Abstract
Whole-Body Periodic Acceleration (WBPA) has been reported to induce endothelial nitric oxide and cause vasodilation. However, the effects of WBPA on blood pressure and cardiovascular hemodynamics are still unclear and controversial. The objective of this study was to determine whether a single session of 160-degree V-shape Whole-Body Periodic Acceleration (WBPA-V-160), i.e., periodic motion of the supine body headward to footward, improved blood pressure and cardiovascular parameters. A pre-evaluation and post-evaluation of blood pressure and cardiovascular hemodynamics via DynaPulse Noninvasive and Quantitative Hemodynamic Profile Analysis were performed after a single 30 min trial of WBPA-V-160 with a moving distance, headward to footward, of 2 mm, at a constant frequency of 4 Hz. Systolic BP, diastolic BP, heart rate, end systolic pressure, end diastolic pressure, mean arterial BP, and pulse pressure at post-evaluation were significantly lower than at pre-evaluation after WBPA-V-160, whereas systemic vascular compliance and brachial artery distensibility at post-evaluation were significantly higher than at pre-evaluation. The WBPA-V-160, performed for 30 min, did improve blood pressure and cardiovascular hemodynamics by lowing the BP parameters and enhancing systemic vascular compliance.
1. Introduction
Whole-body periodic acceleration (WBPA), or periodic acceleration (pGz), is a method that applies repetitive headward to footward periodic motion to the body in the horizontal position [1]. The periodic motion of WBPA has been reported to induce arterial pulsatile shear stress on the endothelium and to stimulate endothelial nitric oxide release [2]. WBPA is regarded as a noninvasive approach for cardiovascular protection, as shown in animal studies [3], via enhancing antioxidative capacity [4], releasing cardiovascular protective mediators [5], and improving coronary microcirculation [6]. WBPA has been shown to improve flow-mediated vasodilatation and brachial artery endothelial function in 20 healthy volunteers [7] and improve coronary microcirculation in healthy subjects and in patients with coronary artery disease [8] via upregulating endothelial nitric oxide synthase. WBPA increased vasodilatation and reduced the dicrotic notch in healthy adults and adult patients with inflammatory disease, which is similar to the response seen after giving nitric oxide-donor drugs to patients [2].
The effects of WBPA, when in the horizontal supine position, on blood pressure are still controversial, potentially due to the various designs of WBPA devices with different moving distances from headward to footward, and different frequencies. In WBPA design, the key component to induce pulsatile shear stress is the abdominal compartments moving headward to footward to produce intrathoracic pressure gradients for oscillatory periodic acceleration in the horizontal supine position [9]. WBPA manufactured by Non-Invasive Monitoring Systems, Inc. (NIMS) was designed to move headward to footward by about 2.4 cm to generate enough acceleration to stimulate endothelial nitric oxide release, and this WBPA was approved by FDA as medical device [10]. WBPA at a constant frequency of 4 Hz for the oscillatory period produced an inspiratory, inward displacement of the rib cage volume along with an outward displacement of abdominal volume and vice versa during expiration [9]. It is unknown whether a 160-degree V-shape WBPA (WBPA-V-160) could lower blood pressure more easily than WBPA in the horizontal supine position. It is not known whether a WBPA-V-160 in a semi-supine position with a minor moving distance, from headward to footward, of 2 mm can improve cardiovascular hemodynamics or not.
Peripheral and central blood pressure (BP) parameters can be used to predict cardiovascular risks and hypertension for clinical practice [11]. Some studies have reported that WBPA did not change arterial BP and heart rate in animals [9] and in diabetic patients [6], whereas some have reported that 60 min of WBPA lowered BP in piglets [12]. Hemodynamic analysis of the cardiovascular system includes peripheral and central BP parameters (e.g., systolic BP, diastolic BP, and heart rate) and central BP parameters (e.g., end systolic pressure, end diastolic pressure, and pulse pressure). DynaPulse Noninvasive and Quantitative Hemodynamic Profile Analysis can be used to evaluate central BP parameters and cardiovascular hemodynamics [13,14]. The Pulse Dynamic noninvasive method has been validated and the central aortic BP, vascular compliance and waveform can be measured without catheterization [14].
Cardiac output is the product of the stroke volume, which is the volume of blood pumped from the left ventricle per beat, and the heart rate, i.e., the number of heart beats per minute. In an anesthetized model of severe hemorrhagic shock in pigs after 40 mL/kg blood loss, cardiac output, BP, and oxygen delivery were dropped similarly between WBPA (1 h before and during) and non-WBPA conditions, but the regional blood flow was much better preserved in the case of WBPA than in non-WBPA [15]. Neither cardiac output nor stroke volume was reported after WBPA in humans.
