Dental Trauma Epidemiology in Primary Dentition: A Cross-Sectional Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. DT Recorded
3.2. DT Distribution According to Age and Gender
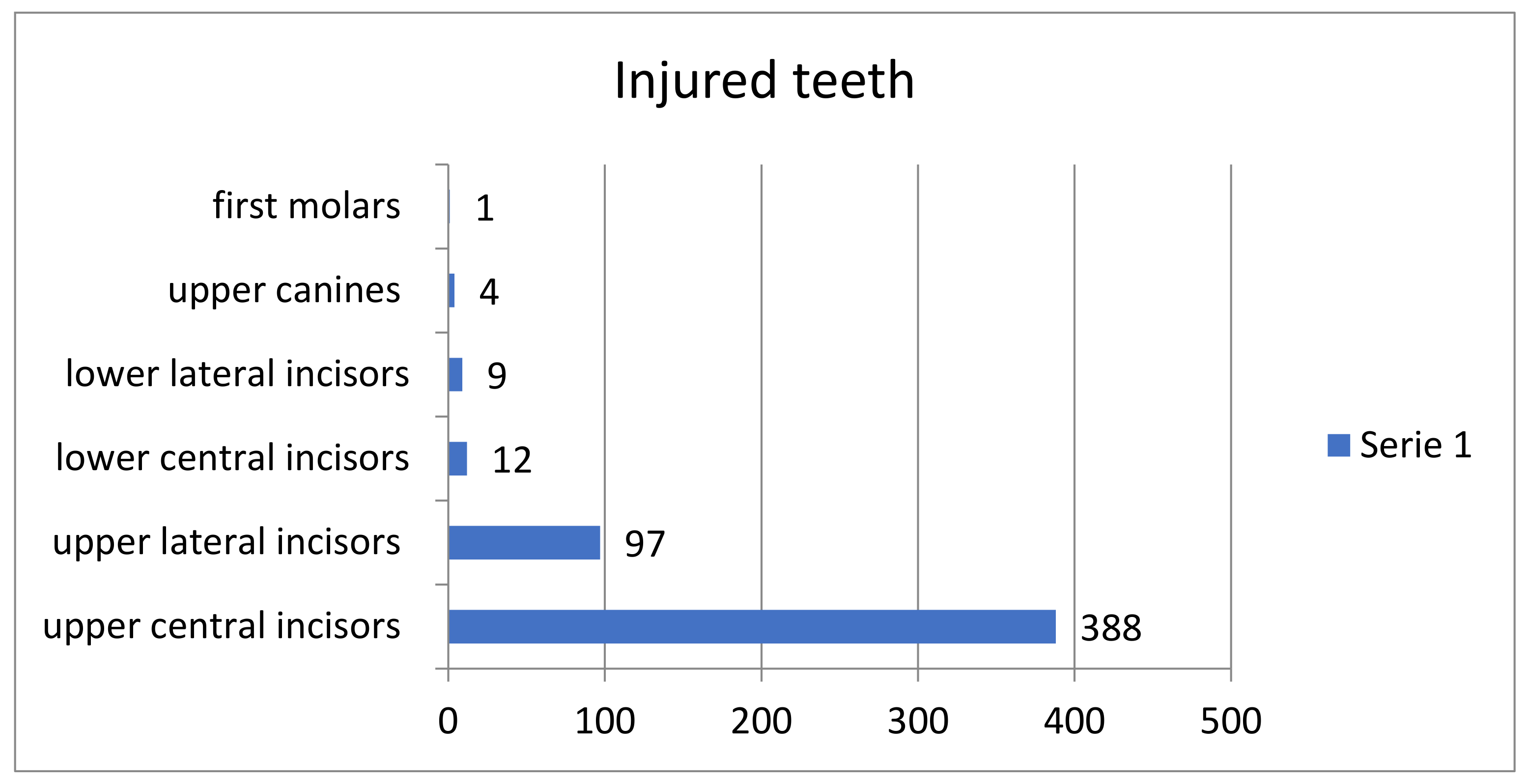
3.3. Injured Teeth
3.4. Type of DT
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sleet, D.A. The global challenge of child injury prevention. Int. J. Environ. Res. Public Health 2018, 15, 1921. [Google Scholar] [CrossRef]
- Petti, S.; Glendor, U.; Andersson, L. World traumatic dental injury prevalence and incidence, a meta-analysis-One billion living people have had traumatic dental injuries. Dent. Traumatol. 2018, 34, 71–86. [Google Scholar] [CrossRef]
- Petersson, E.E.; Andersson, L.; Sorensen, S. Traumatic oral vs non-oral injuries. Swed. Dent. J. 1997, 21, 55–68. [Google Scholar]
- Glendor, U.; Halling, A.; Andersson, L.; Eilert-Petersson, E. Incidence of traumatic tooth injuries in children and adolescents in the county of Vastmanland, Sweden. Swed. Dent. J. 1996, 20, 15–28. [Google Scholar]
- Flores, M.T.; Onetto, J.E. How does orofacial trauma in children affect the developing dentition? Long-term treatment and associated complications. Dent. Traumatol. 2019, 35, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Bagattoni, S.; Carli, E.; Gatto, M.R.; Gasperoni, I.; Piana, G.; Lardani, L. Predisposing factors involved in the aetiology of Molar Incisor Hypomineralization: A case-control study. Eur. J. Paediatr. Dent. 2022, 23, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Kramer, P.F.; Onetto, J.; Flores, M.T.; Borges, T.S.; Feldens, C.A. Traumatic Dental Injuries in the primary dentition: A 15-year bibliometric analysis of Dental Traumatology. Dent. Traumatol. 2016, 32, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O. Etiology and pathogenesis of traumatic dental injuries. A clinical study of 1298 cases. Scand. J. Dent. Res. 1970, 78, 329–342. [Google Scholar] [CrossRef]
- Glendor, U. Epidemiology of traumatic dental injuries—A 12 year review of the literature. Dent. Traumatol. 2008, 24, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Elkarmi, R.F.; Hamdan, M.A.; Rajab, L.D.; Abu-Ghazaleh, S.B.; Sonbol, H.N. Prevalence of traumatic dental injuries and associated factors among preschool children in Amman, Jordan. Dent. Traumatol. 2015, 31, 487–492. [Google Scholar] [CrossRef] [PubMed]
- Bagattoni, S.; Lardani, L.; D’Alessandro, G.; Piana, G. Oral health status of Italian children with Autism Spectrum Disorder. Eur. J. Paediatr. Dent. 2021, 22, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Bagattoni, S.; D’Alessandro, G.; Gatto, M.R.; Piana, G. Self-induced soft-tissue injuries following dental anesthesia in children with and without intellectual disability. A prospective study. Eur. Arch. Paediatr. Dent. 2020, 21, 617–622. [Google Scholar] [CrossRef]
