Dry Needling versus Diacutaneous Fibrolysis for the Treatment of the Mechanical Properties of the Teres Major Muscle: A Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
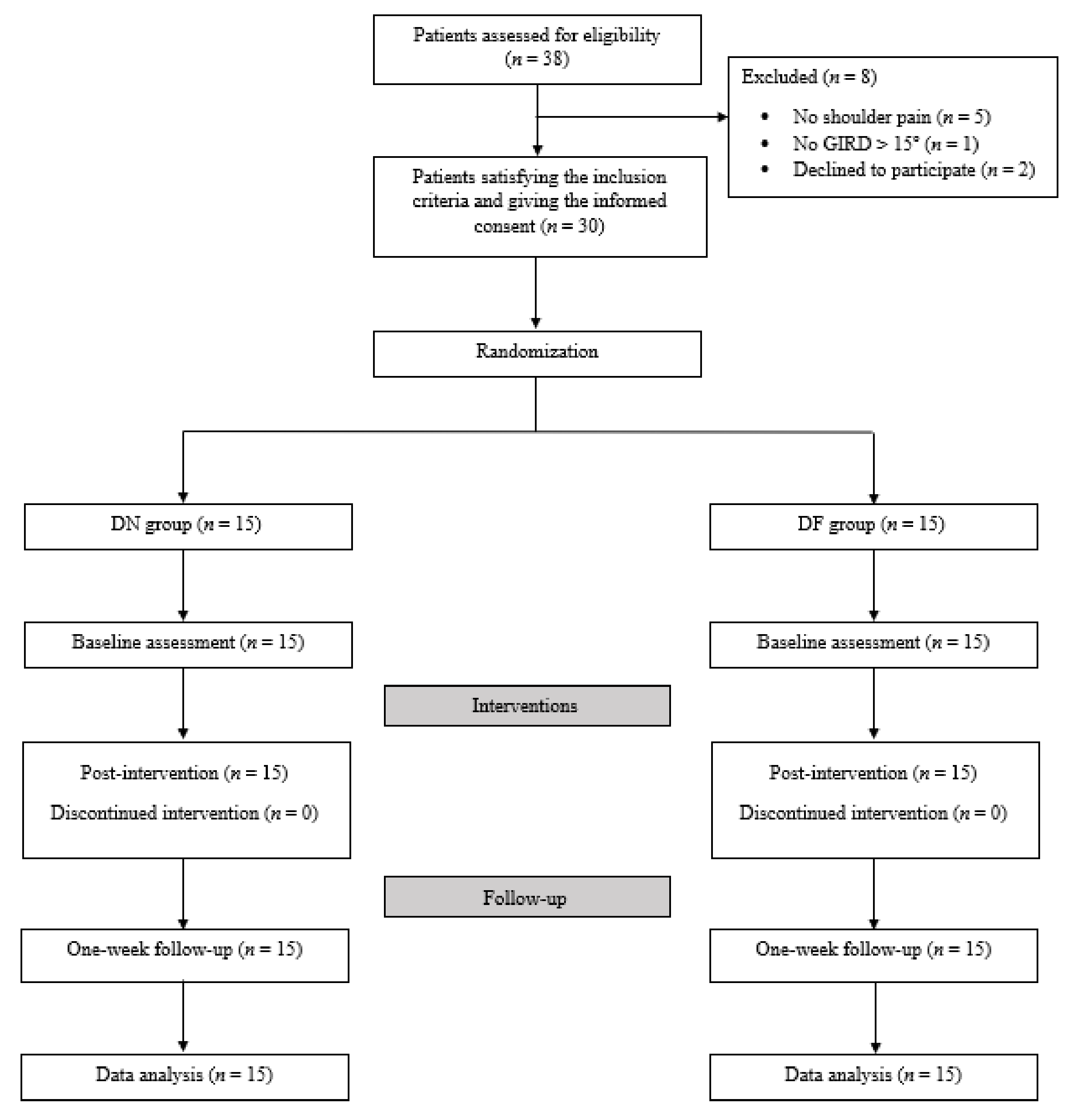
2.1. Study Design
2.2. Sample Size
2.3. Participants
2.4. Allocation and Blinding
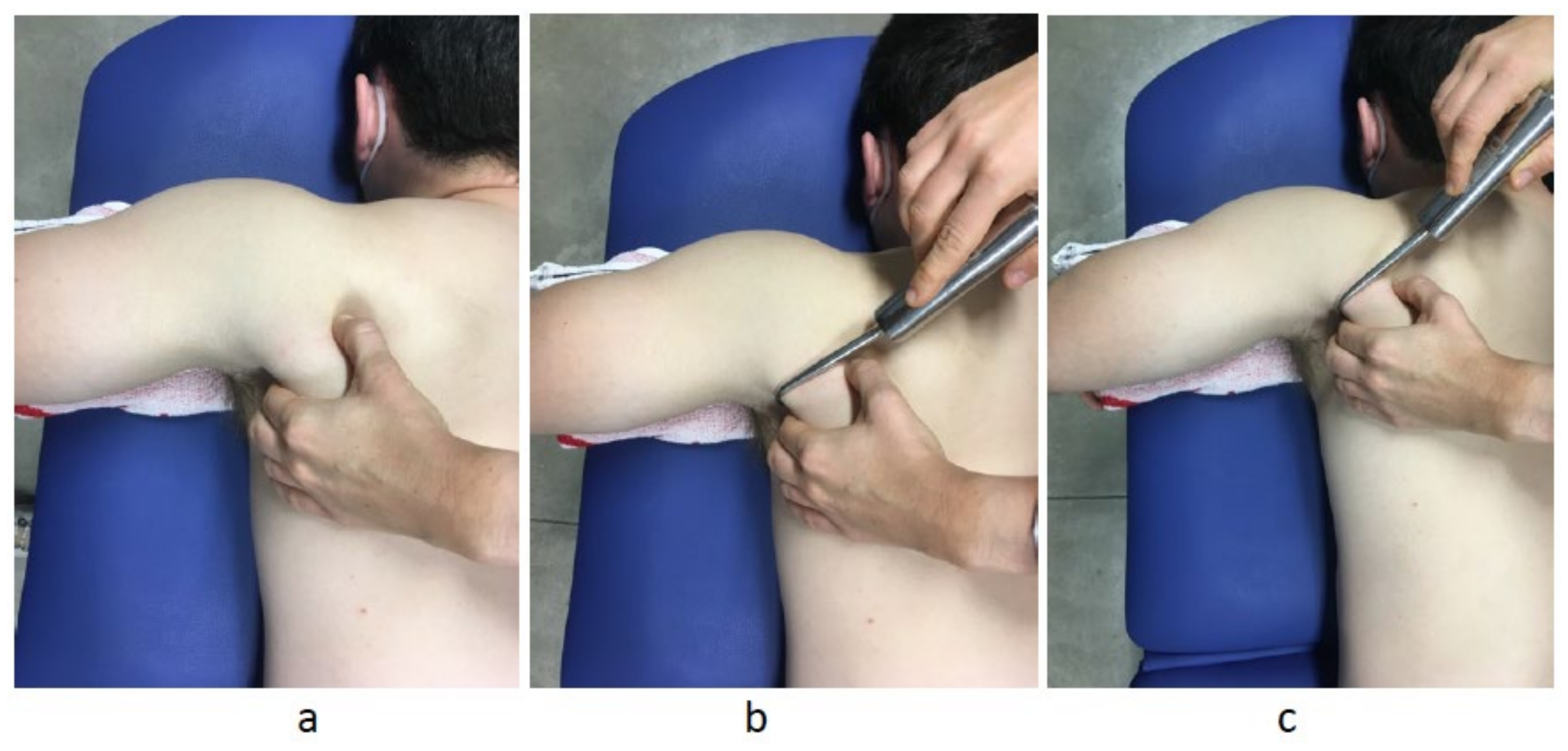
2.5. Interventions
2.6. Outcomes and Measurement Instruments
2.6.1. Mechanical Properties of the Teres Major Muscle
2.6.2. Pain Intensity
2.6.3. ROM
2.6.4. Posterior Shoulder Muscle Extensibility
2.7. Reliability of the Measures
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raya-González, J.; Clemente, F.M.; Beato, M.; Castillo, D. Injury profile of male and female senior and youth handball players: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 3925. [Google Scholar] [CrossRef]
- Ceballos-Laita, L.; Pérez-Manzano, A.; Mingo-Gómez, T.; Hernando-Garijo, I.; Medrano-De-La-Fuente, R.; Estébanez-de-Miguel, E.; Jiménez-del-Barrio, S. Range of motion and muscle function on shoulder joints of young handball athletes. J. Back Musculoskelet. Rehabil. 2021, 35, 161–167. [Google Scholar] [CrossRef]
- Wilk, K.E.; MacRina, L.C.; Fleisig, G.S.; Porterfield, R.; Simpson, C.D.; Harker, P.; Paparesta, N.; Andrews, J.R. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am. J. Sports Med. 2011, 39, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, S.S.; Morgan, C.D.; Kibler, W.B. The disabled throwing shoulder: Spectrum of pathology Part I: Pathoanatomy and biomechanics. Arthrosc. J. Arthrosc. Relat. Surg. 2003, 19, 404–420. [Google Scholar] [CrossRef]
- Burkhart, S.S.; Morgan, C.D.; Kibler, W.B. The disabled throwing shoulder: Spectrum of Pathology Part II: Evaluation and treatment of SLAP lesions in throwers. Arthrosc. J. Arthrosc. Relat. Surg. 2003, 19, 531–539. [Google Scholar] [CrossRef]
- Almeida, G.P.L.; Silveira, P.F.; Rosseto, N.P.; Barbosa, G.; Ejnisman, B.; Cohen, M. Glenohumeral range of motion in handball players with and without throwing-related shoulder pain. J. Shoulder Elb. Surg. 2013, 22, 602–607. [Google Scholar] [CrossRef]
- Ceballos-Laita, L.; Medrano-De-la-fuente, R.; Estébanez-De-miguel, E.; Moreno-Cerviño, J.; Mingo-Gómez, M.T.; Hernando-Garijo, I.; Jiménez-Del-barrio, S. Effects of dry needling in teres major muscle in elite handball athletes. A randomised controlled trial. J. Clin. Med. 2021, 10, 4260. [Google Scholar] [CrossRef] [PubMed]
