Oral Health Literacy Levels of Nursing Professionals and Effectiveness of Integrating Oral Health Training into Nursing Curricula: A Systematic Review
Abstract
1. Introduction
- To understand the knowledge and attitudes of nursing professionals towards providing oral healthcare.
- To understand the perceived barriers towards oral healthcare promotion. Additionally, the general practices related to oral care and practice were explored.
- To identify the existing trainings and resources, understand the perception towards incorporating oral health training into nursing curricula, and determine the effectiveness of integrating oral health training into the training of nursing professionals.
2. Methods
2.1. Literature Search
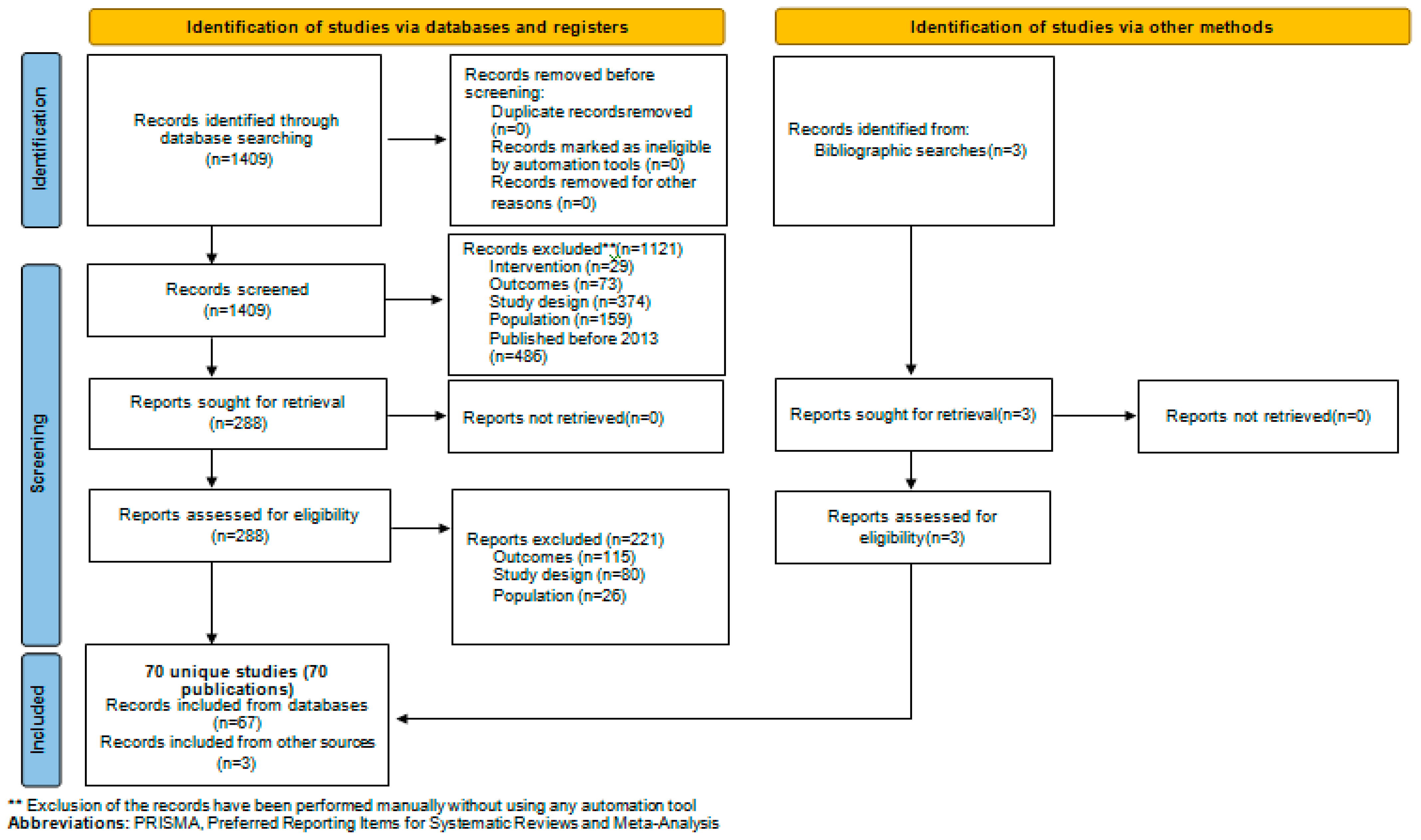
2.2. PRISMA Protocol (Study Selection and Data Extraction)
2.3. Quality Assessment of the Included Studies and Two-Step Review
3. Results
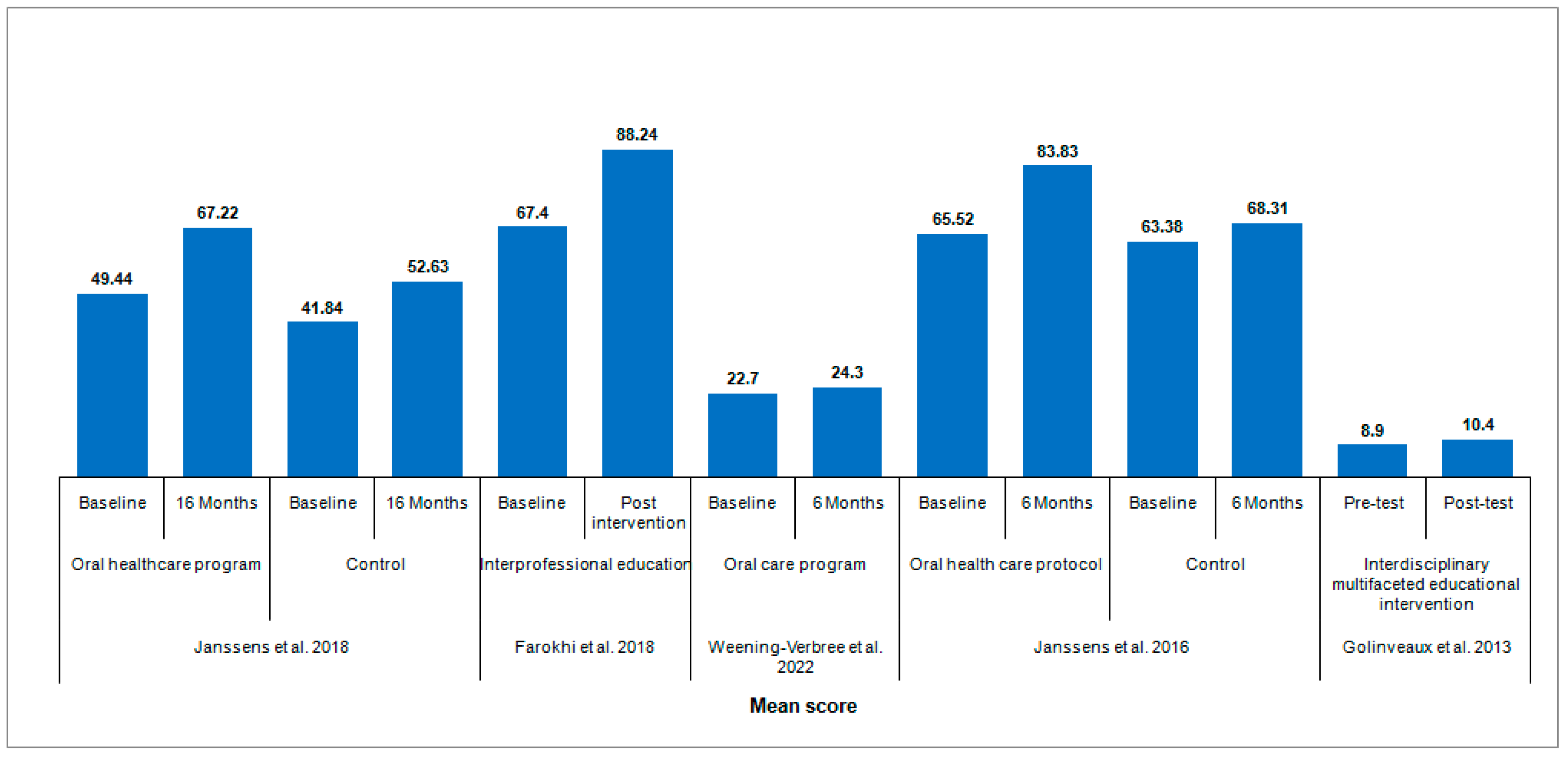
3.1. Knowledge of Oral Healthcare among Nursing Professionals
