Implementation of a Nutrition-Oriented Clinical Decision Support System (CDSS) for Weight Loss during the COVID-19 Epidemic in a Hospital Outpatient Clinic: A 3-Month Controlled Intervention Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Anthropometric and Body Composition Measurements
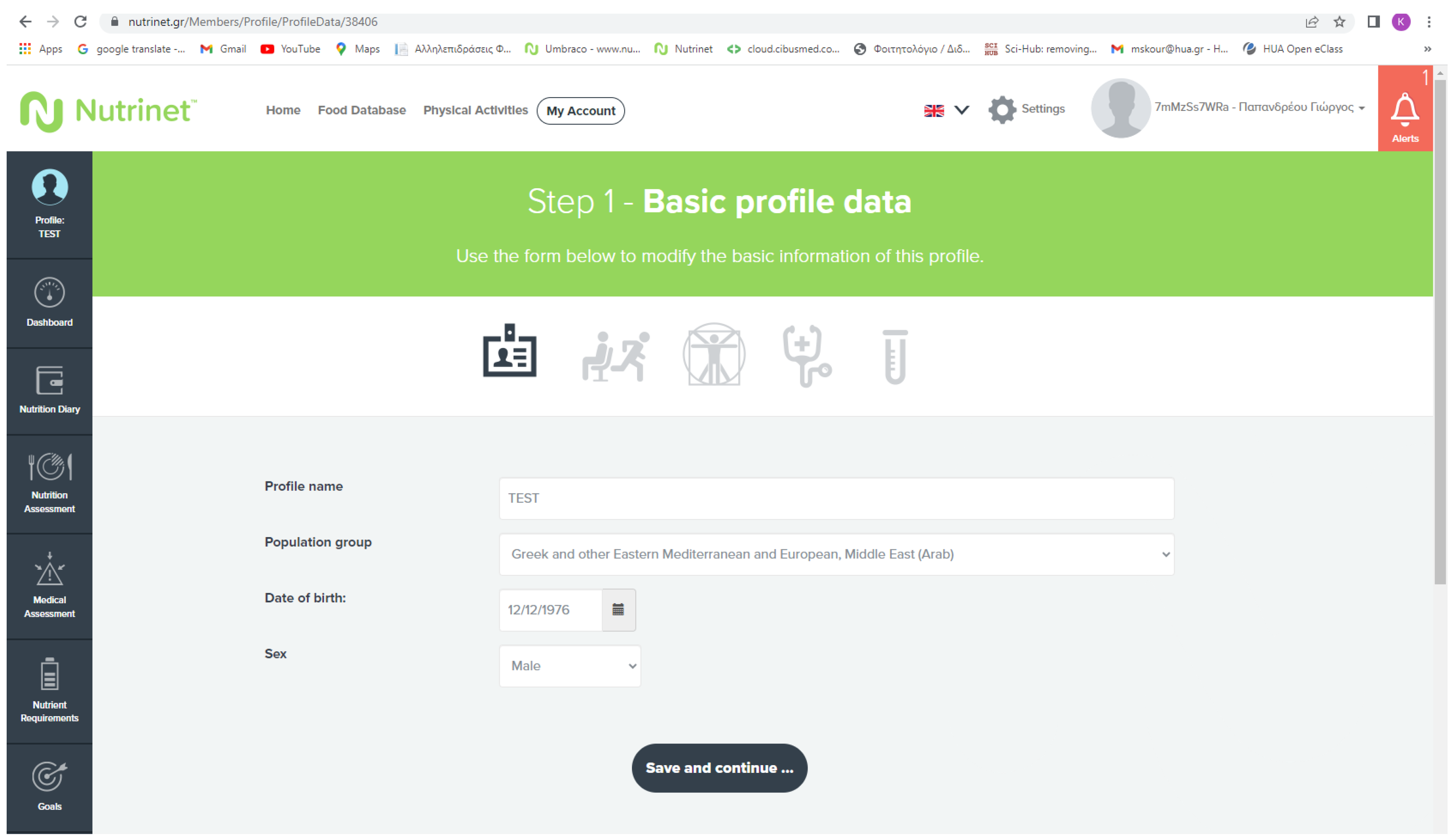
2.4. Nutrition-Oriented CDSS
2.4.1. Medical and Pharmaceutical History
2.4.2. Dietary Assessment
2.4.3. Physical Activity Assessment
2.4.4. Formulation of Personalized Tailored Dietary Plans
2.4.5. Dietary Monitoring and Evaluation
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sutton, R.T.; Pincock, D.; Baumgart, D.C.; Sadowski, D.C.; Fedorak, R.N.; Kroeker, K.I. An Overview of Clinical Decision Support Systems: Benefits, Risks, and Strategies for Success. NPJ Digit. Med. 2020, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Papandreou, P.; Nousiou, K.; Papandreou, G.; Steier, J.; Skouroliakou, M.; Karageorgopoulou, S. The Use of a Novel Clinical Decision Support System for Reducing Medication Errors and Expediting Care in the Provision of Chemotherapy. Health Technol. 2022, 12, 515–521. [Google Scholar] [CrossRef]
- Nimee, F.; Gioxari, A.; Steier, J.; Skouroliakou, M. Bridging the Gap: Community Pharmacists’ Burgeoning Role as Point-Of-Care Providers During the COVID-19 Pandemic Through the Integration of Emerging Technologies. J. Nutr. Health Food Sci. 2021, 9, 1–9. [Google Scholar] [CrossRef]
- Papandreou, P.; Gioxari, A.; Nimee, F.; Skouroliakou, M. Application of Clinical Decision Support System to Assist Breast Cancer Patients with Lifestyle Modifications during the COVID-19 Pandemic: A Randomised Controlled Trial. Nutrients 2021, 13, 2115. [Google Scholar] [CrossRef]
- Swan, W.I.; Vivanti, A.; Hakel-Smith, N.A.; Hotson, B.; Orrevall, Y.; Trostler, N.; Beck Howarter, K.; Papoutsakis, C. Nutrition Care Process and Model Update: Toward Realizing People-Centered Care and Outcomes Management. J. Acad. Nutr. Diet. 2017, 117, 2003–2014. [Google Scholar] [CrossRef]
- Henry, S.B.; Douglas, K.; Galzagorry, G.; Lahey, A.; Holzemer, W.L. A Template-Based Approach to Support Utilization of Clinical Practice Guidelines Within an Electronic Health Record. J. Am. Med. Inform. Assoc. 1998, 5, 237–244. [Google Scholar] [CrossRef]
- Detopoulou, P.; Tsouma, C.; Papamikos, V. COVID-19 and Nutrition: Summary of Official Recommendations. Top. Clin. Nutr. 2022, 37, 187–202. [Google Scholar] [CrossRef]
- Detopoulou, P.; Demopoulos, C.A.; Antonopoulou, S. Micronutrients, Phytochemicals and Mediterranean Diet: A Potential Protective Role against COVID-19 through Modulation of PAF Actions and Metabolism. Nutrients 2021, 13, 462. [Google Scholar] [CrossRef]
- Detopoulou, P.; Al-Khelefawi, Z.H.; Kalonarchi, G.; Papamikos, V. Formulation of the Menu of a General Hospital After Its Conversion to a “COVID Hospital”: A Nutrient Analysis of 28-Day Menus. Front. Nutr. 2022, 9, 833628. [Google Scholar] [CrossRef]
