Taxonomic Exploration of Healthcare IoT: Challenges, Solutions, and Future Frontiers
Abstract
:1. Introduction
1.1. Motivation
1.2. Contributions
- Examining primary approaches to IoT-based medical management systems;
- Presenting an SLR and examining possible approaches to IoT-based medical management systems;
- Discussing important IoT challenges within the context of the methodologies under discussion;
- Offering the category of the methods investigated and highlighting their key characteristics.
1.3. Roadmap of the SLR
- Why should IoT be incorporated into healthcare systems, practically speaking?
- What are the available research fields for IoT-based healthcare systems?
- What triumphs have been attained in this area?
- What current procedures and strategies are being used to integrate IoT into healthcare systems?
- What are the key challenges facing the IoT, its emerging trends, and open questions?
- What new HIoT system research areas should be developed?
- Studies that define the use of IoT in healthcare;
- Studies made by researchers and professionals;
- Peer-reviewed articles;
- Articles published in English.
- IoT and contemporary healthcare researchers want to analyze the related investigations;
- Medical professionals are interested in applying modern methods, approaches, strategies, and technologies while working within the constraints of HIoT systems.
2. Background
2.1. Internet of Things
2.2. Healthcare
- Perception Layer: At the bottom of the hierarchy, we have this layer, which we may refer to as ’hardware’ or ’physical’. By collecting and signalling data, this layer prepares data for transmission to the network layer.
- Network Layer: In this layer, all smart devices are connected, and health data can be exchanged among them. The cutting-edge technologies used by this layer allow patients to securely transmit and receive health data from the base station.
- Middleware Layer: In this layer, services are dispensed with names and addresses associated with requests. Non-homogeneous items can be used with HIoT applications without requiring peculiar equipment platforms. Health data are collected from the network layer and cached here.
- Application Layer: Data from other layers are analyzed and combined in this layer to dispense healthcare services. Healthcare services can be dispensed at this layer to meet the needs of patients. In this layer, graphs, business models, and flowcharts that control all activities and healthcare services can be produced. HIoT systems cannot succeed without technological innovations, business models, and appropriate business models.
- (1)
- Data generation: The process of generating the required data involves using a variety of sensors, medical devices, and even direct data entry by patients or other involved healthcare teams. The perception layer is used for this phase, while the network layer is used to transpose the data collected.
- (2)
- Data processing: In the data processing stage, collected data are analysed using well-known mechanisms including machine learning techniques and data analysis tools. Through the middleware layer, this stage is completed.
- (3)
- Information consuming: In the information consumption phase, any decisions that medical teams must make on behalf of patients can be made utilizing the outputs and analytics from the data processing phase. This analytical information can even be used to activate the actuators. The application and business layers are used for this phase.
2.3. Criteria for Evaluating HIoT Approaches
- (1)
- Security and Privacy: Smart healthcare systems must prioritise security and privacy in order to protect health data against attacks such as side-channel attacks, physical attacks, and malicious attacks, as well as to maintain privacy and prevent unauthorised ingress to health data.
- (2)
- Accuracy: Accuracy is essential for healthcare system carers. Depending on how the system is used, accuracy in healthcare IoT systems refers to how accurately the data collected reflect the patient’s condition, how accurate the data used in the computation were, and how accurately the decision was made.
- (3)
- Performance: Healthcare providers must perform well in order to obtain precise data, process the data, and offer services quickly. This parameter is a combination of efficiency, load balancing, resource utilization, overhead, and computing time, as well as network quality of service (QoS) factors including throughput, latency, delivery rate, mean time between failures, and bandwidth usage.
- (4)
- Time: The time it takes for consumers to receive service after making a request is described by this parameter. The concept of time encompasses calculation time, average response time, execution time (run-time), and latency (as the time lag in healthcare systems).
- (5)
- Cost: This refers to the overall expense a patient who requests healthcare services may incur to receive the best care possible. The cost of computation, communication, data storage, and the upkeep of the desired service are all included.
- (6)
- Energy: Energy conservation is crucial for device and network survival, since HIoT devices lack resources and are powered with meagre energy resources. Additionally, when there are more HIoT devices linked to the network, the network’s energy usage grows as well. On the other hand, more energy use results in higher operating expenses, more carbon dioxide produced, and a shorter network lifetime.
- (7)
- Interoperability: Interoperability refers to the capability of more than two HIoT systems to communicate and exchange information in a dependable, consistent, and efficient manner, use the information exchanged, and share resources. More than one medical informatics system, for example, may be necessary. The capacity to successfully grasp data across organizational or system boundaries is referred to as data interoperability. HIoT systems require the usage of standardized communication as well as a number of other interoperability-supporting technologies.
- (8)
- Scalability: This refers to the capability of the system to extend and build an IoT-based healthcare methodology as service needs and expectations grow. These capabilities can be leveraged to create smart devices, new operations that act as user service nodes, and network infrastructures, while not adjusting the quality or effectiveness of healthcare services. Extending the system requires either the addition of new hardware or services or improvement of the operation of current hardware or services.
- (9)
- Reliability: The capacity of a system to carry out its necessary functions under pre-determined circumstances and at a predetermined time. A healthcare system based on IoT is said to be reliable if it can provide requested services to patients in most conditions.
