Compassionate Embodied Virtual Experience Increases the Adherence to Meditation Practice
Abstract
1. Introduction
2. Materials and Methods
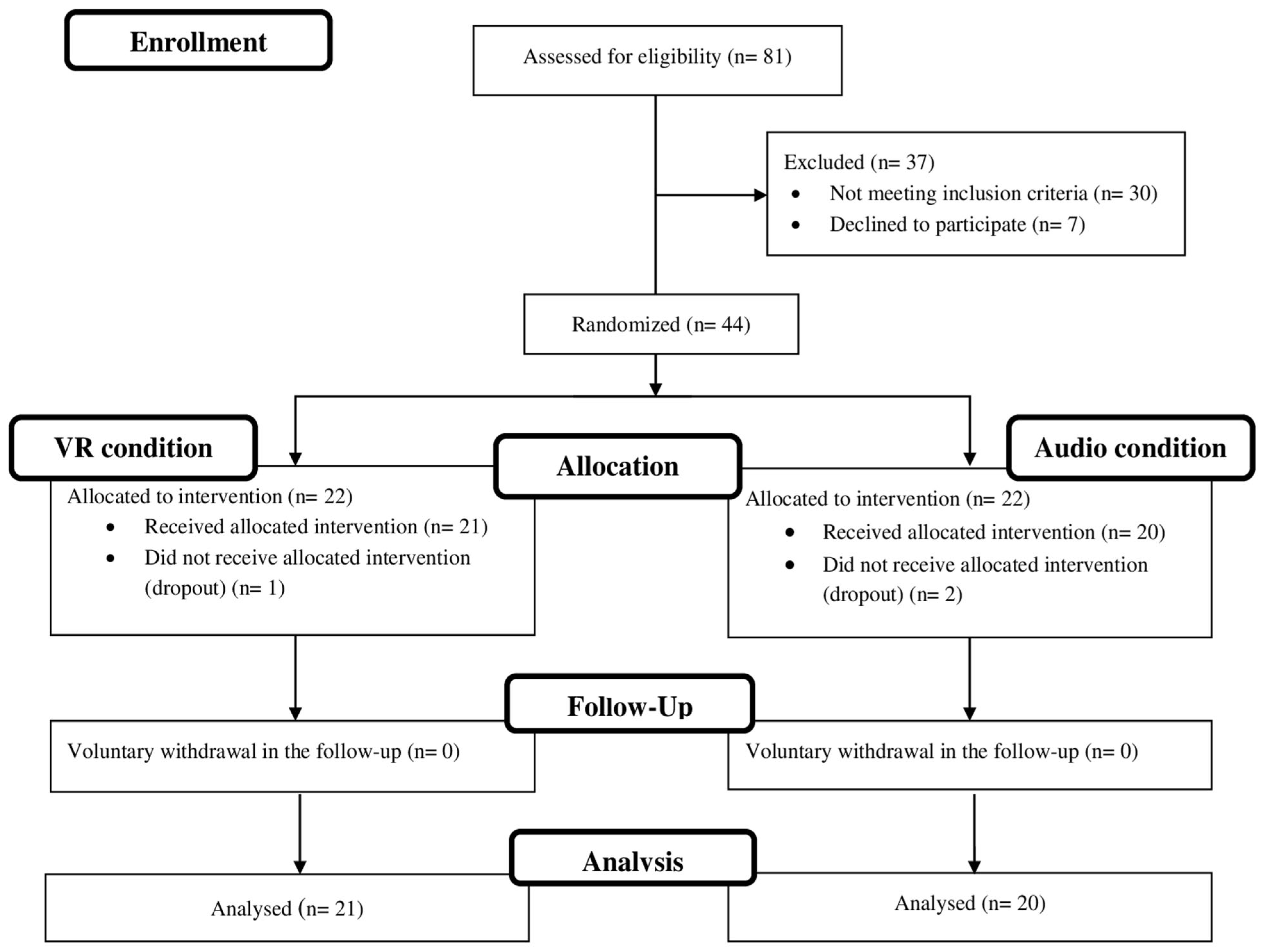
2.1. Participants
2.2. Measures
2.2.1. Pre- and Postintervention Measures
2.2.2. Pre- and Post-In-Person Session Measures
2.2.3. Post-In-Person Session Measures
2.2.4. Daily Follow-Up after the In-Person Session
2.3. Procedure
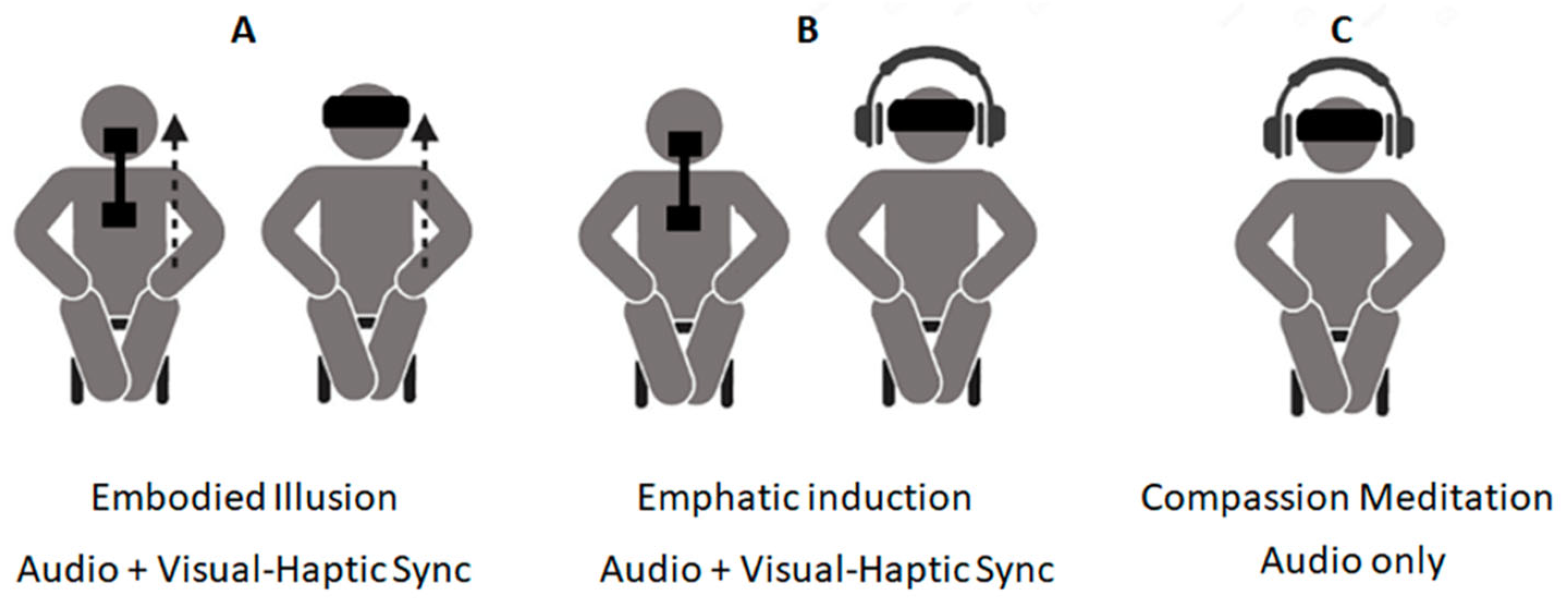
2.3.1. The VR Condition
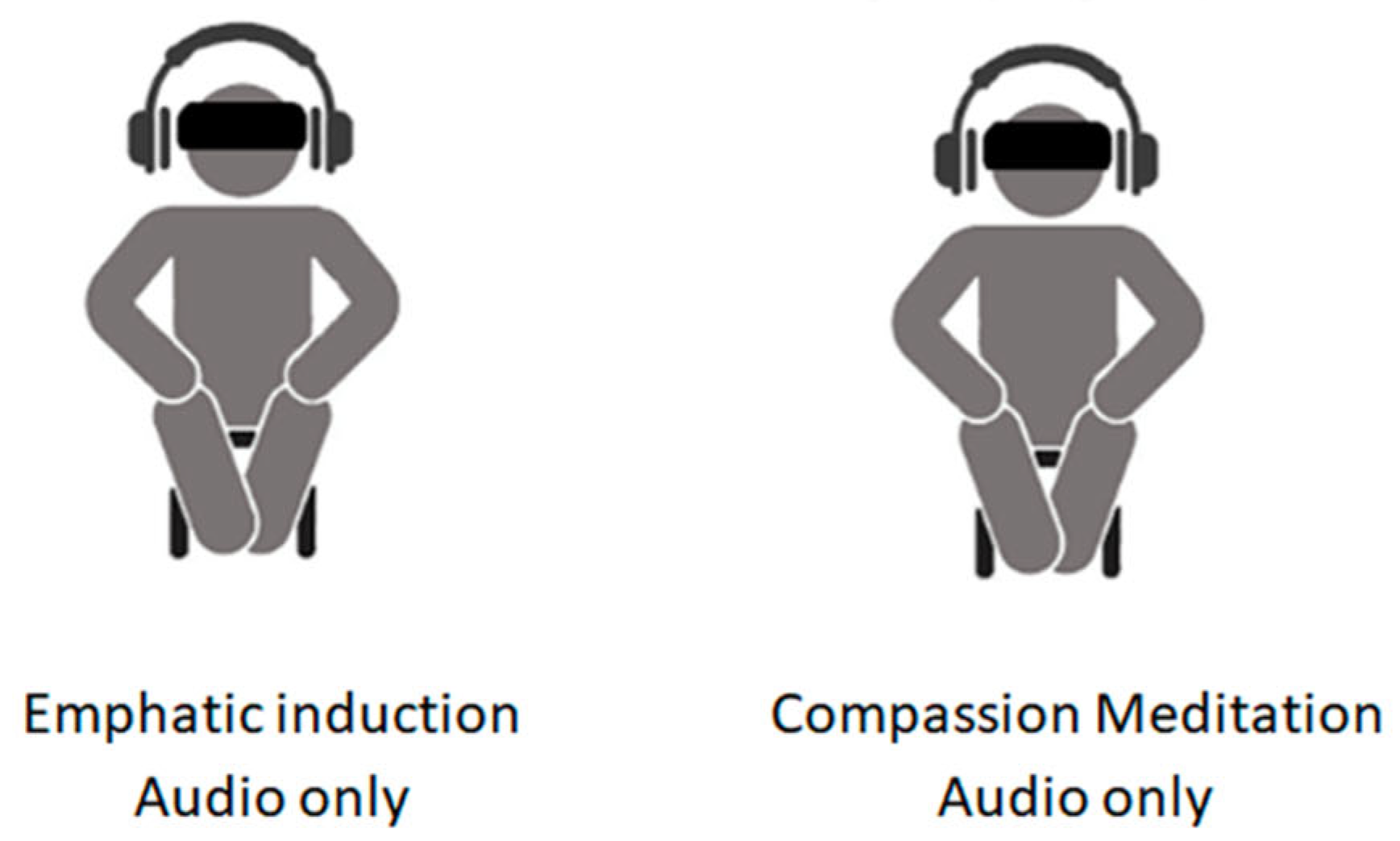
2.3.2. The Audio Condition
2.4. Data Analyses
3. Results
3.1. Efficacy of the In-Person Session Practices
3.2. Efficacy of the Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
References
- Ventura, S.; Badenes-Ribera, L.; Herrero, R.; Cebolla, A.; Galiana, L.; Baños, R. Virtual reality as a medium to elicit empathy: A meta-analysis. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.J.; Le, A.M.T.; Bailenson, J.N. The effect of embodied experiences on self-other merging, attitude, and helping behavior. Media Psychol. 2013, 16, 7–38. [Google Scholar] [CrossRef]
- Groom, V.; Bailenson, J.N.; Nass, C. The influence of racial embodiment on racial bias in immersive virtual environments. Soc. Influ. 2009, 4, 231–248. [Google Scholar] [CrossRef]
- Rosenberg, R.S.; Baughman, S.L.; Bailenson, J.N. Virtual Superheroes: Using superpowers in virtual reality to encourage prosocial behavior. PLoS ONE 2013, 8, e55003. [Google Scholar] [CrossRef] [PubMed]
