Abstract
Background: Three-dimensional (3D) printing is an innovative technology widely used in dentistry for manufacturing objects of various shapes using different materials. It has gained increasing popularity in the field of pediatric dentistry, particularly in the production of space maintainers, which serve as a preventive orthodontic treatment following the early loss of primary molars. Aims: In this systematic review, we present a comprehensive overview of the manufacturing process for space maintainers, ranging from traditional procedures to the advancements in 3D printing technology. Materials and Methods: Our review adheres to the PRISMA criteria and includes scientific articles published until 27 May 2023, without any restriction on the publication period and language. To conduct our research, we searched electronic databases, such as Medline, Web of Science, and Embase, using specific keywords and MeSH terms. Results: We identified 9 articles that discussed the CAD/CAM manufacturing and 3D printing of various types of space maintainers. Conclusions: Based on this systematic review, it is evident that 3D-printed space maintainers offer great potential as an alternative to conventionally processed ones, by addressing their limitations. However, further studies are required to evaluate the accuracy, efficacy, and clinical success rates of different 3D printing technologies, materials, and designs for additive manufacturing of space maintainers.
1. Introduction
Since the 1980s, the innovative technology of three-dimensional (3D) printing, also referred to as additive manufacturing, has gained prominence as a manufacturing technique. The first application of 3D printing in dentistry can be traced back to the early 2000s. One of the initial uses was in the fabrication of dental models and molds for prosthodontics and orthodontics. In recent years, it has experienced rapid development in different fields of dentistry [1]. The literature has identified several advantages associated with implementing a digital workflow, wherein 3D printing plays a crucial role. These advantages include enhanced predictability in oral rehabilitation, more effective treatment options, reduced chairside time, minimized human errors in the manufacturing process, shorter procedure durations, increased patient comfort, and the potential to enhance the treatment skills of practitioners [2,3,4,5].
In the field of pediatric dentistry, the implementation of digitalization offers numerous benefits, such as improved patient cooperation and reduced fear among children. This is achieved by minimizing chairside procedure durations, thereby increasing children’s enthusiasm for regular dental appointments [2,3,4]. Preserving primary teeth until the normal exfoliation process is a crucial aspect of pediatric dentistry. Beyond their aesthetic, speech, and mastication functions, primary teeth play a vital role in guiding and facilitating the eruption of permanent teeth [4,6]. In cases involving congenitally missing teeth or the early loss of primary teeth, the effective management of the space during primary, mixed, and early permanent dentition becomes imperative. This approach ensures the maintenance of proper masticatory and speech function, while also preventing malocclusion resulting from undesirable tooth movement [4,7,8,9,10,11].
A dentist may recommend various types of removable or fixed space maintainers (SMs), including band and loop, crown and loop, distal end shoe, lingual arch, Nance, and transpalatal arch, which are based on factors such as the number of lost teeth, stage of dental development, age of the child, and whether unilateral or bilateral tooth loss is present in the affected dental arch [4]. The American Academy of Pediatric Dentistry (AAPD) recommends the use of space maintainers (SMs) as an essential aspect of preventive orthodontics. This is due to their ability to maintain the position of existing dentition, which helps prevent the loss of arch length, width, and perimeter [12,13,14]. Therefore, SMs are recommended to maintain the space, mostly in the premature loss of a single primary molar, until the eruption of the succeeding tooth, or the insertion of an implant [4,7,8,10,11].
Within the various types of space maintainers, removable space maintainers (RSMs) offer the advantage of not only preserving the mesiodistal space but also maintaining the vertical height of the teeth, thus, restoring their aesthetic appearance. When designing RSMs, it is essential to consider a long lingual base, with or without a very short vestibular base. This design consideration is crucial because the fixation of RSMs should not solely rely on snap rings on the buccal side, and it is important to ensure that the development and growth of the dental arch remain undisturbed [15,16].
The conventional manufacturing process of removable space maintainers (RSMs) is intricate and requires skilled technicians. It is a technique-sensitive procedure, and ensuring the precision and fit of RSMs can be challenging due to the shrinkage of self-curing resin during polymerization [17,18]. However, with the advent of computer-aided design/computer-aided manufacturing (CAD/CAM) technology, manufacturing more accurate RSMs has become possible. These RSMs can be made from materials such as poly methyl methacrylate (PMMA) or acrylic resin, which are lightweight and provide stable results [16]. In case of any growth-related changes, 3D-printed RSMs offer added flexibility as they can be easily trimmed, adjusted, relined, or even reprinted since digital files are readily available [19].
The band and loop is the most commonly used type of fixed space maintainer (SM), particularly in cases of unilateral tooth loss or bilateral loss of primary molars when the permanent incisors have not fully erupted [12,13,20,21,22]. In situations where there is early loss of a primary first molar, placing an SM on the primary second molar before the eruption of the permanent first molar is crucial to prevent mesial migration and loss of space [23]. This type of SM consists of two components: the loop, which passively rests on the adjacent tooth and extends over the edentulous space, and the band that encircles the abutment tooth [20,21,22].
Lab-based band and loop SMs have certain disadvantages, including solder failure, corrosion, time-consuming construction, inadequate band pinching, and the potential development of caries along the band’s margin [24,25]. Challenges such as transferring the pinched band onto the impression and controlling the flame during the soldering process further complicate the procedure, as overheating can lead to breakage [26]. Additionally, achieving optimal results with lab-based SMs requires close collaboration between the dentist and the dental lab technician [27].
As an alternative to the conventional band and loop SMs and to overcome their disadvantages, some studies have suggested the use of technique-sensitive fiber-reinforced composite resin (FRCR)-based space maintainers, including polyethylene fibers, pre-impregnated silanized E-glass fibers with Bis-GMA, with or without PMMA, and CAD/CAM-aided ceramic-based and polymer-based SMs [16,21,25,28,29,30,31,32,33].