- Fieseler, G.; Jungermann, P.; Koke, A.; Irlenbusch, L.; Delank, K.S.; Schwesig, R. Range of motion and isometric strength of shoulder joints of team handball athletes duringthe playing season, part II: Changes after midseason. J. Shoulder Elb. Surg. 2015, 24, 391–398. [Google Scholar] [CrossRef]
- Fieseler, G.; Jungermann, P.; Koke, A.; Irlenbusch, L.; Delank, K.S.; Schwesig, R. Glenohumeral range of motion (ROM) and isometric strength of professional team handball athletes, part III: Changes over the playing season. Arch. Orthop. Trauma Surg. 2015, 135, 1691–1700. [Google Scholar] [CrossRef]
- Barra-López, M.E.; López-de-Celis, C.; Pérez-Bellmunt, A.; Puyalto-de-Pablo, P.; Sánchez-Fernández, J.J.; Lucha-López, M.O. The supporting role of the teres major muscle, an additional component in glenohumeral stability? An anatomical and radiological study. Med. Hypotheses 2020, 141, 109728. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-del-Barrio, S.; Jiménez-Rejano, J.J.; Rebollo-Salas, M.; Mingo-Gómez, M.T.; Lorenzo-Muñoz, A.; Ceballos-Laita, L. Increased Tone and Stiffness of the Teres Major Muscle in Elite Handball Athletes: A Cross-Sectional Study. Appl. Sci. 2023, 13, 8457. [Google Scholar] [CrossRef]
- Barra López, M.E.; López de Celis, C.; Fernández Jentsch, G.; Raya de Cárdenas, L.; Lucha López, M.O.; Tricás Moreno, J.M. Effectiveness of Diacutaneous Fibrolysis for the treatment of subacromial impingement syndrome: A randomised controlled trial. Man. Ther. 2013, 18, 418–424. [Google Scholar] [CrossRef]
- Barra, M.E.; López, C.; Fernández, G.; Murillo, E.; Villar, E.; Raya, L. The immediate effects of diacutaneous fibrolysis on pain and mobility in patients suffering from painful shoulder: A randomized placebo-controlled pilot study. Clin. Rehabil. 2011, 25, 339–348. [Google Scholar] [CrossRef]
- López-de-Celis, C.; Barra-López, M.-E.; González-Rueda, V.; Bueno-Gracia, E.; Rodríguez-Rubio, P.-R.; Tricás-Moreno, J.-M. Effectiveness of diacutaneous fibrolysis for the treatment of chronic lateral epicondylalgia: A randomized clinical trial. Clin. Rehabil. 2018, 32, 644–653. [Google Scholar] [CrossRef] [PubMed]
- Arias-Buría, J.L.; Fernández-de-las-Peñas, C.; Palacios-Ceña, M.; Koppenhaver, S.L.; Salom-Moreno, J. Exercises and Dry Needling for Subacromial Pain Syndrome: A Randomized Parallel-Group Trial. J. Pain 2017, 18, 11–18. [Google Scholar] [CrossRef]
