Recent Advances of Artificial Intelligence in Healthcare: A Systematic Literature Review
Abstract
:1. Introduction
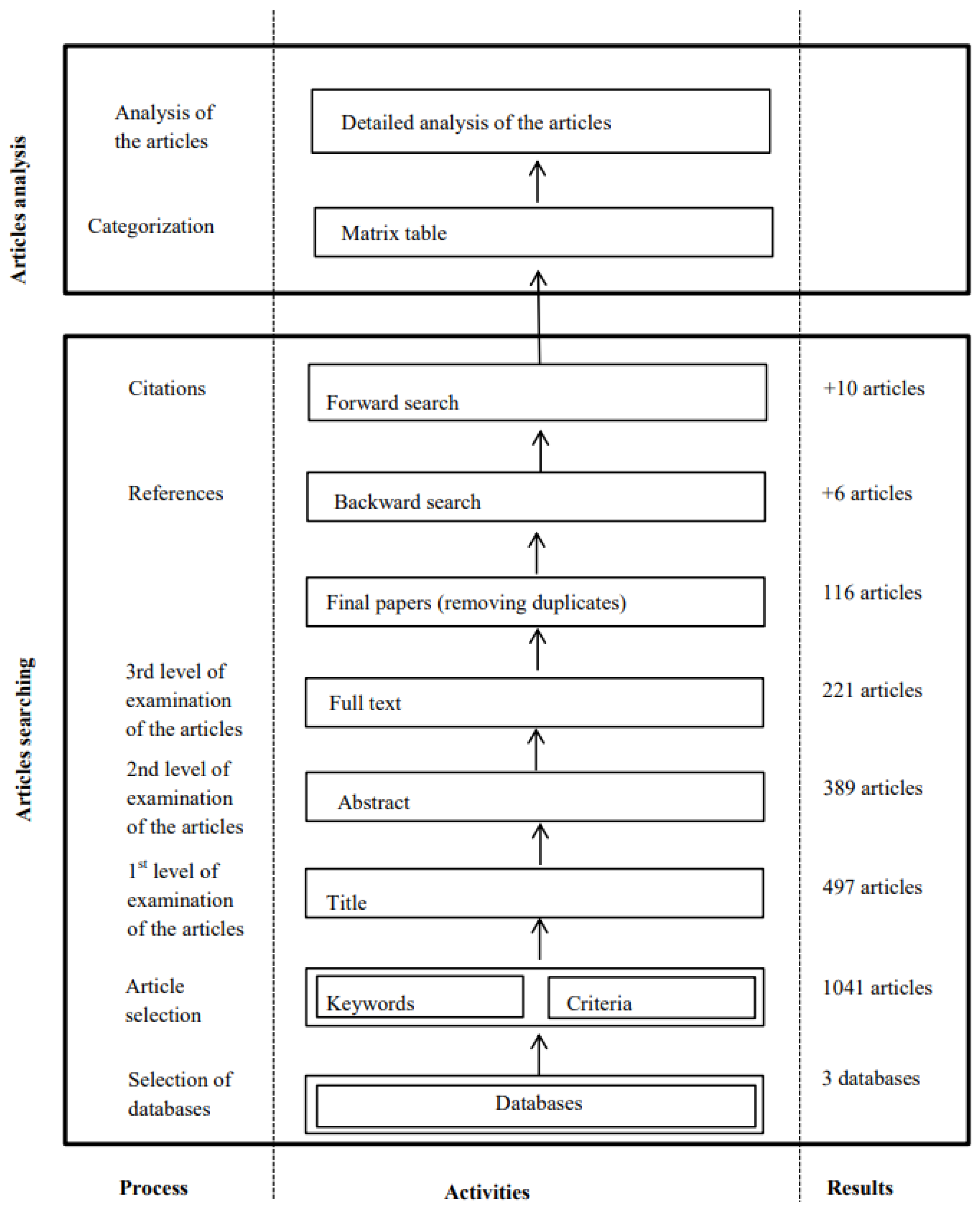
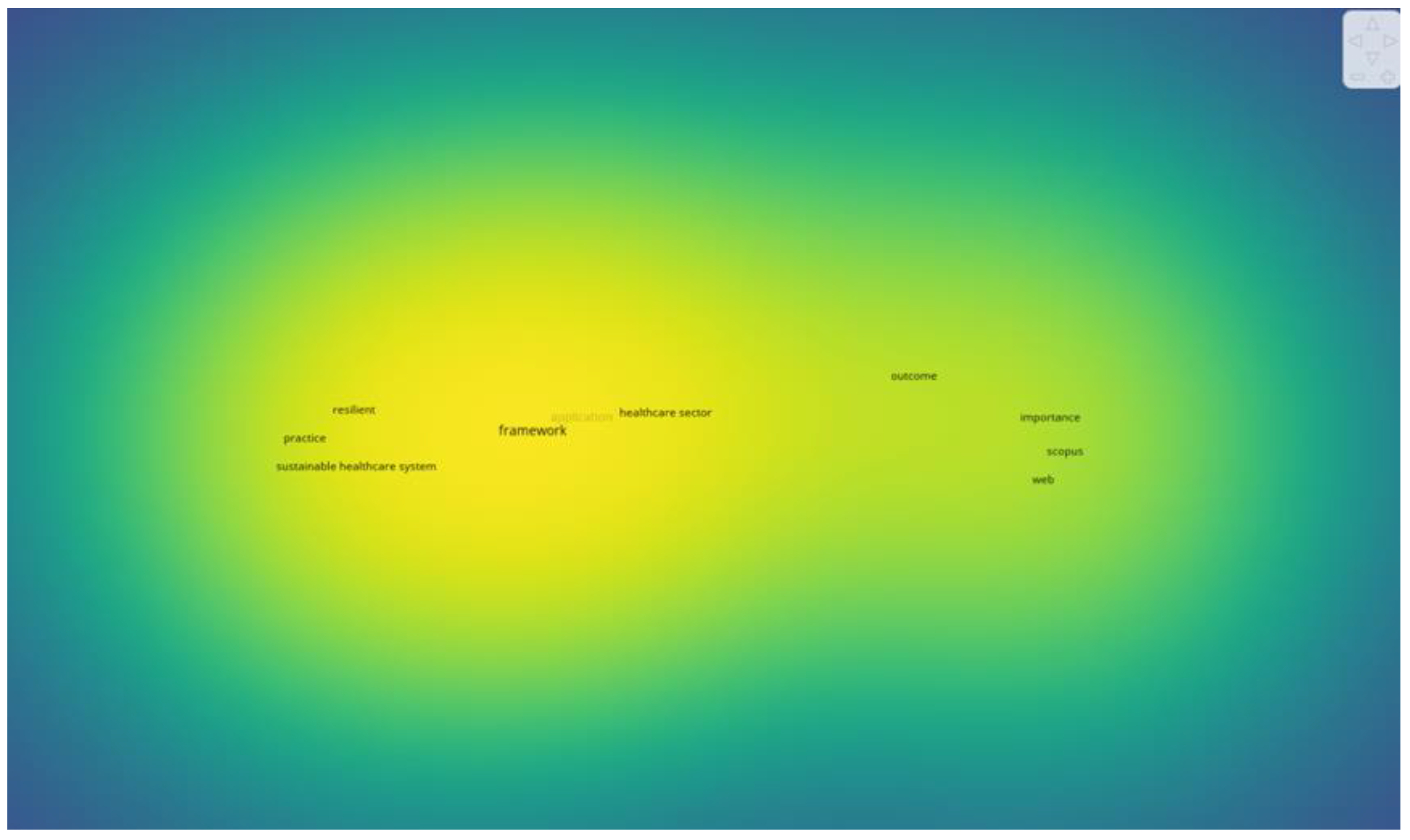
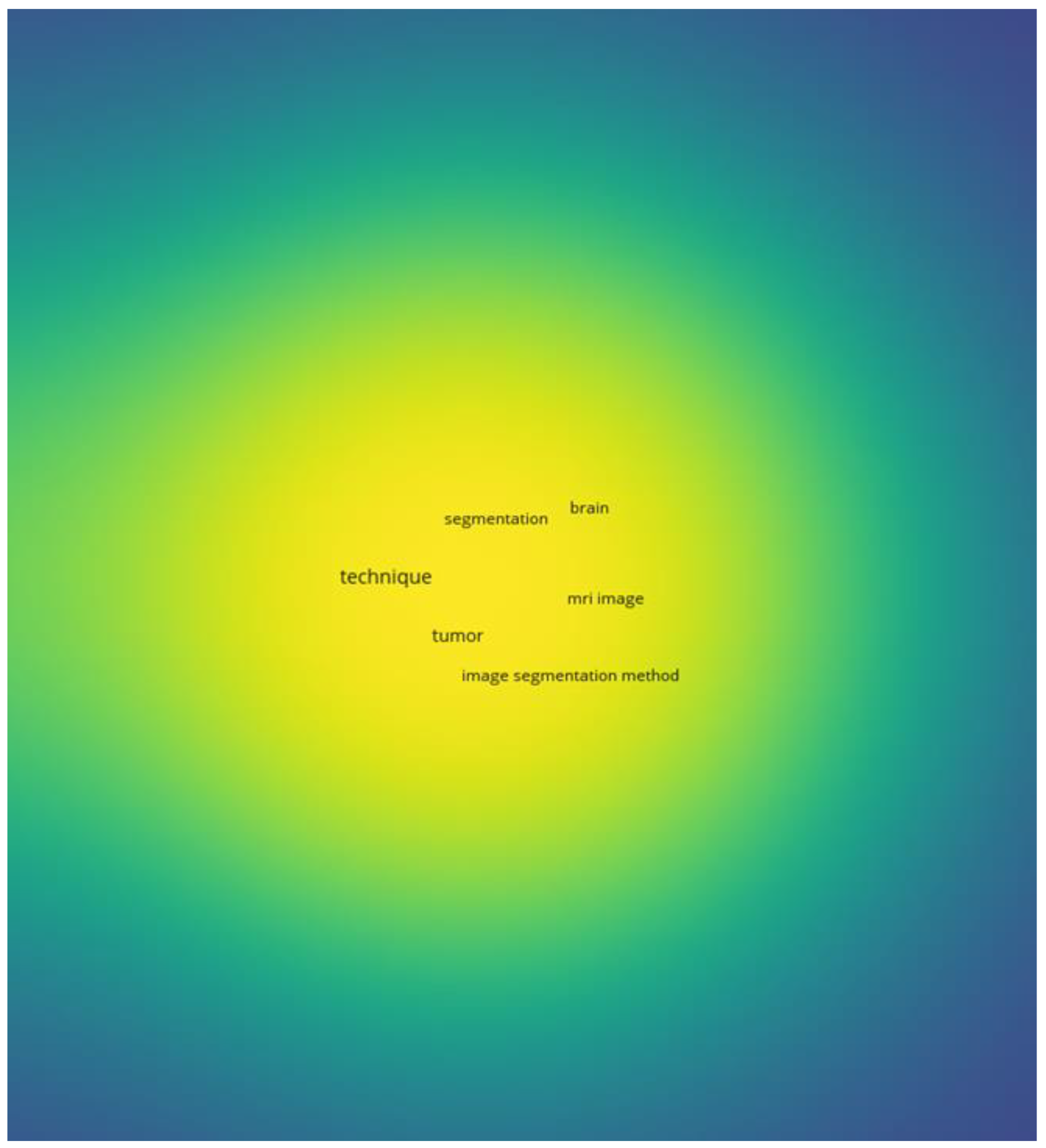
2. Literature Review Methodology
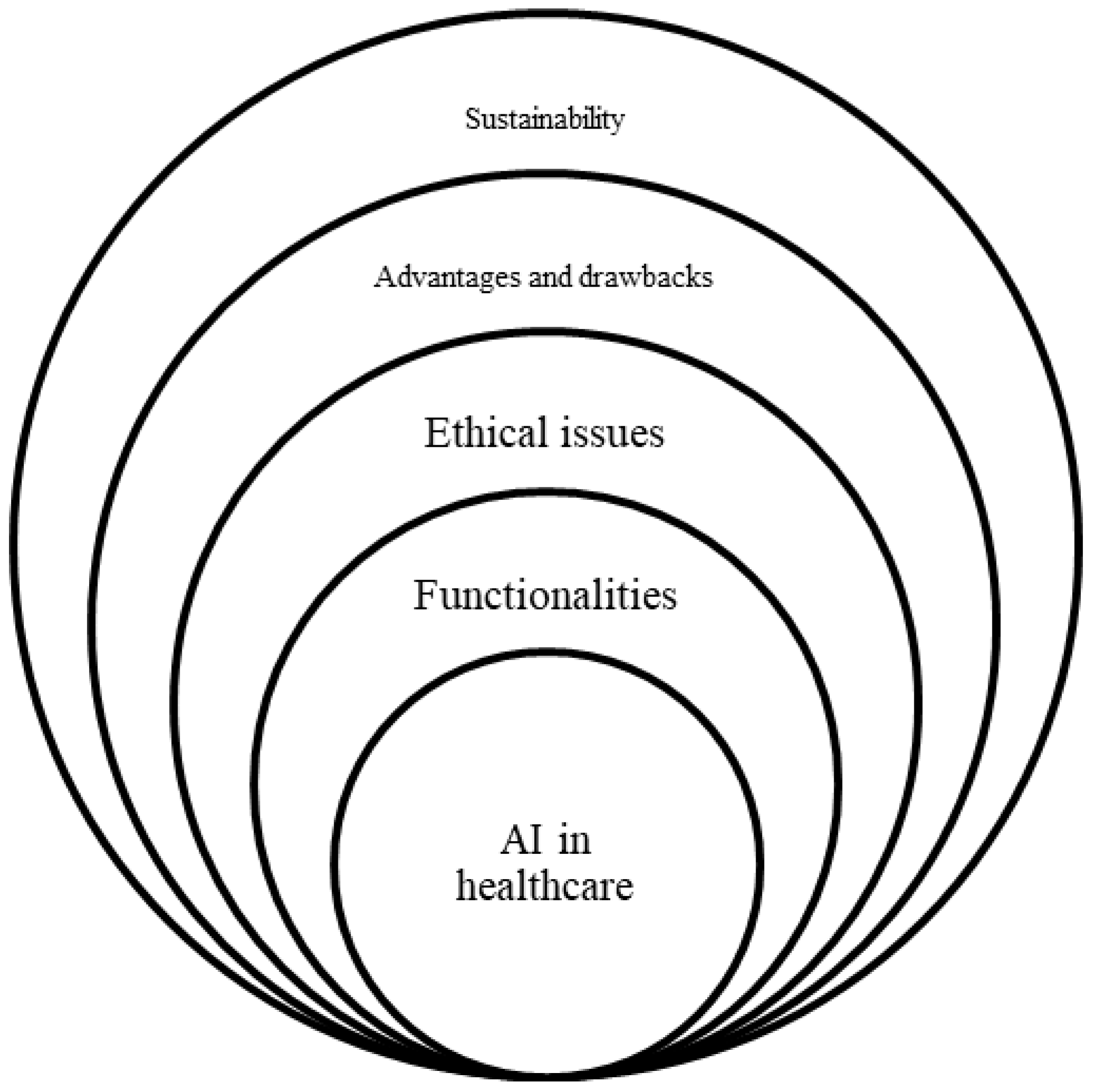
3. Classification Framework for Analysis
3.1. Healthcare Activities Using AI
3.2. Advantages and Drawbacks for the Healthcare Sector
3.3. Ethical Issues about AI
3.4. Social Sustainability and AI
3.5. AI in Hospital Management
3.6. AI and Machine Learning in Disease Diagnosis
3.7. AI and Machine Learning in Remote Patient Monitoring
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aerts, A.; Bogdan-Martin, D. Leveraging data and AI to deliver on the promise of digital health. Int. J. Med. Inform. 2021, 150, 104456. [Google Scholar] [CrossRef] [PubMed]
- Ali, O.; Abdelbaki, W.; Shrestha, A.; Elbasi, E.; Alryalat, M.A.A.; Dwivedi, Y.K. A systematic literature review of artificial intelligence in the healthcare sector: Benefits, challenges, methodologies, and functionalities. J. Innov. Knowl. 2023, 8, 100333. [Google Scholar] [CrossRef]
- Li, B.H.; Hou, B.C.; Yu, W.T.; Lu, X.B.; Yang, C.W. Applications of artificial intelligence in intelligent manufacturing: A review. Front. Inf. Technol. Electron. Eng. 2017, 18, 86–96. [Google Scholar] [CrossRef]
- Kaplan, A.; Haenlein, M. Rulers of the world, unite! The challenges and opportunities of artificial intelligence. Bus. Horiz. 2020, 63, 37–45. [Google Scholar] [CrossRef]
- Chien, C.F.; Dauzere-Peres, S.; Huh, W.T.; Jang, Y.J.; Morrison, J.R. Artificial intelligence in manufacturing and logistics systems: Algorithms, applications, and case studies. Int. J. Prod. Res. 2020, 58, 2730–2731. [Google Scholar] [CrossRef]
- Kumar, P.; Sharma, S.K.; Dutot, V. Artificial intelligence (AI)-enabled CRM capability in healthcare: The impact on service innovation. Int. J. Inf. Manag. 2023, 69, 102598. [Google Scholar] [CrossRef]
- Aiken, R.M.; Epstein, R.G. Ethical guidelines for AI in education: Starting a conversation. Int. J. Artif. Intell. Educ. 2000, 11, 163–176. [Google Scholar]
- Bansal, A.; Padappayil, R.P.; Garg, C.; Singal, A.; Gupta, M.; Klein, A. Utility of artificial intelligence amidst the COVID 19 pandemic: A review. J. Med. Syst. 2020, 44, 156. [Google Scholar] [CrossRef]
- Chee, M.L.; Ong, M.E.H.; Siddiqui, F.J.; Zhang, Z.; Lim, S.L.; Ho, A.F.W.; Liu, N. Artificial intelligence applications for COVID-19 in intensive care and emergency settings: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 4749. [Google Scholar] [CrossRef]
- Minz, A.; Mahobiya, C. MR Image Classification Using ad Boost for Brain Tumor Type. In Proceedings of the IEEE 7th International Advance Computing Conference, Hyderabad, India, 5–7 January 2017; pp. 701–705. [Google Scholar]
- Ribbens, A.; Hermans, J.; Maes, F.; Vandermeulen, D.; Suetens, P. Unsupervised segmentation, clustering, and group wise registration of heterogeneous populations of brain MR images. IEEE Trans. Med. Imaging 2014, 33, 201–224. [Google Scholar] [CrossRef]
- Strachna, O.; Asan, O. Reengineering Clinical Decision Support Systems for Artificial Intelligence. In Proceedings of the IEEE International Conference on Healthcare Informatics, Oldenburg, Germany, 30 November–3 December 2020; pp. 1–3. [Google Scholar]
- Comito, C.; Falcone, D.; Forestiero, A. Current Trends and Practices. In Smart Health Monitoring and Clinical Decision Support. In Proceedings of the IEEE International Conference on Bioinformatics and Biomedicine, Seoul, Republic of Korea, 16–19 December 2020; pp. 2577–2584. [Google Scholar]
- Bernardini, M.; Romeo, L.; Frontoni, E.; Amini, M.R. A semi-supervised multitask learning approach for predicting short-term kidney disease evolution. IEEE J. Biomed. Health Inform. 2021, 25, 3983–3994. [Google Scholar] [CrossRef]
- Yu, H.; Zhou, Z. Optimization of IoT-based artificial intelligence assisted telemedicine health analysis system. IEEE Access 2021, 9, 85034–85048. [Google Scholar] [CrossRef]
- Chen, Z. An AI-Based heart failure treatment adviser system. IEEE J. Transl. Eng. Health Med. 2018, 6, 1–10. [Google Scholar] [CrossRef]
- Dhieb, N.; Ghazzai, H.; Besbes, H.; Massoud, Y. A Secure AI-Driven architecture for automated insurance systems: Fraud detection and risk measurement. IEEE Access 2020, 8, 58546–58558. [Google Scholar] [CrossRef]
- Merhi, M.I. An evaluation of the critical success factors impacting artificial intelligence implementation. Int. J. Inf. Manag. 2022, 69, 102545. [Google Scholar] [CrossRef]