3. Related Works
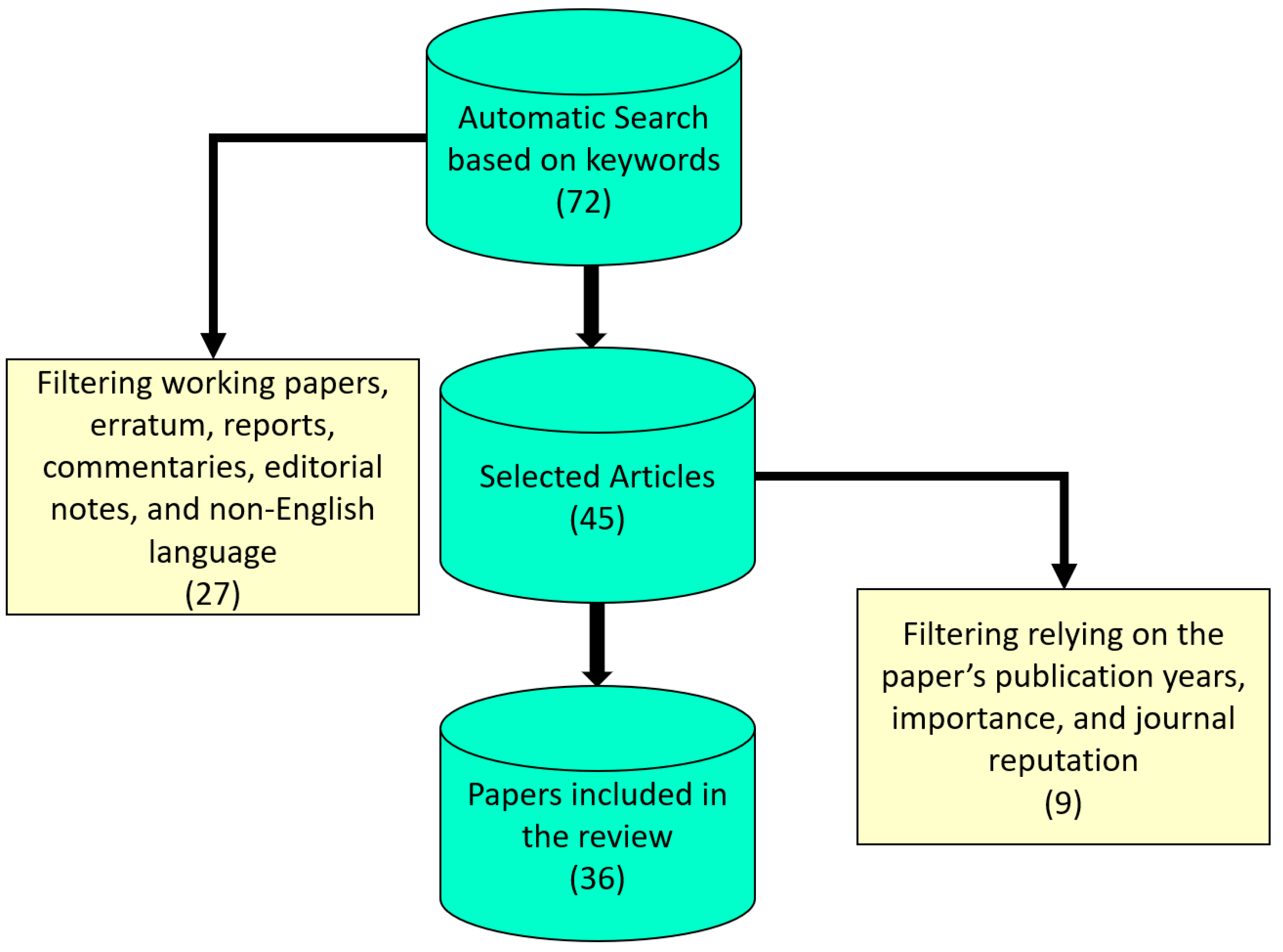
4. Research Methodology
- Planning and conducting
- Reviewing process
- Inclusion and exclusion
- Quality assessment
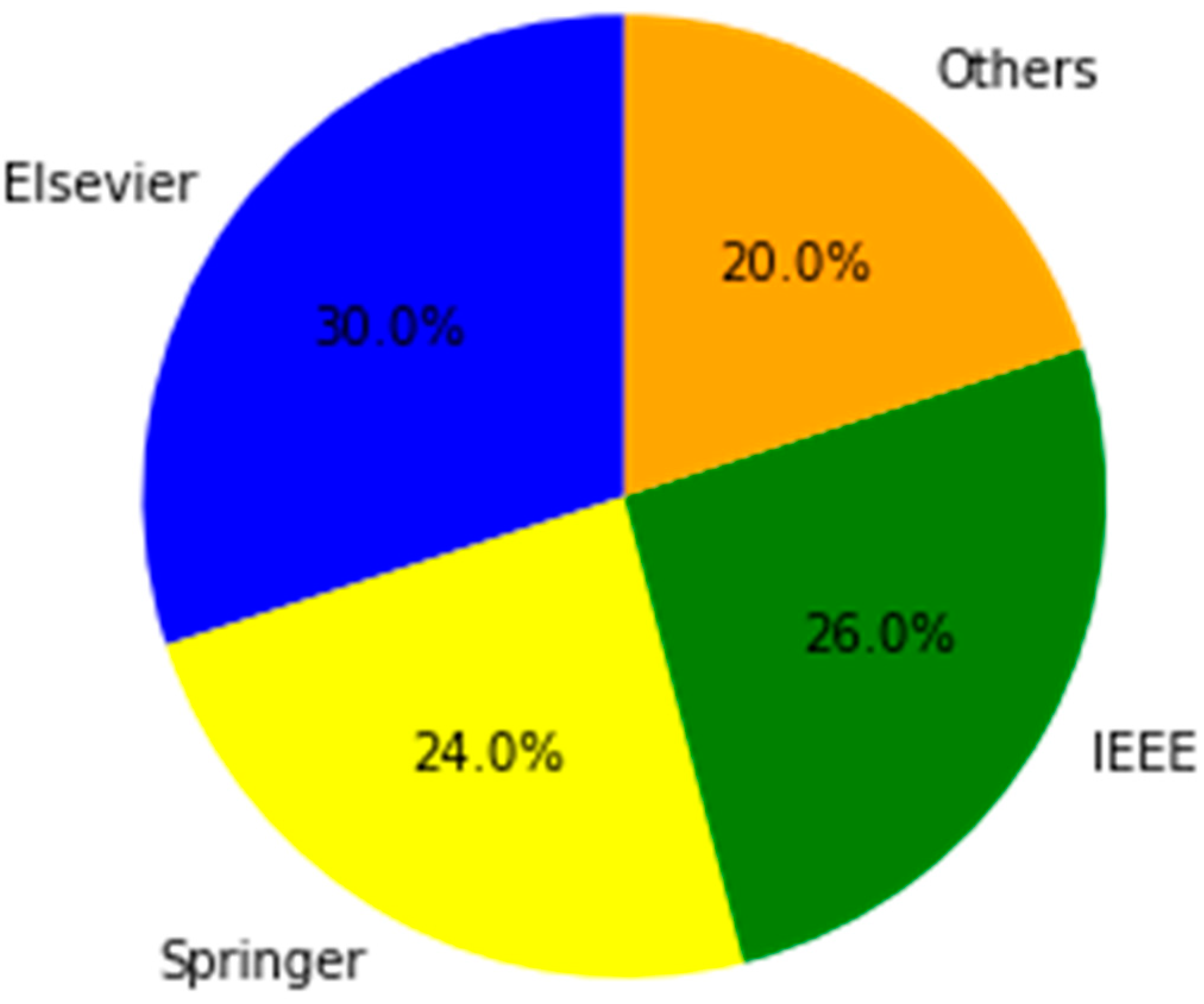
4.1. Plan and Conduct
4.2. Review Process
- Will the study make the review procedure very clear?
- Is the analysis approach appropriate for the topic under consideration?
- Was the research evaluation carried out correctly?