Digital impressions have emerged as a technology that enhances patient confidence and cooperation, increases procedural efficiency, and reduces long-term costs. Instead of relying on conventional dental casts, digital impressions allow dental professionals to work with digital 3D models [11,34]. This technology also enables digital documentation, eliminating the need for physical storage of patient data [35]. Intraoral scanners, which capture digital impressions, offer a safer alternative to conventional impressions by eliminating the risk of aspiration or ingestion [11,34]. In fact, a study revealed that 77% of patients prefer intraoral scans over traditional impressions [36].
In pediatric dentistry, the use of intraoral scanners has several advantages. It improves children’s cooperation by allowing pauses during scanning and offers a real-time visual representation of what is happening in the mouth through familiar photographs, thereby sparking the child’s curiosity [11,34]. When utilizing intraoral scanners in pediatric patients, it is crucial to consider the size of the scanner head. This factor affects intraoral maneuverability and scanning time and should be compatible with the shallow vestibules and limited mouth opening in children and young patients [37].
There are two approaches to consider after generating digital models: printing the models and proceeding with a conventional procedure or utilizing a digital process for the design stage of the space maintainer. Due to various clinical and procedural challenges associated with conventional space maintainers, alternative 3D-printed SMs have been proposed and documented. Presently, through the integration of digital 3D models into a CAD/CAM system, it is possible to 3D-print dental models, design SMs based on digital 3D models, and fabricate more accurate space maintainers using 3D-printing technologies [16,27].
The aim of this review was to comprehensively assess the viability of using digital 3D-printed SMs, based on published evidence. To achieve this objective, we provide a detailed analysis of the various materials and manufacturing technologies utilized in the production of digital 3D-printed SMs, highlighting the advantages and disadvantages associated with each approach.
2. Materials and Methods
2.1. Eligibility Criteria
The inclusion criteria for this review encompassed original articles, case reports, technique reports, pilot studies, and clinical research that discussed the utilization of CAD/CAM or 3D printing technology in the manufacturing of fixed or removable space maintainers specifically for pediatric patients. Published articles without any language restrictions were included.
Conversely, review articles, clinical trials, and randomized clinical trials were excluded from consideration. Additionally, studies reporting on other types of preventive orthodontic appliances, such as lingual retainers, were also excluded from the review.
2.2. Design and Search Strategy
In conducting this systematic review, the PRISMA 2020 guidelines were followed. This review is based on a systematic literature search of published papers in Medline, Embase, and Web of Science databases with no time and language restriction, up to 27 May 2023, and using the search strategy described in Table 1. The reference list of the included articles was manually searched to identify any additional potential papers.

Table 1.
Search strategy.
We have addressed the patient, intervention, comparison, and outcome (PICO) question, as follows:
Patient: children with the early loss of primary teeth in need of space maintainers.
Intervention: fixed or removable space maintainer.
Comparison: additive manufacturing and conventional production of space maintainers.
Outcome: advantages and disadvantages, including cost-efficiency, precision, time-efficacy, and patient cooperation.
2.3. Data Collection and Study Quality Assessment
Two independent examiners screened the titles and abstracts from the initial search. Articles that were deemed relevant, based on the predefined inclusion criteria, by at least one of the reviewers were selected for the next phase, which involved assessing the full-text versions of the articles. Finally, both examiners entered all relevant information into a dedicated data sheet specifically designed for this systematic review.
2.4. Risk of Bias Assessment
The available number of studies on 3D-printed space maintainers (SMs) was limited, with only three studies providing quantitative data. However, the specific success and failure rates were not reported. Due to the scarcity of studies and the heterogeneous nature of the quality and data structure among them, it was not feasible to conduct a pooled random-effects meta-analysis or utilize statistical tests such as Cochran’s Q test or I2 value. Additionally, the Newcastle–Ottawa assessment scale, as well as forest and funnel plots, could not be employed due to the limitations mentioned above.
3. Results