- Sqalli, M.T.; Al-Thani, D. AI-Supported Health Coaching Model for Patients with Chronic Diseases. In Proceedings of the 16th International Symposium on Wireless Communication Systems, Oulu, Finland, 27–30 August 2019; pp. 452–456. [Google Scholar]
- Zhou, L. A rapid, accurate and machine-agnostic segmentation and quantification method for CT-Based COVID-19 diagnosis. IEEE Trans. Med. Imaging 2020, 39, 2638–2652. [Google Scholar] [CrossRef]
- Tobore, I.; Li, J.; Yuhang, L.; Al-Handarish, Y.; Kandwal, A.; Nie, Z.; Wang, L. Deep learning intervention for health care challenges: Some biomedical domain considerations. JMIR mHealth uHealth 2019, 7, e11966. [Google Scholar] [CrossRef]
- Kitsios, F.; Kamariotou, M. Information Systems Strategy and Strategy-as-Practice: Planning Evaluation in SMEs. In Proceedings of the Americas Conference on Information Systems (AMCIS2019), Cancun, Mexico, 15–17 August 2019; pp. 1–10. [Google Scholar]
- Wahl, B.; Cossy-Gantner, A.; Germann, S.; Schwalbe, N.R. Artificial intelligence (AI) and global health: How can AI contribute to health in resource-poor settings? BMJ Glob. Health 2018, 3, e000798. [Google Scholar] [CrossRef] [Green Version]
- Kaur, A.; Garg, R.; Gupta, P. Challenges Facing AI and Big Data for Resource Poor Healthcare System. In Proceedings of the 2nd International Conference on Electronics and Sustainable Communication Systems, Coimbatore, India, 4–6 August 2021; pp. 1426–1433. [Google Scholar]
- Goodarzian, F.; Ghasemi, P.; Gunasekaren, A.; Taleizadeh, A.A.; Abraham, A. A sustainable-resilience healthcare network for handling COVID-19 pandemic. Ann. Oper. Res. 2021, 312, 761–825. [Google Scholar] [CrossRef]
- Pee, L.G.; Pan, S.; Cui, L. Artificial intelligence in healthcare robots: A social informatics study of knowledge embodiment. J. Assoc. Inf. Sci. Technol. 2019, 70, 351–369. [Google Scholar] [CrossRef]
- Maduri, P.K.; Dewangan, Y.; Yadav, D.; Chauhan, S.; Singh, K. IoT Based Patient Health Monitoring Portable Kit. In Proceedings of the 2nd International Conference on Advances in Computing, Communication Control and Networking, Greater Noida, India, 18–19 December 2020; pp. 513–516. [Google Scholar]
- Hossen, M.S.; Karmoker, D. Predicting the Probability of COVID-19 Recovered in South Asian Countries Based on Healthy Diet Pattern Using a Machine Learning Approach. In Proceedings of the 2nd International Conference on Sustainable Technologies for Industry 4.0, Dhaka, Bangladesh, 19–20 December 2020; pp. 1–6. [Google Scholar]
- Dharani, N.; Krishnan, G. ANN Based COVID-19 Prediction and Symptoms Relevance Survey and Analysis. In Proceedings of the 5th International Conference on Computing Methodologies and Communication, Erode, India, 8–10 April 2021; pp. 1805–1808. [Google Scholar]
- Duan, L.; Street, W.N.; Xu, E. Health-care information systems: Data mining methods in the creation of a clinical recommender system. Enterp. Inf. Syst. 2011, 5, 169–181. [Google Scholar] [CrossRef]
- Antoniou, Z.C.; Panayides, A.S.; Pantzaris, M.; Constantinides, A.G.; Pattichis, C.S.; Pattichis, M.S. Real-Time adaptation to time-varying constraints for medical video communications. IEEE J. Biomed. Health Inform. 2018, 22, 1177–1188. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Ma, J.; Li, J.; Huang, M.; Sadiq, N.; Ai, Y. Robust watermarking algorithm for medical volume data in internet of medical things. IEEE Access 2020, 8, 93939–93966. [Google Scholar] [CrossRef]
- Xie, X.; Zang, Z.; Ponzoa, J.M. The information impact of network media, the psychological reaction to the COVID-19 pandemic, and online knowledge acquisition: Evidence from Chinese college students. J. Innov. Knowl. 2020, 5, 297–305. [Google Scholar] [CrossRef]
- Gunasekeran, D.V.; Tseng, R.M.W.W.; Tham, Y.C.; Wong, T.Y. Applications of digital health for public health responses to COVID-19: A systematic scoping review of artificial intelligence, telehealth and related technologies. NPJ Digit. Med. 2021, 4, 40. [Google Scholar] [CrossRef] [PubMed]
- Charan, S.; Khan, M.J.; Khurshid, K. Breast Cancer Detection in Mammograms using Convolutional Neural Network. In Proceedings of the International Conference on Computing, Mathematics and Engineering Technologies, Sukkur, Pakistan, 3–4 March 2018; pp. 1–5. [Google Scholar]
- Woo, Y.; Andres, P.T.C.; Jeong, H.; Shin, C. Classification of Diabetic Walking through Machine Learning: Survey Targeting Senior Citizens. In Proceedings of the International Conference on Artificial Intelligence in Information and Communication, Jeju Island, Republic of Korea, 20–23 April 2021; pp. 435–437. [Google Scholar]
