Immediate versus Delayed Implant Placement in Patients with Tooth Agenesis: An In-Line Retrospective Pilot Study Comparing Clinical and Patient-Related Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setup
2.2. Patient Characteristics
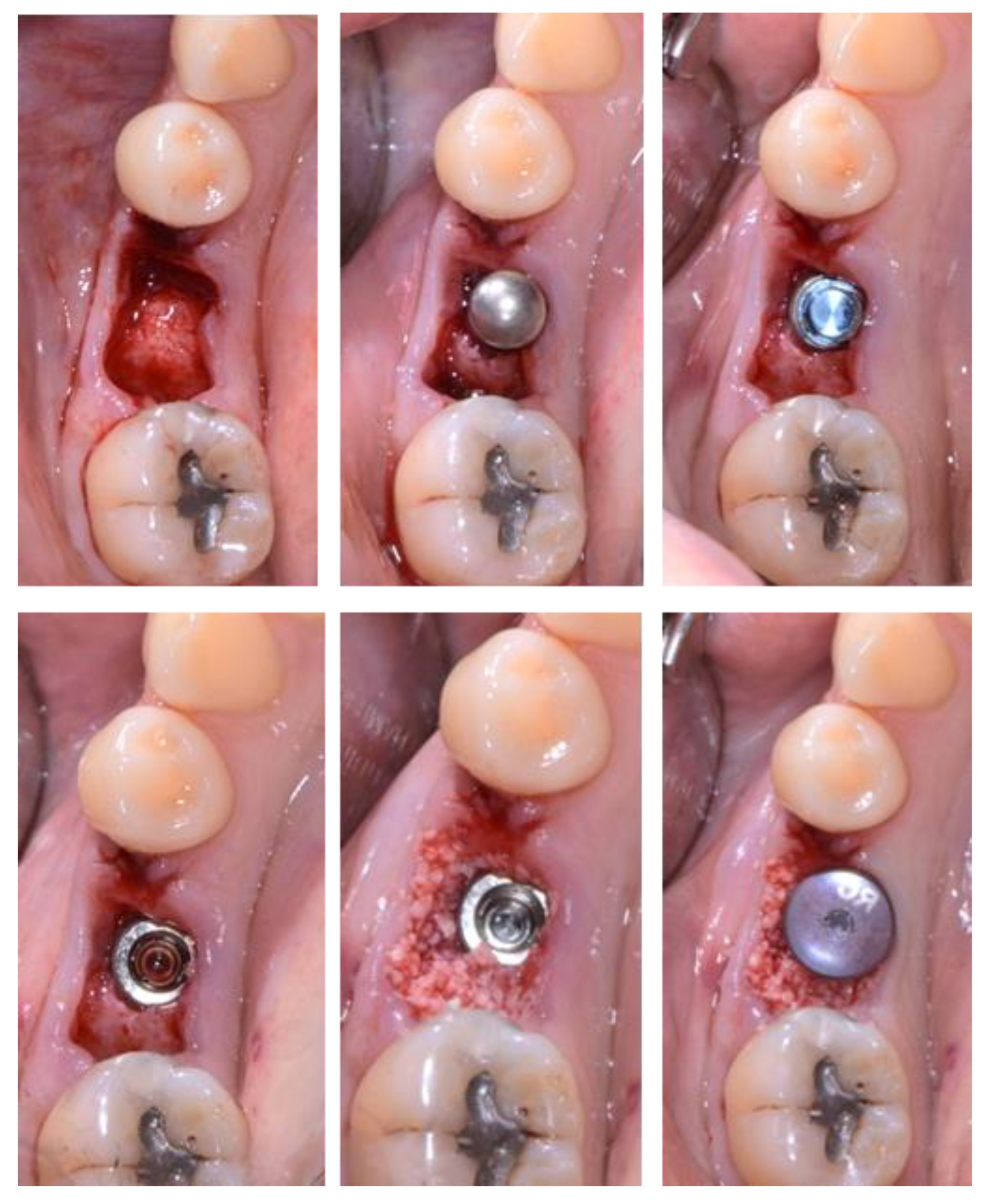
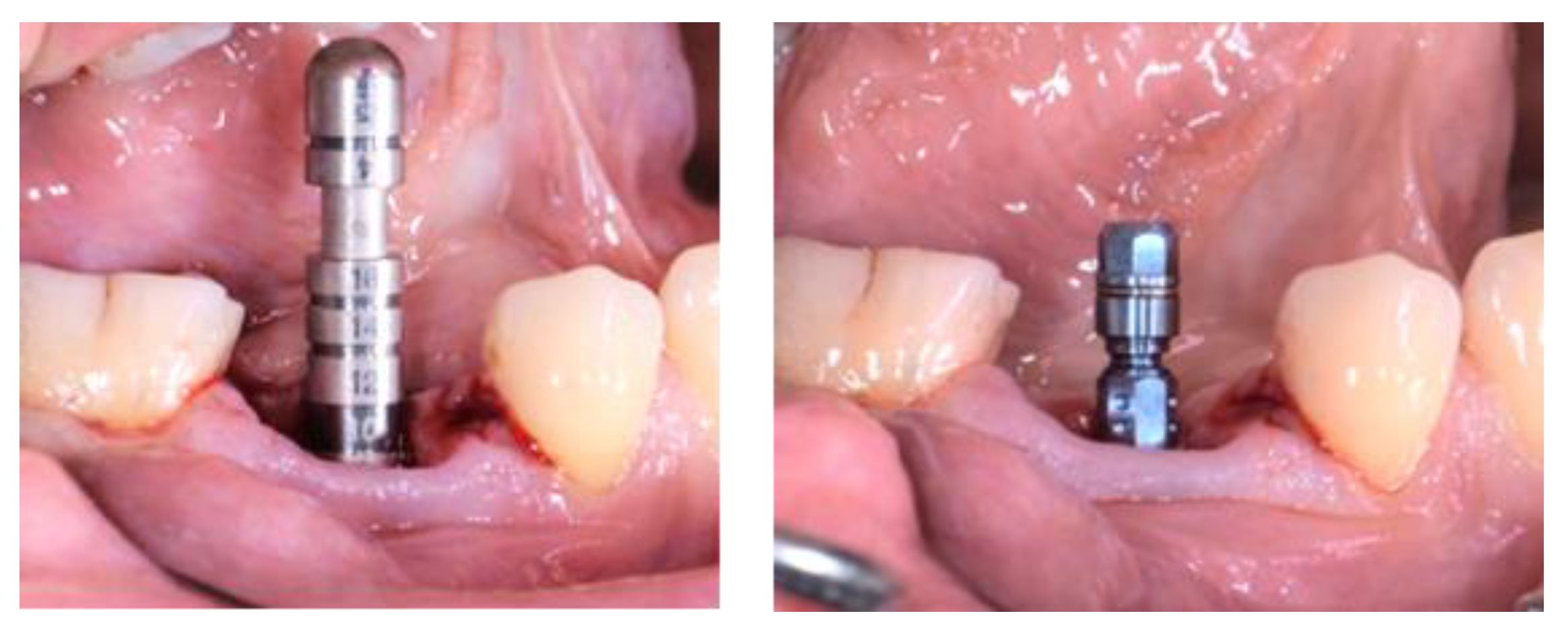
2.3. Treatment Procedure
2.4. Data Collection and Analysis
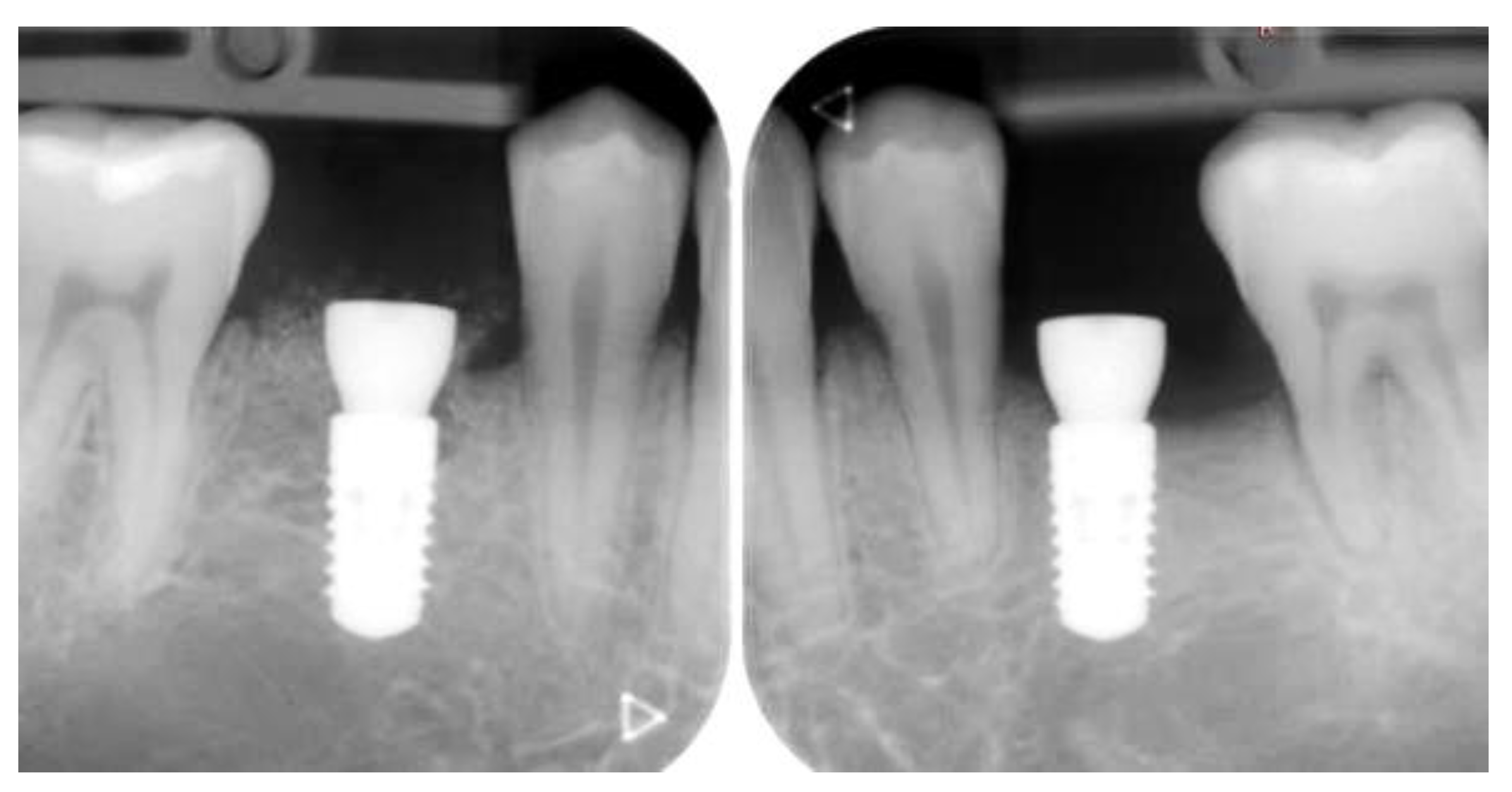
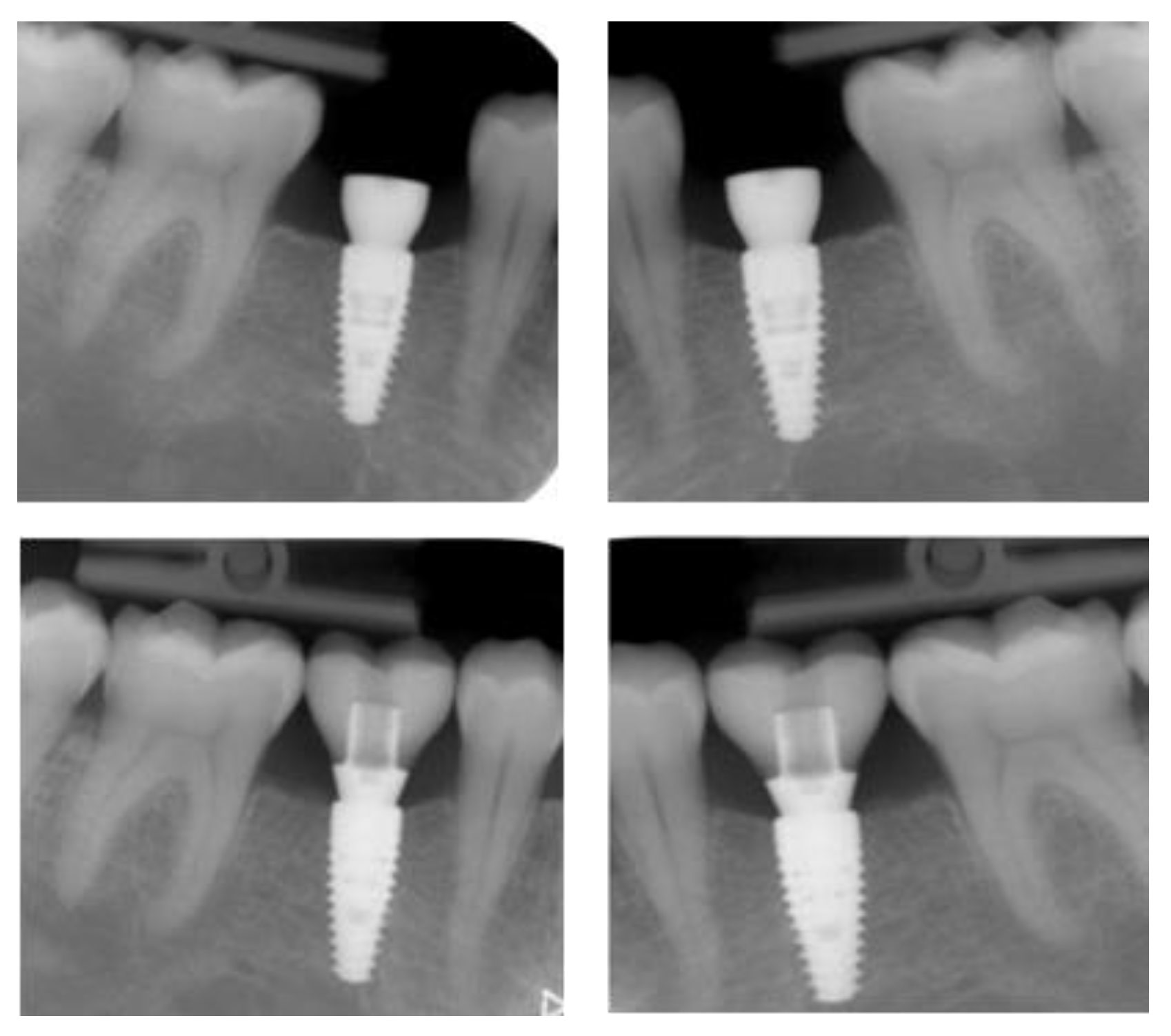
2.4.1. Radiographic Measurements
2.4.2. Patient and Clinician-Reported Outcomes
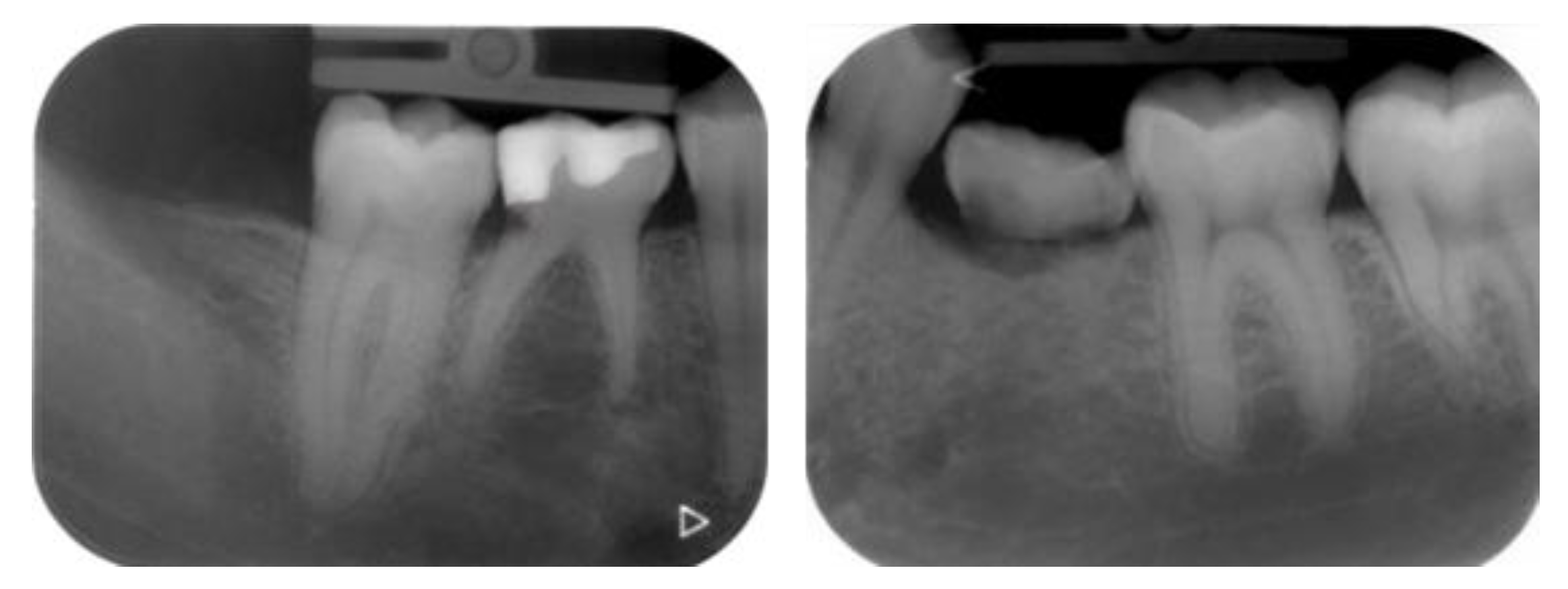
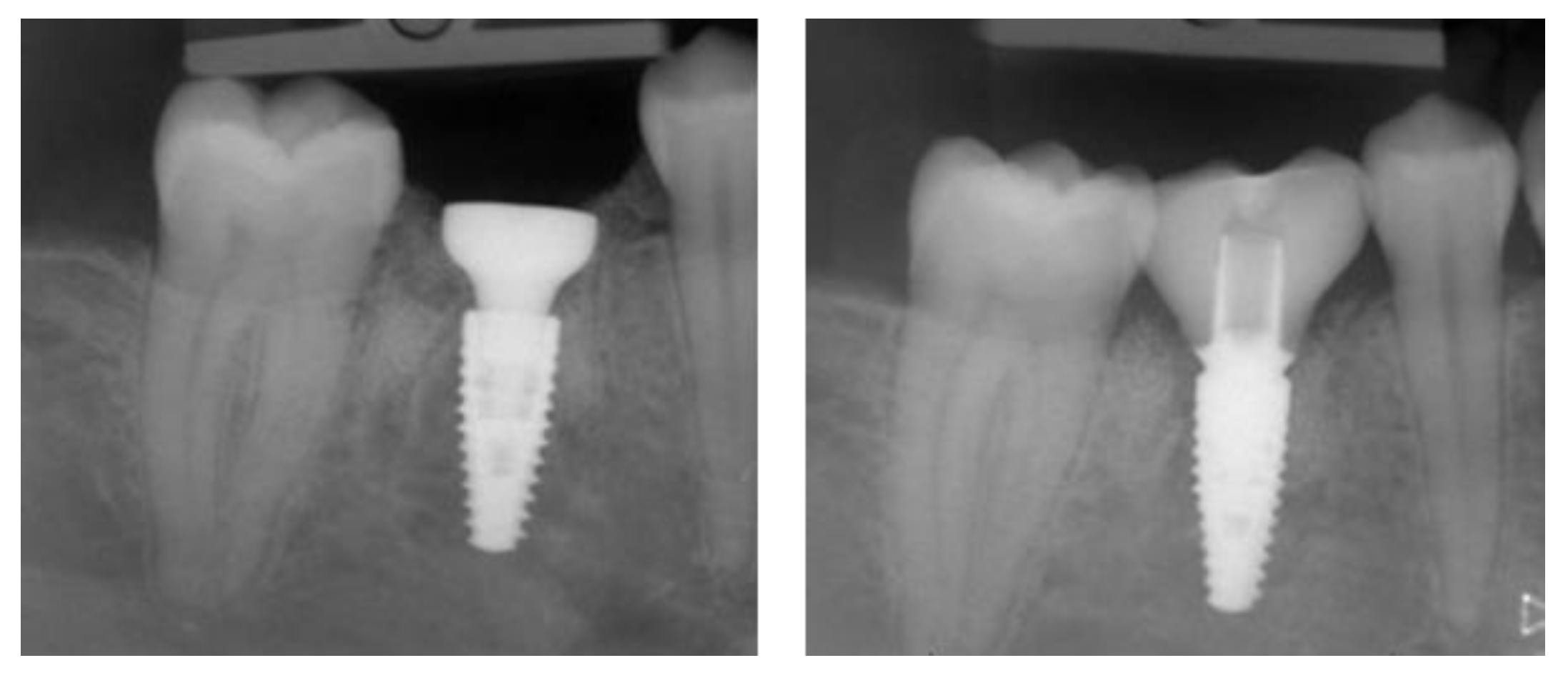
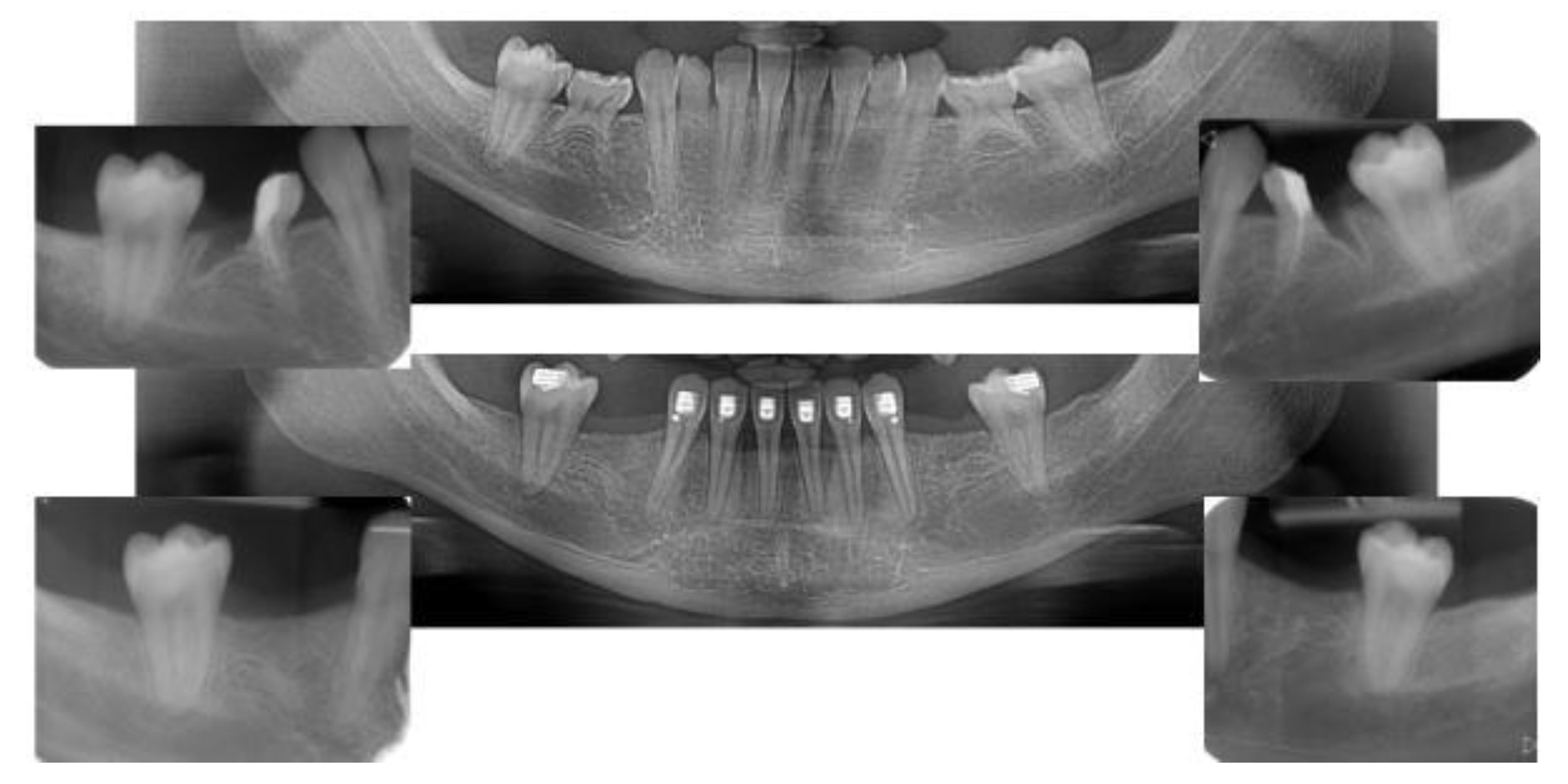
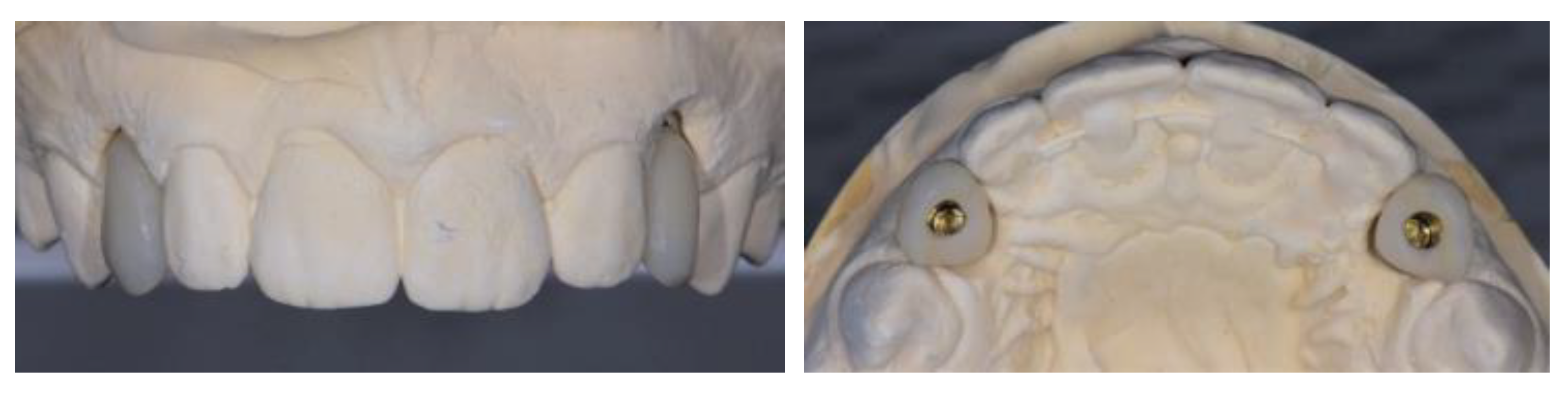
2.5. Individual Cases Description
- Case 1:
- Case 2:
- Case 3:
- Case 4:
- Case 5:
3. Results
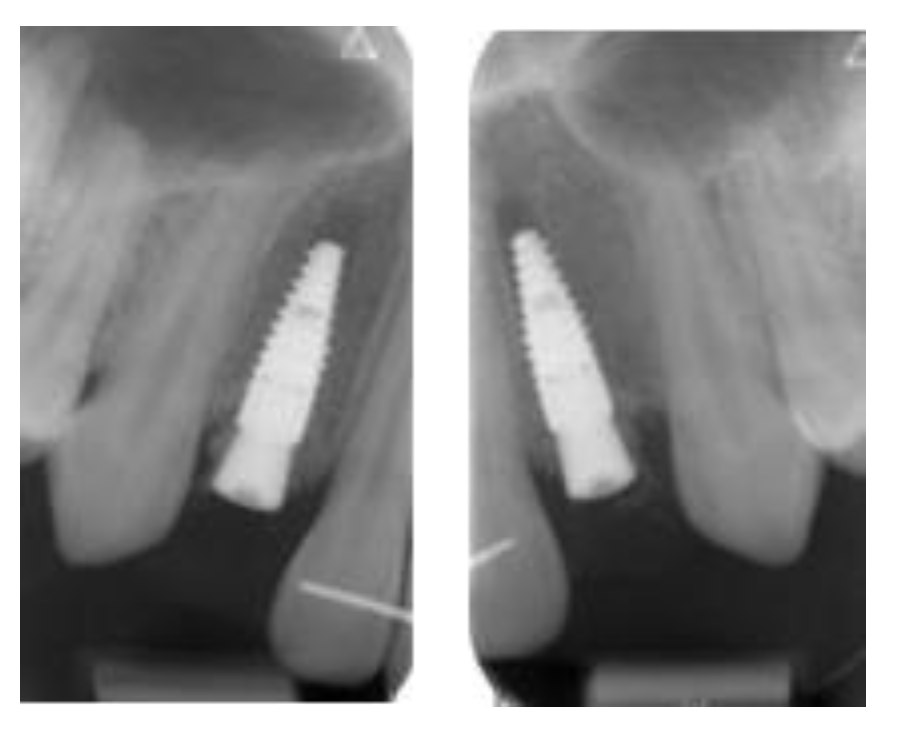
3.1. Clinical Results
3.2. Marginal Bone Level Outcomes
| Mesial Marginal Bone Level (2D) [mm] after Immediate Placement | ||||||||
|---|---|---|---|---|---|---|---|---|
| Patient | 1 | 2 | 3 | 4 | 5 | Median | IQR | |
| Implant position | 45 | 35 | 45 | 45 | 13 | 23 | NA | NA |
| Post-OP mesial | 1.8 | 0.0 | 0.1 | 3.0 | 0.4 | 0.4 | 0.4 | 0.18–1.45 |
| 1 year mesial | 0.6 | 0.0 | 0.1 | 1.5 | 0.1 | 0.1 | 0.1 | 0.1–0.48 |
| Post-OP distal | 1.2 | 0.0 | 0.1 | 3.0 | 0.4 | 0.4 | 0.4 | 0.18–1.0 |
| 1 year distal | 0.6 | 0.0 | 0.1 | 1.5 | 0.2 | 0.0 | 0.2 | 0.03–0.5 |
| Marginal Bone Level (2D) [mm] after Delayed Placement | ||||||||
|---|---|---|---|---|---|---|---|---|
| Patient | 1 | 2 | 3 | 4 | 5 | Median | IQR | |
| Implant position | 35 | 45 | 35 | 35 | 35 | 45 | NA | NA |
| Post-OP mesial | 2.0 | 1.0 | 0.2 | 0.6 | 0.2 | 0.2 | 0.4 | 0.2–0.9 |
| 1 year mesial | 1.6 | 0.5 | 0.0 | 0.3 | 0.1 | 0.1 | 0.3 | 0.1–0.45 |
| Post-OP distal | 0.0 | 0.5 | 0.0 | 0.6 | 0.1 | 0.1 | 0.1 | 0.03–0.4 |
| 1 year distal | 0.0 | 0.2 | 0.0 | 0.3 | 0.1 | 0.1 | 0.1 | 0.03–0.18 |
