Featured Application
Specific application or a potential application of the work includes novel solutions in exoskeletons technology.
Abstract
An aging population, the effects of pandemics and civilization-related conditions, and limited leapfrogging in the number of rehabilitation and physiotherapy specialists are driving demand for modern assistive technologies, especially upper and lower limb exoskeletons. Patient-tailored devices are a rapidly developing group of technologies, both from a biomechanics, informatics, and materials engineering perspective. In particular, the technological development of 3D printing, the expanding range of available materials and their properties (including contact with living tissue and bodily fluids), and the possibility of selecting and optimizing them using artificial intelligence (including machine learning) are encouraging the emergence of new concepts, particularly within the Industry 4.0 paradigm. The article provides an overview of what is available in this area, including an assessment of as yet untapped research and industrial and, in part, clinical potential.
1. Introduction
Exoskeletons, personalized to the patient’s needs, are a dynamically developing group of technologies, combining the achievements of biomechanics, computer science, material engineering, and clinical disciplines. In particular, technological development in the field of 3D printing expands the number of available materials and the range of their properties, including in the area of mechanical parameters or contact of the print with living tissue and body fluids. This also applies to increasing the possibilities of selecting and optimizing individual solutions using artificial intelligence (AI), including machine learning (ML), i.e., a data-driven approach. This is conducive to the emergence of new concepts, especially within the Industry 4.0 and Industry 5.0 paradigms. The first of the above paradigms includes the wider use of computerization, robotization, automation, artificial intelligence, and technical control throughout the entire production process [1,2,3,4]. It accelerates green and digital transitions through the effective development of self-managing production processes based on open software and secure communication standards, allowing for direct communication and cooperation among many sensors, controllers, machines, devices, logistics systems, products, and services within the Internet of Things (IoT). The second paradigm, an emerging one, places man and his environment at the center of the production process, creating favorable conditions for the transformation towards a more sustainable, resilient, and human-centered industry [5].
Technological developments, the opening up of clinical practice (diagnosis, treatment, rehabilitation, and care) to computerization, robotization, automation, and reliance on artificial intelligence (AI), 3D scanning, and 3D printing (including living tissues), not only allow avoidance of hospitalization or reduced length of stay in the hospital, a faster transition to increasingly effective rehabilitation but also gives new meaning to the term ‘disabled person’. The number of economically active people with disabilities, children with disabilities learning and taking an active part in the life of their communities, or elderly people becoming active despite neurodegenerative deficits are just some of the daily visible effects of this revolution. The growing interest of scientists and clinicians in modern technologies and their wider availability do not always translate into their comprehensive use, but rather their use as part of pilot projects and research, often interdisciplinary. Exoskeletons combined with functional electrical stimulation (FES) and brain-computer interfaces are already being used. However, most are designed for gait and posture rehabilitation, particularly in stroke patients, and less commonly in patients with fractures near the hip joint and arthroplasty or implantation of a knee prosthesis. Another revolution is the prosthesis with haptic functions, restoring not only the possibility of movement but also feeling [6].
It must be remembered that this development will not be possible without the collection of sufficiently large data sets, patient cases, and the resulting experience and knowledge of specialists and their supporting systems.
Data, both from healthy people and patients, as well as from the observations and tips of specialists, are a key element necessary for the stimulation of the development of modern medicine, from prevention and early screening diagnostics to the last stages of patient care. This creates opportunities to improve the quality of monitoring of health outcomes, including quality of life, rehabilitation, and care needs, which are often unrecognized without an external professional assessment. It also provides convergence of health data from purely clinical to electronically monitored (blood pressure measurement or sensors for runners) to self-reported observations or as a result of social media counseling, etc. On the other hand, data collection should be organized in the form of an information system, and data at the micro- and macro-levels should complement each other and contribute to the creation of new knowledge, perhaps also identifying gaps and catalyzing needs as part of dedicated, personalized diagnostics, therapy, rehabilitation, and care. Hence the need not only to disseminate sensors but also to extract biomarkers and algorithms that infer from their complex configurations about the future state of health, identify potential interventions, and warn of deterioration [7].
In this context, 3D printing of exoskeletons, their optimization based on AI, and the resulting virtual rehabilitation already have great potential, both in the form of independent, relatively low-cost, precise personalized interventions for patients as well as elements of larger systems that collect and process biomedical data and carry subsequent phases of development, including those based on new materials or 3D printing technologies unknown today. This article aims to provide an overview of the materials and technologies available in the above-mentioned area, including an assessment of how far their identified research and industrial, and partly clinical, potential has been realized to date (Table 1).

Table 1.
Milestones in 3D printing.
The history of the development of 3D printing, particularly in the area of medical applications such as the exoskeletons we are designing, has been inextricably linked since the 1980s to the support of technology, processes, and data analysis (inputs, process parameters, product lifecycle) through AI (Figure 1).
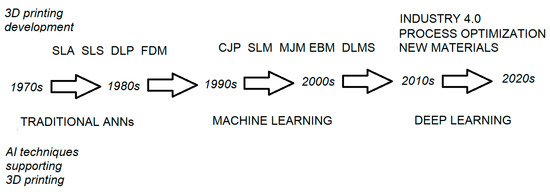
Figure 1.
Milestones in 3D printing versus the development of AI technologies supporting them.
Identifying and disseminating the role of AI in the design and manufacture of personalized 3D printed products, in particular upper limb exoskeletons, in the light of our own research is presented in Figure 2. With regard to the support of 3D printing with AI, greater importance is given to the
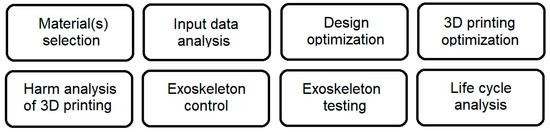
Figure 2.
Key areas of 3D printing exoskeleton support based on AI.
- Collection of data and designs in repositories;
- Data auditing (including for further use by AI);
- Cyber security, as the consequences of negligence in this area can be disastrous for individuals or company operations;
- Analysis of bulk data extracted from Internet of Things (IoT) systems, including within the Industry 4.0 or eHealth paradigms.
2. Materials Development
The basic materials used for 3D printing include:
- PET (polyethylene terephthalate), also PETG (combined with glycerol/glycerin, the simplest stable trihydric alcohol).
- HIPS—high-impact polystyrene.
- ABS—acrylonitrile-butadiene-styrene terpolymer.
- FLEX—a mix of materials with increased flexibility for printing seals and energy absorbers, also in versions with increased resistance to operating fluids (oils, etc.) and chemicals (paints, varnishes, solvents, etc.).
- special materials: silicon carbide, silicon nitride, aluminum oxide, zirconium dioxide, materials with mineral additives, or wood.
- metal powders: titanium (medical Ti6Al4V), stainless steel, cobalt-chrome, CoCrMo (cobalt-chromium-molybdenum), copper.
- medical polymeric materials with metallic properties, such as PEEK.