- Detopoulou, P.; Panoutsopoulos, G.I.; Kalonarchi, G.; Alexatou, O.; Petropoulou, G.; Papamikos, V. Development of a Tool for Determining the Equivalence of Nutritional Supplements to Diabetic Food Exchanges. Nutrients 2022, 14, 3267. [Google Scholar] [CrossRef]
- Wells Mulherin, D.; Walker, R.; Holcombe, B.; Guenter, P. ASPEN Report on Nutrition Support Practice Processes with COVID-19: The First Response. Nutr. Clin. Pract. 2020, 35, 783–791. [Google Scholar] [CrossRef]
- Papandreou, P.; Gioxari, A.; Daskalou, E.; Vasilopoulou, A.; Skouroliakou, M. Personalized Nutritional Intervention to Improve Mediterranean Diet Adherence in Female Patients with Multiple Sclerosis: A Randomized Controlled Study. Dietetics 2022, 1, 25–38. [Google Scholar] [CrossRef]
- Papandreou, P.; Gioxari, A.; Daskalou, E.; Grammatikopoulou, M.G.; Skouroliakou, M.; Bogdanos, D.P. Mediterranean Diet and Physical Activity Nudges versus Usual Care in Women with Rheumatoid Arthritis: Results from the MADEIRA Randomized Controlled Trial. Nutrients 2023, 15, 676. [Google Scholar] [CrossRef] [PubMed]
- Papandreou, P.; Amerikanou, C.; Vezou, C.; Gioxari, A.; Kaliora, A.C.; Skouroliakou, M. Improving Adherence to the Mediterranean Diet in Early Pregnancy Using a Clinical Decision Support System; A Randomised Controlled Clinical Trial. Nutrients 2023, 15, 432. [Google Scholar] [CrossRef] [PubMed]
- Tchang, B.G.; Morrison, C.; Kim, J.T.; Ahmed, F.; Chan, K.M.; Alonso, L.C.; Aronne, L.J.; Shukla, A.P. Weight Loss Outcomes with Telemedicine During COVID-19. Front. Endocrinol. 2022, 13, 793290. [Google Scholar] [CrossRef]
- Ufholz, K.; Werner, J. The Efficacy of Mobile Applications for Weight Loss. Curr. Cardiovasc. Risk Rep. 2023, 17, 83–90. [Google Scholar] [CrossRef]
- Bailly, S.; Fabre, O.; Legrand, R.; Pantagis, L.; Mendelson, M.; Terrail, R.; Tamisier, R.; Astrup, A.; Clément, K.; Pépin, J.-L. The Impact of the COVID-19 Lockdown on Weight Loss and Body Composition in Subjects with Overweight and Obesity Participating in a Nationwide Weight-Loss Program: Impact of a Remote Consultation Follow-Up—The CO-RNPC Study. Nutrients 2021, 13, 2152. [Google Scholar] [CrossRef] [PubMed]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, without Use of the Preparative Ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef]
- Pasternak, R.C. 2001 National Cholesterol Education Program (NCEP) Guidelines on the Detection, Evaluation and Treatment of Elevated Cholesterol in Adults: Adult Treatment Panel III (ATP III). ACC Curr. J. Rev. 2002, 11, 37–45. [Google Scholar] [CrossRef]
- American Diabetes Association Standards of Medical Care in Diabetes—2014. Diabetes Care 2014, 37 (Suppl. S1), S14–S80. [CrossRef]
- U.S. Department of Agriculture (USDA), Agricultural Research Service. FoodData Central. 2021. Available online: https://fdc.nal.usda.gov/ (accessed on 8 July 2023).
