Abstract
The presence of microbial biofilms in the wounds affects negatively the healing process and can contribute to therapeutic failures. This study aimed to establish the effective parameters of cold atmospheric plasma (CAP) against wound-related multispecies and monospecies biofilms, and to evaluate the cytotoxicity and genotoxicity of the protocol. Monospecies and multispecies biofilms were formed by methicillin-resistant Staphylococcus aureus (MRSA), Pseudomonas aeruginosa and Enterococcus faecalis. The monospecies biofilms were grown in 96 wells plates and multispecies biofilm were formed on collagen membranes. The biofilms were exposed to helium CAP for 1, 3, 5 and 7 min. In monospecies biofilms, the inhibitory effect was detected after 1 min of exposure for E. faecalis and after 3 min for MRSA. A reduction in P. aeruginosa biofilm’s viability was detected after 7 min of exposure. For the multispecies biofilms, the reduction in the overall viability was detected after 5 min of exposure to CAP. Additionally, cytotoxicity and genotoxicity were evaluated by MTT assay and static cytometry, respectively. CAP showed low cytotoxicity and no genotoxicity to mouse fibroblastic cell line (3T3). It could be concluded that He-CAP showed inhibitory effect on wound-related multispecies biofilms, with low cytotoxicity and genotoxicity to mammalian cells. These findings point out the potential application of CAP in wound care.
1. Introduction
Chronic wounds, such as venous ulcers, diabetic foot ulcers, and pressure ulcers, are considered one of the most challenging problems in the medical area and affect millions of patients worldwide [1,2]. The prevalence of chronic wounds is estimated in 2.21 per 1000 in the population [3] and these rates tend to rise due to the ageing population and increasing prevalence of obesity and associated conditions, such as diabetes and cardiovascular diseases [4]. This condition has significant economic impact on health systems [2,5], with 2 to 3% of the budget in health applied in the treatment of chronic wounds in developed countries [1].
Microbial biofilms significantly affect wound healing and can contribute to therapeutic failures [6]. For these reasons, they have emerged as an important topic of discussion in the treatment of wounds [7]. The infections of wounds are usually polymicrobial, as their microenvironment is favorable for microbial growth [8,9]. Despite this, previous evidence showed that species diversity in infected wounds is relatively low. It has been reported that Staphylococcus aureus, Enterococcus faecalis and Pseudomonas aeruginosa are the most prevalent species [4,10], with occurrence of 93.5%, 71.7% and 52.2%, respectively [11]. Other bacterial species, such as Proteus mirabilis, Klebsiella pneumoniae and Escherichia coli were also isolated from wounds [12,13]. The increasing rates of antimicrobial resistance also contributes to the unfavorable scenario [14,15].
Thus, the control of the microbial biofilms is considered critical to the success of wound healing [7,16]. The conventional therapeutic alternatives are focused on the reduction or eradication of biofilms by using debridement techniques and treatments with negative pressure or ultrasound [17,18]. Other methods include the use of wound dressing impregnated with antimicrobial substances or compounds, such as gentian violet and methylene blue [15], honey [19], Aloe vera [20], nitric oxide releasing polymer [21], polyhexamethylene-biguanides [22] and ethylenediamine tetra acetic acid (EDTA) [23]. However, there is still need for alternatives to wound care, in particular, focusing on biofilm control [17,21,24].
Cold atmospheric plasma (CAP) has emerged as an attractive alternative approach to the biofilm control and is considered a rapid, environmental-friendly, energy saving, and versatile technology [25,26]. Plasma is described as the fourth state of matter and is usually generated from a gaseous precursor in which a high electric field is applied, producing an electric discharge [27]. Plasma is a complex mixture composed of ions, reactive radicals, neutral particles, molecules and electrons, as well as excited species and energetic photons [28,29]. These plasma components can damage cell structures, such as lipids, protein and DNA, and increase the levels of intracellular reactive species [30]. Thus, the biological activity of plasma is a product of synergetic action of several factors, such as neutral reactive species (oxygen reactive species—ROS, reactive nitrogen species—RNS) and UV radiation [31]. The anti-inflammatory and tissue repair inducing [32,33] effects have been considered highly promising for the treatment of several diseases.
The efficiency of CAP against the bacterial biofilms has been reported in the literature [34]. CAP was able to reduce the viability of monospecies biofilms of methicillin resistant S. aureus (MRSA) [35], P. aeruginosa [36] and E. faecalis [37]. Monospecies biofilms formed by E. faecalis [38,39] or Escherichia coli [40] were also inhibited by CAP. One of the main advantages of CAP when compared to conventional antibiotics is that the development of treatment resistance was not detected so far. Repeated exposure to CAP did not induce resistance in S. aureus [41]. The hypothesis is that as CAP does not have specific target structures [35], the chance of resistance development with plasma is lower since several targets are activated and not a specific one [42]. Besides the antimicrobial activity, anti-inflammatory and tissue repair inducing effects (stimulating cellular proliferation and migration and the pro-angiogenic effects) of CAP have been also reported [14,32,43,44].
The biological effects of CAP lead to the hypothesis that this technology can be useful for the treatment of infected wounds. However, to the best of our knowledge, little is known on the effects of CAP on wound-related multispecies biofilms. Thus, the present work aimed to study the effect of He-CAP on wound-related multispecies biofilms and confirm the safety of the protocol.
2. Materials and Methods
2.1. Plasma Jet Device
The plasma jet device used in this study consists of a plasma reactor with dielectric barrier discharge (DBD) configuration. The plasma generated in this primary DBD reactor is transported through a 1.0-m-long, flexible polyurethane tube (Kangaroo TM Nasogastric Feeding Tube, 10 Fr/Ch), connected to the reactor exit. A thin metal wire is installed inside the plastic tube acting as floating electrode. The wire penetrates few millimeters inside the primary discharge chamber, crosses the whole tube length and terminates about 2 mm before the plastic tube exit. When high voltage is applied to the primary DBD reactor, a remote plasma plume is ignited at the downstream end of the plastic tube. This device was already described in previous works [45,46,47,48]. In the present study, the reactor was connected to a Minipuls4 AC power supply (GBS Elektronik GmbH, Radeberg, Germany) and an amplitude modulated voltage signal (12 kV amplitude) with voltage duty cycle of 22% was employed. The system was fed with helium (99.5% purity) at a flow rate of 2.0 slm. The distance between the plastic tube tip and the surface to be treated was set at 1.5 cm.
The characteristic optical emission spectrum of this plasma jet was previously reported by Kostov et al. and Nishime et al., [45,46,47,48]. Briefly, weak emission lines of helium were detected with nitrogen emission bands being predominant in the spectrum, showing that excited nitrogen (N2-second positive system) and ionized nitrogen species (N2+-first negative system) were produced in the plasma plume. Peaks associated to atomic oxygen (777 nm and 844 nm) and the OH band at 308 nm were also present indicating the production of ROS.