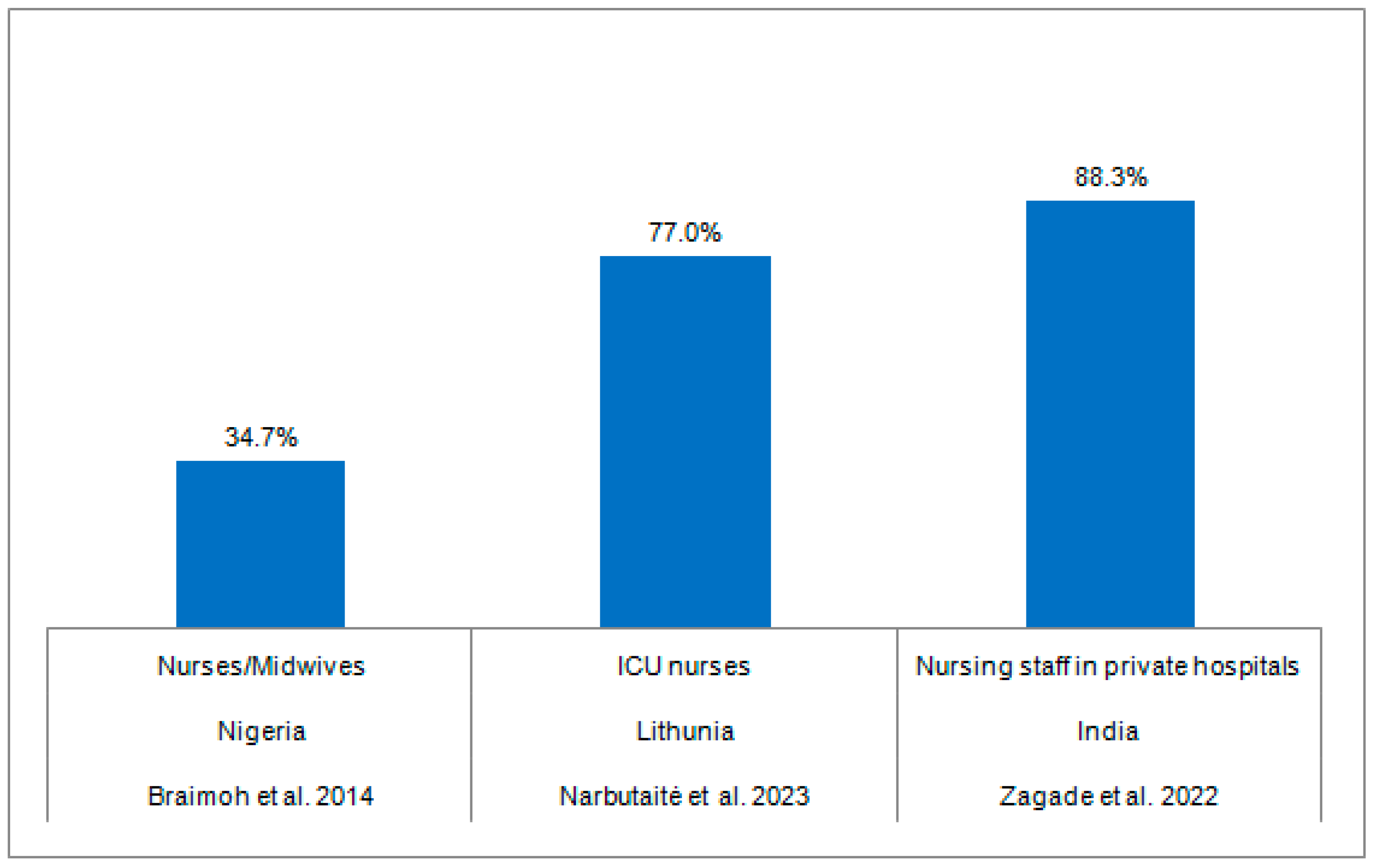
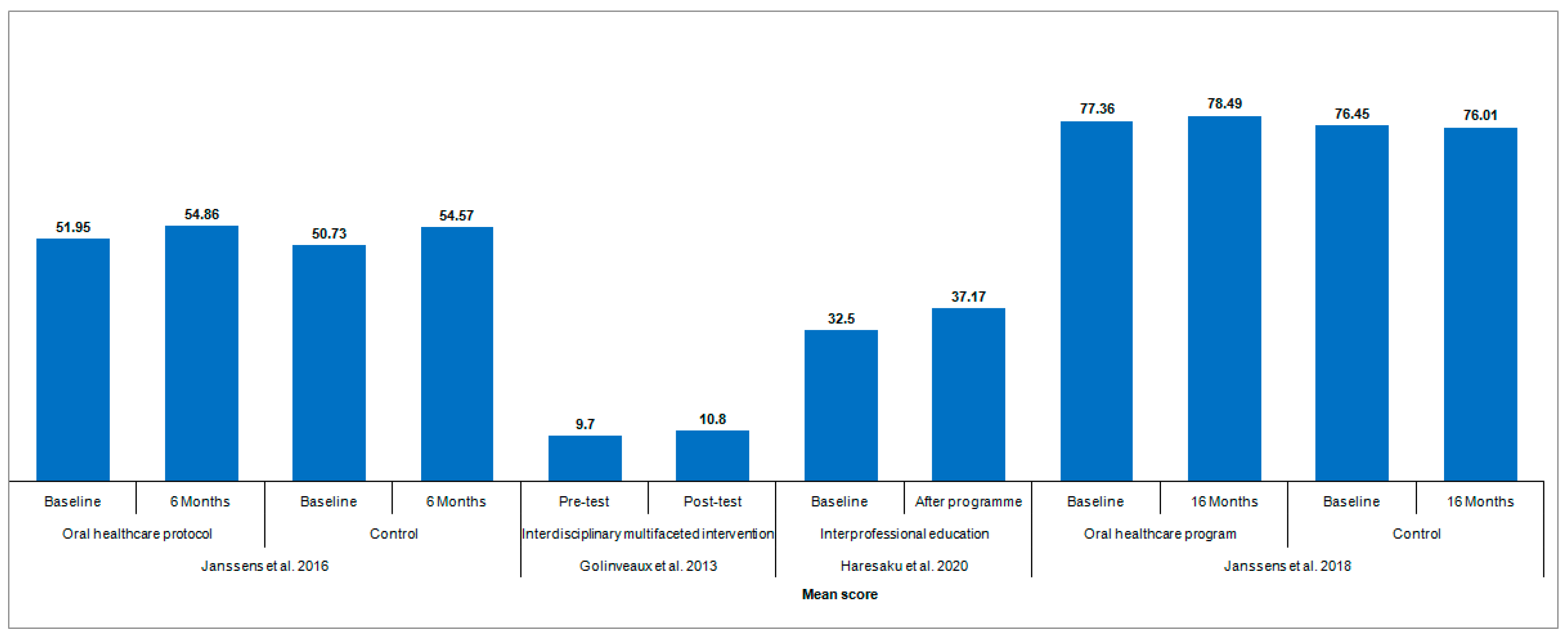
3.2. Attitudes of Nursing Professionals towards Oral Healthcare
3.3. Barriers to Oral Healthcare Promotion
3.4. Oral Care and Practices
3.5. Trainings and Resources to Promote Oral Healthcare
3.6. Quality Assessment of the Included Studies
4. Discussion
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030. Available online: https://www.who.int/publications-detail-redirect/9789240061484 (accessed on 20 July 2023).
