rui, J.; Zhang, Y.; Zhao, Y.; Huang, C.; Liu, S.; Song, B. Computed tomography-based radiomics for predicting lymphovascular invasion in rectal cancer. Eur. J. Radiol. 2022, 146, 110065. [Google Scholar]
- Ge, Y.X.; Xu, W.B.; Wang, Z.; Zhang, J.Q.; Zhou, X.Y.; Duan, S.F.; Hu, S.D.; Fei, B.J. Prognostic value of CT radiomics in evaluating lymphovascular invasion in rectal cancer: Diagnostic performance based on different volumes of interest. J. X-ray Sci. Technol. 2021, 29, 663–674. [Google Scholar] [CrossRef]
- Liu, C.; Meng, Q.; Zeng, Q.; Chen, H.; Shen, Y.; Li, B.; Cen, R.; Huang, J.; Li, G.; Liao, Y.; et al. An Exploratory Study on the Stable Radiomics Features of Metastatic Small Pulmonary Nodules in Colorectal Cancer Patients. Front Oncol. 2021, 11, 661763. [Google Scholar] [CrossRef]
- Markich, R.; Palussière, J.; Catena, V.; Cazayus, M.; Fonck, M.; Bechade, D.; Buy, X.; Crombé, A. Radiomics complements clinical, radiological, and technical features to assess local control of colorectal cancer lung metastases treated with radiofrequency ablation. Eur Radiol. 2021, 31, 8302–8314. [Google Scholar]
- Giannini, V.; Defeudis, A.; Rosati, S.; Cappello, G.; Mazzetti, S.; Panic, J.; Regge, D.; Balestra, G. An innovative radiomics approach to predict response to chemotherapy of liver metastases based on CT images. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2020, 2020, 1339–1342. [Google Scholar]
- Taghavi, M.; Staal, F.C.; Simões, R.; Hong, E.K.; Lambregts, D.M.; van der Heide, U.A.; Beets-Tan, R.G.; Maas, M. CT radiomics models are unable to predict new liver metastasis after successful thermal ablation of colorectal liver metastases. Acta Radiol. 2021, 2841851211060437. [Google Scholar]
- Staal, F.C.R.; Taghavi, M.; van der Reijd, D.J.; Gomez, F.M.; Imani, F.; Klompenhouwer, E.G.; Meek, D.; Roberti, S.; de Boer, M.; Lambregts, D.M.J.; et al. Predicting local tumour progression after ablation for colorectal liver metastases: CT-based radiomics of the ablation zone. Eur. J. Radiol. 2021, 141, 109773. [Google Scholar] [CrossRef]
- Liu, P.; Zhu, H.; Zhu, H.; Zhang, X.; Feng, A.; Zhu, X.; Sun, Y. Predicting Survival for Hepatic Arterial Infusion Chemotherapy of Unresectable Colorectal Liver Metastases: Radiomics Analysis of Pretreatment Computed Tomography. J. Transl. Int. Med. 2022, 10, 56–64. [Google Scholar]
- Giannini, V.; Rosati, S.; Defeudis, A.; Balestra, G.; Vassallo, L.; Cappello, G.; Mazzetti, S.; De Mattia, C.; Rizzetto, F.; Torresin, A.; et al. Radiomics predicts response of individual HER2-amplified colorectal cancer liver metastases in patients treated with HER2-targeted therapy. Int J Cancer 2020, 147, 3215–3223. [Google Scholar]
- Creasy, J.M.; Cunanan, K.M.; Chakraborty, J.; McAuliffe, J.C.; Chou, J.; Gonen, M.; Kingham, V.S.; Weiser, M.R.; Balachandran, V.P.; Drebin, J.A.; et al. Differences in Liver Parenchyma are Measurable with CT Radiomics at Initial Colon Resection in Patients that Develop Hepatic Metastases from Stage II/III Colon Cancer. Ann. Surg. Oncol. 2021, 28, 1982–1989. [Google Scholar] [CrossRef]
- Taghavi, M.; Staal, F.; Gomez Munoz, F.; Imani, F.; Meek, D.B.; Simões, R.; Klompenhouwer, L.G.; van der Heide, U.A.; Beets-Tan, R.G.H.; Maas, M. CT-Based Radiomics Analysis Before Thermal Ablation to Predict Local Tumor Progression for Colorectal Liver Metastases. Cardiovasc. Intervent Radiol. 2021, 44, 913–920. [Google Scholar] [CrossRef]
- Starmans, M.P.A.; Buisman, F.E.; Renckens, M.; Willemssen, F.E.J.A.; van der Voort, S.R.; Groot Koerkamp, B.; Grünhagen, D.J.; Niessen, W.J.; Vermeulen, P.B.; Verhoef, C.; et al. Distinguishing pure histopathological growth patterns of colorectal liver metastases on CT using deep learning and radiomics: A pilot study. Clin Exp Metastasis 2021, 38, 483–494. [Google Scholar]