2.2. Bacterial Strains and Growth Conditions
The bacterial strains used in this study were: methicillin resistant S. aureus (MRSA) (ATCC 33591), P. aeruginosa (ATCC 27853) and E. faecalis (ATCC 29212). Strains were grown in tryptic soy agar for 24 h at 37 °C, under aerobiosis. After this period, standardized suspensions containing 108 cells/mL in sterile saline solution (NaCl 0.9%) were prepared with the aid of a spectrophotometer (P. aeruginosa: λ = 600, OD 0.115; E. faecalis: λ = 760, OD 1.278 and MRSA: λ = 600, OD 0.462). Then, these suspensions were diluted in TS broth obtaining the final concentration of 106 cells/mL.
2.3. Effect of CAP on Monospecies Biofilms
Monospecies bacterial biofilms of MRSA (ATCC 33591), P. aeruginosa (ATCC 27853) and E. faecalis (ATCC 29212) were grown in 96 wells plates, as these experiments aimed to standardize the ideal parameters of plasma device in a cost-effective manner. Standardized suspension (106 cells/mL) of each strain in Tryptic soy broth (200 µL) was added to each well. Plates were incubated for 90 min at 37 °C and 80 rpm for initial adherence. After this period, the culture medium was removed, and the wells were washed twice with physiologic solution (NaCl 0.9%). Then, 200 μL of fresh Tryptic soy broth medium were added to each well and the plates were incubated for 48 h. Subsequently, the culture medium was removed, and the biofilms were washed twice with physiologic solution (NaCl 0.9%). Biofilms were exposed to CAP for 1, 3, 5 and 7 min. A non-exposed treated group was included for comparative purposes. The number of viable cells was determined after serial dilution in physiologic solution and plating on brain heart infusion agar. The results were expressed as colony forming units per mL (CFU/mL). Three independent experiments were performed in triplicate.
2.4. Effect of CAP on Multispecies Biofilms
Multispecies biofilms were formed by MRSA (ATCC 33591), P. aeruginosa (ATCC 27853) and E. faecalis (ATCC 29212) on collagen membranes (Geistlich Bio-Gide®), according to the methodology described by [49,50]. First, standardized suspensions containing 106 cells/mL in physiologic solution (NaCl 0.9%) of each microorganism were prepared spectrophotometrically, using the same parameters described before. The collagen membranes were positioned on the surface of tryptic soy agar supplemented by fetal bovine serum solution (50% fetal bovine serum and 50% NaCl 0.9% solution). The smooth layer of the collagen membrane was considered for the growth of multispecies biofilm. Then, aliquots of 10 µL of each bacterial suspension were mixed up in a microtube and the total volume was transferred to the membrane’s surface. Plates were incubated at 37 °C for 24 h. Then, the biofilms were exposed to CAP for 1, 3, 5 and 7 min. The biofilms were mechanically dispersed, and the number of viable cells was determined by plating method. The recovery of each species was carried out by plating the resuspended biofilm in selective culture media (mannitol salt agar, cetrimide agar and Enterococcosel agar, respectively). The experiments were performed in triplicate in three different experiments (n = 9). A negative control (exposed only to helium flow and without ignition) was included for comparative purposes.
2.5. Morphologic Analysis of the Biofilms by Scanning Electron Microscopy
Multispecies biofilms exposed to CAP for 1, 3, 5 and 7 min were analyzed morphologically by scanning electron microscopy. After exposure to CAP, the biofilms were prepared by standard fixation protocol 2.5% glutaraldehyde solution in 0.1 M phosphate buffer (pH 7.4) for 24 h and serial dehydration in ethanol (Synth, 99.8%), for 10 min in each concentration [51]. After 24 h under room temperature, the biofilms were metallized in gold. The specimens were analyzed by scanning electron microscopy with Field-emission gun (SEM-FEG). The analysis was performed using a Tescan Vega 3 microscope with accelerating voltage of 10 kV and magnification of 10 k×. Two fields per membrane were analyzed. The first was located at the central region of the membrane and the other at the peripheral region (approximately 2.5 mm from the center).
2.6. Cytotoxicity Evaluation
For evaluating the cytotoxicity of CAP, mouse fibroblastic cell line (3T3) were grown in DMEM (Dulbecco’s Modified Eagle’s medium) supplemented with 10% of inactivated fetal bovine serum (FBS), 100 IU mL−1 of penicillin, and 100 μg mL−1 of streptomycin. After, 200 μL of a suspension containing 3.6 × 104 cells/mL were transferred to the wells of 96-well plates. Plates were incubated for 24 h at 37 °C and in an atmosphere of 95% air and 5% CO2. After, the culture medium was removed and 30 μL of Hanks’ Balanced Salt Solution with 10 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid were added. The cells were exposed to CAP for 1, 3, 5 and 7 min using the same parameters adopted for microbiological evaluations. The cell viability was determined immediately, 24 and 48 h after plasma exposure, using the MTT colorimetric method at 570 nm. For the analyses of later effects (24 and 48 h), the culture medium was immediately added after plasma jet exposure. The experiments were performed in triplicate in two independent experiments. The results were expressed as a percentage of viable cells (%), using the number of cells grown in wells without CAP exposure as the negative control.
The morphological grading of cytotoxicity, according to [52], was: 0 (not cytotoxic)—no reduction of cell growth; 1 (slight)—only slight growth inhibition observable; 2 (mild)—not more than 50% growth inhibition; 3 (moderate)–more than 50% growth inhibition observable; 4 (severe)—nearly complete or complete destruction of the cell layers.
2.7. Genotoxicity Evaluation
Genotoxicity was evaluated by static cytometry method for cell DNA ploidy analysis. NIH-3T3 cells were cultivated according to Felisbino et al. [53], with modifications. Cells (5 × 104 cells/mL) were seeded in 96-well plates in Dulbecco Modified Eagle Medium (DMEM) supplemented with 10% inactivated bovine fetal serum and penicillin/streptomycin 1% and maintained at 37 °C and 5% CO2 for 24 h. Then, cells were washed once with Hanks’ Balanced Salt Solution (HBSS) and 50 μL of HBSS were added per well for CAP treatment. Cells were exposed to CAP for 1, 3, 5, and 7 min. A non-treated group was included for comparative purposes. After treatment, residual HBSS was aspirated, culture medium was added, and plates were maintained at 37 °C and 5% CO2 for 24 h. Cells were released from plate with trypsin, fixed in 4% formalin and transferred to glass slides. Next, slides were stained by Feulgen‘s method and covered with cover glass.
Nuclear IOD (integrated optical density) was performed through static cytometry. Images were digitalized with Olympus QColor3 camera in 400× magnification. Image analysis were performed in a Carl Zeiss image system and KS300 software (Carl Zeiss, Oberkochen, Germany) in black and white with a Feulgen filter for 570 nm wavelength. DNA index (DI) was obtained dividing resulting IOD by the mean of IOD from 20 lymphocytes used as diploid control. DI was classified as diploid (DI = 0.9–1.1), slightly aneuploid (DI = 1.2–1.4), moderated aneuploid (DI = 1.5–1.7), and severely aneuploid (DI > 1.8), based on Lima et al. [54]. IOD is equivalent but not identical to DNA content. A total of 100 cells were analyzed.
2.8. Data Analysis
Data was analyzed for normality using Shapiro Wilk test. After, data of cell viability of biofilms (CFU/mL) were compared by Kruskal Wallis followed by Dunn’s post hoc test. The values of cytotoxicity were obtained by percentage analysis. For the genotoxicity assays, from the DI values x the number of cells, histograms of the frequency of distribution of the DI values by group were obtained. The analyses were carried out using GraphPad Prism, version 7.0 (Graphpad Software Inc., La Jolla, CA, USA). The significance levels were set at 5%, 1% or 0.1% (p < 0.05, 0.01 and 0.001), according to the statistical analyses’ outcomes.
