Author Contributions
Conceptualization, A.P., D.D.-D. and K.P.; methodology, M.D.-D., D.D.-D. and A.P.; software, D.D.-D.; validation, M.D.-D.; formal analysis, A.P. and D.D.-D.; investigation, A.P., D.D.-D. and K.M.; resources, M.D.-D. and K.P.; data curation, D.D.-D. and M.D.-D.; writing—original draft preparation, A.P., D.D.-D. and M.D.-D.; writing—review and editing, A.P., D.D.-D., M.D.-D., K.M. and K.P.; visualization, D.D.-D.; supervision, A.P.; project administration, K.P.; funding acquisition, K.P. All authors have read and agreed to the published version of the manuscript.
Figure 1.
The CT scan of a tooth with a pantographic curve, with the blue line marking the angle and perspective for the front view, can be generated separately. The red line marks the pantographic curve.
Figure 1.
The CT scan of a tooth with a pantographic curve, with the blue line marking the angle and perspective for the front view, can be generated separately. The red line marks the pantographic curve.
Figure 2.
The procedure leading to the creation of a three-dimensional bone model is (a) a CT scan, axial tooth’s cross-sections, (b) a three-dimensional image of the bone structure and teeth; yellow: axial plane, green: longitudinal plane, pink: transverse plane, (c) tooth’s transverse cross-sections, and (d) tooth’s longitudinal cross-sections.
Figure 2.
The procedure leading to the creation of a three-dimensional bone model is (a) a CT scan, axial tooth’s cross-sections, (b) a three-dimensional image of the bone structure and teeth; yellow: axial plane, green: longitudinal plane, pink: transverse plane, (c) tooth’s transverse cross-sections, and (d) tooth’s longitudinal cross-sections.
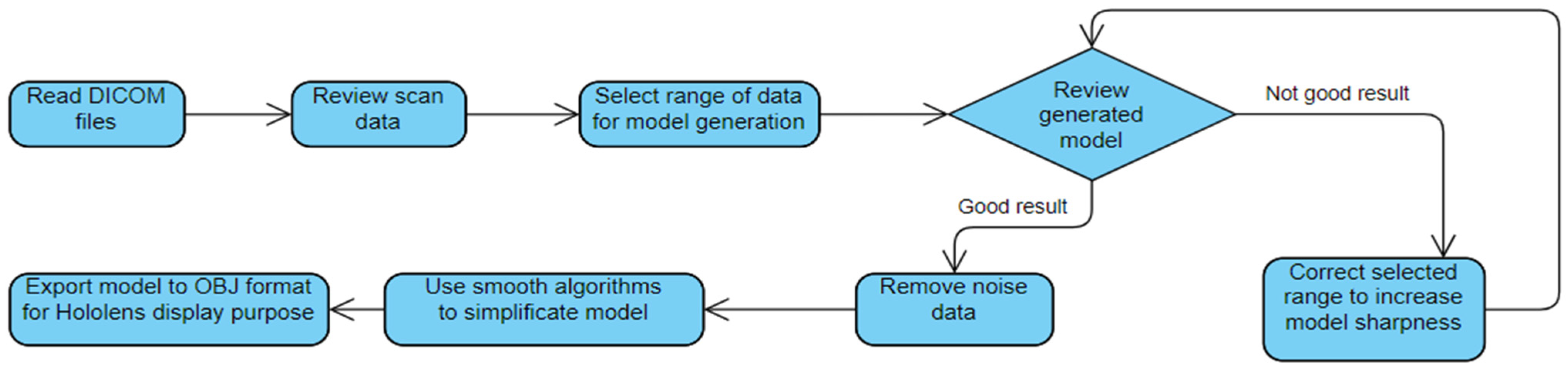
Figure 3.
The scheme of the MR-based supporting system for root canal treatment.
Figure 3.
The scheme of the MR-based supporting system for root canal treatment.