Systemic arterial compliance is calculated as the ratio of the stroke volume index to arterial pulse pressure [16]. Systemic vascular resistance, also known as total peripheral resistance, is the amount of force exerted on circulating blood by the vasculature of the body. Systemic vascular resistance is defined as the systemic mean arterial BP minus the right arterial pressure divided by the cardiac output [17]. Neither systemic vascular compliance nor decreased systemic vascular resistance has been reported after WBPA in humans.
Brachial arterial compliance is defined as the ability of a hollow brachial artery to distend and increase in volume with increasing transmural pressure or the tendency of a hollow brachial artery to resist recoiling toward its original dimensions upon application of a distending or compressing force [18]. Arterial distensibility can be defined as the capability of arteries to stretch and is a metric of the stiffness of arteries. Brachial artery distensibility can be a cardiovascular risk marker in asymptomatic individuals [19]. Brachial artery resistance is the resistance that must be overcome to push blood through the brachial artery and create flow. The effects of WBPA on brachial artery compliance, brachial artery distensibility, and brachial artery resistance have not yet been reported in humans.
It is still unknown whether a single session of WBPA-V-160 generates a lower BP than WBPA in the horizontal supine position with the same moving distance, the same acceleration, and the same periodic frequency. It is still not known whether WBPA-V-160 with a minor moving distance, from headward to footward, of 2 mm can improve central BP parameters (e.g., end systolic pressure, end diastolic pressure, mean arterial BP, and pulse pressure), indirect cardiac parameters (e.g., LV ejection time, stroke volume, and cardiac output), systemic vascular (SV) parameters (e.g., SV compliance and SV resistance), or brachial artery (BA) parameters (e.g., BA compliance, BA distensibility, and BA resistance). We hypothesized that WBPA-V-160 can lower BP more easily than WBPA in the horizontal supine position as well as that WBPA-V-160 with a moving distance, from headward to footward, of 2 mm can improve BP and cardiovascular hemodynamics.
2. Materials and Methods
2.1. Study Design
This study included two parts, the first part being a pilot study (n = 10 repeated ×3 trials) to compare the effects of a control, a 160 degree V-shape Whole-Body Periodic Acceleration (WBPA-V-160) versus WBPA in a 180 degree position on BP and exhaled nitric oxide, the second part being a study with a pretest–post-test design (n = 20) to investigate the acute effects of a single session of 30 min of WBPA-V-160 on blood pressure (BP) and cardiovascular parameters.
2.2. Part 1: A Pilot Study
Ten voluntary participants were involved in the pilot study. No subjects with asthma or high inflammatory status were included in the pilot study. A pre-evaluation and post-evaluation of peripheral blood pressure using an Omron HEM-7000 intelligent digital blood pressure monitor (HEM-7000, Omron, Kyoto, Japan) and exhaled nitric oxide using a NIOX portable exhaled nitric oxide analyzer (MINO, Aeorcrine, Solna, Sweden) were performed after either a single 30 min session of control non-Whole-Body Periodic Acceleration (non-WBPA), 180-degree (supine position) WBPA, or 160-degree V-shape WBPA (WBPA-V-160) generated by a brushless motor (Guangdong Nuozhou Health Technology Co., Ltd., Guangdong, China) with a moving distance, from headward to footward, of 6 mm with a frequency 4 Hz on three separate days. The 180-degree (supine position) WBPA and 160-degree WBPA generated the same acceleration in the Z planes and had both 0 G in the X and Y planes. The value of 4 Hz was selected in the 180-degree (supine position) WBPA and 160-degree V-shape WBPA (WBPA-V-160) because the movements of the abdominal compartment in the WBPA-V-160 were largest and their breathing patterns were still comfortable in most participants (Figure 1).
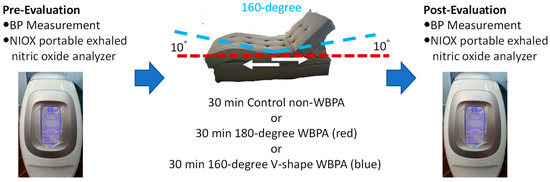
Figure 1.
Flow chart of this pilot study (part 1).
