AI-Based Stroke Disease Prediction System Using Real-Time Electromyography Signals
Abstract
1. Introduction
2. Related Works
2.1. Concept of Stroke
2.2. Stroke Prediction Using Traditional Techniques
2.3. Stroke Prediction Using Machine Learning and Deep Learning
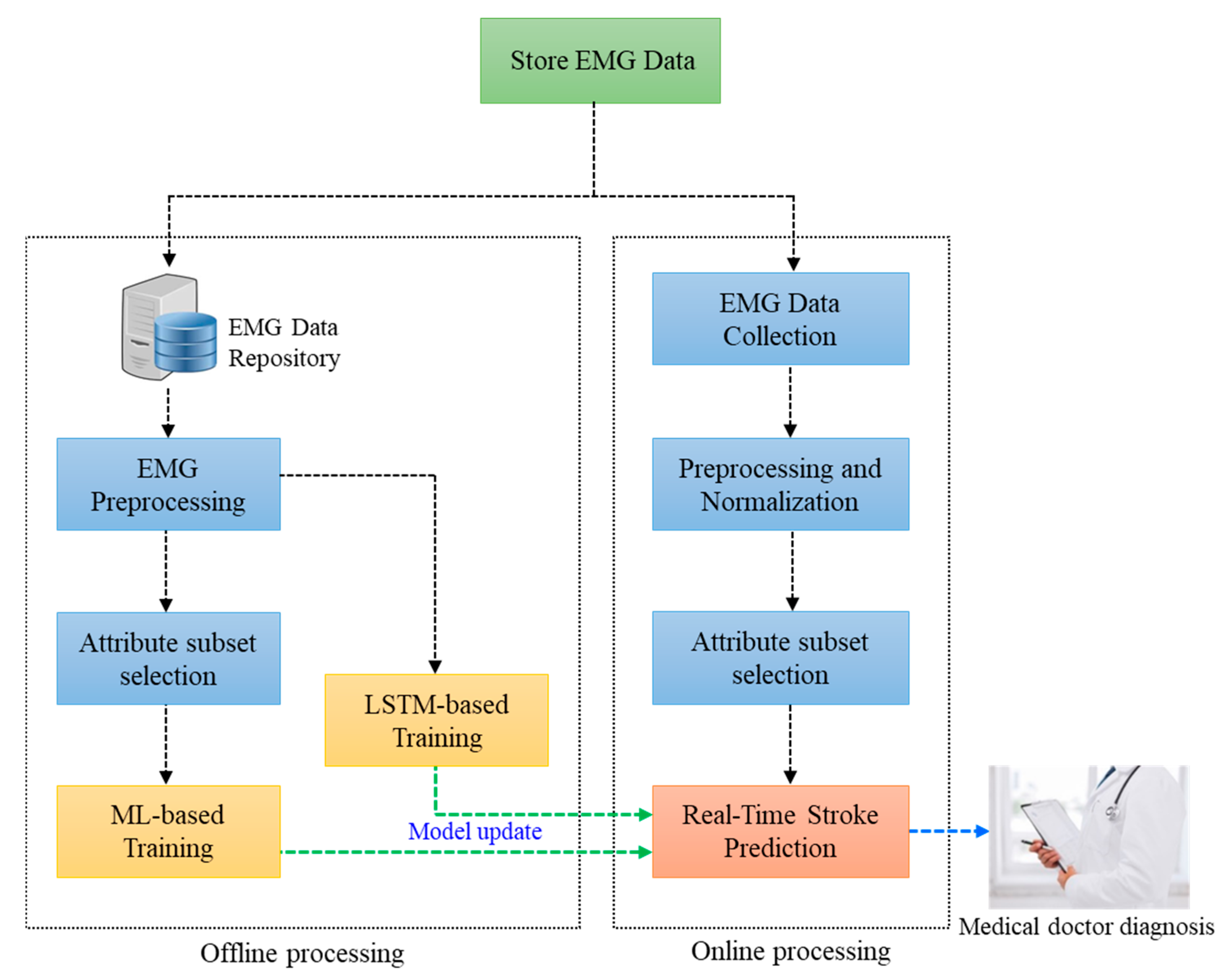
3. Artificial Intelligence-Based Stroke Disease Prediction System Using EMG
4. Experiments and Analysis
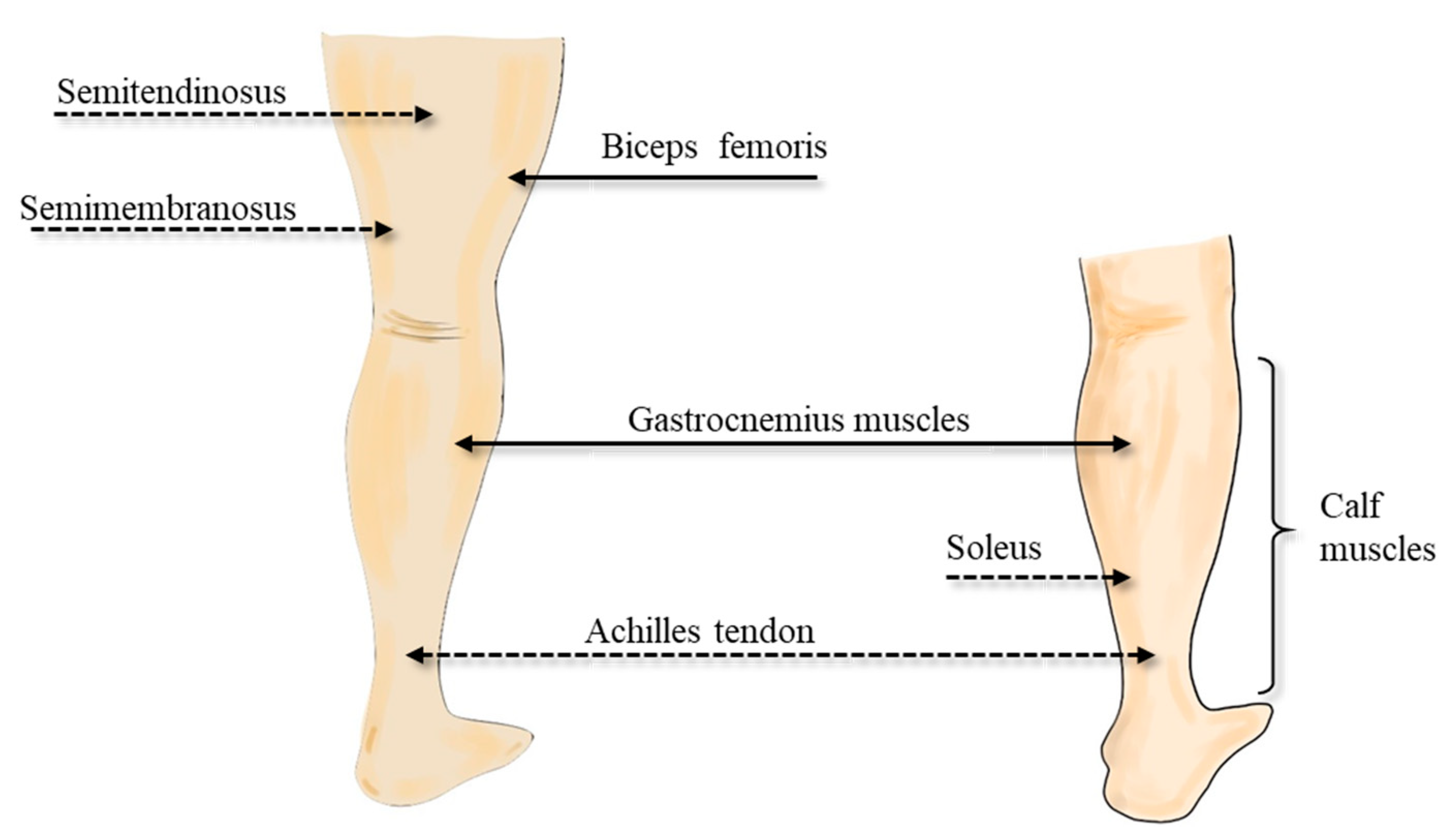
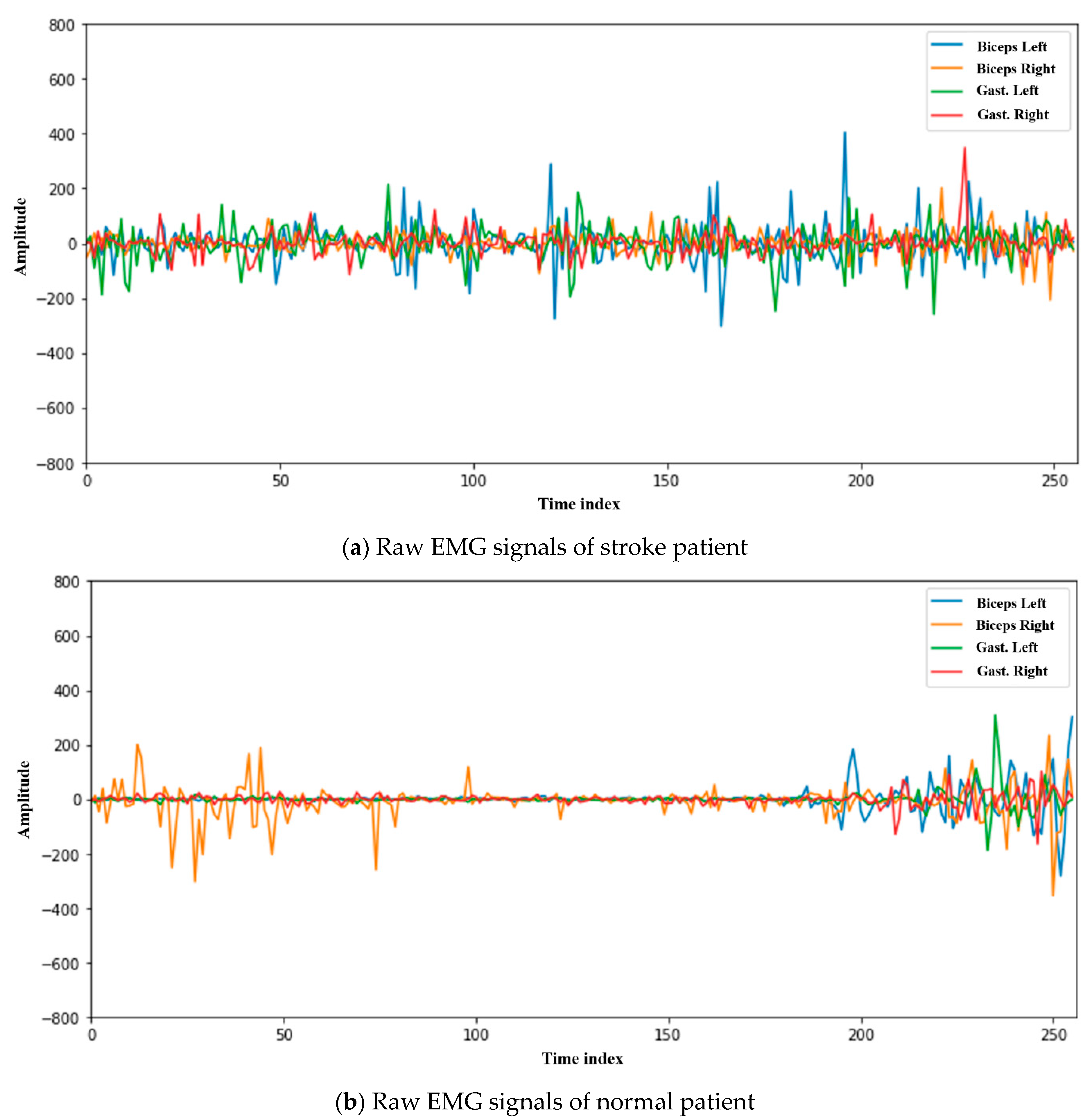
4.1. Dataset and Experimental Analysis
4.2. Experiment and Analysis Based on Machine Learning
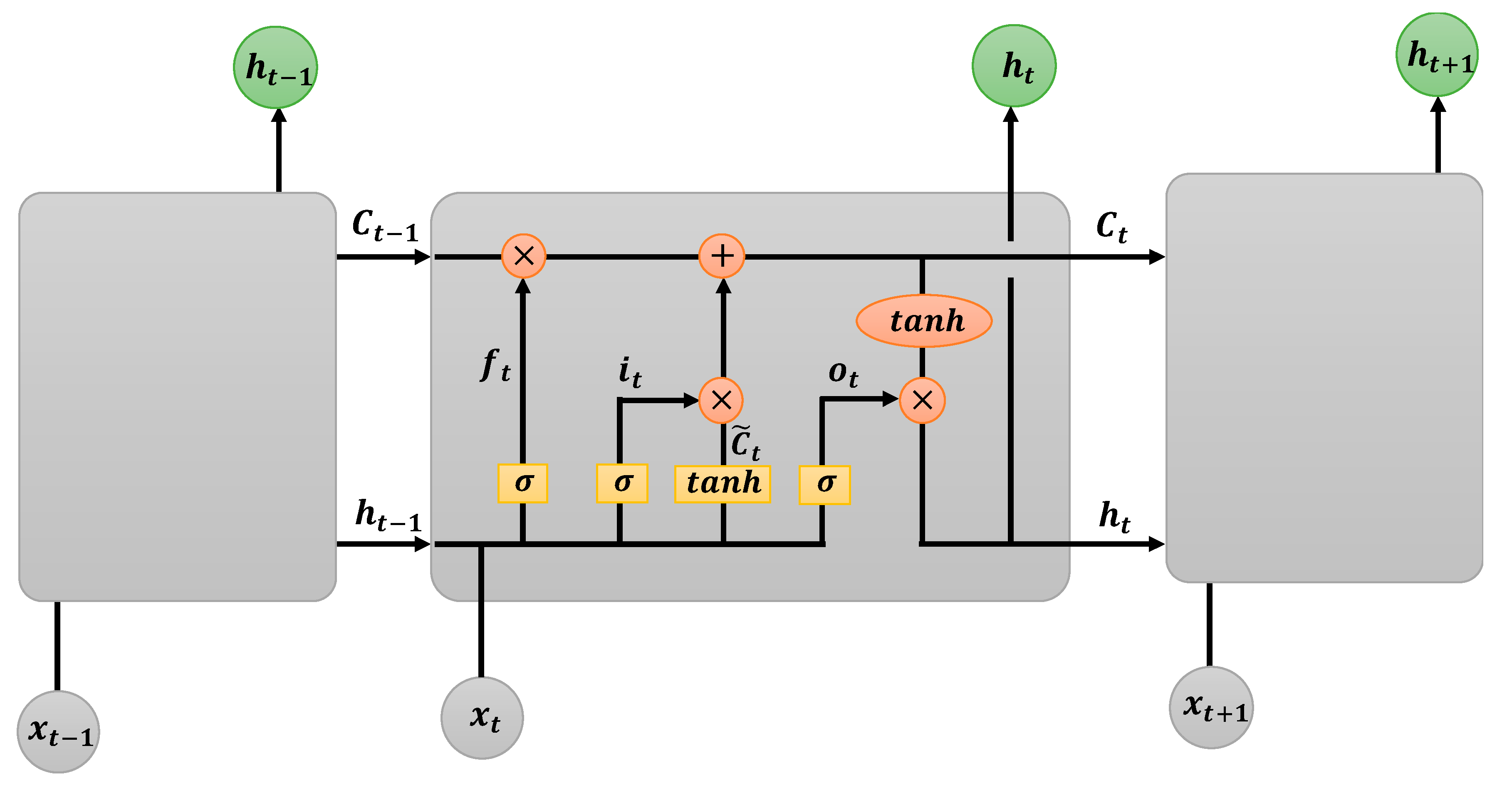
4.3. Experiment and Analysis Based on Deep Learning
4.4. Results and Discussions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mohammadi, M.; Al-Fuqaha, A.; Sorour, S.; Guizani, M. Deep learning for IoT Big data and streaming analytics: A survey. IEEE Commun. Surv. Tutor. 2018, 20, 2923–2960. [Google Scholar] [CrossRef]