- Cheng, J.; Wei, J.; Tong, T.; Sheng, W.; Zhang, Y.; Han, Y.; Gu, D.; Hong, N.; Ye, Y.; Tian, J.; et al. Prediction of Histopathologic Growth Patterns of Colorectal Liver Metastases with a Noninvasive Imaging Method. Ann. Surg. Oncol. 2019, 26, 4587–4598. [Google Scholar] [CrossRef]
- Tharmaseelan, H.; Hertel, A.; Tollens, F.; Rink, J.; Woźnicki, P.; Haselmann, V.; Ayx, I.; Nöremberg, D.; Schoenberg, S.O.; Froelich, M.F. Identification of CT Imaging Phenotypes of Colorectal Liver Metastases from Radiomics Signatures-Towards Assessment of Interlesional Tumor Heterogeneity. Cancers 2022, 14, 1646. [Google Scholar] [CrossRef]
- Devoto, L.; Ganeshan, B.; Keller, D.; Groves, A.; Endozo, R.; Arulampalam, T.; Chand, M. Using texture analysis in the development of a potential radiomic signature for early identification of hepatic metastasis in colorectal cancer. Eur. J. Radiol. Open 2022, 9, 100415. [Google Scholar]
- Dohan, A.; Gallix, B.; Guiu, B.; Le Malicot, K.; Reinhold, C.; Soyer, P.; Bennouna, J.; Ghiringhelli, F.; Barbier, E.; Boige, V.; et al. Early evaluation using a radiomic signature of unresectable hepatic metastases to predict outcome in patients with colorectal cancer treated with FOLFIRI and bevacizumab. Gut 2020, 69, 531–539. [Google Scholar]
- Taghavi, M.; Trebeschi, S.; Simões, R.; Meek, D.B.; Beckers, R.C.J.; Lambregts, D.M.J.; Verhoef, C.; Houwers, J.B.; van der Heide, U.A.; Beets-Tan, R.G.H.; et al. Machine learning-based analysis of CT radiomics model for prediction of colorectal metachronous liver metastases. Abdom Radiol (NY) 2021, 46, 249–256. [Google Scholar] [CrossRef]
- Li, Y.; Gong, J.; Shen, X.; Li, M.; Zhang, H.; Feng, F.; Tong, T. Assessment of Primary Colorectal Cancer CT Radiomics to Predict Metachronous Liver Metastasis. Front. Oncol. 2022, 12, 861892. [Google Scholar] [CrossRef]
- Li, M.; Li, X.; Guo, Y.; Miao, Z.; Liu, X.; Guo, S.; Zhang, H. Development and assessment of an individualized nomogram to predict colorectal cancer liver metastases. Quant Imaging Med. Surg. 2020, 10, 397–414. [Google Scholar] [CrossRef]
- Rocca, A.; Brunese, M.C.; Santone, A.; Avella, P.; Bianco, P.; Scacchi, A.; Scaglione, M.; Bellifemine, F.; Danzi, R.; Varriano, G.; et al. Early Diagnosis of Liver Metastases from Colorectal Cancer through CT Radiomics and Formal Methods: A Pilot Study. J. Clin. Med. 2021, 11, 31. [Google Scholar]
- Lee, S.; Choe, E.K.; Kim, S.Y.; Kim, H.S.; Park, K.J.; Kim, D. Liver imaging features by convolutional neural network to predict the metachronous liver metastasis in stage I-III colorectal cancer patients based on preoperative abdominal CT scan. BMC Bioinform. 2020, 21 (Suppl. S13), 382. [Google Scholar]
- Huang, Y.; He, L.; Dong, D.; Yang, C.; Liang, C.; Chen, X.; Ma, Z.; Huang, X.; Yao, S.; Liang, C.; et al. Individualized prediction of perineural invasion in colorectal cancer: Development and validation of a radiomics prediction model. Chin. J. Cancer Res. 2018, 30, 40–50. [Google Scholar] [CrossRef]
- Li, Y.; Eresen, A.; Shangguan, J.; Yang, J.; Benson, A.B.; Yaghmai, V.; Zhang, Z. Preoperative prediction of perineural invasion and KRAS mutation in colon cancer using machine learning. J. Cancer Res. Clin. Oncol. 2020, 146, 3165–3174. [Google Scholar] [CrossRef]
- Li, M.; Jin, Y.M.; Zhang, Y.C.; Zhao, Y.L.; Huang, C.C.; Liu, S.M.; Song, B. Radiomics for predicting perineural invasion status in rectal cancer. World J. Gastroenterol. 2021, 27, 5610–5621. [Google Scholar]
- Li, M.; Sun, K.; Dai, W.; Xiang, W.; Zhang, Z.; Zhang, R.; Wang, R.; Li, Q.; Mo, S.; Han, L.; et al. Preoperative prediction of peritoneal metastasis in colorectal cancer using a clinical-radiomics model. Eur. J. Radiol. 2020, 132, 109326. [Google Scholar] [CrossRef]