2.3. Participants of Part 2
A total of 20 voluntary participants who did not suffer from motion sickness or motion disability were recruited in this study. All participants were screened using inclusion and exclusion criteria. The inclusion criteria for participants were: (1) over 20 years old and younger than 60 years old; (2) did not suffer from motion sickness or motion disability (i.e., Parkinson’s diseases); (3) agreed to take part in a 10 min pre-evaluation, 30 min of WBPA-V-160, and 10 min post-evaluation; and (4) signed informed consent was received. The exclusion criteria were: (1) a history of motion sickness or motion disability; (2) cardiovascular diseases (e.g., arrhythmias, medicated hypertension, valvular heart disease, coronary artery diseases, peripheral venous diseases, peripheral artery diseases, stroke, cardiac surgery, etc.); (3) diagnosis of any diseases (e.g., neurological diseases, tumor, cancer, etc.); (4) a history of surgery (e.g., brain surgery); and (4) currently using medication (e.g., anti-hypertensive drugs, anti-depressive drugs, anti-diabetic drugs, etc.), alcohol or smoking.
Twenty voluntary participants who did not suffer from motion sickness or motion disability met the inclusion criteria. All the voluntary participants accepted the experimental terms and signed the consent form before pre-evaluation. This study was reviewed by the China Medical University Hospital and conducted according to the Declaration of Helsinki. Informed consent was obtained from all the subjects involved in this study.
2.4. DynaPulse Noninvasive and Quantitative Hemodynamic Profile Analysis of Part 2
DynaPulse Noninvasive and Quantitative Hemodynamic Profile Analysis was used to pre-evaluate BP and cardiovascular hemodynamics [13,14] (Figure 2). The Pulse Dynamic noninvasive method was validated with catheterization at UCSD Medical Center Cath-Lab [14] and showed good agreement for noninvasive cardiovascular hemodynamics comparing to catheterization data. A Pulse Dynamic Noninvasive Blood Pressure Monitor (DynaPulse 200M), which can obtain BP readings and pulse waveforms, then transmitted the gathered information to the DynaPulse Analysis Center (DAC), via the Internet, for the immediate analysis of all Hemodynamic Profiles (Figure 2).
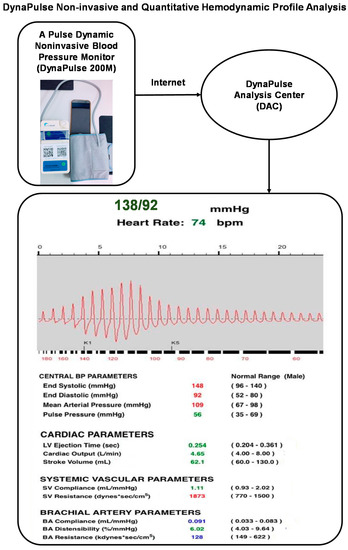
Figure 2.
DynaPulse Noninvasive and Quantitative Hemodynamic Profile Analysis. DAC report: out of normal range with higher cardiovascular risks (red), normal range (green), and out of normal range with lower cardiovascular risks (blue).
2.5. V-Shape 160-Degree Whole-Body Periodic Acceleration (WBPA-V-160) of Part 2
All voluntary participants underwent WBPA-V-160 (Kuang Yu Mental Working Co., Ltd., Changhua, Taiwan) as shown in Figure 3 with a moving distance of 2 mm, 4 ± 0.1 Hz, ±0.8 G in pGz (Figure 3. Intervention part). The dimensions of the WBPA-V-160 was (L) 1755 × (W) 920 × (H) 570 mm; the weight was 49 Kg (Net); the motor characteristic was a brushed motor (DC24V-75W*1. −45 W*1. −25 W*1); the power was 110~220 V 50~60 Hz; the range of vibration frequency was from 3−9 Hz. The bi-directional acceleration from headward to footward horizontally was pGz 0.8 G (X:0 G, Y:0 G, Z: ± 0.8 G), the moving distance from headward to footward was 2 mm and the frequency was set at 4 Hz.
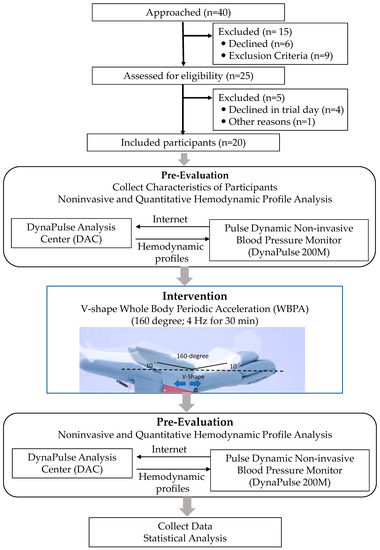
Figure 3.