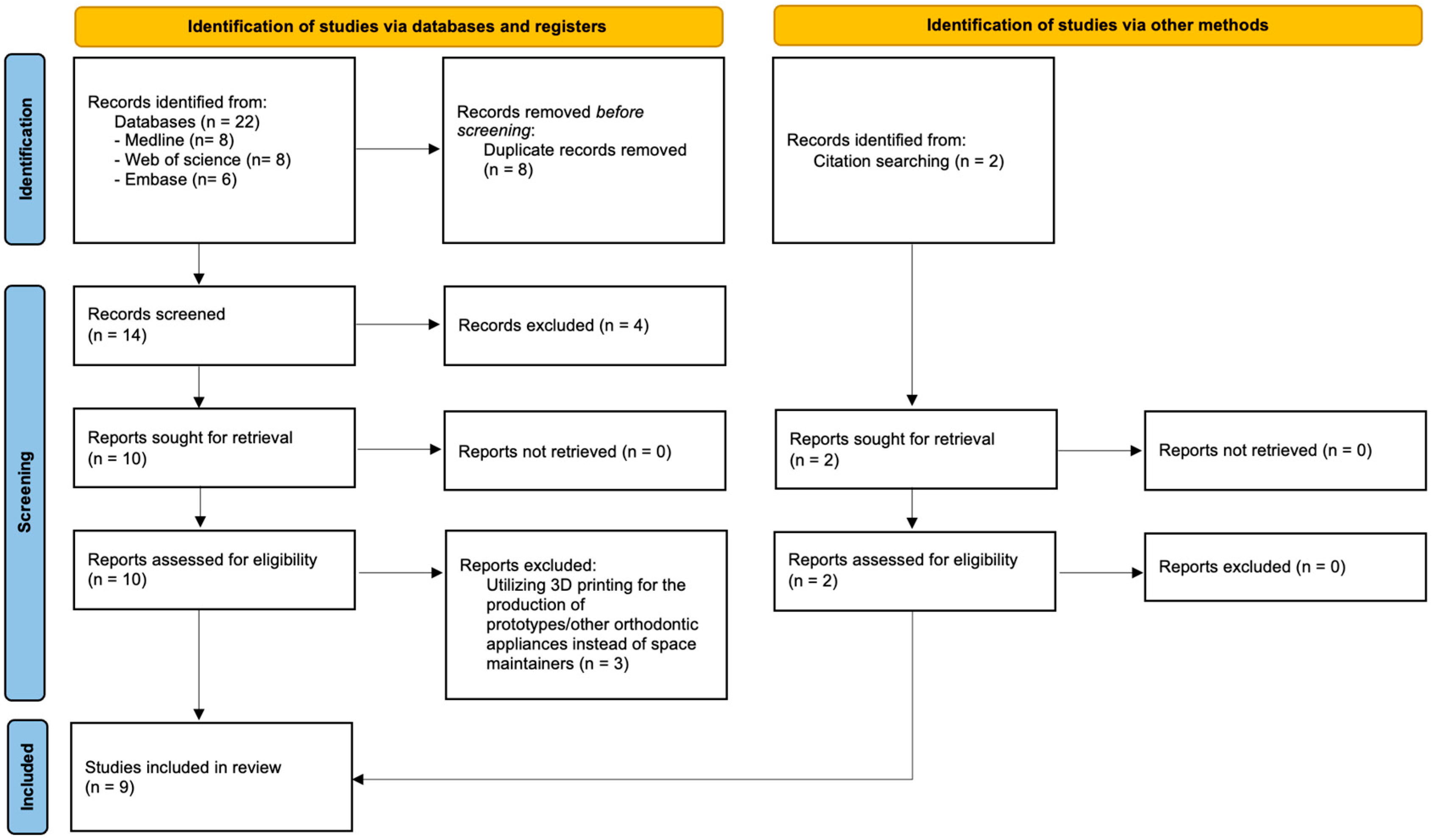
A flow diagram of the literature selection process in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) is shown in Figure 1 [38]. As shown, the search identified a total of 22 records. After screening the records for eligibility, nine studies were included.
Figure 1.
Flow diagram of study selection using PRISMA 2020.
Table 2 presents an overview of the included studies, highlighting their respective characteristics. Four studies reported the milling of space maintainers using materials such as PMMA and polyether ether ketone (PEEK). Three studies specifically examined titanium-based space maintainers that were manufactured utilizing metal 3D printers and micro laser sintering technology. Additionally, two studies investigated the use of zirconia-based space maintainers.

Table 2.
Characteristics of included articles.
4. Discussion
In this systematic review, the objective was to offer a comprehensive understanding of the manufacturing process of space maintainers in pediatric dentistry, ranging from traditional methods to the utilization of 3D printing technology. A total of nine articles were examined, which focused on the 3D printing of various types of space maintainers. The results indicate that 3D-printed space maintainers exhibit promising potential as an alternative to conventionally processed ones, effectively addressing their limitations.
The advancement of additive manufacturing technologies has prompted rapid progress within the healthcare sector, encompassing various fields of dentistry [43]. The applications of 3D-printing span across education, research, patient awareness, and digital treatment planning by utilizing 3D models, as well as clinical utilization [35,44,45]. While there is a wealth of literature exploring the implementation of this technology in prosthodontics, reconstructive and restorative dentistry [46,47], implantology, oral surgery [48], and orthodontics [49,50], research in the field of pediatric dentistry remains relatively limited.
The clinical implementation of 3D printing in pediatric dentistry includes the development of a 3D-printed fluoride adhesive film, enabling the creation of a slow-release delivery system. This is particularly relevant due to the challenges posed by the continuous flow of saliva and the act of chewing, which make it difficult to maintain an optimal fluoride concentration within the oral cavity [4,27,40,51,52,53,54]. In prosthetic procedures within the realm of pediatric dentistry, the utilization of 3D-printed crowns has demonstrated superior marginal integrity and retention, resulting in fewer instances of cementation failure compared to crowns fabricated through CAD/CAM techniques. Moreover, 3D-printed partial or complete dentures have proven to be beneficial for patients presenting with diverse teeth abnormalities [51,55,56].
Additive manufacturing offers a notable advantage in presurgical planning for cancer cases and reconstruction planning of mandible fractures, which are the second-most prevalent facial fractures in children. By utilizing a 3D-printed mandible model, the placement of titanium plates becomes more challenging due to the presence of tooth germs in growing patients. Additionally, this approach significantly reduces surgical time under general anesthesia [57,58,59,60,61]. The application of 3D-printing technology also contributes to the enhanced success rate of autotransplantation. This is achieved by reducing the extraoral time interval between the tooth extraction and the transplantation through recipient bone site modification and the preparation of the tooth for a temporary crown prior to extraction [62]. Furthermore, 3D printing finds utility in the creation of space maintainers and various orthodontic appliances, including Hawley retainers, brackets, and clear aligners. These applications of 3D printing significantly benefit the fields of preventive and corrective orthodontics [57,58,59,60,61].
Remarkably, the number of studies investigating the utilization of CAD/CAM and 3D-printing technology in the manufacturing of space maintainers (SMs) is limited. Among the existing studies, a variety of methodologies, materials, and technologies have been reported. While the more advanced and advantageous 4D printing technology has been introduced, which is capable of creating self-folding structures that reshape over time or space, it has not been applied in the field of pediatric dentistry, and therefore, no scientific reports on its implementation were found [43,63].
- Manufacturing technologies
In clinical dental practices, the choice of additive materials and their corresponding applications determine the manufacturing technology that is employed. Various technologies including stereolithography, digital light processing, photopolymer, material, and binder jetting, alongside selective laser sintering/melting, and fused filament fabrication can be utilized depending on the specific requirements [64].
