Significance of Haptic and Virtual Reality Simulation (VRS) in the Dental Education: A Review of Literature
Abstract
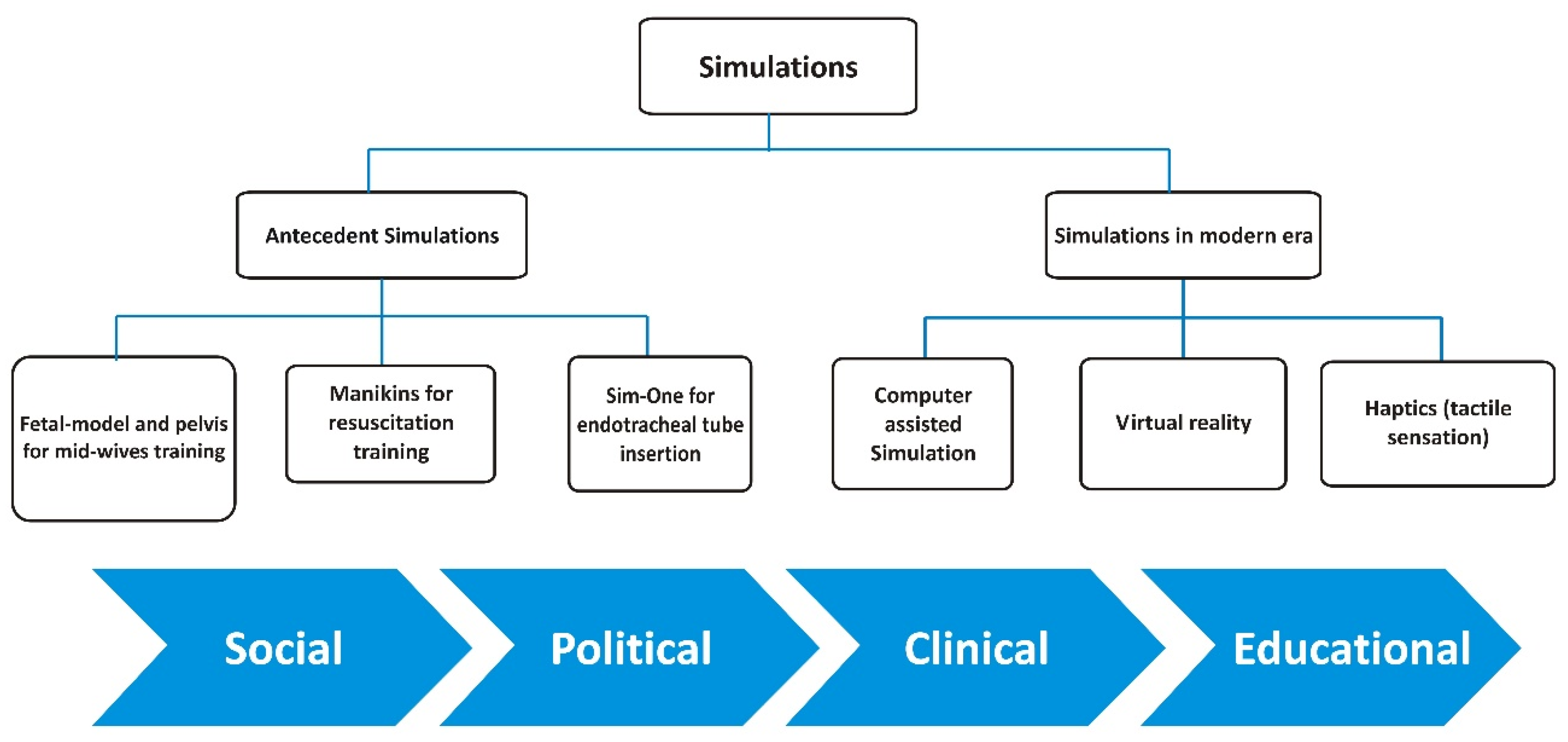
1. Introduction
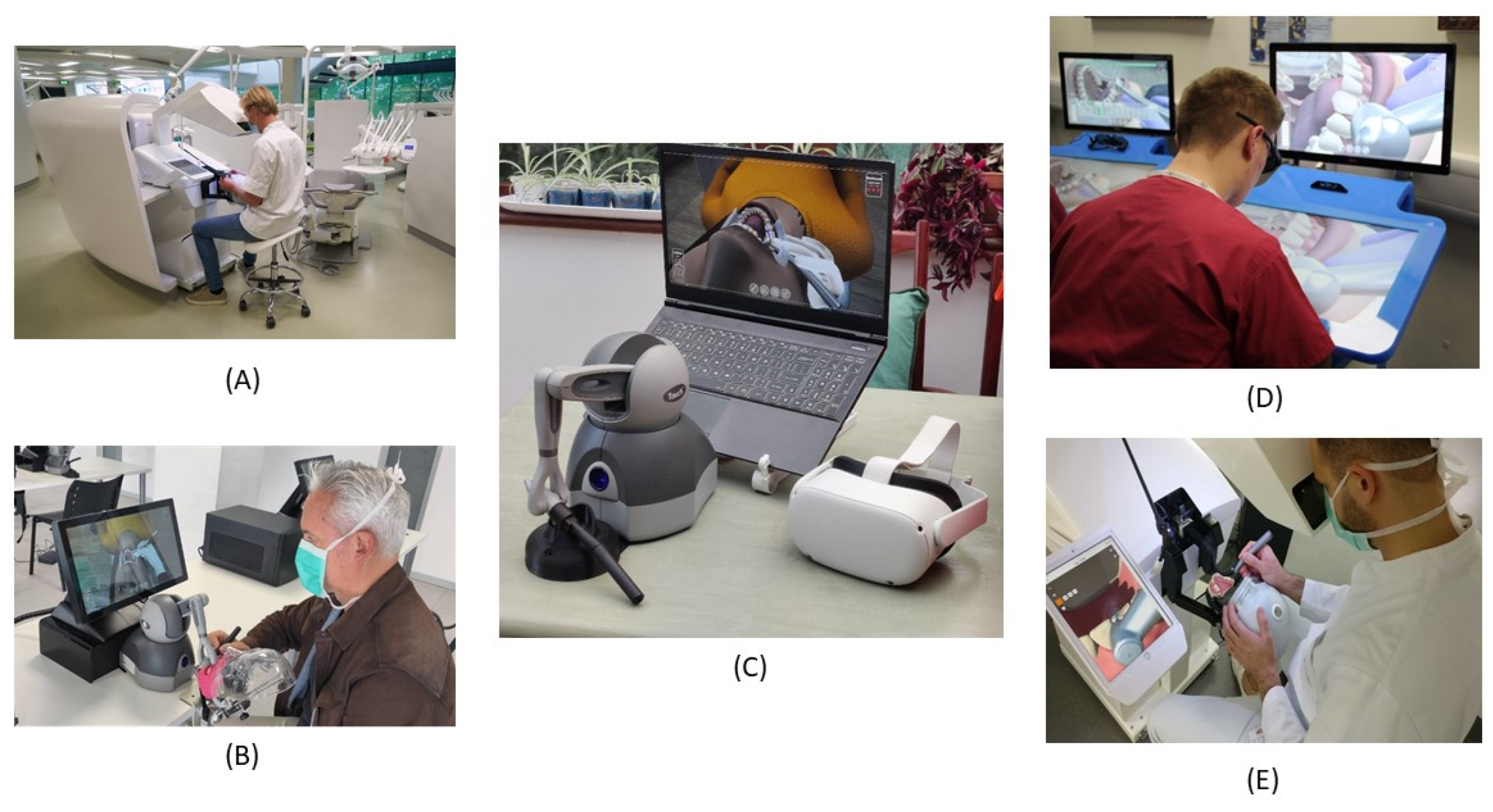
2. Virtual Reality in Periodontology (Gum Diseases)
3. Virtual Reality (VR) Simulation in Restorative Dentistry (Dental Caries Management)
4. Virtual Reality in Maxillo-Facial Surgery
5. Virtual Reality Simulation (VRS) in Prosthodontics (Crown & Fixed Partial Denture)
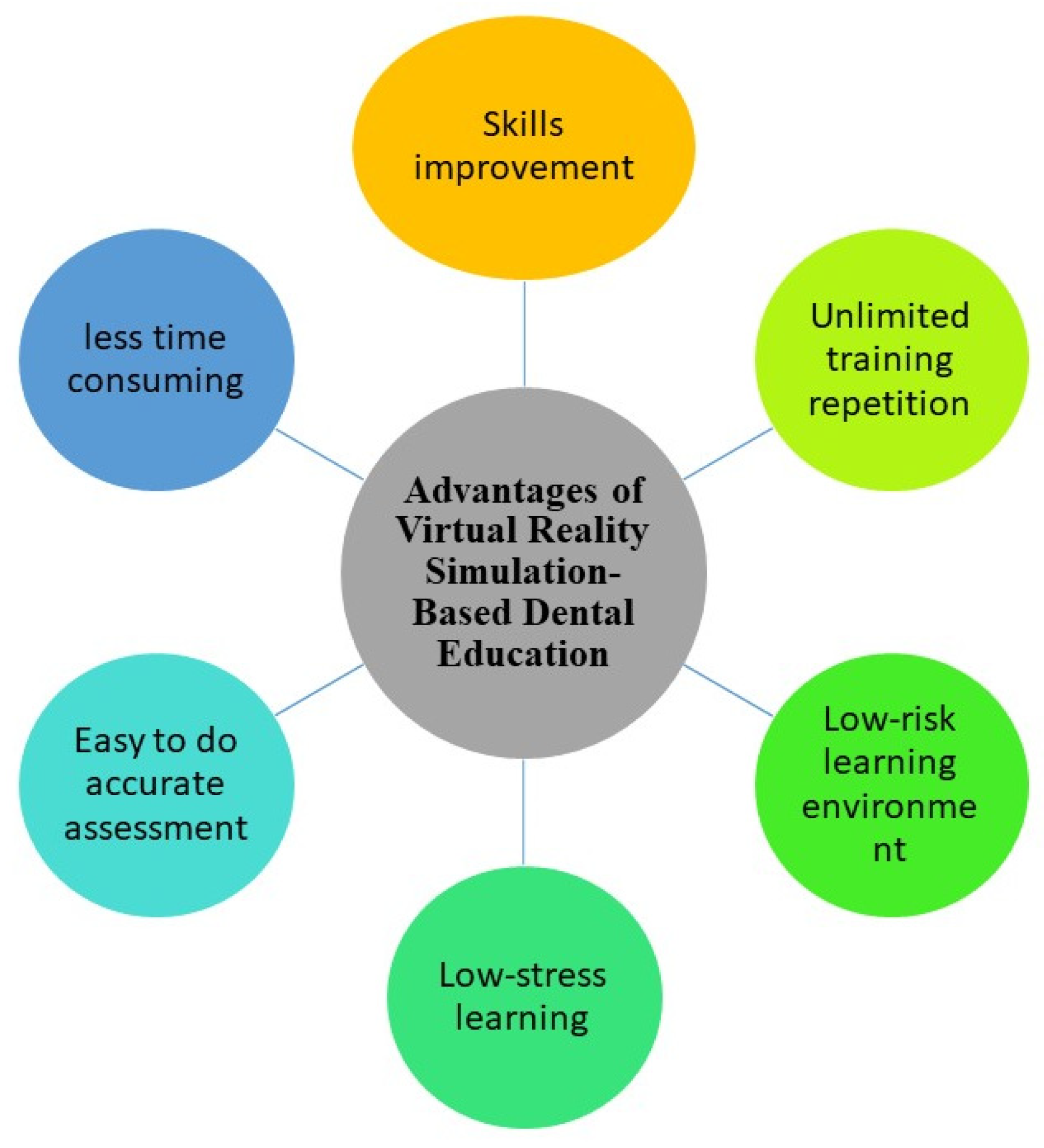
6. Significance of Technology Enhanced Simulation Education in Dentistry
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pawar, A.M. Simulation in Dentistry. EC Dent. Sci. 2017, 3, 115–121. [Google Scholar]
- Ker, J.; Bradley, P. Simulation in Medical Education. Underst. Med. Educ. Evid. Theory Pract. 2010, 164–180. [Google Scholar] [CrossRef]
- Perry, S.; Bridges, S.M.; Burrow, M.F. A review of the use of simulation in dental education. Simul. Healthc. 2015, 10, 31–37. [Google Scholar] [CrossRef]
- Plessas, A. Computerized Virtual Reality Simulation in Preclinical Dentistry: Can a Computerized Simulator Replace the Conventional Phantom Heads and Human Instruction? Simul. Healthc. 2017, 12, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, R.; Vervoorn, J.M.; Buchanan, J. Simulation in Dentistry and Oral Health. In The Comprehensive Textbook of Healthcare Simulation; Springer: New York, NY, USA, 2013; pp. 329–340. [Google Scholar]
- Perry, S.; Burrow, M.F.; Leung, W.K.; Bridges, S.M. Simulation and curriculum design: A global survey in dental education. Aust. Dent. J. 2017, 62, 453–463. [Google Scholar] [CrossRef]
- Higgins, D.; Hayes, M.; Taylor, J.; Wallace, J. A scoping review of simulation-based dental education. MedEdPublish 2020, 9, 1–14. [Google Scholar] [CrossRef]
- Gali, S.; Patil, A. The Technology of Haptics in Dental Education. J. Dent. Orofac. Res. 2018, 14, 70–75. [Google Scholar]
- Dutã, M.; Amariei, C.I.; Bogdan, C.M.; Popovici, D.M.; Ionescu, N.; Nuca, C.I. An overview of virtual and augmented reality in dental education. Oral. Health Dent. Manag. 2011, 10, 42–49. [Google Scholar]
- Roy, E.; Bakr, M.M.; George, R. The need for virtual reality simulators in dental education: A review. Saudi Dent. J. 2017, 29, 41–47. [Google Scholar] [CrossRef]
- Luciano, C.; Banerjee, P.; DeFenti, T. Haptics-based virtual reality periodontal training simulator. Virtual Real. 2009, 13, 69–85. [Google Scholar] [CrossRef]
- Kim, B.; Yang, E.; Choi, N.; Kim, S.; Ryu, J. Effects of auditory feedback and task difficulty on the cognitive load and virtual presence in a virtual reality dental simulation. J. Korean Dental Assoc. 2020, 58, 670–682. [Google Scholar]
- Ben-Gal, G.; Weiss, E.I.; Gafni, N.; Ziv, A. Testing manual dexterity using a virtual reality simulator: Reliability and validity. Eur. J. Dent. Educ. 2013, 17, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Hattori, A.; Tonami, K.; Tsuruta, J.; Hideshima, M.; Kimura, Y.; Nitta, H.; Araki, K. Effect of the haptic 3D virtual reality dental training simulator on assessment of tooth preparation. J. Dent. Sci. 2021. [Google Scholar] [CrossRef]
- Dixon, J.; Towers, A.; Martin, N.; Field, J. Re-defining the virtual reality dental simulator: Demonstrating concurrent validity of clinically relevant assessment and feedback. Eur. J. Dent. Educ. 2021, 25, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, J.A. Use of simulation technology in dental education. J. Dent. Educ. 2001, 65, 1225–1231. [Google Scholar] [CrossRef] [PubMed]
- Urbankova, A.; Engebretson, S.P. The use of haptics to predict preclinic operative dentistry performance and perceptual ability. J. Dent. Educ. 2011, 75, 1548–1557. [Google Scholar] [CrossRef]
- Jasinevicius, T.R.; Landers, M.; Nelson, S.; Urbankova, A. An Evaluation of Two Dental Simulation Systems: Virtual Reality versus Contemporary Non-Computer-Assisted. J. Dent. Educ. 2004, 68, 1151–1162. [Google Scholar] [CrossRef]
- Evans, A.W. Assessing competence in surgical dentistry. Br. Dent. J. 2001, 190, 343–346. [Google Scholar] [CrossRef] [PubMed]
- Massie, T.H.; Salisbury, J.K. The phantom haptic interface: A device for probing virtual objects. In Proceedings of the ASME Winter Annual Meeting, Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systems, Chicago, IL, USA, 20 November 1994; Volume 55, pp. 295–300. [Google Scholar]
