Abstract
The aim of this retrospective single-cohort study was to evaluate the clinical outcome of four-to-five implants immediately restored with metal-resin screw-retained cross-arch fixed prostheses in edentulous jaws 10 years after loading. One-hundred-and-four consecutive patients received four to five implants placed with a torque superior 35 Ncm. One-hundred-and-twenty-seven metal-resin screw-retained fixed prostheses (59 mandibular and 68 maxillary) were to be delivered within 3 days. Outcome measures, evaluated by the treating clinician, were: prosthesis and implant failures, prosthetic modifications, peri-implant mucositis, and biological and prosthetic complications. A total of 549 implants were placed. Twenty-one implants failed in 14 patients and 102 prostheses were remade, at least once, in 81 patients: 2 due to implant failures and 33 because of fractures of the prostheses. In particular, 25 original metal-resin prostheses had to be remade because of fractures versus only eight of the replacement monolithic metal-resin prostheses. All patients were wearing fixed prostheses at the end of the follow-up. Thirty-six biological complications occurred in 22 patients. Eighty-six prosthetic complications occurred in 42 patients. In conclusion, immediately loaded cross-arch prostheses supported by four-to-five immediately placed implants are a viable therapeutic option if robust prostheses are made.
1. Introduction
Four implants are often placed to support fixed cross-arch prosthesis [1,2]. While it may be difficult to place more than four implants between the mental foramina without risking compromise to oral hygiene procedures, more implants can be placed distal to the mental foramina if there is sufficient bone height above the mandibular canal. In the upper jaw, the number of implants to be inserted may be limited by large pneumatized maxillary sinuses and by reduced bone volumes [3,4]. The reduction of tissue volumes, hard and soft, can be treated with regenerative techniques [5,6,7,8]. In addition implants can also be placed in a tilted position so that a more distal emergence of the implant neck can reduce the length of the prosthetic cantilevers [9]. The length of the prosthetic cantilever may be a problem because of the consequences it might create. The presence of an extended cantilever generates increased stress and excessive force relief on the implants involved. A retrospective study conducted by Tirone et al., classified fractures according to fracture location in cases of full-arch rehabilitation [10]. This study showed that there was a statistically significant relationship between cantilever extension and two types of fractures considered, fractures that occurred between but not involving the two most posterior screw-access openings (that are more prevalent) and fractures of the distal cantilever. A comparative study by Ozan et al., evaluates the relationship between cantilever length and implant inclination, concluding that a reduction in force relief on the involved structures and stress on the peri-implant bone can be obtained by reducing cantilever length by tilting the posterior implant [11].
The more implants inserted, the higher the costs for the patient. In addition, a greater number of implants also means more precision in the fabrication of the prosthetic structure that will be passively fitted to finalize the work. Bhering et al. conducted a comparative study between all-on-four and all-on-six treatment concepts [12]. After a distribution of the sample by the material used and the treatment performed, they concluded that all-on-six approach, when it is possible to execute, and stiffer framework materials had the most favorable biomechanical behavior.
In addition, implants can be loaded immediately after their placement without significantly increasing the risk for failures [13], especially in fully edentulous mandibles [14,15,16], but also in fully edentulous maxillae [17,18].
Edentulous patients would like to have a functional fixed prosthesis without delay, after a minimal surgical intervention and at a reduced biological and financial cost, providing that failure risks are not excessively increased [19]. Therefore, it would be interesting to know whether it could be possible to rehabilitate fully edentulous patients with fixed cross-arch prostheses supported by four-to-five immediately loaded implants. A previous publication of the same patient material presented the 1-year data [18].
The aim of the present retrospective single cohort study was to evaluate the clinical outcomes of immediately loaded maxillary and/or mandibular cross-arch metal-resin screw-retained fixed prostheses on four-to-five immediately placed dental implants without bone augmentation in totally edentulous maxillary and/or mandibular jaws with a 7-year follow-up.
2. Materials and Methods
This study was conducted as a retrospective single-cohort study, in compliance with the ethical standards of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Federico II University of Naples (5 March 2018; No 347/18).
2.1. Study Design
Data from consecutively edentulous subjects, compliant with eligibility criteria reported in Table 1, and rehabilitated with immediately loaded mandibular, or maxillary, or both cross-arch implant-supported prostheses, were retrospectively collected.

Table 1.
Inclusion and exclusion criteria.
The present article is reported according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines (www.strobe-statement.org, accessed on 1 May 2022) and presents the 7-year after-loading data.