4.3. Inclusion and Exclusion Criteria
4.4. Quality Assessment
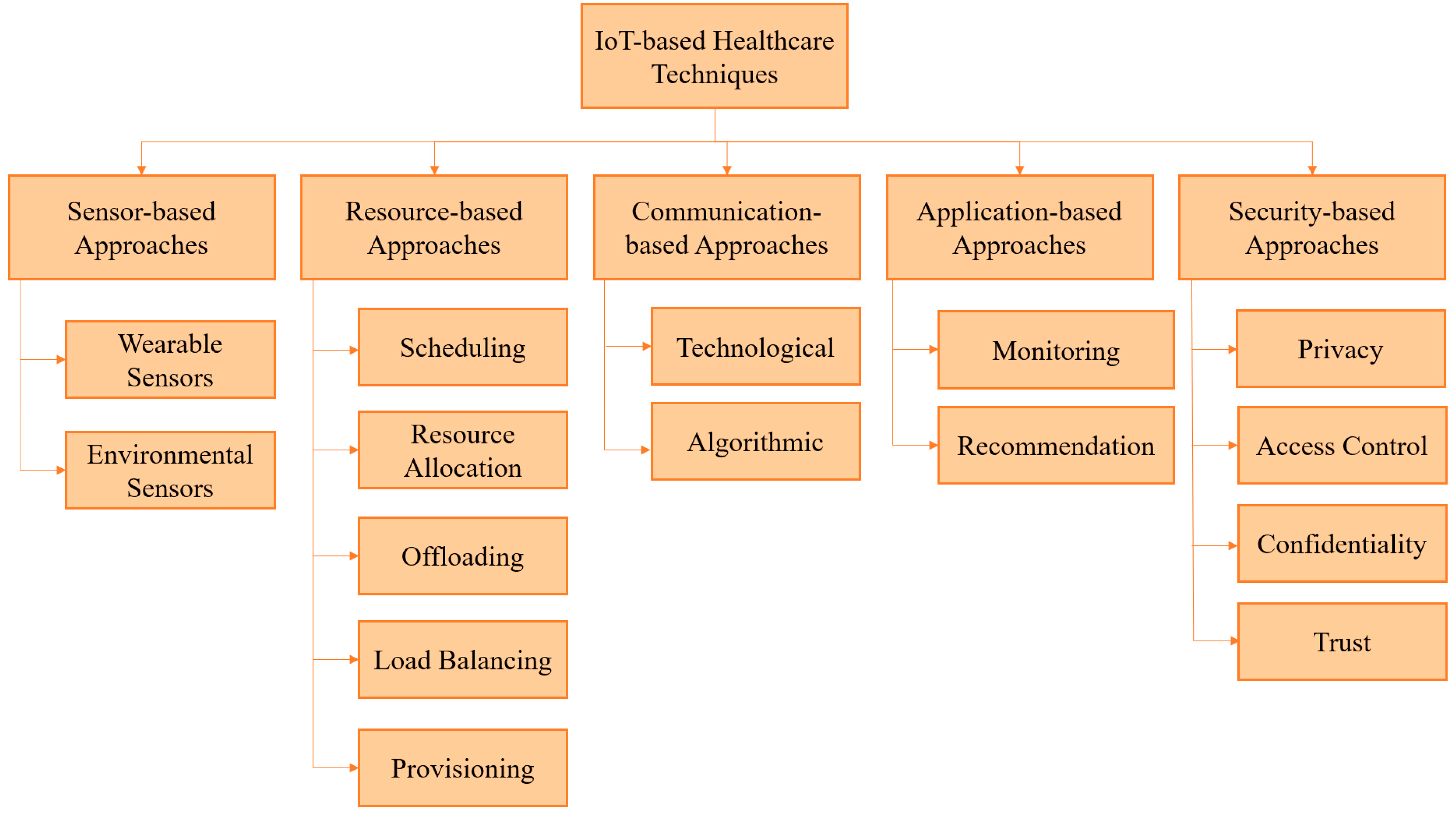
4.5. Sensor-Based Approaches
4.5.1. Wearable Sensors
4.5.2. Environmental Sensors
4.6. Resource-Based Approaches
4.6.1. Scheduling
4.6.2. Resource Allocation
4.6.3. Offloading
4.6.4. Load Balancing
4.6.5. Provisioning
4.7. Communication-Based Approaches
4.7.1. Technological
4.7.2. Algorithmic
4.8. Application-Based Approaches
4.8.1. Monitoring
4.8.2. Recommendation
4.9. Security-Based Approaches
4.9.1. Privacy
4.9.2. Access Control
4.9.3. Confidentiality
4.9.4. Trust
5. Results and Discussions
6. Open Concerns and Potential Developments
6.1. Issues
- (1)
- Trust and Privacy: Trust and privacy management is a significant open problem in IoT-based healthcare systems for data ingress and storage. Controlling access to credentials, protecting the privacy of patients and service providers, and preventing unauthorized access to any of these are all examples of trust. IoT-based systems for the healthcare industry are developed based on the data collected by IoT devices. As IoT devices are connected to the network, their susceptibility to data breaches rises [43]. However, the analyzed studies show that only a few papers have properly assessed this important parameter. As a result, trust and privacy are extremely difficult to sustain, as open concerns. Reducing the risk of critical data being hacked and improving data security is especially tough.
- (2)
- Power Management: Reduced energy usage, according to the reviewed literature, is the key to minimizing high operational costs and large carbon emissions in HIoT systems. Furthermore, a typical HIoT network is made up of tiny devices with limited battery life. As a result, fundamental features such as data migration and systematic standby control are critical to minimizing energy consumption while maintaining the quality of smart healthcare services. As a result, low-power devices must be developed in order to extend the life of HIoT systems and limit the likelihood of patients being disconnected. As a result, another challenge for HIoT is power management [44].
- (3)
- Fog Computing: Fog computing, which is location-aware and dependent on environment, context, and application needs, is an integral part of healthcare IoT. Furthermore, low and predictable latency is required to deliver services to end users in emergency situations, to save bandwidth, and save battery usage while essential data are delivered to the fog for processing and storing, and to diminish the volume of data transposed to the cloud. More activities are required to fulfil the aforementioned needs in HIoT systems, despite considerable advancements in this field. Fog computing is therefore exceedingly difficult for researchers.
- (4)
- Resource Management: HIoT nodes’ assignments are enormous despite their modest computational and storage capacity. Therefore, in the HIoT context, managing and effectively deploying smart healthcare equipment is essential. In general, resource management might result in greater research and analysis. Furthermore, resource management should successfully enact a wide range of services in order to make the most use of existing resources and deliver relevant services in HIoT. This is owing to smart gadgets’ mobility and relocation capabilities. Therefore, resource management is another crucial unresolved topic in this study.