- Deng, Y. A new framework to reduce doctor’s workload for medical image annotation. IEEE Access 2019, 7, 107097–107104. [Google Scholar] [CrossRef]
- Khan, M.; Mehran, M.T.; Haq, Z.U.; Ullah, Z.; Naqvi, S.R.; Ihsan, M.; Abbass, H. Applications of artificial intelligence in COVID-19 pandemic: A comprehensive review. Expert Syst. Appl. 2021, 185, 115695. [Google Scholar] [CrossRef]
- Chen, X.; Xie, H.; Zou, D.; Hwang, G. Application and theory gaps during the rise of Artificial Intelligence in Education. Comput. Educ. Artif. Intell. 2020, 1, 100002. [Google Scholar] [CrossRef]
- Johnson, M.; Albizri, A.; Harfouche, A.A.; Fosso-Wamba, W. Integrating human knowledge into artificial intelligence for complex and ill-structured problems: Informed artificial intelligence. Int. J. Inf. Manag. 2022, 64, 10247. [Google Scholar] [CrossRef]
- Webster, J.; Watson, R.T. Analyzing the Past to Prepare for the Future: Writing a Literature Review. MIS Q. 2002, 26, xiii–xxiii. [Google Scholar]
- Kamboj, S.; Rahman, Z. Marketing capabilities and firm performance: Literature review and future research agenda. Int. J. Product. Perform. Manag. 2015, 64, 1041–1067. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Abbas, Z.; Raza, S.; Ejaz, K. Systematic reviews and their role in evidence—Informed health care. J. Pak. Med. Assoc. 2008, 58, 461–467. [Google Scholar]
- Kitsios, F.; Kamariotou, M.; Talias, M.A. Corporate sustainability strategies and decision support methods: A bibliometric analysis. Sustainability 2020, 12, 521. [Google Scholar] [CrossRef] [Green Version]
- Kitsios, F.; Kamariotou, M. Artificial intelligence and business strategy towards digital transformation: A research agenda. Sustainability 2021, 13, 2025. [Google Scholar] [CrossRef]
- Mahdi, S.S.; Battineni, G.; Khawaja, M.; Allana, R.; Siddiqui, M.K.; Agha, D. How does artificial intelligence impact digital healthcare initiatives? A review of AI applications in dental healthcare. Int. J. Inf. Manag. Data Insights 2023, 3, 100144. [Google Scholar] [CrossRef]
- Vishwakarma, L.P.; Singh, R.K.; Mishra, R.; Kumari, A. Application of artificial intelligence for resilient and sustainable healthcare system: Systematic literature review and future research directions. Int. J. Prod. Res. 2023, 1–23. [Google Scholar] [CrossRef]
- Siala, H.; Wang, Y. SHIFTing artificial intelligence to be responsible in healthcare: A systematic review. Soc. Sci. Med. 2022, 296, 114782. [Google Scholar] [CrossRef]
- Jahan, R.; Tripathi, M.M. Brain Tumor Detection using Machine Learning in MR Images. In Proceedings of the 10th IEEE International Conference on Communication Systems and Network Technologies, Bhopal, India, 18–19 June 2021; pp. 664–668. [Google Scholar]
- Ladgham, A.; Torkhani, G.; Sakly, A.; Mtibaa, A. Modified Support Vector Machines for MR Brain Images Recognition. In Proceedings of the International Conference on Control, Decision and Information Technologies, Hammamet, Tunisia, 6–8 May 2013; pp. 32–35. [Google Scholar]
- Rong, G.; Mendez, A.; Assi, E.B.; Zhao, B.; Sawan, M. Artificial intelligence in healthcare: Review and prediction case studies. Engineering 2020, 6, 291–301. [Google Scholar] [CrossRef]
- Wu, F.; Wu, T.; Yuce, M.R. Design and Implementation of a Wearable Sensor Network System for IoT-Connected Safety and Health Applications. In Proceedings of the 5th World Forum on Internet of Things, Limerick, Ireland, 15–18 April 2019; pp. 87–90. [Google Scholar]
- Gandhi, M.; Singh, V.K.; Kumar, V. IntelliDoctor—AI Based Medical Assistant. In Proceedings of the 5th International Conference on Science Technology Engineering and Mathematics, Chennai, India, 14–15 March 2019; pp. 162–168. [Google Scholar]
- Jaiman, V.; Urovi, V. A consent model for blockchain-based health data sharing platforms. IEEE Access 2020, 8, 143734–143745. [Google Scholar] [CrossRef]
- Zheng, X.; Mukkamala, R.R.; Vatrapu, R.; Ordieres-Mere, J. Blockchain-Based Personal Health Data Sharing System using Cloud Storage. In Proceedings of the 20th International Conference on e-Health Networking, Applications and Services, Ostrava, Czech Republic, 17–20 September 2018; pp. 1–6. [Google Scholar]
- Thakkar, B.A.; Hasan, M.I.; Desai, M.A. Health Care Decision Support System for Swine Flu Prediction using Naïve Bayes Classifier. In Proceedings of the International Conference on Advances in Recent Technologies in Communication and Computing, Kottayam, Kerala, India, 16–17 October 2010; pp. 101–105. [Google Scholar]