2.2. Study Sample
Subjects included in the study were treated between January 2014 and December 2015 in a private dental practice in Sala Consilina, Salerno, Italy.
Subjects were categorized according to what they declared about smoking habits: non-smokers, moderate smokers (up to 10 cigarettes per day), heavy smokers (more than 10 cigarettes per day), and were also classified according to the type of dentition in the opposite jaw (natural/fixed or full dentures).
2.3. Surgical Protocol
All treatments were performed by the same expert operator. Dental and medical history was obtained and clinical examinations and panoramic radiographs were performed on all patients.
Depending on the anatomical conditions, preliminary screening was performed on panoramic radiographs, with patients wearing thermoplastic radiographic guides with small gutta-percha balls as landmarks. When needed, for three-dimensional evaluation of bone volumes, cone beam computed tomography (CBCT) scans were taken still using the thermoplastic radiographic guide [20,21]. Such guides were also used during surgery to facilitate the ideal implant positioning.
Healthy periodontal conditions’ stability and periodontal risk factors’ control were achieved in all partially edentulous subjects. All patients received professional oral hygiene prior to the implant surgery and prophylactic antibiotic therapy with 2 g of amoxicillin plus clavulanic acid orally one hour prior to the intervention [22]. Patients allergic to penicillin were given 500 mg of clarithromycin 1 h prior to the surgery. Patients rinsed with a chlorhexidine mouthwash 0.2% for 1 min just prior to the intervention [23]. Local anesthesia was administered using mepivacaine with adrenaline 1:100,000 or 1:50,000.
Crestal incisions were made and, in the presence of large bone volumes at implant sites, minimal flaps were elevated up to the coronal portion of the alveolar process. In the presence of reduced bone volumes, larger flaps were elevated, exposing the mental foramina in mandibles or the prominence of the maxillary sinuses.
When present, residual teeth/roots were carefully extracted to minimize damage to the buccal plate, and sites were thoroughly cleaned from all granulation tissue. SPI-Contact (Thommen Medical; Grenchen, Switzerland) conical–cylindrical implants with a smooth 1.5 mm long collar, 11 mm in length, and 4.5 mm in diameter were inserted. Implants were placed following the protocol suggested by the manufacturer, except for the use of a 4.0 mm profile drill in order to underprepare the sites thus achieving a higher insertion torque. However, in a small number of patients (10%) Anyone (MegaGen Implant, Gyeongbuk, South Korea) implant 4 × 11.5 mm were placed. In case of anatomic limitation, distal implants were distally tilted in the premolar areas (Figure 1) [24].
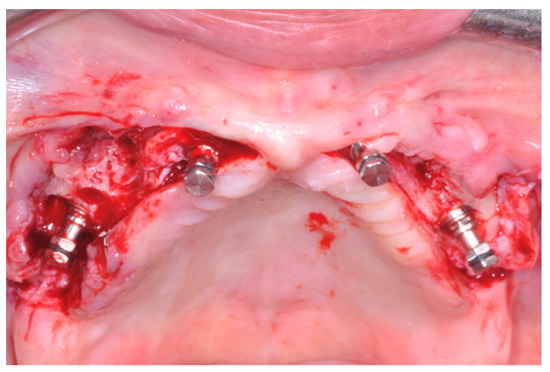
Figure 1.
Four implants were placed, the distal ones being distally tilted.
Implants were placed with the 1.5 mm polished neck in a supracrestal position, also in the case of post-extractive implants. They were inserted with a torque of 70 Newton/cm and, once the motor stopped, implant stability was confirmed manually using the SPI-MONO torque ratchet (Thommen, Grenchen, Switzerland). If one of the four implants could not be placed with a minimum torque of 35 Ncm, a fifth implant was added near to the implant which did not achieve the required torque [25]. If two or more implants could not achieve a torque above 35 Ncm, implants were submerged and loaded conventionally after 3 months [26].
To decrease possible interference with the peri-implant bone, a manual bone profiler was used and healing abutments were placed. To maximize the primary wound closure, a platelet rich fibrine membrane (PRF) was placed to cover the site. PRF has also been shown to be successful in promoting hard and soft tissue healing even in oro-maxillofacial surgery [27]. Subsequently, healing abutments were positioned and single resorbable sutures (Vicryl 4-0 SH1 plus 22 mm 1/2c; Ethicon, New Brunswick, NJ, USA) were placed.
