Engineering and Manufacturing of a Dynamizable Fracture Fixation Device System
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
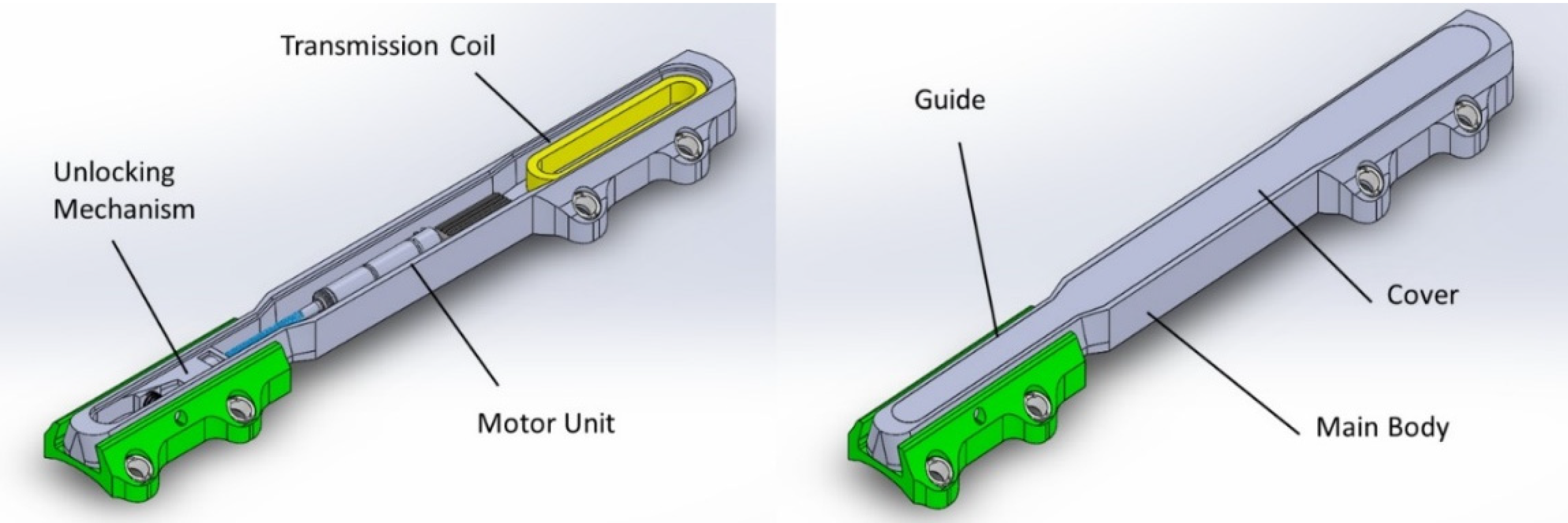
- The two parts (the ‘body’ and the ‘guide’) are coupled through a dove-tail prismatic guide in order to allow the axial translation and prevent both flexion and torsion;
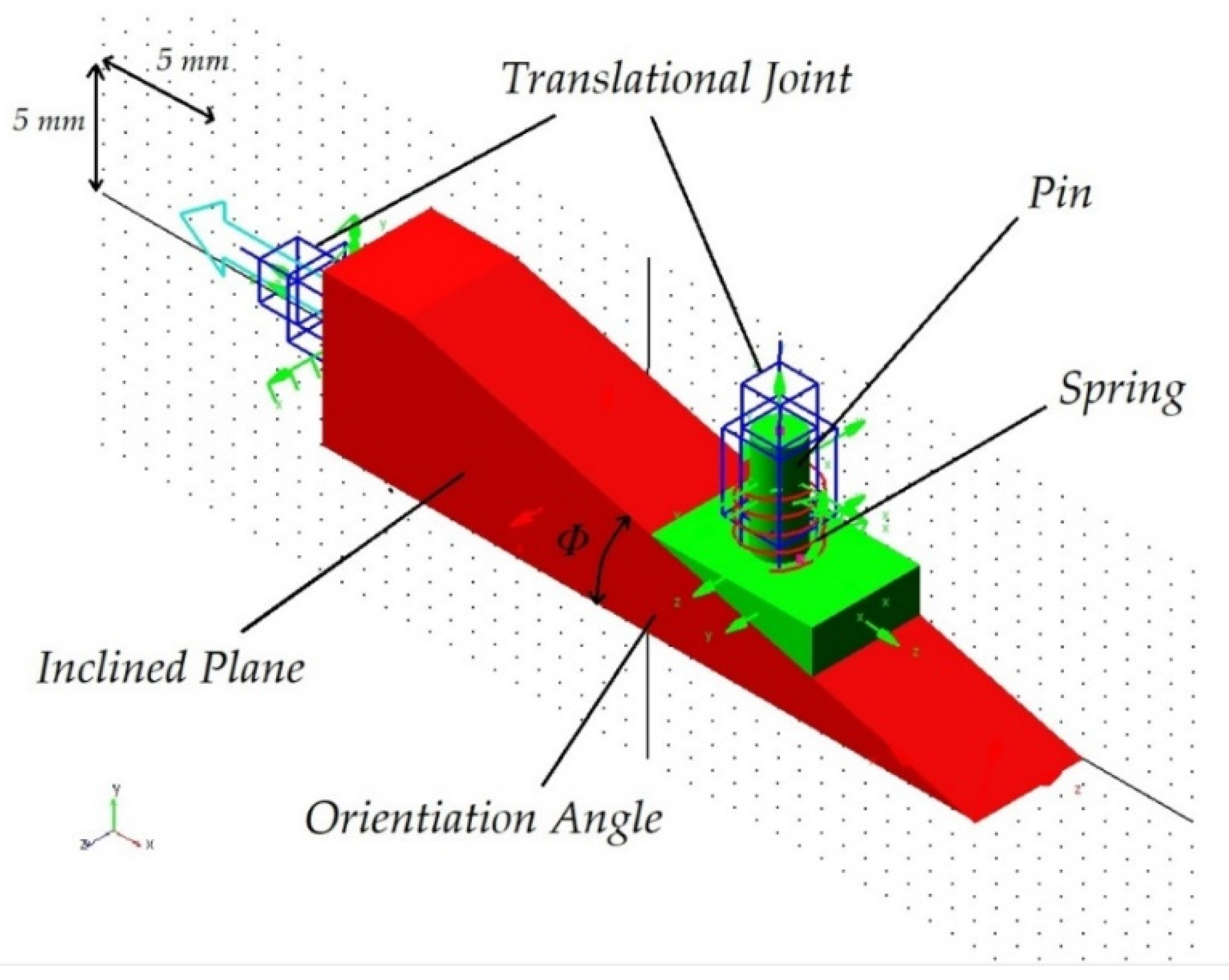
- In the ‘locked’ configuration, the axial translation is blocked through a pin, pre-loaded by a spring and supported, inferiorly, by an inclined plane;
- In the ‘unlocked’ configuration, the lower support of the pin lowers due to a horizontal translation of the inclined plane, provided by the actuator; the pin is so disengaged by the pre-loaded spring.