- Barbot, B.; Kaufman, J.C. What makes immersive virtual reality the ultimate empathy machine? Discerning the underlying mechanisms of change. Comput. Hum. Behav. 2020, 111, 106431. [Google Scholar] [CrossRef]
- Longo, M.R.; Schüür, F.; Kammers, M.P.; Tsakiris, M.; Haggard, P. What is embodiment? A psychometric approach. Cognition 2008, 107, 978–998. [Google Scholar] [CrossRef]
- Hopkins, J. Cultivating Compassion; Broadway Books: New York, NY, USA, 2001. [Google Scholar]
- Kirby, J.N.; Tellegen, C.L.; Steindl, S.R. A meta-analysis of compassion-based interventions: Current state of knowledge and future directions. Behav. Ther. 2017, 48, 778–792. [Google Scholar] [CrossRef]
- López, A.; Sanderman, R.; Ranchor, A.V.; Schroevers, M.J. Compassion for others and self-compassion: Levels, correlates, and relationship with psychological well-being. Mindfulness 2018, 9, 325–331. [Google Scholar] [CrossRef]
- Cosley, B.J.; McCoy, S.K.; Saslow, L.R.; Epel, E.S. Is compassion for others stress buffering? Consequences of compassion and social support for physiological reactivity to stress. J. Exp. Soc. Psychol. 2010, 46, 816–823. [Google Scholar] [CrossRef]
- Brito-Pons, G.; Campos, D.; Cebolla, A. Implicit or explicit compassion? Effects of compassion cultivation training and comparison with mindfulness-based stress reduction. Mindfulness 2018, 9, 1494–1508. [Google Scholar] [CrossRef]