- Fraser, R.G.; Barnes, G.T.; Hickey, N.; Luna, R.; Katzenstein, A.; Alexander, B.; McElvein, R.; Zorn, G.; Sabbagh, E.; Robinson, C.A., Jr. Potential value of digital radiography: Preliminary observations on the use of dual-energy subtraction in the evaluation of pulmonary nodules. Chest 1986, 89, 249S–252S. [Google Scholar]
- Niklason, L.T.; Hickey, N.M.; Chakraborty, D.P.; Sabbagh, E.A.; Yester, M.V.; Fraser, R.G.; Barnes, G.T. Simulated pulmonary nodules: Detection with dual-energy digital vs conventional radiography. Radiology 1986, 160, 589–593. [Google Scholar] [CrossRef]





| CAD Model | Method | Function | Data Base | Nº Scanners | Nº Nodules | Sensitivity | Specificity | FPs/Scan | Accuracy | AUC | Year |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Amer HM et al. [8] | CAD conventional | Detection | ELCAP | 40 | NA | 100% | 99.20% | NA | 99.60% | NA | 2019 |
| Gu Y. et al. [9] | CAD | Detection | LIDC-IDRI | 154 | 204 | 87.81% | NA | 1.057 | NA | NA | 2019 |
| Wagner A-K et al. [10] | CAD conventional | Detection | Private | 100 | 106 | 87.00% | NA | NA | NA | NA | 2019 |
| Huang X. et al. [11] | CAD + DL + CNN | Detection | LUNA16 | 888 | NA | NA | NA | 1 4 | 94.60% | NA | 2019 |
| Huang W. et al. [12] | CAD + DL + CNN | Detection | LUNA16; Ali Tianch | NA | 1795 | 81.70% 85.10% 88.30% 90.70% | NA | 0.125 0.25 1 4 | 91.40% | NA | 2019 |
| Li L et al. [13] | CAD + DL + CNN | Detection | Private | 346 | 812 | 86.20% | NA | 1.53 | NA | NA | 2019 |
| Tan H. et al. [14] | CAD + DL + CNN | Detection | LUNA16 | 888 | 1186 | 86.4% 85.2% | NA | 4 1 | NA | 2019 | |
| Zheng S et al. [15] | CAD + DL + CNN | Detection | LUNA16 | 888 | 1186 | 92.70% 94.20% | NA | 1 2 | NA | NA | 2020 |
| Gong L et al. [16] | CAD + DL + CNN | Detection | LUNA16 | 888 | 1186 | 93.60% 95.70% | NA | 1 4 | NA | NA | 2019 |
| Tan J et al. [17] | CAD + DL + CNN | Detection | LIDC-IDRI | 208 | NA | 80.10% 94.0% | NA | 1.89 4.01 | NA | NA | 2019 |
| Tran G. et al. [18] | CAD + DL + CNN | Classification | LUNA16 | 888 | 1186 | 96.00% | 97.30% | NA | 97.20% | 0.9820 | 2019 |
| Tammemagi M et al [19] | CAD conventional (volume) | Classification | NSLT | 3680 | 6009 | 75.00% | 75.00% | NA | NA | 0.8210 | 2019 |
| Tammemagi M et al [19] | CAD conventional (diameter) | Classification | NSLT | 3680 | 6009 | 75.00% | 75.00% | NA | NA | 0.810 | 2019 |
| Xie Y. et al. [20] | CAD + DL + CNN | Classification | LIDC-IDRI | 1018 | 1945 | 84.94% | 96.59% | NA | 92.53% | 0.9581 | 2019 |
| Zhao X. et al. [21] | CAD + DL + CNN | Classification | LIDC-IDRI | 1018 | 368 | 91.00% | NA | NA | 88.00% | 0.94 | 2019 |
| Da Silva et al. [22] | CAD + DL + CNN | Classification | LIDC-IDRI | 833 | 1296 | 79.40% | 83.80% | NA | 83.30% | NA | 2020 |
| Kailasam SP et al [23] | CAD + DL + CNN | Classification | LIDC-IDRI | NA | 467 | NA | NA | NA | 95.32% | NA | 2019 |
| Wu P et al. [24] | CAD + DL + CNN | Classification | LIDC-IDRI | 1018 | NA | 97.70% | 98.35% | NA | 98.23% | NA | 2020 |
| Zhang S. et al. [25] | CAD + DL + CNN | Classification | LIDC-IDRI | 1018 | NA | NA | NA | NA | 97.04% | NA | 2019 |
| Liu A et al. [26] | Radiomics-CT | Classification | Private | 263 | 263 | NA | NA | NA | NA | 0.809 | 2020 |
| Mao L et al. [27] | Radiomics-LDCT | Classification | Private | 98 | 98 | NA | NA | NA | 89.80% | 0.97 | 2019 |
| Xu Y [28] | Radiomics-CT | Classification | Private | 373 | 373 | 89.00% | 74.00% | NA | 77.00% | 0.84 | 2019 |
| Zhou Z et al. [29] | Radiomics-LDCT | Classification | LIDC-IDRI | 1018 | 1226 | 85.80% | 90.70% | NA | 88.90% | 0.935 | 2019 |
| Asuntha A et al. [30] | CAD + DL + CNN | Detection and Classification | LIDC-IDRI | 1018 | NA | 97.93% | 96.32% | NA | 95.62% | NA | 2020 |