- Righolt, A.J.; Jevdjevic, M.; Marcenes, W.; Listl, S. Global-, regional-, and country-level economic impacts of dental diseases in 2015. J. Dent. Res. 2018, 97, 501–507. [Google Scholar] [CrossRef]
- Spanemberg, J.C.; Cardoso, J.A.; Slob, E.M.G.B.; López-López, J. Quality of life related to oral health and its impact in adults. J. Stomatol. Oral. Maxillofac. Surg. 2019, 120, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Weening-Verbree, L.F.; Schuller, D.A.A.; Cheung, S.L.; Zuidema, P.D.S.U.; Schans, P.D.C.P.V.; Hobbelen, D.J.S.M. Barriers and facilitators of oral health care experienced by nursing home staff. Geriatr. Nurs. 2021, 42, 799–805. [Google Scholar] [CrossRef]
- Tadin, A.; Poljak Guberina, R.; Domazet, J.; Gavic, L. Oral hygiene practices and oral health knowledge among students in Split, Croatia. Healthcare 2022, 10, 406. [Google Scholar] [CrossRef] [PubMed]
- Poudel, P.; Griffiths, R.; Wong, V.W.; Arora, A.; Flack, J.R.; Khoo, C.L.; George, A. Oral health knowledge, attitudes and care practices of people with diabetes: A systematic review. BMC Public Health 2018, 18, 577. [Google Scholar] [CrossRef] [PubMed]
- Poudel, P.; Griffiths, R.; Wong, V.W.; Arora, A.; Flack, J.R.; Khoo, C.L.; George, A. Perceptions and practices of general practitioners on providing oral health care to people with diabetes—A qualitative study. BMC Fam. Pract. 2020, 21, 34. [Google Scholar] [CrossRef]
- Bhagat, V.; Hoang, H.; Crocombe, L.A.; Goldberg, L.R. Incorporating oral health care education in undergraduate nursing curricula—A systematic review. BMC Nurs. 2020, 19, 66. [Google Scholar] [CrossRef]
- IOM (Institute of Medicine); NRC (National Research Council). Improving Access to Oral Health Care for Vulnerable and Underserved Populations; The National Academies Press: Washington, DC, USA, 2011. [Google Scholar] [CrossRef]
- Abou El Fadl, R.; Blair, M.; Hassounah, S. Integrating maternal and children’s oral health promotion into nursing and midwifery practice—A systematic review. PLoS ONE 2016, 11, e0166760. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef]
- Veerasamy, A.; Lyons, K.; Crabtree, I.; Brunton, P. Geriatric oral health care content and barriers to its incorporation in undergraduate nursing curricula: New Zealand survey. J. Dent. Educ. 2023, 87, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Janssens, B.; Vanobbergen, J.; Lambert, M.; Schols, J.M.; De Visschere, L. Effect of an oral healthcare programme on care staff knowledge and attitude regarding oral health: A non-randomised intervention trial. Clin. Oral Investig. 2018, 22, 281–292. [Google Scholar] [CrossRef]
- Farokhi, M.R.; Muck, A.; Lozano-Pineda, J.; Boone, S.L.; Worabo, H. Using interprofessional education to promote oral health literacy in a faculty-student collaborative practice. J. Dent. Educ. 2018, 82, 1091–1097. [Google Scholar] [CrossRef]
- Weening-Verbree, L.F.; Schuller, A.A.; Zuidema, S.U.; Hobbelen, J.S. Evaluation of an oral care program to improve the oral health of home-dwelling older people. Int. J. Environ. Res. Public Health 2022, 19, 7251. [Google Scholar] [CrossRef]
- Dsouza, R.; Quinonez, R.; Hubbell, S.; Brame, J. Promoting oral health in nursing education through interprofessional collaborative practice: A quasi-experimental survey study design. Nurse Educ. Today 2019, 82, 93–98. [Google Scholar] [CrossRef]
- Khanbodaghi, A.; Natto, Z.S.; Forero, M.; Loo, C.Y. Effectiveness of interprofessional oral health program for pediatric nurse practitioner students at Northeastern University, United States. BMC Oral Health 2019, 19, 170. [Google Scholar] [CrossRef] [PubMed]
- Olatosi, O.O.; Oladugba, A.; Oyapero, A.; Belie, F.; Owais, A.I.; Weber-Gasparoni, K.; Sote, E.O.; Butali, A. A pre-experimental study to assess the impact of an interdisciplinary educational intervention on nurses’ knowledge of perinatal and infant oral health care. J. Int. Soc. Prev. Community Dent. 2019, 9, 619. [Google Scholar] [PubMed]
- Coan, L.L.; Wijesuriya, U.A.; Seibert, S.A. Collaboration of dental hygiene and nursing students on hospital units: An interprofessional education experience. J. Dent. Educ. 2019, 83, 654–662. [Google Scholar] [CrossRef]