- Ajayi, O.O.; Bagula, A.B.; Ma, K. Fourth industrial revolution for development: The relevance of Cloud federation in healthcare support. IEEE Access 2019, 7, 185322–185337. [Google Scholar] [CrossRef]
- Morrar, R.; Arman, H.; Mousa, S. The fourth industrial revolution (Industry 4.0): A social innovation perspective. Technol. Innov. Manag. Rev. 2017, 7, 12–20. [Google Scholar] [CrossRef]
- Garcia, A.R. AI, IoT, Big data, and technologies in digital economy with blockchain at sustainable work satisfaction to smart mankind: Access to 6th dimension of human rights. In Smart Governance for Cities: Perspectives and Experiences, 2nd ed.; Lopes, N.V.M., Ed.; Springer: Gewerbestrasse, Switzerland, 2020; pp. 83–131. [Google Scholar]
- Johnson, C.O.; Nguyen, M.; Roth, G.A.; Nichols, E.; Alam, T. Global, regional, and national burden of stroke, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 439–458. [Google Scholar] [CrossRef]
- Subudhi, A.; Dash, M.; Sabut, S. Automated segmentation and classification of brain stroke using expectation-maximization and random forest classifier. Biocybern. Biomed. Eng. 2020, 40, 277–289. [Google Scholar] [CrossRef]
- Lee, H.J.; Lee, J.S.; Choi, J.C.; Cho, Y.J.; Kim, B.J.; Bae, H.J.; Kim, D.E.; Ryu, W.S.; Cha, J.K.; Kim, D.H.; et al. Simple estimates of symptomatic intracranial hemorrhage risk and outcome after intravenous thrombolysis using age and stroke severity. J. Stroke 2017, 19, 229–231. [Google Scholar] [CrossRef]
- Kim, Y.D.; Jung, Y.H.; Saposnik, G. Traditional risk factors for stroke in East Asia. J. Stroke 2016, 18, 273–285. [Google Scholar] [CrossRef]
- Poorthuis, M.H.; Algra, A.M.; Algra, A.; Kappelle, L.J.; Klijn, C.J. Female-and male-specific risk factors for stroke: A systematic review and meta-analysis. JAMA Neurol. 2017, 29, 86–93. [Google Scholar] [CrossRef]
- Malik, V.; Ganesan, A.N.; Selvanayagam, J.B.; Chew, D.P.; McGavigan, A.D. Is atrial fibrillation a stroke risk factor or risk marker? An appraisal using the bradford hill framework for causality. J. Heart Lung Circ. 2020, 29, 86–93. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. The Third National Health and Nutrition Examination Survey (NHANES III 1988-94) Reference Manuals and Reports. National Center for Health Statistics: Bethesda, MD, USA, 1996. Available online: https://wwwn.cdc.gov/nchs/nhanes/nhanes3/ManualsAndReports.aspx (accessed on 27 September 2020).