| Bhandary A et al. [31] | CAD + DL + CNN | Detection and Classification | LIDC-IDRI | 1018 | NA | 98.09% | 95.63% | NA | 97.27% | 0.996 | 2020 |
| Bansal G et al. [32] | CAD + DL + ResNet | Detection and Classification | LUNA16 | 888 | NA | 87.10% | 89.66% | NA | 88.33% | 0.88 | 2020 |
| El-Bana S et al. [33] | CAD + DL + TL | Detection and Classification | LUNA16; KAGGLE | 888; 1397 | NA | 96.40% | 99.40% | 0.6 | 97.00% | NA | 2020 |
| Masood A et al. [34] | CAD + DL + CNN | Detection | LUNA16 | 888 | NA | 81.20% 97.80% 98.53% 98.66% | NA | 0.125 1 4 8 | NA | NA | 2019 |
| Masood A et al. [34] | CAD + DL + CNN | Detection | LIDC-IDRI; ANODE09 | 1190 | NA | 98.40% | NA | 2.1 | NA | NA | 2019 |
| Nasrullah N et al [35] | CAD + DL-CNN | Detection and Classification | LIDC-IDRI | 1200 | 3250 | 94.00% | 90.00% | NA | 91.13% | 0.99 | 2019 |
| Nasrullah N et al [35] | CAD + DL-CNN + Biomarkers | Detection and Classification | LIDC-IDRI | 1018 | 2562 | 93.97% | 89.93% | NA | 88.79% | NA | 2019 |
| Shanid M et al. [36] | CAD + DL + DBN | Detection and Classification | LIDC-IDRI | 1018 | NA | NA | NA | NA | 96.00% | NA | 2019 |
| Zhang C. et al. [37] | CAD + DL + CNN | Detection and Classification | LUNA16; KAGGLE | 757 | 855 | 84.4% | 83.00% | NA | 83.70% | 0.803 | 2019 |
| Author | Year | Type | N | Target | ROI | RF | Results | Conclusions |
|---|---|---|---|---|---|---|---|---|
| Xue [43] | 2022 | R | 121 | Prognostic prediction | NA | NA | C-Index 0.782, 0.721 and 0.677 | Combined nomogram (radiomic-clinical) improves the accuracy of survival prognostic. |
| Huang [44] | 2022 | R | 512 | Prognostic prediction | M | 45 | HR 6.670, 2.866 and 3.342 | Radiomic features could be used for predicting OS |
| Dercle [45] | 2022 | R | 1584 | Prognostic prediction | NA | NA | HR incremented from 3.93 to 21.04 using RF | Combined model with radiomic features can provide information and improve decisions |
| Badic [46] | 2019 | R | 61 | Prognostic prediction | SA | 21 | rs max = 0.49 for first order features rs max = 0.770 for some second and third order features | Some radiomics features with moderate correlations between NCE-CT and CE-CT images |
| Mühlberg [47] | 2021 | R | 103 | Prognostic prediction | A | >1500 | AUC 0.73 and 0.76 for 1-year survival prediction | Geometric distribution and RF yield prognostic information |
| Li [48] | 2020 | R | 148 | Prognostic prediction | M | 17 | AUC of 0.842 and 0.802 for the combined model The combined model showed better prediction of OS | Combined model can help to predict distant metastasis |
| Zhao [49] | 2021 | R | 80 | Treatment response | M | 48 | C-index of 0.8335 and 0.9182 | RF are prognostic factors and predictive markers of OS |
| Ye [50] | 2022 | R | 139 | Treatment response | M | 1316 | AUC 0.871 and 0.745 for PFS | Combined model had better prediction results |
| Rabe [51] | 2022 | R | 29 | Treatment response | SA | 175 | AUC 0.80; S 0.73; Spec 0.79 | 8 RF had a significant association with treatment response |
| Cai [52] | 2020 | R | 381 | Treatment response | M | 85 | AUC of 0.74 and 0.82 | Radiomics score is an independent prognostic factor |
| Defeudis [53] | 2021 | R | 92 | Treatment response | M | 75 | S 0.61; Spec 0.60; PPV 0.57; NPV 0.64 | Promising results for determining the chemotherapy response |
| Lutsyk [54] | 2021 | R | 140 | Treatment response | M | 850 | Acc 0.63 405 RF were different (p < 0.001) between groups | Imagine features can help to determine complete and non-complete response |
| Bibault [55] | 2018 | R | 95 | Treatment response | M | 1683 | Acc of 0.80 | DL with clinical and RF can predict complete neoadjuvant chemotherapy response |