- Janssens, B.; De Visschere, L.; van der Putten, G.J.; de Lugt–Lustig, K.; Schols, J.M.; Vanobbergen, J. Effect of an oral healthcare protocol in nursing homes on care staffs’ knowledge and attitude towards oral health care: A cluster-randomised controlled trial. Gerodontology 2016, 33, 275–286. [Google Scholar] [CrossRef]
- De Mey, L.; Çömlekçi, C.; de Reuver, F.; van Waard, I.; van Gool, R.; Scheerman, J.F.; van Meijel, B. Oral hygiene in patients with severe mental illness: A pilot study on the collaboration between oral hygienists and mental health nurses. Perspect. Psychiatr. Care 2016, 52, 194–200. [Google Scholar] [CrossRef]
- Golinveaux, J.; Gerbert, B.; Cheng, J.; Duderstadt, K.; Alkon, A.; Mullen, S.; Lin, B.; Miller, A.; Zhan, L. Oral health education for pediatric nurse practitioner students. J. Dent. Educ. 2013, 77, 581–590. [Google Scholar] [CrossRef]
- Haresaku, S.; Miyoshi, M.; Kubota, K.; Aoki, H.; Kajiwara, E.; Monji, M.; Naito, T. Effect of interprofessional education on oral assessment performance of nursing students. Clin. Exp. Dent. Res. 2020, 6, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Walker, K.; Jackson, R.; Edwards, P.C.; Vadaparampil, S.T. HPV and oral cancer: The need to integrate oral health practices into nursing education. Clin. J. Oncol. Nurs. 2018, 22, E166–E173. [Google Scholar]
- Nierenberg, S.; Hughes, L.P.; Warunek, M.; Gambacorta, J.E.; Dickerson, S.S.; Campbell-Heider, N. Nursing and dental students’ reflections on interprofessional practice after a service-learning experience in Appalachia. J. Dent. Educ. 2018, 82, 454–461. [Google Scholar] [CrossRef]
- Suminski, J.A. Oral care: Exploring education, attitudes, and behaviors among nurses caring for patients with breast cancer. Clin. J. Oncol. Nurs. 2017, 21, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Azodo, C.C.; Ezeja, E.B.; Ehizele, A.O.; Ehigiator, O. Oral assessment and nursing interventions among Nigerian nurses-knowledge, practices and educational needs. Ethiop. J. Health Sci. 2013, 23, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Veerasamy, A.; Lyons, K.; Crabtree, I.; Brunton, P. Knowledge of nursing graduates on oral health care for older people in the long-term care. J. Dent. Educ. 2022, 86, 830–838. [Google Scholar] [CrossRef]
- Dagnew, Z.A.; Abraham, I.A.; Beraki, G.G.; Mittler, S.; Achila, O.O.; Tesfamariam, E.H. Do nurses have barriers to quality oral care practice at a generalized hospital care in Asmara, Eritrea? A cross-sectional study. BMC Oral Health 2020, 20, 149. [Google Scholar] [CrossRef]
- Yimenu, D.K.; Adelo, E.S.; Siraj, E.A.; Kassie, T.A.; Hammeso, W.W.; Demeke, C.A.; Emiru, Y.K. Health professionals oral health knowledge and practice: Unleashing the hidden challenges. J. Multidiscip. Healthc. 2020, 13, 459–469. [Google Scholar] [CrossRef]
- Cianetti, S.; Anderini, P.; Pagano, S.; Eusebi, P.; Orso, M.; Salvato, R.; Lombardo, G. Oral health knowledge level of nursing staff working in semi-intensive heart failure units. J. Multidiscip. Healthc. 2020, 13, 165–173. [Google Scholar] [CrossRef]
- Andargie, S.T.; Kassahun, C.W. Knowledge and attitude of nurses’ towards patient’s oral care at University of Gondar comprehensive specialized hospital, Northwest Ethiopia. Int. J. Afr. Nurs. Sci. 2019, 11, 100165. [Google Scholar] [CrossRef]
- Ab Malik, N.; Yatim, S.M.; Hussein, N.; Mohamad, H.; McGrath, C. Oral hygiene practices and knowledge among stroke-care nurses: A multicentre cross-sectional study. J. Clin. Nurs. 2018, 27, 1913–1919. [Google Scholar] [CrossRef]
- El-Soussi, A.H.; Asfour, H.I. A return to the basics; nurses’ practices and knowledge about interventional patient hygiene in critical care units. Intensive Crit. Care Nurs. 2017, 40, 11–17. [Google Scholar] [CrossRef]
- Groenkjaer, L.L. Oral care in hepatology nursing. Gastroenterol. Nurs. 2015, 38, 22–30. [Google Scholar] [CrossRef]
- Rwakatema, D.S.; Ananduni, K.N.; Katiti, V.W.; Msuya, M.; Chugulu, J.; Kapanda, G. Oral health in nursing students at Kilimanjaro Christian Medical Centre teaching hospital in Moshi, Tanzania. BMC Oral Health 2015, 15, 23. [Google Scholar] [CrossRef] [PubMed]