- (5)
- Multi-objective Optimization: It is obvious that some QoS aspects of HIoT systems were taken into account, while others were not. For instance, some algorithms only take into account cost and delay, ignoring other considerations like reliability and electricity. Therefore, an ideal mechanism that takes into account various aims to make a tradeoff between various QoS parameters in HIoT systems may still be a work in progress.
6.2. Challenges
- (1)
- Scalability: In the healthcare system, scalability is crucial. This implies a system’s ability to meet shifting demands and adapt to developments that will become more significant in the future. According to the literature review, some of the suggested methods for HIoT systems can work on a limited scale, and only a few nodes or devices can vouch for their authenticity. Scalability is an important element. However, it appears to be a challenge because the offered ways were generally applied in confined contexts.
- (2)
- Interoperability and Standardization: In the HIoT, interoperability is crucial for the transposition of information and resources between patients and smart objects. Open-source frameworks with reliable connections are the main obstacle to interoperability; standards must be established so that horizontal platforms can be operable, programmable, and communicable, regardless of the model or the manufacturer, among devices, operating systems, and applications. It is also important to acquire dynamic and flexible architectures that are interoperable with large-scale IoT applications, and to be able to interface with nonhomogeneous data centres and smart devices with scalable architecture. The interoperability and standardization of HIoT systems are the primary unresolved issues.
- (3)
- Mobility: The literature has paid less attention to mobility as one of the biggest obstacles in HIoT. When it comes to IoT healthcare systems, mobility means providing patients with the ability to connect to the gateway whenever and wherever they want. A mobile network improves the quality of service, makes information accessible no matter where users are, and makes the network fault-tolerant. It is essential in the healthcare industry that mobility protocols are dependable so that packet losses, network failures, and end-to-end delays are minimized. Therefore, mobility presents an intriguing research problem.
- (4)
- Real Testbed Environment: Only 24% of the examined research was carried out in actual testbeds, while the rest was assessed using simulation tools. The HIoT methodologies suggested in these studies should be enacted in real situations. To be completely honest, all of the suggested methods need to be put to the test in actual settings in order to determine whether or not they can deliver a system of healthcare that is adequate. Real testbed implementation is difficult as a result.
6.3. Trends
- (1)
- Blockchain: Blockchain is a possible solution for the edge/IoT environment in the future. Health data can be securely managed and analyzed using blockchain technology. It is the greatest technology for the healthcare system because it cannot be altered or deleted from blocks [8]. It may be that the Internet of edge-blocks can be used to help the current edge-IoT environment handle decentralized end-user requests transparently and autonomously. Furthermore, it is a permanent, clear consensus system that relies on peer-to-peer and distributed communication rather than centralised authority; it is also an immutable, clear consensus protocol. Due to the fact that researchers have not given this issue much consideration, blockchain in HIoT may prove to be an important future development.
- (2)
- Tactile Internet: The term Tactile Internet (TI) refers to the concept of sensory connectedness on the Internet [6]. In a digital environment, it develops perception skills by reproducing stimuli and senses using standardized communication among devices. Researchers are looking into TI-based applications in the areas of healthcare and robotics in particular as a result of the emergence of 5G communications technology. TI can be used in a variety of ways in healthcare, including Parkinson’s disease tremor suppression, remote surgery, interactive medical training, trauma rehabilitation, and virtual and augmented reality. As a result, TI applications offer some HIoT possibilities that could present worthwhile research opportunities in the future.
- (3)
- Software-Defined Networks/Network Function Virtualization: Support for software-defined networks (SDN) in IoT systems helps improve IoT administration due to resource constraints. The integration of IoT and network function virtualization (NFV) allows for the rapid creation, administration, and deployment of novel applicant-based services. Future research in this exciting area will aid in meeting the QoS needs of HIoT [44].
- (4)
- Online Social Networks: In the digital era, online social networks can serve as a reliable platform link between healthcare providers and healthcare consumers at any time and in any place. Through this paradigm, remote healthcare providers can share health data with their patients through computationally and strongly resource-rich social networks. Social network nodes include friendship, employment, shared interests, knowledge, status, and other nodes that can be collocated to exchange information, knowledge, or financial assistance. This HIoT paradigm is a whole new arena for predicting a patient’s health status, and it offers numerous research opportunities.
- (5)
- Big Data Analytics: Modern smart healthcare solutions are built upon IoT big data analytics. Consequently, the development of contemporary medical telematics and informatics, including illness diagnosis, remote and instantaneous health monitoring, preventative systems, and emergency and alerting systems, is attributable to the convergence of big data analytics and the Internet of Things [46]. Combined with a complex background of other health-related information, data collected from diverse devices in IoT environments contains a great deal of long-term information about users’ personal lives. In order to generate intelligence for the creation of policies and more informed clinical decision making, it is important to investigate how to explore all of this huge data under IoT systems. However, this topic has not received much attention among all the investigations. In IoT-based healthcare systems, big data analytics are therefore needed for further research.
- (6)
- Service Quality: Applications using instantaneous HIoT have recently been developed. QoS concerns revolve around HIoT data’s quality and timeliness for supporting decisions. The timely collection, analysis, transposition, and use of data generated by healthcare sensors is essential; however, there are times when the pertinent data are not instantly accessible, which seems to be an issue for HIoT systems. The diversity, volume, and speed of the instantaneous data produced by IoT devices creates a significant barrier for data analysis. The immediate and life-critical nature of medical wearable systems necessitates a high standard of service quality. There are significant gaps in a variety of areas, including the instantaneous monitoring of patients, the collection of data, and decision-making support based on QoS. It goes without saying that the QoS must be the foundation for overcoming these difficulties [45].
- (7)
- Internet of Nano Things: Nanorobots, precision medicine, minimally invasive surgery, nanosensors, and nanorobot swarms for inaccessible human body parts are some of the applications of the IoNT. Nanorobots can deliver medications to certain organs with extreme precision. Furthermore, as a possible future avenue in sensing and precision medicine, the IoNT is driving a nanoscale network revolution.