3.3. Patient Post-Surgical Pain, Preference, and Patient and Clinician Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bondemark, L.; Tsiopa, J. Prevalence of Ectopic Eruption, Impaction, Retention and Agenesis of the Permanent Second Molar. Angle Orthod. 2007, 77, 773–778. [Google Scholar] [CrossRef]
- Al-Ani, A.H.; Antoun, J.S.; Thomson, W.M.; Merriman, T.R.; Farella, M. Hypodontia: An Update on Its Etiology, Classification, and Clinical Management. BioMed Res. Int. 2017, 2017, 9378325. [Google Scholar] [CrossRef] [PubMed]
- Nunn, J.H.; Carter, N.E.; Gillgrass, T.J.; Hobson, R.S.; Jepson, N.J.; Meechan, J.G.; Nohl, F.S. The Interdisciplinary Management of Hypodontia: Background and Role of Paediatric Dentistry. Br. Dent. J. 2003, 194, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Brook, A.H. Dental Anomalies of Number, Form and Size: Their Prevalence in British Schoolchildren. J. Int. Assoc. Dent. Child 1974, 5, 37–53. [Google Scholar]
- Flores-Mir, C. More Women in Europe and Australia Have Dental Agenesis than Their Counterparts in North America: What Is the Prevalence of Dental Agenesis of Permanent Teeth? Evid. Based Dent. 2005, 6, 22–23. [Google Scholar] [CrossRef] [PubMed]
- Polder, B.J.; Van’t Hof, M.A.; Van Der Linden, F.P.G.M.; Kuijpers-Jagtman, A.M. A Meta-Analysis of the Prevalence of Dental Agenesis of Permanent Teeth. Commun. Dent. Oral Epidemiol. 2004, 32, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Bjerklin, K.; Al-Najjar, M.; Karestedt, H.; Andren, A. Agenesis of Mandibular Second Premolars with Retained Primary Molars. A Longitudinal Radiographic Study of 99 Subjects from 12 Years of Age to Adulthood. Eur. J. Orthod. 2008, 30, 254–261. [Google Scholar] [CrossRef]
- Hvaring, C.L.; Ogaard, B.; Stenvik, A.; Birkeland, K. The Prognosis of Retained Primary Molars without Successors: Infraocclusion, Root Resorption and Restorations in 111 Patients. Eur. J. Orthod. 2014, 36, 26–30. [Google Scholar] [CrossRef]
- Dos Santos, C.C.O.; Melo, D.L.; da Silva, P.P.; Normando, D. What Is the Survival Rate of Deciduous Molars in Cases with Agenesis of Premolar Successors? A Systematic Review. Angle Orthod. 2022, 92, 110–117. [Google Scholar] [CrossRef]