- Trichopoulou, A.; Georga, K. Composition Tables of Food and Greek Dishes; Parisianos SA.: Athens, Greece, 2004. [Google Scholar]
- National Academy of Sciences. Nutrition—Dietary Reference Intakes. Available online: https://nap.nationalacademies.org/collection/57/dietary-reference-intakes (accessed on 8 July 2023).
- Hamwi, G.J. Therapy: Changing Dietary Concepts. In Diabetes Mellitus: Diagnosis and Treatment; Danowski, T.S., Ed.; American Diabetes Association: New York, NY, USA, 1964; Volume 1, pp. 73–78. [Google Scholar]
- Alberti, K.G.; Zimmet, P.; Shaw, J. Metabolic syndrome—A new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 Compendium of Physical Activities: A Second Update of Codes and MET Values. Med. Sci. Sports Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- Salinas, J.J.; Sheen, J.; Shokar, N.; Wright, J.; Vazquez, G.; Alozie, O. An Electronic Medical Records Study of Population Obesity Prevalence in El Paso, Texas. BMC Med. Inf. Decis. Mak. 2022, 22, 46. [Google Scholar] [CrossRef]
- Alexeeva, O.; Keswani, R.N.; Pandolfino, J.E.; Liebovitz, D.; Gregory, D.; Yadlapati, R. Electronic Clinical Decision Support Tools for Obesity and Gastroesophageal Reflux Disease: The Provider’s Perspective. Am. J. Gastroenterol. 2018, 113, 916. [Google Scholar] [CrossRef] [PubMed]
- Naureckas, S.M.; Zweigoron, R.; Haverkamp, K.S.; Kaleba, E.O.; Pohl, S.J.; Ariza, A.J. Developing an Electronic Clinical Decision Support System to Promote Guideline Adherence for Healthy Weight Management and Cardiovascular Risk Reduction in Children: A Progress Update. Behav. Med. Pract. Policy Res. 2011, 1, 103–107. [Google Scholar] [CrossRef][Green Version]
- Rattay, K.T.; Ramakrishnan, M.; Atkinson, A.; Gilson, M.; Drayton, V. Use of an Electronic Medical Record System to Support Primary Care Recommendations to Prevent, Identify, and Manage Childhood Obesity. Pediatrics 2009, 123, S100–S107. [Google Scholar] [CrossRef]
- Skiba, D.J.; Gance-Cleveland, B.; Gilbert, K.; Gilbert, L.; Dandreaux, D. Comparing the Effectiveness of CDSS on Provider’s Behaviors to Implement Obesity Prevention Guidelines. In Proceedings of the NI 2012: 11th International Congress on Nursing Informatics, Montreal, QC, Canada, 23–27 June 2012; Volume 2012, p. 376. [Google Scholar]
- Rossi, M.; Campbell, K.L.; Ferguson, M. Implementation of the Nutrition Care Process and International Dietetics and Nutrition Terminology in a Single-Center Hemodialysis Unit: Comparing Paper vs. Electronic Records. J. Acad. Nutr. Diet. 2014, 114, 124–130. [Google Scholar] [CrossRef]
- Chen, W.; Howard, K.; Gorham, G.; O’Bryan, C.M.; Coffey, P.; Balasubramanya, B.; Abeyaratne, A.; Cass, A. Design, Effectiveness, and Economic Outcomes of Contemporary Chronic Disease Clinical Decision Support Systems: A Systematic Review and Meta-Analysis. J. Am. Med. Inform. Assoc. 2022, 29, 1757–1772. [Google Scholar] [CrossRef]
- Bray, G.A.; Ryan, D.H. Evidence-based Weight Loss Interventions: Individualized Treatment Options to Maximize Patient Outcomes. Diabetes Obes. Metab. 2021, 23, 50–62. [Google Scholar] [CrossRef]
- Paulsen, M.M.; Paur, I.; Gjestland, J.; Henriksen, C.; Varsi, C.; Tangvik, R.J.; Andersen, L.F. Effects of Using the MyFood Decision Support System on Hospitalized Patients’ Nutritional Status and Treatment: A Randomized Controlled Trial. Clin. Nutr. 2020, 39, 3607–3617. [Google Scholar] [CrossRef]
