Three-Dimensional Printed Custom-Made Prostheses after Partial Scapulectomy: A Case Report
Abstract
1. Introduction
2. Detailed Case Description
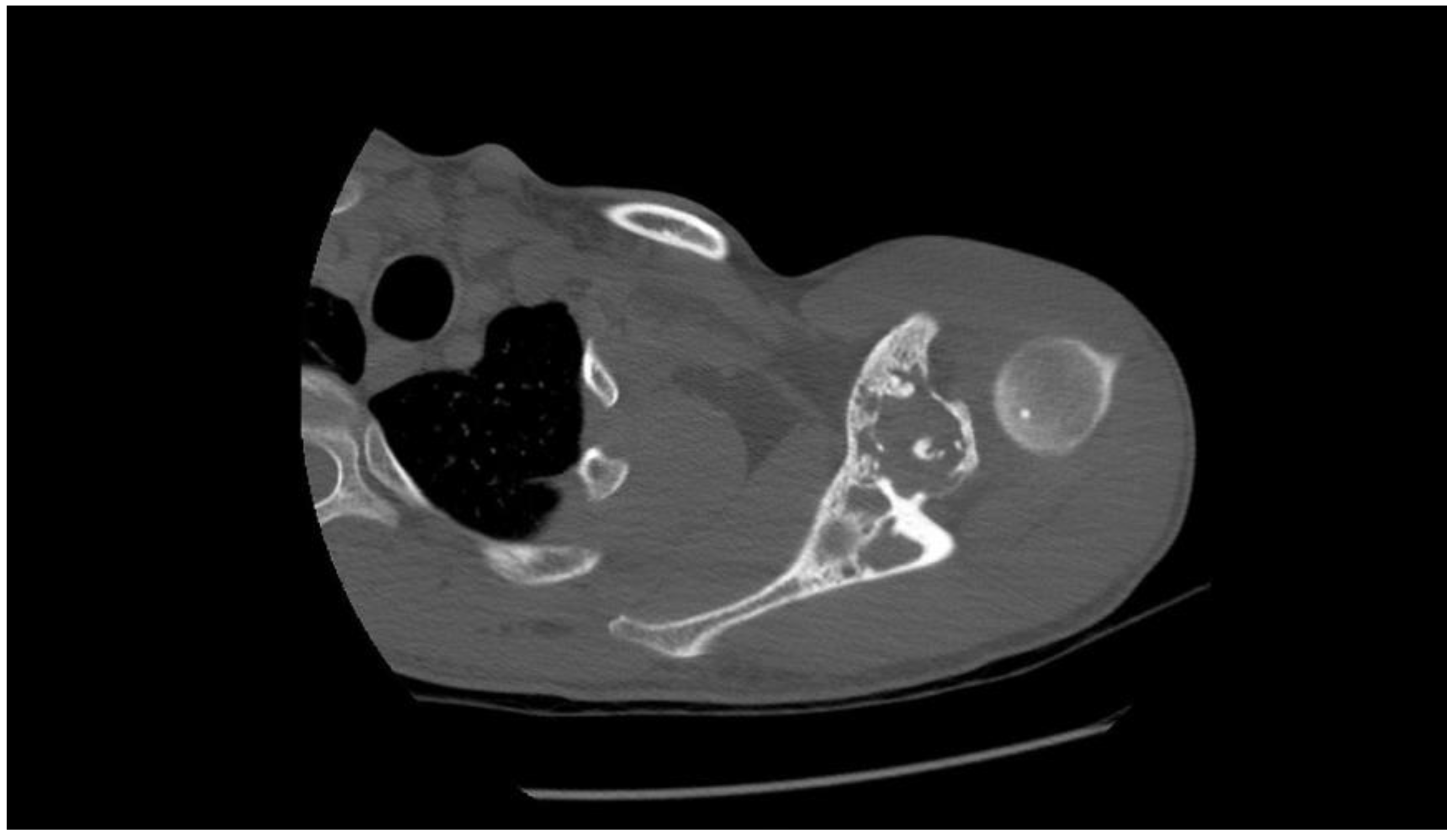
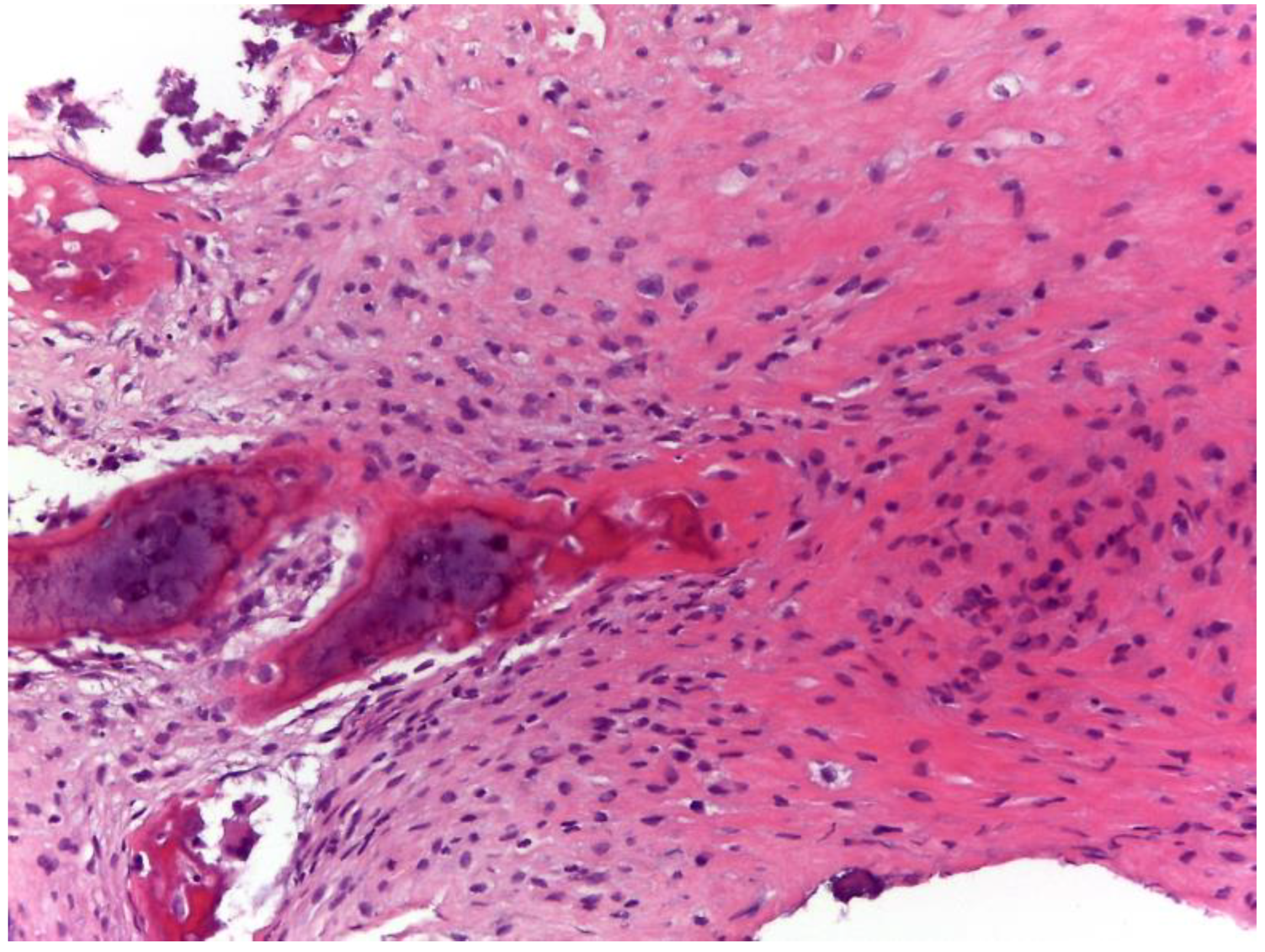
2.1. Oncological Staging
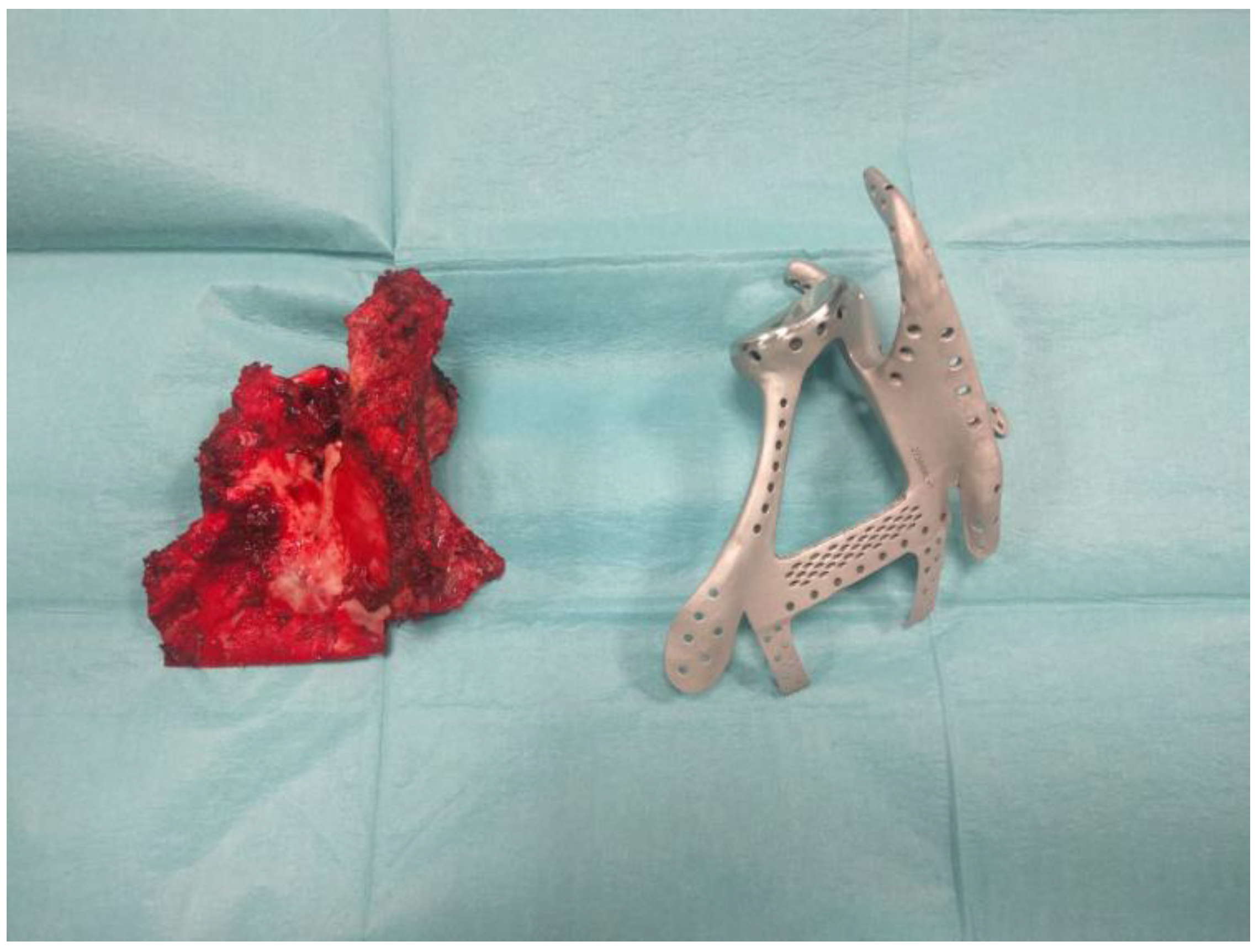
2.2. Prostheses Project
2.3. Surgery
2.4. Follow-Up
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arndt, C.A.; Crist, W.M. Common musculoskeletal tumors of childhood and adolescence. N. Engl. J. Med. 1999, 341, 342–352. [Google Scholar] [CrossRef]
- Sobin, L.H.; Fleming, I.D. TNM Classification of Malignant Tumors, fifth edition (1997). Union Internationale Contre le Cancer and the American Joint Committee on Cancer. Cancer 1997, 80, 1803–1804. [Google Scholar] [CrossRef]
- Choi, J.H.; Ro, J.Y. The 2020 WHO Classification of Tumors of Soft Tissue: Selected Changes and New Entities. Adv. Anat. Pathol. 2021, 28, 44–58. [Google Scholar] [CrossRef]
- Schwab, J.H.; Antonescu, C.R.; Athanasian, E.A.; Boland, P.J.; Healey, J.H.; Morris, C.D. A comparison of intramedullary and juxtacortical low-grade osteogenic sarcoma. Clin. Orthop. Relat. Res. 2008, 466, 1318–1322. [Google Scholar] [CrossRef] [PubMed]
- Malhas, A.M.; Sumathi, V.P.; James, S.L.; Menna, C.; Carter, S.R.; Tillman, R.M.; Jeys, L.; Grimer, R.J. Low-grade central osteosarcoma: A difficult condition to diagnose. Sarcoma 2012, 2012, 764796. [Google Scholar] [CrossRef]