- Kikuchi, M. The Japanese system of dental clinical training. Prosthodont. Res. Pract. 2007, 6, 78–80. [Google Scholar] [CrossRef][Green Version]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S173–S182. [Google Scholar] [CrossRef] [PubMed]
- Hefti, A.F. Periodontal probing. Crit. Rev. Oral Biol. Med. 1997, 8, 336–356. [Google Scholar] [CrossRef] [PubMed]
- Gerber, J.A.; Tan, W.C.; Balmer, T.E.; Salvi, G.E.; Lang, N.P. Bleeding on probing and pocket probing depth in relation to probing pressure and mucosal health around oral implants. Clin. Oral Implants Res. 2009, 20, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, A.D.; Bashook, P.G.; Drummond, J.; Ashrafi, S.; Zefran, M. Assessment of faculty perception of content validity of Periosim©, a haptic-3D virtual reality dental training simulator. J. Dent. Educ. 2007, 71, 1574–1582. [Google Scholar] [CrossRef] [PubMed]
- Kolesnikov, M.; Žefran, M.; Steinberg, A.D.; Bashook, P.G. PerioSim: Haptic virtual reality simulator for sensorimotor skill acquisition in dentistry. In Proceedings of the IEEE International Conference on Robotics and Automation, Kobe, Japan, 12–17 May 2009; pp. 689–694. [Google Scholar]
- Yamaguchi, S.; Yoshida, Y.; Noborio, H.; Murakami, S.; Imazato, S. The usefulness of a haptic virtual reality simulator with repetitive training to teach caries removal and periodontal pocket probing skills. Dent. Mater. J. 2013, 32, 847–852. [Google Scholar] [CrossRef]
- Wang, D.; Zhang, Y.; Hou, J.; Wang, Y.; Lv, P.; Chen, Y.; Zhao, H. iDental: A haptic-based dental simulator and its preliminary user evaluation. IEEE Trans. Haptics 2011, 5, 332–343. [Google Scholar] [CrossRef]
- Rees, J.S.; Jenkins, S.M.; James, T.; Dummer, P.M.; Bryant, S.; Hayes, S.J.; Oliver, S.; Stone, D.; Fenton, C. An initial evaluation of virtual reality simulation in teaching pre-clinical operative dentistry in a UK setting. Eur. J. Prosthodont. Restor. Dent. 2007, 15, 89–92. [Google Scholar]
- Welka, A.; Splietha, C.; Wierinckc, E.; Gilpatrickd, R.O.; Meyera, G. Computer-assisted Learning and Simulation Systems in Dentistry–A Challenge to Society. Int. J. Comput. Dent. 2006, 9, 253–265. [Google Scholar]
- Robinson, P.B.; Lee, J.W. The use of real time video magnification for the pre-clinical teaching of crown preparations. Br. Dent. J. 2001, 190, 506–510. [Google Scholar] [CrossRef][Green Version]
- Norman, G.T.; Schmidt, H.G. The psychological basis of problem-based learning: A review of the evidence. Acad. Med. 1992, 67, 557–565. [Google Scholar] [CrossRef]
- Quinn, F.; Keogh, P.; McDonald, A.; Hussey, D. A pilot study comparing the effectiveness of conventional training and virtual reality simulation in the skills acquisition of junior dental students. Eur. J. Dent. Educ. 2003, 7, 13–19. [Google Scholar] [CrossRef]
- Germans, D.M.; Spoelder, H.J.W.; Renambot, L.; Bal, H.E.; van Daatselaar, S.; van der Stelt, P. Measuring in virtual reality: A case study in dentistry. IEEE Trans. Instrum. Meas. 2008, 57, 1177–1184. [Google Scholar] [CrossRef]
- Suebnukarn, S.; Hataidechadusadee, R.; Suwannasri, N.; Suprasert, N.; Rhienmora, P.; Haddawy, P. Access cavity preparation training using haptic virtual reality and microcomputed tomography tooth models. Int. Endod. J. 2011, 44, 983–989. [Google Scholar] [CrossRef]
- Toosi, A.; Arbabtafti, M.; Richardson, B. Virtual reality haptic simulation of root canal therapy. In Applied Mechanics and Materials; Trans Tech Publications, Ltd.: Freynbach, Switzerland, 2014; Volume 666, pp. 388–392. [Google Scholar]
- Suebnukarn, S.; Chaisombat, M.; Kongpunwijit, T.; Rhienmora, P. Construct validity and expert benchmarking of the haptic virtual reality dental simulator. J. Dent. Educ. 2014, 78, 1442–1450. [Google Scholar] [CrossRef] [PubMed]
- Suebnukarn, S.; Haddawy, P.; Rhienmora, P.; Gajananan, K. Haptic Virtual Reality for Skill Acquisition in Endodontics. J. Endod. 2010, 36, 53–55. [Google Scholar] [CrossRef]
- Reymus, M.; Liebermann, A.; Diegritz, C. Virtual reality: An effective tool for teaching root canal anatomy to undergraduate dental students—A preliminary study. Int. Endod. J. 2020, 53, 1581–1587. [Google Scholar] [CrossRef]
- Wang, D.; Zhao, X.; Shi, Y.; Zhang, Y.; Hou, J.; Xiao, J. Six degree-of-freedom haptic simulation of probing dental caries within a narrow oral cavity. IEEE Trans. Haptics 2016, 9, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Osnes, C.; Keeling, A.J. Developing haptic caries simulation for dental education. J. Surg. Simul. 2017, 4, 29–34. [Google Scholar] [CrossRef]