- Parise Gré, C.; Schweigert Bona, V.; Pedrollo Lise, D.; Monteiro Júnior, S. Esthetic Rehabilitation of Retained Primary Teeth-A Conservative Approach: Rehabilitation of Retained Primary Teeth. J. Prosthodont. 2019, 28, e41–e44. [Google Scholar] [CrossRef]
- Kiliaridis, S.; Sidira, M.; Kirmanidou, Y.; Michalakis, K. Treatment Options for Congenitally Missing Lateral Incisors. Eur. J. Oral Implantol. 2016, 9 (Suppl. 1), S5–S24. [Google Scholar] [PubMed]
- Yap, A.K.W.; Klineberg, I. Dental Implants in Patients with Ectodermal Dysplasia and Tooth Agenesis: A Critical Review of the Literature. Int. J. Prosthodont. 2009, 22, 268–276. [Google Scholar]
- Priest, G. The Treatment Dilemma of Missing Maxillary Lateral Incisors-Part II: Implant Restoration. J. Esthet. Restor. Dent. 2019, 31, 319–326. [Google Scholar] [CrossRef] [PubMed]
- King, P.; Maiorana, C.; Luthardt, R.; Sondell, K.; Øland, J.; Galindo-Moreno, P.; Nilsson, P. Clinical and Radiographic Evaluation of a Small-Diameter Dental Implant Used for the Restoration of Patients with Permanent Tooth Agenesis (Hypodontia) in the Maxillary Lateral Incisor and Mandibular Incisor Regions: A 36-Month Follow-Up. Int. J. Prosthodont. 2016, 29, 147–153. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heuberer, S.; Dvorak, G.; Mayer, C.; Watzek, G.; Zechner, W. Dental Implants Are a Viable Alternative for Compensating Oligodontia in Adolescents. Clin. Oral Implant. Res. 2015, 26, e22–e27. [Google Scholar] [CrossRef]
- Buser, D.; Chappuis, V.; Belser, U.C.; Chen, S. Implant Placement Post Extraction in Esthetic Single Tooth Sites: When Immediate, When Early, When Late? Periodontol. 2000 2017, 73, 84–102. [Google Scholar] [CrossRef]
- Koh, R.U.; Rudek, I.; Wang, H.-L. Immediate Implant Placement: Positives and Negatives. Implant. Dent. 2010, 19, 98–108. [Google Scholar] [CrossRef]