- Laser sintering
Approximately 21 years ago, laser sintering technology emerged as a groundbreaking advancement in the dental field, ultimately, revolutionizing the processing of non-precious alloys. This technology was initially utilized for printing metallic structures, such as crowns, bridges, or clasp-retained cast-metal frameworks [65,66]. Laser sintering operates on a powder-based layer-additive manufacturing technique, thereby employing a continuous or pulse mode laser beam as a heat source to scan and fuse powders together [67].
The first documented case of fabricating 3D-printed band-loop space maintainers was reported by Pawar et al. [27]. They digitally designed a space maintainer using a 3D model and utilized titanium powder metallurgy with micro laser sintering technology for manufacturing. The authors discovered that incorporating innovative digital technology into the design and production process of space maintainers made it more convenient and time-efficient compared to conventional methods. This signifies the promising potential of 3D printing technology in the field of pediatric dentistry [27].
This finding aligns with another study where researchers utilized micro laser sintering technology and titanium powder metallurgy to manufacture a 3D-printed space maintainer for an uncooperative patient. They observed a notable improvement in the child’s cooperation following the placement of the 3D-printed space maintainer. Additionally, during the 6-month follow-up visit, the 3D-printed space maintainer remained intact without any signs of plaque accumulation or gingival inflammation. The authors attributed the resilience of the 3D-printed space maintainer to its single-unit fabrication, which eliminated the need for soldering, and its precise adaptation that did not disrupt occlusion. They also noted that the 3D-printed space maintainer featured a more complex structure with finer details. They concluded that even though the 3D-printed SM was not the most cost-effective option, the benefits outweighed the disadvantages [55]. It is important to consider that reduced plaque accumulation or gingival inflammation may also be influenced by the oral hygiene practices of the patient.
In a study conducted in 2022, the fitting of conventional and 3D-printed metallic band-loop space maintainers was examined. The conventional group consisted of a 0.9 mm loop piece made from thick stainless-steel wire, which was soldered to a prefabricated stainless steel molar band. For the digital group, space maintainers were designed digitally and fabricated using an HBD-100 metal 3D printer with titanium powder metallurgy. To assess the fit, the space maintainers from both groups were digitally evaluated by superimposing the standard tessellation language (STL) files obtained from scans. After performing a best-fit alignment, the abutment teeth were selected, and a 3D deviation analysis was conducted. The results indicated no significant differences in the fit of the conventional and 3D-printed metallic band-loop space maintainers (p-value = 0.56) [39].
- Milling
In comparison to the additive manufacturing process, subtractive processes, such as CAD/CAM milling, are slower and result in more material waste. Another characteristic of the milling process is that it does not allow for adjustments in mechanical and aesthetic properties during 3D printing since the properties are predetermined by the manufacturer of the prefabricated blocks [65,68].
A study in 2022 introduced a fully digital workflow for manufacturing fixed esthetic space maintainers in growing patients [2]. In this study, a scan taken prior to tooth extraction enabled the restoration of the pontic in the space maintainer using a digital wax pattern. In cases where only an intraoral scan was available after extraction, the CAD software’s “copy/mirror” tool was used to replicate the pontic from the contralateral tooth. The position of the pontic was adjusted within the dental arch, and two digitally designed clasp retainers were placed on adjacent teeth. Subsequently, the STL file of the designed space maintainer was imported into a milling machine, and the space maintainer was milled from PMMA material. After extraction, the 3D-printed space maintainer was cemented in place and its fit was assessed [2].
The authors concluded that the fully digital workflow and CAD/CAM fabrication technique led to favorable clinical outcomes and could be used not only on pediatric patients but also on any patients who were waiting for prostheses or dental implants [2]. The results of this study align with the findings of Guo et al. (2020), who conducted a comparative analysis of the fit accuracy of space maintainers manufactured using two different methods: milling PMMA and conventional techniques. The space between the tissue surface and the space maintainer was measured using 3D variation analysis. The quantitative assessments revealed statistically significant differences between the conventional space maintainers and the PMMA digital space maintainers. This study examined the feasibility of employing CAD/CAM technology in the fabrication of space maintainers and lays the groundwork for future clinical applications in this field [42].
In the studies conducted by Ierardo et al. [33] and Guo et al. [16], PEEK material was utilized in the fabrication of removable space maintainers (RSMs) using a CAD/CAM system [16,33]. PEEK, a semi-crystalline polymer, exhibits favorable characteristics, including biocompatibility, mechanical strength, durability, lightweight, dimensional stability, and low affinity for plaque accumulation. These properties make PEEK a promising alternative material for manufacturing space maintainers [33,69,70,71,72]. Furthermore, a study conducted in 2020 demonstrated the high suitability of removable PEEK space maintainers for clinical applications. However, it should be noted that PEEK space maintainers have certain limitations, particularly in the anterior tooth region, such as the higher fabrication cost and limited color options [16].
In the aforementioned study, removable space maintainers were produced using two different methods. The first method involved conventional manufacturing using a Type 2 Class I denture base polymer powder (self-curing denture powder, 1R, biomimetic color, NISSIN™, Osaka, Japan). The second method utilized a 5-axis numerical-control milling machine to fabricate space maintainers out of PEEK material. The objective of this study was to assess the suitability of the digital technique and computer-aided manufacturing in space maintainer production [16].
Following a series of qualitative and quantitative evaluations, the researchers reported that the CAD/CAM-fabricated removable space maintainers demonstrated a favorable fit and were deemed suitable for clinical applications. In addition, the group that received PEEK-based space maintainers exhibited significantly smaller maximum and mean distances compared to the conventional group, as indicated by statistical analysis (p-value < 0.05) [16].