After surgery, analgesics (ibuprofen 600 mg) were suggested to be taken twice a day during meals on patient demand. A soft diet was recommended for 45 days. Oral hygiene procedures were professionally implemented during the days following surgery. Patients were instructed to avoid brushing at the surgical site and rinsing until suture removal, about 10 days after surgery. They were trained to clean the prostheses with a gauze moistened with 0.2% chlorhexidine, then to use a soft and then medium toothbrush and finally the waterjet.
2.4. Prosthetic Protocol
Prosthetic procedures were initiated immediately after implant placement. Patients were trained to clean the prostheses with a gauze moistened with 0.2% chlorhexidine, then to use a soft and then medium toothbrush and finally the waterjet.
Individual trays were used to take impressions and were perforated to allow their seating over the transfers. Impregum F (Espe Dental AG, Seefeld, Germany) was used as the impression material. Definitive screw-retained prostheses were made by placing titanium abutments (VARIOtemp for fixed prostheses, Thommen) on the model, which were connected using titanium rods 2 mm in diameter soldered with an argon syncrystallization device (WELDER INTRAORAL MIDI, Implamed, Cremona, Italy), an intraoral welder, to create a rigid framework. It was not necessary to use angulated abutments for tilted implants since the abutments tolerated substantial disparallelism between implants. The framework was covered with wax and 12 preformed resin teeth were added. The second day, the framework was tried in patient’s mouth to check aesthetic, function, and phonetic. It was then finalized with a lining in acrylic resin. Cantilevers including maximum one premolar and one molar in extension per side were allowed. Cantilever length did not exceed 1.5 cm. On the third day after surgery, prostheses were screwed onto the implants using a standard torque of 25 Ncm and the screw households were sealed with gutta-percha. A panoramic radiograph was taken to check proper abutment seating on the implants. Prostheses were designed to have a group function occlusal scheme and were adjusted to have homogeneous occlusal contacts also on cantilevers, when present. Sutures were removed after approximately 10 days by cutting the knot and leaving the remaining portion of the absorbable suture inside the soft tissues to be spontaneously resorbed. Oral hygiene instructions were delivered.
2.5. Follow-Up
Patients were seen again after 1 and 3 months. Primary implant stability was measured at the time of implant placement by insertion torque. At the 3-month follow-up, the prostheses were rebased and implant stability was simultaneously checked, swinging the implant with the handles of two instruments.
Six months after the surgery, patients were recalled for maintenance therapy and occlusion was checked when screw-retained prostheses were removed to be cleaned (Figure 2). Subsequent maintenance follow-ups depended on the patient’s degree of hygiene, verified in the sixth month.

Figure 2.
Patient smile at 1 year after loading.
In case of framework fracture, or to prevent them, the original metal-resin prostheses were gradually replaced by newly made screw-retained monobloc white resin (top.lign professional, Bredent, Senden, Germany) prostheses using a reinforced titanium framework, characterized externally by layers of enamel resin of various shades of pink and white colors (monolithic resin metal reinforced prostheses; Figure 3).
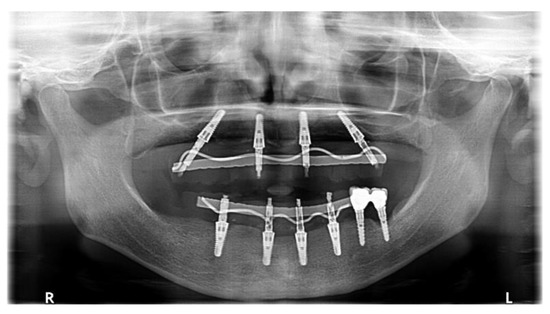
Figure 3.
Panoramic view at 7-year after loading. Both protheses were replaced by monolithic ones in the prosthesis recall program.
2.6. Clinical and/or Radiographic Outcome Measures
The following outcome measures, assessed by the same single expert operator, were retrospectively evaluated:
- Prosthesis failure: a fixed prosthesis lost due to implant failure(s), or requiring to be replaced for any reason [28];
- Implant failure;
- Any prosthetic modification after delivery (soft tissue decubitus, occlusion adjustment, early phonetic problems, prosthetic relining, prosthetic screw replacement, vestibular-lingual prosthetic flange reduction) [29];
- Any other prosthetic complications, also comprising fracture of the abutment screw, framework, detachment of resin teeth, etc.;
- Peri-implant mucositis;
- Peri-implantitis [30];
- Any other biological, also including peri-implant mucosa hemorrhage, soft tissue hypertrophy/hyperplasia, recession, and dehiscence, fistulas, and numbness of the lower lip and chin etc., [29,30].