- Holzinger, D.; Juergens, P.; Shahim, K.; Reyes, M.; Schicho, K.; Millesi, G.; Perisanidis, C.; Zeilhofer, H.F.; Seemann, R. Accuracy of soft tissue prediction in surgery-first treatment concept in orthognathic surgery: A prospective study. J. Cranio-Maxillofac. Surg. 2018, 46, 1455–1460. [Google Scholar] [CrossRef]
- Metzler, P.; Geiger, E.J.; Alcon, A.; Ma, X.; Steinbacher, D.M. Three-dimensional virtual surgery accuracy for free fibula mandibular reconstruction: Planned versus actual results. J. Oral Maxillofac. Surg. 2014, 72, 2601–2612. [Google Scholar] [CrossRef]
- D’Souza, K.M.; Aras, M.A. Types of implant surgical guides in dentistry: A review. J. Oral Implantol. 2012, 38, 643–652. [Google Scholar] [CrossRef]
- Gulati, M.; Anand, V.; Salaria, S.K.; Jain, N.; Gupta, S. Computerized implant-dentistry: Advances toward automation. J. Indian Soc. Periodontol. 2015, 19, 5. [Google Scholar] [CrossRef] [PubMed]
- Holst, S.; Blatz, M.B.; Eitner, S. Precision for computer-guided implant placement: Using 3D planning software and fixed intraoral reference points. J. Oral Maxillofac. Surg. 2007, 65, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Verstreken, K.; Van Cleynenbreugel, J.; Martens, K.; Marchal, G.; van Steenberghe, D.; Suetens, P. An image-guided planning system for endosseous oral implants. IEEE Trans. Med. Imaging 1998, 17, 842–852. [Google Scholar] [CrossRef]
- Tardieu, P.B.; Vrielinck, L.; Escolano, E. Computer-assisted implant placement. A case report: Treatment of the mandible. Int. J. Oral Maxillofac. Implants 2003, 18, 599–604. [Google Scholar]
- Sarment, D.P.; Sukovic, P.; Clinthorne, N. Accuracy of implant placement with a stereolithographic surgical guide. Int. J. Oral Maxillofac. Implants 2003, 18, 571–577. [Google Scholar]
- Pflesser, B.; Petersik, A.; Tiede, U.; Höhne, K.H.; Leuwer, R. Volume cutting for virtual petrous bone surgery. Comput. Aided Surg. 2002, 7, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Rhienmora, P.; Haddawy, P.; Suebnukarn, S.; Dailey, M.N. A VR environment for assessing dental surgical expertise. In Frontiers in Artificial Intelligence and Applications; IOS Press: Amsterdam, The Netherlands, 2009; Volume 200, pp. 746–748. [Google Scholar]
- Kusumoto, N.; Sohmura, T.; Yamada, S.; Wakabayashi, K.; Nakamura, T.; Yatani, H. Application of virtual reality force feedback haptic device for oral implant surgery. Clin. Oral Implants Res. 2006, 17, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Schendel, S.; Montgomery, K.; Sorokin, A.; Lionetti, G. A surgical simulator for planning and performing repair of cleft lips. J. Cranio-Maxillofac. Surg. 2005, 33, 223–228. [Google Scholar] [CrossRef]
- Chang, H.-W.; Lin, H.-H.; Chortrakarnkij, P.; Kim, S.G.; Lo, L.-J. Intraoperative navigation for single-splint two-jaw orthognathic surgery: From model to actual surgery. J. Cranio-Maxillofac. Surg. 2015, 43, 1119–1126. [Google Scholar] [CrossRef]
- Yu, H.; Shen, S.G.; Wang, X.; Zhang, L.; Zhang, S. The indication and application of computer-assisted navigation in oral and maxillofacial surgery—Shanghai’s experience based on 104 cases. J. Cranio-Maxillofac. Surg. 2013, 41, 770–774. [Google Scholar] [CrossRef]
- Heiland, M.; Petersik, A.; Pflesser, B.; Tiede, U.; Schmelzle, R.; Höhne, K.-H.; Handels, H. Realistic haptic interaction for computer simulation of dental surgery. Int. Congr. Ser. 2004, 1268, 1226–1229. [Google Scholar] [CrossRef]
- Ioannou, I.; Kazmierczak, E.; Stern, L. Comparison of oral surgery task performance in a virtual reality surgical simulator and an animal model using objective measures. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 5114–5117. [Google Scholar] [CrossRef]
- Wang, D.; Tong, H.; Shi, Y.; Zhang, Y. Interactive haptic simulation of tooth extraction by a constraint-based haptic rendering approach. In Proceedings of the 2015 IEEE International Conference on Robotics and Automation (ICRA), Seattle, WA, USA, 26–30 May 2015; pp. 278–284. [Google Scholar] [CrossRef]
- Joseph, D.; Jehl, J.-P.; Maureira, P.; Perrenot, C.; Miller, N.; Bravetti, P.; Ambrosini, P.; Tran, N. Relative contribution of haptic technology to assessment and training in implantology. Biomed Res. Int. 2014, 2014, 413951. [Google Scholar] [CrossRef]
- Ogawa, T.; Ikawa, T.; Shigeta, Y.; Kasama, S.; Ando, E.; Fukushima, S.; Hattori, A.; Suzuki, N. Virtual reality image applications for treatment planning in prosthodontic dentistry. In Medicine Meets Virtual Reality 18: NextMed; IOS Press: Amsterdam, The Netherlands, 2011; Volume 163, pp. 422–424. [Google Scholar]