Thermosetting photopolymers account for almost half of the 3D printing materials market. Low-budget 3D printers printing with FDM technology mainly use ABS and PLA.
The starting point for material technology in medical 3D printing seems obvious. The variety of new materials allows the selection (and, over time, also combining) of plastics, materials with properties similar to glass or ceramics, metals (steel, titanium, aluminum), living cells, and multi-material printing, enabling even the incorporation of electronic printed circuits into exoskeletons without the need to install them separately. The exoskeletons obtained in this way are already lighter and more compact, and over time they can become even more energy-efficient, which will extend their autonomy and give their users greater independence. Unfortunately, so far we have not used all the possibilities in this area, and most of the 3D printing materials are still waiting for their chance to be tested in real products.
From the material side, 3D printed exoskeletons require not only optimization of material properties (chemical and physical parameters) but also complex 3D printing processes that maximize the effect. The requirements also apply to the inclusion of non-printed parts (e.g., joints, bearings, or load-bearing elements), including the total mass of the exoskeleton and its distribution, which is most often compared to the distribution of weight in a natural limb. The exoskeleton must be a solution to a dynamic system of equations with many variables that are highly correlated with each other and often must remain in dynamic equilibrium. Despite the progress in the area of 3D printing materials, their effectiveness is still limited by both a large number of process features that need to be optimized as well as the need to personalize the exoskeleton and the specific scope of requirements that cannot be changed (dimensions and weight of individual elements of the exoskeleton, ranges, and speeds of movement). The progress in the area of computational methods and techniques is noticeable here—it was observed that compared to the results from the approach based on traditional artificial neural networks (ANN), material optimization implemented by means of deep learning (DL) improved the quality of products as well as allowed to take into account in planning and producing a wider set of printing parameters not previously found. Hence, despite proven solutions, it is worth looking for new ones with perhaps greater potential and wider applications, as well as implementing several previous stages in one computational process, by taking into account a greater number of potential sets of features and solutions, perhaps too complex for traditional approaches [8].
We can already see how the hitherto relatively simple rehabilitation or telerehabilitation systems are evolving into advanced systems that creatively improve the motivation of exercisers and increase the effectiveness of existing rehabilitation techniques and physical exercises. Not only an objective assessment of movement but also a holistic approach within the paradigm of evidence-based medicine is becoming increasingly important. Hence, such an important element as the material from which the device for exercise and daily support of functions is made for almost 24 h a day (the exoskeleton), being in constant contact with the living tissue of the user, must be of significant objective importance for the effectiveness of the entire therapeutic process, which must be estimated or measured and taken into account in the treatment planning process. This poses much greater requirements than the traditional selection of, e.g., orthoses because both the range of supported functions and the therapeutic impact are much wider and more multidimensional. It is like comparing a wheelchair on a ramp to climbing stairs freely. The accumulation of potential users means that immediately after exoskeletons gain sufficiently high popularity, there may be a revolution in other areas, such as urban planning or the automotive industry, because even patients after a stroke or other neurological or neurodegenerative diseases will be able to use them, and the group of users will expand. This is due to both the therapeutic and preventive roles of the exoskeleton, such as preventing the progression of neuromuscular pathologies by moving in an upright position. This progress, however, may cause an increase in the prices of plastics and actuators, even greater with intensive use and the frequent need to replace worn-out exoskeletal elements. Despite the possibility of recycling, it is worth ensuring the optimization of the selection of materials and 3D printing procedures, which will ensure less filament consumption (up to approx. 17%), reduce the amount of waste and its potential impact on the environment, reduce the time needed for the full diagnostic and production processes, and reduce their costs. As a whole, they shorten the time of institutionalized rehabilitation and accelerate the achievement of independence, which affects the user’s self-esteem and quality of life. Maintaining the high quality of personalized 3D printed medical products with some cost reduction (due to less waste of materials) can provide a competitive advantage, also thanks to the image of a company that cares about the environment. A non-optimal combination of material properties, technological parameters, and construction may weaken the achievable effectiveness, intensity, complexity, and specificity of exercises with the use of an exoskeleton. Personalized 3D printed solutions still need to be subject to computational optimization of the 3D printing process in terms of features and selection of materials in order to achieve, for example, the maximum tensile strength of the hand exoskeleton component based on the optimization of an artificial neural network (ANN) supported by genetic algorithms (GA). This requires a comparison of selected (key) parameters of at least two different materials for 3D printing using an ANN supported by a genetic algorithm, built and trained in the MATLAB environment, in terms of a specific criterion of maximizing the maximum tensile force of the exoskeleton. The balance between technical possibilities and security limitations requires further analysis. Currently, such optimization methods are available for PLA and PLA+ [9].
Additive manufacturing can support the effective printing of personalized functional exoskeleton elements, and AI-based optimization can play a key role in increasing the efficiency and safety of the final product (a medical device) and supporting the sometimes seemingly contradictory limitations encountered when adapting the solution to the needs of the patient [10].
How far nature-inspired exoskeleton models can go has been shown by a study on the microstructure of the sea urchin Paracentrotus lividus exoskeleton and the extraction of design concepts, including the foamy (stereo) microstructure. The digital models took into account the number of knots, the thickness of the rods, and the smoothness of the meshes of such a Voronoi mesh and allowed the printing of cubic samples (3D structures) using the FFF (fonted filamentation) method with polylactic acid (PLA), olyme acid/polyhydroxyalkanoate compound (PLA/PHA), and wood fiber composite polylactic acid/polyhydroxyalkanoate (PLA/PHA). The mixture of PLA and PHA has little effect on the mechanical behavior of the print, and the addition of wood fibers results in a significant decrease in strength [11].
It must be taken into account that the formulas of raw materials and complex printing processes must ensure the stability of the solutions (parameter stability, or their thermal or aging compensation) [12].
Optimizing 3D printing procedures now focuses on AI-assisted design or injection simulation—this reduces filament consumption, reduces waste, and reduces environmental impact, but that is not all. The monitoring of materials and medical devices throughout the product lifecycle is driven by both the Medical Devices Regulation (MDR) and ISO13485 and should be cost-effective and socially promoted [13].
What is interesting is that humans are already able to produce by 3D printing bionic composite plates with properties far superior to natural ones. These properties range from classical impact resistance (at low velocity from a drop tower), the effect of layer angle on the resistance of the composite plate, or the mode of crack propagation in composite plates. The best results were obtained with the 0°/30°/0°/30° arrangement, and further research may result in the development of even more impact-resistant lightweight protective structures for exoskeleton components [14].
Biopolymers and their derivatives, including a carbohydrate polymer (highly deacetylated chitin—chitosan), can be widely used in the development of materials for 3D printing, including medical devices. The production of chitosan is mainly based on chitin from the exoskeleton of crustaceans or dung beetles (Heliocopris Hope). Chitosan extraction procedures (chitosan IR, SEM, NMR, ash content, and degree of deacetylation) are complex and result in the production of a 3D printable hydrogel, which can also be used in multi-material printing [15].