Periodontal indexes were not collected due to the potential inaccuracy in periodontal probing around dental implants without full-arch protheses removal [31].
2.7. Statistical Analysis
Frequencies and percentages for categorical data were computed. A chi-square test was used to assess the association between smoke and implant failure. An independent samples t-test was used to compare the mean ages of the subjects with failure versus success. A standard statistical software package (SPSS, version 28.0; SPSS IBM, Armonk, NY, USA) was used. The level of significance was set at p < 0.05.
3. Results
One-hundred-and-four patients were recruited and treated from January 2014 to December 2015. One-hundred-twenty-seven metal-resin screw-retained fixed prostheses (59 mandibular and 68 maxillary) were delivered on 549 implants (195 were post-extractive implants). The follow-up focused on the time between implant placement and 7 years after implant loading. The main baseline patient, site, and treatment characteristics are presented in Table 2.

Table 2.
Patients and interventions characteristics (104 patients).
At the time of placement, 30 implants in 22 patients did not achieve the minimal insertion torque required (above 35 Ncm). Twelve maxillary prostheses were conventionally loaded, because at least two implants could not be placed with a torque superior to 35 Ncm.
Twenty-one implants failed in 14 patients (Table 3). Two patients experienced early failures about one month after implant placement, most likely due to infection as they experienced severe pain. One patient lost three mandibular implants in position 3.5, 4.2, 4.5 (implant position replacing the missing tooth in its natural location, indicated according to the numbering of the dental formula) and another two maxillary implants in position 1.6 and 1.2. The latter also lost, 2 months later, the implant in position 2.3. The remaining six patients lost one implant each (5 maxillary and one mandibular implants) and these failures were discovered 3 months after loading during relining of the prostheses. After the first year, seven patients lost eight implants, two due to facture and six due to peri-implantitis. Eight of the early failed implants in five patients were post-extractive. One of the patients presenting with implant failure was bruxist and celiac. Patients with celiac disease have increased enamel wear due to these parafunctional activities; these could also increase the masticatory load, which causes prosthetic fractures as well [32].

Table 3.
Description of the implant failures that occurred up to 7-year post-loading.
There was no association between smoke and implant failure (Χ2 = 0.81; p = 0.66) and there were no statistically significant differences in patients’ mean age between implant failure (62.2 y) and implant success (61.1 y) (p = 0.32).
One-hundred-two prostheses were remade, at least once, in 81 patients.
Two prostheses were remade because of implant failures in two patients. One was actually remade twice, the first time after implant failures and the second time in the frame of the recall program for prosthesis replacement.
Twenty-five original protheses in 23 patients were not remade and were still in function.
All prostheses were in function at the time of writing this manuscript. Any prosthetic modification after loading is reported in Table 4.

Table 4.
Description of normal prosthetic modifications up to seventh year in function.
Peri-implant mucositis due to plaque accumulation occurred in 35 patients (Table 5). They were solved with professional cleaning and chlorhexidine.

Table 5.
Description of peri-implant mucositis episodes.
Thirty-three prostheses in 30 patients were remade because of prosthesis fractures (details on the number of fractures are described in Table 6). One prosthesis was remade twice. In particular, 25 original metal-resin prostheses had to be remade versus only eight monolithic prostheses. Seventy-six prostheses were remade in the recall program for prosthesis replacement. Of these remade prostheses, 17 were remade a second time, 7 because of fractures beyond repair and 10 for various reasons.

Table 6.
Description of biological complications occurred up to seventh year in function.
Complications (Table 6 and Table 7): 36 biological complications occurred in 22 patients (Table 6), pain in relation to implant failures (7 patients). The failed implants were removed and replaced with other implants. Peri-implantitis affected 15 patients and were treated either with surgical or non-surgical debridement or implant removal.

Table 7.
Description of prosthetic complications occurred up to seventh year in function.
The following 86 prosthetic complications occurred in 42 patients (Table 7): sixty-seven fractures of the prostheses occurred in 30 patients. Prostheses were either repaired in the lab or replaced by a new more robust monolithic prosthesis. Prosthesis lining chipping affected 19 patients. They were easily repaired in the lab.