- Suebnukarn, S.; Phatthanasathiankul, N.; Sombatweroje, S.; Rhienmora, P.; Haddawy, P. Process and outcome measures of expert/novice performance on a haptic virtual reality system. J. Dent. 2009, 37, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, H.; Ikeda, M.; Araki, K. Evaluation of a virtual reality simulation system for porcelain fused to metal crown preparation at Tokyo Medical and Dental University. J. Dent. Educ. 2013, 77, 782–792. [Google Scholar] [CrossRef]
- Feeney, L.; Reynolds, P.A.; Eaton, K.A.; Harper, J. A description of the new technologies used in transforming dental education. Br. Dent. J. 2008, 204, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Esser, C.; Kerschbaum, T.; Winkelmann, V.; Krage, T.; Faber, F. A comparison of the visual and technical assessment of preparations made by dental students. Eur. J. Dent. Educ. 2006, 10, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Rhienmora, P.; Haddawy, P.; Khanal, P.; Suebnukarn, S.; Dailey, M.N. A virtual reality simulator for teaching and evaluating dental procedures. Methods Inf. Med. 2010, 49, 396–405. [Google Scholar] [CrossRef]
- de Boer, I.R.; Wesselink, P.R.; Vervoorn, J.M. Student performance and appreciation using 3D vs. 2D vision in a virtual learning environment. Eur. J. Dent. Educ. 2016, 20, 142–147. [Google Scholar] [CrossRef] [PubMed]

| Devices | PerioSim® | Voxel Man | DentSim™ | IDEA Simulation | Simodont® | SIMtoCARE | Virteasy Dental © |
|---|---|---|---|---|---|---|---|
| Software used | Modified version of GhostTM (SensAble Technologies, MA) Coin3D software Fast Light ToolKit (FLTK) | VOXEL-MAN Dental (University Medical Centre Hamburg- Eppendorf, Hamburg, Germany) | DentSim™ software Tracking software Proprietary tracking cards Proprietary interface card to A- Dec hardware (Image Navigation Ltd.’s, NY, USA) | Manual DexterityTM, Caries Detection, Scaling & Root- PlanningTM, OralMedTM and PreDenTouchTM (IDEA Dental, Las Vegas, NV, USA) | Nissin Simodont Dental Trainer Courseware software (Nissin B.V., Nieuw-Vennep, ND) | SIMtoCARE B.V. SIMtoCARE student App. Case editor application. Reporting in MS Excel on Teacher station. Supports many procedures: manual dexterity, operative dentistry, prosthodontics, endo access to the root cavity, implantology, periodontics. | HRV Simulation Virteasy Dental—Simulation software capable of 3D and full VR. Virteasy Editor—Exercise management and creation. Virteasy Assistant—Data management tool for progress tracking, student feedback and grading. |
| Hardware specifications | Two computer monitors with haptic device Crystal Eyes Stereo GlassesTM and a Crystal Eyes WorkstationTM (Stereo Graphics Corp.TM, San Rafael, CA) used for 3D viewing APHANToMTM haptic device from SensAble TechnologiesTM (SensAble Technologies, MA) with 3-degrees of freedom VR William’s periodontal probe (Hu-FriedyTM, Chicago, IL) or periodontal explorer (Hu-Friedy) | Workstation computer, 3D LCD monitor, 3D glasses, force feedback device, and a space navigator Similar to the Phantom device used in IDEA | The A-dec patient manikin used in conjunction with DentSim™ Pentium IV PC 2.66 GHz with 512 MB RAM | A stylus, with six degrees of freedom, attached to a stand (Phantom Omni, Sensable Technologies, Wilmington, MA, USA) | Two projectors Panel Pc 3D glasses Handpiece connected to force feedback sensors, mirror measured in 6 DOF with limited range. | 4K autostereo screen (3D) No need for 3D glasses Integrated iPad Handpiece and mirror with large working range. Handpiece connected to force feedback sensors Finger support for upper and lower jaw | Fully integrated simulator with two HD screens. No need for 3D glasses. Oculus VR headset (optional use). 3D printable and customisable finger rest. High fidelity haptic device with weighted metal dental handpiece and 6 DOF movement. Electromagnetic tracking device for dental mirror. 3D mouse. |
| Use external camera | No | No | Yes, Dual CCD IR tracking camera | No | No | No | No—Navigation screen is equipped with a camera for future functionality. |
| Ergonomic postures | No | No | Yes | No | Yes | Yes (height adjustable) | Yes & height adjustable |
| Instant feedbacks | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Exam simulation | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Wi-fi | No | No | No | No | No | Yes (optional, wired is standard) | Yes (optional use) |
