Ergonomic Evaluation of Different Surgeon Positions for Total Knee Arthroplasty Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Configuration and Instrumentation of the Recording Space
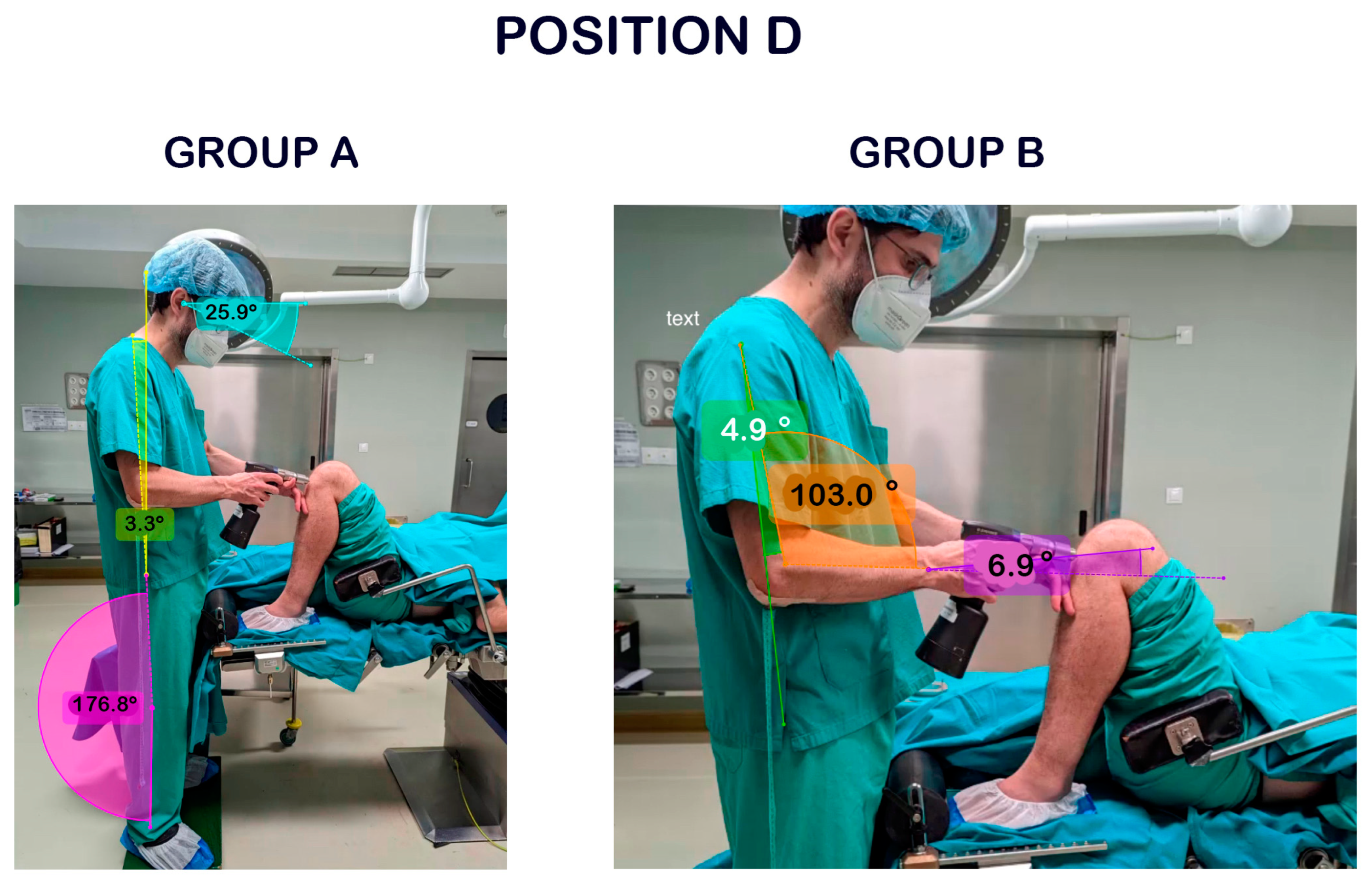
2.2. Images Capture for Angles Measurement
2.3. Rapid Entire Body Assessment (REBA)
2.4. Kinovea and REBA Observers’ Agreement
- (A)
- To define the measurement points for the angles (cervical tilt, trunk, legs, arm, forearm, and wrist);
- (B)
- To take into account the following points for the REBA application:
- (1)
- To measure the most unfavourable posture in each step, with measurements always being taken on the working arm at each step;
- (2)
- To consider that the trunk is upright if it is <5° and that the wrist is deviated if it is >15°;
- (3)