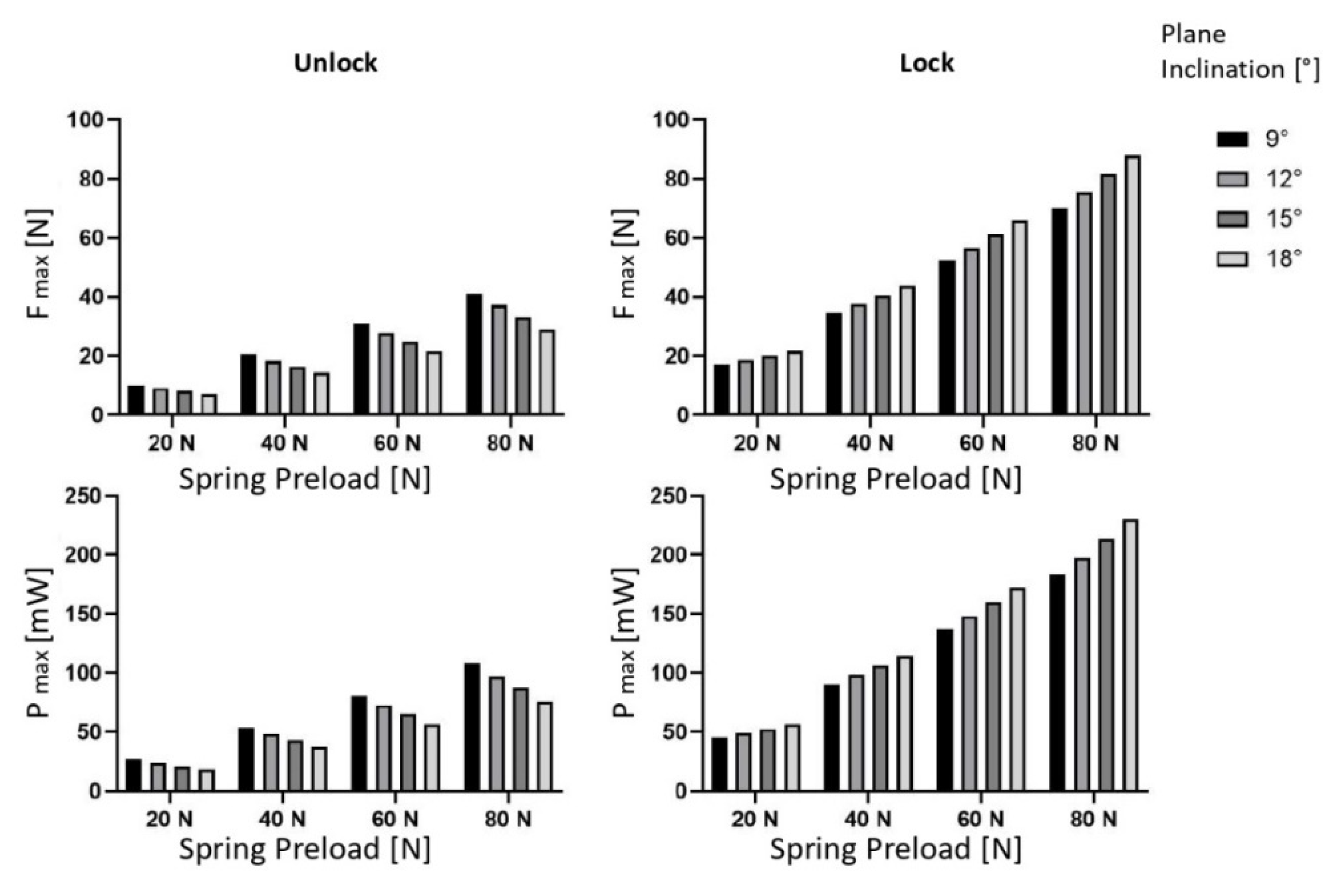
2.1. Multibody Analysis
- Friction coefficients between the inclined plane and the pin head, between the inclined plane and the main body, and between the pin and its housing;
- The stiffness and the preload of the spring;
- The angle of inclination of the sliding plane.
- The pin is free to translate vertically, with a given friction;
- The inclined plane is free to translate horizontally with respect to the main body, with a given friction;
- The contact between the main body and the guide were modelled by means of an impact formulation, where a high contact stiffness value was assigned considering that both parts are made of metal (stiffness k = 100,000 N/mm, damping c = 10 Ns/mm).
- The inclined plane was forced to move horizontally, with a sinusoidal waveform x = 5 sin(2π/12 t) in order to reproduce both the release and the subsequent lock in 6 s.