- Covani, U.; Cornelini, R.; Calvo-Guirado, J.L.; Tonelli, P.; Barone, A. Bone Remodeling around Implants Placed in Fresh Extraction Sockets. Int. J. Periodontics Restor. Dent. 2010, 30, 601–607. [Google Scholar]
- Schropp, L.; Isidor, F. Timing of Implant Placement Relative to Tooth Extraction. J. Oral Rehabil. 2008, 35, 33–43. [Google Scholar] [CrossRef]
- De Rouck, T.; Collys, K.; Wyn, I.; Cosyn, J. Instant Provisionalization of Immediate Single-Tooth Implants Is Essential to Optimize Esthetic Treatment Outcome. Clin. Oral Implant. Res. 2009, 20, 566–570. [Google Scholar] [CrossRef]
- Perez, A.; Valente, N.A.; Trottet, L.; Chatelain, S.; Alfonsi, F.; Barone, A. Immediate Implants in the Esthetic Area: Our Perspective and Clinical Guidelines. J. Oral Sci. Rehabil. 2018, 4, 16–23. [Google Scholar]
- Cosyn, J.; Eghbali, A.; Hermans, A.; Vervaeke, S.; De Bruyn, H.; Cleymaet, R. A 5-Year Prospective Study on Single Immediate Implants in the Aesthetic Zone. J. Clin. Periodontol. 2016, 43, 702–709. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Polyzos, I.P.; Felice, P.; Worthington, H.V. Timing of Implant Placement after Tooth Extraction: Immediate, Immediate-Delayed or Delayed Implants? A Cochrane Systematic Review. Eur. J. Oral Implantol. 2010, 3, 189–205. [Google Scholar] [PubMed]
- Kinaia, B.M.; Shah, M.; Neely, A.L.; Goodis, H.E. Crestal Bone Level Changes around Immediately Placed Implants: A Systematic Review and Meta-Analyses with at Least 12 Months’ Follow-up after Functional Loading. J. Periodontol. 2014, 85, 1537–1548. [Google Scholar] [CrossRef] [PubMed]
- Moraschini, V.; Porto Barboza, E. Immediate versus Conventional Loaded Single Implants in the Posterior Mandible: A Meta-Analysis of Randomized Controlled Trials. Int. J. Oral Maxillofac. Surg. 2016, 45, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Al-Sawai, A.-A.; Labib, H. Success of Immediate Loading Implants Compared to Conventionally-Loaded Implants: A Literature Review. J. Investig. Clin. Dent. 2016, 7, 217–224. [Google Scholar] [CrossRef]