As we can see, the main materials used for the production of 3D-printed exoskeletons are PLA, followed by ABS. The possibilities are therefore vast, and new 3D printing materials are constantly emerging. For biomedical applications, we cannot forget about their classification, certification, and monitoring to ensure user safety. Perhaps the solution here is materials with a controlled shelf life that self-degrade after the expiration date, making them unusable.
3. Development of Technologies and Applications
3D printing in combination with AI increases versatility and allows for the process or product to be adapted to specific needs, often resulting in faster development/modification of the project, greater efficiency, and greater savings [16]. Even cheap exoskeletons can already generate traffic efficiently using open-source BCI configurations (e.g., OpenViBE) with an accuracy of 86% [17]. Combined metal-polymer elements can be a technological breakthrough in the field of 3D-printed exoskeletons. It is all about the strength properties of the combination of the metal shell and the metal-polymer filler [18]. The design challenges include, above all, the development of a 3D-printed exoskeleton of the hand with five fingers, physiological ranges of motion, adequate strength, and possible grips [19]. Work is still underway to standardize and maintain the quality of 3D-printed medical devices, which will grow as the technology matures [20]. In the process of designing and testing a 3D-printed exoskeleton, it is necessary to ensure the greatest usability and comfort, mainly through personalization, fitting, and testing [21]. The main component used to propel exoskeletons are artificial muscles, although current methods of producing them are difficult and laborious and require thorough computational simulations [22]. An effective and practical design of a 3D printed chainmail with programmed directional functions for the exoskeleton of the hand with variable stiffness/flexibility, depending on the direction, was also developed [23]. Often, also for exoskeletons, a rigid acrylonitrile butadiene styrene (ABS) structure is combined in the support area with a flexible thermoplastic polyurethane (TPU) structure [24]. Flexo soft exoskeleton weighs 330 g (with battery) and provides grip on objects up to 81 mm in diameter and grip force up to 48 N and grip on objects up to 81 mm in diameter when controlled via wireless sEMG or smartphone app for rehabilitation programs via Bluetooth [25]. Traditional rigid exoskeletons have numerous disadvantages, such as limited mobility, safety, ergonomics, autonomy, and high costs. Hence the attempts to develop a soft, textile exoskeleton (using 3D printed components and ready-made fabrics) to support elbow flexion and extension as well as opening and closing the hand with low power consumption, low weight, and low cost. The movement is controlled by a machine learning algorithm based on a system model built based on sensory data [26]. Similarly, a 3D-printed exoskeleton is pneumatically actuated by soft modules (EAsoftM) with passive joints (compensating for gravity) and active joints (moving the shoulder and elbow joints) [27]. The 3D printing of exoskeletons for children with motor deficits enables rapid prototyping, low costs, and easy adjustment to the patient’s dimensions [28]. Exoskeletons for wrist rehabilitation still have disadvantages, such as heavy weight, an uncertain trajectory of movement, etc. However, stable training of wrist rehabilitation in three degrees of freedom with compact and lightweight device characteristics can be achieved [29]. Exoskeletons can also be used by patients who have lost hand function due to burns [30]. A new, cheap, and effective in-home rehabilitation 3D printed exoskeleton for hand rehabilitation may have a spring and cable drive to transmit movement and force. In healthy individuals, activation of the extensor muscles of the fingers and flexors of the wrist increased by 184.1% and 197.8%, respectively. The weight of the device, less than 400 g, is still large [31]. Spinal cord injuries (SCI) also affect hand function and general movement. The 3D-printed hand-held exoskeleton (made of PLA) allows for control using electromyographic (EMG) signals and supports grip functions in patients after SCI in the cervical section (with tetraplegia) [32]. The Soft Flexible 3D Printed Composite Actuator (SECA) offers flexion and extension controlled by the predictive control method of the iterative learning model (ILMPC). This allows cylinder bending angles of up to 137° and an output force of 2.45 N [33]. A 3D-printed exoskeleton can also facilitate optimal guidance and placement of the cannula, which extends the functionality of the exoskeleton [34]. Disorders, weakness, or injuries to the hand may result in reduced grip strength and/or a limited ability to hold objects. Hence the effort to develop a five-fingered 3D-printed (ABS and acrylic) exoskeleton for the hand, will reduce the effort of gripping [35]. Exoskeletons may reduce complications and mortality from stroke and other severe neurological deficits, but possibly inefficient man-machine coupling in the exoskeleton could disrupt the wearer’s natural movement and even damage joints and muscles. The ergonomic soft 3D-printed exoskeleton with 7 degrees of freedom allows for partially solving the above-mentioned problems. Problems using the rules of functional anatomy and sports biomechanics (musculoskeletal tension line model). In patients in the exoskeleton, the similarity of the trajectory of human and platform movement exceeded 87%, muscle signals decreased by 58.17%, and the level of joint movement increased by 174% [36]. The fact that a high percentage of patients abandon supportive solutions, including exoskeletons, is indicated as a threat to therapy, which indicates the need for training and monitoring of use and, more broadly, promoting physical activity [37]. The use of polymer airbags allows monitoring of the interaction forces between the forearm and the rigid orthosis as well as data acquisition [38]. Most of the devices supporting the restoration of functional hand movement are very complex and expensive. Hence, attempts to develop budget solutions, e.g., a 3D printed thermoplastic exoskeleton to strengthen the grip, supporting the independent, reinforced movement of the index, middle, and ring fingers, equipped with three linear actuators, an Arduino-based control system, and a power supply [39]. It is possible to eliminate continuous supervision of the therapeutic effect of the exoskeleton by the physiotherapist in favor of filming and periodically checking, including through objective tests, the progress of the improvement process [40]. The exoskeleton frame for the upper limb can already be 3D printed in one piece (also with connectors)—this saves assembly time, better adjusts it to the expectations and needs of the patient, and reduces, for example, joint misalignments. Hall sensors measure angles in joints with an average accuracy of 1.25°. The tendons attached to the fingertips transmit the forces from the motors. High-linearity force/torque sensors have been shown to be accurate to 0.5937 N [41].
As you can see, the main areas of application of 3D-printed exoskeletons are still motor dysfunctions after stroke and SCI.
4. Control of Exoskeleton
So far, it has not been clearly decided whether 3D-printed exoskeletons require a specific type of control. It is believed that the construction of this exoskeleton can be as close as possible to the normal dimensions and weight of individual limb elements, and the control method should not be too different from the natural one (here: based on BCI). 3D printing has enabled the design and manufacture of exoskeletons as intelligent and multi-functional tools, combining additive manufacturing from various materials with intelligent control systems. Developed, e.g., a multifunctional biomimetic soft actuator with a pneumatic movement system imitating the movement of a human finger with bending from −180° to 180° (but without reaching extremes). The proportional-integral-derivative controller allows for monitoring the position of the exoskeleton in real time by a single-axis soft deflection sensor built into the actuator [42].