- Moein, M.; Davarpanah, M.; Montazeri, M.A.; Ataei, M. Classifying Ear Disorders using Support Vector Machines. In Proceedings of the 2nd International Conference on Computational Intelligence and Natural Computing, Wuhan, China, 13–14 September 2010; pp. 321–324. [Google Scholar]
- Nimmagadda, S.L.; Nimmagadda, S.K.; Dreher, H. Multidimensional Data Warehousing & Mining of Diabetes & Food-Domain Ontologies for e-Health. In Proceedings of the 9th IEEE International Conference on Industrial Informatics, Lisbon, Portugal, 26–29 July 2011; pp. 682–687. [Google Scholar]
- Bennett, C.; Doub, T.; Bragg, A.; Luellen, J.; Regenmorter, C.V.; Lockman, J.; Reiserer, R. Data Mining Session-Based Patient Reported Outcomes (PROs) in Mental Health Setting: Toward Data-Driven Clinical Decision Support and Personalized Treatment. In Proceedings of the 1st International Conference on Healthcare Informatics, Imaging and Systems Biology, San Jose, CA, USA, 26–29 July 2011. [Google Scholar]
- Seebock, P. Unsupervised identification of disease marker candidates in retinal OCT imaging data. IEEE Trans. Med. Imaging 2019, 38, 1037–1047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGregor, C. Health Analytics as a Service with Artemis Cloud: Service Availability. In Proceedings of the 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society, Montreal, QC, Canada, 20–24 July 2020; pp. 5644–5648. [Google Scholar]
- Albu, A. From Logical Inference to Decision Trees in Medical Diagnosis. In Proceedings of the E-Health and Bioengineering Conference, Sinaia, Romania, 22–24 June 2017; pp. 65–68. [Google Scholar]
- Patii, N.; Iyer, B. Health Monitoring and Tracking System for Soldiers using Internet of Things (IoT). In Proceedings of the International Conference on Computing, Communication and Automation, Greater Noida, India, 5–6 May 2017; pp. 1347–1352. [Google Scholar]
- Yang, G. IoT-based remote pain monitoring system: From device to cloud platform. IEEE J. Biomed. Health Inform. 2018, 22, 1711–1719. [Google Scholar] [CrossRef] [PubMed]
- Ciprian, C.; Masychev, K.; Ravan, M.; Reilly, J.P.; Maccrimmon, D. A machine learning approach using effective connectivity to predict response to clozapine treatment. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 2598–2607. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Zhang, X.; Wang, X.; Yang, G.; Guizani, N.; Du, X. Efficient and traceable patient health data search system for hospital management in smart cities. IEEE Internet Things J. 2021, 8, 6425–6436. [Google Scholar] [CrossRef]
- Hassan, T.; Hameed, A.; Nisar, S.; Kamal, N.; Hasan, O. Al-Zahrawi: A telesurgical robotic system for minimal invasive surgery. IEEE Syst. J. 2016, 10, 1035–1045. [Google Scholar] [CrossRef]
- Rahman, M.A.; Abualsaud, K.; Barnes, S.; Rashid, M.; Abdullah, S.M. A Natural User Interface and Blockchain-Based in-Home Smart Health Monitoring System. In Proceedings of the IEEE International Conference on Informatics, IoT, and Enabling Technologies, Doha, Qatar, 2–5 February 2020; pp. 262–266. [Google Scholar]
- Sakkos, D.; Mccay, K.D.; Marcroft, C.; Embleton, N.D.; Chattopadhyay, S.; Ho, E.S.L. Identification of abnormal movements in infants: A deep neural network for body part-based prediction of cerebral palsy. IEEE Access 2021, 9, 94281–94292. [Google Scholar] [CrossRef]
- Kumar, S.; Raut, R.D.; Narkhede, B.E. A proposed collaborative framework by using artificial intelligence-internet of things (AI-IoT) in COVID-19 pandemic situation for healthcare workers. Int. J. Healthc. Manag. 2020, 13, 337–345. [Google Scholar] [CrossRef]
- Khan, M.; Yaseen, Q.; Mumtaz, A.; Saleem, A.; Ishaq, S.; Udeen, H. Severe Analysis of Cardiac Disease Detection using the Wearable Device by Artificial Intelligence. In Proceedings of the International Conference for Innovation in Technology, Bangalore, India, 6–8 November 2020; pp. 1–8. [Google Scholar]
- Chauhan, T.; Rawat, S.; Malik, S.; Singh, P. Supervised and Unsupervised Machine Learning Based Review on Diabetes Care. In Proceedings of the 7th International Conference on Advanced Computing and Communication Systems, Coimbatore, India, 19–20 March 2021; pp. 581–585. [Google Scholar]
- Ahmed, I.; Jeon, G.; Piccialli, F. A Deep-Learning-based smart healthcare system for patient’s discomfort detection at the edge of Internet of Things. IEEE Internet Things J. 2021, 8, 10318–11032. [Google Scholar] [CrossRef]
- Wu, H.; Bowers, D.M.; Huynh, T.T.; Souvenir, R. Biomedical Video Denoising using Supervised Manifold Learning. In Proceedings of the IEEE 10th International Symposium on Biomedical Imaging, San Francisco, CA, USA, 7–11 April 2013; pp. 1244–1247. [Google Scholar]