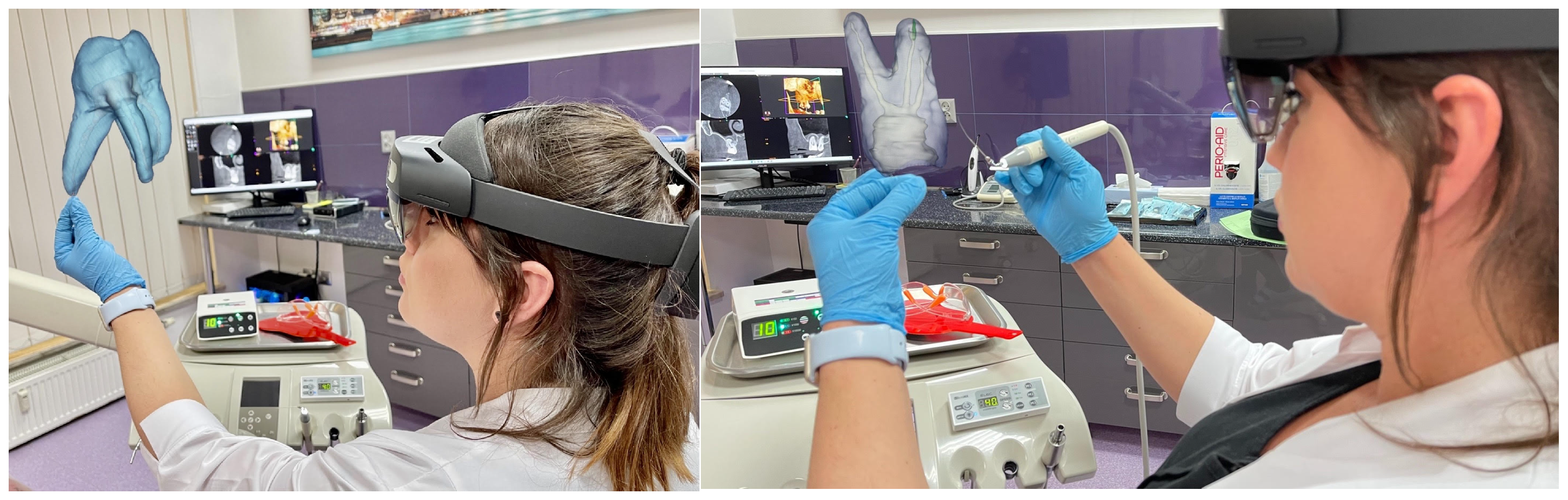
Figure 4.
The MR-based supporting system for root canal treatment.
Figure 4.
The MR-based supporting system for root canal treatment.
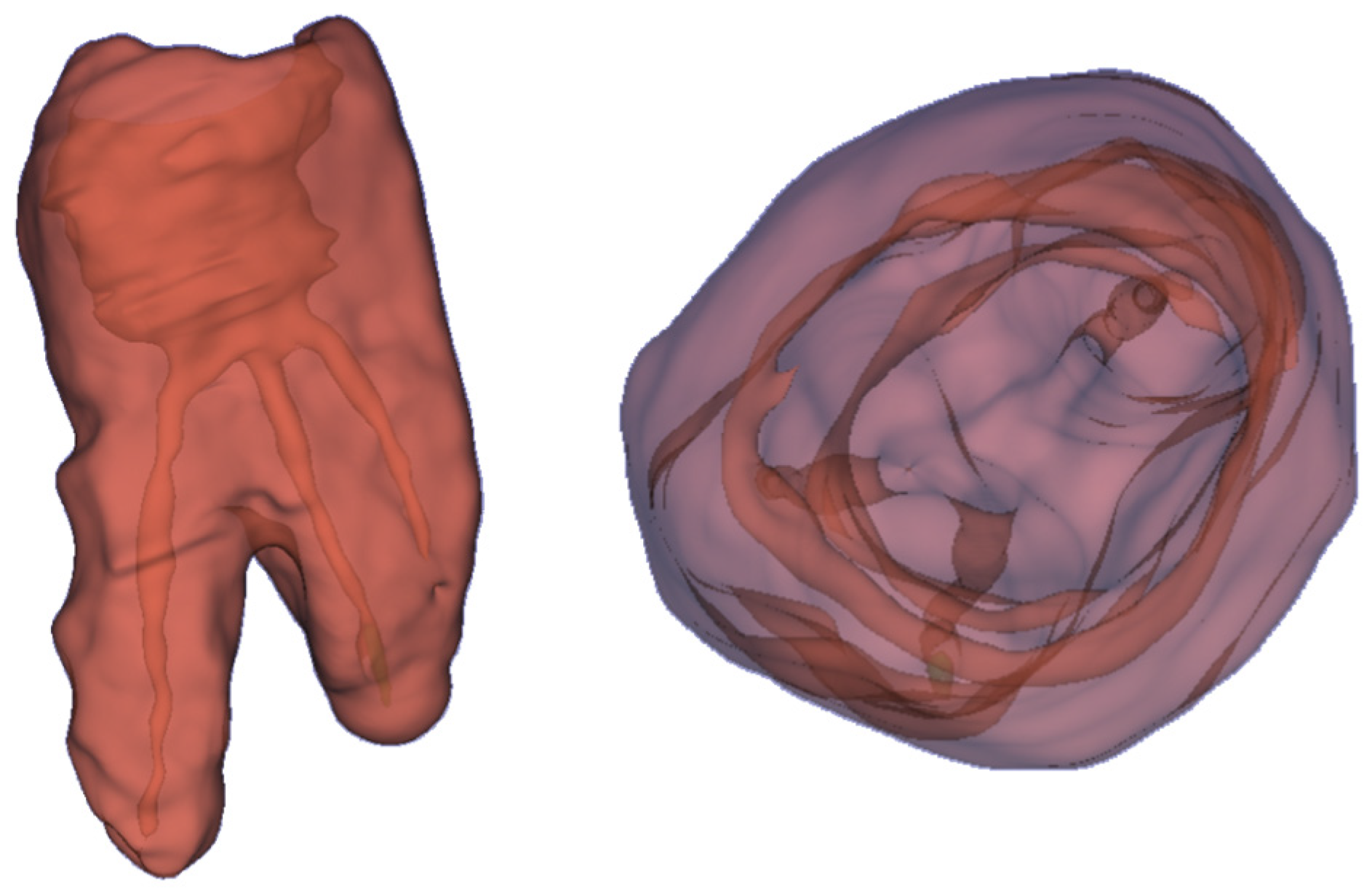
Figure 5.
The 3D holograms of the tooth, with visible root canals.
Figure 5.
The 3D holograms of the tooth, with visible root canals.
Figure 6.
The screenshot of the application enables the creation of 3D holograms based on the CT scan (DICOM data).
Figure 6.
The screenshot of the application enables the creation of 3D holograms based on the CT scan (DICOM data).
Figure 7.
The CT scan of the tooth was used for the analysis of the root canals in the transverse plane, in the case of tooth 17 with carious pulp exposure.
Figure 7.