- To consider that the neck and trunk are rotated if they are not directed to where the feet are looking;
- (4)
- To consider that the arm is in internal rotation if the hand is not placed in the same line as the elbow but more to the body’s centre;
- (5)
- To apply the static-posture correction factor in all steps;
- (6)
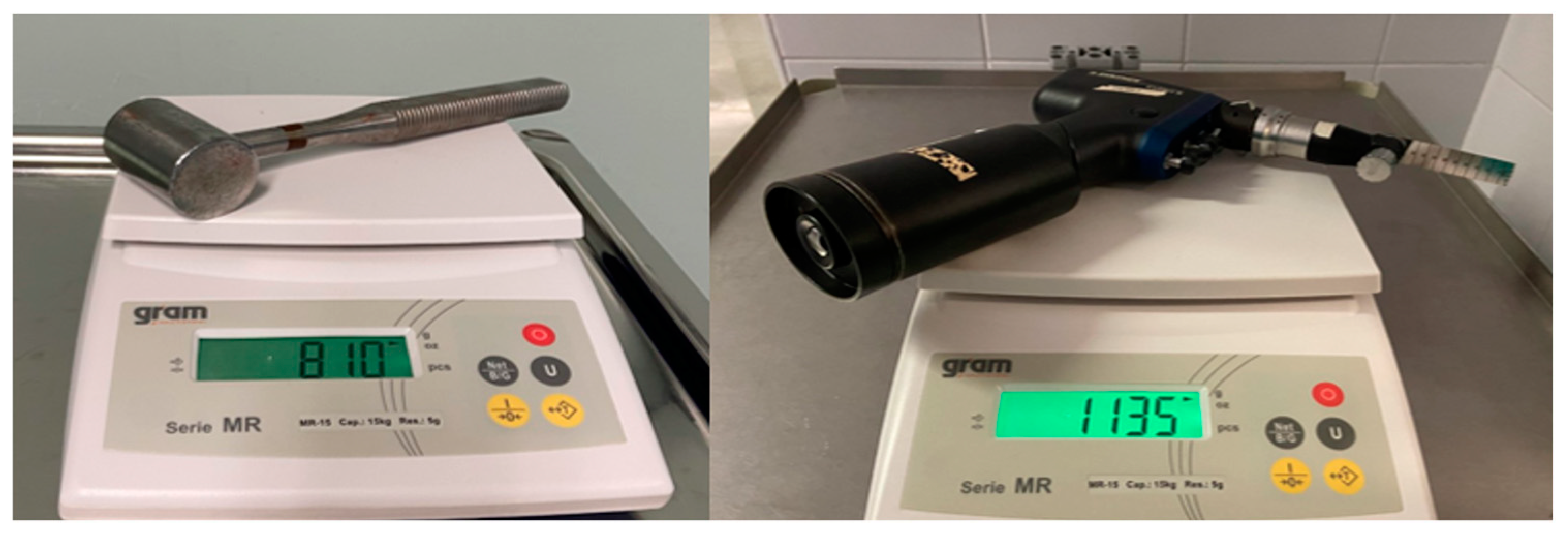
- To apply the repetitive-action correction factor in steps where a saw or a hammer is used, i.e., bone cutting or implantation of prosthetic material is performed;
- (7)
- To consider the neutral wrist angle since grasping the instruments does not require flexion or extension of the wrist. However, the need for lateral wrist deviation was considered a correction factor, depending on the activity and position of the surgeon.