| Zhang [56] | 2022 | R | 215 | Treatment response | M | 275 | AUC of 0.92 and 0.89 | CT-based radiomics could be helpful in the treatment planning |
| Giannini [57] | 2022 | R | 301 | Treatment response | M | 107 | S 99–94%, Spec 95–99%, PPV 85–92%, NPV 90–87% | Delta radiomics signature was able to predict non-response |
| Vandendorpe [58] | 2019 | R | 121 | Treatment response | M | 36 | AUC of 0.70 predicting downstaging OR 13.25 for Radscore as independent factor | This prognostic score may lead to improve the treatment |
| Zhuang [59] | 2021 | R | 177 | Treatment response | M | 1218 | AUC 0.997 and 0.822 for prediction of CR | CT-based radiomics can help in the prediction of complete chemotherapy response |
| Wang [60] | 2022 | R | 191 | Treatment response | M | 1130 | AUC of 0.68 for locoregional failure FS. AUC of 0.64 for OS | CT-based radiomics can predict the NAR punctuation and the survival outcomes |
| Dercle [61] | 2020 | R | 667 | Treatment response | M | 3499 | AUC 0.80 and 0.72 for sensitivity to anti-EGFR AUC of 0.59 and 0.55 for chemotherapy response | RF can help in the early prediction of the success of treatment with Cetuximab |
| Yuan [62] | 2020 | R | 91 | Treatment response | NA | 8 | Acc of 83.9% differentiating TRG 0 vs. TRG 1–3 | Promising results for predicting pathologic complete response. |
| Bonomo [63] | 2022 | R | 201 | Treatment response | M | 1150 | AUC of 0.65 on prediction of GR | CT-base radiomics has potential predictive ability for identifying patients with GR |
| Fan [64] | 2021 | R | 299 | Treatment response | SA | 1561 | OR de 239,993 (p < 0.001) for recurrence risk AUC of 0.954 and 0.906 | Radiomic signature is an independent risk predictor and a non-invasive biomarker |
| Badic [65] | 2022 | R | 193 | Treatment response | SA | 88 | BAcc was 0.78 for recurrence prediction | CT-based radiomics had a good predictive performance of recurrence |
| Hong [66] | 2022 | R | 292 | Risk factors prediction | NA | NA | AUC 0.799 for combined model AUC of 0.679 for CT staging only | Combined model can improve the detection of high-risk colon cancer |
| Ge [67] | 2020 | R | 225 | Risk factors prediction | M | 396 | AUC 0.93 for the differentiation between mucinous and non-mucinous CRC | CT RF could be utilized as a noninvasive biomarker to identify MA from NMA patients |
| Hu [68] | 2016 | p | 40 | Risk factors prediction | M | 775 | 496 RF showed high reproducibility 225 shoed median reproducibility 54 showed low reproducibility | Some RF showed stability and could be used for treatment monitoring |
| Dou [69] | 2022 | R | 32 | Risk factors prediction | M | 125 | 3 parameters are associated with high and low risk group of metastases | Some RF could be used to help the T staging |
| Liu [70] | 2021 | R | 134 | Risk factors prediction | M | 854 (16) | AUC 0.945 and 0.754 for radiomic signature AUC 0.981 and 0.822 with multiscale nomogram | The multiscale nomogram could be used to facilitate the individualized preoperatively assessing metastasis in CRC patients |
| Huang [71] | 2018 | R | 366 | Risk factors prediction | M | 10959 | AUC of 0.8122 and 0.735 in discrimination between high and low CRC grade. | This radiomics signature can help with personal treatment |
| Liang [72] | 2016 | R | 494 | Risk factors prediction | M | 16 | AUC 0.792 and 0.708 | Radiomics signature can discriminate between stages I-II and III-IV |
| Badic [73] | 2019 | R | 64 | Gene expression | SA | 27 | ABCC2, CD166, CDKNV1 and INHBB genes has significant correlation with RF | Combined RF with genetic and pathological information can help to patient management |
| Chu [74] | 2020 | R | 163 141 | Prognostic prediction Gene expression | M | 12 | AUC 0.641 for prognostic prediction AUC 0.829 and 0.727 for CXCL8 | Combined model had better results. There are associations between RF and CXCL8 |