No statistical significant difference was found in the association between smoking and mucositis (p = 0.672) or peri-implantitis (p = 0.108) (Chi-square test). In addition, no statistical significant difference was found comparing the age averages with mucositis or peri-implantitis (t-test).
4. Discussion
The aim of the present retrospective single cohort study was to assess the clinical outcomes of immediately loaded maxillary and/or mandibular cross-arch metal-resin screw-retained fixed prostheses on four-to-five immediately placed dental implants without bone augmentation in totally edentulous maxillary and/or mandibular jaws with a 7-year follow-up, in order to evaluate whether four-to-five immediately loaded implants supporting fixed cross-arch prostheses could be a reliable treatment option to rehabilitate edentulous patients
The choice to evaluate all clinical outcomes is aimed to analyze the average performance of this type of rehabilitation in a medium-to-long-term follow-up.
The findings of the present study are encouraging since only 14 patients lost in total 21 implants up to 7 years after loading and all patients have their implant-supported fixed prostheses in function. Of the 549 implants inserted, 21 failed and 18 dropped out, showing an implant survival rate at seven years of 96%. More specifically, 3 patients out of 14 lost three implants each, while 1 patient lost 2 implants, and the remaining 10 patients lost 1 implant each.
One-hundred-and-two prostheses were remade, which is a high number. However only 2 prostheses were remade because of implant failures, the other 33 prostheses had to be remade because of mechanical failures of the prostheses themselves. In particular, 25 of the original metal-resin prostheses constructed adding commercially available denture teeth had to be remade versus only 8 of the replacement monolithic metal-resin prostheses. This clearly indicates an insufficient robustness of the original delivered metal-resin prostheses. This type of prosthetic design should be considered as a provisional and not as a definitive prosthesis. Therefore, it was decided to start a free-of-charge recall program to replace the original metal-resin prostheses with a new and more robust design. A similar problem was described in a 5-year post-loading prospective study including 80 patients rehabilitated with immediately loaded screw-retained prostheses supported by only two mandibular implants [33]. Two different types of frameworks were used: titanium laser-welded rods and cast silver-palladium alloy frameworks. Significantly, more mechanical complications occurred at laser-welded prostheses (19 patients out of 46 versus 6 patients out of 34; p = 0.032). In particular, nine laser-welded prostheses versus only one cast prostheses had to be remade.
Only those implants that achieved an insertion torque superior to 35 Ncm were immediately loaded. This appears to be a clinically sound decision. In fact, a randomized controlled split-mouth trial, evaluating the clinical outcome of immediately loaded implants placed with an insertion torque between 25 and 35 Ncm versus implants placed with a torque superior to 80 Ncm, showed statistically scarcer failure using insertion torque above 80 Ncm [34]. In addition, no implant inserted with a torque above 30 Ncm failed either. An insertion torque superior to 80 Ncm is a very high torque and it may be that good results could be obtained also with lower torque values, as suggested by the present study or by another trial in which implants inserted with a torque of 32 Ncm were also loaded immediately [35]. Most likely, an insertion torque superior to 35 Ncm for loading four-to-five splinted implants, as in the present study, is adequate to ensure good success rates of immediately loaded implants.
Most of the early implant failures affected immediate post-extractive implants (8 out of 12). This observation is in line with other studies that showed trends for post-extractive implants to fail more often than delayed-placed implants [13,36]. During the follow-up, two implant fractures occurred, which may indicate an excessive loading on the implant in relation to its robustness.
Complications may seem very frequent when compared with other similar studies. A special effort was made to detect and report all events, also those less commonly. In the majority of studies, complications are under-reported, if not reported at all, which can generate a great bias in implantology. Knowledge of complications may help to solve them.
Compared with the 1-year follow-up publication, it was decided to consider soft tissue decubitus, occlusion adjustments, early phonetic problems prosthetic relining, prosthetic screw replacement, and vestibular-lingual prosthetic flange reduction as normal prosthetic modifications instead of real prosthetic complications. The same consideration was made for peri-implant mucositis, which were solved with professional cleaning and chlorhexidine. This decision was made since, once solved, they rarely recurred during the follow-up period. The real complications were divided into biological complications and prosthetic complications (Table 6 and Table 7).
The decision of replacing the original metal-resin prostheses with the monoblock white resin ones led to a reduction of fracture percentage from 76% to 12%. The more common complications of monoblock prostheses were prosthetic chippings, which were easily repaired in the lab without the necessity of making a new prosthesis.