- Patnana, A.K.; Chugh, A.; Chugh, V.K.; Kumar, P.; Vanga, N.R.V.; Singh, S. The prevalence of traumatic dental injuries in primary teeth: A systematic review and meta-analysis. Dent. Traumatol. 2021, 37, 383–399. [Google Scholar] [CrossRef] [PubMed]
- De Amorim, L.F.; da Costa, L.R.; Estrela, C. Retrospective study of traumatic dental injuries in primary teeth in a Brazilian specialized pediatric practice. Dent. Traumatol. 2011, 27, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Wendt, F.P.; Torriani, D.D.; Assunção, M.C.F.; Romano, A.R.; Bonow, M.L.M.; da Costa, C.T.; Goettems, M.L.; Hallal, P.C. Traumatic dental injuries in primary dentition: Epidemiological study among preschool children in South Brazil. Dent. Traumatol. 2010, 26, 168–173. [Google Scholar] [CrossRef]
- Kramer, P.F.; Zembruski, C.; Ferreira, S.H.; Feldens, C.A. Traumatic dental injuries in Brazilian preschool children. Dent. Traumatol. 2003, 19, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Cavalcanti, A.L. Prevalence and characteristics of injuries to the head and orofacial region in physically abused children and adolescents—A retrospective study in a city of the Northeast of Brazil. Dent. Traumatol. 2010, 26, 149–153. [Google Scholar] [CrossRef]
- Lee, L.Y.; Ilan, J.; Mulvey, T. Human biting of children and oral manifestations of abuse: A case report and literature review. J. Dent. Child. 2002, 69, 92–95. [Google Scholar]
- AAPD. Oral and Dental Aspects of Child Abuse and Neglect. Pediatr. Dent. 2018, 40, 243–249. [Google Scholar]
- Bulut, E.; Güçlü, Z.A. Evaluation of primary teeth affected by dental trauma in patients visiting a university clinic, Part 1: Epidemiology. Clin. Oral Investig. 2022, 26, 6783–6794. [Google Scholar] [CrossRef]
- Elbay, M.; Elbay, Ş.; Uğurluel, C.; Kaya, C. Evaluation of the 156 dental traumatic injury cases who applied to pediatric dentistry clinic in a university hospital: Retrospective study. Selcuk. Dent. J. 2016, 3, 48–55. [Google Scholar] [CrossRef]
- Bagattoni, S.; Sadotti, A.; D’Alessandro, G.; Piana, G. Dental trauma in Italian children and adolescents with special health care needs. A cross-sectional retrospective study. Eur. J. Paediatr. Dent. 2017, 18, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Ng, L.; Malandris, M.; Cheung, W.; Rossi-Fedele, G. Traumatic dental injuries presenting to a paediatric emergency department in a tertiary children’s hospital, Adelaide, Australia. Dent. Traumatol. 