| Huang [75] | 2022 | R | 71 | Prognostic prediction Gene expression | M | 1037 | 10 RF with AUC 0.46–0.56 for recurrence prediction. | Association RF-recurrence prediction. Association with some gene expression. |
| Hoshino [76] | 2022 | R | 24 | Gene expression | M | 1037 | AUC of 0.732 and 0.812 for predicting TBM status. S of 0.857, Spec of 0.600 and Acc of 0.682 | The accurate inference of the TBM status is possible using radiogenomics |
| Yang [77] | 2018 | R | 117 | Gene expression | M | 346 | AUC 0.869–0.829; S 0.757–0.686; Spec 0.833–0.857 | Radiomic signature based on CT is associated with KRAS/NRAS/BRAF mutations |
| Shi [78] | 2020 | R | 159 | Gene expression | SA | 851 | AUC of 0.95 and 0.79 for the combined model for distinguishing between wild type and mutant | Radiomics together with semantic features can improve non-invasive assessment of KRAS status of LmCRC |
| González-Castro [79] | 2020 | R | 47 | Gene expression | M | 30 | Acc of 0.83; Kappa index of 0.647; S of 0.889 and Spec of 0.75 for the prediction of KRAS mutation | RF based on CT images can predict the KRAS mutation status |
| Wu [80] | 2020 | R | 279 | Gene expression | M | 50 | C index of 0.719 for Radiomics; 0.754 for DL-radiomics; 0.815 and 0.932 for combined model (1st and 2nd cohorts) in the prediction of KRAS mutation | This is a model that incorporates standard radiomics with deep learning-based radiomics. |
| He [81] | 2020 | R | 157 | Gene expression | M | 1025 | AUC of 0.818 | CT-based radiomics can predict KRAS mutation. |
| Hu [82] | 2022 | R | 231 | Gene expression | M | 1316 | AUC was 0.8826 for arterial and venous phase model | CT-based radiomics has potential to predict KRAS mutation |
| Jang [83] | 2021 | R | 110 | Gene expression | NA | 378 | AUC of 0.73 radiogenomics model AUC of 0.63 DL model | Radiomics model obtained better results than deep learning |
| Xue [84] | 2022 | R | 172 | Gene expression | NA | 1018 | AUC of 0.75 and 0.84 (2D and 3D radiomics models) for the 8 selected RF; AUC of 0.92 for the combined nomogram | CT-Radiomics can predict KRAS mutations. Combined nomogram improves the results |
| Xue [85] | 2022 | R | 140 | Gene expression | NA | NA | AUC of 0.93 and 0.87 for the 5 best RF; AUC of 0.95 and 0.88 for a combined nomogram | CT-based radiomics is associated with BRAF mutation |
| Negreros-Osuna [86] | 2020 | R | 145 | Gene expression | M | 24 | Some RF were significantly different between BRAF mutant and wild-type (p < 0.05) Some RF were associated with better 5-year OS (HR 0.40) | RF can serve as potential biomarkers for determining BRAF mutation status and as predictors of 5-year OS |
| Fan [87] | 2019 | R | 119 | MSI status | SA | 398 | Radiomics: AUC 0.688; Acc 0.713; S 0.517; Spec 0.858. Clinical: AUC 0.598; Acc 0.632; S 0.371; Spec 0.825. Combined model: AUC 0.752; Acc 0.765; S 0.663; Spec 0.842 | CT-based radiomics are associated with MSI status |
| Li [88] | 2021 | R | 368 | MSI status | M | 1628 | AUC 0.79 and 0.73 | Combined model can predict MSI status |
| Ying [89] | 2022 | R | 276 | MSI status | M | 1037 | AUC 0.87 and 0.90 | Combined nomogram can predict MSI status |
| Chen [90] | 2022 | R | 837 | MSI status | NA | 10 | AUC of 0.788 and 0.775 (radiomics) AUC of 0.777 and 0.767 (combined model) AUC of 0.768 and 0.623 (clinical model) | The radiomics signature showed a robust model for identifying the MSI status |
| Pei [91] | 2022 | R | 762 | MSI status | M | 340 | AUC of 0.74 and 0.77 for the combined nomogram | The radiomics combined nomogram could be used to predict MSI status. |
| Cao [92] | 2021 | R | 502 | MSI status | M | 1037 | 32 RF showed correlation with MSI status. AUC of 0.898–0.964; ACC of 0.837–0.918; S of 0.821–1 for the combined nomogram | CT-based radiomics can predict MSI status |