CONSORT Flow Diagram of part 2.
2.6. Procedure of Part 2
Based on the inclusion criteria and exclusion criteria, this study included 20 voluntary participants. All participants accepted the research terms and signed a consent form before the experiment. Pre-evaluation information, participants’ characteristics (age, body height, body weight, waist circumstance, hip circumstance, body mass index, and waist-hip ratio), and noninvasive and quantitative hemodynamic measurements were collected and taken. The intervention of WBPA-V-160 was performed with a moving distance, from headward to footward, of 2 mm, with 4 ± 0.1 Hz 0–0.8 G periodic motion for 30 min. A post-evaluation, taking noninvasive and quantitative hemodynamic measurements, was performed 5 min after the WBPA-V-160 intervention. The CONSORT flow chart for this study is shown in Figure 3.
2.7. Data Analysis
All the data are presented as mean ± SD. The Shapiro–Wilk test was used to determine the distribution (normal or non-normal) of the data collected. Student’s paired t-test was performed using SPSS Version 20 (IBM Corp) to analyze the pre–post effects. p < 0.05 was considered statistically significant. In part 2, sample size and power calculations were conducted using G*Power software (3.1.0). Based on SBP, a sample of least 19 participants (n = 20 in each group), would allow us to detect pre–post effects, with a power of 80% and analpha level of 0.05 (Supplement 1 in Supplementary Materials).
3. Results
3.1. Part 1: A Pilot Study for Comparing Control, 180-Degree WBPA, and WBPA-V-160
In the pilot study, the SBP and exhaled nitric oxide did not change after Control non-WBPA without turning on the motor (Table 1). Additionally, the SBP and exhaled nitric oxide were not found to be significantly changed after the 180-degree WBPA in ten participants (Table 1). In contrast, the SBP, DBP, and HR were significantly decreased after 30 min of the WBPA-V-160 (4 ± 0.1 Hz) and the exhaled nitric oxide was significantly increased after 30 min of the WBPA-V-160 (Table 1). Because of the same moving distance of 6 mm, the same periodic frequency of 4 Hz, and the same acceleration in the Z planes between the 180-degree (supine position) WBPA and WBPA-V-160, the WBPA-V-160, as compared to the 180-degree WBPA, significantly lowered the SBP, DBP, and HR and increased the exhaled nitric oxide.

Table 1.
Pilot study for comparing control, 180-degree WBPA, and WBPA-V-160.
3.2. Part 2: Body Characteristics of Participants
All twenty participants (thirteen men and seven women) completed the study protocol without any complaints or experiencing adverse effects. The average age of the participants was 45.8 ± 10.8 years old, ranging from 26 to 59. Their average height was 165.1 ± 7.0 cm, ranging from 152 cm to 172 cm. The average body weight and body mass index of all participants were 88.8 ± 14.0 Kg and 25.6 ± 5.2 Kg/m2, respectively (Table 2).

Table 2.
Characteristics of participants.
3.3. Part 2: Pre-BP and Post-BP Parameters after 30 min of WBPA-V-160
The post-systolic BP of all participants (112.6 ± 15.5) was significantly lower than the pre-systolic BP (117.4 ± 15.2 mmHg) (Table 3). The differences and effect size of pre-post parameters are shown in Supplement 2 in Supplementary Materials. The diastolic BP (68.4 ± 9.7 mmHg) at post-evaluation was significantly lower than it was at pre-evaluation (70.9 ± 10.3 mmHg). The heart rate (beats/min) decreased from 72 ± 12 to 68.9 ± 10.9 after 30 min of WBPA-V-160 (Table 3, Figure 4). The data of systolic BP, diastolic BP, and heart rates at pre-evaluation versus post-evaluation are shown in Figure 4.

Table 3.
Pre–post blood pressure (BP) and hemodynamic profiles after 30 min of WBPA-V-160.
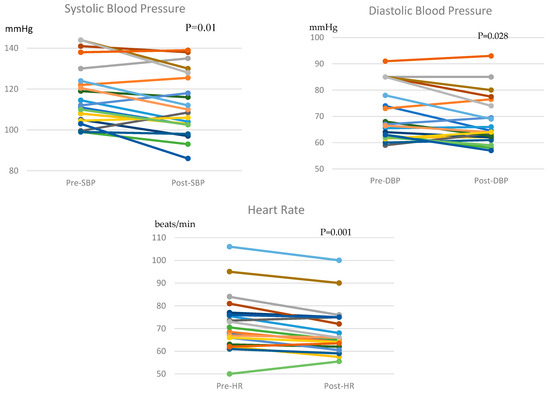
Figure 4.