- Bonilla, C.; Brauer, P.; Royall, D.; Keller, H.; Hanning, R.M.; DiCenso, A. Use of Electronic Dietary Assessment Tools in Primary Care: An Interdisciplinary Perspective. BMC Med. Inf. Decis. Mak. 2015, 15, 14. [Google Scholar] [CrossRef]
- Burke, L.E.; Conroy, M.B.; Sereika, S.M.; Elci, O.U.; Styn, M.A.; Acharya, S.D.; Sevick, M.A.; Ewing, L.J.; Glanz, K. The Effect of Electronic Self-Monitoring on Weight Loss and Dietary Intake: A Randomized Behavioral Weight Loss Trial. Obesity 2011, 19, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Carter, M.C.; Burley, V.J.; Nykjaer, C.; Cade, J.E. Adherence to a Smartphone Application for Weight Loss Compared to Website and Paper Diary: Pilot Randomized Controlled Trial. J. Med. Internet Res. 2013, 15, e32. [Google Scholar] [CrossRef] [PubMed]
- Raaijmakers, L.C.H.; Pouwels, S.; Berghuis, K.A.; Nienhuijs, S.W. Technology-Based Interventions in the Treatment of Overweight and Obesity: A Systematic Review. Appetite 2015, 95, 138–151. [Google Scholar] [CrossRef] [PubMed]
- Hansel, B.; Giral, P.; Gambotti, L.; Lafourcade, A.; Peres, G.; Filipecki, C.; Kadouch, D.; Hartemann, A.; Oppert, J.-M.; Bruckert, E.; et al. A Fully Automated Web-Based Program Improves Lifestyle Habits and HbA1c in Patients with Type 2 Diabetes and Abdominal Obesity: Randomized Trial of Patient E-Coaching Nutritional Support (The ANODE Study). J. Med. Internet Res. 2017, 19, e360. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 5. Facilitating Behavior Change and Well-Being to Improve Health Outcomes: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45 (Suppl. S1), S60–S82. [Google Scholar] [CrossRef]
- Yon, B.A.; Johnson, R.K.; Harvey-Berino, J.; Gold, B.C.; Howard, A.B. Personal Digital Assistants Are Comparable to Traditional Diaries for Dietary Self-Monitoring During a Weight Loss Program. J. Behav. Med. 2007, 30, 165–175. [Google Scholar] [CrossRef]
- Tsai, A.G.; Wadden, T.A. Systematic Review: An Evaluation of Major Commercial Weight Loss Programs in the United States. Ann. Intern. Med. 2005, 142, 56. [Google Scholar] [CrossRef]
- Ravussin, E.; Lillioja, S.; Knowler, W.C.; Christin, L.; Freymond, D.; Abbott, W.G.H.; Boyce, V.; Howard, B.V.; Bogardus, C. Reduced Rate of Energy Expenditure as a Risk Factor for Body-Weight Gain. N. Engl. J. Med. 1988, 318, 467–472. [Google Scholar] [CrossRef]
- Detopoulou, P.; Voulgaridou, G.; Papadopoulou, S. Cancer, Phase Angle and Sarcopenia: The Role of Diet in Connection with Lung Cancer Prognosis. Lung 2022, 200, 347–379. [Google Scholar] [CrossRef]
- Papadopoulou, S.K.; Detopoulou, P.; Voulgaridou, G.; Tsoumana, D.; Spanoudaki, M.; Sadikou, F.; Papadopoulou, V.G.; Zidrou, C.; Chatziprodromidou, I.P.; Giaginis, C.; et al. Mediterranean Diet and Sarcopenia Features in Apparently Healthy Adults over 65 Years: A Systematic Review. Nutrients 2023, 15, 1104. [Google Scholar] [CrossRef] [PubMed]
- AlAufi, N.S.; Chan, Y.M.; Waly, M.I.; Chin, Y.S.; Mohd Yusof, B.-N.; Ahmad, N. Application of Mediterranean Diet in Cardiovascular Diseases and Type 2 Diabetes Mellitus: Motivations and Challenges. Nutrients 2022, 14, 2777. [Google Scholar] [CrossRef] [PubMed]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-Style Diet for the Primary and Secondary Prevention of Cardiovascular Disease. Cochrane Database Syst. Rev. 2019, 2019, CD009825. [Google Scholar] [CrossRef]