| Direct transfer of data to programme convenor/tutor | Not available | Not available | Yes Run-time control application enables the instructor to control run-time grades | Yes The software contains a replay mode. Upon completion of a specified task, it can be watched in full by the student or the instructor | Yes The teacher station allows instructor to watch six simulators live at once and record all preparations for evaluation and giving feedback later | Yes Remote viewing of the iPad and simulator view of all simulators simultaneously. | Yes—through Virteasy Assistant. |
| Teeth used | Animated | Animated | Plastic teeth | Animated | Animated | Animated (virtual reality mixed with reality) | Animated—from micro-CT scans |
| Right and left operation | Available | Available | Available | Available | Available | Available | Available |
| Ability to use off campus | Possible | Possible | Not possible | Possible | Not possible | Possible (with additional server) | Yes |
| Reported real life experience | Tactile sensation is realistic for teeth and not so for gingiva [11]. | N/A | Realistic experience using plastic teeth on a real manikin [12]. | Tactile sensation still needs to be tuned to simulate a genuine sensation [13]. | 3D images are realistic. However, the texture of healthy decayed and restored tooth structure still needs improvement [14]. | Latest technology with high resolution realistic 3D models in auto stereo and mixed with the real view of the hands and finger support (mixed reality). | The results of this study demonstrate that it is possible to provide reliable and clinically relevant qualitative feedback via a VR dental simulator [15]. |
| Author | Scope | Sample Size | Main Findings | Conclusion | Future Recommendations | Limitations |
|---|---|---|---|---|---|---|
| Yamag Uchi et al. [27] | Caries removal and periodontal probing skills were assessed, using haptic virtual reality simulator. | Caries removal: 7 Periodontal pocket probing task: 26 | Significantly higher training scores were obtained after the first training session. | In-contrast to a conventional stimulator, a VR simulator can be used for multiple purposes and can be utilized as a training tool for efficient evaluation within a short period of time. | Scores for cutting should also be incorporated for future training evaluations | The simulator failed to replicate an exact clinical environment, use of hand instruments, electric engine and tools with cutting properties should be incorporated. Moreover, for a more realistic approach, soft tissues and face models should be developed. |
| Steinberg et al. [25] | Perio-sim was developed, using haptic technology and VR graphics | 30 | Highly realistic graphics were formed for teeth in contrast to the gingiva. However, Periosim® can serve well to evaluate basic skills | Periosim® can be a valuable tool to develop tactile skills in students | A significantly greater realistic touch for gingiva and the addition of a sound system is highly recommended. A six-degree freedom unit should be established. Furthermore, students trained with Periosim® should be contrasted with learners, trained with conventional methods to evaluate the efficiency of the system. | Few defects in terms of stiffness and deformability were observed in graphs, thus the exact difference between the tooth and gingiva couldn’t be evaluated. Collision with the lateral aspect of the device couldn’t be evaluated due to the “three-degree freedom” nature of the system. |
| Koesni kov et al. [26] | Development of a haptic simulator for investigation of sensorimotor skills | 30 | Models, demonstrating force and position pathways were developed along with a haptic playback system | The simulator proved to be a useful tool as it could record the procedure performed by the facilitator while the trainees could easily follow the force and position pathways formed by the teacher. | For future investigations more complex features for a more realistic approach needs to be incorporated such as gingival tactile feel. | The gingival tactile feel could not be evaluated. The system lacked complex effects. |
| Wang et al. [28] | Development of iDental simulator for quantitative and qualitative analysis | 29 | The simulator was able to sustain construct validity, thus differentiating students from experts | Bimanual coordination could be practiced using this haptic feedback system and the results could be evaluated quantitatively and qualitatively. | 3-DOF model designed, led to penetration of probe into the gingiva and tooth thus incorporation of a 6DOF model would give more reliable results. | Users gave rough readings at points where the occlusion was serious such as central lingual point of the tooth. |