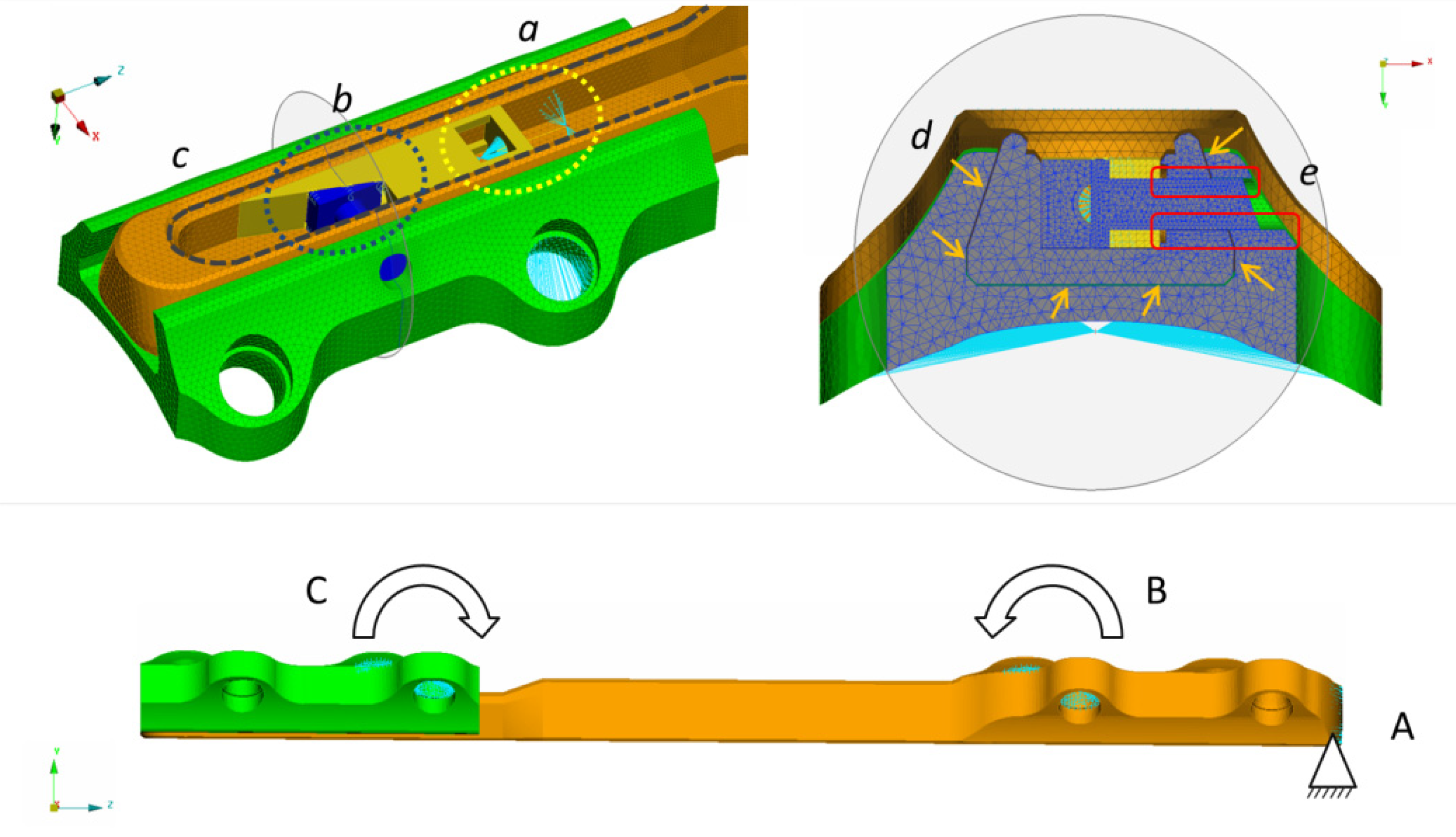
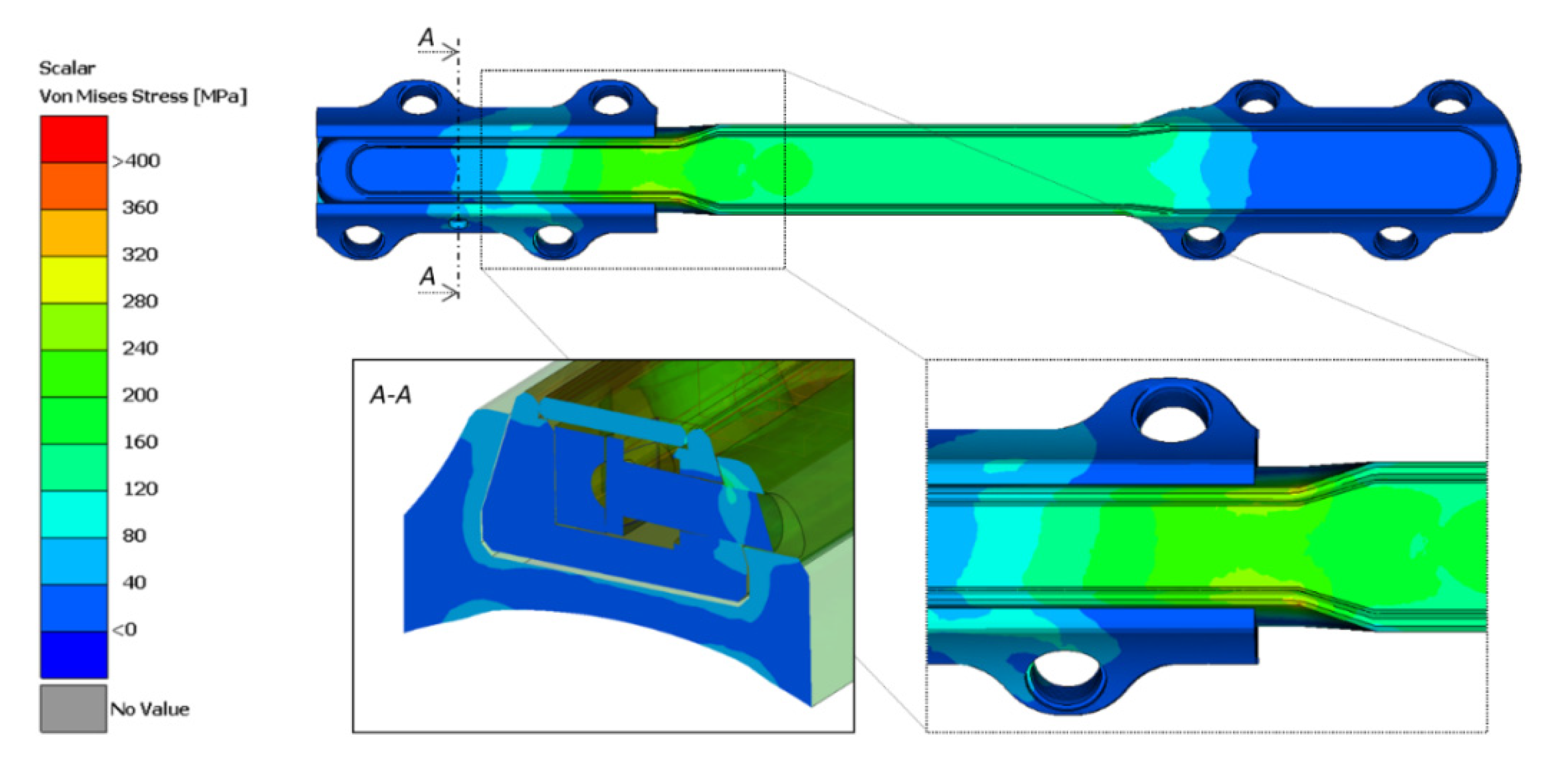
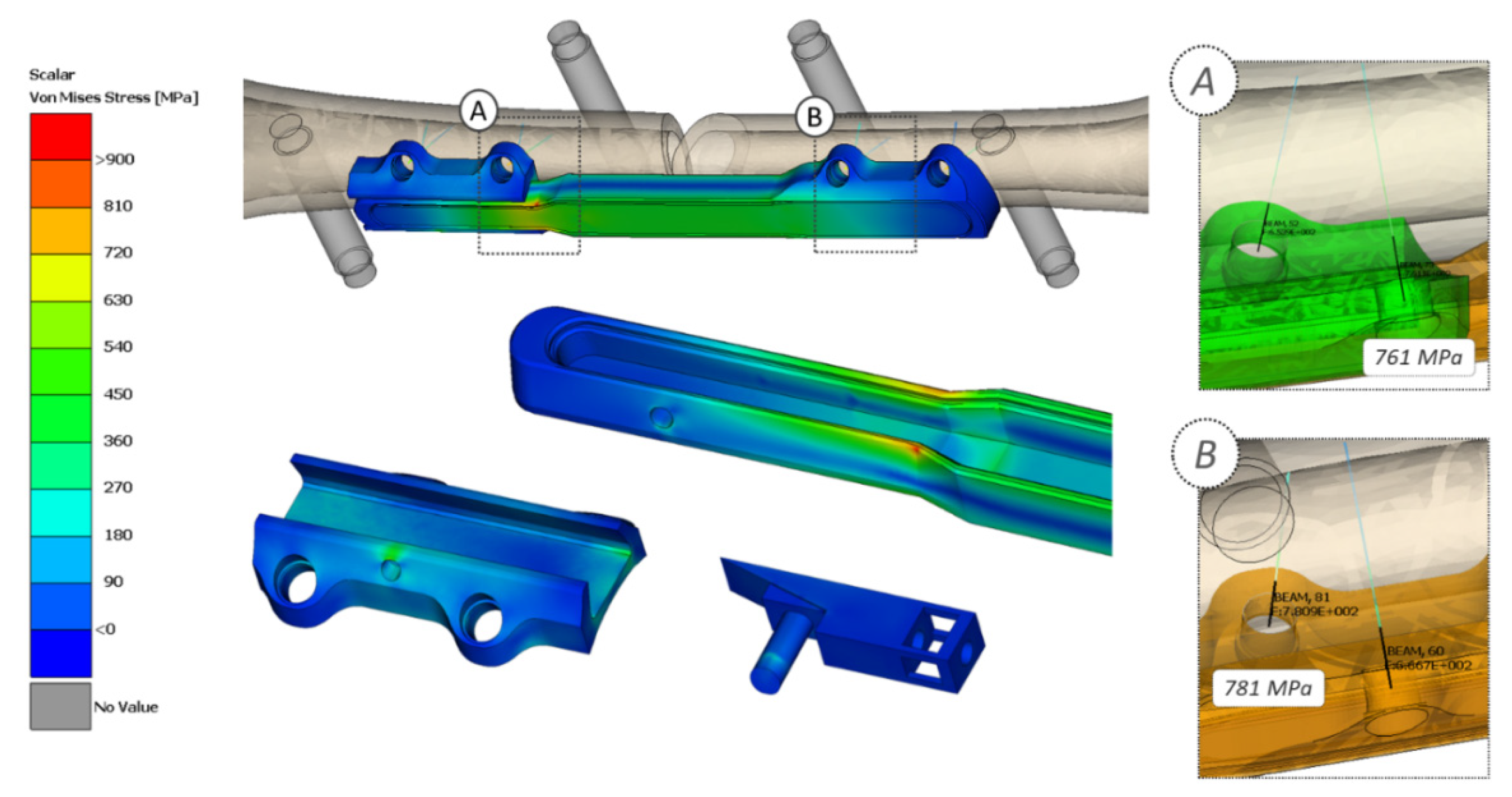
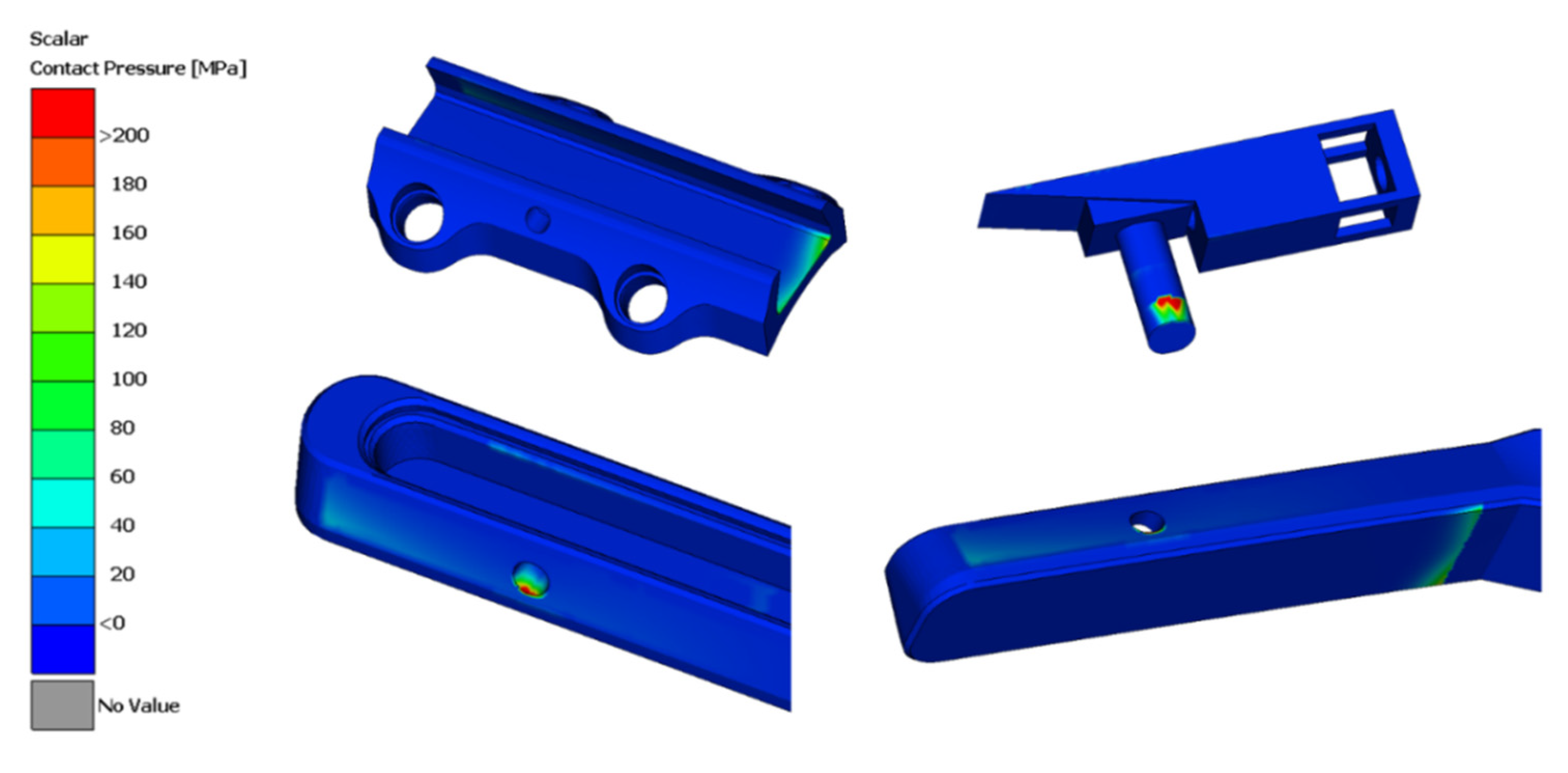
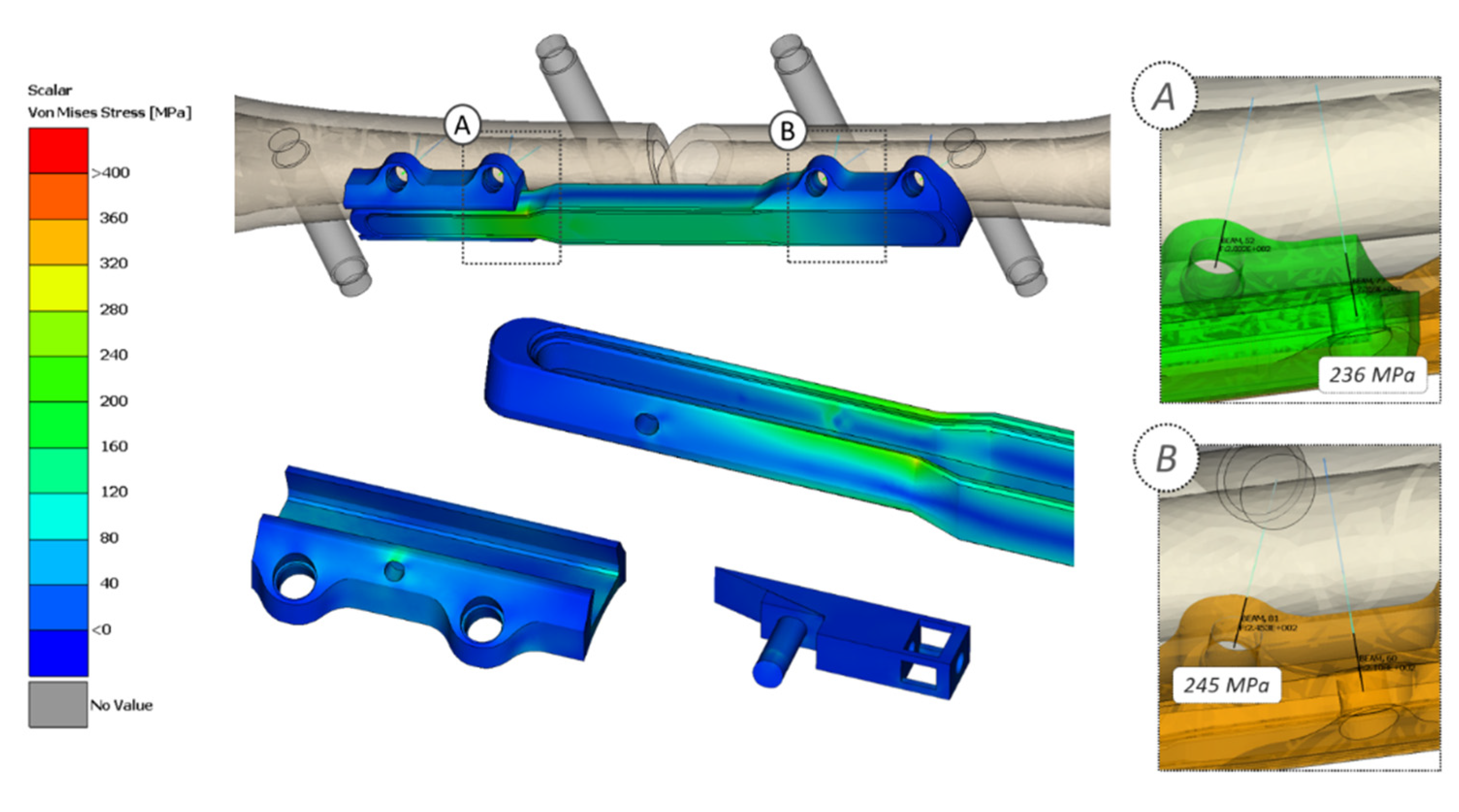
2.2. Stress Analysis
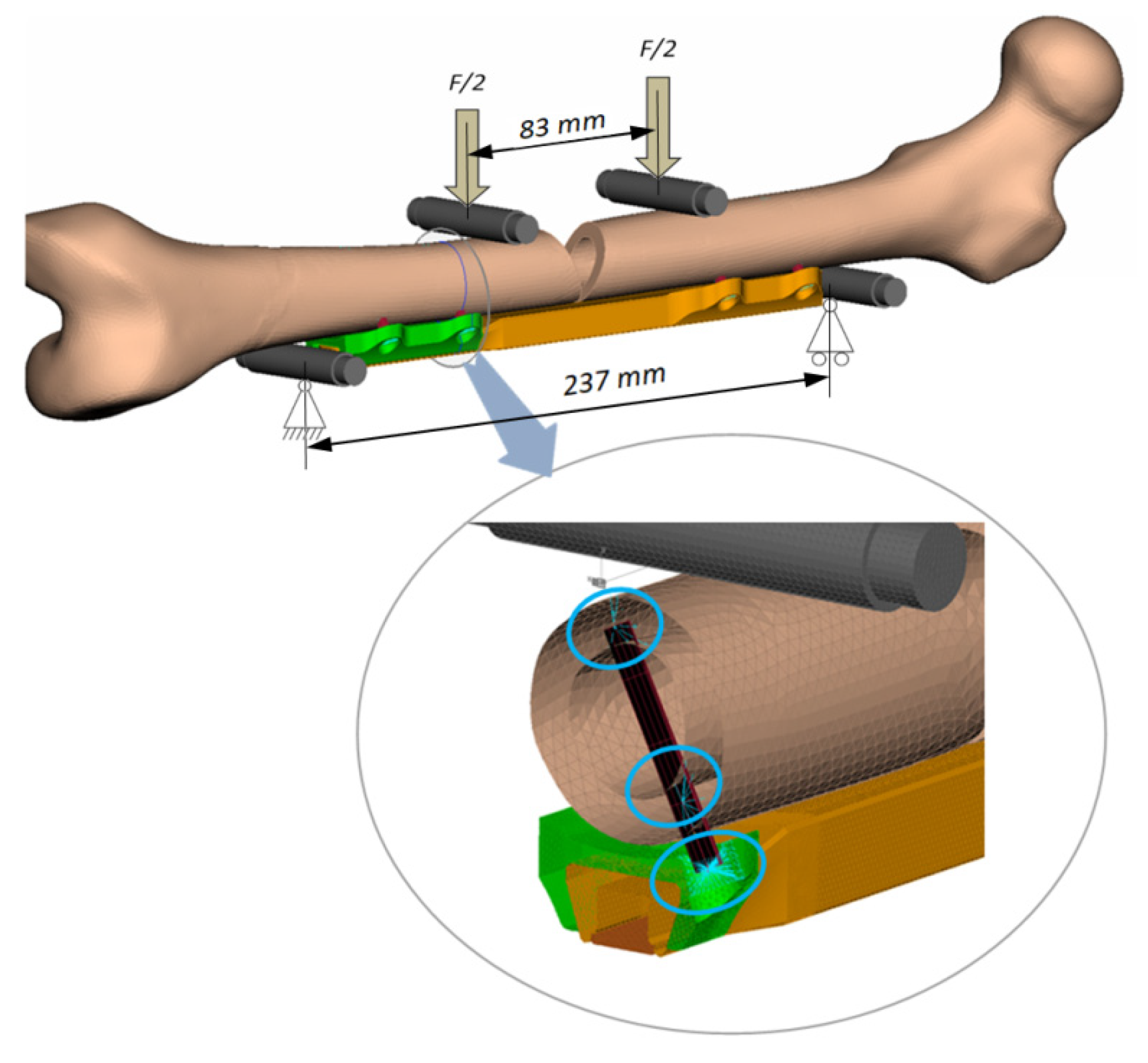
- A standard femur (Sawbones®, Europe AB, Malmoe, Sweden), whose geometry was modified in order to reproduce a central