- Choong, P.F.; Pritchard, D.J.; Rock, M.G.; Sim, F.H.; McLeod, R.A.; Unni, K.K. Low grade central osteogenic sarcoma. A long-term followup of 20 patients. Clin. Orthop. Relat. Res. 1996, 322, 198–206. [Google Scholar] [CrossRef]
- Andresen, K.J.; Sundaram, M.; Unni, K.K.; Sim, F.H. Imaging features of low-grade central osteosarcoma of the long bones and pelvis. Skelet. Radiol. 2004, 33, 373–379. [Google Scholar] [CrossRef]
- Kurt, A.M.; Unni, K.K.; McLeod, R.A.; Pritchard, D.J. Low-grade intraosseous osteosarcoma. Cancer 1990, 65, 1418–1428. [Google Scholar] [CrossRef] [PubMed]
- Pritsch, T.; Bickels, J.; Wu, C.C.; Squires, M.H.; Malawer, M.M. Is scapular endoprosthesis functionally superior to humeral suspension? Clin. Orthop. Relat. Res. 2007, 456, 188–195. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, M.I.; Sim, F.H.; Chao, E.Y. Limb salvage for neoplasms of the shoulder girdle. Intermediate reconstructive and functional results. J. Bone Jt. Surg. Am. 1996, 78, 1872–1888. [Google Scholar] [CrossRef]
- Malawer, M.M.; Meller, I.; Dunham, W.K. A new surgical classification system for shoulder-girdle resections. Analysis of 38 patients. Clin. Orthop. Relat. Res. 1991, 267, 33–44. [Google Scholar] [CrossRef]