3. Results
3.1. Effect of CAP on Wound-Related Monospecies Biofilms
Monospecies biofilms formed by MRSA, P. aeruginosa or E. faecalis were exposed to CAP. Figure 1 shows the results for antibiofilm effect. The median value (CFU/mL) of the non-treated control for E. faecalis was 1.0 × 109; for treatment groups the median values (CFU/mL) were 5.8 × 107 (reduction of 1.2 log, p < 0.05), 5.2 × 107 (reduction of 1.3 log, p < 0.01), 1.4 × 107 (reduction of 1.9 log, p < 0.001) and 3.3 × 107 (reduction of 1.5 log, p < 0.01) after 1, 3, 5 and 7 min of CAP exposure, respectively. The median value (CFU/mL) of the non-treated control for MRSA was 6.4 × 108; for treatment groups the median values (CFU/mL) were 8.0 × 106 (reduction of 1.9 log, p > 0.05), 3.0 × 106 (reduction of 2.3 log, p < 0.05), 8.0 × 105 (reduction of 2.9 log, p < 0.001) and 1.4 × 106 (reduction of 2.7 log, p < 0.001) after 1, 3, 5 and 7 min of CAP exposure, respectively. The median value (CFU/mL) of the non-treated control for P. aeruginosa was 5.0 × 107; for treatment group the median values (CFU/mL) were 4.0 × 106 (reduction of 1.1 log, p > 0.05), 4.0 × 106 (reduction of 1.1 log, p > 0.05), 4.0 × 106 (reduction of 1.1 log, p > 0.05) and 2.2 × 105 (reduction of 2.4 log, p < 0.05) after 1, 3, 5 and 7 min of CAP exposure, respectively.
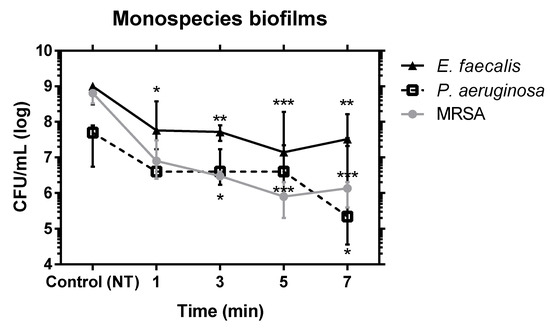
Figure 1.
Median and interquartile range of MRSA, P. aeruginosa and E. faecalis viable cells (CFU/mL) recovered after exposure of monospecies biofilms to (CAP) for 1, 3, 5 and 7 min. Kruskal–Wallis test and Dunn’s multiple comparison * p < 0.05; ** p < 0.01; *** p < 0.001.
3.2. Effect of CAP on Multispecies Biofilms
The effect of CAP on multispecies biofilms formed by MRSA, P. aeruginosa and E. faecalis can be observed in Figure 2. The median value (CFU/mL) of the non-treated control for E. faecalis was 2.3 × 109; for treatment groups the median values (CFU/mL) were 5.0 × 108 (reduction of 0.66 log, p < 0.01), 8.0 × 108 (reduction of 0.5 log, p < 0.05), 3.0 × 108 (reduction of 0.9 log, p < 0.001) and 7.0 × 108 (reduction of 0.5 log, p < 0.05) after 1, 3, 5 and 7 min of CAP exposure, respectively. The median value (CFU/mL) of the non-treated control for MRSA was 1.7 × 108; for treatment groups the median values (CFU/mL) were 1.1 × 108 (reduction of 0.2 log, p > 0.05), 3.7 × 107 (reduction of 0.66 log, p > 0.05), 2.0 × 107 (reduction of 0.9 log, p < 0.05) and 4.0 × 107 (reduction of 0.6 log, p < 0.05) after 1, 3, 5 and 7 min of CAP exposure, respectively. The median value (CFU/mL) of the non-treated control for P. aeruginosa was 3.0 × 107; for treatment group the median values (CFU/mL) were 6.0 × 106 (reduction of 0.7 log, p > 0.05), 5.0 × 106 (reduction of 0.8 log, p > 0.05), 1.0 × 106 (reduction of 1.5 log, p < 0.001) and 3.0 × 106 (reduction of 1.0 log, p > 0.05) after 1, 3, 5 and 7 min of CAP exposure, respectively.
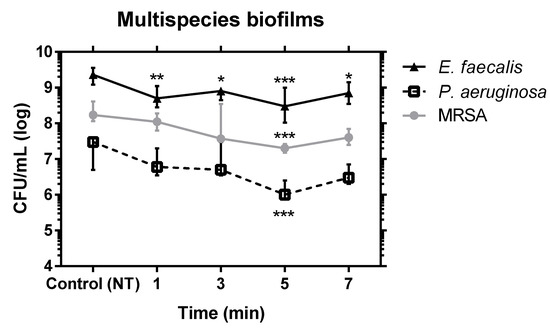
Figure 2.
Median and interquartile range of MRSA, P. aeruginosa and E. faecalis viable cells (CFU/mL) recovered after exposure of multispecies biofilms to CAP for 1, 3, 5 and 7 min. Kruskal–Wallis test and Dunn’s multiple comparison post hoc test * p < 0.05; ** p < 0.01; *** p < 0.001.
3.3. Morphologic Analysis of the Multispecies Biofilms by Scanning Electron Microscopy
The biofilms morphology was analyzed by scanning electron microscopy (SEM) in order to confirm presence of biofilm and corroborate the reduction in cell viability observed in microbiological analyses. To assess the effects of CAP in biofilm, a polymicrobial culture comprised of a 1:1:1 ratio of MRSA, E. faecalis and P. aeruginosa was grown.
Figure 3 shows the micrographs obtained without treatment and after exposure to CAP. Untreated biofilm (control) showed the presence of high cell density of the cocci and bacilli. No differences were observed between the images from central and lateral fields.
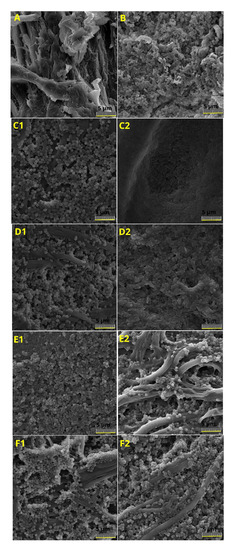
Figure 3.
Scanning electron microscopy (SEM) of multispecies biofilms formed by MRSA, P. aeruginosa and E. faecalis non-treated or treated for 1–7 min: (A) Collagen membrane without biofilm, (B) negative control (C1), biofilm after exposure to CAP for 1 min (central region), (C2) biofilm after exposure CAP for 1 min (lateral region), (D1) biofilm after exposure to CAP for 3 min (central region), (D2) biofilm after exposure to CAP for 3 min (lateral region), (E1) biofilm after exposure to CAP for 5 min (central region), (E2) biofilm after exposure to CAP for 5 min (lateral region), (F1) biofilm after exposure to CAP for 7 min (central region) and (F2) biofilm after treatment by CAP for 7 min (lateral region). Scale bare represents 5 µm.