- Braimoh, M.; Ogunbodede, E.; Adeniyi, A. Integration of oral health into primary health care system: Views of primary health care workers in Lagos State, Nigeria. J. Public Health Afr. 2014, 5, 328. [Google Scholar] [CrossRef] [PubMed]
- Philip, P.; Villarosa, A.; Gopinath, A.; Elizabeth, C.; Norman, G.; George, A. Oral health knowledge, attitude and practices among nurses in a tertiary care hospital in Bangalore, India: A cross-sectional survey. Contemp. Nurse 2019, 55, 261–274. [Google Scholar] [CrossRef] [PubMed]
- Haresaku, S.; Monji, M.; Miyoshi, M.; Kubota, K.; Kuroki, M.; Aoki, H.; Yoshida, R.; Machishima, K.; Makino, M.; Naito, T. Factors associated with a positive willingness to practice oral health care in the future amongst oral healthcare and nursing students. Eur. J. Dent. Educ. 2018, 22, e634–e643. [Google Scholar] [CrossRef]
- Yavagal, P.C.; Dalvi, T.M.; Benson, T.; Lakshmi, S.; Yann, T.H.; Gowda, T. Knowledge, attitude and practices related to oral health among nursing students in Davangere City: A cross-sectional survey. Oral Health Prev. Dent. 2020, 18, 493–498. [Google Scholar]
- An, R.; Chen, W.F.; Li, S.; Wu, Z.; Liu, M.; Sohaib, M. Assessment of the oral health literacy and oral health behaviors among nurses in China: A cross-sectional study. BMC Oral Health 2022, 22, 602. [Google Scholar] [CrossRef]
- Lakshmi, K.P.; Venkatalakshmi, S.; Bharath, C.; Saravanan, N.; Reddy, L.S.; Nagilla, J. Correlation of knowledge, attitude, and practice with their oral health status among young adults of nursing care: A cross-sectional survey. J. Pharm. Bioallied Sci. 2022, 14, S82. [Google Scholar] [CrossRef]
- Narbutaitė, J.; Skirbutytė, G.; Virtanen, J.I. Oral care in intensive care units: Lithuanian nurses’ attitudes and practices. Acta Odontol. Scand. 2023, 2, 1–6. [Google Scholar] [CrossRef]
- Zagade, H.; Varma, S.; Suragimath, G.; Zope, S. Knowledge, awareness, and practices of oral health for debilitated patients, among nursing staff of Krishna hospital. Int. J. Pharm. Res. Allied Sci. 2022, 11, 73–80. [Google Scholar] [CrossRef]
- Haresaku, S.; Kubota, K.; Yoshida, R.; Aoki, H.; Nakashima, F.; Iino, H.; Uchida, S.; Miyazono, M.; Naito, T. Effect of multi-professional education on the perceptions and awareness of oral health care among undergraduate nursing students in a nursing school. J. Dent. Educ. 2021, 85, 786–793. [Google Scholar] [CrossRef]
- Gu, L.; Chen, L.; Li, X.; Chen, W.; Zhang, L. Self-efficacy and attitudes of nurses providing oral care in geriatric care facilities: A cross-sectional study in Shanghai. Nurs. Open 2023, 10, 202–207. [Google Scholar] [CrossRef]
- Fernandes, S.; Shah, H.; Bafna, Y.; Patel, D.; Mistry, H.; Shah, K. Knowledge and attitude about emergency management of avulsed tooth amongst paramedical students of Visnagar, Gujarat: A questionnaire-based cross-sectional study. J. Clin. Diagn. Res. 2022, 16, ZC16–ZC20. [Google Scholar] [CrossRef]
- Paulsamym, P.; Venkatesan, K.; Muthu Mohamed, J.M.; Alshahrani, S.; Ramaiah, R.; Easwaran, V.; El-Sherbiny, M.; Dosoky, M.; Abdulla Khan, N.; Prabahar, K.; et al. Empowerment of primary healthcare providers on the prevention and management of dental or oral health issues among post-chemotherapy patients in pandemic. J. Healthc. Eng. 2022, 2022, 9087776. [Google Scholar] [CrossRef] [PubMed]
- Bashir, R.; Rizvi, K.F.; Fatima, K.; Ahmed, M.; Sami, A. Oral health care awareness among nursing students of Karachi, Pakistan. Rawal Med. J. 2021, 46, 106–110. [Google Scholar]
- Ahmad, M.S.; Abuzar, M.A.; Razak, I.A.; Rahman, S.A.; Borromeo, G.L. Perceptions of oral health education and practice among nursing students in Malaysia and Australia. Int. J. Dent. Hyg. 2021, 19, 215–222. [Google Scholar] [CrossRef]
- Alkhtib, A.; Temple-Smith, M.; Messer, L.B.; Pirotta, M.; Morgan, M.; Sajnani, A. Knowledge, attitudes and practices of primary health care providers towards oral health of preschool children in Qatar. J. Prev. Med. Hyg. 2020, 61, E205–E214. [Google Scholar] [PubMed]
- Ahmed, F.; Rao, A.; Shenoy, R.; Suprabha, B.S. Knowledge, attitude, and behavior of nurses toward delivery of primary oral health care in Dakshina Kannada, India. J. Indian Soc. Pedod. Prev. Dent. 2018, 36, 21–25. [Google Scholar] [PubMed]