- Enneking, W.F.; Spanier, S.S.; Goodman, M.A. A system for the surgical staging of musculoskeletal sarcoma. 1980. Clin. Orthop. Relat. Res. 2003, 415, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Parel, I.; Jaspers, E.; de Baets, L.; Amoresano, A.; Cutti, A.G. Motion analysis of the shoulder in adults: Kinematics and electromyography for the clinical practice. Eur. J. Phys. Rehabil. Med. 2016, 52, 575–582. [Google Scholar] [PubMed]
- Yian, E.H.; Ramappa, A.J.; Arneberg, O.; Gerber, C. The Constant score in normal shoulders. J. Shoulder Elb. Surg. 2005, 14, 128–133. [Google Scholar] [CrossRef]
- Constant, C.R.; Murley, A.H. A clinical method of functional assessment of the shoulder. Clin. Orthop. Relat. Res. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Padua, R.; Padua, L.; Ceccarelli, E.; Romanini, E.; Zanoli, G.; Amadio, P.; Campi, A. Italian version of the Disability of the Arm, Shoulder and Hand (DASH) questionnaire. Cross-cultural adaptation and validation. J. Hand Surg. Br. 2003, 28, 179–186. [Google Scholar] [CrossRef]
- Franchignoni, F.; Vercelli, S.; Giordano, A.; Sartorio, F.; Bravini, E.; Ferriero, G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J. Orthop. Sports Phys. Ther. 2014, 44, 30–39. [Google Scholar] [CrossRef]