- Zhang, Y. Collaborative unsupervised domain adaptation for medical image diagnosis. IEEE Trans. Image Process. 2020, 29, 7834–7844. [Google Scholar] [CrossRef]
- Azghadi, M.R. Hardware implementation of deep network accelerators towards healthcare and biomedical applications. IEEE Trans. Biomed. Circuits Syst. 2020, 14, 1138–1159. [Google Scholar] [CrossRef]
- Yanhong, F.; Bin, W.; Fengjuan, H.; Wenqiang, T. Research on Teleoperation Surgery Simulation System Based on Virtual Reality. In Proceedings of the 11th World Congress on Intelligent Control and Automation, Shenyang, China, 29 June–4 July 2014; pp. 5830–5834. [Google Scholar]
- Shim, S.; Ji, D.; Lee, S.; Choi, H.; Hong, J. Compact bone surgery robot with a high-resolution and high-rigidity remote center of motion mechanism. IEEE Trans. Biomed. Eng. 2020, 67, 2497–2506. [Google Scholar] [CrossRef]
- Gayathri, B.M.; Sumathi, C.P. Mamdani Fuzzy Inference System for Breast Cancer Risk Detection. In Proceedings of the International Conference on Computational Intelligence and Computing Research, Tamil Nadu, India, 10–12 December 2015; pp. 1–6. [Google Scholar]
- Katarya, R.; Srinivas, P. Predicting Heart Disease at Early Stages using Machine Learning: A Survey. In Proceedings of the International Conference on Electronics and Sustainable Communication Systems, Coimbatore, India, 2–4 July 2020; pp. 302–305. [Google Scholar]
- Harinishree, M.S.; Aditya, C.R.; Sachin, D.N. Detection of Breast Cancer using Machine Learning Algorithms—A Survey. In Proceedings of the 5th International Conference on Computing Methodologies and Communication, Erode, India, 8–10 April 2021; pp. 1598–1601. [Google Scholar]
- Amrane, M.; Oukid, S.; Gagaoua, I.; Ensari, T. Breast Cancer Classification using Machine Learning. In Proceedings of the Electric Electronics, Computer Science, Biomedical Engineerings’ Meeting, Istanbul, Turkey, 18–19 April 2018; pp. 1–4. [Google Scholar]
- Murray, M.; Macedo, M.; Glynn, C. Delivering Health Intelligence for Healthcare Services. In Proceedings of the 1st International Conference on Digital Data Processing, London, UK, 15–17 November 2019; pp. 88–91. [Google Scholar]
- Wong, D.L.T. An integrated wearable wireless vital signs biosensor for continuous inpatient monitoring. IEEE Sens. J. 2020, 20, 448–462. [Google Scholar] [CrossRef]
- Sasubilli, S.M.; Kumar, A.; Dutt, V. Machine Learning Implementation on Medical Domain to Identify Disease Insights using TMS. In Proceedings of the International Conference on Advances in Computing and Communication Engineering, Las Vegas, NV, USA, 22–24 June 2020; pp. 1–4. [Google Scholar]
- Razaak, M.; Martini, M.G.; Savino, K. A study on quality assessment for medical ultrasound video compressed via HEVC. IEEE J. Biomed. Health Inform. 2014, 18, 1552–1559. [Google Scholar] [CrossRef] [Green Version]
- Roa, D.; Bautista, J.; Rodríguez, N.; Villamil, M.P.; Jimenez, A.; Bernal, O. Data Mining: A New Opportunity to Support the Solution of Public Health Issues in Colombia. In Proceedings of the 6th Colombian Computing Congress, Manizales, Colombia, 4–6 May 2011; pp. 1–6. [Google Scholar]
- Rawte, V.; Anuradha, G. Fraud Detection in Health Insurance using Data Mining Techniques. In Proceedings of the International Conference on Communication, Information & Computing Technology, Mumbai, India, 15–17 January 2015; pp. 1–5. [Google Scholar]
- Daltayanni, M.; Wang, C.; Akella, R. A Fast-Interactive Search System for Healthcare Services. In Proceedings of the Annual SRII Global Conference, San Jose, CA, USA, 24–27 July 2012; pp. 525–534. [Google Scholar]
- Gangopadhyay, A.; Chen, S. Health Care Fraud Detection with Community Detection Algorithms. In Proceedings of the International Conference on Smart Computing, St. Louis, MO, USA, 18–20 May 2016; pp. 1–5. [Google Scholar]
- Anbarasi, M.S.; Dhivya, S. Fraud Detection using Outlier Predictor in Health Insurance Data. In Proceedings of the International Conference on Information Communication and Embedded Systems, Chennai, India, 23–24 February 2017; pp. 1–6. [Google Scholar]
- Thorntonl, D.; Capelleveen, G.; Poe, M. Outlier-based health insurance fraud detection for U.S. Medicaid data. Int. J. Enterp. Inf. Syst. 2015, 27, 684–694. [Google Scholar]
- Yang, W.S.; Hwang, S.Y. A hybrid approach for fraud detection in health insurance. Expert Syst. Appl. 2014, 31, 56–68. [Google Scholar] [CrossRef]
- Bagde, P.R.; Chaudhari, M.S. Analysis of fraud detection mechanism in health insurance using statistical data mining techniques. Int. J. Comput. Sci. Inf. Technol. 2016, 7, 925–926. [Google Scholar]