The CT scan of the tooth was used for the analysis of the root canals in the transverse plane, in the case of tooth 17 with carious pulp exposure.
Figure 8.
The 3D of tooth 17 with carious pulp exposure.
Figure 8.
The 3D of tooth 17 with carious pulp exposure.
Figure 9.
The CT scan of the tooth was used for the analysis of the root canals in the transverse plane, in the case of tooth 16, where the yellow line denotes the axial plane, and the green line denotes the longitudinal plane.
Figure 9.
The CT scan of the tooth was used for the analysis of the root canals in the transverse plane, in the case of tooth 16, where the yellow line denotes the axial plane, and the green line denotes the longitudinal plane.
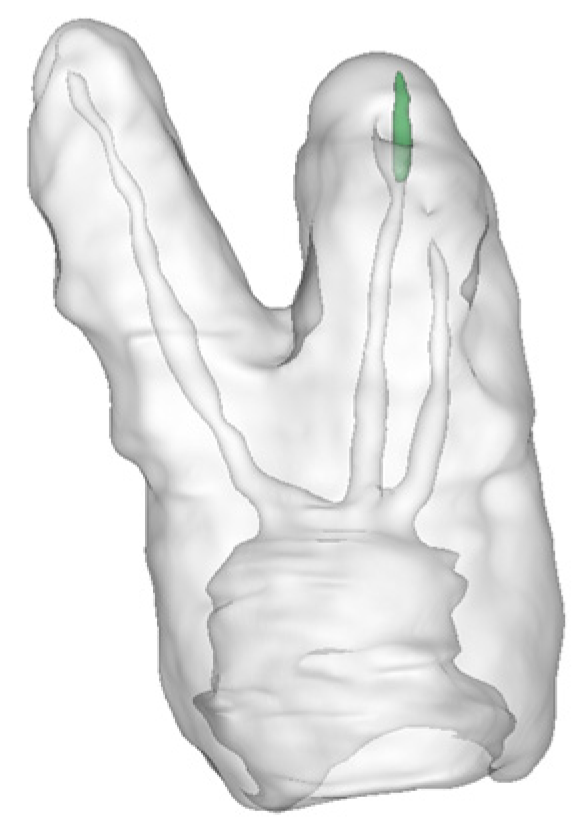
Figure 10.
The 3D hologram of tooth 16, is subjected to endodontic treatment due to periodic pain.
Figure 10.