- Wu, X.; Guo, X.; Zhang, Z. The Efficacy of Mobile Phone Apps for Lifestyle Modification in Diabetes: Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth 2019, 7, e12297. [Google Scholar] [CrossRef] [PubMed]
- Detopoulou, P.; Aggeli, M.; Andrioti, E.; Detopoulou, M. Macronutrient Content and Food Exchanges for 48 Greek Mediterranean Dishes: Macronutrient Content and Exchanges for 48 Greek Dishes. Nutr. Diet. 2017, 74, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Detopoulou, P.; Fragopoulou, E.; Nomikos, T.; Yannakoulia, M.; Stamatakis, G.; Panagiotakos, D.B.; Antonopoulou, S. The Relation of Diet with PAF and Its Metabolic Enzymes in Healthy Volunteers. Eur. J. Nutr. 2015, 54, 25–34. [Google Scholar] [CrossRef]
- Fragopoulou, E.; Detopoulou, P.; Alepoudea, E.; Nomikos, T.; Kalogeropoulos, N.; Antonopoulou, S. Associations between Red Blood Cells Fatty Acids, Desaturases Indices and Metabolism of Platelet Activating Factor in Healthy Volunteers. Prostaglandins Leukot. Essent. Fat. Acids 2021, 164, 102234. [Google Scholar] [CrossRef]
- Psaltopoulou, T.; Panagiotakos, D.B.; Pitsavos, C.; Chrysochoou, C.; Detopoulou, P.; Skoumas, J.; Stefanadis, C. Dietary Antioxidant Capacity Is Inversely Associated with Diabetes Biomarkers: The ATTICA Study. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 561–567. [Google Scholar] [CrossRef]
- Nomikos, T.; Detopoulou, P.; Fragopoulou, E.; Pliakis, E.; Antonopoulou, S. Boiled Wild Artichoke Reduces Postprandial Glycemic and Insulinemic Responses in Normal Subjects but Has No Effect on Metabolic Syndrome Patients. Nutr. Res. 2007, 27, 741–749. [Google Scholar] [CrossRef]
- Mebrahtu, T.F.; Skyrme, S.; Randell, R.; Keenan, A.-M.; Bloor, K.; Yang, H.; Andre, D.; Ledward, A.; King, H.; Thompson, C. Effects of Computerised Clinical Decision Support Systems (CDSS) on Nursing and Allied Health Professional Performance and Patient Outcomes: A Systematic Review of Experimental and Observational Studies. BMJ Open 2021, 11, e053886. [Google Scholar] [CrossRef]
- Chopra, S.; Malhotra, A.; Ranjan, P.; Vikram, N.K.; Sarkar, S.; Siddhu, A.; Kumari, A.; Kaloiya, G.S.; Kumar, A. Predictors of Successful Weight Loss Outcomes amongst Individuals with Obesity Undergoing Lifestyle Interventions: A Systematic Review. Obes. Rev. 2021, 22, e13148. [Google Scholar] [CrossRef] [PubMed]
- Stubbs, J.; Whybrow, S.; Teixeira, P.; Blundell, J.; Lawton, C.; Westenhoefer, J.; Engel, D.; Shepherd, R.; Mcconnon, Á.; Gilbert, P.; et al. Problems in Identifying Predictors and Correlates of Weight Loss and Maintenance: Implications for Weight Control Therapies Based on Behaviour Change: Predicting Weight Outcomes. Obes. Rev. 2011, 12, 688–708. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, P.J.; Going, S.B.; Sardinha, L.B.; Lohman, T.G. A Review of Psychosocial Pre-Treatment Predictors of Weight Control. Obes. Rev. 2005, 6, 43–65. [Google Scholar] [CrossRef] [PubMed]
- Morgan, P.J.; Hollis, J.L.; Young, M.D.; Collins, C.E.; Teixeira, P.J. Workday Sitting Time and Marital Status: Novel Pretreatment Predictors of Weight Loss in Overweight and Obese Men. Am. J. Men’s Health 2018, 12, 1431–1438. [Google Scholar] [CrossRef] [PubMed]