- Jumelle, A.K.L. Ethical Assessment in e-Health. In Proceedings of the 16th International Conference on e-Health Networking, Applications and Services, Natal, Brazil, 15–18 October 2014; pp. 262–268. [Google Scholar]
- Paranjape, K.; Schinkel, M.; Panday, R.N.; Car, J.; Nanayakkara, P. Introducing artificial intelligence training in medical education. JMIR Med. Educ. 2019, 5, e16048. [Google Scholar] [CrossRef]
- Torner, J.; Skouras, S.; Molinuevo, J.L.; Gispert, J.D.; Alpiste, F. Multipurpose virtual reality environment for biomedical and health applications. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 1511–1520. [Google Scholar] [CrossRef]
- Gupta, A.; Cecil, J.; Pirela-Cruz, M.; Ramanathan, P. A virtual reality enhanced cyber-human framework for orthopedic surgical training. IEEE Syst. J. 2019, 13, 3501–3512. [Google Scholar] [CrossRef]
- Rahman, M.M.; Khatun, F.; Uzzaman, A.; Sami, S.I.; Bhuiyan, M.A.A.; Kiong, T.S. A comprehensive study of artificial intelligence and machine learning approaches in confronting the coronavirus (COVID-19) pandemic. Int. J. Health Serv. 2021, 51, 446–461. [Google Scholar] [CrossRef]
- Ling, Y.; An, Y.; Liu, M.; Hu, X. An Error Detecting and Tagging Framework for Reducing Data Entry Errors in Electronic Medical Records (EMR) System. In Proceedings of the International Conference on Bioinformatics and Biomedicine, Shanghai, China, 18–21 December 2013; pp. 249–254. [Google Scholar]
- Hasan, M.; Fukuda, A.; Maruf, R.I.; Yokota, F.; Ahmed, A. Errors in Remote Healthcare System: Where, How and by Whom? In Proceedings of the TENCON 2017—2017 IEEE Region 10 Conference, Penang, Malaysia, 5–8 November 2017; pp. 170–175. [Google Scholar]
- Goldberg, S.I. A Weighty Problem: Identification, Characteristics and Risk Factors for Errors in EMR Data. In Proceedings of the AMIA Annual Symposium Proceedings, Washington, DC, USA, 13–17 November 2010; pp. 251–255. [Google Scholar]
- Madanan, M.; Zulkefli, N.A.M.; Velayudhan, N.C. Designing a Hybrid Artificial Intelligent Clinical Decision Support System using Artificial Neural Network and Artificial Bee Colony for Predicting Heart Failure Rate. In Proceedings of the International Conference on Computer Communication and Informatics, Coimbatore, India, 19–22 July 2021; pp. 1–7. [Google Scholar]
- Aljaaf, A.J.; Al-Jumeily, D.; Hussain, A.J.; Fergus, P.; Al-Jumaily, M.; Abdel-Aziz, K. Toward an Optimal Use of Artificial Intelligence Techniques within a Clinical Decision Support System. In Proceedings of the Science and Information Conference, London, UK, 28–30 July 2015; pp. 548–554. [Google Scholar]
- Kusano, T.; Paliyawan, P.; Harada, T.; Thawonmas, R. Towards Adaptive Motion Gaming AI with Player’s Behavior Modeling for Health Promotion. In Proceedings of the 6th Global Conference on Consumer Electronics, Nagoya, Japan, 24–27 October 2017; pp. 1–2. [Google Scholar]
- Srivastava, B.; Rossi, F. Rating AI systems for bias to promote trustable applications. IBM J. Res. Dev. 2019, 63, 51–59. [Google Scholar] [CrossRef]
- Lim, A.K.; Thumper, C. Opportunities and Challenges of Internet-Based Health Interventions in the Future Internet. In Proceedings of the 12th International Conference on Information Technology—New Generations, Las Vegas, NV, USA, 13–15 April 2015; pp. 567–573. [Google Scholar]
- Mohr, D.C.; Cuijpers, P.; Lehman, K. Supportive accountability: A model for providing human support to enhance adherence to eHealth interventions. J. Med. Internet Res. 2011, 13, 30e. [Google Scholar] [CrossRef] [PubMed]
- Tsang, K.C.H.; Pinnock, H.; Wilson, A.M.; Shah, S.A. Application of Machine Learning to Support Self-Management of Asthma with mHealth. In Proceedings of the 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society, Montreal, QC, Canada, 20–24 July 2020; pp. 5673–5677. [Google Scholar]
- Floridi, L.; Cowls, J.; Beltrametti, M.; Chatila, R.; Chazerand, P.; Dignum, V.; Vayena, E. AI4People—An ethical framework for a good AI society: Opportunities, risks, principles, and recommendations. Minds Mach. 2018, 28, 689–707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, B.K.; Miller, G.T.; Fonda, S.J.; Yeaw, R.E.; Gaudaen, J.C.; Pavliscsak, H.H.; Pamplin, J.C. Advanced digital health technologies for COVID-19 and future emergencies. Telemed. E-Health 2020, 26, 1226–1233. [Google Scholar] [CrossRef]
- Schwalbe, N.; Wahl, B. Artificial intelligence and the future of global health. Lancet 2020, 395, 1579–1586. [Google Scholar] [CrossRef]