The major limitation of the present study is the retrospective design. In addition, treatments were delivered under normal clinical conditions, using broad patient inclusion criteria, therefore the results of this could be extrapolated to wider patient populations with similar characteristics. However, the number of patients treated could be further expanded to have a more representative sample and different types of implants could be used.
5. Conclusions
Immediately loaded cross-arch prostheses supported by four-to-five implants are a viable therapeutic option. Monoblock prostheses presented a lower percentage of fractures than non-mono-block metal resin prostheses, making them a better option.
Author Contributions
Conceptualization, G.P. and A.A.; methodology, F.D., M.C. and F.G.; validation, A.A., F.G. and M.C.; investigation, G.P. and F.G.; data curation, F.D. and M.C.; writing—original draft preparation, M.C., A.A. and M.L.; writing—review and editing, G.P., M.L. and M.C.; visualization, M.C.; supervision, G.P. and M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Federico II University of Naples (5 March 2018; No 347/18).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All the data are presented in the article.
Acknowledgments
We are in debt to Marco Esposito for his suggestions on how to write this manuscript and to Stefano Martina for his contribution to improve our statistical analysis.
Conflicts of Interest
Only 1-year follow-up was partially supported by Thommen Medical (Grenchen, Switzerland), the manufacturer of the implants evaluated in this investigation, however data belonged to the authors and by no means did the manufacturer interfere with the conduct of the trial or the publication of the results.
References
- Brånemark, P.I.; Hansson, B.O.; Adell, R.; Breine, U.; Lindström, J.; Hallén, O.; Ohman, A. Osseointegrated Implants in the Treatment of the Edentulous Jaw. Experience from a 10-Year Period. Scand. J. Plast. Reconstr. Surg. Suppl. 1977, 16, 1–132. [Google Scholar] [PubMed]
- Chan, M.H.; Nudell, Y.A. All-on-4 Concept Update. Dent. Clin. N. Am. 2021, 65, 211–227. [Google Scholar] [CrossRef] [PubMed]
- Tavelli, L.; Borgonovo, A.E.; Re, D.; Maiorana, C. Sinus Presurgical Evaluation: A Literature Review and a New Classification Proposal. Minerva Stomatol. 2017, 66, 115–131. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.C.; Kim, S.; Kim, D.H.; Herr, Y.; Chung, J.H.; Shin, S.I. Factors Affecting Maxillary Sinus Pneumatization Following Posterior Maxillary Tooth Extraction. J. Periodontal Implant Sci. 2021, 51, 285–295. [Google Scholar] [CrossRef]
- Urban, I.A.; Monje, A. Guided Bone Regeneration in Alveolar Bone Reconstruction. Oral Maxillofac Surg. Clin. N. Am. 2019, 31, 331–338. [Google Scholar] [CrossRef]
- Lang, N.P.; Hämmerle, C.H.; Brägger, U.; Lehmann, B.; Nyman, S.R. Guided Tissue Regeneration in Jawbone Defects Prior to Implant Placement. Clin Oral Implant. Res. 1994, 5, 92–97. [Google Scholar] [CrossRef]
- Gallucci, G.O.; Benic, G.I.; Eckert, S.E.; Papaspyridakos, P.; Schimmel, M.; Schrott, A.; Weber, H.-P. Consensus Statements and Clinical Recommendations for Implant Loading Protocols. Int. J. Oral Maxillofac. Implant. 2014, 29, 287–290. [Google Scholar] [CrossRef]
- Caggiano, M.; D’Ambrosio, F.; Giordano, F.; Acerra, A.; Sammartino, P.; Iandolo, A. The “Sling” Technique for Horizontal Guided Bone Regeneration: A Retrospective Case Series. Appl. Sci. 2022, 12, 5889. [Google Scholar] [CrossRef]
- Zampelis, A.; Rangert, B.; Heijl, L. Tilting of Splinted Implants for Improved Prosthodontic Support: A Two-Dimensional Finite Element Analysis. J. Prosthet. Dent. 2007, 97, S35–S43. [Google Scholar] [CrossRef]