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Nasajpour, M.; Pouriyeh, S.; Parizi, R.M.; Dorodchi, M.; Valero, M.; Arabnia, H.R. Internet of Things for current COVID-19 and future pandemics: An exploratory study. J. Healthc. Inform. Res. 2020, 4, 325–364. [Google Scholar] [CrossRef]
- Huifeng, W.; Kadry, S.N.; Raj, E.D. Continuous health monitoring of sportsperson using IoT devices based wearable technology. Comput. Commun. 2020, 160, 588–595. [Google Scholar] [CrossRef]
- Abdellatif, A.A.; Khafagy, M.G.; Mohamed, A.; Chiasserini, C.F. EEG-based transceiver design with data decomposition for healthcare IoT applications. IEEE Internet Things J. 2018, 5, 3569–3579. [Google Scholar] [CrossRef]
- Abdelmoneem, R.M.; Benslimane, A.; Shaaban, E. Mobility-aware task scheduling in cloud-Fog IoT-based healthcare architectures. Comput. Netw. 2020, 179, 107348. [Google Scholar] [CrossRef]
- AbdulGhaffar, A.; Mostafa, S.M.; Alsaleh, A.; Sheltami, T.; Shakshuki, E.M. Internet of things based multiple disease monitoring and health improvement system. J. Ambient Intell. Humaniz. Comput. 2020, 11, 1021–1029. [Google Scholar] [CrossRef]
- Abou-Nassar, E.M.; Iliyasu, A.M.; El-Kafrawy, P.M.; Song, O.Y.; Bashir, A.K.; Abd El-Latif, A.A. DITrust chain: Towards blockchain-based trust models for sustainable healthcare IoT systems. IEEE Access 2020, 8, 111223–111238. [Google Scholar] [CrossRef]
- Singh, S.; Rathore, S.; Alfarraj, O.; Tolba, A.; Yoon, B. A framework for privacy-preservation of IoT healthcare data using Federated Learning and blockchain technology. Future Gener. Comput. Syst. 2022, 129, 380–388. [Google Scholar] [CrossRef]
- Alamri, B.; Crowley, K.; Richardson, I. Blockchain-based identity management systems in health IoT: A systematic review. IEEE Access 2022, 10, 59612–59629. [Google Scholar] [CrossRef]
- Aghili, S.F.; Mala, H.; Shojafar, M.; Peris-Lopez, P. LACO: Lightweight three-factor authentication, access control and ownership transfer scheme for e-health systems in IoT. Future Gener. Comput. Syst. 2019, 96, 410–424. [Google Scholar] [CrossRef]
- Ahmadi, H.; Arji, G.; Shahmoradi, L.; Safdari, R.; Nilashi, M.; Alizadeh, M. The application of internet of things in healthcare: A systematic literature review and classification. Univers. Access Inf. Soc. 2019, 18, 837–869. [Google Scholar] [CrossRef]
- Ahmadi, Z.; Haghi Kashani, M.; Nikravan, M.; Mahdipour, E. Fog-based healthcare systems: A systematic review. Multimed. Tools Appl. 2021, 80, 36361–36400. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Latif, R.; Latif, S.; Abbas, H.; Khan, F.A. Malicious insiders attack in IoT based multi-cloud e-healthcare environment: A systematic literature review. Multimed. Tools Appl. 2018, 77, 21947–21965. [Google Scholar] [CrossRef]
- Habibzadeh, H.; Dinesh, K.; Shishvan, O.R.; Boggio-Dandry, A.; Sharma, G.; Soyata, T. A survey of healthcare Internet of Things (HIoT): A clinical perspective. IEEE Internet Things J. 2019, 7, 53–71. [Google Scholar] [CrossRef]
- Akhbarifar, S.; Javadi HH, S.; Rahmani, A.M.; Hosseinzadeh, M. A secure remote health monitoring model for early disease diagnosis in cloud-based IoT environment. Pers. Ubiquitous Comput. 2020, 27, 697–713. [Google Scholar] [CrossRef] [PubMed]
- Aktas, F.; Ceken, C.; Erdemli, Y.E. IoT-based healthcare framework for biomedical applications. J. Med. Biol. Eng. 2018, 38, 966–979. [Google Scholar] [CrossRef]
- Al-Fuqaha, A.; Guizani, M.; Mohammadi, M.; Aledhari, M.; Ayyash, M. Internet of things: A survey on enabling technologies, protocols, and applications. IEEE Commun. Surv. Tutor. 2015, 17, 2347–2376. [Google Scholar] [CrossRef]
- Alam, M.M.; Malik, H.; Khan, M.I.; Pardy, T.; Kuusik, A.; Le Moullec, Y. A survey on the roles of communication technologies in IoT-based personalized healthcare applications. IEEE Access 2018, 6, 36611–36631. [Google Scholar] [CrossRef]
- Alhussein, M.; Muhammad, G.; Hossain, M.S.; Amin, S.U. Cognitive IoT-cloud integration for smart healthcare: Case study for epileptic seizure detection and monitoring. Mob. Netw. Appl. 2018, 23, 1624–1635. [Google Scholar] [CrossRef]
- Ali, M.S.; Vecchio, M.; Pincheira, M.; Dolui, K.; Antonelli, F.; Rehmani, M.H. Applications of blockchains in the Internet of Things: A comprehensive survey. IEEE Commun. Surv. Tutor. 2018, 21, 1676–1717. [Google Scholar] [CrossRef]
- Alladi, T.; Chamola, V. HARCI: A two-way authentication protocol for three entity healthcare IoT networks. IEEE J. Sel. Areas Commun. 2020, 39, 361–369. [Google Scholar] [CrossRef]
- Alzahrani, B.A. Secure and efficient cloud-based IoT authenticated key agreement scheme for e-health wireless sensor networks. Arab. J. Sci. Eng. 2021, 46, 3017–3032. [Google Scholar] [CrossRef]
- Amin, M.; Shehwar, D.; Ullah, A.; Guarda, T.; Tanveer, T.A.; Anwar, S. A deep learning system for health care IoT and smartphone malware detection. Neural Comput. Appl. 2020, 34, 11283–11294. [Google Scholar] [CrossRef]
- Karimi, Y.; Haghi Kashani, M.; Akbari, M.; Mahdipour, E. Leveraging big data in smart cities: A systematic review. Concurr. Comput. Pract. Exp. 2021, 33, e6379. [Google Scholar] [CrossRef]
- Najafizadeh, A.; Salajegheh, A.; Rahmani, A.M.; Sahafi, A. Privacy-preserving for the internet of things in multi-objective task scheduling in cloud-fog computing using goal programming approach. Peer-Peer Netw. Appl. 2021, 14, 3865–3890. [Google Scholar] [CrossRef]
- Ashton, K. That ‘internet of things’ thing. RFID J. 2009, 22, 97–114. [Google Scholar]
- Sofla, M.S.; Kashani, M.H.; Mahdipour, E.; Mirzaee, R.F. Towards effective offloading mechanisms in fog computing. Multimed. Tools Appl. 2022, 81, 1997. [Google Scholar] [CrossRef]