- Kan, J.Y.K.; Rungcharassaeng, K.; Deflorian, M.; Weinstein, T.; Wang, H.-L.; Testori, T. Immediate Implant Placement and Provisionalization of Maxillary Anterior Single Implants. Periodontol. 2000 2018, 77, 197–212. [Google Scholar] [CrossRef]
- Bertl, K.; Bertl, M.H.; Heimel, P.; Burt, M.; Gahleitner, A.; Stavropoulos, A.; Ulm, C. Alveolar Bone Resorption after Primary Tooth Loss Has a Negative Impact on Straightforward Implant Installation in Patients with Agenesis of the Lower Second Premolar. Clin. Oral Implant. Res. 2018, 29, 155–163. [Google Scholar] [CrossRef]
- Weber, H.P.; Buser, D.; Fiorellini, J.P.; Williams, R.C. Radiographic Evaluation of Crestal Bone Levels Adjacent to Nonsubmerged Titanium Implants. Clin. Oral Implant. Res. 1992, 3, 181–188. [Google Scholar] [CrossRef]
- Brånemark, P.I.; Hansson, B.O.; Adell, R.; Breine, U.; Lindström, J.; Hallén, O.; Ohman, A. Osseointegrated Implants in the Treatment of the Edentulous Jaw. Experience from a 10-Year Period. Scand. J. Plast. Reconstr. Surg. Suppl. 1977, 16, 1–132. [Google Scholar]
- Gotfredsen, K.; Carlsson, G.E.; Jokstad, A.; Fyrberg, K.A.; Berge, M.; Bergendal, B.; Bergendal, T.; Ellingsen, J.-E.; Gunne, J.; Hofgren, M.; et al. Implants and/or Teeth: Consensus Statements and Recommendations. J. Oral. Rehabil. 2008, 35, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.T.; Beagle, J.; Jensen, S.S.; Chiapasco, M.; Darby, I. Consensus Statements and Recommended Clinical Procedures Regarding Surgical Techniques. Int. J. Oral Maxillofac. 2009, 24, 272–278. [Google Scholar]
- Hämmerle, C.H.F.; Chen, S.T.; Wilson, T.G. Consensus Statements and Recommended Clinical Procedures Regarding the Placement of Implants in Extraction Sockets. Int. J. Oral Maxillofac. Implants 2004, 19, 26–28. [Google Scholar] [PubMed]
- Chen, S.T.; Buser, D. Esthetic Outcomes Following Immediate and Early Implant Placement in the Anterior Maxilla--a Systematic Review. Int. J. Oral. Maxillofac. Implants 2014, 29, 186–215. [Google Scholar] [CrossRef]