Controlling the exoskeleton must take into account several aspects in the area of symmetrical and asymmetric geometry and the behavior of the biological hand. 3D printing allows for the production and prototyping of both the mechanical design itself and the entire exoskeleton, along with the control system. As part of the tests, multiple sources of feedback can be used to determine symmetric and asymmetric activities described by torque, position, trajectory, and the laws of motion [43]. An integral part of controlling the exoskeleton is the detection, interpretation, and support of the intention of human movement, within the so-called feedforward control. Most of these types of solutions are based on surface electromyography (sEMG), which requires precise placement of electrodes on the muscles. This leads to attempts to build physical interfaces for exoskeletons with integrated 3D-printed sEMG and pressure sensors. Multimodal information from flexible, conductive sensors is fed to a classifier (usually K-Nearest Neighbors—kNN), calibrated against an EMG-based unimodal classifier. This gives a very good prediction performance even with a minimal number of sEMG electrodes and without their precise placement [44]. 3D-printed exoskeletons can also be used as scaffolds to induce soft tissue and bone growth. In addition, 3D printing with bioink allows for the production of complex geometries, including blood vessels, bones, cartilage, fabrics such as skin, and in the future also whole organs and simple devices built into the patient’s body, e.g., for drug delivery or controlled stimulation [45]. In exoskeleton control, not only movement control but also the reception and processing of sensory stimuli are important. A combination of 3D printing techniques using soft materials and haptic fingertip stimulation has already been demonstrated. 3D printing from soft materials (PLA) was used to create soft pneumatic haptic feedback actuators (6.8 ± 0.23 g each with PLA attachment and Velcro), as the tactile stimulation of the fingertips is synchronized with the movement of the entire hand exoskeleton. The aforementioned haptic stimulation increases the engagement level of individuals during exoskeleton-assisted glass grasping exercises [46]. In order to combine the advantages of rigid and soft exoskeletons, hybrid exoskeletons consisting of both rigid and soft components are being built where needed. However, these require expensive multi-material 3D printers and multi-step machining processes (including casting or machining) with a limited material selection. Modified technologies such as fused deposition modeling (FDM) have recently made it possible to deposit the filament onto a heated thermoplastic base layer, which improves the bonding strength between the stiffer material and the flexible (but non-stretchable) base layer. This enables the previously unattainable advantages of locally stiff and locally soft exoskeletons with the improved fatigue strength of 3D-printed components [47]. The joint control of a 3D-printed exoskeleton is illustrated using a serial viscoelastic joint as an example. It is constructed by assembling 3D-printed compression elements with non-linear elastic silicone springs that have internal damping. This translates into higher performance, a compact design, a lower price, simpler and more stable control (a torque controller), and a torque transfer of 4.5 Nm at 20 degrees. Solutions of this type increase the safety of exoskeletons interacting with the human body [48]. It is also worth remembering that improper design of the exoskeleton in relation to the natural mechanical behavior of the body segment, in particular the skin, can cause tissue strain, pressure ulcers, and ulcerations. Differences in kinematics between patients may affect skin deformations, and thus the design and manufacture of rehabilitation products should be at least partially personalized. It is not known whether it is possible to standardize the design of the exoskeleton (or parts of it adjacent to the skin) between people with the same movement disorder. It appears that in healthy people, such a similarity occurs [49]. Breakthrough work may involve enhancing the activity of motor proteins to create a type of motorized exoskeleton that actuates protein-based robotic structures. It may be possible to combine and assemble such 3D-printed modules into larger structures that perform complex mechanical tasks when activated by light (such as waving or grasping) [50]. There is a consensus that stroke can result in functional deficits in the upper limbs (affecting self-care, learning, and working opportunities) and deficits in the lower limbs (limiting mobility). For the above reasons, exoskeletons are a group of solutions ideally suited to the needs of this patient group. They have a two-pronged effect: (1) immediate improvement through support for function and strength and partial pressure relief; and (2) shaping long-term improvement through built-in rehabilitation function, maintaining an upright posture, and allowing gradual progress in restoring function even in those with severe deficits. 3D-printed exoskeletons are better suited to the patient structurally (dimensions, method, and degree of support) and functionally (they support therapeutic goals relevant to the patient, giving them increased motivation). So-called soft exoskeletons in particular are becoming increasingly popular as they have better plastic properties, are lighter, are safer, and are more ergonomic, especially for less experienced users. The study by Noronha et al. presented an improved version of a 3D-printed partial hand exoskeleton (personalized structures to prevent unwanted joint hyperextension). In a sample of 10 post-stroke patients, a significant reduction in mean muscle activity, a reduction in co-activation of muscle pairs associated with pathological muscle synergies, and a significant increase in elbow flexion angle were observed [51].
5. Own Experiences
Proposed areas of AI-assisted support for the manufacture of a personalized 3D printed product, based on our own experience in testing a hand exoskeleton, include:
- Analyzing the changes made to successive generations of the exoskeleton.
- Identifying deficiencies from a biomechanical point of view.
- Identifying shortcomings from a technical point of view.
- Identification of components that are difficult to manufacture quickly using the planned 3D printing methods.
- Development and planning of retrofit proposals for testing.
- Optimization of developed materials and technological solutions from the point of view of usability and technology.
- Analysis of test prints of exoskeleton elements and the possibilities of their integration into a working prototype.
- Movement tests with the help of a system of sensors and/or cameras are necessary to refine the computational model.
- Strength tests of the prototype (compression, tensile, etc.).
- Testing of the prototype under laboratory conditions.
- Additional experimental testing (filmed in multiple planes).
- Additional numerical simulations.
- Refinement of the design and improvement of the prints.
- Improving the fit for the patient.
The use of the digital twin of the exoskeleton is an integral part of the Industry 4.0 paradigm, effective in the context of sustainable production and maintenance, the acquisition of data and its conversion into knowledge, and the use of models to simulate tasks and processes and their improvement. It also allows for continuous automatic monitoring of processes and process parameters, intelligent eco-design, and consideration of sustainable production and maintenance [52]. AI-based optimization yields one free print after every 6.67 prints (i.e., from materials that were previously wasted) [53]. The combination of the use of real-world data from hand exoskeleton research, new methods for their analysis using DL, and a transparent and scalable 3D printed fabric product design offers the possibility of producing a personalized chainmail with adjustable mechanical parameters (stiffness and flexion angles in different directions) better suited to the needs and goals of therapy in a particular patient [54,55]. AI-based software (Matlab 16.0, MathWorks, Natick, MA, USA) is used to assess the amount of contamination generated by 3D printing systems; it is self-learning as more data is entered, complementing previously used metrics and 3D printing software (printer-specific) [56]. Remote monitoring helps in the early diagnosis of micro-injuries and the resulting gradual deterioration of motor skills, affecting the need for exoskeleton modifications [57,58,59], which has often been a challenge in diagnosis, therapy, and care to date.