- Lewis, A.; Edwards, S.; Whiting, G.; Donnelly, F. Evaluating student learning outcomes in oral health knowledge and skills. J. Clin. Nurs. 2018, 27, 2438–2449. [Google Scholar] [CrossRef] [PubMed]
- Saddki, N.; Mohamad Sani, F.E.; Tin-Oo, M.M. Oral care for intubated patients: A survey of intensive care unit nurses. Nurs. Crit. Care 2017, 22, 89–98. [Google Scholar] [CrossRef]
- Qu, X.; Xie, H.; Zhang, Q.; Zhou, X.; Shi, Z. A survey on oral care practices for ventilator-assisted patients in intensive care units in 3A hospitals of mainland China. Int. J. Nurs. Pract. 2015, 21, 699–708. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.; Badovinac, A.; Spalj, S.; Par, M.; Slaj, M.; Plančak, D. Factors influencing intensive care nurses’ knowledge and attitudes regarding ventilator-associated pneumonia and oral care practice in intubated patients in Croatia. Am. J. Infect. Control 2014, 42, 1115–1117. [Google Scholar] [CrossRef]
- Rabiei, S.; Mohebbi, S.Z.; Yazdani, R.; Virtanen, J.I. Primary care nurses’ awareness of and willingness to perform children’s oral health care. BMC Oral Health 2014, 14, 26. [Google Scholar] [CrossRef]
- Dogan, B. Differences in oral health behavior and attitudes between dental and nursing students. Clin. Exp. Health Sci. 2013, 3, 34–40. [Google Scholar] [CrossRef][Green Version]
- Archer, N.; Martin, K.; Johnston, L. Oral health ambassador scheme: Training needs analysis in the community setting. Br. Dent. J. 2022, 1–5. [Google Scholar] [CrossRef]
- Wei, X.; Jing, M.; Zhang, X.; Li, C.; Li, L. Nurses’ practice and educational needs in oral care for postoperative patients with oral cancer in ICUs: A multicenter cross-sectional study. BMC Oral Health 2022, 22, 389. [Google Scholar] [CrossRef]
- Pesaressi, E.; Villena, R.S.; van der Sanden, W.J.; Mulder, J.; Frencken, J.E. Barriers to adopting and implementing an oral health programme for managing early childhood caries through primary health care providers in Lima, Peru. BMC Oral Health 2014, 14, 17. [Google Scholar] [CrossRef]
- Hilton, S.; Sheppard, J.J.; Hemsley, B. Feasibility of implementing oral health guidelines in residential care settings: Views of nursing staff and residential care workers. Appl. Nurs. Res. 2016, 30, 194–203. [Google Scholar] [CrossRef]
- Adib-Hajbaghery, M.; Ansari, A.; Azizi-Fini, I. Intensive care nurses’ opinions and practice for oral care of mechanically ventilated patients. Indian J. Crit. Care Med. 2013, 17, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Peña, M.; Orozco Restrepo, L.A.; Barrios Arroyave, F.A.; Suárez Brochero, O.F. Impact of an educational intervention aimed at nursing staff on oral hygiene care on the incidence of ventilator-associated pneumonia in adults ventilated in intensive care unit. Invest. Educ. Enferm. 2021, 39, e06. [Google Scholar] [CrossRef] [PubMed]
- Zurmehly, J. Oral care education in the prevention of ventilator-associated pneumonia: Quality patient outcomes in the intensive care unit. J. Contin. Educ. Nurs. 2013, 44, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Branco, A.; Lourençone, E.M.S.; Monteiro, A.B.; Fonseca, J.P.; Blatt, C.R.; Caregnato, R.C.A. Education to prevent ventilator-associated pneumonia in intensive care unit. Rev. Bras. Enferm. 2020, 73, e20190477. [Google Scholar] [CrossRef]
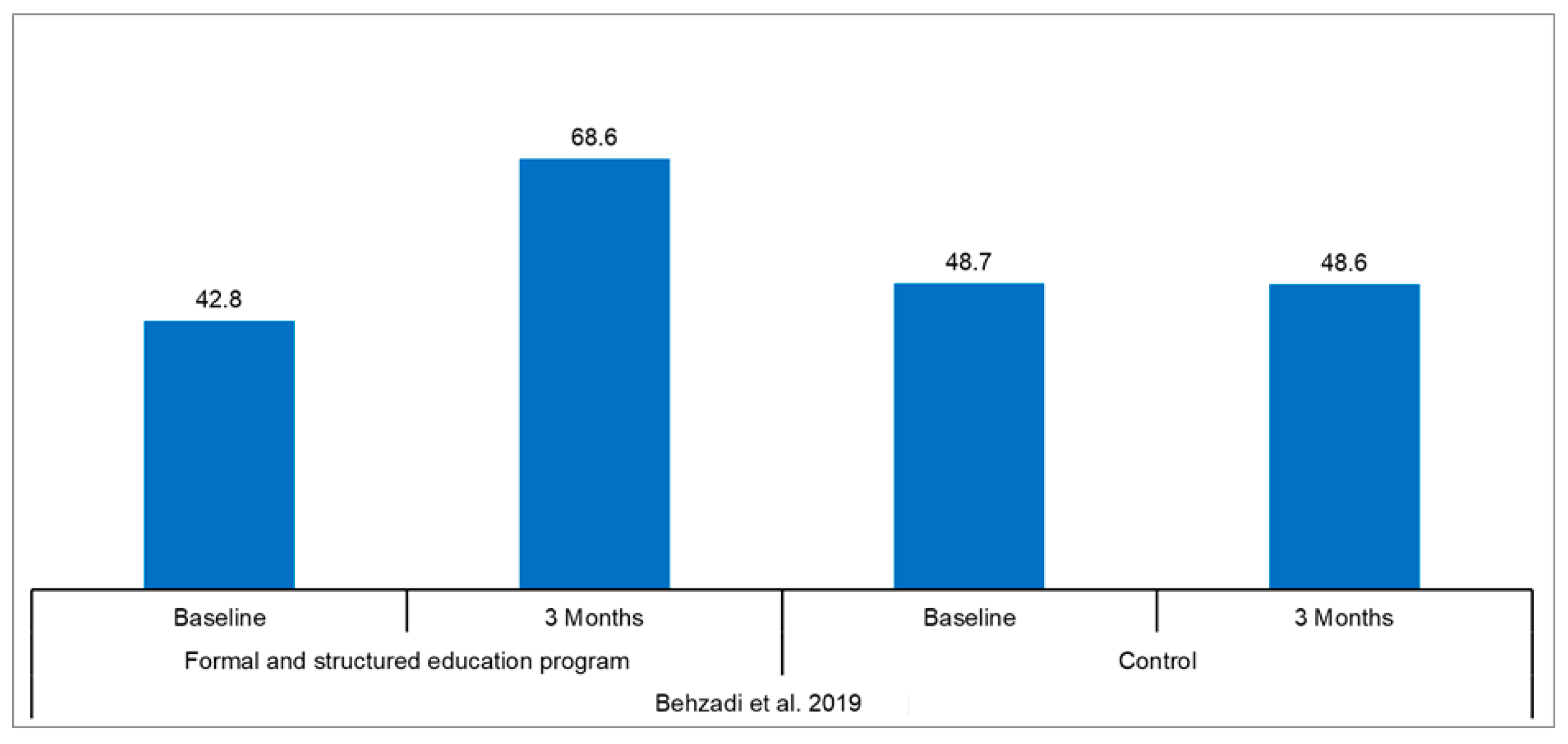
- Behzadi, F.; Khanjari, S.; Haghani, H. Impact of an education program on the performance of nurses in providing oral care for mechanically ventilated children. Aust. Crit. Care 2019, 32, 307–313. [Google Scholar] [CrossRef]
- Czarnecki, G.A.; Kloostra, S.J.; Boynton, J.R.; Inglehart, M.R. Nursing and dental students’ and pediatric dentistry residents’ responses to experiences with interprofessional education. J. Dent. Educ. 2014, 78, 1301–1312. [Google Scholar] [CrossRef]
- Yavuz, B.; Gerçeker, G.Ö.; Gümüş, M.; Yılmaz, H.B. An investigation of pediatric nurses’ oral care practices. J. Pediatr. Res. 2020, 7, 179–184. [Google Scholar] [CrossRef]
- Haresaku, S.; Kubota, K.; Miyoshi, M.; Obuse, M.; Aoki, H.; Nakashima, F.; Muramatsu, M.; Maeda, H.; Uchida, S.; Miyazono, M.; et al. A survey of oral assessment and healthcare education at nursing schools in Japan. Int. Dent. J. 2022; in press. [Google Scholar] [CrossRef]