- Canellas, J.V.D.S.; Medeiros, P.J.D.; Figueredo, C.M.D.S.; Fischer, R.G.; Ritto, F.G. Which Is the Best Choice after Tooth Extraction, Immediate Implant Placement or Delayed Placement with Alveolar Ridge Preservation? A Systematic Review and Meta-Analysis. J. Cranio-Maxillofac. Surg. 2019, 47, 1793–1802. [Google Scholar] [CrossRef]
- Perez, A.; Caiazzo, A.; Valente, N.A.; Toti, P.; Alfonsi, F.; Barone, A. Standard vs. Customized Healing Abutments with Simultaneous Bone Grafting for Tissue Changes around Immediate Implants. 1-year Outcomes from a Randomized Clinical Trial. Clin. Implant Dent. Relat. Res. 2020, 22, 42–53. [Google Scholar] [CrossRef]
- Sarnachiaro, G.O.; Chu, S.J.; Sarnachiaro, E.; Gotta, S.L.; Tarnow, D.P. Immediate Implant Placement into Extraction Sockets with Labial Plate Dehiscence Defects: A Clinical Case Series: Implant Placement into Sockets with Defects. Clin. Implant Dent. Relat. Res. 2016, 18, 821–829. [Google Scholar] [CrossRef]
- Donos, N.; Asche, N.V.; Akbar, A.N.; Francisco, H.; Gonzales, O.; Gotfredsen, K.; Haas, R.; Happe, A.; Leow, N.; Navarro, J.M.; et al. Impact of Timing of Dental Implant Placement and Loading: Summary and Consensus Statements of Group 1-The 6th EAO Consensus Conference 2021. Clin. Oral Implants Res. 2021, 32 (Suppl. 21), 85–92. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Cortellini, P.; Graziani, F.; Cairo, F.; Lang, N.P.; Abundo, R.; Conforti, G.P.; Marquardt, S.; Rasperini, G.; Silvestri, M.; et al. Immediate versus Delayed Implant Placement after Anterior Single Tooth Extraction: The Timing Randomized Controlled Clinical Trial. J. Clin. Periodontol. 2017, 44, 215–224. [Google Scholar] [CrossRef]
- Roccuzzo, A.; Imber, J.; Lempert, J.; Hosseini, M.; Jensen, S.S. Narrow Diameter Implants to Replace Congenital Missing Maxillary Lateral Incisors: A 1-year Prospective, Controlled, Clinical Study. Clin. Oral Implant. Res. 2022, 33, 844–857. [Google Scholar] [CrossRef]
- Attia, S.; Schaaf, H.; El Khassawna, T.; Malhan, D.; Mausbach, K.; Howaldt, H.-P.; Streckbein, P. Oral Rehabilitation of Hypodontia Patients Using an Endosseous Dental Implant: Functional and Aesthetic Results. J. Clin. Med. 2019, 8, 1687. [Google Scholar] [CrossRef]