fracture with the classical “V shape” cutting having 20 mm base;
- Four metallic rollers were modelled and positioned in order to reproduce the exact loading setup of the four-point bending test (prescribed by ASTM F382 regulation);
- The plate–bone connections were modelled with rigid kinematic joints (RBE2) connected to each other with specific flexible elements (circular beams whose minimum section has a diameter equal to 3.5 mm) in order to reproduce the screws contribution inside the model.
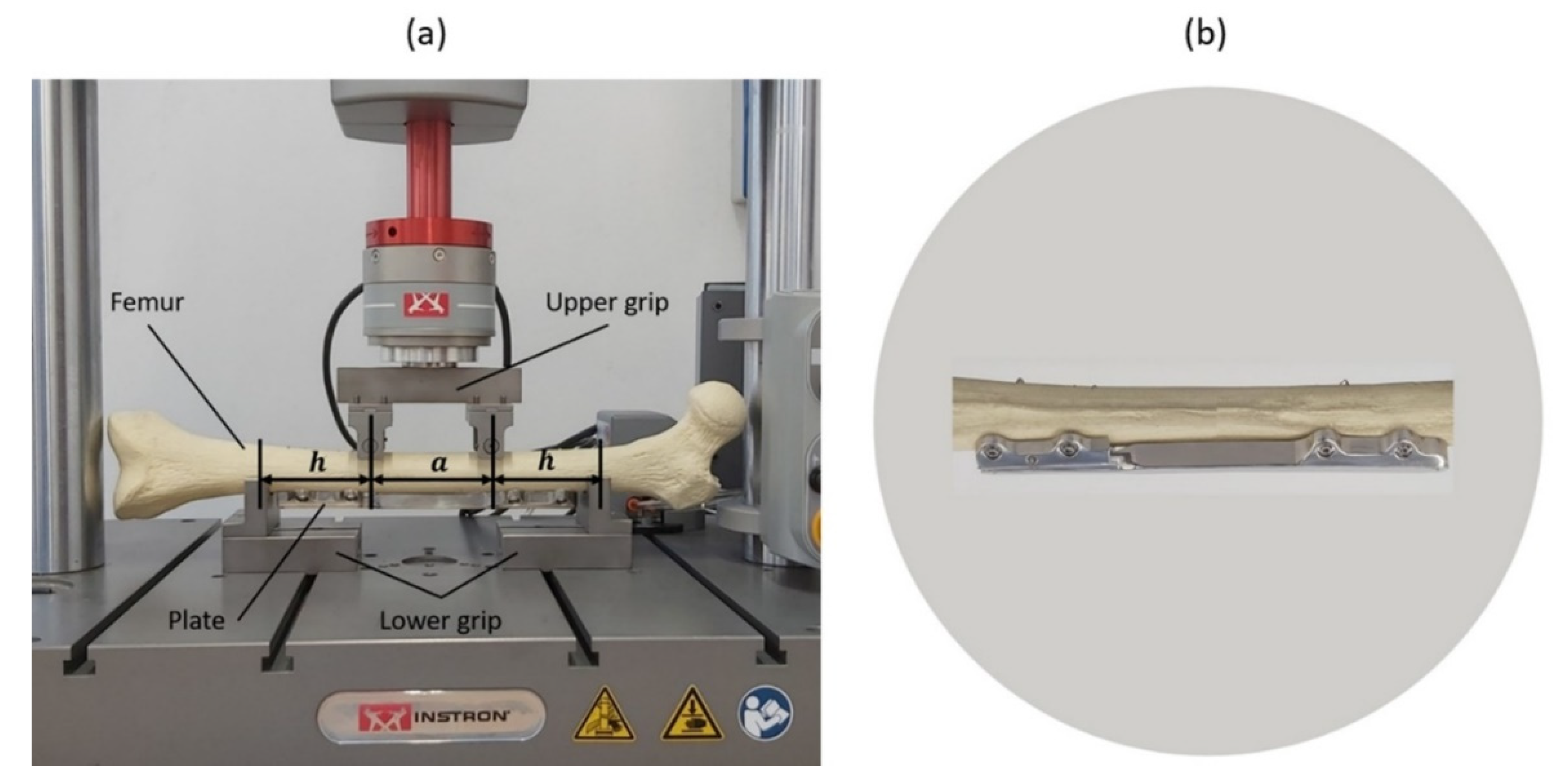
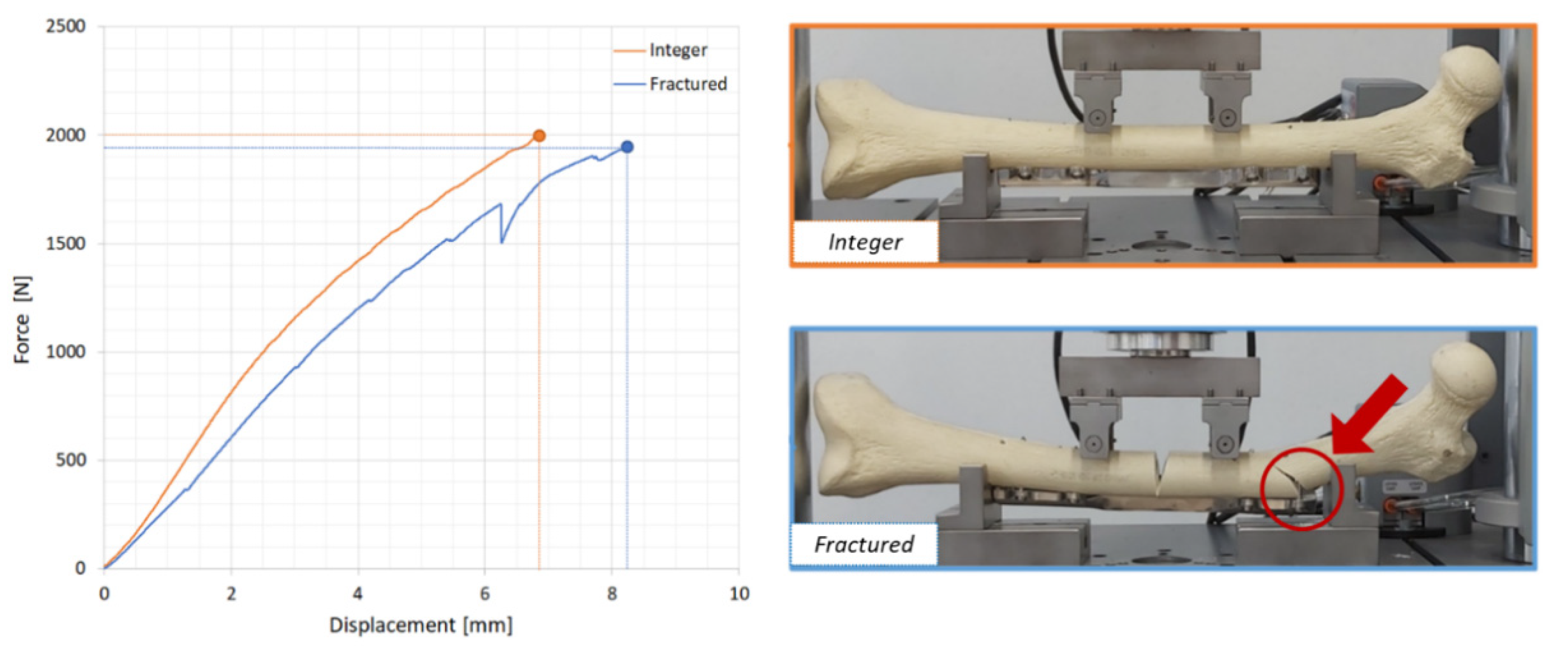
2.3. Experimental Tests
- The upper grip bears two rollers, whose distance was set equal to ‘a’ (83 mm);
- The lower grip bears two supports, whose distance is equal to ‘2 h + a’ (237 mm).
2.4. Manufacturing Flow
3. Results and Discussion
3.1. Output of the Multibody Model
3.2. Output of the Finite Element Model
3.3. Experimental Tests
3.4. Manufacturing Flow
- Step 1: Sourcing of raw materials;
- Step 2: Machine processing: folding, milling, drilling, threading, wire erosion; roughing, burr removal; washing; packaging in labelled bags;
- Step 3: Acceptance check;
- Step 4: Acceptance; belt sanding; polishing; washing; final check; packaging, shipping;
- Step 5: Solvent washing; sandblasting; quality control (QC), single packaging in plastic trays;
- Step 6: Acceptance check;
- Step 7: Marking; washing; preliminary packaging (Clean Room ISO 7 Operational);
- Step 8: Sterilization;
- Step 9: Acceptance check;
- Step 10: Final packaging and labelling; release.