2020, 36, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Wu, T.T.; Li, J.Y.; Wang, P.X.; Guo, Q.Y. Retrospective study on 696 cases of traumatic dental injuries of primary dentition in Xi’an, China. Eur. J. Paediatr. Dent. 2022, 23, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Day, P.F.; Flores, M.T.; O’Connell, A.C.; Abbott, P.V.; Tsilingaridis, G.; Fouad, A.F.; Cohenca, N.; Lauridsen, E.; Bourguignon, C.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. Dent. Traumatol. 2020, 36, 343–359. [Google Scholar] [CrossRef] [PubMed]
- Malmgren, B.; Andreasen, J.O.; Flores, M.T.; Robertson, A.; Di Angelis, A.J.; Andersson, L.; Cavalleri, G.; Cohenca, N.; Day, P.; Hicks, M.L.; et al. International Association of Dental Traumatology. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. Dent. Traumatol. 2012, 28, 174–182. [Google Scholar] [CrossRef]
- Tewari, N.; Mathur, V.P.; Singh, N.; Singh, S.; Pandey, R.K. Long-term effects of traumatic dental injuries of primary dentition on permanent successors: A retrospective study of 596 teeth. Dent. Traumatol. 2018, 34, 129–134. [Google Scholar] [CrossRef] [PubMed]


| DT Cause | Females n (%) | Males n (%) | p |
|---|---|---|---|
| accidental falls | 84 (55) | 123 (69) | |
| collisions (people) | 53 (34) | 39 (23) | |
| collisions (objects) | 10 (6) | 9 (5) | 0.532 |
| sport-related DT | 3 (2) | 5 (3) | |
| road accidents | 3 (2) | 1 (0.5) | |
| abuse | 1 (1) | 0 (0) |
| DT Setting | Females n (%) | Males n (%) | p |
|---|---|---|---|
| home | 85 (55) | 95 (54) | |
| school | 33 (21) | 44 (25) | 0.8929 |
| playground | 29 (19) | 30 (17) | |
| other | 7 (5) | 8 (4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fitzgibbon, R.; Carli, E.; Piana, G.; Montevecchi, M.; Bagattoni, S. Dental Trauma Epidemiology in Primary Dentition: A Cross-Sectional Retrospective Study. Appl. Sci. 2023, 13, 1878. https://doi.org/10.3390/app13031878
Fitzgibbon R, Carli E, Piana G, Montevecchi M, Bagattoni S. Dental Trauma Epidemiology in Primary Dentition: A Cross-Sectional Retrospective Study. Applied Sciences. 2023; 13(3):1878. https://doi.org/10.3390/app13031878
Chicago/Turabian StyleFitzgibbon, Raquel, Elisabetta Carli, Gabriela Piana, Marco Montevecchi, and Simone Bagattoni. 2023. "Dental Trauma Epidemiology in Primary Dentition: A Cross-Sectional Retrospective Study" Applied Sciences 13, no. 3: 1878. https://doi.org/10.3390/app13031878
APA StyleFitzgibbon, R., Carli, E., Piana, G., Montevecchi, M., & Bagattoni, S. (2023). Dental Trauma Epidemiology in Primary Dentition: A Cross-Sectional Retrospective Study. Applied Sciences, 13(3), 1878. https://doi.org/10.3390/app13031878