The pre-SBP, post-SBP, pre-DBP, post-DBP, pre-HR, and post-HR of the individual systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rates (HR). p < 0.05 indicates significant decreases in SBP, DBP, and HR after 30 min of WBPA-V-160.
3.4. Pre–Post Central BP Parameters after 30 min of WBPA-V-160 of Part 2
The end systolic pressure, end diastolic pressure, mean arterial BP, and pulse pressure, i.e., the central BP parameters, all significantly decreased after 30 min of WBPA-V-160 (Table 3).
3.5. Pre–Post Indirect Cardiac Parameters after 30 min of WBPA-V-160 of Part 2
The indirect cardiac parameters, such as LV ejection time and stroke volume, were similar between pre-evaluation and post-evaluation (Table 3). The data of cardiac output at pre-evaluation versus post-evaluation are shown in Figure 5. Cardiac output is the product of the heart rate (HR) and stroke volume (SV). Due to the reduction in heart rate after 30 min of WBPA-V-160, cardiac output was decreased after 30 min of WBPA-V-160.
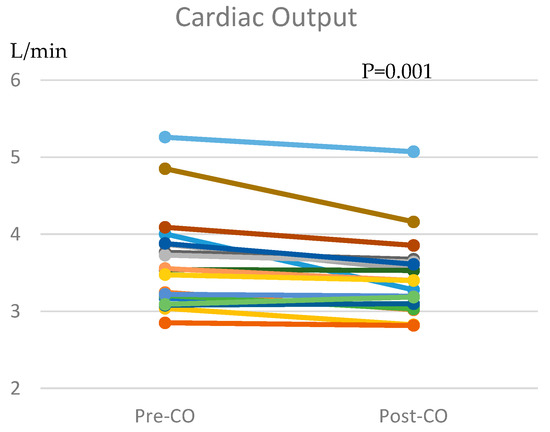
Figure 5.
The pre-CO and post-CO of the individual cardiac output (CO). p < 0.05 indicates significant decreases in CO after 30 min of WBPA-V-160.
3.6. Pre–Post Systemic Vascular (SV) Compliance after 30 of min WBPA-V-160 of Part 2
The systemic vascular (SV) compliance at post-evaluation (0.98 ± 0.18 mL/mmHg) was significantly higher than at pre-evaluation (0.91 ± 0.140) (Table 3). The data of SV compliance at pre-evaluation versus post-evaluation are shown in Figure 6. There was no difference between pre- and post-systemic vascular (SV) resistance (Table 3).
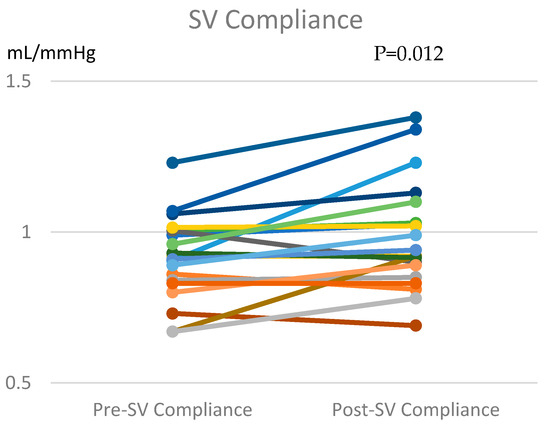
Figure 6.
The pre-SV compliance and post--SV compliance of the individual systemic vascular (SV) compliance. p < 0.05 means significant increases in SV compliance after 30 min of WBPA-V-160.
3.7. Pre–Post Brachial Artery (BA) Parameters after 30 min of WBPA-V-160 of Part 2
The brachial artery (BA) distensibility at post-evaluation (6.30 ± 1.22%/mmHg) was significantly higher than at pre-evaluation (5.82 ± 1.01) after 30 min of WBPA-V-160 (Table 3). The data of BA distensibility at pre-evaluation versus post-evaluation are shown in Figure 7. However, BA compliance and BA resistance were not different after 30 min of WBPA-V-160.
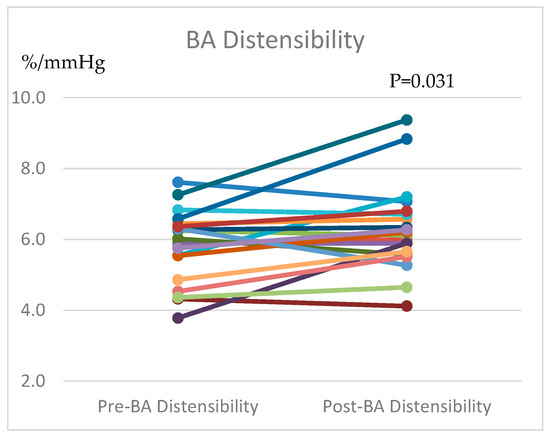
Figure 7.