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mujtaba, A. Characteristics on fractures of tibia and fibula in car impacts to pedestrians and bicyclists—Influences of car bumper height and shape. Annu. Proc. Assoc. Adv. Automot. Med. 2007, 67, 14–21. [Google Scholar]
- Gulati, D.; Aggarwal, A.N.; Kumar, S.; Agarwal, A. Skeletal injuries following unintentional fall from height. Turk. J. Trauma Emerg. Surg. 2012, 18, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Axelrod, T.; McMurtry, R. Open reduction and internal fixation of comminuted, intraarticular fractures of the distal radius. J. Hand Surg. 1990, 15, 1–11. [Google Scholar] [CrossRef]
- Terzini, M.; Mossa, L.; Bignardi, C.; Costa, P.; Audenino, A.L.; Vezzoni, A.; Zanetti, E.M. A structural numerical model for the optimization of double pelvic osteotomy in the early treatment of canine hip dysplasia. Veter. Comp. Orthop. Traumatol. 2017, 30, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Pascoletti, G.; Cianetti, F.; Putame, G.; Terzini, M.; Zanetti, E.M. Numerical simulation of an intramedullary elastic nail: Expansion phase and load-bearing behavior. Front. Bioeng. Biotechnol. 2018, 6, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sonderegger, J.; Grob, K.R.; Kuster, M.S. Dynamic plate osteosynthesis for fracture stabilization: How to do it. Orthop. Rev. 2010, 2, 4. [Google Scholar] [CrossRef] [PubMed]
- Henschel, J.; Tsai, S.; Fitzpatrick, D.C.; Marsh, J.L.; Madey, S.M.; Bottlang, M. Comparison of 4 methods for dynamization of locking plates. J. Orthop. Trauma 2017, 31, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Bottlang, M.; Tsai, S.; Bliven, E.K.; Von Rechenberg, B.; Klein, K.; Augat, P.; Henschel, J.; Fitzpatrick, D.C.; Madey, S.M. Dynamic stabilization with active locking plates delivers faster, stronger, and more symmetric fracture-healing. J. Bone Jt. Surg. Am. Vol. 2016, 98, 466–474. [Google Scholar] [CrossRef]
- Claes, L.; Wilke, H.J.; Augat, P.; Rübenacker, S.; Margevicius, K. Effect of dynamization on gap healing of diaphyseal fractures under external fixation. Clin. Biomech. 1995, 10, 227–234. [Google Scholar] [CrossRef]
- Larsson, S.; Kim, W.; Caja, V.L.; Egger, E.L.; Inoue, N.; Chao, E.Y. Effect of early axial dynamization on tibial bone healing. Clin. Orthop. Relat. Res. 2001, 388, 240–251. [Google Scholar] [CrossRef] [PubMed]
- Yamaji, T.; Ando, K.; Wolf, S.; Augat, P.; Claes, L. The effect of micromovement on callus formation. J. Orthop. Sci. 2001, 6, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Foxworthy, M.; Pringle, R. Dynamization timing and its effect on bone healing when using the orthofix dynamic axial fixator. Injury 1995, 26, 117–119. [Google Scholar] [CrossRef]
- Yaneva-Deliverska, M.; Deliversky, J.; Lyapina, M. Biocompatibility of medical devices—Legal regulations in the European Union. J. IMAB Annu. Proc. 2015, 21, 705–708. [Google Scholar] [CrossRef]
- Zyga, S. Application of ISO 13485:2003 in biomedical engineering: A systematic review. Int. J. Caring Sci. 2011, 4, 58–65. [Google Scholar]
- El-Domiaty, A.; El-Fadaly, M.; Nassef, A.E. Wear characteristics of ultrahigh molecular weight polyethylene (UHMWPE). J. Mater. Eng. Perform. 2002, 11, 577–583. [Google Scholar] [CrossRef]
- Terzini, M.; Serino, G.; Lugas, T.A.; Dichio, G.; Costa, P.; Audenino, A.L. Strategies to Speed up the Standardized Bone Plates Mechanical Testing for Regulatory Purposes; Pedrizetti, G., Accardo, A., Marceglia, S., Brun, F., Eds.; 2020; Available online: https://portal.issn.org/resource/ISSN/2724-2129 (accessed on 29 September 2020).
- Zanetti, E.M.; Ciaramella, S.; Calì, M.; Pascoletti, G.; Martorelli, M.; Asero, R.; Watts, D.C. Modal analysis for implant stability assessment: Sensitivity of this methodology for different implant designs. Dent. Mater. 2018, 34, 1235–1245. [Google Scholar] [CrossRef] [PubMed]
- Pascoletti, G.; Calì, M.; Bignardi, C.; Conti, P.; Zanetti, E.M. Mandible morphing through principal components analysis. In International Conference on Design, Simulation, Manufacturing: The Innovation Exchange; Springer: Cham, Switzerland, 2019; pp. 15–23. [Google Scholar]
- Ambu, R.; Motta, A.; Calì, M. Design of a customized neck orthosis for FDM manufacturing with a new sustainable bio-composite. In International Conference on Design, Simulation, Manufacturing: The Innovation Exchange; Springer: Cham, Switzerland, 2019; pp. 707–718. [Google Scholar]
- L. KLEIN SA. AISI 316 LVM Implant: Materials and Raw Manufacturing Data. Available online: http://www.kleinmetals.ch/steel/316-lvm-f-138-implants.htm (accessed on 10 August 2020).

| Variable | Value | |
|---|---|---|
| INPUT DATA | Plane Inclination (°) | 9°–18° |
| Friction Coefficient | 0.15–0.60 | |
| Spring Pre-load (N) | 20–80 | |
| Spring Stiffness (N/mm) | 20 | |
| Input Displacement (mm) | 5 sin(2π/12 t) | |
| OUTPUT DATA | Force Maximum (N) Power Required (mW) |
| Component | Element Type | Number of Elements | Element Size (mm) | Material Type |
|---|---|---|---|---|
| Main Body | 3D Tetra4 | 415,456 | 0.3–0.8 | AISI 316LVM |
| Guide | 3D Tetra4 | 134,410 | 0.3–0.8 | AISI 316LVM |
| Cover | 3D Tetra4 | 267,582 | 0.4–0.5 | AISI 316LVM |
| Pin | 3D Tetra4 | 46,147 | 0.2–0.3 | AISI 316LVM |
| Inclined Plane | 3D Tetra4 | 33,209 | 0.4–0.5 | AISI 316LVM |
| Bone | 3D Tetra4 | 230,396 | 1.8–2.2 | Sawbones® |
| Rollers | 2D Shell | 21,336 | 0.8–1.2 | Stainless steel |
| Screws | 1D Beam | 4 × 8 | 7 × 3.5 | Stainless steel |
| Total n° of Elements: | 1,148,568 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dichio, G.; Calì, M.; Terzini, M.; Putame, G.; Zanetti, E.M.; Costa, P.; Audenino, A.L. Engineering and Manufacturing of a Dynamizable Fracture Fixation Device System. Appl. Sci. 2020, 10, 6844. https://doi.org/10.3390/app10196844
Dichio G, Calì M, Terzini M, Putame G, Zanetti EM, Costa P, Audenino AL. Engineering and Manufacturing of a Dynamizable Fracture Fixation Device System. Applied Sciences. 2020; 10(19):6844. https://doi.org/10.3390/app10196844
Chicago/Turabian StyleDichio, Giancarlo, Michele Calì, Mara Terzini, Giovanni Putame, Elisabetta Maria Zanetti, Piero Costa, and Alberto Luigi Audenino. 2020. "Engineering and Manufacturing of a Dynamizable Fracture Fixation Device System" Applied Sciences 10, no. 19: 6844. https://doi.org/10.3390/app10196844
APA StyleDichio, G., Calì, M., Terzini, M., Putame, G., Zanetti, E. M., Costa, P., & Audenino, A. L. (2020). Engineering and Manufacturing of a Dynamizable Fracture Fixation Device System. Applied Sciences, 10(19), 6844. https://doi.org/10.3390/app10196844