- Mroz, J.E.; Pullen, C.H.; Hageman, P.A. Health and Appearance Reasons for Weight Loss as Predictors of Long-Term Weight Change. Health Psychol. Open 2018, 5, 1–8. [Google Scholar] [CrossRef]
- Speakman, J.R.; Selman, C. Physical Activity and Resting Metabolic Rate. Proc. Nutr. Soc. 2003, 62, 621–634. [Google Scholar] [CrossRef]
- Poobalan, A.; Aucott, L.; Smith, W.C.S.; Avenell, A.; Jung, R.; Broom, J.; Grant, A.M. Effects of Weight Loss in Overweight/Obese Individuals and Long-Term Lipid Outcomes—A Systematic Review. Obes. Rev. 2004, 5, 43–50. [Google Scholar] [CrossRef]
- Mittendorfer, B.; Patterson, B.W.; Klein, S. Effect of Sex and Obesity on Basal VLDL-Triacylglycerol Kinetics. Am. J. Clin. Nutr. 2003, 77, 573–579. [Google Scholar] [CrossRef]
- Ginsberg, H.N.; Le, N.A.; Gibson, J.C. Regulation of the Production and Catabolism of Plasma Low Density Lipoproteins in Hypertriglyceridemic Subjects. Effect of Weight Loss. J. Clin. Investig. 1985, 75, 614–623. [Google Scholar] [CrossRef]
- Jourdan, M.; Margen, S.; Bradfield, R.B. The Turnover Rate of Serum Glycerides in the Lipoproteins of Fasting Obese Women during Weight Loss. Am. J. Clin. Nutr. 1974, 27, 850–858. [Google Scholar] [CrossRef]
- Bakaloudi, D.R.; Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Chourdakis, M. Impact of the First COVID-19 Lockdown on Body Weight: A Combined Systematic Review and a Meta-Analysis. Clin. Nutr. 2022, 41, 3046–3054. [Google Scholar] [CrossRef] [PubMed]
- Kuk, J.L.; Christensen, R.A.G.; Kamran Samani, E.; Wharton, S. Predictors of Weight Loss and Weight Gain in Weight Management Patients during the COVID-19 Pandemic. J. Obes. 2021, 2021, 4881430. [Google Scholar] [CrossRef] [PubMed]
- Papazisis, Z.; Nikolaidis, P.T.; Trakada, G. Sleep, Physical Activity, and Diet of Adults during the Second Lockdown of the COVID-19 Pandemic in Greece. Int. J. Environ. Res. Public Health 2021, 18, 7292. [Google Scholar] [CrossRef] [PubMed]
- Nomikos, T.; Georgoulis, M.; Chrysohoou, C.; Damigou, E.; Barkas, F.; Skoumas, I.; Liberopoulos, E.; Pitsavos, C.; Tsioufis, C.; Sfikakis, P.P.; et al. Comparative Performance of Equations to Estimate Low-density Lipoprotein Cholesterol Levels and Cardiovascular Disease Incidence: The ATTICA Study (2002–2022). Lipids 2023, 58, 159–170. [Google Scholar] [CrossRef] [PubMed]

| CDSS Intervention Group (n = 39) | Dietary Advice Group (n = 21) | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | p-Value § | Baseline | Follow-Up | p-Value ‡ | p-Value ∫ | |
| Age (y) | 48.9 ± 13.4 | NA | NA | 67.0 ± 16.4 | NA | NA | <0.001 |
| Sex (men), n (%) | 28 (71.8%) | NA | NA | 4 (16%) | NA | NA | <0.001 |
| Body weight (kg) | 95.5 ± 21.8 | 90.6 ± 19.9 | <0.001 | 73.4 ± 10.1 | 72.8 ± 11.3 | 0.563 | <0.001 |
| BMI (kg/m2) | 35.2 (28.4–37.5) | 33.2 (27.4–35.4) | <0.001 | 26.4 (22.4–28.5) | 24.9 (21.7–27.4) | 0.434 | <0.001 |
| Total body fat (%) | 44.9 ± 11.3 | 41.9 ± 10.5 | <0.001 | 35.7 ± 5.7 | 35.6 ± 5.9 | 0.469 | 0.001 |
| Lean tissue (kg) | 25.4 (21.7–29.1) | 24.6 (21.8–27.9) | 0.050 | NA | NA | NA | NA |
| Lean mass index (kg/m2) | 9.31 ± 1.29 | 8.98 ± 1.31 | 0.048 | NA | NA | NA | NA |
| Glucose (mg/dL) † | 89 (80–97) | 87 (85–97) | 0.478 | 91 ± 12.4 | 91.2 ± 15.6 | 0.612 | 0.733 |
| Glycated hemoglobin, HbA1c (%) | 5.26 ± 0.55 | 4.97 ± 0.41 | 0.017 | 5.10 ± 0.84 | NA | NA | 0.573 |
| Total-cholesterol (mg/dL) | 186 ± 45 | 164 ± 37 | 0.628 | 193 ± 38 | 197 ± 40 | 0.582 | 0.554 |