6. Discussion
The presented approach allows you to design, manufacture, and recycle relatively complex objects (exoskeletons) from their physical counterparts or digital twins. It allows for bypassing the existing geographical, time, technological, and material limitations, as well as reducing the harmful impact on living organisms and the natural environment. This may contribute to the increase in the effectiveness of saving human life and health and the improvement of the quality of life, especially in people with deficits, including neurodegenerative, i.e., as a result of progressive aging processes. This opens up interesting opportunities for further development, including applications in diagnostics, therapy, rehabilitation, and care. Their wide implementation will require interdisciplinary research, including clinical research on large groups of patients. This is a great challenge because the adopted paradigm of personalized therapy makes it difficult to study homogeneous groups and ensure uniformity of the therapeutic interventions; moreover, research may require precise determination of the long-term impact on patient’s health, new measurement methods and techniques, as well as new qualifications for specialists in the fields of engineering and medicine. Problems with the implementation of randomized controlled trials (RCTs) may result in a re-evaluation of the currently applicable criteria of credibility and relevance toward studies and computational models [60,61,62,63,64,65,66]. SWOT (strengths, weaknesses, opportunities, and threats) analysis is shown in Table 2.

Table 2.
SWOT analysis of the 3D printed exoskeleton.
6.1. Limitations of Own R
6.1.1. Limitations of AI-Supported 3D Printing
In light of today’s state of knowledge and practice, there is no doubt that 3D scanning, 3D printing, and reverse engineering are a combination of innovative technologies bringing significant conceptual, technological, economic, and social changes in almost every area of everyday clinical practice thanks to the expected jump to personalized therapy, the replacement of traditional implant manufacturing models (including from living tissue), drugs, dressings, and rehabilitation supplies, as well as shortening the chain of their distribution to production “on demand”. Despite the advancement of research, there is also no doubt that the possibilities of 3D printing in biomedical applications have not yet been fully explored and exploited. In addition, technologies that directly or indirectly affect the lives and health of patients should be well-researched and safe, in accordance with the paradigm of evidence-based medicine (EBM), so their implementation is inevitably delayed until approvals and certificates are obtained [67,68,69].
Critics of the use of 3D printing and reverse engineering in biomedicine raise the argument that unproven, temporary, and even improvised solutions are often created. Tendencies to implement innovative ideas as soon as possible, overestimating the capabilities of the described group of technologies, and attempts to use them in the absence of a sufficient number of research and publications are among the greatest future threats in the field of clinical 3D printing applications.
6.1.2. Directions for Further Research
Despite the above limitations and being in the initial phase of development of the above-mentioned a group of technologies can inspire changes in everyday clinical practice today, especially in the area of teaching aids and the selection and production of rehabilitation supplies. However, this requires the involvement of interdisciplinary teams of clinicians, researchers, and engineers. This requires research and development of 3D technology to be focused on the creative solving of key clinical problems, the adaptation of subsequent generations of solutions to the needs of patients, and the continuous identification, monitoring, and elimination of threats so that the developed solutions are optimal and fully clinically functional [70,71].
Currently, AI is used for the design, printing, and post-production of 3D printed objects. But AI supporting 3D printing is currently the main topic of many studies [63,64,65], allowing us to monitor and adjust the 3D printing process to correct errors in real time. New materials with unique properties can be used for 3D printing. Smart manufacturing systems can use ML to learn the complex control policies of individualized mass-produced items, such as exoskeletons. Such intelligent 3D printing production lines can more easily, in real time, adapt to changing tasks and conditions of their implementation, including the workplace environment, improving efficiency, and accuracy, or avoiding unnecessary downtime. The main areas of dynamic development in the use of AI in industrial 3D printing include, primarily:
- Generative design.
- Automated mass production, personalized.
- Meeting the criteria of sustainable development and the green deal by the industry (e.g., less waste and pollution).
- Improving the ownership of products and services in line with the expectations of all stakeholder groups.
- New, yet unknown applications [72].
7. Conclusions
The field of AI applications in personalized mass medical device manufacturing is still developing, and more research is needed to draw more definitive conclusions. A study using a combination of different diagnostic methods with AI to assess a patient’s condition and the acceptability and feasibility of interventions will be valuable in measuring outcomes and predicting the effectiveness of therapy, rehabilitation, and care, including remote care.
Most of the solutions used so far mainly involve a data-driven (ML) approach. There is a lack of larger ML and DL systems collecting and analyzing data, and the data itself is often unstructured and disconnected and does not cover all useful areas.
Another breakthrough is expected related to the wider use of AI in 3D printing (diagnostics and selection of functional parameters, selection of technologies and combining materials, optimization of control and improvement of utility properties, and environmental friendliness), which will expand the possibilities of using personalized exoskeletons in the rehabilitation of patients with congenital and acquired injuries. This will make it easier to combine solutions (hybridization) in order to better adapt them to the needs of a patient or even a healthy person (e.g., an athlete). Accuracy of 80–90% obtained with the help of AI may prove to be sufficient for most clinical applications, and results above 90% will no longer be uncommon.
Further research will show how to optimize low-cost, more efficient solutions for multi-task and multi-material additive manufacturing of exoskeletons.
Author Contributions
Conceptualization, D.M. and I.R.; methodology, D.M., I.R., P.K. and J.D.; software, D.M., I.R., P.K. and J.D.; validation, D.M., I.R., P.K. and J.D.; formal analysis, D.M., I.R., P.K. and J.D.; investigation, D.M., I.R., P.K. and J.D.; resources, D.M., I.R., P.K. and J.D.; data curation, D.M., I.R., P.K. and J.D.; writing—original draft preparation, D.M., I.R., P.K. and J.D.; writing—review and editing, D.M., I.R., P.K. and J.D.; visualization, D.M., I.R., P.K. and J.D.; supervision, I.R.; project administration, I.R.; funding acquisition, D.M. and I.R. All authors have read and agreed to the published version of the manuscript.
Funding
The work presented in the paper has been financed under a grant to maintain the research potential of Kazimierz Wielki University.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- European Commission. Digital transformation of European Industry and Enterprises. Strategic Policy Forum on Digital Entrepreneurship. 2015. Available online: https://www.digitaleurope.org/resources/digital-transformation-of-european-industry-and-enterprises-a-report-of-the-strategic-policy-forum-on-digital-entrepreneurship/ (accessed on 11 July 2023).
- Boston Consulting Group. Industry 4.0: The Future of Productivity and Growth in Manufacturing Industries. 2015. Available online: https://www.bcg.com/publications/2015/engineered_products_project_business_industry_4_future_productivity_growth_manufacturing_industries (accessed on 11 July 2023).
- Roland Berger Consultants. Industry 4.0: The New Industrial Revolution, How Europe Will Succeed; Roland Berger Consultants: Singapore, 2014. [Google Scholar]
- Westkämper, E. Towards the Re-Industrialization of Europe: A Concept for Manufacturing for 2030; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- European Commision. Industry 5.0. Towards a Sustainable, Human-Centric and Resilient European Industry. 2021. Available online: https://op.europa.eu/en/publication-detail/-/publication/468a892a-5097-11eb-b59f-01aa75ed71a1/ (accessed on 11 July 2023).