| Author | Year | Scope | Sample Size | Main Findings | Conclusion | Future Recommendations | Limitations |
|---|---|---|---|---|---|---|---|
| Desmond [34] | 2008 | Quantitative measurement of the length of the root canal using VR | 7 | A novel method for the measurement of the length of a root canal was introduced, which was safer in terms of radiation and gave more accurate results in contrast to traditional X-ray method. | Measurements using VR technology gave results for complex cases and was proved to be economical and more accurate as compared to classical methods. | For future studies, a more realistic environment such as a phantom head or real patients is preferred as compared to the separate teeth used in this experiment. Collaborative work with peer discussions is highly recommended. The calibration process can be improved in future studies by performing usability analysis | Separate teeth on an optical bench were used, thus a realistic environment could not be provided. |
| Suebnukarn [35] | 2010 | kinematic information concerned with movement was investigated using VR | 32 | Increased performance in skills and retention sessions was observed. | The system proposed had the ability to record student’s performance related to kinematic data. | A more realistic environment should be provided and transfer of motor skills from a virtual setting to the patient would serve well in a patient’s interest. | In the present study, a computer screen was the only mode of interaction available between the virtual tooth and tool, thus visual hand alignment with the simulated tool would be an advantage for future research. |
| Toosi [36] | 2015 | Virtual jaw model was obtained from CT data of a live patient and VR simulator was utilized for root canal treatment. | Not mentioned | K-files from the internal tooth surface could be haptically simulated. Beam deflection model was utilized to simulate K-file deflection. Marching cube’s methodology visualized bone removal. Furthermore, to solve the beam model, Runge-Kutta’s method was used | A VR method was proposed, which used Phantom haptic models to clean internal tooth surface using simulated K-files to bur enamel and dentin. | Need of more work on this technology for expanding more endodontic procedures via this system. | N/A |
| Suebnukarn [37] | 2014 | Skills were assessed using VR simulator | 34 | Fortified on quantitative analysis, a competency criterion was proposed which proved that with repeated practice on simulators, students can augment their skills | VR simulator can be used as an invaluable tool for training dental students and differentiate the capabilities of expert practitioners with students. | The model should also evaluate the learning capabilities of students in a real clinical environment. | The model lacked a more realistic approach. |
| Suebnukarn [38] | 2010 | Assessment of endodontic skills | 20 | Improved skills in post-trained students were observed in terms of force pattern and coordination. | Haptic VR technology used in the study, proved that students learnt faster and had a better knowledge related to force and bimanual dexterity. | Transferability knowledge from VR setting to the clinical environment would be beneficial for future research purposes. | Students were not accessed in a proper clinical setting; thus, the exact transferability knowledge could not be evaluated. |
| Suebnukarn [35] | 2011 | To minimize access preparation errors, micro-CT tooth models were utilized to investigate the effectiveness of VR simulators. | 32 | Equivalent results to reduce procedural errors was observed when VR simulators were compared with phantom heads. | Micro-CT models of teeth along with VR simulators is a valuable tool for skill development in endodontics. | Skills of VR operators should also be evaluated in a clinical setting. | Skills acquired, were not evaluated in a clinical setting. |
| Reymus [39] | 2020 | An economical method using VR technology was used to teach third-year operative students. | 42 | VR simulators were reported to be equally good in contrast to CBCT and more beneficial as compared to radiography for detection of anatomical features of root canals. | Integration of VR simulators was highly appreciated | The performance of students after each technique should be evaluated in a randomized manner. Students should be divided into groups and to reduce biasness, the investigator should ensure that they don’t have any prior knowledge | Student’s performance after each method would have given a better evaluation of each proposed method. |