- Tirone, F.; Salzano, S.; Rolando, E.; Pozzatti, L.; Rodi, D. Framework Fracture of Zirconia Supported Full Arch Implant Rehabilitation: A Retrospective Evaluation of Cantilever Length and Distal Cross-Sectional Connection Area in 140 Patients Over an Up-To-7 Year Follow-Up Period. J. Prosthodont. 2022, 31, 121–129. [Google Scholar] [CrossRef]
- Ozan, O.; Kurtulmus-Yilmaz, S. Biomechanical Comparison of Different Implant Inclinations and Cantilever Lengths in All-on-4 Treatment Concept by Three-Dimensional Finite Element Analysis. Int. J. Oral Maxillofac. Implant. 2018, 33, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Bhering, C.L.B.; Mesquita, M.F.; Kemmoku, D.T.; Noritomi, P.Y.; Consani, R.L.X.; Barão, V.A.R. Comparison between All-on-Four and All-on-Six Treatment Concepts and Framework Material on Stress Distribution in Atrophic Maxilla: A Prototyping Guided 3D-FEA Study. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 69, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Maghaireh, H.; Worthington, H.V. Interventions for Replacing Missing Teeth: Different Times for Loading Dental Implants. Cochrane Database Syst. Rev. 2013, 2013, CD003878. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Abati, S.; Romeo, E.; Vogel, G. Implant-Retained Mandibular Overdentures with Brånemark System MKII Implants: A Prospective Comparative Study between Delayed and Immediate Loading. Int. J. Oral Maxillofac. Implant. 2001, 16, 537–546. [Google Scholar]
- Romeo, E.; Chiapasco, M.; Lazza, A.; Casentini, P.; Ghisolfi, M.; Iorio, M.; Vogel, G. Implant-Retained Mandibular Overdentures with ITI Implants. Clin. Oral Implant. Res. 2002, 13, 495–501. [Google Scholar] [CrossRef]
- Cannizzaro, G.; Leone, M.; Esposito, M. Immediate versus Early Loading of Two Implants Placed with a Flapless Technique Supporting Mandibular Bar-Retained Overdentures: A Single-Blinded, Randomised Controlled Clinical Trial. Eur. J. Oral Implant. 2008, 1, 33–43. [Google Scholar]
- Giordano, F.; Esposito, M. Immediate Loading of Fixed Prostheses in Fully Edentulous Jaws—1-Year Follow-up from a Single-Cohort Retrospective Study. Eur. J. Oral Implant. 2017, 10, 339–348. [Google Scholar]
- Cannizzaro, G.; Leone, M.; Esposito, M. Immediate Functional Loading of Implants Placed with Flapless Surgery in the Edentulous Maxilla: 1-Year Follow-up of a Single Cohort Study. Int. J. Oral Maxillofac. Implant. 2007, 22, 87–95. [Google Scholar]
- Lee, D.J.; Saponaro, P.C. Management of Edentulous Patients. Dent. Clin. N. Am. 2019, 63, 249–261. [Google Scholar] [CrossRef]
- Sbordone, C.; Toti, P.; Brevi, B.; Martuscelli, R.; Sbordone, L.; Di Spirito, F. Computed Tomography-Aided Descriptive Analysis of Maxillary and Mandibular Atrophies. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 99–105. [Google Scholar] [CrossRef]
- Di Spirito, F.; Toti, P.; Brevi, B.; Martuscelli, R.; Sbordone, L.; Sbordone, C. Computed Tomography Evaluation of Jaw a Trophies before and after Surgical Bone Augmentation. Int. J. Clin. Dent. 2019, 12, 259–270. [Google Scholar]
- D’Ambrosio, F.; Di Spirito, F.; Amato, A.; Caggiano, M.; Lo Giudice, R.; Martina, S. Attitudes towards Antibiotic Prescription and Antimicrobial Resistance Awareness among Italian Dentists: What Are the Milestones? Healthcare 2022, 10, 1585. [Google Scholar] [CrossRef] [PubMed]
- Ramaglia, L.; Di Spirito, F.; Sirignano, M.; La Rocca, M.; Esposito, U.; Sbordone, L. A 5-Year Longitudinal Cohort Study on Crown to Implant Ratio Effect on Marginal Bone Level in Single Implants. Clin. Implant Dent. Relat. Res. 2019, 21, 916–922. [Google Scholar] [CrossRef] [PubMed]