- Dahl, C.J.; Lutz, A.; Davidson, R.J. Reconstructing and deconstructing the self: Cognitive mechanisms in meditation practice. Trends Cogn. Sci. 2015, 19, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Rinpoche, R.T.; Mullen, K. The Buddhist use of compassionate imagery in mind healing. In Compassion: Conceptualisations, Research and Use in Psychotherapy; Routledge: Abingdon, UK, 2005; pp. 218–238. [Google Scholar]
- Navarrete, J.; Campos, D.; Diego-Pedro, R.; González-Hernández, E.; Herrero, R.; Baños, R.M.; Cebolla, A. Compassion-based meditation quality practice and its impact on the positive attitudes toward others. Mindfulness 2021. under review. [Google Scholar]
- Cebolla, A.; Herrero, R.; Ventura, S.; Miragall, M.; Bellosta-Batalla, M.; Llorens, R.; Baños, R.M. Putting oneself in the body of others: A pilot study on the efficacy of an embodied virtual reality system to generate self-compassion. Front. Psychol. 2019, 10, 1521. [Google Scholar] [CrossRef]
- Falconer, C.J.; Slater, M.; Rovira, A.; King, J.A.; Gilbert, P.; Antley, A.; Brewin, C.R. Embodying compassion: A virtual reality paradigm for overcoming excessive self-criticism. PLoS ONE 2014, 9, e111933. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, E.C.; Bertrand, P.; Lesur, M.E.R.; Palomo, P.; Demarzo, M.; Cebolla, A. Virtual body swap: A new feasible tool to be explored in health and education. In Proceedings of the 2016 XVIII Symposium on Virtual and Augmented Reality (SVR), Gramado, Brazil, 21–24 June 2016; pp. 81–89. [Google Scholar]