2.5. Data Analysis
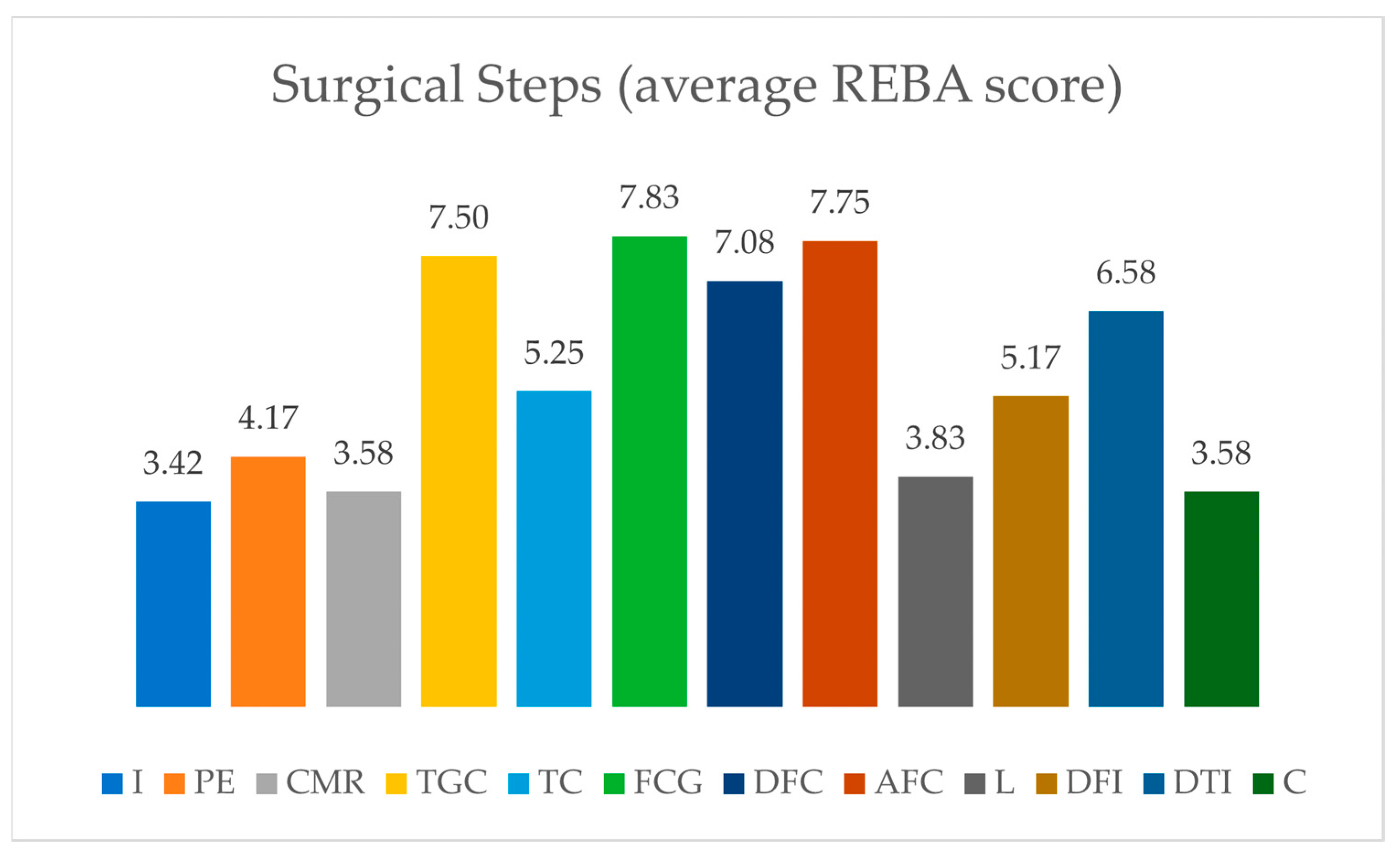
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McQuivey, K.S.; Deckey, D.G.; Christopher, Z.K.; Rosenow, C.S.; Mi, L.; Spangehl, M.J.; Bingham, J.S. Surgical Ergonomics and Musculoskeletal Pain in Orthopaedic Surgery Residents: A Multicenter Survey Study. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2021, 5, e20.00119. [Google Scholar] [CrossRef] [PubMed]
- McQuivey, K.S.; Christopher, Z.K.; Deckey, D.G.; Mi, L.; Bingham, J.S.; Spangehl, M.J. Surgical Ergonomics and Musculoskeletal Pain in Arthroplasty Surgeons. J. Arthroplast. 2021, 36, 3781–3787.e7. [Google Scholar] [CrossRef] [PubMed]
- AlQahtani, S.M.; Alzahrani, M.M.; Harvey, E.J. Prevalence of musculoskeletal disorders among orthopedic trauma surgeons: An OTA survey. Can. J. Surg. 2016, 59, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, S.M.; Alzahrani, M.M.; Tanzer, M. Adult Reconstructive Surgery: A High-Risk Profession for Work-Related Injuries. J. Arthroplast. 2016, 31, 1194–1198. [Google Scholar] [CrossRef] [PubMed]
- Aaron, K.A.; Vaughan, J.; Gupta, R.; Ali, N.-E.-S.; Beth, A.H.; Moore, J.M.; Ma, Y.; Ahmad, I.; Jackler, R.K.; Vaisbuch, Y. The risk of ergonomic injury across surgical specialties. PLoS ONE 2021, 16, e0244868. [Google Scholar] [CrossRef]
- Alaqeel, M.; Tanzer, M. Improving ergonomics in the operating room for orthopaedic surgeons in order to reduce work-related musculoskeletal injuries. Ann. Med. Surg. 2020, 56, 133–138. [Google Scholar] [CrossRef]