In another study, the manufacturing process of three prototypes, namely lingual arch (1.3 mm thick), band and loop, and removable plate, was described. These prototypes were fabricated using PEEK material through a digital workflow employing the Roland DWX-50 5-axis milling machine [33]. According to patient feedback, the PEEK space maintainers were found to be comfortable and satisfactory, offering ease of polishing and cleaning. Notably, no instances of fracturing or decementation were reported, indicating the durability and reliability of the PEEK prototypes [33].
- Stereolithography
Stereolithography (SLA) is the oldest and most widely employed 3D-printing technique in dentistry. It involves the creation of a layered structure using UV-sensitive material that undergoes polymerization [55,64,68,73]. Another type of space maintainer made from clear photopolymer resin material has been reported, although no specific results were provided for this particular space maintainer, as only the cementation of the 3D-printed metal-based space maintainer was discussed [27].
- Other technologies
The first utilization of CAD/CAM technology to fabricate a zirconia-based space maintainer was reported in 2017 [25]. This innovative approach demonstrated notable characteristics, including high flexural strength, exceptional resistance to thermal shock, low thermal expansion, and availability in various shades [25,74].
In the study conducted by Soni et al. [25], the zirconia-based space maintainer exhibited positive outcomes. There were no indications of tissue irritation or gingival inflammation during the 6-month follow-up period, and patients did not report any difficulties with mastication. These findings highlight that ceramic space maintainers offer a viable alternative to conventional band and loop designs, by providing advantages such as improved aesthetics and strength [25].
In a study conducted by Lee et al. in 2022, further advantages of employing CAD/CAM technology for the production of zirconia-based space maintainers were reported [41]. These benefits encompassed improved retention of the space maintainer, reduced risk of cement loss, enhanced mechanical and biological properties, and increased satisfaction among patients and parents [41].
In summarizing Table 3, multiple studies have identified several advantages of CAD/CAM technology, including:

Table 3.
Advantages and disadvantages of using CAD/CAM technology in SM manufacturing.
- -
- improved patient cooperation and comfort
- -
- decreased chair-side and laboratory time
- -
- enhanced precision
- -
- enhanced efficacy and effectiveness
- Strengths and Limitations
The presented review article excels in providing the most up-to-date comprehensive and systematic approach for assessing the evolving field of additive manufactured space maintainers in pediatric dentistry, which currently has limited specific research. By establishing a strong foundation, this article paves the way for future work in this area.
This systematic review encompassed case reports due to the limited availability of literature and the absence of long-term systematic studies for result comparison. The majority of studies did not provide information regarding the cost and printing location using different additive manufacturing technologies for space maintainers. Consequently, it was not feasible to conduct a cost-effectiveness analysis considering the point of care or laboratory printing. Furthermore, the heterogeneity of methodologies among the included articles restricted the ability to compare success rates, materials, and printing technologies.
5. Conclusions
Recent advancements in digitalization within the field of pediatric dentistry offer a less invasive and highly precise procedure that is more cost-effective for patients and more appealing for practitioners. These developments have the viability and potential to revolutionize the traditional workflow for fabricating space maintainers, leading to improved clinical outcomes.
The existing studies on the application of CAD/CAM technology for fabricating space maintainers in pediatric dentistry suggest a promising future in overcoming the limitations and difficulties associated with conventional manufacturing processes. Further research is warranted to explore the integration of digital workflows into routine dental practice. It is crucial to assess the impact of various materials, designs, and construction methods on clinical survival time, as well as to verify the accuracy and reliability. Additionally, evaluating the cost of machines and training requirements for individuals involved in the clinical application of this technology is essential. These areas are recommended as key areas for future studies to facilitate the successful clinical implementation of CAD/CAM technology in pediatric dentistry.
Author Contributions
Conceptualization, P.Z. (Paridokht Zarean), P.Z. (Parichehr Zarean) and K.W.N.; methodology, P.Z. (Paridokht Zarean), P.Z. (Parichehr Zarean), P.S. and K.W.N.; software, P.Z. (Paridokht Zarean), P.Z. (Parichehr Zarean) and K.W.N.; validation, P.Z. (Paridokht Zarean), P.Z. (Parichehr Zarean) and K.W.N.; formal analysis, P.Z. (Paridokht Zarean), P.Z. (Parichehr Zarean), P.S. and K.W.N.; investigation, P.Z. (Paridokht Zarean), P.Z. (Parichehr Zarean) and K.W.N.; data curation, P.Z. (Paridokht Zarean), P.Z. (Parichehr Zarean) and K.W.N.; writing—original draft preparation, P.Z(Paridokht Zarean). and P.Z. (Parichehr Zarean); writing—review and editing, P.Z. (Paridokht Zarean), P.Z. (Parichehr Zarean), P.S. and K.W.N.; visualization, P.Z. (Paridokht Zarean) and P.Z. (Parichehr Zarean); supervision, K.W.N.; project administration, P.Z. (Paridokht Zarean), P.Z. (Parichehr Zarean) and K.W.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available upon request to the authors.