- Butera, A.; Pascadopoli, M.; Pellegrini, M.; Gallo, S.; Zampetti, P.; Cuggia, G.; Scribante, A. Domiciliary Use of Chlorhexidine vs. Postbiotic Gels in Patients with Peri-Implant Mucositis: A Split-Mouth Randomized Clinical Trial. Appl. Sci. 2022, 12, 2800. [Google Scholar] [CrossRef]
- Butera, A.; Pascadopoli, M.; Pellegrini, M.; Gallo, S.; Zampetti, P.; Scribante, A. Oral Microbiota in Patients with Peri-Implant Disease: A Narrative Review. Appl. Sci. 2022, 12, 3250. [Google Scholar] [CrossRef]
- Vale, G.C.; Mayer, M.P.A. Effect of Probiotic Lactobacillus Rhamnosus By-Products on Gingival Epithelial Cells Challenged with Porphyromonas Gingivalis. Arch. Oral Biol. 2021, 128, 105174. [Google Scholar] [CrossRef] [PubMed]



















| Patient | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Gender | M | F | F | M | F |
| Age | 24 | 35 | 44 | 27 | 21 |
| Tooth agenesis | 35, 45 | 35, 45 | 35, 45 | 35, 45 | 35, 45, 14, 17, 24, 27, 44, 47, 34, 37 |
| Implant Type | BLT RC | BLT RC | BLT RC | #45: BLT RC #35: BL RC | #13, 23: BLT NC #35, 45: BL RC |
| Implant dimensions | #35: Ø4.1 × 10 #45: Ø4.1 × 10 | #35: Ø4.1 × 10 #45: Ø4.1 × 10 | #35: Ø4.1 × 10 #45: Ø4.1 × 10 | #35: Ø4.1 × 10 #45: Ø4.1 × 10 | #13, 23: Ø3.3 × 12 #35, 45: Ø4.1 × 10 |
| Insertion Torque [N/cm] | #35: 33 #45: 30 | #35: 45 #45: 40 | #35: 36 #45: 39 | #35: 35 #45: 37 | #13: 35, #23: 38 #35: 40, #45: 40 |
| Patient | ||||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| Immediate (L/R) | R (45) | L (35) | R (45) | R (45) | R (13) | L (23) |
| 3 days | 0 | 0 | 1 | 1 | 0 | 0 |
| 1 week | 0 | 0 | 0 | 0 | 0 | 0 |
| 2 months | 0 | 0 | 0 | 0 | 0 | 0 |
| Delayed (L/R) | L (35) | R (45) | L (35) | L (35) | L (35) | R (45) |
| 3 days | 3 | 3 | 1 | 2 | 3 | 2 |
| 1 week | 1 | 0 | 0 | 1 | 1 | 0 |
| 2 months | 0 | 0 | 0 | 0 | 0 | 0 |
| Category | Patient Satisfaction | Clinician Satisfaction | ||