The 3D hologram of tooth 16, is subjected to endodontic treatment due to periodic pain.
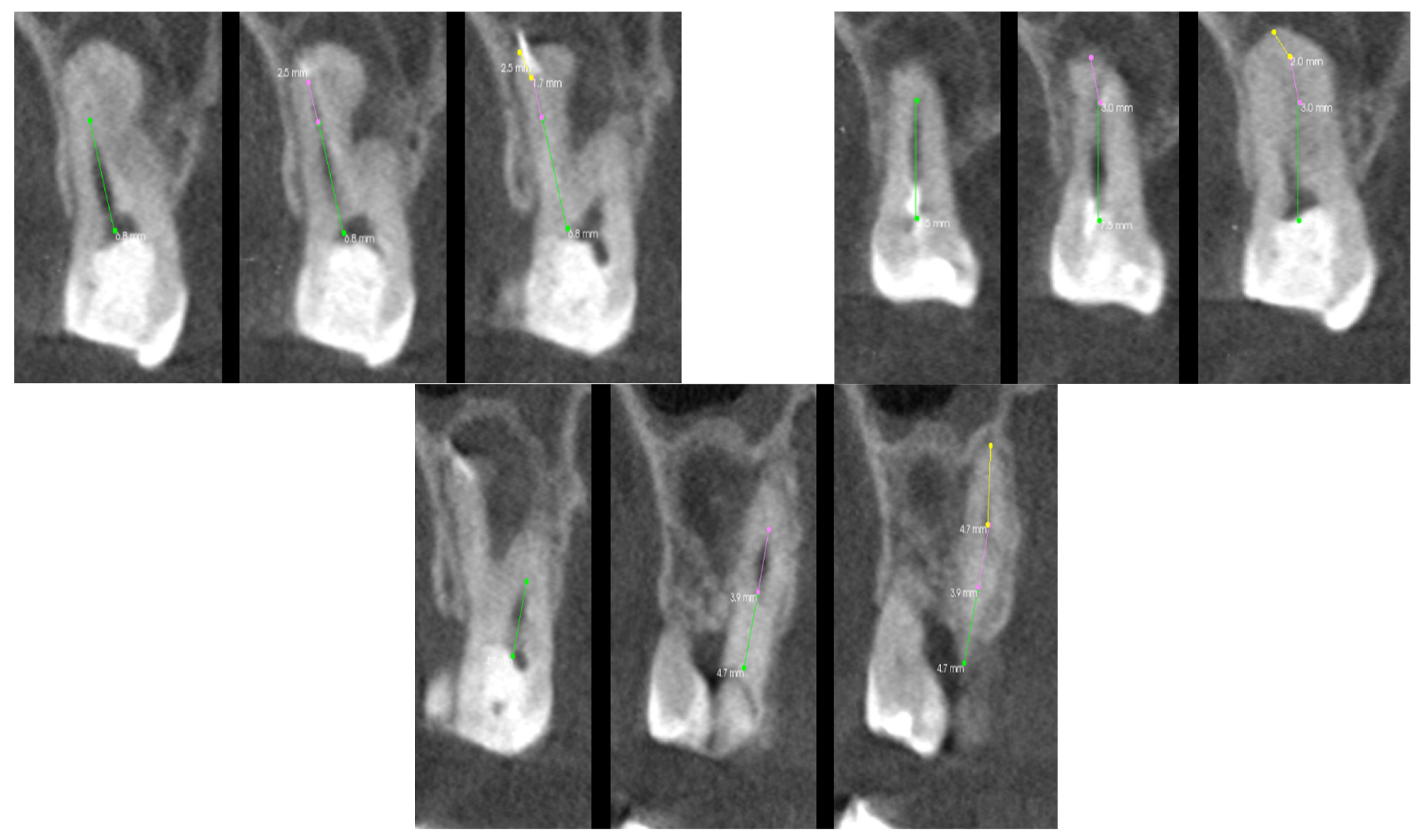
Figure 11.
The CT scan of the tooth was used for the analysis of the root canals in the transverse plane, in the case of tooth 15.
Figure 11.
The CT scan of the tooth was used for the analysis of the root canals in the transverse plane, in the case of tooth 15.
Figure 12.
The 3D hologram of tooth 15, subjected to endodontic treatment.
Figure 12.
The 3D hologram of tooth 15, subjected to endodontic treatment.