Acknowledgments
The authors thank Christian Appenzeller-Herzog for his assistance with the literature searches.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tsolakis, I.A.; Gizani, S.; Panayi, N.; Antonopoulos, G.; Tsolakis, A.I. Three-Dimensional Printing Technology in Orthodontics for Dental Models: A Systematic Review. Children 2022, 9, 1106. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, L.P.; Dourado, P.H.N.; de Araújo, C.A.R.; No-Cortes, J.; Pinhata-Baptista, O.H. Digital workflow to produce esthetic space maintainers for growing patients. J. Prosthet. Dent. 2022, 2022, S0022-3913. [Google Scholar] [CrossRef] [PubMed]
- Dursun, E.; Costa, A.M.-D.; Moussally, C. Chairside CAD/CAM Composite Onlays for the Restoration Of Primary Molars. J. Clin. Pediatr. Dent. 2018, 42, 349–354. [Google Scholar] [CrossRef]
- Dhanotra, K.G.; Bhatia, R. Digitainers-Digital Space Maintainers: A Review. Int. J. Clin. Pediatr. Dent. 2021, 14 (Suppl. 1), S69–S75. [Google Scholar] [CrossRef] [PubMed]
- Jheon, A.H.; Oberoi, S.; Solem, R.C.; Kapila, S. Moving towards precision orthodontics: An evolving paradigm shift in the planning and delivery of customized orthodontic therapy. Orthod. Craniofac. Res. 2017, 20 (Suppl. 1), 106–113. [Google Scholar] [CrossRef] [PubMed]
- Barbería, E.; Lucavechi, T.; Cárdenas, D.; Maroto, M. Free-end space maintainers: Design, utilization and advantages. J. Clin. Pediatr. Dent. 2006, 31, 5–8. [Google Scholar] [CrossRef]
- Nadelman, P.; Magno, M.B.; Pithon, M.M.; Castro, A.C.R.; Maia, L.C. Does the premature loss of primary anterior teeth cause morphological, functional and psychosocial consequences? Braz. Oral Res. 2021, 35, e092. [Google Scholar] [CrossRef]
- Uribe, F.; Meiers, J.C.; Nanda, R. Fixed retention of congenitally missing maxillary lateral incisors using a chairside, prefabricated fiber-reinforced composite bridge. World J. Orthod. 2008, 9, 349–354. [Google Scholar]
- Dogan, M.C.; Dogan, S.K.; Kendi, E. Complications of pediatric denture misuse: A case report. Oral Health Prev Dent. 2005, 3, 127–130. [Google Scholar]
- Watt, E.; Ahmad, A.; Adamji, R.; Katsimpali, A.; Ashley, P.; Noar, J. Space maintainers in the primary and mixed dentition-a clinical guide. Br. Dent. J. 2018, 225, 293–298, Erratum in: Br. Dent. J. 2018, 225, 555. [Google Scholar] [CrossRef]
- Vij, A.A.; Reddy, A. Using digital impressions to fabricate space maintainers: A case report. Clin. Case Rep. 2020, 8, 1274–1276. [Google Scholar] [CrossRef] [PubMed]
- Cornelius, C.P.; Ehrenfeld, M. The Use of MMF Screws: Surgical Technique, Indications, Contraindications, and Common Problems in Review of the Literature. Craniomaxillofac Trauma Reconstr. 2010, 3, 55–80. [Google Scholar] [CrossRef] [PubMed]
- Fathian, M.; Kennedy, D.B.; Nouri, M.R. Laboratory-made space maintainers: A 7-year retrospective study from private pediatric dental practice. Pediatr Dent. 2007, 29, 500–506. [Google Scholar]
- American Academy of Pediatric Dentistry. Management of the developing dentition and occlusion in pediatric dentistry. The reference manual of pediatric dentistry. Chic. Ill Am. Acad. Pediatr. Dent. 2020, 33, 393–409. [Google Scholar]
- Law, C.S. Management of premature primary tooth loss in the child patient. J. Calif. Dent. Assoc. 2013, 41, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Wang, Y.; Zhao, Y.; Liu, H. Computer-aided design of polyetheretherketone for application to removable pediatric space maintainers. BMC Oral Health. 2020, 20, 201. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, N.; Grover, J.; Panthri, P. Space maintenance with an innovative “tube and loop” space maintainer (Nikhil appliance). Int. J. Clin. Pediatr. Dent. 2016, 9, 86. [Google Scholar]
- Kawara, M.; Komiyama, O.; Kimoto, S.; Kobayashi, N.; Kobayashi, K.; Nemoto, K. Distortion behavior of heat-activated acrylic denture-base resin in conventional and long, low-temperature processing methods. J. Dent. Res. 1998, 77, 1446–1453. [Google Scholar] [CrossRef]
- Krishnamurthy, D.M.; Singh, R.; Mistry, G. Interim three-dimensional printed overlay prosthesis for an adolescent patient with oligodontia. J. Indian Prosthodont. Soc. 2021, 21, 304–307. [Google Scholar] [CrossRef]
- Ahmad, A.J.; Parekh, S.; Ashley, P.F. Methods of space maintenance for premature loss of a primary molar: A review. Eur. Arch. Paediatr. Dent. 2018, 19, 311–320. [Google Scholar] [CrossRef]
- Garg, A.; Samadi, F.; Jaiswal, J.N.; Saha, S. ‘Metal to resin’: A comparative evaluation of conventional band and loop space maintainer with the fiber reinforced composite resin space maintainer in children. J. Indian Soc. Pedod. Prev. Dent. 2014, 32, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Wright, G.Z.; Kennedy, D.B. Space control in the primary and mixed dentitions. Dent. Clin. N. Am. 1978, 22, 579–601. [Google Scholar] [CrossRef]
- Laing, E.; Ashley, P.; Naini, F.B.; Gill, D.S. Space maintenance. Int. J. Paediatr. Dent. 2009, 19, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Kirzioğlu, Z.; Ertürk, M.S. Success of reinforced fiber material space maintainers. J. Dent. Child. 2004, 71, 158–162. [Google Scholar]