- Wolf, P.A.; D’Agostino, R.B.; Belanger, A.J.; Kannel, W.B. Probability of stroke: A risk profile from the Framingham study. Am. Heart Assoc. 1991, 22, 312–318. [Google Scholar] [CrossRef]
- D’Agostino Wolf, P.A.; Belanger, A.J.; Kannel, W.B. Stroke risk profile: Adjustment for antihypertensive medication: The Framingham Study. Am. Heart Assoc. 1994, 25, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Hense, H.W.; Schulte, H.; Lowel, H.; Assmann, G.; Kell, U. Framingham risk function overestimates risk of coronary heart disease in men and women from Germany-results from the MONICA Augsburg and the RPOCAM cohorts. Eur. Heart J. 2003, 24, 937–945. [Google Scholar] [CrossRef]
- Menotti, A.; Lanti, M.; Puddu, P.E.; Kromhout, D. Coronary heart disease incidence in northern and southern European populations: A reanalysis of the seven countries study for a European coronary risk chart. Heart 2000, 84, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Hong, Y.; D’Agostino Sr, R.B.; Wu, Z.; Wang, W.; Sun, J.; Wilson, P.W.F.; Kannel, W.B.; Zhao, D. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese multi-provincial cohort study. JAMA Netw. 2004, 291, 2591–2599. [Google Scholar] [CrossRef]
- Jee, S.H.; Park, J.W.; Lee, S.Y.; Nam, B.H.; Ryu, H.G.; Kim, S.Y.; Kim, Y.N.; Lee, J.K.; Choi, S.M.; Yun, J.E. Stroke risk prediction model: A risk profile from the Korean study. Atherosclerosis 2008, 197, 318–325. [Google Scholar] [CrossRef]
- Yu, J.; Kim, D.; Park, H.; Chon, S.; Cho, K.; Kim, S.; Yu, S.; Park, S.; Hong, S. Semantic Analysis of NIH stroke scale using machine learning techniques. In Proceedings of the 2019 International Conference on Platform Technology and Service (PlatCon), Jeju, Korea, 28–30 January 2019; pp. 82–86. [Google Scholar]
- Zhang, Q.; Xie, Y.; Ye, P.; Pang, C. Acute ischaemic stroke prediction from physiological time series patterns. Australas. Med. J. 2013, 6, 280–286. [Google Scholar] [CrossRef]
- Sengupta, A.; Rajan, V.; Bhattacharya, S.; Sarma, G.R.K. A statistical model for stroke outcome prediction and treatment planning. In Proceedings of the 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 2516–2519. [Google Scholar]
- Statistics Korea. The Cause of Death Statistics in Koreans. Available online: http://kostat.go.kr/portal/korea/kor_nw/1/6/2/index.board (accessed on 27 September 2020).
- Bushnell, C.D.; Johnston, D.C.; Goldstein, L.B. Retrospective assessment of initial stroke severity: Comparison of the NIH stroke scale and the Canadian neurological scale. J. Stroke 2001, 32, 656–660. [Google Scholar] [CrossRef]
- Lai, S.M.; Duncan, P.W.; Keighley, J. Prediction of functional outcome after stroke: Comparison of the orpington prognostic scale and the NIH stroke scale. Am. Heart Assoc. 1998, 29, 1838–1842. [Google Scholar] [CrossRef]
- Meyer, B.C.; Lyden, P.D. The modified National Institutes of Health Stroke Scale: Its time has come. Int. J. Stroke 2009, 4, 267–273. [Google Scholar] [CrossRef]
- Lee, J.S.; Park, J.M.; Park, T.H.; Lee, K.B.; Lee, S.J.; Cho, Y.J.; Han, M.K.; Bae, H.J.; Lee, J.Y. Development of a stroke prediction model for Korean. Korean Neurol. Assoc. 2010, 28, 13–21. [Google Scholar]
- Trialists’ Collaboration Antithrombotic. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. Br. Med. J. (BMJ) 2002, 324, 71–86. [Google Scholar] [CrossRef]
- Kannel, W.B.; McGee, D.L.; Castelli, W.P. Latest perspectives on cigarette smoking and cardiovascular disease: The Framingham study. J. Card. Rehabil. 1984, 4, 267–277. [Google Scholar]
- Carroll, K.J. On the use and utility of the Weibull model in the analysis of survival data. Control. Clin. Trials 2003, 24, 682–701. [Google Scholar] [CrossRef]
- Burn, J.; Dennis, M.; Bamford, J.; Sandercock, P.; Wade, D. Long-term risk of recurrent stroke after a first-ever stroke. Am. Heart Assoc. 1994, 25, 333–337. [Google Scholar]