The pre-BA distensibility and post-BA distensibility of the individual brachial artery (BA) distensibility. p < 0.05 means significant increases in BA distensibility after 30 min of WBPA-V-160.
4. Discussion
Our major findings can be summarized as follows: (1) The WBPA-V-160, as compared to the 180-degree WBPA, significantly lowered the SBP, DBP, and HR and increased the exhaled nitric oxide with the same moving distance of 6 mm, the same periodic frequency of 4 Hz, and the same acceleration in the Z planes. (2) The systolic BP, diastolic BP, heart rate, end systolic pressure, end diastolic pressure, mean arterial BP, and pulse pressure became lower after a single 30 min session of WBPA-V-160, with a moving distance, from headward to footward, of 2 mm (4 ± 0.1 Hz). (3) Due to the reduced heart rates and unchanged stroke volume after the 30 min of WBPA-V-160, the cardiac output was decreased after 30 min of WBPA-V-160. (4) The systemic vascular compliance and brachial artery distensibility became higher after 30 min of WBPA-V-160.
The systolic BP, diastolic BP, and mean arterial BP were significantly lower after 30 min of WBPA-V-160. One study reported that WBPA, with increments in acceleration and the frequency held constant at 4 ± 0.1 Hz, led to almost linear increases in minute ventilation but did not change the arterial BP and heart rate in animals [9]. One study reported that a 45 min session of WBPA improved coronary microcirculation by using transthoracic Doppler echocardiography for the assessment of coronary flow reserve but did not change the BP in eight Type II diabetic patients [6]. In a previous study of 20 anesthetized piglets, the mean arterial BP decreased from 115 ± 10 at baseline to 90 ± 8 after 60 min of WBPA [12]. The current study is the first to report the central BP parameters (e.g., end systolic pressure, end diastolic pressure, mean arterial BP, and pulse pressure) becoming lower after 30 min of WBPA-V-160 with a moving distance of only 2 mm. The findings show that the pressure in a ventricle at the end of contraction and its pressure at the lowest volume of blood were reduced after 30 min of WBPA-V-160.
Neither cardiac output nor stroke volume after WBPA has been reported in previous human studies. In the current study, the cardiac output decreased after a single 30 min session of WBPA-V-160 due to the reduced heart rate and unchanged stroke volume. The lowered heart rate and similar stroke volume after WBPA-V-160 suggest that subjects had a lower cardiac output and lower heart rates after WBPA-V-160.
Neither systemic vascular compliance nor systemic vascular resistance has been reported after WBPA in humans. This study presented that systemic vascular compliance could be improved after WBPA-V-160 with a moving distance of 2 mm at a constant frequency of 4 Hz in human subjects. An increase in the total systemic arterial compliance after exercise training was reported partially due to the changes in BP and partially due to the changes in intrinsic arterial compliance [20]. We might speculate that this WBPA-V-160-induced systemic vascular compliance might be partially due to the changes in BP and partially due to the changes in intrinsic arterial compliance. Since systemic vascular compliance is the ability of the systemic vessel wall to expand and contract passively with changes in pressure, we could speculate that the WBPA-V-160-enhanced systemic vascular compliance might be partially due to the endothelial nitric oxide in the whole-body, causing muscles around the arteries to smooth and causing arterial relaxation. Of course, future studies are required to answer how passive exercise WBPA-V-160 improves systemic vascular compliance.
In previous studies, neither brachial artery compliance, brachial artery distensibility, nor brachial artery resistance has been reported after WBPA or WBPA-V-160 in humans. The non-invasive measures of brachial arteries, such as brachial artery distensibility, are effective in assessing cardiovascular risk [19]. Brachial artery distensibility is a measure of arterial stiffness [19]. Since arterial stiffness can be improved by nitric oxide [21], brachial artery distensibility was increased after 30 min of WBPA-V-160, which might imply that WBPA-V-160 might have the potential to improve arterial stiffness due to the increased nitric oxide.