- Schlussel, A.T.; Maykel, J.A. Ergonomics and Musculoskeletal Health of the Surgeon. Clin. Colon Rectal Surg. 2019, 32, 424–434. [Google Scholar] [CrossRef]
- Neumann, J.; Angrick, C.; Höhn, C.; Zajonz, D.; Ghanem, M.; Roth, A.; Neumuth, T. Surgical workflow simulation for the design and assessment of operating room setups in orthopedic surgery. BMC Med. Inform. Decis. Mak. 2020, 20, 145. [Google Scholar] [CrossRef]
- Alzahrani, M.M.; Alqahtani, S.M.; Tanzer, M.; Hamdy, R.C. Musculoskeletal disorders among orthopedic pediatric surgeons: An overlooked entity. J. Child. Orthop. 2016, 10, 461–466. [Google Scholar] [CrossRef]
- Al-Mohrej, O.A.; Elshaer, A.K.; Al-Dakhil, S.S.; Sayed, A.I.; Aljohar, S.; AlFattani, A.A.; Alhussainan, T.S. Work-related musculoskeletal disorders among Saudi orthopedic surgeons: A cross-sectional study. Bone Jt. Open 2020, 1, 47–54. [Google Scholar] [CrossRef]
- Cohen-Rosenblum, A.R.; Varady, N.H.; Leonovicz, O.; Chen, A.F. Repetitive Musculoskeletal Injuries: A Survey of Female Adult Reconstruction Surgeons. J. Arthroplast. 2022, 37, 1474–1477.e6. [Google Scholar] [CrossRef] [PubMed]
- Ceyhan, E.; İnci, F.; Koçak, C.; Yavuz, İ.; Tirin, H.; Harput, G.; Gürhan, U. Why is left total knee arthroplasty surgery harder for right-handed orthopedic surgeons? Side analysis in total knee arthroplasty. Kırıkkale Üniversitesi Tıp Fakültesi Derg. 2020, 22, 357–364. [Google Scholar] [CrossRef]
- Prótesis de Rodilla: Número de Operaciones por Países 2020. Available online: https://es.statista.com/estadisticas/634751/numero-de-protesis-de-rodilla-colocadas-en-paises-de-la-ocde/ (accessed on 27 December 2022).