- Calvo-Lobo, C.; Pacheco-Da-Costa, S.; Martínez-Martínez, J.; Rodríguez-Sanz, D.; Cuesta-Álvaro, P.; López-López, D. Dry Needling on the Infraspinatus Latent and Active Myofascial Trigger Points in Older Adults with Nonspecific Shoulder Pain: A Randomized Clinical Trial. J. Geriatr. Phys. Ther. 2018, 41, 1–13. [Google Scholar] [CrossRef]
- Arias-Buría, J.L.; Valero-Alcaide, R.; Cleland, J.A.; Salom-Moreno, J.; Ortega-Santiago, R.; Atín-Arratibel, M.A.; Fernández-De-Las-Peñas, C. Inclusion of trigger point dry needling in a multimodal physical therapy program for postoperative shoulder pain: A randomized clinical trial. J. Manip. Physiol. Ther. 2015, 38, 179–187. [Google Scholar] [CrossRef]
- Navarro-santana, M.J.; Gómez-Chiguano, G.F.; Cleland, J.A.; Arias-Buria, J.L.; Fernández-de-las-Peñas, C.; Plaza-manzano, G. Effects of Trigger Point Dry Needling for Nontraumatic Shoulder Pain of Musculoskeletal Origin: A Systematic Review and Meta-Analysis. Phys. Ther. Rehabil. J. 2020, 101, pzaa216. [Google Scholar] [CrossRef]
- Isabel de-la-Llave-Rincón, A.; Puentedura, E.J.; Fernández-de-las-Peñas, C. Clinical presentation and manual therapy for upper quadrant musculoskeletal conditions. J. Man. Manip. Ther. 2011, 19, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Dommerholt, J.; Mayoral del Moral, O.; Gröbli, C. Trigger Point Dry Needling. J. Man. Manip. Ther. 2006, 14, 70E–87E. [Google Scholar] [CrossRef]
- López-De-Celis, C.; Pérez-Bellmunt, A.; Bueno-Gracia, E.; Fanlo-Mazas, P.; Zárate-Tejero, C.A.; Llurda-Almuzara, L.; Arróniz, A.C.; Rodriguez-Rubio, P.R. Effect of diacutaneous fibrolysis on the muscular properties of gastrocnemius muscle. PLoS ONE 2020, 15, e243225. [Google Scholar] [CrossRef]
- Sánchez-Infante, J.; Bravo-Sánchez, A.; Jiménez, F.; Abián-Vicén, J. Effects of dry needling on mechanical and contractile properties of the upper trapezius with latent myofascial trigger points: A randomized controlled trial. Musculoskelet. Sci. Pract. 2021, 56, 102456. [Google Scholar] [CrossRef]
- Simons, D.; Travell, J.G.; Simons, L. Myofascial Pain and Dysfunction: The Trigger Point Manual, 2nd ed.; Editorial Panamericana: Madrid, Spain, 2007. [Google Scholar]
- Hong, C.; Torigoe, Y. Electrophysiological characteristics of localized twitch responses in responsive taut bands of rabbit skeletal muscle fibers. J. Musculoskelet. Pain 1994, 2, 17–43. [Google Scholar] [CrossRef]