|---|---|---|---|---|
| N | % | N | % | |
| Not reported | 0 | 0% | 0 | 0% |
| Completely satisfied | 4 | 80% | 5 | 100% |
| Partly satisfied | 1 | 20% | 0 | 0% |
| Not satisfied | 0 | 0% | 0 | 0% |
| Not able to judge | 0 | 0% | 0 | 0% |
| Category | Patient Satisfaction | Clinician Satisfaction | ||
|---|---|---|---|---|
| N | % | N | % | |
| Not reported | 0 | 0% | 0 | 0% |
| Completely satisfied | 5 | 100% | 5 | 100% |
| Partly satisfied | 1 | 0% | 0 | 0% |
| Not satisfied | 0 | 0% | 0 | 0% |
| Not able to judge | 0 | 0% | 0 | 0% |
| Treatment Preference | Reason | |||
|---|---|---|---|---|
| N | % | N | % | |
| Not reported | 0 | 0% | 0 | 0% |
| Immediate | 4 | 80% | Less pain and faster (4), Immediate restoration (1) | 80% |
| Delayed | 0 | 0% | 0 | 0% |
| No difference | 1 | 20% | Same perception | 0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alexandre, P.; Hamzah, S.; Lombardi, T. Immediate versus Delayed Implant Placement in Patients with Tooth Agenesis: An In-Line Retrospective Pilot Study Comparing Clinical and Patient-Related Outcomes. Appl. Sci. 2023, 13, 9368. https://doi.org/10.3390/app13169368
Alexandre P, Hamzah S, Lombardi T. Immediate versus Delayed Implant Placement in Patients with Tooth Agenesis: An In-Line Retrospective Pilot Study Comparing Clinical and Patient-Related Outcomes. Applied Sciences. 2023; 13(16):9368. https://doi.org/10.3390/app13169368
Chicago/Turabian StyleAlexandre, Perez, Shabana Hamzah, and Tommaso Lombardi. 2023. "Immediate versus Delayed Implant Placement in Patients with Tooth Agenesis: An In-Line Retrospective Pilot Study Comparing Clinical and Patient-Related Outcomes" Applied Sciences 13, no. 16: 9368. https://doi.org/10.3390/app13169368
APA StyleAlexandre, P., Hamzah, S., & Lombardi, T. (2023). Immediate versus Delayed Implant Placement in Patients with Tooth Agenesis: An In-Line Retrospective Pilot Study Comparing Clinical and Patient-Related Outcomes. Applied Sciences, 13(16), 9368. https://doi.org/10.3390/app13169368