In the groups exposed to CAP, SEM images showed dispersed biofilm clusters with moderate differences in the amount of microorganisms according to the analyzed field. After 1 and 3 min of exposure to CAP (Figure 3C1,D1), there was a greater presence of diplococci in the central field, the cell density in the biofilm was lower than in the non-treated control. In the lateral field, the cell density was higher and the presence of bacilli could be noticed (Figure 3C2,D2). After 5 min of exposure to CAP, the images showed a reduction in the cell density in the biofilm mostly in the center field. On the other hand, 7 min exposure to CAP leads to a visible biofilm reduction over the entire analyzed area.
3.4. Cytotoxicity
The 3T3 cells were exposed to the plasma jet for 1, 3, 5 and 7 min (Figure 4). The cytotoxicity immediately after exposure to plasma for all times was classified as Grade 0 (not cytotoxic), as the cell viability was 100% when compared to the unexposed control, except for 3 min, which was Grade 1 (slight), since the cell viability was 93.1% [52].
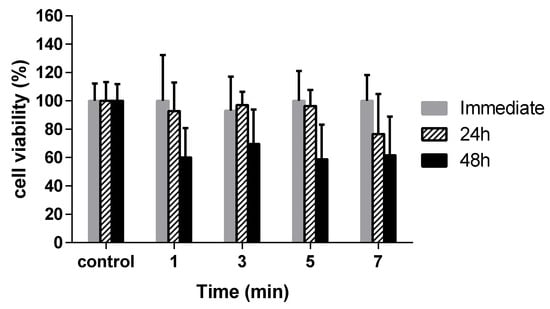
Figure 4.
Cytotoxicity analysis of non-thermal plasma at atmospheric pressure expressed in cell viability. The 3T3 cells were exposed to CAP for 1, 3, 5 and 7 min. The cell viability was determined immediately (gray bar), 24 h (striped bar) and 48 h (black bar) after plasma exposure.
After 24 h of exposure to plasma, cytotoxicity was classified as Grade 1 (slight) for the exposure time for 1 to 5 min [52]. The exposure for 7 min was classified as Grade 2 (mild), since the cell viability was 76.6%. After 48 h of exposure to plasma, cytotoxicity was classified as Grade 2 (mild) for all times [52].
3.5. Genotoxicity
According to obtained results, all groups of 3T3 cells can be classified as slightly aneuploid (DI ≥ 1.2). Non-treated group (NT) presented DNA index (DI) mean of 1.27. These results suggest that CAP was not genotoxic. Table 1 shows DI median, mean, and standard deviation (SD) of studied groups. Figure 5 represents the distribution histogram of obtained DI × number of cells for all analyzed periods of time.

Table 1.
Median, mean and standard deviation (SD) of DNA index (DI) obtained by static cytometry of 3T3 cells’ nucleus when treated with cold atmospheric plasma for 1 (P1), 3 (P3), 5 (P5), and 7 (P7) minutes. NT = non-treated group.
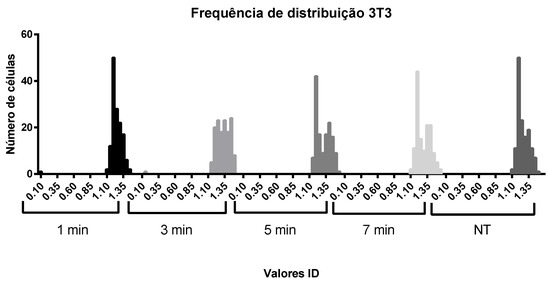
Figure 5.
Histogram of distribution of DNA indices (ID) obtained × number of corresponding cells 4.
4. Discussion
The outcomes of this study showed that He-cold atmospheric plasma significantly reduced the viability of wound-related mono and multispecies biofilms. S. aureus, P. aeruginosa and E. faecalis are opportunistic pathogenic bacteria which cause chronic infections due a number of virulence factors and can interfere with wound healing process, in particular when strains resistant to antimicrobials are involved [55]. To the best of our knowledge, this is the first report on the activity of CAP on wound related multispecies biofilms, formed by MRSA, P. aeruginosa and E. faecalis, by using a model of wound-related biofilm.
Although the main goal of this study was to evaluate the effect of cold atmospheric plasma in multispecies biofilms, experiments with monospecies biofilms were carried out in order to establish the operation parameters of the plasma device that generated antimicrobial activity against the tested microbial species. For this purpose and taking in account the cost of membrane used in the multispecies experiments, monospecies biofilms were grown in 96-well plates. We observed that the exposure to CAP for 5 min reduced in 3 log the viable cells of MRSA monospecieis biofilms. This result corroborates the findings reported by Xu et al. [56], in which a plasma jet operating with 20 kV of voltage, frequency of 38 kHz, and He flow rate of 6.7 slm reduced in 3.6 log S. aureus biofilms after 10 min exposure. CAPs generated using other working gases also showed similar inhibitory effects. Matthes et al. [41] observed a reduction of 1.7 log in MRSA biofilms after repeated 20 s exposure to Ar plasma during 6 h. Besides, Wang et al. [57] observed a decrease of 4.67 ± 0.29 log in the viability of S. aureus biofilms after 10 min exposure to N2 CAP.
We also detected a significant reduction in the viability of E. faecalis monospecies biofilm after 1 min exposure in the present study. The reduction varied from 1.2 to 1.9 log when compared to the untreated control group. This result is interesting, since E. faecalis monospecies biofilms appear to be resistant to other therapies. In the case of E. faecalis monospecies biofilm, it seems that other CAP generation setups lead to higher inhibitory effects when compared to He-CAP used in this study. Theinkon et al. [37] observed 3 log reduction in E. faecalis (ATCC 29212) biofilm viability after 5 min exposure to CAP generated by a surface micro-discharge reactor in open air operating with voltage of 3.5 kVp-p and a frequency of 4.0 kHz. It is important to highlight that in this study, differently than in ours, the treatment was applied indirectly (without direct contact between target and plasma) and the distribution of reactive species occurred by means of thermal convection and diffusion. Another study using CAP of Ar (98%) and O2 (2%) observed 90% reduction in the viability of the 7-day biofilm of E. faecalis formed within the dental root canals of human teeth after 8 min of exposure [58].
For P. aeruginosa monospecies biofilms, we detected that He-CAP reduced in 2.4 log/CFU after 7 min of exposure. Alkawareed et al. [59] used a plasma jet with gas mixture (He/O2) with voltage of 6 kV, frequency of 40 kHz and gas flow rate of 2 slm for treatment of P. aeruginosa and obtained a reduction of 4 log after treatment for 4 min. Besides, Gabriel et al. [36] reported a reduction of 5 log in P. aeruginosa counts after exposition for 90 s to microwave plasma jet (2.45 GHz) in air with flow rate of 5 slm, while we observed a reduction of 2.4 log after 7 min of exposure. However, it is important to mention that in both aforementioned studies the temperatures of CAP were above 40 °C, which could explain the higher reduction of the viable cells.