- Hong, C.Z.; Torigoe, Y. The localized twitch responses in responsive taut bands of rabbit skeletal muscle fibers are related to the reflexes at spinal cord level. J. Musculoskelet. Pain 1995, 3, 15–33. [Google Scholar] [CrossRef]
- Ceballos-Laita, L.; Jiménez-del-Barrio, S.; Marín-Zurdo, J.; Moreno-Calvo, A.; Marín-Boné, J.; Albarova-Corral, M.I.; Estébanez-de-Miguel, E. Effectiveness of Dry Needling Therapy on Pain, Hip Muscle Strength and Physical Function in Patients With Hip Osteoarthritis: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2021, 102, 959–966. [Google Scholar] [CrossRef]
- Ditroilo, M.; Hunter, A.M.; Haslam, S.; De Vito, G. The effectiveness of two novel techniques in establishing the mechanical and contractile responses of biceps femoris. Physiol. Meas. 2011, 32, 1315–1326. [Google Scholar] [CrossRef]
- Llurda-Almuzara, L.; Pérez-Bellmunt, A.; López-de-Celis, C.; Aiguadé, R.; Seijas, R.; Casasayas-Cos, O.; Labata-Lezaun, N.; Alvarez, P. Normative data and correlation between dynamic knee valgus and neuromuscular response among healthy active males: A cross-sectional study. Sci. Rep. 2020, 10, 17206. [Google Scholar] [CrossRef] [PubMed]
- Aird, L.; Samuel, D.; Stokes, M. Quadriceps muscle tone, elasticity and stiffness in older males: Reliability and symmetry using the MyotonPRO. Arch. Gerontol. Geriatr. 2012, 55, e31–e39. [Google Scholar] [CrossRef]
- Tashjian, R.Z.; Deloach, J.; Porucznik, C.A.; Powell, A.P. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J. Shoulder Elb. Surg. 2009, 18, 927–932. [Google Scholar] [CrossRef]
- Laudner, K.; Compton, B.D.; McLoda, T.A.; Walters, C.M. Acute effects of instrument assisted soft tissue mobilization for improving posterior shoulder range of motion in collegiate baseball players. Int. J. Sports Phys. Ther. 2014, 9, 1–7. [Google Scholar]
- Lim, J.Y.; Kim, T.H.; Lee, J.S. Reliability of measuring the passive range of shoulder horizontal adduction using a smartphone in the supine versus the side-lying position. J. Phys. Ther. Sci. 2015, 27, 3119–3122. [Google Scholar] [CrossRef] [PubMed]
- Tyler, T.F.; Roy, T.; Nicholas, S.J.; Gleim, G.W. Reliability and validity of a new method of measuring posterior shoulder tightness. J. Orthop. Sport. Phys. Ther. 1999, 29, 262–274. [Google Scholar] [CrossRef] [PubMed]