Some limitations were also present in this research. In this pilot study, the increased nitric oxide detected via NIOX after WBPA-V-160 cannot be isolated from inducible nitric oxide versus endothelial nitric oxide. We investigated the acute effects of a single 30 min trial of WBPA-V-160 at a constant frequency of 4 Hz on cardiovascular hemodynamics. Based on the preliminary findings of this pilot study, because we did not see any change in the BP and exhaled nitric oxide after the control non-WBPA without turning on the motor, we decided to investigate the acute effects of a single 30 min session of WBPA-V-160 without control. It is still unknown whether the long-term effects of a 60 min trial or a 3-month WBPA-V-160 program could have better effects on BP, or whether different effects can be found in WBPA-V-160 with various moving distances (2 mm, 6 mm or 2.4 cm) from headward to footward, or frequency. Because we did not video record the moving abdominal compartment in the pilot study, we cannot observe the relationship between the movement of the abdominal compartment and nitric oxide release. The moving distance of 2 mm in the WBPA-V-160 was enough to improve the blood pressure and cardiovascular hemodynamics in healthy subjects. It is unknown whether the therapeutic effects of WBPA-V-160 with a longer moving distance from headward to footward in hypertensive patients are better. Future studies will need to answer these questions.
5. Conclusions
This study suggests a 160-degree V-shape Whole-Body Periodic Acceleration (WBPA-V-160) with a moving distance of 2 mm, 4 Hz, pGz: ±0.8 G, as a potential therapeutic regimen for lowering BP and improving cardiovascular hemodynamics, such as lowing central BP parameters, increasing systemic vascular compliance, and reducing artery stiffness.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app12189116/s1, Supplement 1: Sample size and power calculations. Supplement 2: The differences and effect size of pre-post parameters.
Author Contributions
Concept: J.K.S.W., C.-J.W., Y.-Y.L., S.-D.L.; Methodology: J.K.S.W., C.-J.W., S.-D.L.; Validation: J.K.S.W., Y.-Y.L., S.-D.L.; Data curation: C.-J.W., Y.-Y.L.; Funding acquisition: J.K.S.W., S.-D.L.; Writing—original draft preparation: J.K.S.W., Y.-Y.L.; Writing—revision and editing: J.K.S.W., C.-J.W., Y.-Y.L., S.-D.L.; Supervision: S.-D.L.; Project administration: S.-D.L. All authors have read and agreed to the published version of the manuscript.
Funding
Asia University and Asia University Hospital. ASIA-107-AUH-02. The study was partially supported by China Medical University and National Taipei University of Nursing and Health Sciences.
Institutional Review Board Statement
This study was reviewed by the Institutional Review Board of the China Medical University Hospital and only healthy normal subjects were included in the pilot study, which was conducted according to the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors would like to thank Guangdong Nuozhou Health Technology Co., Ltd. and Youzhi Health Technology Co., Ltd. for providing adjustable 180- to 160-degree V-shape Whole-Body Periodic Acceleration and NIOX portable exhaled nitric oxide analyzer in the pilot study. The authors would like to thank Kuang Yu Mental Working Co., Ltd. for providing the 160-degree V-shape Whole-Body Periodic Acceleration and thank all voluntary participants. In addition, we acknowledge the support of Pulse Metric, Inc., which provided DynaPulse-200M devices from Gordon Hsu.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Adams, J.A.; Wu, H.; Bassuk, J.A.; Arias, J.; Uryash, A.; Jorapur, V.; Lamas, G.A.; Kurlansky, P. Periodic acceleration (pgz) prior to whole body ischemia reperfusion injury provides early cardioprotective preconditioning. Life Sci. 2010, 86, 707–715. [Google Scholar] [CrossRef] [PubMed]
- Sackner, M.A.; Gummels, E.; Adams, J.A. Nitric oxide is released into circulation with whole-body, periodic acceleration. Chest 2005, 127, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.A.; Pastuszko, P.; Uryash, A.; Wilson, D.; Padrino, J.R.L.; Nadkarni, V.; Pastuszko, A. Whole body periodic acceleration (pgz) as a non-invasive preconditioning strategy for pediatric cardiac surgery. Med. Hypotheses 2018, 110, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Uryash, A.; Bassuk, J.; Kurlansky, P.; Altamirano, F.; Lopez, J.R.; Adams, J.A. Antioxidant properties of whole body periodic acceleration (pgz). PLoS ONE 2015, 10, e0131392. [Google Scholar]