- Soni, H.K. Application of CAD-CAM for Fabrication of Metal-Free Band and Loop Space Maintainer. Clin. Diagn. Res. 2017, 11, ZD14–ZD16. [Google Scholar] [CrossRef]
- Hill, C.J.; Sorenson, H.W.; Mink, J.R. Space maintenance in a child dental care program. J. Am. Dent. Assoc. 1975, 90, 811–815. [Google Scholar] [CrossRef]
- Pawar, B.A. Maintenance of space by innovative three-dimensional-printed band and loop space maintainer. J. Indian Soc. Pedod. Prev. Dent. 2019, 37, 205–208. [Google Scholar] [CrossRef]
- Kargul, B.; Caglar, E.; Kabalay, U. Glass fiber reinforced composite resin space maintainer: Case reports. J. Dent. Child. 2003, 70, 258–261. [Google Scholar]
- Kargul, B.; Caglar, E.; Kabalay, U. Glass fiber-reinforced composite resin as fixed space maintainers in children: 12-month clinical follow-up. J. Dent. Child. 2005, 72, 109–112. [Google Scholar]
- Mittal, S.; Sharma, A.; Sharma, A.K.; Gupta, K.K.; Gaur, A.; Pathania, V. Banded versus Single-sided bonded space maintainers: A Comparative Study. J. Dent. Sci. 2018, 10, 29–36. [Google Scholar]
- Subramaniam, P.; Babu, G.; Sunny, R. Glass fiber-reinforced composite resin as a space maintainer: A clinical study. J. Indian Soc. Pedod. Prev. Dent. 2008, 26 (Suppl. 3), S98–S103. [Google Scholar] [PubMed]
- Tuloglu, N.; Bayrak, S.; Tunc, E.S. Different clinical applications of bondable reinforcement ribbond in pediatric dentistry. Eur. J. Dent. 2009, 3, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Ierardo, G.; Luzzi, V.; Lesti, M.; Vozza, I.; Brugnoletti, O.; Polimeni, A.; Bossù, M. Peek polymer in orthodontics: A pilot study on children. J. Clin. Exp. Dent. 2017, 9, e1271–e1275. [Google Scholar] [CrossRef] [PubMed]
- Zarean, P.; Zarean, P.; Thieringer, F.M.; Mueller, A.A.; Kressmann, S.; Erismann, M.; Sharma, N.; Benitez, B.K. A Point-of-Care Digital Workflow for 3D Printed Passive Presurgical Orthopedic Plates in Cleft Care. Children 2022, 9, 1261. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, C.; Madhuri, G.; Sharma, N.; Ranjan, S.; Ade, S.; Pusa, D. Glimpse of 3D printing in dentistry: A review. J. Adv. Med. Dent. Scie Res. 2021, 9, 127–130. [Google Scholar]
- Vasudavan, S.; Sullivan, S.R.; Sonis, A.L. Comparison of intraoral 3D scanning and conventional impressions for fabrication of orthodontic retainers. J. Clin. Orthod. 2010, 44, 495–497. [Google Scholar]
- Yilmaz, H.; Aydin, M.N. Digital versus conventional impression method in children: Comfort, preference and time. Int. J. Paediatr. Dent. 2019, 29, 728–735. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Tokuc, M.; Yilmaz, H. Comparison of fit accuracy between conventional and CAD/CAM-fabricated band-loop space maintainers. Int. J. Paediatr. Dent. 2022, 32, 764–771. [Google Scholar] [CrossRef]
- Khanna, S.; Rao, D.; Panwar, S.; Pawar, B.A.; Ameen, S. 3D Printed Band and Loop Space Maintainer: A Digital Game Changer in Preventive Orthodontics. J. Clin. Pediatr. Dent. 2021, 45, 147–151. [Google Scholar] [CrossRef]
- Lee, J.H. Fully digital workflow for the fabrication of a tooth-colored space maintainer for a young patient. J. Esthet. Restor. Dent. 2022, 35, 561–566. [Google Scholar] [CrossRef]
- Guo, H.; Zhao, Y.; Feng, S.; Liu, H. Laser Medical Image Reconstruction and Computer Aided Design of Polymethyl Methacrylate for Pediatric Removable Space Maintainer Applications. J. Med. Imaging Health Inform. 2020, 10, 2842–2848. [Google Scholar] [CrossRef]
- Mondal, K.; Tripathy, P.K. Preparation of Smart Materials by Additive Manufacturing Technologies: A Review. Materials 2021, 14, 6442. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, S.; Nahar, P.; Ali, H.M. Current perspectives of 3D printing in dental applications. Braz. Dent. Sci. 2021, 24, 1–9. [Google Scholar] [CrossRef]
- Oberoi, G.; Nitsch, S.; Edelmayer, M.; Janjić, K.; Müller, A.S.; Agis, H. 3D Printing-Encompassing the Facets of Dentistry. Front. Bioeng. Biotechnol. 2018, 6, 172. [Google Scholar] [CrossRef]
- Zandinejad, A.; Khanlar, L.N.; Barmak, A.B.; Ikeda, M.; Tagami, J.; Masri, R. Shear bond strength of porcelain to milled and stereolithography additively manufactured zirconia with and without surface treatment: An in vitro study. J. Prosthet. Dent. 2023, in press. [CrossRef]
- Revilla-León, M.; Gómez-Polo, M.; Park, S.H.; Barmak, A.B.; Özcan, M. Adhesion of veneering porcelain to cobalt-chromium dental alloys processed with casting, milling, and additive manufacturing methods: A systematic review and meta-analysis. J. Prosthet. Dent. 2022, 128, 575–588. [Google Scholar] [CrossRef]
- Hegedus, T.; Kreuter, P.; Kismarczi-Antalffy, A.A.; Demeter, T.; Banyai, D.; Vegh, A.; Geczi, Z.; Hermann, P.; Payer, M.; Zsembery, A.; et al. User Experience and Sustainability of 3D Printing in Dentistry. Int. J. Environ. Res. Public Health 2022, 19, 1921. [Google Scholar] [CrossRef]
- Huang, S.; Wei, H.; Li, D. Additive manufacturing technologies in the oral implant clinic: A review of current applications and progress. Front. Bioeng. Biotechnol. 2023, 11, 1100155. [Google Scholar] [CrossRef]