- Tyler, T.F.; Nicholas, S.J.; Roy, T.; Gleim, G.W. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am. J. Sports Med. 2000, 28, 668–673. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Hillsdale, N., Ed.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 1988; ISBN 9781483276489. [Google Scholar]
- Mcnair, P.J.; Dombroski, E.W.; Hewson, D.J.; Stanley, S.N. Stretching at the ankle joint: Viscoelastic responses to holds and continuous passive motion. Med. Sci. Sport. Exerc. 2001, 33, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Davidoff, R.A. Skeletal muscle tone and the misunderstood stretch reflex. Neurology 1992, 42, 951–963. [Google Scholar] [CrossRef] [PubMed]
- Hung, C.J.; Hsieh, C.L.; Yang, P.L.; Lin, J.J. Relationship between posterior shoulder muscle stiffness and rotation in patients with stiff shoulder. J. Rehabil. Med. 2010, 42, 216–220. [Google Scholar] [CrossRef]
- Lluch, E.; Pecos-Martín, D.; Domenech-García, V.; Herrero, P.; Gallego-Izquierdo, T. Effects of an anteroposterior mobilization of the glenohumeral joint in overhead athletes with chronic shoulder pain: A randomized controlled trial. Musculoskelet. Sci. Pract. 2018, 38, 91–98. [Google Scholar] [CrossRef]
- Albertin, E.S.; Miley, E.N.; May, J.; Baker, R.T.; Reordan, D. Effectiveness of stretching on posterior shoulder tightness and glenohumeral internal rotation deficit: A systematic review of randomised controlled trials. J. Sport Rehabil. 2018, 29, 622–627. [Google Scholar]
- Moore, S.D.; Laudner, K.G.; Mcloda, T.A.; Shaffer, M.A. The immediate effects of muscle energy technique on posterior shoulder tightness: A randomized controlled trial. J. Orthop. Sports Phys. Ther. 2011, 41, 400–407. [Google Scholar] [CrossRef]
- Lo, C.-L.; Hsueh, Y.-H.; Wang, C.-H.; Chang, H.-Y. Comparison of the Acute Effects of Kinesio Taping and Sleeper Stretching on the Shoulder Rotation Range of Motion, Manual Muscle Strength, and Sub-Acromial Space in Pitchers with Glenohumeral Internal Rotation Deficit. Medicina 2021, 57, 102. [Google Scholar] [CrossRef]
- Gulpinar, D.; Ozer, S.T.; Yesilyaprak, S.S. Effects of rigid and kinesio taping on shoulder rotation motions, posterior shoulder tightness, and posture in overhead athletes: A randomized controlled trial. J. Sport Rehabil. 2019, 28, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Kamali, F.; Sinaei, E.; Morovati, M. Comparison of Upper Trapezius and Infraspinatus myofascial trigger point therapy by dry needling in overhead athletes with unilateral shoulder impingement syndrome. J. Sport Rehabil. 2018, 29, 622–627. [Google Scholar] [CrossRef] [PubMed]