- DE Vico, G.; Bonino, M.; Spinelli, D.; Schiavetti, R.; Sannino, G.; Pozzi, A.; Ottria, L. Rationale for Tilted Implants: FEA Considerations and Clinical Reports. Oral Implant. 2011, 4, 23–33. [Google Scholar]
- Greenstein, G.; Cavallaro, J. Implant Insertion Torque: Its Role in Achieving Primary Stability of Restorable Dental Implants. Compend. Contin. Educ. Dent. 2017, 38, 88–95, quiz 96. [Google Scholar] [PubMed]
- Tettamanti, L.; Andrisani, C.; Bassi, M.A.; Vinci, R.; Silvestre-Rangil, J.; Tagliabue, A. Immediate Loading Implants: Review of the Critical Aspects. Oral Implant. 2017, 10, 129–139. [Google Scholar] [CrossRef]
- Cortese, A.; Caggiano, M.; Carlino, F.; Pantaleo, G. Zygomatic Fractures: Technical Modifications for Better Aesthetic and Functional Results in Older Patients. Int. J. Surg. 2016, 33 (Suppl. 1), S9–S15. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Bordin, T.B.; Kim, Y.-J.; El-Rafie, K.; Pagni, S.E.; Natto, Z.S.; Teixeira, E.R.; Chochlidakis, K.; Weber, H.-P. Technical Complications and Prosthesis Survival Rates with Implant-Supported Fixed Complete Dental Prostheses: A Retrospective Study with 1- to 12-Year Follow-Up. J. Prosthodont. 2020, 29, 3–11. [Google Scholar] [CrossRef]
- La Monaca, G.; Pranno, N.; Annibali, S.; Di Carlo, S.; Pompa, G.; Cristalli, M.P. Immediate Flapless Full-Arch Rehabilitation of Edentulous Jaws on 4 or 6 Implants According to the Prosthetic-Driven Planning and Guided Implant Surgery: A Retrospective Study on Clinical and Radiographic Outcomes up to 10 Years of Follow-Up. Clin. Implant. Dent. Relat. Res. 2022, 1–14. [Google Scholar] [CrossRef]
- D’Ambrosio, F.; Caggiano, M.; Schiavo, L.; Savarese, G.; Carpinelli, L.; Amato, A.; Iandolo, A. Chronic Stress and Depression in Periodontitis and Peri-Implantitis: A Narrative Review on Neurobiological, Neurobehavioral and Immune-Microbiome Interplays and Clinical Management Implications. Dent. J. 2022, 18, 10–49. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Barizan Bordin, T.; Kim, Y.-J.; DeFuria, C.; Pagni, S.E.; Chochlidakis, K.; Rolim Teixeira, E.; Weber, H.-P. Implant Survival Rates and Biologic Complications with Implant-Supported Fixed Complete Dental Prostheses: A Retrospective Study with up to 12-Year Follow-Up. Clin. Oral Implant. Res. 2018, 29, 881–893. [Google Scholar] [CrossRef]
- Amato, M.; Zingone, F.; Caggiano, M.; Iovino, P.; Bucci, C.; Ciacci, C. Tooth Wear Is Frequent in Adult Patients with Celiac Disease. Nutrients 2017, 9, 1321. [Google Scholar] [CrossRef] [PubMed]
- Cannizzaro, G.; Felice, P.; Lazzarini, M.; Ferri, V.; Leone, M.; Trullenque-Eriksson, A.; Esposito, M. Immediate Loading of Two Flapless Placed Mandibular Implants Supporting Cross-Arch Fixed Prostheses: A 5-Year Follow-up Prospective Single Cohort Study. Eur. J. Oral Implant. 2016, 9 (Suppl. 1), 165–177. [Google Scholar]
- Cannizzaro, G.; Leone, M.; Ferri, V.; Viola, P.; Gelpi, F.; Federico, G.; Esposito, M. Immediate Loading of Single Implants Inserted Flapless with Medium or High Insertion Torque: A 6-Month Follow-up of a Split-Mouth Randomised Controlled Trial. Eur. J. Oral Implant. 2012, 5, 333–342. [Google Scholar]
- Ottoni, J.M.P.; Oliveira, Z.F.L.; Mansini, R.; Cabral, A.M. Correlation between Placement Torque and Survival of Single-Tooth Implants. Int. J. Oral Maxillofac. Implantol. 2005, 20, 769–776. [Google Scholar]
- Esposito, M.; Barausse, C.; Pistilli, R.; Jacotti, M.; Grandi, G.; Tuco, L.; Felice, P. Immediate Loading of Post-Extractive versus Delayed Placed Single Implants in the Anterior Maxilla: Outcome of a Pragmatic Multicenter Randomised Controlled Trial 1-Year after Loading. Eur. J. Oral Implantol. 2015, 8, 347–358. [Google Scholar] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).