After determining the optimal parameters for monospecies biofilms, the effect of CAP on multispecies biofilms was studied. The study of mixed-species biofilms is relevant as, clinically, they can cause persistent infections and usually lead to worse infections [60,61,62]. The model of polymicrobial biofilm obtained on a porcine collagen membrane gave strong evidences that CAP can reduce the bacterial biofilm viability in complex models. The model described by Brackman e Coenye [8] for wound-related biofilms was selected because it mimics the conditions observed in wounds, by using a culture medium with a constitution close to the exudate and a nutrient flow diffusion from the bottom up. Besides, the model also mimics the air-wound-liquid interface that occurs in vivo [8].
The selection of the microbial species used to form the multispecies biofilms were based on their relevance in the context of chronic wounds infection. Previous studies reported that S. aureus and P. aeruginosa were the most prevalent species in wounds [4,11]. Besides, the presence of certain species, such as E. faecalis, seems to be related to worse clinical course of the wound [4,10,63].
In this study, P. aeruginosa was more susceptible to CAP in a multispecies biofilm, with reduction of 1.48 log. It is an unexpected result since previous report suggested that P. aeruginosa is one of the most benefited species in a mixed species culture, probably because it is present in a more protected niche of the biofilm [64].
It is known that CAP generates large variety of reactive species that can cause decontamination. Among them, ROS (e.g., O3, O2-, OH, O) are indicated as the major agent responsible for bactericidal effects of plasmas [65]. In plasma jets, the generated plasma plume excites and ionizes air molecules present in the surrounding ambient leading to formation of RONS [66]. The concentration of generated reactive species can be enhanced by adding molecular gases (e.g., air, O2 or N2) to the main carrier gas or applying a shielding gas curtain around the plasma plume [67]. In plasma jets, the produced reactive species are driven by the gas flow to the sample allowing short and long-living species to act on the treated surface, which can increase the treatment efficiency when compared to indirect methods. The plasma jet device used in the present study was operated with commercial low-grade purity helium that contains few impurities (mostly air) and ROS formation in the plasma plume was detected in previous studies [47,48]. Thus, the MRSA biofilm was significantly more susceptible than P. aeruginosa and E. faecalis under ROS-dominated conditions. Interestingly, the increased susceptibility of MRSA in a polymicrobial biofilm with P. aeruginosa, E. faecalis and Klebsiella pneumoniae, to RNS-dominated conditions were previously reported Modic et al. [31].
Our results showed that exposure to CAP for 1, 3, 5 and 7 min was not cytotoxic for fibroblasts 3T3 cells analyzed immediately after the exposure. Similarly, Borges et al. [45] found the cell viability to be higher than 80% immediately and 24 h after amplitude modulated cold atmospheric pressure plasma jet (AM-CAPPJ) exposure of Vero cells for 3 and 5 min. On the other hand, Borges et al. [45] showed that cell viability was maintained at around 80%, 48 h after AM-CAPPJ exposure, which was different from the present work where the cell viability has decreased to around 60% after 48 h. This could be explained by the internal cell signaling cascade that some reactive species may trigger as previously described [30,68,69]. Therefore, a potential cytotoxicity may be related to this lower cell viability after 48 h (late effects) in relation to the immediate time or 24 h, which could have side effects on cells. However, further chronic toxicity studies of CAP should be carried out. These late effects on fibroblasts could also exist for microorganisms and should be investigated in future studies.
Aiming the clinical application of CAP for wound care, it was extremally important to investigate whether plasma conditions would lead to DNA damage or not. In this study, all tested periods of treatments presented a DNA index between 1.2 and 1.33 (mean and median) which, according to the score, represents a slight ploidy, but taking into account that the CAP group was into the same score; median 1.24 and mean 1.27, we believe treatment was not genotoxic. Our results are coincident with others in the literature. Boxhammer et al. [70] observed no mutations, through EPRT assay, on V79 cells after 30 to 240 s of CAP treatment using a MiniFlatPlaSter device. Only a decrease in the proliferation rate was observed. Wende et al. [71] and Bekeschus et al. [72] tested the KINPen® trough different methods of evaluation, and found no signals of genotoxicity due to plasma treatment. Wende et al. [71] assays used up to 180 s of CAP in non-cancer cells (HaCat and MRC5 cells) and melanoma cells (SK-Mel-147 cells) and did not find mutagenic changes with CAP treatment as well. They used HPRT1 mutation assay, micronucleus formation assay, and clonogenic assay, to confirm their findings. Kludge et al. [73] used the KINPen MED™ to evaluate CAP genotoxicity using HET-MN model and also observed no genotoxic alterations on CAP treatment. In our study, static cytometry was chosen to calculate DNA index and, in that way, evaluate possible mutations caused by cold plasma treatment and found no genotoxic signals in cells expose up to 7 min (420 s). Different CAP sources, cell types, CAP treatment conditions, and assay models reported make it difficult to compare results, but it seems that CAP safety has been proven by literature.
The inhibitory effect of CAP on wound-related multispecies biofilm with the low cytotoxicity and no genotoxicity observed in this wound-related multispecies biofilm study encourage in vivo studies to evaluate the effects of CAP on infected wounds that can also investigate additional anti-inflammatory and tissue repair inducing effects.
5. Conclusions
In conclusion, exposure to He-CAP for 5 min showed inhibitory effect on wound-related multispecies biofilms formed by methicillin-resistant S. aureus (MRSA), P. aeruginosa and E. faecalis, with low cytotoxicity and genotoxicity to mammalian cells mainly immediately after exposure. These findings point out the application of this innovative technology in the control of infected chronic wounds.