- Wodajo, F.M.; Bickels, J.; Wittig, J.; Malawer, M. Complex reconstruction in the management of extremity sarcomas. Curr. Opin. Oncol. 2003, 15, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.-F.; Yu, X.-C.; Xu, M.; Hu, Y.-C.; Liu, X.-P. Functional Results and Emotional Acceptance after Scapulectomy for Malignant Shoulder Tumors. Orthop. Surg. 2016, 8, 186–195. [Google Scholar] [CrossRef]
- Vahanan, N.M.; Mohanlal, P.; Bose, J.C.; Gangadharan, R.; Karthisundar, V. The functional and oncological results after scapulectomy for scapular tumours: 2–16-year results. Int. Orthop. 2007, 31, 831–836. [Google Scholar] [CrossRef]
- Zhang, K.; Duan, H.; Xiang, Z.; Tu, C. Surgical technique and clinical results for scapular allograft reconstruction following resection of scapular tumors. J. Exp. Clin. Cancer Res. 2009, 28, 45. [Google Scholar] [CrossRef] [PubMed]
- Min, L.; Zhou, Y.; Tang, F.; Zhang, W.; Luo, Y.; Duan, H.; Tu, C. Reconstruction with scapular hemiarthroplasty endoprosthesis after scapulectomy for malignant tumour. Int. Orthop. 2017, 41, 1057–1063. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, G.; Frisoni, T.; Spazzoli, B.; Lucchese, A.; Donati, D. Computer assisted surgery and 3d printing in orthopaedic oncology: A lesson learned by cranio-maxillo-facial surgery. Appl. Sci. 2021, 11, 8584. [Google Scholar] [CrossRef]
- Deng, L.; Zhao, X.; Wei, C.; Qu, W.; Yu, L.; Zhu, S. Application of a three-dimensional printed segmental scapula prosthesis in the treatment of scapula tumors. J. Int. Med. Res. 2019, 47, 5873–5882. [Google Scholar] [CrossRef] [PubMed]