| LDL-cholesterol (mg/dL) | 111 (91–120) | 108 (77–118) | 0.919 | 107 (100–143) | 109 (83–135) | 0.748 | 0.638 |
| HDL-cholesterol (mg/dL) | 55 (46–67) | 50 (40–65) | 0.569 | 49 (56–64) | 53 (65–74) | 0.125 | 0.552 |
| Triglycerides (mg/dL) | 137 (115–152) | 130 (108–160) | 0.005 | 95 (65–155) | 97 (70–121) | 0.808 | 0.554 |
| Men (n = 28) | Women (n = 11) | |||||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | p-Value | Baseline | Follow-Up | p-Value | |
| Body weight (kg) | 87.9 ± 14.9 | 83.3 ± 13.9 | <0.001 | 114.6 ± 25.4 | 109.2 ± 21.4 | <0.001 |
| BMI (kg/m2) | 31.9 (28.3–36.2) | 30.3 (26.7–34.6) | <0.001 | 36.2 (28.8–40.1) | 35.1 (29.4–36.5) | 0.021 |
| Total body fat (%) | 46.9 ± 9.8 | 43.7 ± 9.7 | <0.001 | 39.9 ± 13.8 | 37.3 ± 11.5 | <0.001 |
| Lean tissue (kg) | 22.4 (21.5–26.1) | 23.5 (19.9–25.9) | 0.167 | 35.4 (29.1–41.6) | 32.8 (28.0–38.5) | 0.109 |
| Lean mass index (kg/m2) | 8.83 (8.03–9.22) | 8.80 (7.64–9.16) | 0.178 | 10.83 (9.92–11.67) | 9.90 (9.30–11.76) | 0.091 |
| Glucose (mg/dL) † | 89 (80–93) | 87 (85–97) | 0.010 | 75 (92–98) | 88 (85–96) | 0.220 |
| Glycated hemoglobin, HbA1c (%) | 5.25 ± 0.44 | 5.06 ± 0.46 | 0.151 | 5.31 ± 0.83 | 4.83 ± 0.29 | 0.077 |
| Total-cholesterol (mg/dL) | 182 ± 38 | 164 ± 39 | <0.001 | 197 ± 61 | 164.2 ± 38.9 | 0.069 |
| LDL-cholesterol (mg/dL) | 111 (91–119) | 109 (35–121) | 0.237 | 109 (87–138) | 107 (99–130) | 0.109 |
| HDL-cholesterol (mg/dL) | 55 (45–67) | 50 (40–52) | 0.343 | 59 (45–68) | 57 (41–65) | 0.705 |
| Triglycerides (mg/dL) | 137 (110–144) | 130 (108–138) | 0.018 | 135 (116–189) | 140 (107–194) | 0.109 |
| Pattern 1: High BMI–High % Body Fat | Pattern 2: High BMI–High Lean Tissue | |
|---|---|---|
| BMI at baseline (kg/m2) | 0.873 | 0.473 |
| Lean mass at baseline (kg) | 0.014 | 0.997 |
| Body fat at baseline (%) | 0.975 | −0.195 |
| % variance explained | 60.4% | 38.4 % |
| Total variance explained 98.9% | ||
| The factor loadings (component scores) are interpreted as correlation coefficients (r). Higher absolute values of the loadings indicate that the variable is correlated with the respective component. Numbers in bold indicate absolute loadings greater than 0.45. | ||
| % Weight Loss (r) | |||
|---|---|---|---|
| Total (n = 39) | Women (n = 11) | Men (n = 28) | |
| Age (y) | 0.092 (p = 0.576) | 0.050 (p = 0.884) | 0.130 (p = 0.511) |
| BMI (kg/m2) | 0.292 (p = 0.072) | 0.400 (p = 0.223) | 0.222 (p = 0.256) |
| Body fat (%) | 0.118 (p = 0.473) | 0.127(p = 0.709) | 0.191 (p = 0.332) |
| Lean mass (kg) | 0.108 (p = 0.514) | 0.618 (p = 0.043) | 0.079 (p = 0.690) |
| Lean mass index (kg/m2) | 0.158 (p = 0.337) | 0.618 (p = 0.043) | 0.147 (p = 0.456) |
| High BMI–high % body fat pattern | 0.164 (p = 0.318) | 0.200 (p = 0.555) | 0.185 (p = 0.346) |
| High BMI–high lean tissue pattern | 0.166 (p = 0.313) | 0.618 (p = 0.043) | 0.149 (p = 0.450) |
| Glucose (mg/dL) | −0.270 (p = 0.128) | −0.714 (p = 0.047) | −0.154 (p = 0.462) |
| Glycated hemoglobin, HbA1c (%) | −0.145 (p = 0.428) | −0.143 (p = 0.736) | −0.139 (p = 0.518) |
| Total-cholesterol (mg/dL) | −0.150 (p = 0.377) | 0.231 (p = 0.521) | −0.218 (p = 0.274) |
| HDL-cholesterol (mg/dL) | −0.026 (p = 0.877) | −0.588 (p = 0.074) | 0.199 (p = 0.321) |
| Triglycerides (mg/dL) | −0.410 (p = 0.012) | −0.067 (p = 0.855) | −0.601 (p = 0.001) |