- Secinaro, S.; Calandra, D.; Secinaro, A.; Muthurangu, V.; Biancone, P. The role of artificial intelligence in healthcare: A structured literature review. BMC Med. Inform. Decis. Mak. 2021, 21, 125. [Google Scholar] [CrossRef]
- Morley, J.; Machado, C.C.; Burr, C.; Cowls, J.; Joshi, I.; Taddeo, M.; Floridi, L. The ethics of AI in health care: A mapping review. Soc. Sci. Med. 2020, 260, 113172. [Google Scholar] [CrossRef]
- Sood, S.K.; Rawat, K.S.; Kumar, D. A visual review of artificial intelligence and Industry 4.0 in healthcare. Comput. Electr. Eng. 2022, 101, 107948. [Google Scholar] [CrossRef]
- Jobin, A.; Ienca, M.; Vayena, E. The global landscape of AI ethics guidelines. Nat. Mach. Intell. 2019, 1, 389–399. [Google Scholar] [CrossRef] [Green Version]
- Zerka, F. Blockchain for privacy preserving and trustworthy distributed machine learning in multi-centric medical imaging (C-DistriM). IEEE Access 2020, 8, 183939–183951. [Google Scholar] [CrossRef]
- Peters, D.; Vold, K.; Robinson, D.; Calvo, R.A. Responsible AI—Two frameworks for ethical design practice. IEEE Trans. Technol. Soc. 2020, 1, 34–47. [Google Scholar] [CrossRef]
- Wang, S. Big data privacy in biomedical research. IEEE Trans. Big Data 2020, 6, 296–308. [Google Scholar] [CrossRef]
- Jameel, T.; Ali, R.; Toheed, I. Ethics of Artificial Intelligence: Research Challenges and Potential Solutions. In Proceedings of the 3rd International Conference on Computing, Mathematics and Engineering Technologies, Sukkur, Pakistan, 29–30 January 2020; pp. 1–6. [Google Scholar]
- Richie, C. Environmentally sustainable development and use of artificial intelligence in health care. Bioethics 2022, 36, 547–555. [Google Scholar] [CrossRef]
- Bryson, J.J. Patiency is not a virtue: The design of intelligent systems and systems of ethics. Ethics Inf. Technol. 2018, 20, 15–26. [Google Scholar] [CrossRef] [Green Version]
- Esmaeilzadeh, P. Use of AI-based tools for healthcare purposes: A survey study from consumers’ perspectives. BMC Med. Inform. Decis. Mak. 2020, 20, 170. [Google Scholar] [CrossRef]
- Shaban-Nejad, A.; Michalowski, M.; Brownstein, J.S.; Buckeridge, D.L. Guest editorial explainable AI: Towards fairness, accountability, transparency and trust in healthcare. IEEE J. Biomed. Health Inform. 2021, 25, 2374–2375. [Google Scholar] [CrossRef]
- Chun, R. Ethical character and virtue of organizations: An empirical assessment and strategic implications. J. Bus. Ethics 2005, 57, 269–284. [Google Scholar] [CrossRef]
- Song, S.Y.; Kim, Y.K. Theory of virtue ethics: Do consumers’ good traits predict their socially responsible consumption? J. Bus. Ethics 2018, 152, 1159–1175. [Google Scholar] [CrossRef]
- Chatterjee, S.; Sarker, S.; Fuller, M. A deontological approach to designing ethical collaboration. J. Assoc. Inf. Syst. 2009, 10, 138–169. [Google Scholar] [CrossRef] [Green Version]
- Audi, R. Virtue ethics as a resource in business. Bus. Ethics Q. 2012, 22, 273–291. [Google Scholar] [CrossRef] [Green Version]
- Unberath, M.; Ghobadi, K.; Levin, S.; Hinson, J.; Hager, G.D. Artificial Intelligence-Based Clinical Decision Support for COVID-19—Where Art Thou? Adv. Intell. Syst. 2020, 2, 2000104. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarty, S.; Bass, A.E. Comparing virtue, consequentialist, and deontological ethics-based corporate social responsibility: Mitigating microfinance risk in institutional voids. J. Bus. Ethics 2015, 126, 487–512. [Google Scholar] [CrossRef]
- Vaishya, R.; Javaid, M.; Khan, I.H.; Haleem, A. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 337–339. [Google Scholar] [CrossRef] [PubMed]
- Rigby, M.J. Ethical dimensions of using artificial intelligence in health care. AMA J. Ethics 2019, 21, 121–124. [Google Scholar]
- Van der Schaar, M.; Alaa, A.M.; Floto, A.; Gimson, A.; Scholtes, S.; Wood, A.; Ercole, A. How artificial intelligence and machine learning can help healthcare systems respond to COVID-19. Mach. Learn. 2021, 110, 1–14. [Google Scholar] [CrossRef]
- Combs, C.D.; Combs, P.F. Emerging roles of virtual patients in the age of AI. AMA J. Ethics 2019, 21, E153–E159. [Google Scholar]
- Yu, K.H.; Beam, A.L.; Kohane, I.S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2018, 2, 719–731. [Google Scholar] [CrossRef]
- Powell, J. Trust Me, I’m a chatbot: How artificial intelligence in health care fails the turing test. J. Med. Internet Res. 2019, 21, e16222. [Google Scholar] [CrossRef]
- Abràmoff, M.D.; Leng, T.; Ting, D.S.; Rhee, K.; Horton, M.B.; Brady, C.J.; Chiang, M.F. Automated and computer-assisted detection, classification, and diagnosis of diabetic retinopathy. Telemed. E-Health 2020, 26, 544–550. [Google Scholar] [CrossRef] [Green Version]