- Yang, Y.; Zheng, X.; Guo, W.; Liu, X.; Chang, V. Privacy-preserving smart IoT-based healthcare big data storage and self-adaptive access control system. Inf. Sci. 2019, 479, 567–592. [Google Scholar] [CrossRef]
- Gope, P.; Gheraibia, Y.; Kabir, S.; Sikdar, B. A secure IoT-based modern healthcare system with fault-tolerant decision making process. IEEE J. Biomed. Health Inform. 2020, 25, 862–873. [Google Scholar] [CrossRef]
- Zhou, W.; Piramuthu, S. IoT security perspective of a flexible healthcare supply chain. Inf. Technol. Manag. 2018, 19, 141–153. [Google Scholar] [CrossRef]
- Zou, N.; Liang, S.; He, D. Issues and challenges of user and data interaction in healthcare-related IoT: A systematic review. Libr. Hi Tech. 2020, 38, 769–782. [Google Scholar] [CrossRef]
- Garg, N.; Wazid, M.; Singh, J.; Singh, D.P.; Das, A.K. Security in IoMT-driven smart healthcare: A comprehensive review and open challenges. Secur. Priv. 2022, 5, e235. [Google Scholar] [CrossRef]
- Ali, M.; Naeem, F.; Tariq, M.; Kaddoum, G. Federated learning for privacy preservation in smart healthcare systems: A comprehensive survey. IEEE J. Biomed. Health Inform. 2022, 27, 778–789. [Google Scholar] [CrossRef] [PubMed]
- Soni, G.; Kandasamy, S. Smart garbage bin systems—A comprehensive survey. In Smart Secure Systems—IoT and Analytics Perspective: Second International Conference on Intelligent Information Technologies, ICIIT 2017, Chennai, India, 20–22 December 2017, Proceedings 2; Springer: Singapore, 2018; pp. 194–206. [Google Scholar]
- Xu, G. IoT-assisted ECG monitoring framework with secure data transmission for health care applications. IEEE Access 2020, 8, 74586–74594. [Google Scholar] [CrossRef]
- Hassan, R.; Qamar, F.; Hasan, M.K.; Aman AH, M.; Ahmed, A.S. Internet of Things and its applications: A comprehensive survey. Symmetry 2020, 12, 1674. [Google Scholar] [CrossRef]
- Sharma, A.; Kaur, S.; Singh, M. A comprehensive review on blockchain and Internet of Things in healthcare. Trans. Emerg. Telecommun. Technol. 2021, 32, e4333. [Google Scholar] [CrossRef]
- Khanna, A.; Kaur, S. Internet of things (IoT), applications and challenges: A comprehensive review. Wirel. Pers. Commun. 2020, 114, 1687–1762. [Google Scholar] [CrossRef]
- Salih KO, M.; Rashid, T.A.; Radovanovic, D.; Bacanin, N. A comprehensive survey on the Internet of Things with the industrial marketplace. Sensors 2022, 22, 730. [Google Scholar] [CrossRef]
- Molaei, F.; Rahimi, E.; Siavoshi, H.; Afrouz, S.G.; Tenorio, V. A comprehensive review on internet of things (IoT) and its implications in the mining industry. Am. J. Eng. Appl. Sci. 2020, 13, 499–515. [Google Scholar] [CrossRef]
- Boursianis, A.D.; Papadopoulou, M.S.; Diamantoulakis, P.; Liopa-Tsakalidi, A.; Barouchas, P.; Salahas, G.; Karagiannidis, G.; Wan, S.; Goudos, S.K. Internet of things (IoT) and agricultural unmanned aerial vehicles (UAVs) in smart farming: A comprehensive review. Internet Things 2022, 18, 100187. [Google Scholar] [CrossRef]
- Malliga, S.; Kogilavani, S.V.; Nandhini, P.S. A comprehensive review of applications of Internet of Things for COVID-19 pandemic. In IOP Conference Series: Materials Science and Engineering; IOP Publishing: Bristol, UK, 2021; Volume 1055, No. 1; p. 012083. [Google Scholar]
- Ahmid, M.; Kazar, O. A comprehensive review of the internet of things security. J. Appl. Secur. Res. 2021, 18, 289–305. [Google Scholar] [CrossRef]
- Latif, S.; Driss, M.; Boulila, W.; Huma, Z.E.; Jamal, S.S.; Idrees, Z.; Ahmad, J. Deep learning for the industrial internet of things (iiot): A comprehensive survey of techniques, implementation frameworks, potential applications, and future directions. Sensors 2021, 21, 7518. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Yu, F.R.; Zhou, L.; Yang, X.; He, Z. Applications of the Internet of Things (IoT) in smart logistics: A comprehensive survey. IEEE Internet Things J. 2020, 8, 4250–4274. [Google Scholar] [CrossRef]
- Alhasnawi, B.N.; Jasim, B.H. Internet of Things (IoT) for smart grids: A comprehensive review. J. Xi’an Univ. Arch. 2020, 63, 1006–7930. [Google Scholar]
- Heidari, A.; Jabraeil Jamali, M.A. Internet of Things intrusion detection systems: A comprehensive review and future directions. Clust. Comput. 2022, 26, 3753–3780. [Google Scholar] [CrossRef]
- Kashani, M.H.; Madanipour, M.; Nikravan, M.; Asghari, P.; Mahdipour, E. A systematic review of IoT in healthcare: Applications, techniques, and trends. J. Netw. Comput. Appl. 2021, 192, 103164. [Google Scholar] [CrossRef]
- Farahani, B.; Firouzi, F.; Chang, V.; Badaroglu, M.; Constant, N.; Mankodiya, K. Towards fog-driven IoT eHealth: Promises and challenges of IoT in medicine and healthcare. Future Gener. Comput. Syst. 2018, 78, 659–676. [Google Scholar] [CrossRef]
- Darwish, A.; Hassanien, A.E.; Elhoseny, M.; Sangaiah, A.K.; Muhammad, K. The impact of the hybrid platform of internet of things and cloud computing on healthcare systems: Opportunities, challenges, and open problems. J. Ambient Intell. Humaniz. Comput. 2019, 10, 4151–4166. [Google Scholar] [CrossRef]
- Qi, J.; Yang, P.; Min, G.; Amft, O.; Dong, F.; Xu, L. Advanced internet of things for personalised healthcare systems: A survey. Pervasive Mob. Comput. 2017, 41, 132–149. [Google Scholar] [CrossRef]
- Qi, J.; Yang, P.; Waraich, A.; Deng, Z.; Zhao, Y.; Yang, Y. Examining sensor-based physical activity recognition and monitoring for healthcare using Internet of Things: A systematic review. J. Biomed. Inform. 2018, 87, 138–153. [Google Scholar] [CrossRef]
- Dey, N.; Hassanien, A.E.; Bhatt, C.; Ashour, A.; Satapathy, S.C. (Eds.) Internet of Things and Big Data Analytics toward Next-Generation Intelligence; Springer: Berlin/Heidelberg, Germany, 2018; Volume 35. [Google Scholar]
- Quality of Experience Requirements. Available online: https://www.itu.int/pub/T-TUT-QOS-2022-1 (accessed on 19 September 2023).