- Cohn, M.A.; Fredrickson, B.L. In search of durable positive psychology interventions: Predictors and consequences of long-term positive behavior change. J. Posit. Psychol. 2010, 5, 355–366. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Dickau, L. Experimental evidence for the intention–behavior relationship in the physical activity domain: A meta-analysis. Health Psychol. 2012, 31, 724–727. [Google Scholar] [CrossRef]
- Layous, K.; Nelson, S.K.; Kurtz, J.L.; Lyubomirsky, S. What triggers prosocial effort? A positive feedback loop between positive activities, kindness, and well-being. J. Posit. Psychol. 2016, 12, 385–398. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Kates, A. Can the affective response to exercise predict future motives and physical activity behavior? A systematic review of published evidence. Ann. Behav. Med. 2015, 49, 715–731. [Google Scholar] [CrossRef]
- Van Cappellen, P.; Catalino, L.I.; Fredrickson, B.L. A new micro-intervention to increase the enjoyment and continued practice of meditation. Emotion 2020, 20, 1332–1343. [Google Scholar] [CrossRef]
- Fredrickson, B.L. Chapter One—Positive emotions broaden and build. Adv. Exp. Soc. Psychol. 2013, 47, 1–53. [Google Scholar] [CrossRef]
- Santorelli, S.F.; Kabat-Zinn, J.; Blacker, M.; Meleo-Meyer, F.; Koerbel, L. Mindfulness-Based Stress Reduction (MBSR) Authorized Curriculum Guide 2017; Center for Mindfulness in Medicine, Health Care, and Society, University of Massachusetts Medical School: Worcester, MA, USA, 2017; Available online: https://www.umassmed.edu/contentassets/abe554ad1ced45b98c57e455441d3f95/mbsr-curriculum-guide-2017.pdf (accessed on 27 November 2019).