- Ab Malik, N.; Yatim, S.M.; Lam, O.L.T.; Jin, L.; McGrath, C. Oral health care guidelines, training, and resources among stroke care providers. JDR Clin. Trans. Res. 2017, 2, 312–319. [Google Scholar]
- Stowers, B.A.; Giblin, L.; Laspina, L.; Perry, K. Perceptions of program directors and educators regarding the adequacy of oral health education in nursing assistant curricula. J. Dent. Hyg. 2017, 91, 21–28. [Google Scholar]
- Chan, E.Y.; Hui-Ling Ng, I. Oral care practices among critical care nurses in Singapore: A questionnaire survey. Appl. Nurs. Res. 2012, 25, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Salamone, K.; Yacoub, E.; Mahoney, A.M.; Edward, K.L. Oral care of hospitalised older patients in the acute medical setting. Nurs. Res. Pract. 2013, 2013, 827670. [Google Scholar] [CrossRef] [PubMed]
- Jun, M.K. Oral care practice, perception, and attitude of nurses in intensive care units in Korea: A questionnaire survey. Healthcare 2022, 10, 2033. [Google Scholar] [CrossRef] [PubMed]
- Haresaku, S.; Kubota, K.; Miyoshi, M.; Iino, H.; Monji, M.; Aoki, H.; Hidaka, T.; Sato, Y.; Mori, Y.; Yamada, M.; et al. Effect of educational environments on nursing faculty members’ perceptions regarding oral care. Jpn. J. Nurs. Sci. 2019, 16, 364–372. [Google Scholar] [CrossRef]
- Wong, G.; Koo, T.F.; Fethney, J.; Chen, R. Assessing oral health literacy of university nursing students: A cross-sectional exploratory study. Nurse Educ. Pract. 2021, 53, 103066. [Google Scholar] [CrossRef] [PubMed]
- Alotaibi, A.K.; Alshayiqi, M.; Ramalingam, S. Does the presence of oral care guidelines affect oral care delivery by intensive care unit nurses? A survey of Saudi intensive care unit nurses. Am. J. Infect. Control 2014, 42, 921–922. [Google Scholar] [CrossRef] [PubMed]
- Dolce, M.C.; Haber, J.; Savageau, J.A.; Hartnett, E.; Riedy, C.A. Integrating oral health curricula into nurse practitioner graduate programs: Results of a US survey. J. Am. Assoc. Nurse Pract. 2018, 30, 638–647. [Google Scholar] [CrossRef]
- Perry, A.D.; Iida, H.; Patton, L.L.; Wilder, R.S. Knowledge, perceived ability and practice behaviors regarding oral health among pediatric hematology and oncology nurses. J. Dent. Hyg. 2015, 89, 219–228. [Google Scholar]
- Pai, M.; Ribot, B.; Tane, H.; Murray, J. A study of periodontal disease awareness amongst third-year nursing students. Contemp. Nurse 2016, 52, 686–695. [Google Scholar] [CrossRef]
- Ganz, F.D.; Ofra, R.; Khalaila, R.; Levy, H.; Arad, D.; Kolpak, O.; Ben Nun, M.; Drori, Y.; Benbenishty, J. Translation of oral care practice guidelines into clinical practice by intensive care unit nurses. J. Nurs. Scholarsh. 2013, 45, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Blevins, J.Y. Status of oral health care in hospitalized children. MCN Am. J. Matern. Child Nurs. 2013, 38, 115–119. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Population |
|
|
| Intervention |
|
|
| Comparator |
|
|
| Key outcomes |
|
|
| Study design |
|
|
| Language | English | Non-English |
| Search timeframe | Inception to present (February 2023) | Not applicable |
| Any other criteria | No limits on sample size or countries | Not applicable |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Albougami, A. Oral Health Literacy Levels of Nursing Professionals and Effectiveness of Integrating Oral Health Training into Nursing Curricula: A Systematic Review. Appl. Sci. 2023, 13, 10403. https://doi.org/10.3390/app131810403
Albougami A. Oral Health Literacy Levels of Nursing Professionals and Effectiveness of Integrating Oral Health Training into Nursing Curricula: A Systematic Review. Applied Sciences. 2023; 13(18):10403. https://doi.org/10.3390/app131810403
Chicago/Turabian StyleAlbougami, Abdulrhman. 2023. "Oral Health Literacy Levels of Nursing Professionals and Effectiveness of Integrating Oral Health Training into Nursing Curricula: A Systematic Review" Applied Sciences 13, no. 18: 10403. https://doi.org/10.3390/app131810403
APA StyleAlbougami, A. (2023). Oral Health Literacy Levels of Nursing Professionals and Effectiveness of Integrating Oral Health Training into Nursing Curricula: A Systematic Review. Applied Sciences, 13(18), 10403. https://doi.org/10.3390/app131810403