Author Contributions
Conceptualization, C.Y.K.-I. and G.d.M.G.L.; methodology, M.A.C.d.O., G.d.M.G.L., T.M.C.N., A.V.L.G., B.R.C.d.M., M.V.C., K.G.K., C.Y.K.-I.; software, B.R.C.d.M., M.V.C., K.G.K.; validation, M.A.C.d.O., G.d.M.G.L., T.M.C.N., A.V.L.G., B.R.C.d.M., M.V.C., K.G.K. and C.Y.K.-I.; formal analysis, M.A.C.d.O., G.d.M.G.L., T.M.C.N., A.V.L.G., B.R.C.d.M., M.V.C., K.G.K., C.Y.K.-I.; investigation, M.A.C.d.O., G.d.M.G.L., T.M.C.N., A.V.L.G., B.R.C.d.M., M.V.C., K.G.K., C.Y.K.-I.; resources, C.Y.K.-I.; data curation, M.A.C.d.O., G.d.M.G.L.; writing—original draft preparation, M.A.C.d.O., G.d.M.G.L., T.M.C.N., A.V.L.G. and C.Y.K.-I.; writing—review and editing, M.A.C.d.O., G.d.M.G.L., T.M.C.N., A.V.L.G., B.R.C.d.M., M.V.C., K.G.K., C.Y.K.-I.; visualization, M.A.C.d.O., G.d.M.G.L. and C.Y.K.-I., supervision, G.d.M.G.L., C.Y.K.-I.; project administration, C.Y.K.-I.; funding acquisition, C.Y.K.-I., K.G.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Council for Scientific and Technological Development (CNPq), Grant numbers 405653/2016-6 and 308127/2018-8. This work received financial support from Coordenação deAperfeiçoamento de Pessoal de Nível Superior—CAPES—Brazil.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Frykberg, R.G.; Banks, J. Challenges in the Treatment of Chronic Wounds. Adv. Wound Care 2015, 4, 560–582. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.E.; Foster, D.S.; Longaker, M.T. Management of Chronic Wounds—2018. JAMA J. Am. Med. Assoc. 2018, 320, 1481–1482. [Google Scholar] [CrossRef]
- Martinengo, L.; Olsson, M.; Bajpai, R.; Soljak, M.; Upton, Z.; Schmidtchen, A.; Car, J.; Järbrink, K. Prevalence of chronic wounds in the general population: Systematic review and meta-analysis of observational studies. Ann. Epidemiol. 2019, 29, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Bjarnsholt, T. The role of bacterial biofilms in chronic infections. APMIS. Suppl. 2013, 1–51. [Google Scholar] [CrossRef]
- Olsson, M.; Järbrink, K.; Divakar, U.; Bajpai, R.; Upton, Z.; Schmidtchen, A.; Car, J. The humanistic and economic burden of chronic wounds: A systematic review. Wound Repair Regen. 2019, 27, 114–125. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.K.; Cheng, N.C.; Cheng, C.M. Biofilms in Chronic Wounds: Pathogenesis and Diagnosis. Trends Biotechnol. 2019, 37, 505–517. [Google Scholar] [CrossRef]
- Kim, P.J.; Steinberg, J.S. Wound care: Biofilm and its impact on the latest treatment modalities for ulcerations of the diabetic foot. Semin. Vasc. Surg. 2012, 25, 70–74. [Google Scholar] [CrossRef]
- Brackman, G.; Coenye, T. In vitro and in vivo biofilm wound models and their application. Adv. Exp. Med. Biol. 2016, 897, 15–32. [Google Scholar] [CrossRef]
- Tytgat, H.L.P.; Nobrega, F.L.; van der Oost, J.; de Vos, W.M. Bowel Biofilms: Tipping Points between a Healthy and Compromised Gut? Trends Microbiol. 2019, 27, 17–25. [Google Scholar] [CrossRef]
- Rhoads, D.D.; Wolcott, R.D.; Sun, Y.; Dowd, S.E. Comparison of culture and molecular identification of bacteria in chronic wounds. Int. J. Mol. Sci. 2012, 13, 2535–2550. [Google Scholar] [CrossRef]
- Gjødsbøl, K.; Christensen, J.J.; Karlsmark, T.; Jørgensen, B.; Klein, B.M.; Krogfelt, K.A. Multiple bacterial species reside in chronic wounds: A longitudinal study. Int. Wound J. 2006, 3, 225–231. [Google Scholar] [CrossRef]
- Bessa, L.J.; Fazii, P.; Di Giulio, M.; Cellini, L. Bacterial isolates from infected wounds and their antibiotic susceptibility pattern: Some remarks about wound infection. Int. Wound J. 2015, 12, 47–52. [Google Scholar] [CrossRef]
- Pallavali, R.R.; Degati, V.L.; Lomada, D.; Reddy, M.C.; Durbaka, V.R.P. Isolation and in vitro evaluation of bacteriophages against MDR-bacterial isolates from septic wound infections. PLoS ONE 2017, 12, e0179245. [Google Scholar] [CrossRef]
- Haertel, B.; von Woedtke, T.; Weltmann, K.D.; Lindequist, U. Non-thermal atmospheric-pressure plasma possible application in wound healing. Biomol. Ther. 2014, 22, 477–490. [Google Scholar] [CrossRef]
- Edwards, K. New Twist on an Old Favorite: Gentian Violet and Methylene Blue Antibacterial Foams. Adv. Wound Care 2016, 5, 11–18. [Google Scholar] [CrossRef]
- Julák, J.; Scholtz, V.; Vaňková, E. Medically important biofilms and non-thermal plasma. World J. Microbiol. Biotechnol. 2018, 34, 1–15. [Google Scholar] [CrossRef]
- Wolcott, R. Are chronic wounds, chronic infections? J. Wound Care 2016, 25, S33. [Google Scholar] [CrossRef] [PubMed]
- Han, G.; Ceilley, R. Chronic Wound Healing: A Review of Current Management and Treatments. Adv. Ther. 2017, 34, 599–610. [Google Scholar] [CrossRef] [PubMed]
- Oryan, A.; Alemzadeh, E.; Moshiri, A. Burn wound healing: Present concepts, treatment strategies and future directions. J. Wound Care 2017, 26, 5–19. [Google Scholar] [CrossRef]
- Panahi, Y.; Izadi, M.; Sayyadi, N.; Rezaee, R.; Member, F.; Beiraghdar, F.; Member, F.; Zamani, A.; Sahebkar, A.; Member, F. Comparative trial of Aloe vera/olive oil combination cream versus phenytoin cream in the treatment of chronic wounds. J. Wound Care 2015, 24, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Craven, M.; Kasper, S.H.; Canfield, M.J.; Diaz-Morales, R.R.; Hrabie, J.A.; Cady, N.C.; Strickland, A.D. Nitric oxide-releasing polyacrylonitrile disperses biofilms formed by wound-relevant pathogenic bacteria. J. Appl. Microbiol. 2016, 120, 1085–1099. [Google Scholar] [CrossRef]
- Napavichayanun, S.; Yamdech, R.; Aramwit, P. The safety and efficacy of bacterial nanocellulose wound dressing incorporating sericin and polyhexamethylene biguanide: In vitro, in vivo and clinical studies. Arch. Dermatol. Res. 2016, 308, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Finnegan, S.; Percival, S.L. EDTA: An Antimicrobial and Antibiofilm Agent for Use in Wound Care. Adv. Wound Care 2015, 4, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Thana, P.; Wijaikhum, A.; Poramapijitwat, P.; Kuensaen, C.; Meerak, J.; Ngamjarurojana, A.; Sarapirom, S.; Boonyawan, D. A compact pulse-modulation cold air plasma jet for the inactivation of chronic wound bacteria: Development and characterization. Heliyon 2019, 5, e02455. [Google Scholar] [CrossRef] [PubMed]