- Kruppa, C.; Benner, S.; Brinkemper, A.; Aach, M.; Reimertz, C.; Schildhauer, T.A. New technologies and robotics. Unfallchirurgie 2023, 126, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Kataria, S.; Ravindran, V. Musculoskeletal care—At the confluence of data science, sensors, engineering, and computation. BMC Musculoskelet. Disord. 2022, 23, 169. [Google Scholar] [CrossRef] [PubMed]
- Rojek, I.; Mikołajewski, D.; Kotlarz, P.; Tyburek, K.; Kopowski, J.; Dostatni, E. Traditional Artificial Neural Networks Versus Deep Learning in Optimization of Material Aspects of 3D Printing. Materials 2021, 14, 7625. [Google Scholar] [CrossRef] [PubMed]
- Rojek, I.; Mikołajewski, D.; Kopowski, J.; Kotlarz, P.; Piechowiak, M.; Dostatni, E. Reducing Waste in 3D Printing Using a Neural Network Based on an Own Elbow Exoskeleton. Materials 2021, 14, 5074. [Google Scholar] [CrossRef] [PubMed]
- Rojek, I.; Mikołajewski, D.; Dostatni, E.; Macko, M. AI-Optimized Technological Aspects of the Material Used in 3D Printing Processes for Selected Medical Applications. Materials 2020, 13, 5437. [Google Scholar] [CrossRef] [PubMed]
- Efstathiadis, A.; Symeonidou, I.; Tsongas, K.; Tzimtzimis, E.K.; Tzetzis, D. Parametric Design and Mechanical Characterization of 3D-Printed PLA Composite Biomimetic Voronoi Lattices Inspired by the Stereom of Sea Urchins. J. Compos. Sci. 2023, 7, 3. [Google Scholar] [CrossRef]
- Ansari, M.A.; Crampton, A.; Parkinson, S. A Layer-Wise Surface Deformation Defect Detection by Convolutional Neural Networks in Laser Powder-Bed Fusion Images. Materials 2022, 15, 7166. [Google Scholar] [CrossRef]
- Hanitio, E.W.; Lutfhyansyah, N.R.; Efendi, B.M.; Mardiyati, Y.; Steven, S. From Electronic Waste to 3D-Printed Product, How Multiple Recycling Affects High-Impact Polystyrene (HIPS) Filament Performances. Materials 2023, 16, 3412. [Google Scholar] [CrossRef]
- Wan, M.; Hu, D.; Pei, B. Performance of 3D-Printed Bionic Conch-Like Composite Plate under Low-Velocity Impact. Materials 2022, 15, 5201. [Google Scholar] [CrossRef]
- Godeau, X.Y.; Andrianandrasana, F.J.; Volkova, O.; Szczepanski, C.R.; Zenerino, A.; Montreuil, O.; Godeau, R.P.; Kuzhir, P.; Godeau, G. Investigation on dung beetle’s (Heliocopris Hope, 1838) chitosan valorisation for hydrogel 3D printing. Int. J. Biol. Macromol. 2022, 199, 172–180. [Google Scholar] [CrossRef]
- Rojek, I.; Dostatni, E.; Kopowski, J.; Macko, M.; Mikołajewski, D. AI-Based Support System for Monitoring the Quality of a Product within Industry 4.0 Paradigm. Sensors 2022, 22, 8107. [Google Scholar] [CrossRef]
- Jochumsen, M.; Janjua, T.A.M.; Arceo, J.C.; Lauber, J.; Buessinger, E.S.; Kæseler, R.L. Induction of Neural Plasticity Using a Low-Cost Open Source Brain-Computer Interface and a 3D-Printed Wrist Exoskeleton. Sensors 2021, 21, 572. [Google Scholar] [CrossRef]
- Lubimyi, N.S.; Polshin, A.A.; Gerasimov, M.D.; Tikhonov, A.A.; Antsiferov, S.I.; Chetverikov, B.S.; Ryazantsev, V.G.; Brazhnik, J.; Ridvanov, İ. Justification of the Use of Composite Metal-Metal-Polymer Parts for Functional Structures. Polymers 2022, 14, 352. [Google Scholar] [CrossRef]
- Rojek, I.; Kaczmarek, M.; Kotlarz, P.; Kempiński, M.; Mikołajewski, D.; Szczepański, Z.; Kopowski, J.; Nowak, J.; Macko, M.; Szczepańczyk, A.; et al. Hand Exoskeleton—Development of Own Concept. Appl. Sci. 2023, 13, 3238. [Google Scholar] [CrossRef]
- Rojek, I.; Mikołajewski, D.; Dostatni, E.; Kopowski, J. Specificity of 3D Printing and AI-Based Optimization of Medical Devices Using the Example of a Group of Exoskeletons. Appl. Sci. 2023, 13, 1060. [Google Scholar] [CrossRef]
- Mikołajewski, D.; Rojek, I.; Kotlarz, P.; Dorożyński, J.; Kopowski, J. Personalization of the 3D-Printed Upper Limb Exoskeleton Design—Mechanical and IT Aspects. Appl. Sci. 2023, 13, 7236. [Google Scholar] [CrossRef]
- Mitchell, K.; Raymond, L.; Jin, Y. Material Extrusion Advanced Manufacturing of Helical Artificial Muscles from Shape Memory Polymer. Machines 2022, 10, 497. [Google Scholar] [CrossRef]
- Kopowski, J.; Mikołajewski, D.; Kotlarz, P.; Dostatni, E.; Rojek, I. A Semi-Automated 3D-Printed Chainmail Design Algorithm with Preprogrammed Directional Functions for Hand Exoskeleton. Appl. Sci. 2022, 12, 5007. [Google Scholar] [CrossRef]
- Leal-Junior, A.; Theodosiou, A.; Díaz, C.; Marques, C.; Pontes, M.J.; Kalli, K.; Frizera-Neto, A. Fiber Bragg Gratings in CYTOP Fibers Embedded in a 3D-Printed Flexible Support for Assessment of Human-Robot Interaction Forces. Materials 2018, 11, 2305. [Google Scholar] [CrossRef]
- Mohammadi, A.; Lavranos, J.; Choong, P.; Oetomo, D. Flexo-glove: A 3D Printed Soft Exoskeleton Robotic Glove for Impaired Hand Rehabilitation and Assistance. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; Volume 2018, pp. 2120–2123. [Google Scholar] [CrossRef]
- Xiloyannis, M.; Cappello, L.; Binh, K.D.; Antuvan, C.W.; Masia, L. Preliminary design and control of a soft exosuit for assisting elbow movements and hand grasping in activities of daily living. J. Rehabil. Assist. Technol. Eng. 2017, 4, 2055668316680315. [Google Scholar] [CrossRef]
- Oguntosin, V.W.; Mori, Y.; Kim, H.; Nasuto, S.J.; Kawamura, S.; Hayashi, Y. Design and Validation of Exoskeleton Actuated by Soft Modules toward Neurorehabilitation-Vision-Based Control for Precise Reaching Motion of Upper Limb. Front. Neurosci. 2017, 11, 352. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, C.; Blanco, L.; Del Río, C.; Urendes, E.; Costa, V.; Raya, R. A 3D-printed passive exoskeleton for upper limb assistance in children with motor disorders: Proof of concept through an electromyography-based assessment. PeerJ 2023, 11, e15095. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Li, M.; Wang, J.; Wang, T.; Liang, Z.; He, B.; Xie, J.; Xu, G. A novel wrist rehabilitation exoskeleton using 3D-printed multi-segment mechanism. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2021, 2021, 4769–4772. [Google Scholar] [CrossRef] [PubMed]