- Vocabulary for Performance, Quality of Service, and Quality of Experience. Available online: https://www.itu.int/rec/T-REC-P.10 (accessed on 19 September 2023).
- Guidelines on Regulatory Aspects of Quality of Service. Available online: https://www.itu.int/rec/T-REC-E.800SerSup9/en (accessed on 19 September 2023).
- da Silva, M.P.; Gonçalves, A.L.; Dantas, M.A.R. A conceptual model for quality of experience management to provide context-aware eHealth services. Future Gener. Comput. Syst. 2019, 101, 1041–1061. [Google Scholar] [CrossRef]
- Nasralla, M.M.; Khattak SB, A.; Ur Rehman, I.; Iqbal, M. Exploring the Role of 6G Technology in Enhancing Quality of Experience for m-Health Multimedia Applications: A Comprehensive Survey. Sensors 2023, 23, 5882. [Google Scholar] [CrossRef] [PubMed]
- Ray, P.P.; Dash, D.; De, D. Internet of things-based real-time model study on e-healthcare: Device, message service and dew computing. Comput. Netw. 2019, 149, 226–239. [Google Scholar] [CrossRef]
- Bhatia, M.; Sood, S.K. A comprehensive health assessment framework to facilitate IoT-assisted smart workouts: A predictive healthcare perspective. Comput. Ind. 2017, 92, 50–66. [Google Scholar] [CrossRef]
- Vilela, P.H.; Rodrigues, J.J.; Solic, P.; Saleem, K.; Furtado, V. Performance evaluation of a Fog-assisted IoT solution for e-Health applications. Future Gener. Comput. Syst. 2019, 97, 379–386. [Google Scholar] [CrossRef]
- Ray, P.P.; Thapa, N.; Dash, D.; De, D. Novel implementation of IoT based non-invasive sensor system for real-time monitoring of intravenous fluid level for assistive e-healthcare. Circuit World 2019, 45, 109–123. [Google Scholar] [CrossRef]
- Asif-Ur-Rahman, M.; Afsana, F.; Mahmud, M.; Kaiser, M.S.; Ahmed, M.R.; Kaiwartya, O.; James-Taylor, A. Toward a heterogeneous mist, fog, and cloud-based framework for the internet of healthcare things. IEEE Internet Things J. 2018, 6, 4049–4062. [Google Scholar] [CrossRef]
- Kavitha, K.; Sharma, S.C. Performance analysis of ACO-based improved virtual machine allocation in cloud for IoT-enabled healthcare. Concurr. Comput. Pract. Exp. 2020, 32, e5613. [Google Scholar] [CrossRef]
- Stefanova-Pavlova, M.; Andonov, V.; Stoyanov, T.; Angelova, M.; Cook, G.; Klein, B.; Vassilev, P.; Stefanova, E. Modeling telehealth services with generalized nets. Recent Contrib. Intell. Syst. 2017, 657, 279–290. [Google Scholar]
- Min, M.; Wan, X.; Xiao, L.; Chen, Y.; Xia, M.; Wu, D.; Dai, H. Learning-based privacy-aware offloading for healthcare IoT with energy harvesting. IEEE Internet Things J. 2018, 6, 4307–4316. [Google Scholar] [CrossRef]
- Wang, X.; Cai, S. Secure healthcare monitoring framework integrating NDN-based IoT with edge cloud. Future Gener. Comput. Syst. 2020, 112, 320–329. [Google Scholar] [CrossRef]
- He, S.; Cheng, B.; Wang, H.; Huang, Y.; Chen, J. Proactive personalized services through fog-cloud computing in large-scale IoT-based healthcare application. China Commun. 2017, 14, 1–16. [Google Scholar] [CrossRef]
- Bharathi, R.; Abirami, T.; Dhanasekaran, S.; Gupta, D.; Khanna, A.; Elhoseny, M.; Shankar, K. Energy efficient clustering with disease diagnosis model for IoT based sustainable healthcare systems. Sustain. Comput. Inform. Syst. 2020, 28, 100453. [Google Scholar] [CrossRef]
- Kumar, P.; Silambarasan, K. Enhancing the performance of healthcare service in IoT and cloud using optimized techniques. IETE J. Res. 2022, 68, 1475–1484. [Google Scholar] [CrossRef]
- Catarinucci, L.; De Donno, D.; Mainetti, L.; Palano, L.; Patrono, L.; Stefanizzi, M.L.; Tarricone, L. An IoT-aware architecture for smart healthcare systems. IEEE Internet Things J. 2015, 2, 515–526. [Google Scholar] [CrossRef]
- Catherwood, P.A.; Steele, D.; Little, M.; McComb, S.; McLaughlin, J. A community-based IoT personalized wireless healthcare solution trial. IEEE J. Transl. Eng. Health Med. 2018, 6, 2800313. [Google Scholar] [CrossRef]
- Qiu, T.; Liu, X.; Han, M.; Li, M.; Zhang, Y. SRTS: A self-recoverable time synchronization for sensor networks of healthcare IoT. Comput. Netw. 2017, 129, 481–492. [Google Scholar] [CrossRef]
- Almobaideen, W.; Krayshan, R.; Allan, M.; Saadeh, M. Internet of Things: Geographical Routing based on healthcare centers vicinity for mobile smart tourism destination. Technol. Forecast. Soc. Chang. 2017, 123, 342–350. [Google Scholar] [CrossRef]
- Woo, M.W.; Lee, J.; Park, K. A reliable IoT system for personal healthcare devices. Future Gener. Comput. Syst. 2018, 78, 626–640. [Google Scholar] [CrossRef]
- Sood, S.K.; Mahajan, I. IoT-fog-based healthcare framework to identify and control hypertension attack. IEEE Internet Things J. 2018, 6, 1920–1927. [Google Scholar] [CrossRef]
- Verma, P.; Sood, S.K.; Kalra, S. Cloud-centric IoT based student healthcare monitoring framework. J. Ambient Intell. Humaniz. Comput. 2018, 9, 1293–1309. [Google Scholar] [CrossRef]
- Ullah, F.; Habib, M.A.; Farhan, M.; Khalid, S.; Durrani, M.Y.; Jabbar, S. Semantic interoperability for big-data in heterogeneous IoT infrastructure for healthcare. Sustain. Cities Soc. 2017, 34, 90–96. [Google Scholar] [CrossRef]
- Ali, F.; Islam, S.R.; Kwak, D.; Khan, P.; Ullah, N.; Yoo, S.J.; Kwak, K.S. Type-2 fuzzy ontology–aided recommendation systems for IoT–based healthcare. Comput. Commun. 2018, 119, 138–155. [Google Scholar] [CrossRef]
- Boussada, R.; Hamdane, B.; Elhdhili, M.E.; Saidane, L.A. Privacy-preserving aware data transmission for IoT-based e-health. Comput. Netw. 2019, 162, 106866. [Google Scholar] [CrossRef]
- Elmisery, A.M.; Rho, S.; Botvich, D. A fog based middleware for automated compliance with OECD privacy principles in internet of healthcare things. IEEE Access 2016, 4, 8418–8441. [Google Scholar] [CrossRef]
- Pal, S.; Hitchens, M.; Varadharajan, V.; Rabehaja, T. Policy-based access control for constrained healthcare resources in the context of the Internet of Things. J. Netw. Comput. Appl. 2019, 139, 57–74. [Google Scholar] [CrossRef]