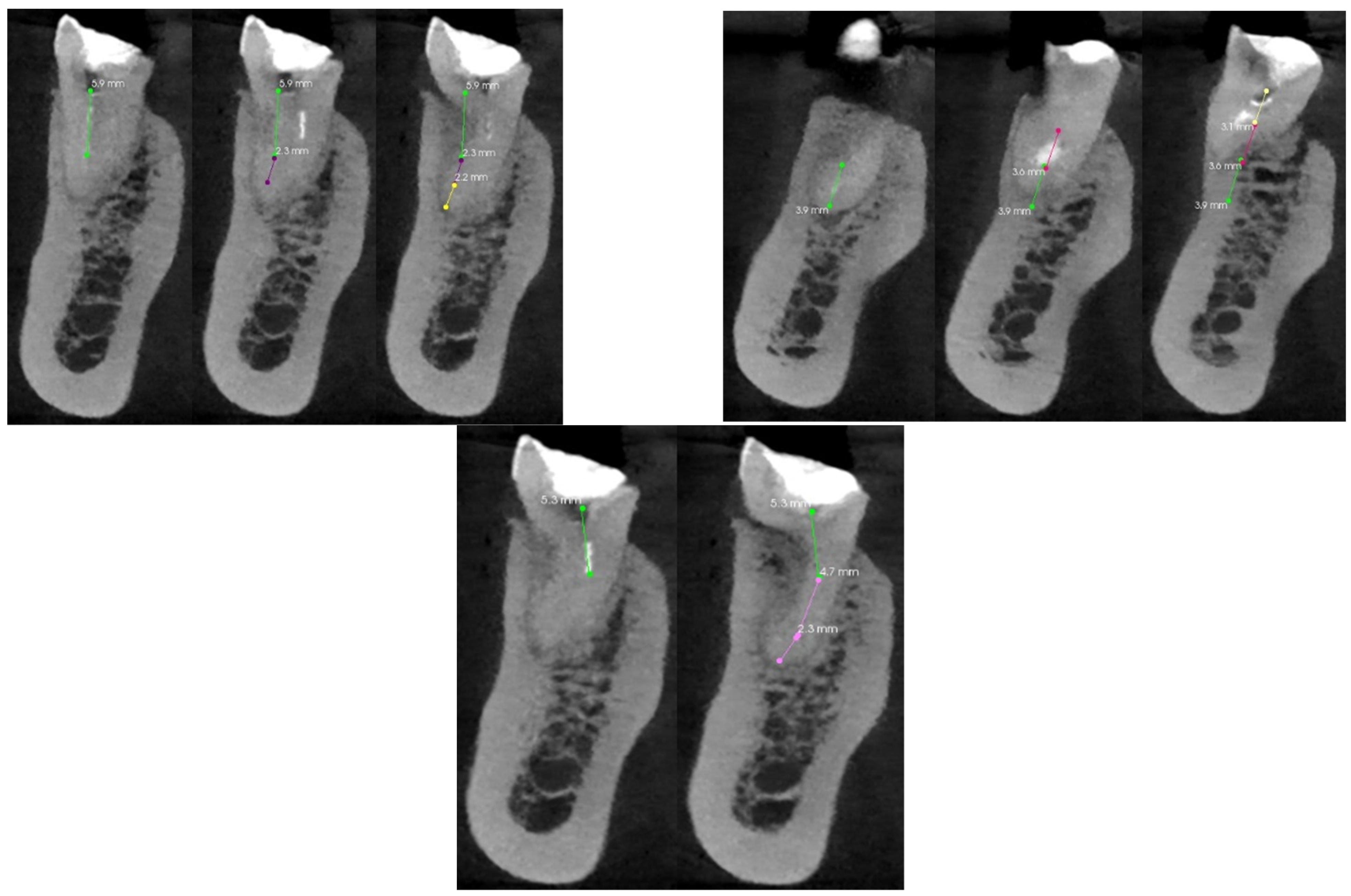
Figure 13.
The CT scan of the tooth was used for the analysis of the root canals in the transverse plane, in the case of tooth 11.
Figure 13.
The CT scan of the tooth was used for the analysis of the root canals in the transverse plane, in the case of tooth 11.
Figure 14.
The 3D hologram of tooth 11, subjected to endodontic treatment.
Figure 14.
The 3D hologram of tooth 11, subjected to endodontic treatment.