- Puig-Diví, A.; Escalona-Marfil, C.; Padullés-Riu, J.M.; Busquets, A.; Padullés-Chando, X.; Marcos-Ruiz, D. Validity and reliability of the Kinovea program in obtaining angles and distances using coordinates in 4 perspectives. PLoS ONE 2019, 14, e0216448. [Google Scholar] [CrossRef] [PubMed]
- Hignett, S.; McAtamney, L. Rapid Entire Body Assessment (REBA). Appl. Ergon. 2000, 31, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Seagull, F.J. Disparities between industrial and surgical ergonomics. Work 2012, 41 (Suppl. 1), 4669–4672. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Chen, Y.-L. An optimal effective working height for hammering tasks. Work 2018, 61, 181–187. [Google Scholar] [CrossRef]
- Cockburn, M.; Schick, M.; Maffiuletti, N.A.; Gygax, L.; Savary, P.; Umstätter, C. Lower working heights decrease contraction intensity of shoulder muscles in a herringbone 30° milking parlor. J. Dairy Sci. 2017, 100, 4914–4925. [Google Scholar] [CrossRef]
- Pekkarinen, A.; Anttonen, H. The effect of working height on the loading of the muscular and skeletal systems in the kitchens of workplace canteens. Appl. Ergon. 1988, 19, 306–308. [Google Scholar] [CrossRef]
- Dairywala, M.I.; Gupta, S.; Salna, M.; Nguyen, T.C. Surgeon Strength: Ergonomics and Strength Training in Cardiothoracic Surgery. Semin. Thorac. Cardiovasc. Surg. 2022, 34, 1220–1229. [Google Scholar] [CrossRef] [PubMed]
- Catanzarite, T.; Tan-Kim, J.; Whitcomb, E.L.; Menefee, S. Ergonomics in Surgery: A Review. Female Pelvic Med. Reconstr. Surg. 2018, 24, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Manasnayakorn, S.; Cuschieri, A.; Hanna, G.B. Ergonomic assessment of optimum operating table height for hand-assisted laparoscopic surgery. Surg. Endosc. 2009, 23, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Berquer, R.; Smith, W.D.; Davis, S. An ergonomic study of the optimum operating table height for laparoscopic surgery. Surg. Endosc. 2002, 16, 416–421. [Google Scholar] [CrossRef]
- Park, A.E.; Zahiri, H.R.; Hallbeck, M.S.; Augenstein, V.; Sutton, E.; Yu, D.; Lowndes, B.R.; Bingener, J. Intraoperative “Micro Breaks” with Targeted Stretching Enhance Surgeon Physical Function and Mental Focus: A Multicenter Cohort Study. Ann. Surg. 2017, 265, 340–346. [Google Scholar] [CrossRef]
- Elzomor, A.; Tunkel, A.; Lee, E.; Jaamour, F.; Davidson, L.; Shaver, T.B.; Niermeyer, W.; Benito, D.; Cole, K.; Zapanta, P. Intraoperative stretching microbreaks reduce surgery-related musculoskeletal pain in otolaryngologists. Am. J. Otolaryngol. 2022, 43, 103594. [Google Scholar] [CrossRef]
- Winters, J.N.; Sommer, N.Z.; Romanelli, M.R.; Marschik, C.; Hulcher, L.; Cutler, B.J. Stretching and Strength Training to Improve Postural Ergonomics and Endurance in the Operating Room. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2810. [Google Scholar] [CrossRef]
- Khan, W.F.; Krishna, A.; Roy, A.; Prakash, O.; Jaryal, A.K.; Deepak, K.K.; Bhattacharjee, H.; Sreenivas, V.; Bansal, V.K. Effect of structured training in improving the ergonomic stress in laparoscopic surgery among general surgery residents. Surg. Endosc. 2021, 35, 4825–4833. [Google Scholar] [CrossRef]
- Jensen, M.J.; Liao, J.; Van Gorp, B.; Sugg, S.L.; Shelton, J.; Corwin, C.; Lal, G. Incorporating Surgical Ergonomics Education into Surgical Residency Curriculum. J. Surg. Educ. 2021, 78, 1209–1215. [Google Scholar] [CrossRef]
- Epstein, S.; Tran, B.N.; Capone, A.C.; Ruan, Q.Z.; Fukudome, E.Y.; Ricci, J.A.; Testa, M.A.; Dennerlein, J.T.; Lee, B.T.; Singhal, D. The Current State of Surgical Ergonomics Education in U.S. Surgical Training: A Survey Study. Ann. Surg. 2019, 269, 778–784. [Google Scholar] [CrossRef]