- Bekeschus, S.; Favia, P.; Robert, E.; von Woedtke, T. White paper on plasma for medicine and hygiene: Future in plasma health sciences. Plasma Process. Polym. 2019, 16, 1–12. [Google Scholar] [CrossRef]
- Šimončicová, J.; Kryštofová, S.; Medvecká, V.; Ďurišová, K.; Kaliňáková, B. Technical applications of plasma treatments: Current state and perspectives. Appl. Microbiol. Biotechnol. 2019, 103, 5117–5129. [Google Scholar] [CrossRef] [PubMed]
- Laroussi, M.; Mendis, D.A.; Rosenberg, M. Plasma interaction with microbes. New J. Phys. 2003, 5. [Google Scholar] [CrossRef]
- Fridman, G.; Friedman, G.; Gutsol, A.; Shekhter, A.B.; Vasilets, V.N.; Fridman, A. Applied plasma medicine. Plasma Process. Polym. 2008, 5, 503–533. [Google Scholar] [CrossRef]
- Gay-Mimbrera, J.; García, M.C.; Isla-Tejera, B.; Rodero-Serrano, A.; García-Nieto, A.V.; Ruano, J. Clinical and Biological Principles of Cold Atmospheric Plasma Application in Skin Cancer. Adv. Ther. 2016, 33, 894–909. [Google Scholar] [CrossRef] [PubMed]
- Laroussi, M. Plasma Medicine: A Brief Introduction. Plasma 2018, 1, 47–60. [Google Scholar] [CrossRef]
- Modic, M.; McLeod, N.P.; Sutton, J.M.; Walsh, J.L. Cold atmospheric pressure plasma elimination of clinically important single- and mixed-species biofilms. Int. J. Antimicrob. Agents 2017, 49, 375–378. [Google Scholar] [CrossRef]
- Chatraie, M.; Torkaman, G.; Khani, M.; Salehi, H.; Shokri, B. In vivo study of non-invasive effects of non-thermal plasma in pressure ulcer treatment. Sci. Rep. 2018, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Wang, L.; Xia, C.; Yang, X.; Cao, Z.; Zheng, L.; Ko, R.; Shen, C.; Yang, C.; Cheng, C. Cold atmospheric plasma promotes different types of superficial skin erosion wounds healing. Int. Wound J. 2019, 16, 1103–1111. [Google Scholar] [CrossRef]
- Gupta, T.T.; Karki, S.B.; Matson, J.S.; Gehling, D.J.; Ayan, H. Sterilization of Biofilm on a Titanium Surface Using a Combination of Nonthermal Plasma and Chlorhexidine Digluconate. Biomed. Res. Int. 2017, 2017. [Google Scholar] [CrossRef]
- Brun, P.; Bernabè, G.; Marchiori, C.; Scarpa, M.; Zuin, M.; Cavazzana, R.; Zaniol, B.; Martines, E. Antibacterial efficacy and mechanisms of action of low power atmospheric pressure cold plasma: Membrane permeability, biofilm penetration and antimicrobial sensitization. J. Appl. Microbiol. 2018, 125, 398–408. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, A.A.; Ugay, M.C.C.F.; Siringan, M.A.T.; Rosario, L.M.D.; Tumlos, R.B.; Ramos, H.J. Atmospheric pressure plasma jet inactivation of Pseudomonas aeruginosa biofilms on stainless steel surfaces. Innov. Food Sci. Emerg. Technol. 2016, 36, 311–319. [Google Scholar] [CrossRef]
- Theinkom, F.; Singer, L.; Cieplik, F.; Cantzler, S.; Weilemann, H.; Cantzler, M.; Hiller, K.A.; Maisch, T.; Zimmermann, J.L. Antibacterial efficacy of cold atmospheric plasma against Enterococcus faecalis planktonic cultures and biofilms in vitro. PLoS ONE 2019, 14, e0223925. [Google Scholar] [CrossRef] [PubMed]
- Üreyen Kaya, B.; Kececi, A.D.; Güldaş, H.E.; Çetin, E.S.; Öztürk, T.; Öksuz, L.; Bozduman, F. Efficacy of endodontic applications of ozone and low-temperature atmospheric pressure plasma on root canals infected with Enterococcus faecalis. Lett. Appl. Microbiol. 2014, 58, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Sun, K.; Ye, G.; Liang, Y.; Pan, H.; Wang, G.; Zhao, Y.; Pan, J.; Zhang, J.; Fang, J. Evaluation of Cold Plasma Treatment and Safety in Disinfecting 3-week Root Canal Enterococcus faecalis Biofilm in Vitro. J. Endod. 2015, 41, 1325–1330. [Google Scholar] [CrossRef]
- Han, L.; Patil, S.; Boehm, D.; Milosavljević, V.; Cullen, P.J.; Bourke, P. Mechanisms of inactivation by high-voltage atmospheric cold plasma differ for Escherichia coli and Staphylococcus aureus. Appl. Environ. Microbiol. 2016, 82, 450–458. [Google Scholar] [CrossRef]
- Matthes, R.; Assadian, O.; Kramer, A. Repeated applications of cold atmospheric pressure plasma does not induce resistance in Staphylococcus aureus embedded in biofilms. GMS Hyg. Infect. Control 2014, 9. [Google Scholar] [CrossRef]
- Jacofsky, M.C.; Lubahn, C.; McDonnell, C.; Seepersad, Y.; Fridman, G.; Fridman, A.; Dobrynin, D. Spatially resolved optical emission spectroscopy of a helium plasma jet and its effects on wound healing rate in a diabetic murine model. Plasma Med. 2014, 4, 177–191. [Google Scholar] [CrossRef]
- Von Woedtke, T.; Schmidt, A.; Bekeschus, S.; Wende, K.; Weltmann, K.D. Plasma medicine: A field of applied redox biology. In Vivo 2019, 33, 1011–1026. [Google Scholar] [CrossRef]
- Tort, S.; Demiröz, F.T.; Coşkun Cevher, Ş.; Sarıbaş, S.; Özoğul, C.; Acartürk, F. The effect of a new wound dressing on wound healing: Biochemical and histopathological evaluation. Burns 2020, 46, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Borges, A.C.; de Morais Gouvêa Lima, G.; Mayumi Castaldelli Nishime, T.; Vidal Lacerda Gontijo, A.; Kostov, K.G.; Koga-Ito, C.Y. Amplitude-modulated cold atmospheric pressure plasma jet for treatment of oral candidiasis: In vivo study. PLoS ONE 2018, 13, e0199832. [Google Scholar] [CrossRef] [PubMed]
- Borges, A.C.; Nishime, T.M.C.; de Moura Rovetta, S.; Lima, G.d.M.G.; Kostov, K.G.; Thim, G.P.; de Menezes, B.R.C.; Machado, J.P.B.; Koga-Ito, C.Y. Cold Atmospheric Pressure Plasma Jet Reduces Trichophyton rubrum Adherence and Infection Capacity. Mycopathologia 2019, 184, 585–595. [Google Scholar] [CrossRef] [PubMed]
- Kostov, K.G.; Nishime, T.M.C.; Machida, M.; Borges, A.C.; Prysiazhnyi, V.; Koga-Ito, C.Y. Study of Cold Atmospheric Plasma Jet at the End of Flexible Plastic Tube for Microbial Decontamination. Plasma Process. Polym. 2015, 12, 1383–1391. [Google Scholar] [CrossRef]
- Nishime, T.M.C.; Wagner, R.; Kostov, K.G. Study of modified area of polymer samples exposed to a he atmospheric pressure plasma jet using different treatment conditions. Polymers 2020, 12. [Google Scholar] [CrossRef]