- Lee, H.R.; Ham, O.K.; Lee, Y.W.; Cho, I.; Oh, H.S.; Rha, J. Knowledge, health-promoting behaviors, and biological risks of recurrent stroke among stroke patients in Korea. Jpn. J. Nurs. Sci. 2014, 11, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Finnigan, S.; van Putten, M.J.A.M. EEG in ischaemic stroke: Quantitative EEG can uniquely inform (sub-)acute prognoses and clinical management. Clin. Neurophysiol. 2013, 124, 10–19. [Google Scholar] [CrossRef]
- Chien, K.L.; Su, T.C.; Hsu, H.C.; Chang, W.T.; Chen, P.C. Constructing the prediction model for the risk of stroke in a Chinese population: Report from a cohort study in Taiwan. J. Stroke 2010, 41, 1858–1864. [Google Scholar] [CrossRef]
- Song, Q.; Liu, X.; Zhou, W.; Wang, L.; Zheng, X.; Wang, X. Long sleep duration and risk of ischemic stroke and hemorrhagic stroke: The Kailuan prospective study. Sci. Rep. 2016, 6, 1–9. [Google Scholar] [CrossRef]
- Shanthi, D.; Sahoo, G.; Saravanan, N. Designing an artificial neural network model for the prediction of thrombo-embolic stroke. Int. J. Biom. Bioinform. (IJBB) 2009, 3, 10–18. [Google Scholar]
- Kasabov, N.; Feigin, V.; Hou, Z.G.; Chen, Y.; Liang, L.; Krishnamurthi, R.; Othman, M.; Parmar, P. Evolving spiking neural networks for personalised modelling, classification and prediction of spatio-temporal patterns with a case study on stroke. Neurocomputing 2014, 134, 269–279. [Google Scholar] [CrossRef]
- Singh, M.S.; Choudhary, P.; Thongam, K. A Comparative Analysis for Various Stroke Prediction Techniques. In Proceedings of the International Conference on Computer Vision and Image Processing (CVIP 2019), Jaipur, India, 27–29 September 2019; pp. 98–106. [Google Scholar]
- Huang, S.; Shen, Q.; Duong, T.Q. Artificial neural network prediction of ischemic tissue fate in acute stroke imaging. J. Cereb. Blood Flow Metab. 2010, 30, 1661–1670. [Google Scholar] [CrossRef] [PubMed]
- Bentley, P.; Ganesalingam, J.; Jones, A.L.C.; Mahady, K.; Epton, S.; Rinne, P.; Sharma, P.; Halse, O.; Mehta, A.; Rueckert, D. Prediction of stroke thrombolysis outcome using CT brain machine learning. NeuroImage Clin. 2014, 4, 635–640. [Google Scholar] [CrossRef] [PubMed]
- Khosla, A.; Cao, Y.; Lin, C.C.Y.; Chiu, H.K.; Hu, J.; Lee, H. An integrated machine learning approach to stroke prediction. In Proceedings of the 16th ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, Washington, DC, USA, 24–28 July 2010; pp. 183–192. [Google Scholar]
- Amini, L.; Azarpazhouh, R.; Farzadfar, M.T.; Mousavi, S.A.; Jazaieri, F.; Khorvash, F.; Norouzi, R.; Toghianfar, N. Prediction and control of stroke by data mining. Int. J. Prev. Med. 2013, 4, 245–249. [Google Scholar]
- Pascanu, R.; Gulcehre, C.; Cho, K.; Bengio, Y. How to construct deep recurrent neural networks. arXiv 2013, arXiv:1312.6026. Available online: https://arxiv.org/abs/1312.6026 (accessed on 27 September 2020).
- Hochreiter, S.; Schmidhuber, J. Long short-term memory. Neural Comput. 1997, 9, 1735–1780. [Google Scholar] [CrossRef] [PubMed]
- Xiao, X.; Zhang, S.; Mercaldo, F.; Hu, G.; Sangaiah, A.K. Android malware detection based on system call sequences and LSTM. Multimed. Tools Appl. 2019, 78, 3979–3999. [Google Scholar] [CrossRef]
- MathWorks, Inc. Long Short-Term Memory Networks. Available online: https://www.https://www.mathworks.com/help/deeplearning/ug/long-short-term-memory-networks.html (accessed on 27 September 2020).
- Chantamit, P.; Goyal, M. Long short-term memory recurrent neural network for stroke prediction. In Proceedings of the International Conference on Machine Learning and Data Mining in Pattern Recognition (MLDM 2018), New York, NY, USA, 15–19 July 2018; pp. 312–323. [Google Scholar]
- WHO. ICD-10: International Statistical Classification of Disease and Related Health Tenth Revision. Volume 2, Geneva. 2004. Available online: https://www.who.int/classifications/icd/ICD-10_2nd_ed_volume2.pdf (accessed on 27 September 2020).
- Yu, Y.; Parsi, B.; Speier, W.; Arnold, C.; Lou, M.; Scalzo, F. LSTM Network for Prediction of Hemorrhagic Transformation in Acute Stroke. In Proceedings of the International Conference on Medical Image Computing and Computer-Assisted Intervention (MICCAI 2019), Shenzhen, China, 13–17 October 2019; pp. 177–185. [Google Scholar]