| Wang [40] | 2016 | For exploration and diagnosis of carious lesions, an approach was introduced using 6DOF haptic interaction. | 5 | Stable simulation of varying levels of decay was possible using this approach. | The proposed method simulated different tissues, depth and surface roughness of caries and can be used to train dental students for their motor skills. | Evaluation of skill transfer from the simulation to a real clinical setting would be an advantage. | The study lacked evaluation in a real clinical setting. |
| Cecilie Osnes [41] | 2017 | Moog Simodont Dental trainer was developed to teach caries removal and cavity design to dental students. | A novel, caries simulation approach was introduced, students were able to practice caries removal, predominantly its tactile and cognitive aspects in a safe environment. | Students were able to prepare a cavity and use correct instruments during each phase. Secondly, they were able to learn the clinical protocols for treating a lesion and preserving healthy tissues. | Evaluation of construct validity and investigate caries algorithm. Secondly precise, simulation of the probe is important. | The simulator was not able to simulate a dental probe, thus correct movements for identifying caries could not be evaluated. |
| Authors | Year | Scope | Sample Size | Main Findings | Conclusion | Recommendations | Limitations |
|---|---|---|---|---|---|---|---|
| Heiland [56] | 2004 | Establishment of a simulator which provided realistic haptic manifestation of structures and with its haptic sensation ability could simulate bone reduction. | 40 | A sagittal, coronal and axial drilling route was accessible during the procedure. | The system opened possibilities for realistic simulations of complex structures. | Incorporation of soft tissue simulations. Inclusion of other complicated procedures such as molar impactions. Incorporation of CBCT technology for the investigation of oral pathologies | The system lacked a realistic approach |
| Ioannou [57] | 2015 | Investigating the effects of integrating VR technology in surgical training in contrast to ovine jaws. | 14 | Performance of trainees was improved after being trained by the simulator. | Comparison of both techniques utilized gave the same results, however, they did not simulate with a real clinical environment. | Effects of VR on different parameters would be an advantage, using larger sample size and longer time period. | Accuracy of simulator’s drilling algorithm was questionable. |
| Wang [58] | 2015 | A haptic simulation model was proposed to train dental students for tooth extractions | The 6-DoF haptic system introduced simulated tooth extraction with a variety of force-displacement forms and proved to be a valuable tool for training students to identify the pattern of force applied and correct posture of the tool used. | The simulator gave promising results to train dental students for coordinated force and motion skills. | Incorporation of torque feedback in the system to create a more realistic environment. | The system lacked a realistic touch. Moreover, the magnitude and stiffness of the system were not appropriate, thus sudden changes could not be simulated. | |
| Joseph [59] | 2014 | Determine the effectiveness of a simulator for evaluating gestural abilities for implant surgery. | 60 | When the two groups were compared, the simulator trained group gave equally good results and proved to be a beneficial tool for implant training. | Simulator trained 3rd-year dental students gave a better performance in contrast to students who were not trained before. | Evaluation of more complex cases | Simulator lacked the ability to simulate complex situations. |
| Authors | Year | Scope | Sample Size | Main Findings | Conclusion | Recommendations | Limitations |
|---|---|---|---|---|---|---|---|
| Kikuchi et al. [62] | 2012 | Access and compare the influence of VRS (Dentsim™) on student’s crown (porcelain fused to metal (PFM)) preparation skills with and without instructor’s feedback. | 43 | A non-significant difference between the two groups was obtained when the students of the two groups were evaluated for their crown preparation skills. | Students trained with VRS gave the same results when compared with the group of students trained by the instructor, therefore the presence of an instructor does not matter and can be substituted with virtual simulators. Secondly, VRS was less time-consuming. | DentSim proved to be an effective virtual simulator for PFM crown preparation. | Instructors did not provide feedback contents since the evaluation criteria were not given any consideration. |