- Epstein, S.; Sparer, E.H.; Tran, B.N.; Ruan, Q.Z.; Dennerlein, J.T.; Singhal, D.; Lee, B.T. Prevalence of Work-Related Musculoskeletal Disorders among Surgeons and Interventionalists: A Systematic Review and Meta-analysis. JAMA Surg. 2018, 153, e174947. [Google Scholar] [CrossRef] [PubMed]


| Score | Risk Level | Level of Preventive Action |
|---|---|---|
| 1 | Negligible | Non-necessary |
| 2–3 | Low | May be necessary |
| 4–7 | Medium | Necessary |
| 8–10 | High | Necessary with priority |
| 11–15 | Very high | Necessary NOW |
| Kinovea Angles | Observer 1.1 * | Observer 1.2 | Observer 2 | Wilcoxon Obs. 1.1 vs. Obs. 2 |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Position A | 61.93 (63.29) | 62.56 (63.57) | 61.83 (63.1) | 0.559 |
| Position B | 59.85 (64.39) | 59.91 (64.84) | 56.28 (61.9) | 0.016 |
| Position C | 60.81 (65.26) | 61.28 (64.98) | 59.8 (63.66) | 0.12 |
| Position D | 59.14 (65.82) | 56.6 (64.9) | 54.71 (64.54) | 0.002 |
| Kinovea Angles | ICC (2,1) Test–Retest Reliability (95% CI) | ICC (2,1) Inter-Rater Analysis (95% CI) |
|---|---|---|
| Position A | 0.996 (0.994–0.998) | 0.995 (0.991–0.997) |
| Position B | 0.996 (0.994–0.997) | 0.977 (0.963–0.986) |
| Position C | 0.996 (0.994–0.997) | 0.994 (0.991–0.997) |
| Position D | 0.946 (0.915–0.966) | 0.943 (0.909–0.964) |
| REBA Scores | Observer 1.1 * | Observer 1.2 | Observer 2 | Wilcoxon Obs. 1.1 vs. Obs. 2 | |
|---|---|---|---|---|---|
| Position A | Mean (SD) | 7 (2.33) | 6.58 (1.97) | 6.5 (2.23) | 0.107 |
| Kappa | Test–retest: 0.804 | Interobserver: 0.943 | |||
| Position B | Mean (SD) | 6.17 (2.58) | 6.17 (2.552) | 5.5 (2.505) | 0.033 |
| Kappa | Test–retest: 0.801 | Interobserver: 0.885 | |||
| Position C | Mean (SD) | 5.67 (2.015) | 5.92 (2.151) | 5.5 (1.931) | 0.317 |
| Kappa | Test–retest: 0.776 | Interobserver: 0.858 | |||
| Position D | Mean (SD) | 3.58 (1.24) | 3.75 (1.545) | 3.42 (1.311) | 0.48 |
| Kappa | Test–retest: 1 | Interobserver: 0.62 |
| REBA Score | ICC (2,1) Test–Retest Reliability (95% CI) | ICC (2,1) Inter-Rater Analysis (95% CI) |
|---|---|---|
| Position A | 0.814 (0.492–0.942) | 0.89 (0.657–0.967) |
| Position B | 0.962 (0.873–0.989) | 0.913 (0.614–0.977) |
| Position C | 0.971 (0.892–0.992) | 0.957 (0.865–0.987) |
| Position D | 0.915 (0.743–0.974) | 0.793 (0.436–0.935) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-Robles, M.; Díaz-Martínez, F.J.; León-Muñoz, V.J.; Marín-Martínez, C.; Murcia-Asensio, A.; Moreno-Cascales, M.; Lajara-Marco, F. Ergonomic Evaluation of Different Surgeon Positions for Total Knee Arthroplasty Surgery. Appl. Sci. 2023, 13, 11842. https://doi.org/10.3390/app132111842
Sánchez-Robles M, Díaz-Martínez FJ, León-Muñoz VJ, Marín-Martínez C, Murcia-Asensio A, Moreno-Cascales M, Lajara-Marco F. Ergonomic Evaluation of Different Surgeon Positions for Total Knee Arthroplasty Surgery. Applied Sciences. 2023; 13(21):11842. https://doi.org/10.3390/app132111842
Chicago/Turabian StyleSánchez-Robles, Marina, Francisco J. Díaz-Martínez, Vicente J. León-Muñoz, Carmelo Marín-Martínez, Antonio Murcia-Asensio, Matilde Moreno-Cascales, and Francisco Lajara-Marco. 2023. "Ergonomic Evaluation of Different Surgeon Positions for Total Knee Arthroplasty Surgery" Applied Sciences 13, no. 21: 11842. https://doi.org/10.3390/app132111842
APA StyleSánchez-Robles, M., Díaz-Martínez, F. J., León-Muñoz, V. J., Marín-Martínez, C., Murcia-Asensio, A., Moreno-Cascales, M., & Lajara-Marco, F. (2023). Ergonomic Evaluation of Different Surgeon Positions for Total Knee Arthroplasty Surgery. Applied Sciences, 13(21), 11842. https://doi.org/10.3390/app132111842