| Wu [93] | 2019 | R | 102 | MSI status | M | 606 | AUC 0.961 and 0.875 for predicting MSI status | Radiomics analysis of iodine-based MD images with DECT can predict MSI status |
| Golia Pernicka [94] | 2019 | R | 198 | MSI status | M | 254 | AUC of 0.80 and 0.79 (combined model) AUC 0.74 and 0.76 (clinical and radiomics model, respectively) | Preoperative prediction of MSI status via radiomics can improve the treatment selection |
| Liu [95] | 2020 | R | 15 | LN metastasis | M | 107 | 73 RF were significant AUC 0.88 | Some RF showed significance in differentiating nonmetastatic LN from metastatic LN. |
| Cheng [96] | 2022 | R | 191 | LN metastasis | NA | NA | AUC 0.830 and 0.712 | 9 radiomic features had significant results for LN metastasis prediction |
| Huang [97] | 2016 | R | 526 | LN metastasis | M | 150 | C index 0.718 and 0.773 for radiomics signature. C index 0.763 for the prediction nomogram. | The radiomics signature combined with clinical risk factors helps in preoperative prediction of LN metastasis. |
| Eresen [98] | 2020 | R | 390 | LN metastasis | M | 146 | ACC of 0.6538–0.6282, S of 0.8387–0.8462 and Spec of 0.4713–0.4103 for the clinical model ACC of 0.8109–0.7949, S of 0.8387–0.7436 and Spec of 0.7834–0.8462 for combined model | The texture of LN provided information about the histological status of the LN |
| Li [99] | 2022 | R | 351 | Prediction LVI | M | 3095 | AUC of the combined model was 0.843 | RF combined with clinical factors had good performance in prediction of LVI |
| Ge [100] | 2021 | R | 169 | Prediction LVI | M | 396 | AUC of 0.90 for the peri-tumoral features AUC of 0.82 for the tumor features | CT-radiomics model based on the peritumoral zone improves prediction of LVI |
| Liu [101] | 2021 | R | 57 | Lung metastasis | M | 1724 | 90 RF remained unchanged in metastatic nodules | RF could be useful for investigating pulmonary nodules |
| Markich [102] | 2021 | R | 48 | Lung metastasis | NA | 64 | C-index of 0.74 for the combined model with 4 RF | RF can help to discriminate nodules at risk of local progression |
| Giannini [103] | 2020 | R | 95 | Liver metastasis | M | 22 | Acc 0.61; S 0.73; Spec 0.47 | Radiomics model can predict the likelihood of response of liver metastasis in CRC |
| Taghavi [104] | 2021 | p | 94 | Liver metastasis | NA | NA | AUC 0.60 | Radiomics models cannot predict new liver metastases of CRC |
| Staal [105] | 2021 | R | 82 | Liver metastasis | M | 56 | C-index of 0.78 | RF from the ablation zone could help in the prediction of local tumor progression |
| Liu [106] | 2022 | R | 63 | Liver metastasis | M | 851 | C-index 0.758 and 0.743 for OS AUC for the 1-y survival 0.850 and 0.694 AUC for the 2-y survival 0.845 and 0.909 AUC for the 3-y survival 0.819 and 0.835 | Radiomics signature based on CT images can predict the outcome of hepatic arterial infusion chemotherapy |
| Giannini [107] | 2020 | R | 38 | Liver metastasis | M | 24 | S 0.89 and 0.90; Spec 0.85 and 0.42 for HER2 therapy response | This method is effective in predicting behavior of metastasis to HER2 treatment |
| Creasy [108] | 2021 | R | 120 | Liver metastasis | SA | 254 | 44 RF with p < 0.05 | There are RF that showed different distributions between patients with liver recurrence |
| Taghavi [109] | 2021 | R | 90 | Liver metastasis | M | 1593 | C Index of 0.79 in the combined model; 0.78 for the radiomics model; 0.56 for the clinical model | CT-based radiomics pre-ablation could help to predict local progression |
| Starmans [110] | 2021 | R | 76 | Liver metastasis | M | 564 | AUC 0.69 for predicting dHPG | This model has potential for automatically distinguishing dHGP from rHGP |