- Segal, Z.V.; Williams, J.M.G.; Teasdale, J.D. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse, 2nd ed.; Guilford Publications: New York, NY, USA, 2013. [Google Scholar]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Personal. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Robles, R.; Páez, F. Estudio sobre la traducción al español y las propiedades psicométricas de las escalas de afecto positivo y negativo (PANAS). Salud Ment. 2003, 26, 69–75. [Google Scholar]
- Sprecher, S.; Fehr, B. Compassionate love for close others and humanity. J. Soc. Pers. Relatsh. 2005, 22, 629–651. [Google Scholar] [CrossRef]
- Tanay, G.; Bernstein, A. State Mindfulness Scale (SMS): Development and initial validation. Psychol. Assess. 2013, 25, 1286–1299. [Google Scholar] [CrossRef] [PubMed]
- Kirschner, H.; Kuyken, W.; Wright, K.; Roberts, H.; Brejcha, C.; Karl, A. Soothing your heart and feeling connected: A new experimental paradigm to study the benefits of self-compassion. Clin. Psychol. Sci. 2019, 7, 545–565. [Google Scholar] [CrossRef]
- Brocklebank, S.; Lewis, G.J.; Bates, T.C. Personality accounts for stable preferences and expectations across a range of simple games. Pers. Individ. Differ. 2011, 51, 881–886. [Google Scholar] [CrossRef]
- Millisecond Software. Inquisit’s Dictator Game (Computer Software), 2020. Available online: https://www.millisecond.com/download/library/dictatorgame/ (accessed on 13 November 2019).