- Joo, S.Y.; Lee, S.Y.; Cho, Y.S.; Yi, S.; Seo, C.H. Clinical Utility of an Exoskeleton Robot Using Three-Dimensional Scanner Modeling in Burn Patient: A Case Report. J. Burn Care Res. 2021, 42, 1030–1034. [Google Scholar] [CrossRef] [PubMed]
- Serbest, K.; Kutlu, M.; Eldogan, O.; Tekeoglu, I. Development and control of a home-based training device for hand rehabilitation with a spring and cable driven mechanism. Biomed. Tech. 2021, 66, 395–403. [Google Scholar] [CrossRef]
- Yoo, H.J.; Lee, S.; Kim, J.; Park, C.; Lee, B. Development of 3D-printed myoelectric hand orthosis for patients with spinal cord injury. J. Neuroeng. Rehabil. 2019, 16, 162. [Google Scholar] [CrossRef]
- Heung, K.H.L.; Tang, Z.Q.; Ho, L.; Tung, M.; Li, Z.; Tong, R.K.Y. Design of a 3D Printed Soft Robotic Hand for Stroke Rehabilitation and Daily Activities Assistance. IEEE Int. Conf. Rehabil. Robot. 2019, 2019, 65–70. [Google Scholar] [CrossRef]
- Barabás, I.J.; Hartyánszky, I.; Kocher, A.; Merkely, B. A 3D printed exoskeleton facilitates HeartMate III inflow cannula position. Interact. CardioVascular Thorac. Surg. 2019, 29, 644–646. [Google Scholar] [CrossRef]
- Triolo, E.R.; Stella, M.H.; BuSha, B.F. A force augmenting exoskeleton for the human hand designed for pinching and grasping. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; Volume 2018, pp. 1875–1878. [Google Scholar] [CrossRef]
- Li, N.; Yang, T.; Yu, P.; Chang, J.; Zhao, L.; Zhao, X.; Elhajj, I.H.; Xi, N.; Liu, L. Bio-inspired upper limb soft exoskeleton to reduce stroke-induced complications. Bioinspir. Biomim. 2018, 13, 066001. [Google Scholar] [CrossRef]
- Scott, R.A.; Callisaya, M.L.; Duque, G.; Ebeling, P.R.; Scott, D. Assistive technologies to overcome sarcopenia in ageing. Maturitas 2018, 112, 78–84. [Google Scholar] [CrossRef]
- Alavi, N.; Zampierin, S.; Komeili, M.; Cocuzza, S.; Debei, S.; Menon, C. A preliminary investigation into the design of pressure cushions and their potential applications for forearm robotic orthoses. Biomed. Eng. Online 2017, 16, 54. [Google Scholar] [CrossRef]
- Gearhart, C.J.; Varone, B.; Stella, M.H.; Bu Sha, B.F. An effective 3-fingered augmenting exoskeleton for the human hand. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; Volume 2016, pp. 590–593. [Google Scholar] [CrossRef]
- Lei, C.; Phan, A.; Allison, G. Design and fabrication of a three dimensional printable non-assembly articulated hand exoskeleton for rehabilitation. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; Volume 2015, pp. 4627–4630. [Google Scholar] [CrossRef]
- Weiss, P.; Heyer, L.; Munte, T.F.; Heldmann, M.; Schweikard, A.; Maehle, E. Towards a parameterizable exoskeleton for training of hand function after stroke. IEEE Int. Conf. Rehabil. Robot. 2013, 2013, 6650505. [Google Scholar] [CrossRef]
- Kladovasilakis, N.; Sideridis, P.; Tzetzis, D.; Piliounis, K.; Kostavelis, I.; Tzovaras, D. Design and Development of a Multi-Functional Bioinspired Soft Robotic Actuator via Additive Manufacturing. Biomimetics 2022, 7, 105. [Google Scholar] [CrossRef]
- Birouaș, F.I.; Țarcă, R.C.; Dzitac, S.; Dzitac, I. Preliminary Results in Testing of a Novel Asymmetric Underactuated Robotic Hand Exoskeleton for Motor Impairment Rehabilitation. Symmetry 2020, 12, 1470. [Google Scholar] [CrossRef]
- Langlois, K.; Geeroms, J.; Van De Velde, G.; Rodriguez-Guerrero, C.; Verstraten, T.; Vanderborght, B.; Lefeber, D. Improved Motion Classification with an Integrated Multimodal Exoskeleton Interface. Front. Neurorobot. 2021, 15, 693110. [Google Scholar] [CrossRef]
- Marew, T.; Birhanu, G. Three dimensional printed nanostructure biomaterials for bone tissue engineering. Regen. Ther. 2021, 18, 102–111. [Google Scholar] [CrossRef]
- Li, M.; Chen, J.; He, G.; Cui, L.; Chen, C.; Secco, E.L.; Yao, W.; Xie, J.; Xu, G.; Wurdemann, H. Attention Enhancement for Exoskeleton-Assisted Hand Rehabilitation Using Fingertip Haptic Stimulation. Front. Robot. AI 2021, 8, 602091. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.; Zhou, Z.; Gravish, N. Flexoskeleton Printing Enables Versatile Fabrication of Hybrid Soft and Rigid Robots. Soft Robot. 2020, 7, 770–778. [Google Scholar] [CrossRef]
- Chiaradia, D.; Tiseni, L.; Frisoli, A. Compact Series Visco-Elastic Joint (SVEJ) for Smooth Torque Control. IEEE Trans. Haptics 2020, 13, 226–232. [Google Scholar] [CrossRef]
- Barrios-Muriel, J.; Romero Sánchez, F.; Alonso Sánchez, F.J.; Rodríguez Salgado, D. In vivo measurement of surface skin strain during human gait to improve the design of rehabilitation devices. Comput. Methods Biomech. Biomed. Eng. 2019, 22, 1219–1228. [Google Scholar] [CrossRef]
- Jia, H.; Flommersfeld, J.; Heymann, M.; Vogel, S.K.; Franquelim, H.G.; Brückner, D.B.; Eto, H.; Broedersz, C.P.; Schwille, P. 3D printed protein-based robotic structures actuated by molecular motor assemblies. Nat. Mater. 2022, 21, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Noronha, B.; Ng, C.Y.; Little, K.; Xiloyannis, M.; Kuah, C.W.K.; Wee, S.K.; Kulkarni, S.R.; Masia, L.; Chua, K.S.G.; Accoto, D. Soft, Lightweight Wearable Robots to Support the Upper Limb in Activities of Daily Living: A Feasibility Study on Chronic Stroke Patients. IEEE Trans. Neural. Syst. Rehabil. Eng. 2022, 30, 1401–1411. [Google Scholar] [CrossRef] [PubMed]
- Rojek, I.; Mikołajewski, D.; Dostatni, E. Digital Twins in Product Lifecycle for Sustainability in Manufacturing and Maintenance. Appl. Sci. 2021, 11, 31. [Google Scholar] [CrossRef]
- Mikula, K.; Skrzypczak, D.; Izydorczyk, G.; Warchoł, J.; Moustakas, K.; Chojnacka, K.; Witek-Krowiak, A. 3D printing filament as a second life of waste plastics—A review. Environ. Sci. Pollut. Res. Int. 2021, 28, 12321–12333. [Google Scholar] [CrossRef]
- Bhat, C.; Kumar, A.; Lin, S.C.; Jeng, J.Y. Adaptive Mechanical Properties and Stretchability of Novel Chainmail Fabrics Based on Overlapping Tessellation Strategies. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4485345 (accessed on 19 June 2023).