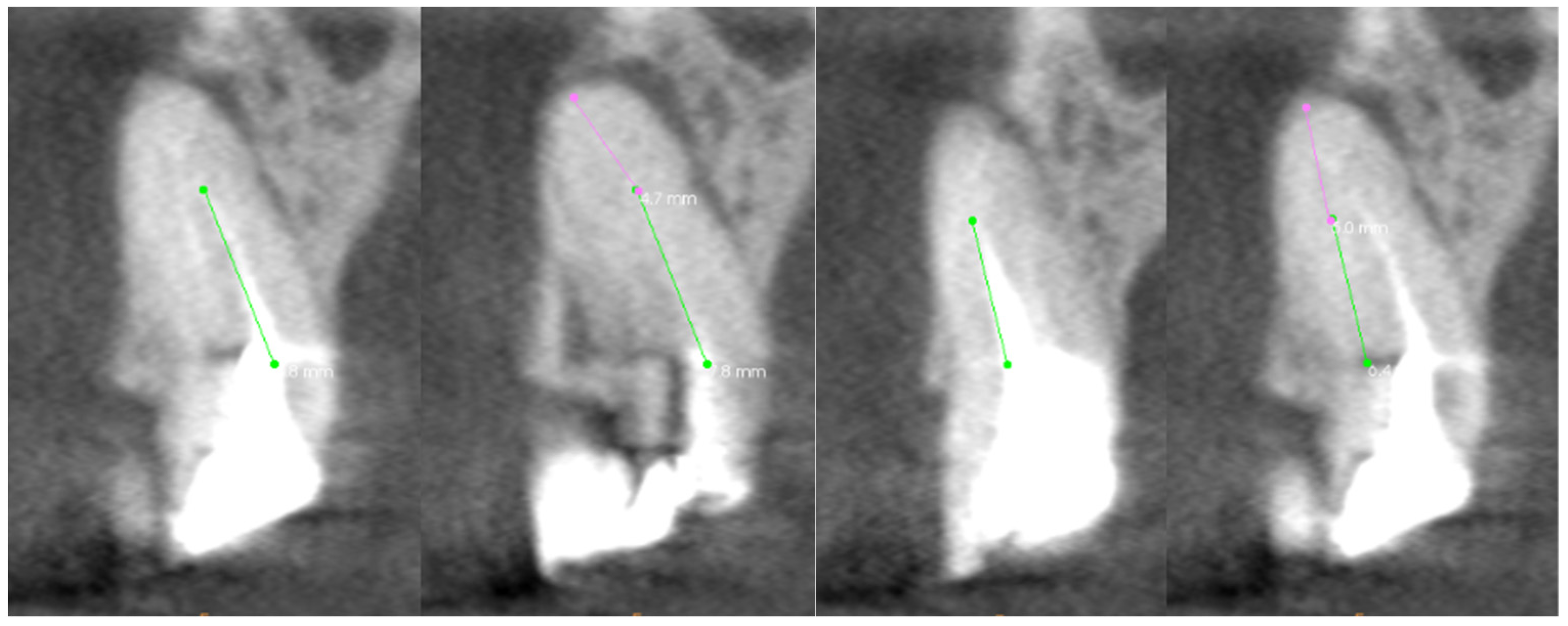
Figure 15.
The CT scan of the tooth was used for the analysis of the root canals in the transverse plane, in the case of tooth 46.
Figure 15.
The CT scan of the tooth was used for the analysis of the root canals in the transverse plane, in the case of tooth 46.