- Klomp, A.; Van der Krogt, J.M.; Meskers, C.G.M.; De Groot, J.H.; De Vlugt, E.; Van der Helm, F.C.T.; Arendzen, J.H. Design of a concise and comprehensive protocol for post stroke neuromechanical assessment. J. Bioeng Biomed. Sci. 2012, S1, 1–8. [Google Scholar] [CrossRef]
- Schleenbaker, R.E.; Mainous, A.G. Electromyographic biofeedback for neuromuscular reeducation in the hemiplegic stroke patient: A meta-analysis. Arch. Phys. Med. Rehabil. 1993, 74, 1301–1304. [Google Scholar] [CrossRef]
- Pang, M.Y.C.; Eng, J.J.; Dawson, A.S.; McKay, H.A. A community-based fitness and mobility exercise program for older adults with chronic stroke: A randomized, controlled trial. J. Am. Geriatr. Soc. 2005, 53, 1667–1674. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Tinti-Wald, D. Accuracy of weightbearing estimation by stroke versus healthy subjects. Percept. Mot. Ski. 1991, 73, 935–941. [Google Scholar] [CrossRef]
- Shao, Q.; Bassett, D.N.; Manal, K.; Buchanan, T.S. An EMG-driven model to estimate muscle forces and joint moments in stroke patients. Comput. Biol. Med. 2009, 39, 1083–1088. [Google Scholar] [CrossRef] [PubMed]
- Geurts, A.C.H.; Haart, M.D.; Nes, I.J.W.; Duysens, J. A review of standing balance recovery from stroke. Gait Posture 2005, 22, 267–281. [Google Scholar] [CrossRef] [PubMed]
- Hall, M. Correlation-based Feature Selection for Machine Learning. Ph.D. Thesis, Department of Computer Science, The University of Waikato, Hamilton, NZ, USA, 1998. [Google Scholar]
- Yu, J.; Lee, B.B.; Park, D. Real-time cooling load forecasting using a hierarchical multi-class SVDD. Multimed. Tools Appl. 2014, 71, 293–307. [Google Scholar] [CrossRef]


| Contents | Attributes | Description | |
|---|---|---|---|
| Number | |||
| 1 | BFL_Mmax | The value from the lowest point of the negative peak of the left biceps femoris to the positive peak. | |
| 2 | BFR_Mmax | The value from the lowest point of the negative peak of the right biceps femoris to the positive peak. | |
| 3 | LGL_Mmax | The value from the lowest point of the negative peak of the left gastrocnemius muscle to the positive peak. | |
| 4 | LGR_Mmax | The value from the lowest point of the negative peak of the right gastrocnemius muscle to the positive peak. | |
| 5~8 | BFL_PositivePeak, BFR_PositivePeak, LGL_PositivePeak, LGR_PositivePeak | The maximum value of the positive peak based on 0 of biceps femoris/gastrocnemius muscle on the left and right. | |
| 9~12 | BFL_NegativePeak, BFR_NegativePeak, LGL_NegativePeak, LGR_NegativePeak | The minimum value of the negative peak from 0 of the left and right femoral/gastrocnemius muscles. | |
| 13~16 | BFL_5_PPIMean, BFR_5_PPIMean, LGL_5_PPIMean, LGR_5 PPIMean | The average value of the five-forward positive peak-interval (PP-I) based on the current positive peak point of the left/right biceps femoris/gastrocnemius muscle. | |
| 17~20 | BFL_10_PPIMean, BFR_10_PPIMean, LGL_10_PPIMean, LGR_10 PPIMean | The average value of the 10-forward PP-I based on the current positive peak point of the left/right biceps femoris/gastrocnemius muscle. | |
| 21~24 | BFL_5 PPISD, BFR_5 PPISD, LGL_5 PPISD, LGR_5 PPISD | The standard deviation of the five-forward PP-I based on the current positive peak point of the left/right biceps femoris/gastrocnemius muscle. | |
| 25~28 | BFL_10 PPISD, BFR_10 PPISD, LGL_10 PPISD, LGR_10 PPISD | The standard deviation of the 10-forward PP-I based on the current positive peak point of the left/right biceps femoris/gastrocnemius muscle. | |
| 29 | Class Labeling | Normal or Stroke | |
| Data Sets | Train (70)/ Test (30) | Train (80)/ Test (20) | 5-Fold CV | 10-Fold CV 1 | 20-Fold CV | |
|---|---|---|---|---|---|---|
| Methods | ||||||
| C4.5 Decision Tree | 78.22 | 78.23 | 78.78 | 79.65 | 79.43 | |
| C5.0 Decision Tree | 79.48 | 79.68 | 80.01 | 80.32 | 80.29 | |
| Naïve Bayes | 62.82 | 63.06 | 62.81 | 62.80 | 62.85 | |
| Logistic Regression (LR) | 71.45 | 70.25 | 70.33 | 70.33 | 70.33 | |
| ANN (MLP) | 66.16 | 59.17 | 64.47 | 68.63 | 66.15 | |
| Random Forest (RF) | 85.03 | 85.35 | 85.67 | 85.78 | 85.82 | |