- Revilla-León, M.; Sadeghpour, M.; Özcan, M. A Review of the Applications of Additive Manufacturing Technologies Used to Fabricate Metals in Implant Dentistry. J. Prosthodont. 2020, 29, 579–593. [Google Scholar] [CrossRef]
- Lee, S. Prospect for 3D printing technology in medical, dental and pediatric dental field. J. Korean Acad. Pediatr. Dent. 2016, 43, 93–108. [Google Scholar] [CrossRef]
- Byakodi, J. Application of 3D printing in dentistry-review. Eur. J. Pharm. Med. Res. 2019, 6, 139–141. [Google Scholar]
- Jindal, P.; Juneja, M.; Siena, F.L.; Bajaj, D.; Breedon, P. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Nagib, R.; Szuhanek, C.; Moldoveanu, B.; Negrutiu, M.L.; Sinescu, C.; Brad, S. Custom designed orthodontic attachment manufactured using a biocompatible 3D printing material. Mater. Plast. 2017, 54, 757–758. [Google Scholar] [CrossRef]
- Al-Halabi, M.N.; Bshara, N.; Nassar, J.A.; Comisi, J.C.; Rizk, C.K. Clinical Performance of Two Types of Primary Molar Indirect Crowns Fabricated by 3D Printer and CAD/CAM for Rehabilitation of Large Carious Primary Molars. Eur. J. Dent. 2021, 15, 463–468. [Google Scholar] [CrossRef]
- Pillai, S.; Upadhyay, A.; Khayambashi, P.; Farooq, I.; Sabri, H.; Tarar, M.; Lee, K.T.; Harb, I.; Zhou, S.; Wang, Y.; et al. Dental 3D-Printing: Transferring Art from the Laboratories to the Clinics. Polymers 2021, 13, 157. [Google Scholar] [CrossRef]
- Du, Y.; Yang, D.; Pang, Y.; Liu, C.; Zhang, K. Application of CAD and 3D printing in the treatment of pediatric multiple mandible fractures: A case report. Med. Case Rep. Study Protoc. 2021, 2, e0095. [Google Scholar] [CrossRef]
- Dupret-Bories, A.; Vergez, S.; Meresse, T.; Brouillet, F.; Bertrand, G. Contribution of 3D printing to mandibular reconstruction after cancer. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2018, 135, 133–136. [Google Scholar] [CrossRef]
- Lee, A.Y.; Patel, N.A.; Kurtz, K.; Edelman, M.; Koral, K.; Kamdar, D.; Goldstein, T. The use of 3D printing in shared decision making for a juvenile aggressive ossifying fibroma in a pediatric patient. Am. J. Otolaryngol. 2019, 40, 779–782. [Google Scholar] [CrossRef]
- Dong, Z.; Li, Q.; Bai, S.; Zhang, L. Application of 3-Dimensional Printing Technology to Kirschner Wire Fixation of Adolescent Condyle Fracture. J. Oral Maxillofac. Surg. 2015, 73, 1970–1976. [Google Scholar] [CrossRef]
- Chakravarthy, C.; Gupta, N.C.; Patil, R. A Simplified Digital Workflow for the Treatment of Pediatric Mandibular Fractures Using Three-Dimensional (3D) Printed Cap Splint: A Case Report. Craniomaxillofacial Trauma Reconstr. Open 2019, 3, e67–e70. [Google Scholar] [CrossRef]
- Obregon, F.; Vaquette, C.; Ivanovski, S.; Hutmacher, D.W.; Bertassoni, L.E. Three-dimensional bioprinting for regenerative dentistry and craniofacial tissue engineering. J. Dent. Res. 2015, 94 (Suppl. 9), 143S–152S. [Google Scholar] [CrossRef]
- Tibbits, S. 4D printing: Multi-material shape change. Archit Des. 2014, 84, 116–121. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry-State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Dolabdjian, H.; Strietzel, R. Method of Manufacture of Dental Prostheses and Auxiliary Elements. European Patent Application 1 021 997 B2, 26 July 2000. (In German). [Google Scholar]
- Kumar, S. Selective laser sintering: A qualitative and objective approach. JOM 2003, 55, 43–47. [Google Scholar] [CrossRef]
- Venkatesh, K.V.; Nandini, V.V. Direct metal laser sintering: A digitised metal casting technology. J. Indian Prosthodont Soc. 2013, 13, 389–392. [Google Scholar] [CrossRef] [PubMed]
- Zarean, P.; Malgaroli, P.; Zarean, P.; Seiler, D.; de Wild, M.; Thieringer, F.M.; Sharma, N. Effect of Printing Parameters on Mechanical Performance of Material-Extrusion 3D-Printed PEEK Specimens at the Point-of-Care. Appl. Sci. 2023, 13, 1230. [Google Scholar] [CrossRef]
- Verma, S.; Sharma, N.; Kango, S.; Sharma, S. Developments of PEEK (Polyetheretherketone) as a biomedical material: A focused review. Eur. Polym. J. 2021, 147, 110295. [Google Scholar] [CrossRef]
- Schwitalla, A.D.; Spintig, T.; Kallage, I.; Müller, W.D. Flexural behavior of PEEK materials for dental application. Dent. Mater. 2015, 31, 1377–1384. [Google Scholar] [CrossRef]
- Zoidis, P.; Papathanasiou, I.; Polyzois, G. The Use of a Modified Poly-Ether-Ether-Ketone (PEEK) as an Alternative Framework Material for Removable Dental Prostheses. A Clinical Report. J. Prosthodont. 2016, 25, 580–584. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Fang, Y.; Liao, Y.; Chen, G.; Gao, C.; Zhu, P. 3D printing and digital processing techniques in dentistry: A review of literature. Adv. Eng. Mater. 2019, 21, 1801013. [Google Scholar] [CrossRef]
- Mcomie, M. Aesthetic Long-Span Bridge Using BruxZir. Dental Tribune Middle East & Africa Edition; September–October. Available online: https://www.yumpu.com/en/document/read/50868219/esthetic-long-span-bridgeusing-bruxzir (accessed on 27 May 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).