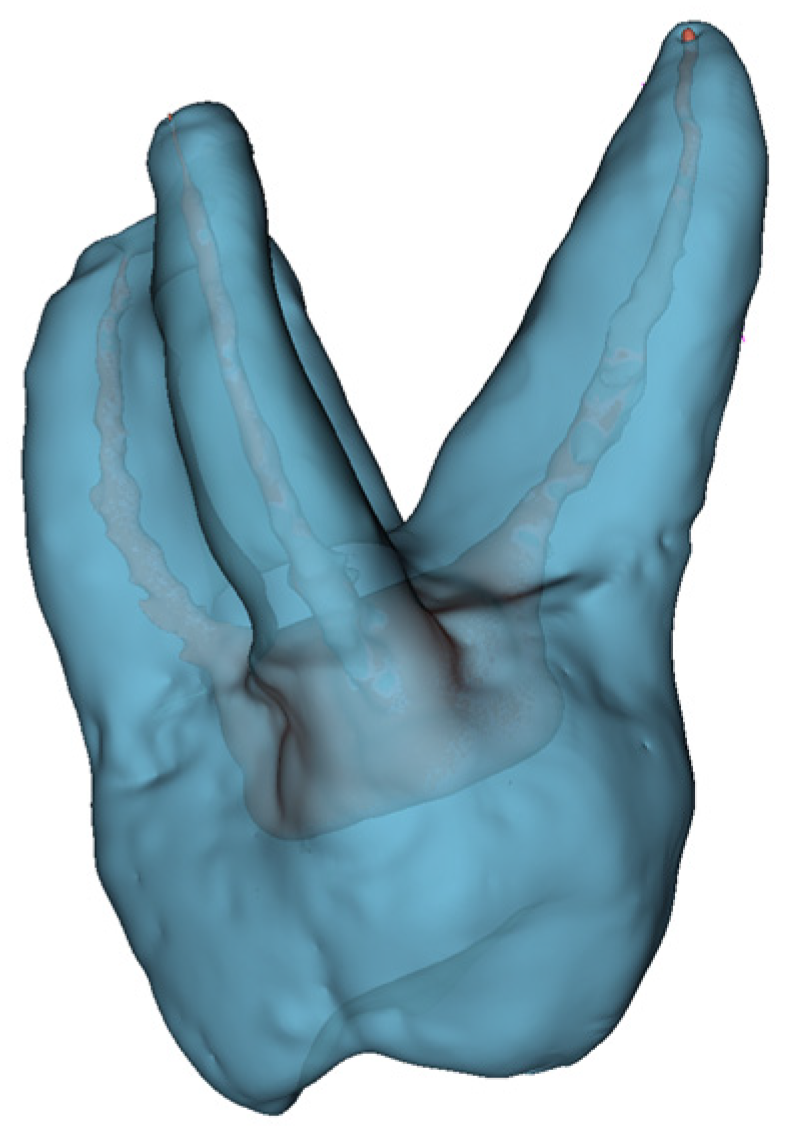
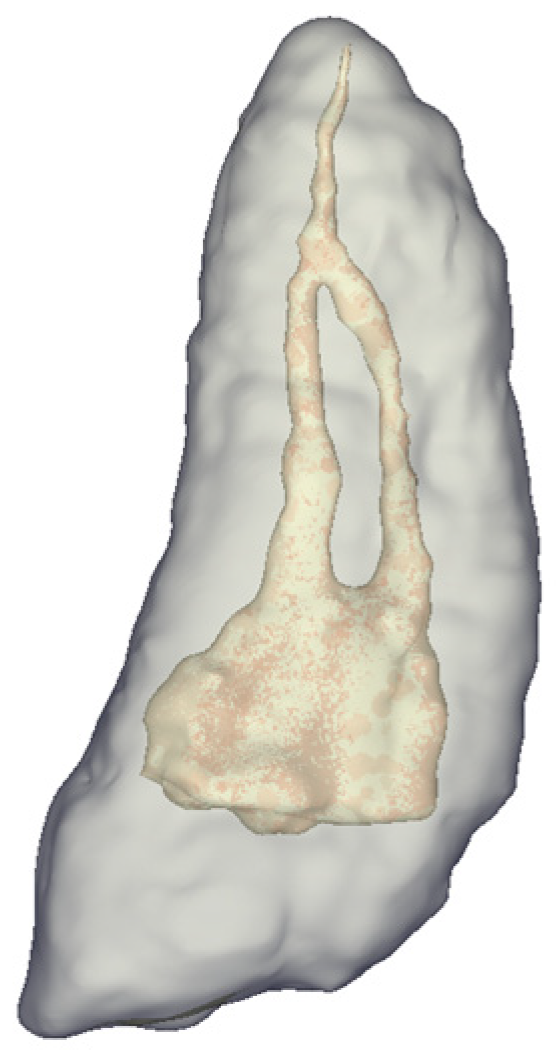
Figure 16.
The 3D hologram of tooth 46, subjected to endodontic treatment.
Figure 16.
The 3D hologram of tooth 46, subjected to endodontic treatment.
Table 1.
Parameters of the patient’s tooth condition are assessed based on cone beam computed tomography.
Table 1.
Parameters of the patient’s tooth condition are assessed based on cone beam computed tomography.
| Axial Plane | Transverse Plane | Longitudinal Plane |
|---|
| Location of the root canal orifices at the bottom of the tooth chamber | The curvature of the root canal in the buccal-lingual/buccal-palatal dimension | The curvature of the root canal in the mesial-distal dimension |
| Axial and Transverse Planes |
| Connection of two canals, e.g., MB1 and MB2, or buccal and lingual lower molars |
| Transverse and Longitudinal Planes |
| Location of the perforation concerning the length of the root canal |
| Distance of the broken file from the root tip |
| Axial, Transverse, and Longitudinal Planes |
| Uniformity of the filling material |
| The presence of a broken file |
| The presence of perforations |
| The presence of obliteration and calcification |
Table 2.