| ICC (95% CI) | SEM | MDC | |
|---|---|---|---|
| ER ROM (°) | 0.92 (0.88, 0.95) | 2.29 | 6.35 |
| IR ROM (°) | 0.93(0.89, 0.97) | 1.83 | 5.07 |
| HA ROM (°) | 0.90 (0.83, 0.97) | 2.27 | 6.29 |
| Extensibility (°) | 0.92 (0.9, 0.94) | 2.23 | 6.19 |
| Tone (Hz) | 0.98 (0.96, 0.99) | 0.29 | 0.80 |
| Stiffness (N/m) | 0.97 (0.95, 0.98) | 8.99 | 24.91 |
| Characteristics | DN Group (n = 15) | DF Group (n = 15) | p-Value |
|---|---|---|---|
| Age (years) | 25.47 ± 4.99 | 26.20 ± 5.91 | F = 0.13 0.717 |
| Height (cm) | 184.13 ± 4.61 | 183.20 ± 7.46 | F = 0.17 0.684 |
| Weight (kg) | 85.13 ± 8.58 | 89.53 ± 15.01 | F = 0.97 0.333 |
| BMI (Kg/cm2) | 25.07 ± 1.98 | 26.50 ± 2.60 | F = 2.83 0.103 |
| Training days per week (h/w) | 4.13 ± 0.87 | 4.26 ± 0.77 | U = 105.50 0.775 |
| Months since first symptoms | 35.00 ± 24.25 | 47.33 ± 33.83 | F = 1.31 0.261 |
| Outcome | DN Group (n = 15) | DF Group (n = 15) | Between-Group Difference in Change Score | Effect Size of Difference |
|---|---|---|---|---|
| Stiffness [N/m] | ||||
| Baseline | 173.47 ± 25.50 | 173.21 ±26.60 | ||
| Postintervention change score | −18.33 ± 14.08 | −21.28 ± 16.48 | −2.95 (−14.60, 8.70) | 0.1 |
| One-week follow-up change score | −7.6 ± 34.08 | −22.57 ± 11.52 | −14.97 (−34.65, 4.71) | 0.5 |
| Tone [Hz] | ||||
| Baseline | 11.32 ±0.38 | 11.57 ±0.61 | ||
| Postintervention change score | −0.39 ± 0.37 | −0.19 ± 0.45 | 0.20 (−0.11, 0.51) | 0.4 |
| One-week follow-up change score | −0.16 ± 0.53 | −0.30 ± 0.56 | −0.13 (−0.55, 0.28) | 0.2 |
| VAS [points] | ||||
| Baseline | 4.36 ± 2.18 | 3.90 ± 2.24 | ||
| Postintervention change score | −4.36 ± 2.18 | −3.90 ± 2.24 | 0.45 (−1.22, 2.14) | 0.2 |
| One-week follow-up change score | −2.54 ± 1.63 | −2.10 ± 2.51 | 0.53 (−1.06, 2.14) | 0.2 |
| IR ROM [°] | ||||
| Baseline | 19.07 ± 6.59 | 15.79 ± 3.51 | ||
| Postintervention change score | 16.40 ± 9.25 | 15.21 ± 7.24 | −1.18 (−7.55, 5.18) | 0.1 |
| One-week follow-up change score | 13.73 ± 7.13 | 14.35 ± 6.46 | 0.63 (−4.57, 5.82) | 0.1 |
| ER ROM [°] | ||||
| Baseline | 76.67 ± 10.30 | 75.29 ± 10.48 | ||
| Postintervention change score | 7.26 ± 17.69 | 7.92 ± 10.49 | 0.66 (−10.52, 11.85) | 0.1 |