| Pre-Operative | 12 Months Post-Operative | |
|---|---|---|
| CMS Total | 65 | 51 |
| Pain | 10 | 15 |
| ADL | 4 | 4 |
| Hand Position | 10 | 10 |
| ROM | 32 | 22 |
| Strength | 9 | 5 |
| DASH | 35 (4.2%) | 44 (11.7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bianchi, G.; Benedetti, M.G.; Bardelli, R.; Platano, D.; Laranga, R.; Tuzzato, G. Three-Dimensional Printed Custom-Made Prostheses after Partial Scapulectomy: A Case Report. Appl. Sci. 2023, 13, 7056. https://doi.org/10.3390/app13127056
Bianchi G, Benedetti MG, Bardelli R, Platano D, Laranga R, Tuzzato G. Three-Dimensional Printed Custom-Made Prostheses after Partial Scapulectomy: A Case Report. Applied Sciences. 2023; 13(12):7056. https://doi.org/10.3390/app13127056
Chicago/Turabian StyleBianchi, Giuseppe, Maria Grazia Benedetti, Roberta Bardelli, Daniela Platano, Roberta Laranga, and Gianmarco Tuzzato. 2023. "Three-Dimensional Printed Custom-Made Prostheses after Partial Scapulectomy: A Case Report" Applied Sciences 13, no. 12: 7056. https://doi.org/10.3390/app13127056
APA StyleBianchi, G., Benedetti, M. G., Bardelli, R., Platano, D., Laranga, R., & Tuzzato, G. (2023). Three-Dimensional Printed Custom-Made Prostheses after Partial Scapulectomy: A Case Report. Applied Sciences, 13(12), 7056. https://doi.org/10.3390/app13127056