The minimum number of scans for each root canal needed to analyze its entire course and the percentage of the length of the canal visible on the scan, in the case of tooth 17 with carious pulp exposure.
Table 2.
The minimum number of scans for each root canal needed to analyze its entire course and the percentage of the length of the canal visible on the scan, in the case of tooth 17 with carious pulp exposure.
| Type of Root Canal | The Number of Shots Needed to Visualize/Evaluate the Entire Root Canal [pcs.] | Length Visibility of r Per Picture [%] |
|---|
| Canal mesial buccal | 3 | 67.00; 21.00; 12.00 |
| Canal distal buccal | 2 | 79.00; 21.00 |
| Canal mesial palatal | 2 | 78.00; 22.00 |
| Canal distal palatal | 5 | 40.00; 13.00; 9.00; 19.00; 19.00 |
Table 3.
The minimum number of scans for each root canal is needed to analyze its entire course and the percentage of the length of the canal visible on the scan, in the case of the treatment of tooth 16 due to periodic pain.
Table 3.
The minimum number of scans for each root canal is needed to analyze its entire course and the percentage of the length of the canal visible on the scan, in the case of the treatment of tooth 16 due to periodic pain.
| Type of Root Canal | The Number of Shots Needed to Visualize/Evaluate the Entire Root Canal [pcs.] | Length Visibility of r per Picture [%] |
|---|
| Canal mesial buccal | 3 | 60.00; 24.00; 16.00 |
| Canal distal buccal | 3 | 62.00; 23.00; 15.00 |
| Canal palatal | 3 | 35.00; 30.00; 35.00 |
Table 4.
The minimum number of scans for each root canal is needed to analyze its entire course and the percentage of the length of the canal visible on the scan, in the case of the treatment of tooth 15.
Table 4.
The minimum number of scans for each root canal is needed to analyze its entire course and the percentage of the length of the canal visible on the scan, in the case of the treatment of tooth 15.
| Type of Root Canal | The Number of Shots Needed to Visualize/Evaluate the Entire Root Canal [pcs.] | Length Visibility of r per Picture [%] |
|---|
| Canal buccal | 2 | 56.00; 44.00 |
| Canal palatal | 2 | 62.00; 38.00 |
Table 5.
The minimum number of scans for each root canal is needed to analyze its entire course and the percentage of the length of the canal visible on the scan, in the case of the treatment of tooth 11.
Table 5.
The minimum number of scans for each root canal is needed to analyze its entire course and the percentage of the length of the canal visible on the scan, in the case of the treatment of tooth 11.
| Type of Root Canal | The Number of Shots Needed to Visualize/Evaluate the Entire Root Canal [pcs.] | Length Visibility of r per Picture [%] |
|---|
| Canal | 2 | 88.00; 12.00 |
Table 6.
The minimum number of scans for each root canal is needed to analyze its entire course and the percentage of the length of the canal visible on the scan, in the case of the treatment of tooth 11.
Table 6.
The minimum number of scans for each root canal is needed to analyze its entire course and the percentage of the length of the canal visible on the scan, in the case of the treatment of tooth 11.
| Type of Root Canal | The Number of Shots Needed to Visualize/Evaluate the Entire Root Canal [pcs.] | Length Visibility of r per Picture [%] |
|---|
| Canal mesial buccal | 3 | 57.00, 22.00, 21.00 |
| Canal mesial lingual | 2 | 43.00, 57.00 |
| Canal distal | 3 | 37.00, 34.00, 29.00 |
Table 7.
The comparison of the MR application with the traditional methods in root canal treatments.
Table 7.
The comparison of the MR application with the traditional methods in root canal treatments.
| Tooth Number | CBCT Analysis Time | Time to Analyze 3D Models | Time Saved When Using MR Compared to Traditional Methods [%] |
|---|
| 17 | 5 min 50 s | 3 min 28s | 40.57 |
| 16 | 4 min 13 s | 2 min 15 s | 46.46 |
| 15 | 3 min 40 s | 1 min 10 s | 54.83 |
| 11 | 2 min 35 s | 43 s | 72.25 |
| 46 | 4 min 55 s | 2 min 38 s | 46.44 |