- Adams, J.A.; Uryash, A.; Lopez, J.R.; Sackner, M.A. Whole body periodic acceleration improves survival and microvascular leak in a murine endotoxin model. PLoS ONE 2019, 14, e0208681. [Google Scholar]
- Sakaguchi, M.; Fukuda, S.; Shimada, K.; Izumi, Y.; Izumiya, Y.; Nakamura, Y.; Nakanishi, K.; Otsuka, K.; Ogawa, H.; Fujita, M. Preliminary observations of passive exercise using whole body periodic acceleration on coronary microcirculation and glucose tolerance in patients with type 2 diabetes. J. Cardiol. 2012, 60, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Takase, B.; Hattori, H.; Tanaka, Y.; Uehata, A.; Nagata, M.; Ishihara, M.; Fujita, M. Acute effect of whole-body periodic acceleration on brachial flow-mediated vasodilatation assessed by a novel semi-automatic vessel chasing unexef18g system. J. Cardiovasc. Ultrasound 2013, 21, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, S.; Shimada, K.; Kawasaki, T.; Kono, Y.; Jissho, S.; Taguchi, H.; Maeda, K.; Yoshiyama, M.; Fujita, M.; Yoshikawa, J. “Passive exercise” using whole body periodic acceleration: Effects on coronary microcirculation. Am. Heart J. 2010, 159, 620–626. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.A.; Mangino, M.J.; Bassuk, J.; Inman, D.M.; Sackner, M.A. Noninvasive motion ventilation (nimv): A novel approach to ventilatory support. J. Appl. Physiol. 2000, 89, 2438–2446. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sackner, M.A. Whole body periodic acceleration: “Passive exercise” for parkinson’s disease. J. Parkinsonism Restless Legs Syndr. 2012, 2, 1. [Google Scholar] [CrossRef]
- Safar, M.E.; Jankowski, P. Central blood pressure and hypertension: Role in cardiovascular risk assessment. Clin. Sci. 2009, 116, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Martínez, A.; Arias, J.; Bassuk, J.A.; Wu, H.; Kurlansky, P.; Adams, J.A. Adrenomedullin is increased by pulsatile shear stress on the vascular endothelium via periodic acceleration (pgz). Peptides 2008, 29, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Chio, S.-S.; Urbina, E.M.; LaPointe, J.; Tsai, J.; Berenson, G.S. Korotkoff sound versus oscillometric cuff sphygmomanometers: Comparison between auscultatory and dynapulse blood pressure measurements. J. Am. Soc. Hypertens. 2011, 5, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Brinton, T.J.; Cotter, B.; Kailasam, M.T.; Brown, D.L.; Chio, S.-S.; O’Connor, D.T.; DeMaria, A.N. Development and validation of a noninvasive method to determine arterial pressure and vascular compliance. Am. J. Cardiol. 1997, 80, 323–330. [Google Scholar] [CrossRef]
- Bassuk, J.I.; Wu, H.; Arias, J.; Kurlansky, P.; Adams, J.A. Whole body periodic acceleration (pgz) improves survival and allows for resuscitation in a model of severe hemorrhagic shock in pigs. J. Surg. Res. 2010, 164, e281–e289. [Google Scholar] [CrossRef]
- Otsuki, T.; Maeda, S.; Iemitsu, M.; Saito, Y.; Tanimura, Y.; Ajisaka, R.; Miyauchi, T. Systemic arterial compliance, systemic vascular resistance, and effective arterial elastance during exercise in endurance-trained men. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2008, 295, R228–R235. [Google Scholar] [CrossRef][Green Version]
- Trammel, J.; Sapra, A. Physiology, Systemic Vascular Resistance. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- McVeigh, G.E.; Bank, A.J.; Cohn, J.N. Arterial compliance. In Cardiovascular Medicine; Springer: Berlin/Heidelberg, Germany, 2007; pp. 1811–1831. [Google Scholar]
- Chiang, M.-C.; Yin, W.-H.; Lin, Y.-T.; Jen, H.-L.; Wang, J.-J.; Huang, W.-P.; Feng, A.-N.; Yang, Y.-N.; Young, M.S. Brachial artery distensibility as a cardiovascular risk marker in asymptomatic individuals. J. Intern. Med. Taiwan 2005, 16, 1–10. [Google Scholar]
- Cameron, J.D.; Dart, A.M. Exercise training increases total systemic arterial compliance in humans. Am. J. Physiol.-Heart Circ. Physiol. 1994, 266, H693–H701. [Google Scholar] [CrossRef] [PubMed]
- Bellien, J.; Favre, J.; Iacob, M.; Gao, J.; Thuillez, C.; Richard, V.; Joannides, R. Arterial stiffness is regulated by nitric oxide and endothelium-derived hyperpolarizing factor during changes in blood flow in humans. Hypertension 2010, 55, 674–680. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).