- Rojek, I.; Kopowski, J.; Kotlarz, P.; Dorożyński, J.; Dostatni, E.; Mikołajewski, D. Deep Learning in Design of Semi-Automated 3D Printed Chainmail with Pre-Programmed Directional Functions for Hand Exoskeleton. Appl. Sci. 2022, 12, 8106. [Google Scholar] [CrossRef]
- Rojek, I.; Mikołajewski, D.; Macko, M.; Szczepański, Z.; Dostatni, E. Optimization of Extrusion-Based 3D Printing Process Using Neural Networks for Sustainable Development. Materials 2021, 14, 2737. [Google Scholar] [CrossRef]
- Burduk, R.; Rojek, I.; Mikołajewska, E.; Mikołajewski, D. Post-Stroke Gait Classification Based on Feature Space Transformation and Data Labeling. Appl. Sci. 2022, 12, 11346. [Google Scholar] [CrossRef]
- Prokopowicz, P.; Mikołajewski, D.; Tyburek, K.; Mikołajewska, E. Computational gait analysis for post-stroke rehabilitation purposes using fuzzy numbers, fractal dimension and neural networks. Bull. Pol. Acad. Sci. Tech. Sci. 2020, 68, 191–198. [Google Scholar]
- Mikołajewska, E.; Prokopowicz, P.; Mikolajewski, D. Computational gait analysis using fuzzy logic for everyday clinical purposes-preliminary findings. Bio-Algorithms Med-Syst. 2017, 13, 37–42. [Google Scholar] [CrossRef]
- Rojek, I.; Macko, M.; Mikołajewski, D.; Saga, M.; Burczynski, T. Modern methods in the field of machine modeling and simulation as a research and practical issue related to Industry 4.0. Bull. Pol. Acad. Sci. Tech. Sci. 2021, 69, e136719. [Google Scholar] [CrossRef]
- Rahmani Dabbagh, S.; Ozcan, O.; Tasoglu, S. Machine learning-enabled optimization of extrusion-based 3D printing. Methods 2022, 206, 27–40. [Google Scholar] [CrossRef] [PubMed]
- Rojek, I.; Mikołajewski, D.; Kotlarz, P.; Macko, M.; Kopowski, J. Intelligent system supporting technological process planning for machining and 3D printing. Bull. Pol. Acad. Sci. Tech. Sci. 2021, 69, e136722. [Google Scholar]
- Mikolajczyk, T.; Mikołajewska, E.; Al-Shuka, H.F.N.; Malinowski, T.; Kłodowski, A.; Pimenov, D.Y.; Paczkowski, T.; Hu, F.; Giasin, K.; Mikołajewski, D.; et al. Recent Advances in Bipedal Walking Robots: Review of Gait, Drive, Sensors and Control Systems. Sensors 2022, 22, 4440. [Google Scholar] [CrossRef]
- Prokopowicz, P.; Mikołajewski, D.; Mikołajewska, E.; Kotlarz, P. Fuzzy system as an assessment tool for analysis of the health-related quality of life for the people after stroke. In Artificial Intelligence and Soft Computing, Proceedings of the 16th International Conference, ICAISC 2017, Zakopane, Poland, 11–15 June 2017; Lecture Notes in Computer Science (Including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer International Publishing: Berlin/Heidelberg, Germany, 2017; Volume 10245, pp. 710–721. [Google Scholar]
- Mikołajewska, E. Associations between results of post-stroke NDT-Bobath rehabilitation in gait parameters, ADL and hand functions. Adv. Clin. Exp. Med. 2013, 22, 731–738. [Google Scholar]
- Kawala-Janik, A.; Bauer, W.; Al-Bakri, A.; Haddix, C.; Yuvaraj, R.; Cichon, K.; Podraza, W. Implementation of Low-Pass Fractional Filtering for the Purpose of Analysis of Electroencephalographic Signals. In Non-Integer Order Calculus and Its Applications, Proceedings of the 9th International Conference on Non-Integer Order Calculus and Its Applications, Łódź, Poland, 11–13 October 2017; Springer International Publishing: Berlin/Heidelberg, Germany, 2019; Volume 496, pp. 63–73. [Google Scholar]
- Browarska, N.; Kawala-Sterniuk, A.; Zygarlicki, J.; Podpora, M.; Pelc, M.; Martinek, R.; Gorzelanczyk, E.J. Comparison of Smoothing Filters’ Influence on Quality of Data Recorded with the Emotiv EPOC Flex Brain-Computer Interface Headset during Audio Stimulation. Brain Sci. 2021, 11, 98. [Google Scholar] [CrossRef]
- Kawala-Sterniuk, A.; Pelc, M.; Martinek, R.; Wójcik, G.M. Editorial: Currents in biomedical signals processing—Methods and applications. Front. Neurosci. 2022, 16, 989400. [Google Scholar] [CrossRef]
- Schneider, P.; Wójcik, G.M.; Kawiak, A.; Kwasniewicz, L.; Wierzbicki, A. Modeling and Comparing Brain Processes in Message and Earned Source Credibility Evaluation. Front. Hum. Neurosci. 2022, 16, 808382. [Google Scholar] [CrossRef]
- Using Artificial Intelligence to Control Digital Manufacturing. MIT News. Available online: https://news.mit.edu/2022/artificial-intelligence-3-d-printing-0802 (accessed on 11 July 2023).
- Chen, D.; Luo, D.; Xu, W.; Luo, C.; Shen, L.; Yan, X.; Wang, T. Re-perceive 3D printing with Artificial Intelligence. Addit. Manuf. 2023, 1, 443–450. [Google Scholar]
- Krauss, S. Go Beyond Spare Parts with 3D Printing and Machine Learning. Available online: https://www.engineering.com/AdvancedManufacturing/ArticleID/15969/Go-Beyond-Spare-Parts-with-3D-Printing-and-Machine-Learning.aspx (accessed on 11 July 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).