- McCall, B. COVID-19 and artificial intelligence: Protecting health-care workers and curbing the spread. Lancet Digit. Health 2020, 2, e166–e167. [Google Scholar] [CrossRef]
- Lee, D.; Yoon, S.N. Application of artificial intelligence-based technologies in the healthcare industry: Opportunities and challenges. Int. J. Environ. Res. Public Health 2021, 18, 271. [Google Scholar] [CrossRef]
- Lee, S.; Lee, D. Healthcare wearable devices: An analysis of key factors for continuous use intention. Serv. Bus. 2020, 14, 503–531. [Google Scholar] [CrossRef]
- Yoon, S.; Lee, D. Artificial Intelligence and Robots in Healthcare: What are the Success Factors for Technology-based ServiceEncounters? Int. J. Healthc. Manag. 2019, 12, 218–225. [Google Scholar] [CrossRef]
- Chen, J.; See, K.C. Artificial intelligence for COVID-19: Rapid review. J. Med. Internet Res. 2020, 22, e21476. [Google Scholar] [CrossRef]
- Katiyar, S.; Farhana, A. Artificial Intelligence in e-Health: A Review of Current Status in Healthcare and Future Possible Scope of Research. J. Comput. Sci. 2022, 18, 928–939. [Google Scholar] [CrossRef]
- Kumar, Y.; Koul, A.; Singla, R.; Ijaz, M.F. Artificial intelligence in disease diagnosis: A systematic literature review, synthesizing framework and future research agenda. J. Ambient Intell. Humaniz. Comput. 2023, 14, 8459–8486. [Google Scholar] [CrossRef]
- Singh, A.; Mehta, J.C.; Anand, D.; Nath, P.; Pandey, B.; Khamparia, A. An intelligent hybrid approach for hepatitis disease diagnosis: Combining enhanced k-means clustering and improved ensemble learning. Expert Syst. 2021, 38, e12526. [Google Scholar] [CrossRef]
- Gulati, K.; Nayak, K.M.; Priya, B.S.; Venkatesh, B.; Satyam, Y.; Chahal, D. An Examination of How Robots, Artificial Intelligence, and Machinery Learning are Being Applied in the Medical and Healthcare Industries. Int. J. Recent Innov. Trends Comput. Commun. 2022, 10, 298–305. [Google Scholar] [CrossRef]
- Calton, B.; Abedini, N.; Fratkin, M. Telemedicine in the time of coronavirus. J. Pain Symptom Manag. 2020, 60, e12–e14. [Google Scholar] [CrossRef]
- Srivastava, S.; Pant, M.; Agarwal, R. Role of AI techniques and deep learning in analyzing the critical health conditions. Int. J. Syst. Assur. Eng. Manag. 2020, 11, 350–365. [Google Scholar] [CrossRef]
- Xu, Y.; Wang, T.; Chen, Z.; Jin, L.; Wu, Z.; Yan, J.; He, N. The point-of-care-testing of nucleic acids by chip, cartridge and paper sensors. Chin. Chem. Lett. 2021, 32, 3675–3686. [Google Scholar] [CrossRef]

| Authors | Year | Methodology |
|---|---|---|
| Mahdi et al. [47] | 2023 | In areas where AI is now playing a substantial role in clinical dentistry, this study attempts to systematically review that role. |
| Vishwakarma et al. [48] | 2023 | The purpose of this study is to comprehend how AI helps create a robust and sustainable healthcare system. |
| Ali et al. [2] | 2023 | This paper gives a thorough analysis of scholarly works on the use of AI in the healthcare industry. A total of 180 articles have been examined to present a classification framework based on four dimensions: AI-enabled healthcare benefits, challenges, methodologies, and functionalities. |
| Siala and Wang [49] | 2022 | This paper suggests a responsible AI initiative framework that includes five key themes for AI solution developers, healthcare professionals, and policy makers by combining pertinent knowledge from AI governance and ethics. These themes include inclusivity, fairness, inclusivity, sustainability, and transparency. A total of 253 papers were extracted from two databases. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kitsios, F.; Kamariotou, M.; Syngelakis, A.I.; Talias, M.A. Recent Advances of Artificial Intelligence in Healthcare: A Systematic Literature Review. Appl. Sci. 2023, 13, 7479. https://doi.org/10.3390/app13137479
Kitsios F, Kamariotou M, Syngelakis AI, Talias MA. Recent Advances of Artificial Intelligence in Healthcare: A Systematic Literature Review. Applied Sciences. 2023; 13(13):7479. https://doi.org/10.3390/app13137479
Chicago/Turabian StyleKitsios, Fotis, Maria Kamariotou, Aristomenis I. Syngelakis, and Michael A. Talias. 2023. "Recent Advances of Artificial Intelligence in Healthcare: A Systematic Literature Review" Applied Sciences 13, no. 13: 7479. https://doi.org/10.3390/app13137479
APA StyleKitsios, F., Kamariotou, M., Syngelakis, A. I., & Talias, M. A. (2023). Recent Advances of Artificial Intelligence in Healthcare: A Systematic Literature Review. Applied Sciences, 13(13), 7479. https://doi.org/10.3390/app13137479