- Hojat, M. Empathy as Related to Personal Qualities, Career Choice, Acquisition of Knowledge, and Clinical Competence. In Empathy in Health Professions Education and Patient Care; Springer: Cham, Switzerland, 2016. [Google Scholar] [CrossRef]
- Kosslyn, S.M. Image and Brain: The Resolution of the Imagery Debate; MIT Press: Cambridge, MA, USA, 1994. [Google Scholar]
- Incagli, F.; Tarantino, V.; Crescentini, C.; Vallesi, A. The effects of 8-week mindfulness-based stress reduction program on cognitive control: An EEG study. Mindfulness 2019, 11, 756–770. [Google Scholar] [CrossRef]
- Gu, J.; Baer, R.; Cavanagh, K.; Kuyken, W.; Strauss, C. Development and psychometric properties of the Sussex-Oxford compassion scales (SOCS). Assessment 2020, 27, 3–20. [Google Scholar] [CrossRef]
| Baseline Characteristic | VR | Audio | Full Sample | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Gender | ||||||
| Female | 17 | 81 | 16 | 80 | 33 | 80.5 |
| Male | 4 | 19 | 4 | 20 | 8 | 19.5 |
| Highest educational level | ||||||
| Middle school | 2 | 9.5 | 4 | 20 | 6 | 14.6 |
| High school/some college | 13 | 61.9 | 13 | 65 | 26 | 63.4 |
| University or postgraduate degree | 6 | 28.6 | 3 | 15 | 9 | 22 |
| Previous experience a | ||||||
| Meditation practice | 5 | 23.8 | 5 | 25 | 10 | 24.4 |
| Compassion practice | 4 | 19.05 | 2 | 10 | 6 | 14.63 |
| Meditation practice frequency | ||||||
| Never | 18 | 85.71 | 20 | 100 | 38 | 92.68 |
| 1 time per week | 1 | 4.76 | 0 | 0 | 1 | 2.44 |
| 4 times per week | 2 | 9.53 | 0 | 0 | 2 | 4.88 |
| Variables | VR (n = 21) a | Audio (n = 20) a | t-Student | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | t | p | η2 | |
| SMS (Total Score) | 74.65 (14.28) | 85.29 (11.73) | 67.30 (13.34) | 82.68 (11.29) | t (38) = −1.68 | 0.101 | 0.07 |
| SMS (Body subscale) | 20.86 (4.70) | 22.43 (4.14) | 18.05 (4.65) | 21.30 (5.30) | t (39) = −1.92 | 0.062 | 0.09 |
| SMS (Mind subscale) | 53.80 (10.22) | 62.86 (9.10) | 49.25 (10.17) | 61.16 (7.48) | t (38) = −1.41 | 0.166 | 0.05 |
| VAS-SC (Self-compassion) | 11.93 (4.36) | 11.71 (4.58) | 11 (3.52) | 11.48 (3.86) | t (39) = −0.80 | 0.429 | 0.02 |
| VAS-SC (Positive affiliative affect) | 23.44 (3.14) | 23.33 (3.74) | 21.85 (5.72) | 20.90 (5.21) | t (39) = −1.00 | 0.324 | 0.03 |
| VAS-SC (Self-criticism) | 7.40 (1.76) | 7.05 (1.95) | 7.53 (1.73) | 7.08 (1.76) | t (39) = 0.18 | 0.859 | 0 |
| VAS-SC (Energized level) | 6.70 (1.77) | 6.10 (1.37) | 7.00 (2.18) | 5.83 (1.66) | t (39) = 0.31 | 0.761 | 0 |
| PANAS (Positive Affect) | 32.14 (5.58) | 32.53 (7.33) | 30.20 (7.54) | 32.56 (5.60) | t (39) = −0.94 | 0.353 | 0.02 |
| PANAS (Negative Affect) | 16.52 (3.39) | 17.79 (7.49) | 16.75 (4.58) | 17.06 (4.95) | t (39) = 0.18 | 0.858 | 0 |
| CLS | 118.52 (16.54) | 117.63 (16.87) | 122.80 (9.75) | 121.47 (14.82) | t (39) = 1.00 | 0.322 | 0.03 |
| Variables | VR (n = 21) | Audio (n = 20) | ANCOVA | ||||||