- Werthén, M.; Henriksson, L.; Jensen, P.Ø.; Sternberg, C.; Givskov, M.; Bjarnsholt, T. An in vitro model of bacterial infections in wounds and other soft tissues. APMIS. Suppl. 2010, 118, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Hammond, A.A.; Miller, K.G.; Kruczek, C.J.; Dertien, J.; Colmer-Hamood, J.A.; Griswold, J.A.; Horswill, A.R.; Hamood, A.N. An in vitro biofilm model to examine the effect of antibiotic ointments on biofilms produced by burn wound bacterial isolates. Burns 2011, 37, 312–321. [Google Scholar] [CrossRef]
- Gomes, L.C.; Mergulhão, F.J. SEM analysis of surface impact on biofilm antibiotic treatment. Scanning 2017, 2017. [Google Scholar] [CrossRef]
- International Organization of Standardization. ISO 10993-5:2009. Biological Evaluation of Medical Devices—Part 5: Tests for In Vitro Cytotoxicity; ISO: Geneva, Switzerland, 2009; p. 13. [Google Scholar]
- Felisbino, M.B.; Tamashiro, W.M.S.C.; Mello, M.L.S. Chromatin remodeling, cell proliferation and cell death in valproic acid-treated HeLa cells. PLoS ONE 2011, 6, e29144. [Google Scholar] [CrossRef]
- Lima, C.F.; Alves, M.G.O.; Carvalho, B.F.d.C.; de Lima, T.A.; Coutinho-Camillo, C.M.; Soares, F.A.; Scholz, J.; Almeida, J.D. Is DNA ploidy related to smoking? J. Oral Pathol. Med. 2017, 46, 961–966. [Google Scholar] [CrossRef]
- Kondeti, V.S.S.K.; Phan, C.Q.; Wende, K.; Jablonowski, H.; Gangal, U.; Granick, J.L.; Hunter, R.C.; Bruggeman, P.J. Long-lived and short-lived reactive species produced by a cold atmospheric pressure plasma jet for the inactivation of Pseudomonas aeruginosa and Staphylococcus aureus. Free Radic. Biol. Med. 2018, 124, 275–287. [Google Scholar] [CrossRef]
- Xu, Z.; Shen, J.; Zhang, Z.; Ma, J.; Ma, R.; Zhao, Y.; Sun, Q.; Qian, S.; Zhang, H.; Ding, L.; et al. Inactivation effects of non-thermal atmospheric-pressure helium plasma jet on staphylococcus aureus biofilms. Plasma Process. Polym. 2015, 12, 827–835. [Google Scholar] [CrossRef]
- Wang, J.; Yu, Z.; Xu, Z.; Hu, S.; Li, Y.; Xue, X.; Cai, Q.; Zhou, X.; Shen, J.; Lan, Y.; et al. Antimicrobial mechanism and the effect of atmospheric pressure N 2 plasma jet on the regeneration capacity of Staphylococcus aureus biofilm. Biofouling 2018, 34, 935–949. [Google Scholar] [CrossRef]
- Pan, J.; Sun, K.; Liang, Y.; Sun, P.; Yang, X.; Wang, J.; Zhang, J.; Zhu, W.; Fang, J.; Becker, K.H. Cold plasma therapy of a tooth root canal infected with enterococcus faecalis biofilms in vitro. J. Endod. 2013, 39, 105–110. [Google Scholar] [CrossRef]
- Alkawareek, M.Y.; Algwari, Q.T.; Laverty, G.; Gorman, S.P.; Graham, W.G.; O’Connell, D.; Gilmore, B.F. Eradication of Pseudomonas aeruginosa Biofilms by Atmospheric Pressure Non-Thermal Plasma. PLoS ONE 2012, 7, e44289. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Dowd, S.E.; Smith, E.; Rhoads, D.D.; Wolcott, R.D. In vitro multispecies Lubbock chronic wound biofilm model. Wound Repair Regen. 2008, 16, 805–813. [Google Scholar] [CrossRef] [PubMed]
- Trifilio, S.; Zhou, Z.; Fong, J.L.; Zomas, A.; Liu, D.; Zhao, C.; Zhang, J.; Mehta, J. Polymicrobial bacterial or fungal infections: Incidence, spectrum of infection, risk factors, and clinical outcomes from a large hematopoietic stem cell transplant center. Transpl. Infect. Dis. 2015, 17, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Rao, Y.; Shang, W.; Yang, Y.; Zhou, R.; Rao, X. Fighting Mixed-Species Microbial Biofilms with Cold Atmospheric Plasma. Front. Microbiol. 2020, 11, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Fazli, M.; Bjarnsholt, T.; Kirketerp-Møller, K.; Jørgensen, B.; Andersen, A.S.; Krogfelt, K.A.; Givskov, M.; Tolker-Nielsen, T. Nonrandom distribution of Pseudomonas aeruginosa and Staphylococcus aureus in chronic wounds. J. Clin. Microbiol. 2009, 47, 4084–4089. [Google Scholar] [CrossRef]
- Touzel, R.E.; Sutton, J.M.; Wand, M.E. Establishment of a multi-species biofilm model to evaluate chlorhexidine efficacy. J. Hosp. Infect. 2016, 92, 154–160. [Google Scholar] [CrossRef]
- Lu, X.; Ye, T.; Cao, Y.; Sun, Z.; Xiong, Q.; Tang, Z.; Xiong, Z.; Hu, J.; Jiang, Z.; Pan, Y. The roles of the various plasma agents in the inactivation of bacteria. J. Appl. Phys. 2008, 104. [Google Scholar] [CrossRef]
- Laroussi, M. Low-Temperature Plasma Jet for Biomedical Applications: A Review. IEEE Trans. Plasma Sci. 2015, 43, 703–712. [Google Scholar] [CrossRef]
- Schmidt-Bleker, A.; Winter, J.; Iseni, S.; Dünnbier, M.; Weltmann, K.D.; Reuter, S. Reactive species output of a plasma jet with a shielding gas device—Combination of FTIR absorption spectroscopy and gas phase modelling. J. Phys. D Appl. Phys. 2014, 47. [Google Scholar] [CrossRef]
- Barekzi, N.; Laroussi, M. Fibroblast cell morphology altered by low-temperature atmospheric pressure plasma. IEEE Trans. Plasma Sci. 2014, 42, 2738–2739. [Google Scholar] [CrossRef]
- Shahriar, M.A.; Morteza, A.; Hajar, R.; Reza, K.M.; Babak, S. Feasibility of Leukemia Cancer Treatment (K562) by Atmospheric Pressure Plasma Jet. Int. J. Phys. Math. Sci. 2014, 8, 719–722. [Google Scholar]
- Boxhammer, V.; Li, Y.F.; Köritzer, J.; Shimizu, T.; Maisch, T.; Thomas, H.M.; Schlegel, J.; Morfill, G.E.; Zimmermann, J.L. Investigation of the mutagenic potential of cold atmospheric plasma at bactericidal dosages. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2013, 753, 23–28. [Google Scholar] [CrossRef]
- Wende, K.; Bekeschus, S.; Schmidt, A.; Jatsch, L.; Hasse, S.; Weltmann, K.D.; Masur, K.; von Woedtke, T. Risk assessment of a cold argon plasma jet in respect to its mutagenicity. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2016, 798–799, 48–54. [Google Scholar] [CrossRef]
- Bekeschus, S.; Schmidt, A.; Kramer, A.; Metelmann, H.R.; Adler, F.; von Woedtke, T.; Niessner, F.; Weltmann, K.D.; Wende, K. High throughput image cytometry micronucleus assay to investigate the presence or absence of mutagenic effects of cold physical plasma. Environ. Mol. Mutagen. 2018, 59, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Kluge, S.; Bekeschus, S.; Bender, C.; Benkhai, H.; Sckell, A.; Below, H.; Stope, M.B.; Kramer, A. Investigating the mutagenicity of a cold argon-plasma jet in an HET-MN model. PLoS ONE 2016, 11, e0160667. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).