| C&RT | 77.25 | 77.38 | 77.44 | 77.48 | 77.59 | |
| CHAID | 77.01 | 77.12 | 77.57 | 77.41 | 77.37 | |
| Two-Class SVM | 71.12 | 70.58 | 71.18 | 71.47 | 71.51 | |
| Data Sets | Train (70)/ Test (30) | Train (80)/ Test (20) | 5-Fold CV | 10-Fold CV | 20-Fold CV | |
|---|---|---|---|---|---|---|
| Methods | ||||||
| C4.5 Decision Tree | 81.25 | 81.42 | 81.73 | 82.46 | 81.97 | |
| C5.0 Decision Tree | 81.68 | 81.78 | 82.44 | 82.65 | 82.61 | |
| Naïve Bayes | 69.60 | 69.54 | 69.88 | 69.89 | 69.86 | |
| Logistic Regression (LR) | 71.16 | 71.09 | 71.23 | 71.26 | 71.28 | |
| ANN (MLP) | 77.98 | 77.94 | 78.56 | 78.78 | 78.79 | |
| Random Forest (RF) | 85.38 | 85.44 | 85.70 | 85.86 | 85.84 | |
| C&RT | 79.89 | 79.86 | 79.95 | 80.16 | 80.12 | |
| CHAID | 79.08 | 79.03 | 79.38 | 79.59 | 79.58 | |
| Two-Class SVM | 73.33 | 73.31 | 73.63 | 74.07 | 73.72 | |
| Data Sets | Train (70)/ Test (30) | Train (80)/ Test (20) | 5-Fold CV | 10-Fold CV | 20-Fold CV | |
|---|---|---|---|---|---|---|
| Methods | ||||||
| C4.5 Decision Tree | 80.08 | 80.58 | 81.90 | 82.20 | 82.27 | |
| C5.0 Decision Tree | 82.48 | 82.65 | 83.11 | 83.15 | 83.18 | |
| Naïve Bayes | 69.25 | 69.14 | 69.58 | 69.60 | 69.58 | |
| Logistic Regression (LR) | 71.08 | 70.90 | 71.13 | 71.16 | 71.13 | |
| ANN (MLP) | 76.70 | 77.73 | 77.62 | 77.53 | 77.68 | |
| Random Forest (RF) | 85.94 | 85.88 | 86.52 | 86.89 | 86.88 | |
| C&RT | 80.59 | 80.56 | 80.72 | 80.89 | 80.78 | |
| CHAID | 80.42 | 80.37 | 80.67 | 80.91 | 80.98 | |
| Two-Class SVM | 74.01 | 73.98 | 74.24 | 74.67 | 74.15 | |
| Data Sets | Train (70)/ Test (30) | Train (80)/ Test (20) | 5-Fold CV | 10-Fold CV | 20-Fold CV | |
|---|---|---|---|---|---|---|
| Methods | ||||||
| C4.5 Decision Tree | 84.23 | 84.94 | 83.89 | 84.39 | 84.56 | |
| C5.0 Decision Tree | 84.41 | 84.58 | 84.86 | 85.02 | 85.16 | |
| Naïve Bayes | 68.37 | 68.44 | 68.89 | 68.91 | 68.89 | |
| Logistic Regression (LR) | 70.04 | 70.23 | 70.33 | 70.28 | 70.31 | |
| ANN (MLP) | 75.60 | 75.58 | 76.01 | 75.98 | 75.96 | |
| Random Forest (RF) | 89.42 | 89.66 | 89.92 | 90.25 | 90.38 | |
| C&RT | 81.04 | 81.07 | 81.81 | 81.75 | 81.73 | |
| CHAID | 80.98 | 80.93 | 81.02 | 81.11 | 81.15 | |
| Two-Class SVM | 74.55 | 74.62 | 74.55 | 74.81 | 74.83 | |
| LSTM | Iteration | nUnit | Learning Rate | 1st Decay LR | 2nd Decay LR | Number of HN | Accuracy (%) | ||
|---|---|---|---|---|---|---|---|---|---|
| Number | 70/30 | 80/20 | |||||||
| 1 | 500 | 64 | 0.01 | 250 | 375 | 128 | 92.70 | 92.66 | |
| 2 | 500 | 256 | 0.001 | 250 | 375 | 768 | 94.77 | 94.80 | |
| 3 | 1000 | 128 | 0.01 | 500 | 750 | 384 | 95.82 | 95.86 | |
| 4 | 1000 | 256 | 0.001 | 500 | 750 | 768 | 96.44 | 96.48 | |
| 5 | 2000 | 64 | 0.01 | 1000 | 1500 | 128 | 96.870 | 96.924 | |
| 6 | 2000 | 128 | 0.001 | 1000 | 1500 | 384 | 98.958 | 98.952 | |
| 7 | 3000 | 128 | 0.01 | 1500 | 2250 | 384 | 97.78 | 97.74 | |
| 8 | 3000 | 256 | 0.001 | 1500 | 2250 | 768 | 98.56 | 98.62 | |
| 9 | 5000 | 128 | 0.01 | 2500 | 3750 | 384 | 97.86 | 97.88 | |
| 10 | 5000 | 256 | 0.001 | 2500 | 3750 | 768 | 98.74 | 98.74 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, J.; Park, S.; Kwon, S.-H.; Ho, C.M.B.; Pyo, C.-S.; Lee, H. AI-Based Stroke Disease Prediction System Using Real-Time Electromyography Signals. Appl. Sci. 2020, 10, 6791. https://doi.org/10.3390/app10196791
Yu J, Park S, Kwon S-H, Ho CMB, Pyo C-S, Lee H. AI-Based Stroke Disease Prediction System Using Real-Time Electromyography Signals. Applied Sciences. 2020; 10(19):6791. https://doi.org/10.3390/app10196791
Chicago/Turabian StyleYu, Jaehak, Sejin Park, Soon-Hyun Kwon, Chee Meng Benjamin Ho, Cheol-Sig Pyo, and Hansung Lee. 2020. "AI-Based Stroke Disease Prediction System Using Real-Time Electromyography Signals" Applied Sciences 10, no. 19: 6791. https://doi.org/10.3390/app10196791
APA StyleYu, J., Park, S., Kwon, S.-H., Ho, C. M. B., Pyo, C.-S., & Lee, H. (2020). AI-Based Stroke Disease Prediction System Using Real-Time Electromyography Signals. Applied Sciences, 10(19), 6791. https://doi.org/10.3390/app10196791