|---|---|---|---|---|---|---|---|---|---|
| t-Student | t-Student | ||||||||
| t | p | η2 | t | p | η2 | F | p | ηp2 | |
| Pre- and post-in-person session assessment | |||||||||
| SMS (Total Score) | t (19) = −3.17 | 0.005 | 0.35 | t (18) = −3.94 | 0.001 | 0.46 | F (1, 36) = 0.01 | 0.924 | 0.00 |
| SMS (Body subscale) | t (20) = 1.76 | 0.093 | 0.13 | t (19) = 1.93 | 0.068 | 0.16 | F (1, 38) = 0.15 | 0.700 | 0.00 |
| SMS (Mind subscale) | t (19) = 3.47 | 0.003 | 0.39 | t (18) = 4.67 | 0.000 | 0.55 | F (1, 36) = 0.00 | 0.952 | 0.00 |
| VAS-SC (Self-compassion) | t (20) = 0.21 | 0.838 | 0.00 | t (19) = −1.02 | 0.320 | 0.05 | F (1, 38) = 0.35 | 0.556 | 0.00 |
| VAS-SC (Positive affiliative affect) | t (20) = 0.29 | 0.775 | 0.00 | t (19) = 1.50 | 0.150 | 0.11 | F (1, 37) = 1.37 | 0.248 | 0.04 |
| VAS-SC (Self-criticism) | t (19) = 1.85 | 0.079 | 0.15 | t (19) = 1.16 | 0.261 | 0.07 | F (1, 37) = 0.03 | 0.868 | 0.00 |
| VAS-SC (Energized level) | t (20) = 1.78 | 0.090 | 0.14 | t (19) = 2.63 | 0.017 | 0.27 | F (1, 37) = 1.39 | 0.245 | 0.04 |
| Pre- and postintervention assessment | |||||||||
| PANAS (Positive Affect) | t (18) = −0.05 | 0.962 | 0.00 | t (15) = −0.86 | 0.405 | 0.05 | F (1, 32) = 0.23 | 0.633 | 0.01 |
| PANAS (Negative Affect) | t (18) = −0.90 | 0.378 | 0.04 | t (15) = −0.95 | 0.358 | 0.06 | F (1, 32) = 0.00 | 0.947 | 0.00 |
| CLS | t (18) = 0.25 | 0.809 | 0.00 | t (14) = 0.15 | 0.883 | 0.00 | F (1, 31) = 0.07 | 0.797 | 0.00 |
| Variable | VR (n = 21) | Audio (n = 20) | ANCOVA a | ||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | F | p | ηp2 | |
| Imagery Factor (CPQS) b | 60.69 | 13.57 | 64.31 | 15.96 | F (1, 31) = 0.69 | 0.413 | 0.00 |
| Somatic Factor (CPQS) b | 52.41 | 11.73 | 57.11 | 16.31 | F (1, 31) = 2.04 | 0.163 | 0.06 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navarrete, J.; Martínez-Sanchis, M.; Bellosta-Batalla, M.; Baños, R.; Cebolla, A.; Herrero, R. Compassionate Embodied Virtual Experience Increases the Adherence to Meditation Practice. Appl. Sci. 2021, 11, 1276. https://doi.org/10.3390/app11031276
Navarrete J, Martínez-Sanchis M, Bellosta-Batalla M, Baños R, Cebolla A, Herrero R. Compassionate Embodied Virtual Experience Increases the Adherence to Meditation Practice. Applied Sciences. 2021; 11(3):1276. https://doi.org/10.3390/app11031276
Chicago/Turabian StyleNavarrete, Jaime, Marian Martínez-Sanchis, Miguel Bellosta-Batalla, Rosa Baños, Ausiàs Cebolla, and Rocío Herrero. 2021. "Compassionate Embodied Virtual Experience Increases the Adherence to Meditation Practice" Applied Sciences 11, no. 3: 1276. https://doi.org/10.3390/app11031276
APA StyleNavarrete, J., Martínez-Sanchis, M., Bellosta-Batalla, M., Baños, R., Cebolla, A., & Herrero, R. (2021). Compassionate Embodied Virtual Experience Increases the Adherence to Meditation Practice. Applied Sciences, 11(3), 1276. https://doi.org/10.3390/app11031276