- Yang, Y.; Liu, X.; Deng, R.H. Lightweight break-glass access control system for healthcare Internet-of-Things. IEEE Trans. Ind. Inform. 2017, 14, 3610–3617. [Google Scholar] [CrossRef]
- Kaw, J.A.; Loan, N.A.; Parah, S.A.; Muhammad, K.; Sheikh, J.A.; Bhat, G.M. A reversible and secure patient information hiding system for IoT driven e-health. Int. J. Inf. Manag. 2019, 45, 262–275. [Google Scholar] [CrossRef]
- Abd EL-Latif, A.A.; Abd-El-Atty, B.; Abou-Nassar, E.M.; Venegas-Andraca, S.E. Controlled alternate quantum walks based privacy preserving healthcare images in internet of things. Opt. Laser Technol. 2020, 124, 105942. [Google Scholar] [CrossRef]
- Li, H.; Jing, T. A lightweight fine-grained searchable encryption scheme in fog-based healthcare IoT networks. Wirel. Commun. Mob. Comput. 2019, 2019, 1019767. [Google Scholar] [CrossRef]
- Manogaran, G.; Varatharajan, R.; Lopez, D.; Kumar, P.M.; Sundarasekar, R.; Thota, C. A new architecture of Internet of Things and big data ecosystem for secured smart healthcare monitoring and alerting system. Future Gener. Comput. Syst. 2018, 82, 375–387. [Google Scholar] [CrossRef]
- Gope, P.; Hwang, T. BSN-Care: A secure IoT-based modern healthcare system using body sensor network. IEEE Sens. J. 2015, 16, 1368–1376. [Google Scholar] [CrossRef]

| References | Advantages | Disadvantages |
|---|---|---|
| [20]/2020 | Efficient in terms of energy and battery | Lack of interoperability techniques and methods |
| [11]/2021 | Fewer maintenance costs and duplicate patient entries | Failed to identify errors in a timely manner |
| [23]/2021 | High efficiency | Lack of data collection and statistical analysis code |
| [24]/2021 | Improved decision-making skills | Not suitable for real-time deployment |
| [8]/2022 | Security solution for managing and tracking IoMT devices | Restriction imposed on execution in a real network |
| [26]/2022 | High utilization of resources | Lack of service quality |
| [32]/2022 | Scalable | Lack of data for model construction |
| [40]/2022 | Reliable approach | Not resistant to future attacks |
| [57]/2023 | High reliability and accuracy | Not tested for deployment in real time |
| Criterion | Rationale |
|---|---|
| Inclusion 1. Research that outlined the healthcare IoT explicitly | Articles that directly offered IoT-based medical management systems are sought, since this inquiry intends to determine how IoT affects those systems |
| Inclusion 2. Studies conducted by academics or professionals | This study has implications for both commercial and educational strategies |
| Inclusion 3. Published studies in the field of healthcare IoT | Healthcare IoT serves as the reference domain |
| Inclusion 4. A paper subjected to peer-review | A peer-reviewed article guarantees a particular level of consistency and has a reasonable amount of substance |
| Inclusion 5. A report written in English | For reasons of viability, articles published in languages other than English are excluded |
| Exclusion 1. Research that is exclusively published in journals | Since academics and professionals use journals more regularly to gather data and disseminate new research, conference articles, books, unpublished working papers, master’s and doctorate dissertations, and editorial notes were excluded |
| Attributes | Explanation |
|---|---|
| Response time | The reaction time of a task is the amount of time that passes between when a task is entered into the system and when it is completed. |
| Cost | The cost of running or maintaining the IoT at a particular time. |
| Flexibility | Flexibility is the ease with which IoT responds to unpredictability. |
| Scalability | The ability of an IoT system to handle a growing number of subscribers is referred to as scalability. |
| Security | Security prevents unauthorised access to or misdirection of the services provided by IoT devices’ hardware, software, or data. |
| Efficiency | Efficiency is the ratio of productive labour to IoT resources, which translates to the output-to-input ratio for a fog device. |
| Real-time | The medical system requires quick action. Real-time data production, evaluation, and monitoring are crucial for tracking critical health issues, keeping tabs on outbreaks and pathogens, and hastening the adoption of remedies before the healthcare system becomes overburdened. |
| Overhead | In addition to the immediate costs of providing an item or service, overhead also refers to the ongoing costs of running a firm. |
| Issues | Trust and privacy | [6,7,24,27,79] |
| Power management | [44] | |
| Fog computing | [4,11,26,48] | |
| Resource management | [81] | |
| Multi-objective optimization | [24] | |
| Challenges | Scalability | [67] |
| Interoperability and standardization | [77] | |
| Mobility | [4] | |
| Real testbed environment | [58,61] | |
| Trends | Blockchain | [6,7,8,19] |
| Tactile internet | [6,31] | |
| Software-defined networks | [44] | |
| Online social networks | [10,22,56,71] | |
| Big data analytics | [23,27,52] | |
| Service quality | [45,66] | |
| Internet of Nano Things | [87] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alashlam, L.; Alzubi, A. Taxonomic Exploration of Healthcare IoT: Challenges, Solutions, and Future Frontiers. Appl. Sci. 2023, 13, 12135. https://doi.org/10.3390/app132212135
Alashlam L, Alzubi A. Taxonomic Exploration of Healthcare IoT: Challenges, Solutions, and Future Frontiers. Applied Sciences. 2023; 13(22):12135. https://doi.org/10.3390/app132212135
Chicago/Turabian StyleAlashlam, Lutifa, and Ahmad Alzubi. 2023. "Taxonomic Exploration of Healthcare IoT: Challenges, Solutions, and Future Frontiers" Applied Sciences 13, no. 22: 12135. https://doi.org/10.3390/app132212135
APA StyleAlashlam, L., & Alzubi, A. (2023). Taxonomic Exploration of Healthcare IoT: Challenges, Solutions, and Future Frontiers. Applied Sciences, 13(22), 12135. https://doi.org/10.3390/app132212135