| Suebnukarn et al. [61] | 2009 | Compared the performance scores for crown preparation between experts and novices using VR simulation with force feedback. | 20 | Haptic VR system with force feedback can be used to differentiate the performance learners and experts. | The investigated parameters which include force, time and instrument angulation correctly evaluated the clinical skills between the two groups. | Incorporation of VR in dental education would allow standardized evaluation of clinical performance. | The clinical parameters evaluated did not provide immediate feedback, therefore for future research, techniques involving artificial intelligence models are highly recommended. |
| Rhienmora et al. [65] | 2010 | An intelligent tutor demonstrates dental procedures, therefore allowing students to learn and practice the procedures in a virtual training environment. The training module used has an ability to record and replay the procedures, thus allowing students to correctly follow the steps for crown cutting and reproduce the procedure. | The accuracy of the performance assessment was found to have 100% accuracy. | The virtual reality simulator was able to simulate realistic tooth surface and cutting. | A wide assortment of training strategies can be incorporated in the curriculum using this VR simulator, therefore creating opportunities to differentiate between the performance of the operator as a novice or expert. | In a few scenarios, the tooth surface was found to be too rough, therefore force shading algorithm along with its variants needs further investigations. Students faced navigation troubles in the new virtual environment. The system presented in this study was not able to simulate complex dental procedures which | |
| G. Ben-Gal [13] | 2012 | Evaluation of manual dexterity, using a haptic simulator (IDEA), Testing parameters included: completion time, number of successful trials, accuracy and scores | 106 | High reliability of the simulator was observed for all the parameters and consistent results were obtained. Scores for human-based judgement were lower in contrast to the results of this study. | For the parameters tested, the simulator proved to be a valuable tool for assessment, however, the simulator was not able to accurately differentiate between the performances students are trained, dental practitioners. | To increase the sensitivity of the system, adaptations to increase the validity would be helpful to increase the differentiation capacity. | The system lacked the capacity to differentiate between the experts and learners. |
| I. R. de Boer [66] | 2015 | The difference in the performance of students, working in two types of the virtual environment (2D and 3D) was evaluated using Simodont dental trainer | 124 | Students trained in 3D environment performed significantly better in contrast to those working in 2D. | In a virtual training environment, 3D vision proved to be a valuable tool and first choice of preference for the majority of students. | Point of view of experienced professionals should also be considered. | The study did not investigate the results of experts and no comparison of results between novice and experts was drawn. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Imran, E.; Adanir, N.; Khurshid, Z. Significance of Haptic and Virtual Reality Simulation (VRS) in the Dental Education: A Review of Literature. Appl. Sci. 2021, 11, 10196. https://doi.org/10.3390/app112110196
Imran E, Adanir N, Khurshid Z. Significance of Haptic and Virtual Reality Simulation (VRS) in the Dental Education: A Review of Literature. Applied Sciences. 2021; 11(21):10196. https://doi.org/10.3390/app112110196
Chicago/Turabian StyleImran, Eisha, Necdet Adanir, and Zohaib Khurshid. 2021. "Significance of Haptic and Virtual Reality Simulation (VRS) in the Dental Education: A Review of Literature" Applied Sciences 11, no. 21: 10196. https://doi.org/10.3390/app112110196
APA StyleImran, E., Adanir, N., & Khurshid, Z. (2021). Significance of Haptic and Virtual Reality Simulation (VRS) in the Dental Education: A Review of Literature. Applied Sciences, 11(21), 10196. https://doi.org/10.3390/app112110196