| One-week follow-up change score | 6.40 ± 17.05 | 8.28 ± 12.97 | 1.88 (−9.72, 13.49) | 0.1 |
| tROM [°] | ||||
| Baseline | 95.73 ± 11.06 | 91.07 ± 11.20 | ||
| Postintervention change score | 23.66 ± 23.25 | 23.14 ± 13.09 | −0.52 (−15.05, 14.00) | 0.1 |
| One-week follow-up change score | 20.13 ± 21.68 | 22.64 ± 15.56 | 2.50 (−11.96, 16.98) | 0.1 |
| HA ROM [°] | ||||
| Baseline | −9.93 ± 5.32 | −9.57 ± 4.40 | ||
| Postintervention change score | 14.53 ± 11.12 | 13.57 ± 6.52 | −0.96 (−7.97, 6.05) | 0.1 |
| One-week follow-up change score | 19.73 ± 9.04 | 21.00 ± 10.16 | 1.26 (−6.05, 8.58) | 0.1 |
| Extensibility [°] | ||||
| Baseline | −12.20 ± 8.36 | −10.93 ± 9.59 | ||
| Postintervention change score | 6.13 ± 6.85 | 7.37 ± 6.97 | 1.22 (−4.04, 6.49) | 0.1 |
| One-week follow-up change score | 5.80 ± 10.92 | 8.21 ± 8.34 | 2.41 (−5.03, 9.86) | 0.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceballos-Laita, L.; Jiménez-Rejano, J.J.; Rebollo-Salas, M.; Mingo-Gómez, M.T.; Hernández-Lázaro, H.; Jiménez-del-Barrio, S. Dry Needling versus Diacutaneous Fibrolysis for the Treatment of the Mechanical Properties of the Teres Major Muscle: A Randomized Clinical Trial. Appl. Sci. 2023, 13, 10995. https://doi.org/10.3390/app131910995
Ceballos-Laita L, Jiménez-Rejano JJ, Rebollo-Salas M, Mingo-Gómez MT, Hernández-Lázaro H, Jiménez-del-Barrio S. Dry Needling versus Diacutaneous Fibrolysis for the Treatment of the Mechanical Properties of the Teres Major Muscle: A Randomized Clinical Trial. Applied Sciences. 2023; 13(19):10995. https://doi.org/10.3390/app131910995
Chicago/Turabian StyleCeballos-Laita, Luis, José Jesús Jiménez-Rejano, Manuel Rebollo-Salas, María Teresa Mingo-Gómez, Héctor Hernández-Lázaro, and Sandra Jiménez-del-Barrio. 2023. "Dry Needling versus Diacutaneous Fibrolysis for the Treatment of the Mechanical Properties of the Teres Major Muscle: A Randomized Clinical Trial" Applied Sciences 13, no. 19: 10995. https://doi.org/10.3390/app131910995
APA StyleCeballos-Laita, L., Jiménez-Rejano, J. J., Rebollo-Salas, M., Mingo-Gómez, M. T., Hernández-Lázaro, H., & Jiménez-del-Barrio, S. (2023). Dry Needling versus Diacutaneous Fibrolysis for the Treatment of the Mechanical Properties of the Teres Major Muscle: A Randomized Clinical Trial. Applied Sciences, 13(19), 10995. https://doi.org/10.3390/app131910995