| Total (n = 39) | Women (n = 11) | Men (n = 28) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | B | SE | p | |
| Basic Model (R2 = 0.2%, W: 0%, M: 0.1%) | |||||||||
| Age (y) | 0.005 | 0.041 | 0.903 | 0.004 | 0.086 | 0.967 | 0.006 | 0.047 | 0.908 |
| Gender (men vs. women *) | 0.320 | 1.208 | 0.792 | NA | NA | NA | NA | NA | NA |
| Model 1 (R2 = 1.1%, W: 18.6%, M: 2%) | |||||||||
| Age (y) | 0.002 | 0.042 | 0.967 | −0.009 | 0.083 | 0.913 | 0.007 | 0.049 | 0.888 |
| Gender (men vs. women *) | 0.228 | 10.232 | 0.854 | NA | NA | NA | NA | NA | NA |
| Physical activity at baseline § | −0.393 | 0.724 | 0.591 | −1.915 | 10.419 | 0.214 | 0.160 | 0.849 | 0.852 |
| Model 2 (R2 T: 13.5%, W: 83.6%, M: 4.6%) | |||||||||
| Age (y) | 0.004 | 0.041 | 0.928 | −0.069 | 0.049 | 0.207 | 0.023 | 0.053 | 0.665 |
| Gender (men vs. women *) | 2.757 | 1.804 | 0.136 | NA | NA | NA | NA | NA | NA |
| Physical activity at baseline § | −0.017 | 0.785 | 0.983 | −2.568 | 1.093 | 0.057 | 0.524 | 0.941 | 0.583 |
| Pattern 1: High BMI–high% fat | 0.282 | 0.628 | 0.657 | −0.469 | 0.738 | 0.549 | 0.522 | 0.869 | 0.554 |
| Pattern 2: High BMI–high lean tissue | 1.611 | 0.803 | 0.050 | 3.353 | 0.692 | 0.003 | 0.769 | 1.167 | 0.517 |
| Model 3 (R2 T: 20.6%, W: 88.5%, M: 18.6%) | |||||||||
| Age (y) | −0.006 | 0.040 | 0.887 | −0.040 | 0.044 | 0.424 | 0.003 | 0.054 | 0.949 |
| Gender (men vs. women *) | 2.579 | 1.734 | 0.147 | NA | NA | NA | NA | NA | NA |
| Physical activity at baseline § | −0.290 | 0.762 | 0.706 | −30.416 | 0.979 | 0.025 | 0.248 | 0.915 | 0.789 |
| Pattern 1: High BMI–high % fat | 0.128 | 0.610 | 0.835 | −10.245 | 0.703 | 0.151 | 0.411 | 0.840 | 0.630 |
| Pattern 2: High BMI–high lean tissue | 10.307 | 0.818 | 0.121 | 20.415 | 0.717 | 0.028 | 0.727 | 10.123 | 0.524 |
| Triglycerides (mg/dL) | −0.018 | 0.009 | 0.050 | −0.005 | 0.009 | 0.618 | −0.022 | 0.011 | 0.069 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Detopoulou, P.; Papandreou, P.; Papadopoulou, L.; Skouroliakou, M. Implementation of a Nutrition-Oriented Clinical Decision Support System (CDSS) for Weight Loss during the COVID-19 Epidemic in a Hospital Outpatient Clinic: A 3-Month Controlled Intervention Study. Appl. Sci. 2023, 13, 9448. https://doi.org/10.3390/app13169448
Detopoulou P, Papandreou P, Papadopoulou L, Skouroliakou M. Implementation of a Nutrition-Oriented Clinical Decision Support System (CDSS) for Weight Loss during the COVID-19 Epidemic in a Hospital Outpatient Clinic: A 3-Month Controlled Intervention Study. Applied Sciences. 2023; 13(16):9448. https://doi.org/10.3390/app13169448
Chicago/Turabian StyleDetopoulou, Paraskevi, Panos Papandreou, Lida Papadopoulou, and Maria Skouroliakou. 2023. "Implementation of a Nutrition-Oriented Clinical Decision Support System (CDSS) for Weight Loss during the COVID-19 Epidemic in a Hospital Outpatient Clinic: A 3-Month Controlled Intervention Study" Applied Sciences 13, no. 16: 9448. https://doi.org/10.3390/app13169448
APA StyleDetopoulou, P., Papandreou, P., Papadopoulou, L., & Skouroliakou, M. (2023). Implementation of a Nutrition-Oriented Clinical Decision Support System (CDSS) for Weight Loss during the COVID-19 Epidemic in a Hospital Outpatient Clinic: A 3-Month Controlled Intervention Study. Applied Sciences, 13(16), 9448. https://doi.org/10.3390/app13169448