| Cheng [111] | 2019 | R | 126 | Liver metastasis | M | 20 | AUC of 0.926 and 0.939 C-index of 0.941 and 0.833 | A radiomics model can predict the HGPs of liver metastasis of CRC |
| Tharmaseelan [112] | 2022 | R | 47 | Liver metastasis | SA | 4 | Differentiate the images into 5 groups in function of the heterogeneity | RF could characterize the heterogeneity in liver metastasis of CRC |
| Devoto [113] | 2022 | R | 24 | Liver metastasis | A | NA | The metastatic liver was more heterogeneous (p < 0.05) | RF can differentiate a normal appearing metastatic liver from a non-metastatic liver |
| Dohan [114] | 2020 | R | 110 | Liver metastasis | M | 20 | 3 RF with p < 0.005 for predicting OS | RF was able to predict OS and identify good responders better than RECIST 1.1 criteria. |
| Taghavi [115] | 2021 | R | 91 | Liver metastasis | A/M | 1767 | AUC of 0.71; 0.86 and 0.86 | RF can provide valuable biomarkers to identify patients with a high risk for liver metastasis |
| Li [116] | 2022 | R | 323 | Liver metastasis | M | 1288 | AUC 0.79 and 0.72 | Combined model can provide biomarkers to identify patients with high risk of LmCRC |
| Li [117] | 2020 | R | 100 | Liver metastasis | M | 841 | AUC 0.90; 0.86; 0.906 and 0.899 | Nomogram with RF and clinical risk allows a better classification of liver metastasis |
| Rocca [118] | 2021 | R | 30 | Liver metastasis | M | 22 | General Acc of 0.933 | CT-based radiomics can detect LmCRC |
| Lee [119] | 2020 | R | 2019 | Liver metastasis | M | 4096 | AUC of 0.747 in prediction 5-year liver metastasis | Combined model improved the performance |
| Huang [120] | 2018 | R | 346 | Perineural invasion | M | 29 | C index 0.817 for combined nomogram | Combined nomogram was easy and effective |
| Li [121] | 2020 | R | 207 | Perineural invasion Gene expression | M | 306 | AUC of 0.793 (PNI prediction) AUC of 0.862 (KRAS prediction) | Machine learning models can predict PNI and KRAS mutation in CRC patients |
| Li [122] | 2021 | R | 303 | Perineural invasion | M | 3095 | AUC of 0.828 and 0.801 for the combined model for predicting PNI status | The combined model can help to evaluate the PNI status |
| Li [123] | 2020 | R | 779 | Peritoneal metastasis | SA | 8900 | AUC of 0.855 for combined model AUC of 0.764 and 0.771 for radiomics and clinical | Combined model, with CT-based radiomics, can be applied in the prediction of PM |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Porto-Álvarez, J.; Barnes, G.T.; Villanueva, A.; García-Figueiras, R.; Baleato-González, S.; Huelga Zapico, E.; Souto-Bayarri, M. Digital Medical X-ray Imaging, CAD in Lung Cancer and Radiomics in Colorectal Cancer: Past, Present and Future. Appl. Sci. 2023, 13, 2218. https://doi.org/10.3390/app13042218
Porto-Álvarez J, Barnes GT, Villanueva A, García-Figueiras R, Baleato-González S, Huelga Zapico E, Souto-Bayarri M. Digital Medical X-ray Imaging, CAD in Lung Cancer and Radiomics in Colorectal Cancer: Past, Present and Future. Applied Sciences. 2023; 13(4):2218. https://doi.org/10.3390/app13042218
Chicago/Turabian StylePorto-Álvarez, Jacobo, Gary T. Barnes, Alex Villanueva, Roberto García-Figueiras, Sandra Baleato-González, Emilio Huelga Zapico, and Miguel Souto-Bayarri. 2023. "Digital Medical X-ray Imaging, CAD in Lung Cancer and Radiomics in Colorectal Cancer: Past, Present and Future" Applied Sciences 13, no. 4: 2218. https://doi.org/10.3390/app13042218
APA StylePorto-Álvarez, J., Barnes, G. T., Villanueva, A., García-Figueiras, R., Baleato-González, S., Huelga Zapico, E., & Souto-Bayarri, M. (2023). Digital Medical X-ray Imaging, CAD in Lung Cancer and Radiomics in Colorectal Cancer: Past, Present and Future. Applied Sciences, 13(4), 2218. https://doi.org/10.3390/app13042218










